MANAGEMENT OF THE ARTHRITIC JOINT
– JOINT RECONSTRUCTION, ARTHRITIS, AND ARTHROPLASTY > General >
CHAPTER 99 – MANAGEMENT OF THE ARTHRITIC JOINT
disabled by arthritis. Although arthritis has many causes, the common
end result is deterioration of joint surfaces and progressive loss of
joint function. The cause determines the clinical characteristics and
the rate of deterioration for a given arthritic condition. Septic
arthritis is often characterized by rapid deterioration, but primary
osteoarthritis is characterized by a slow, insidious deterioration.
arthritis is enormous. Musculoskeletal diseases account for more than
40% of all patients referred for vocational rehabilitation. Arthritis
is the second most frequent cause of outpatient complaints among
patients with chronic diseases. Musculoskeletal diseases account for
20% of all Medicare hospital costs. The number of days of work lost
annually as a result of rheumatoid arthritis and osteoarthritis is
staggering.
arthritis and their families face is accepting that the disease is
chronic, with little likelihood of spontaneous remission. People with
arthritis must live with their disease, because they will not die of
it. Therefore, accurate diagnosis and early appropriate comprehensive
management are critical.
arthritis were identified. We now recognize more than 100 causes.
Although we may congratulate ourselves on the tremendous advances in
diagnosis and treatment of patients, we have only begun to scratch the
surface. Answers to the management of arthritis are likely to remain
elusive in the near future.
patients who need more intensive treatment than others and the patients
who are more likely to develop functional disability. Involvement with
social services or peer support groups and consultation with other
disciplines are crucial to the care of the patient. Do not allow a
patient to become seriously functionally disabled before suggesting
vocational rehabilitation. Several identifiable work factors are
important
in maintaining employment. The most important factor is having the
autonomy to control the pace and content of work activities.
Accessibility of the workplace is also an important consideration. We
tend to lose sight of the young mother with arthritis and morning
stiffness who is unable to dress her children for school, of the worker
who loses his job because of recurrent absence, and of the marital
breakdowns that are almost twice as frequent among arthritis patients
as in the general population. The financial and social hardships are
substantial.
management plan that addresses specific medical measures to control the
arthritic process. Include the use of appropriate regimens of rest,
exercise, and the various available physical and surgical modalities to
relieve pain and maintain musculoskeletal function. If appropriate,
encourage the use of assistive devices to further these goals and allow
the patient to remain as independent as possible.
education of the patient about the disease process, the modalities of
treatment, and the principles of joint protection and energy
conservation. Many educational pamphlets and books are available from
the Arthritis Foundation (4,29,67,22).
If the patient understands the process and rationale for treatment, he
or she is more likely to comply with the therapeutic regimen. Provide
information about reasonable therapeutic goals and limitation of
activity according to the patient’s functional level. Suggest suitable
modifications of the living and working environments and tasks.
Relatively minor physical modifications may make major differences in
the patient’s independence.
low-inflammatory or high-inflammatory types. Patients with the
low-inflammatory type have low leukocyte counts in the synovial fluid
and laboratory findings consistent with low-level inflammatory
activity; the affected joint often shows focal degeneration. Those with
the high-inflammatory type have high leukocyte counts in the synovial
fluid, laboratory findings consistent with high-level inflammatory
activity, and usually show a more diffuse degeneration of the involved
joints (Table 99.1).
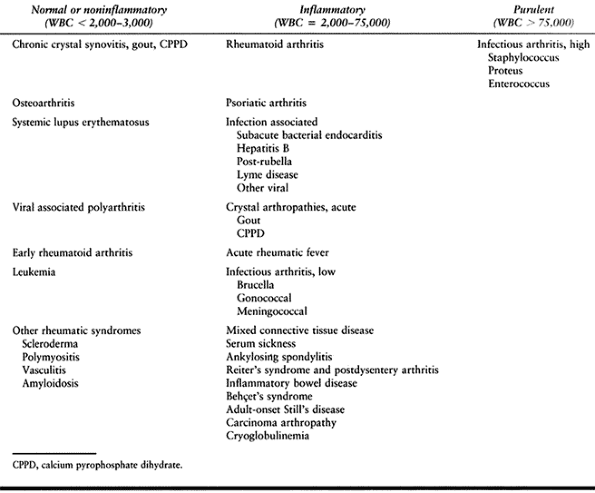 |
|
Table 99.1. Interpretation of Synovial Fluid Findings in the Setting of Undiagnosed Arthritis
|
primary osteoarthritis, produced by intrinsic degeneration of articular
cartilage, and posttraumatic arthritis. The classic type of
high-inflammatory arthritis is rheumatoid arthritis. Other types
include gout, arthritis of psoriasis, lupus erythematosus, ankylosing
spondylitis, arthritis associated with bacterial infection (11),
Reiter’s syndrome, and arthritis of ulcerative colitis. There are some
articular diseases that fit into neither category and that have unique
characteristics, such as aseptic necrosis, “frozen” shoulder and other
joint-stiffening conditions, as well as neuropathic joints.
joints. The pain may arise from soft tissues about the joint that are
under tension or muscles that are in spasm, or from subchondral bone
that is undergoing destruction as a result of the arthritic process.
Other common and significant symptoms and signs of arthritis are loss
of joint motion, instability of joints, and deformity. Many of the
normal components of gait are significantly altered, including walking
speed, step length, cadence, lateral motion of the pelvis, pelvic tilt,
and transverse rotation of the pelvis.
condition vary with the stage of the disease, and often these changes
do not differentiate specific causes. Low-inflammatory and
high-inflammatory arthritis may show chronic inflammation of the
synovium, diffuse articular cartilage damage with fissures and
subchondral cysts, and pannus extending across the articular surface.
The pathology report often reads, “compatible with, but not diagnostic
of, high-inflammatory arthritis.”
that is associated with the immune response. Antibodies produced by
lymphocytes and plasma cells of the synovial membrane combine with
antigens in the synovium (i.e., locally produced and altered IgG or an
unknown antigen, “X”). In systemic lupus erythematosus,
desoxyribonucleic acid (DNA) antigens are the most important finding.
Some or all of these complexes may fix or activate complement, causing
chemotactic substances to be produced. Ingestion of complexes by
polymorphonuclear leukocytes leads to vacuole formation and release of
lysosomal enzymes, which cause the destruction of articular cartilage
and cell death.
biochemical level is thought to be enzymatic degradation of the
articular cartilage (36). In the various types
of arthritic conditions, there is a decrease in the concentration of
chondroitin sulfate, and the existing chondroitin sulfate has a
decreased chain length. The enzymes thought to be responsible are
hyaluronidase, which breaks down mucopolysaccharides, and collagenase,
which breaks down proteins such as collagen.
cartilage degradation and may be found in the synovium, the synovial
fluid polymorphonuclear cells, or the chondrocytes themselves. With the
breakdown of matrix components, the production of new components by the
cells
increases
in an attempt to repair the damage. With disease progression, however,
the balance favors articular cartilage degradation. The mechanical and
lubricating functions of cartilage are lost, and joint collapse
progresses (7,50,75).
arthritis, IgG, IgM, and IgA levels are elevated in the synovial fluid.
Rheumatoid factor, an IgM (19S) antibody that reacts with degraded IgG
(7S) immunoglobulins, is found in 70% to 80% of adults with rheumatoid
arthritis. For this reason, arthritis is considered one of the immune
complex diseases (80). Rheumatoid factor is not
specific to rheumatoid arthritis, because it is also found in
approximately 25% of patients with systemic lupus erythematosus,
scleroderma, and polymyositis. If this factor is found in high titer,
however, it is characteristic of rheumatoid arthritis; usually the
serum and synovial fluid levels of the factor are correspondingly
elevated.
A given arthritic condition, such as rheumatoid arthritis, usually
creates a characteristic clinical picture that is not difficult to
differentiate from other types of arthritis. The problem of diagnosis
arises when the presenting symptom of a patient with arthritis is an
acutely swollen joint or joints. A history of trauma at this point is
often helpful
for
diagnosis of the condition, but if such a history is lacking, the
diagnosis is best approached by turning to radiological and laboratory
examinations.
low-inflammatory osteoarthritis, arthritis secondary to trauma, or
other conditions in which normal joint mechanics have been disrupted
are the irregular narrowing of the joint surface and the appearance of
osteophytes (Fig. 99.1). The radiograph is
characterized by hypertrophic changes about the joint rather than the
atrophic changes seen in high-inflammatory types of arthritis. It is
common for cysts to form along the weight-bearing surfaces in the lower
extremities. It is rare that a patient’s presenting symptom is an acute
attack of arthritis in a joint affected with osteoarthritis, unless he
or she had a fall or other traumatic episode that aggravated a
pre-existing abnormality. In these cases, a radiograph of the joint is
helpful in determining the contribution of degenerative joint disease
to the traumatic episode.
 |
|
Figure 99.1. A:
The drawing depicts degenerative arthritis, which is characterized by focal narrowing of the surface cartilage with subchondral sclerosis on each site of the narrowing. Occasionally, there are subchondral cysts in this area. B: The radiograph shows a cyst in the acetabulum of a hip with degenerative arthritis in a 77-year-old female. |
high-inflammatory arthritis (i.e., rheumatoid arthritis, septic
arthritis, and gout) include diffuse narrowing of the entire joint
surface and the appearance of periarticular cysts (Fig. 99.2).
The cysts are thought to be caused by erosion from the inflamed
synovium at its reflection near the insertion of the joint capsule. The
margins of the cysts are often “fuzzy” during the acute stage and
sclerotic during the chronic stage. The uniform narrowing of the joint
space is thought to be due to enzymatic digestion of the entire
cartilage surface. Another radiographic feature common to
high-inflammatory types of arthritis is osteoporosis of the bones near
the joints.
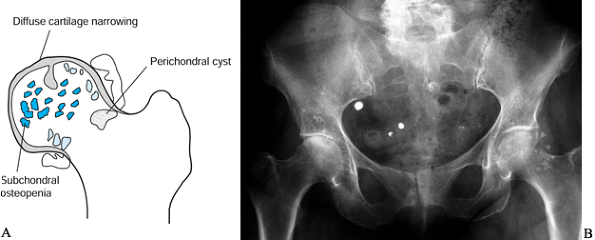 |
|
Figure 99.2. The drawing depicts a high-inflammatory arthritis, which is characterized by diffuse narrowing of the entire joint surface. A: Occasionally, periarticular cysts are seen near the reflection of the synovium. B: The radiograph shows these changes in a 65-year-old woman with rheumatoid arthritis affecting the right hip.
|
evaluation of the patient with the first episode of an acutely painful
joint is arthrocentesis and synovial fluid analysis. The indications
and contraindications for arthrocentesis are illustrated in Table 99.2.
The technique of arthrocentesis involves infiltration of the skin with
a local anesthetic by using a 25-gauge needle, followed by introduction
of a 20-gauge needle into the joint. Joints that contain large amounts
of fluid are the most successfully aspirated, but even these joints may
have hypertrophic synovial folds that can block the needle tip,
resulting in an unsuccessful aspiration. Approaches to various joints
for arthrocentesis are illustrated in Figure 99.3.
 |
|
Table 99.2. Indications and Contraindications for Arthrocentesis
|
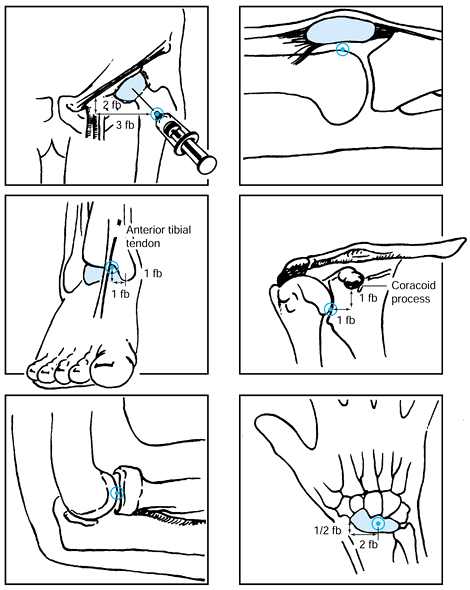 |
|
Figure 99.3.
Sites for introduction of a needle for arthrocentesis of various joints. Some joints are more difficult to aspirate (such as the hip, shoulder, elbow, and ankle) and should be examined with fluoroscopy. The needle is introduced into the subcutaneous tissue, and the fluoroscope is used to ensure that it is on target. |
but synovial biopsies and cartilage biopsies are often not diagnostic.
A few exceptions to this principle are synovial biopsy in tuberculosis
or sarcoidosis, which show the familiar Langhans’ giant cells and
central fibrinoid necrosis; a synovial biopsy in coccidioidomycosis
that demonstrates the characteristic endospore; and a synovial biopsy
from pigmented villonodular synovitis that differentiates this tumorous
condition from arthritis.
laboratory tests: gross appearance and the “string” test, mucin clot,
leukocyte count and differential, microscopic examination of a wet
preparation, polarized light examination, compensated polarized light
examination, Gram stain examination, glucose content, and culture and
sensitivity tests. Compare the glucose value of the synovial fluid with
that of the serum glucose levels. These tests
often confirm the diagnosis and can be carried out with only a few drops of synovial fluid (Table 99.3).
Gout can often be diagnosed by the finding of negatively birefringent
crystals in the fluid; pseudogout is characterized by positively
birefringent crystals; and infection can be diagnosed by the
identification of bacteria by Gram stain.
 |
|
Table 99.3. Categories of Joint Fluid and Disease Associations
|
adult rheumatoid arthritis patients. It is rarely positive in juvenile
rheumatoid arthritis. The lupus erythematosus test demonstrates a
polymorphonuclear cell filled with antinuclear antibody (ANA)
complexes. More frequently used tests are the fluorescent ANA tests,
the results of which are classified as homogeneous, shaggy, or
speckled. Homogeneous, the most common ANA pattern, is seen primarily
in lupus erythematosus but occurs in other diseases as well; shaggy
(peripheral or rim) is more specific to lupus erythematosus and is
often associated with increased disease activity; speckled is
characteristic of mixed connective tissue disease. In lupus
erythematosus, the titers are higher than those in other rheumatic
conditions.
with ankylosing spondylitis, 90% have the gene for the HLA-B27 antigen,
a histocompatibility complex antigen controlled by a gene on chromosome
6. Other arthritic conditions, such as the arthritis of inflammatory
bowel disease, appear to have an increased association with a positive
HLA-B27 test if the arthritis is localized to the spine.
arthritis. However, if the history, physical findings, radiographic
findings, and synovial analysis does not reveal the diagnosis, consider
a synovial biopsy.
nonsurgical and surgical approaches. Surgery should not be considered
as a last alternative to nonsurgical treatment but rather as an adjunct
that may be appropriate at any stage in the treatment of the disease.
The treatment goals in arthritis are to prevent and correct deformity,
preserve function, restore function, and relieve pain. The nonsurgical
treatment primarily consists of drugs, physiotherapy, rest, and use of
orthotic devices.
anti-inflammatory drugs (NSAIDs) remain the first line of therapy in
the treatment of arthritis, and they should be administered in a dose
sufficient to control pain and relieve stiffness (14).
Individualized dosage and emphasis on compliance are necessary. These
drugs are best given after meals or after antacids to prevent
gastrointestinal irritation. The most frequent side effects of NSAIDs
are gastrointestinal irritation and bleeding. Gastrointestinal bleeding
from NSAIDs is particularly a problem for people older than 60, those
who smoke, and those with a history of gastrointestinal ulcer. All
COX-1 NSAIDs can potentially induce gastrointestinal bleeding.
Drug Administration has approved two new NSAIDs that are selectively
inhibitory for cyclooxygenase-2 (COX-2). It was discovered
approximately 10 years ago that there were two forms of cyclooxygenase.
Both forms were inhibitory for the production of prostaglandins and,
therefore, could potentially help inflammation. Inhibition of COX-1,
however, also led to the loss of the protective effects of
prostaglandins on the mucous membranes of the gastrointestinal tract,
which predisposed the patient to upper gastrointestinal ulceration.
Inhibition of COX-2 leads to protection from inflammation but does not
produce the harmful side effect of gastric ulceration. Until recently,
all NSAIDs have been COX-1 inhibitors. The first two of the new class
of drugs, celecoxib and rofecoxib (44,70),
became available in 1999. Celecoxib, in particular, is indicated in
both osteoarthritis and rheumatoid arthritis and appears to spare the
GI tract. It also does not inhibit platelet function. The use of
Celecoxib has changed clinical practice and has made the use of COX-2
inhibitors a standard of care.
as oral agents designed to stimulate aggrecan formation as well as
hyaluronic acid formation. Aggrecan is the major proteoglycan (PG) in
cartilage. It has a long protein core and chondroitin sulfate and
keratin sulfate sidechains attached to it. Hyaluronic acid (hyaluronan)
is made of alternating acetylglucosamine and glucuronic acid building
blocks. It is the core molecule that aggrecan binds to through the link
protein, forming the large PG molecule. It is thought that oral
administration of the building blocks chondroitin sulfate and
glucosamine will stimulate increased formation of the larger molecules.
The glucosamine molecules reach the cellular machinery of the
chondrocyte without being altered by intestinal absorption, while the
chondroitin sulfate preparations undergo partial degeneration. In vitro
studies (tissue culture) have shown that both chondroitin sulfate and
glucosamine will stimulate glycosaminoglycan (GAG), PG, and collagen
synthesis. In vivo studies have not
demonstrated an anti-inflammatory effect on the cyclooxygenase system
or the prostaglandin generation of metalloproteases, and there is
little effect on bradykinin, serotonin, or histamine-mediated
inflammation. However, there appears to be blockage of leukocyte
esterase, hyaluronidase, and superoxide radical generation. Thus, these
drugs might be considered “anti-reactive” as opposed to
anti-inflammatory (21).
and efficacy of glucosamine sulfate. In one study, 80 patients with
focal or general osteoarthritis were randomized to glucosamine 500 mg
three times daily versus placebo for 30 days (14).
Symptoms were reduced in 72% of patients in the glucosamine group and
36% of patients in the placebo group. Improvement was noted in most by
20 days. Another study of 24 outpatients with osteoarthritis showed
significant improvement in the scores for joint pain, tenderness, and
swelling in 80% of patients in the glucosamine group versus 20% of
patients in the placebo group (61).
Two hundred inpatients were randomized to glucosamine 500 mg orally
three times daily versus ibuprofen 400 mg orally three times daily for
4 weeks. No other analgesics, NSAIDs, or corticosteroids were allowed.
Efficacy was measured by Lequesne’s severity index and global
assessment. Ibuprofen response was faster: 48% responded within 1 week,
compared with 28% of the glucosamine treated groups. It should be noted
that it takes 1 to 2 months for glucosamine sulfate to take effect. The
overall response rate was equal: 52% versus 48%. Lequesne’s severity
index improved equally: ibuprofen (severity index = 16) to glucosamine
(severity index = 10), respectively. Adverse effects were significantly
higher in the ibuprofen group (35% ibuprofen versus 6% glucosamine),
and the adverse event–related dropout rate was 7% for ibuprofen and 1%
for glucosamine. Similar results were found in another study (47).
extensively. In a trial comparing chondroitin sulfate (400 mg three
times daily) with diclofenac (50 mg three times daily), adverse
responses were few and equal in both
groups (55).
The response to diclofenac was prompt but was not sustained after
withdrawal. The response to chondroitin sulfate response was slower,
but ultimately greater and sustained 3 months after withdrawal.
rheumatoid arthritis. Chrysotherapy requires careful supervision
because of the possible side effects of nephrotoxicity, blood
dyscrasias, and gold allergy. Gold can be administered parenterally or
orally. Methotrexate is becoming widely used for severe rheumatoid
arthritis, and its use requires monitoring of blood counts and liver
function tests.
(e.g., prednisone). In rheumatoid arthritis, 5 to 10 mg of prednisone
daily in divided doses can give good relief from pain, swelling, and
inflammation. At these low levels, the side effects of cataracts,
decreased resistance to infection, poor wound healing, psychological
consequences, avascular necrosis, and osteoporosis are reduced. High
dosages, such as 40 to 60 mg daily, are reserved for the acutely ill
with life-threatening rheumatic flares. Lowering of high dosages should
be attempted as soon as possible and may require concomitant use of
other anti-inflammatory or antimetabolite drugs. Extremely close
supervision of drug administration and side effects is required in
seriously ill patients. Steroids should be administered only if other
drugs have failed and then for as short a period of time as possible.
severe rheumatoid arthritis is Enbrel (Immunex, Seattle, Washington),
which is a soluble, injectable tumor necrosis factor-α receptor that
has been engineered to resemble human IgG1. Patients with moderate to
severe rheumatoid arthritis self-administer 25 mg two times per week.
The responses in some patients have been dramatic, particularly in
those patients who have failed with other disease-remitting agents. It
is expected in the next several years that similar products will
likewise be approved. The overall goal is to selectively down-regulate
the inflammatory response at the molecular level.
now been studied in a double-blind fashion. There are two preparations
now available, hylan G-F20 (Synvisc, Biomatrix, Richfield, New Jersey),
and hyalectin (Hyalgan, New York, New York); both are processed from
rooster combs. Synvisc has a molecular weight of 6 million and Hyalgan
has a molecular weight of 730,000, as compared with naturally occurring
hyaluronic acid with a molecular weight of 10 million. Because of the
difference in molecular weight, it is recommended that Synvisc be given
three times, 1 week apart; and Hyalgan be given five times, 1 week
apart. Both Hyalgan and Synvisc have been shown to be significantly
better than saline controls (1,13,45,46).
The functional improvement was noted within 2 months after injections
and was sustained for at least 1 year. No significant difference was
noted in radiographic progression.
significant difference at 12 weeks, but there was significant
improvement of Synvisc over the anti-inflammatory drugs by 26 weeks (2).
It was noted that Synvisc plus NSAIDs were superior to Synvisc alone or
NSAIDs alone. Finally, a study comparing Synvisc to intra-articular
steroid injections showed no significant difference by 6 months (39).
They often are helpful in the early rehabilitation of an acute
rheumatic flare. They also provide temporary relief of an acute flare
of chronic synovitis. They should not be used more than two or three
times per year, and at least 2 weeks should pass between repeat
injections. If there is a question of infection, they should not be
used, and the results (particularly the culture) of the synovial
analysis should be examined before a steroid injection is given. The
main limitation of repeated local steroid injection is the risk of
infection and destruction of articular cartilage, tendon, or ligaments.
They should never be injected directly into a tendon, for example, when
treating patella tendonitis, achillis tendonitis, or rotator cuff
tendonitis, but rather into the tendon sheath around the tendon.
pain, and are not capable of significantly increasing deep tissue
temperatures or local circulation. Superficial heat or localized cold
may relieve pain sufficiently to permit exercises. Therapeutic
exercises are designed to increase muscle strength, reduce joint
contractures, and maintain range of motion.
loading exercises that compress the joint. For this reason, the
majority of muscle-strengthening exercises are best done isometrically
in a position of the joint that does not cause pain. On the basis of
clinical experience, we have decided that if an activity or exercise
produces pain that lasts for longer than 10 to 15 minutes after the
activity, the activity is not advised. Passive range-of-motion exercise
within pain tolerance is acceptable, but forceful, painful stressing
must be avoided. Assisted and active range-of-motion and isometric
muscle-strengthening exercises are highly recommended. Swimming,
adaptive physical education, and activities of daily living are
sometimes more appealing to the patient than a boring, structured
exercise program.
periods are essential. Resting with removable splints or braces that
permit limited function of the limb may prevent deformity that would
otherwise occur as a result of pain. Resting night splints may be
applied to stretch out contracted joints, if the deformity is not too
severe. All splints and other orthotic devices must be easy to apply
and remove to permit continuation of the exercise program and, in
conjunction with rest, to relieve pain and correct or prevent
deformity. Complicated dynamic braces are of little value.
Wedging of cylinder casts to overcome flexion deformity is usually ill
advised. The use of orthotic shock absorbers in shoes can decrease
joint impact in the lower extremity by as much as 40% (78).
New developments in continuous passive motion devices appear promising
for improving joint motion and function after surgery and in the
nonsurgical treatment of injuries (66).
procedures to determine whether the problem is due to tendon
contractures, ligament or capsular contractures, bony deformities, or
joint surface deterioration. Also important, consider the social
disabilities suffered by the patient: What is it the patient cannot do
that he or she would like to be able to do? After considering these
factors, devise the treatment plan. Particularly in late-stage disease,
surgery often can help improve the arthritic patient. Rarely can a cure
be obtained.
categories: soft-tissue procedures and bone and joint procedures. The
soft-tissue surgeries include synovectomy, capsulotomy and
capsulectomies, tendon transfers, and other tendon procedures. The bone
and joint procedures include arthroplasty, osteotomy, arthrodesis,
excision of osteophytes and loose bodies that cause locking or
mechanical joint damage, articular resection, chondroplasty to
stimulate repair fibrocartilage, and biologic resurfacing using
autograft or allograft cartilage. These techniques are discussed in Chapter 70 , Chapter 71 and Chapter 72 (Hand), Chapter 86 (Chondral Injuries) Chapter 101, Chapter 102, Chapter 103, Chapter 104, Chapter 105, Chapter 106, Chapter 107, Chapter 108 and Chapter 109 (Arthroplasty, Osteotomies, and Arthrodesis of the Major Joints), Chapter 117 (Foot), Chapter 125 (Osteonecrosis), and Chapter 153 and Chapter 154
(Spine). Conditions that almost always require surgery include unstable
luxation of the cervical spine, ankylosis of the temporal mandibular
joint with risk of starvation, severe ankylosis of both elbows in
extension, severe deformities of the hips and knees, and deformities
that cause severe compression of nerves or imminent or actual tendon
ruptures. Table 99.4 summarizes the common surgical procedures and their indications.
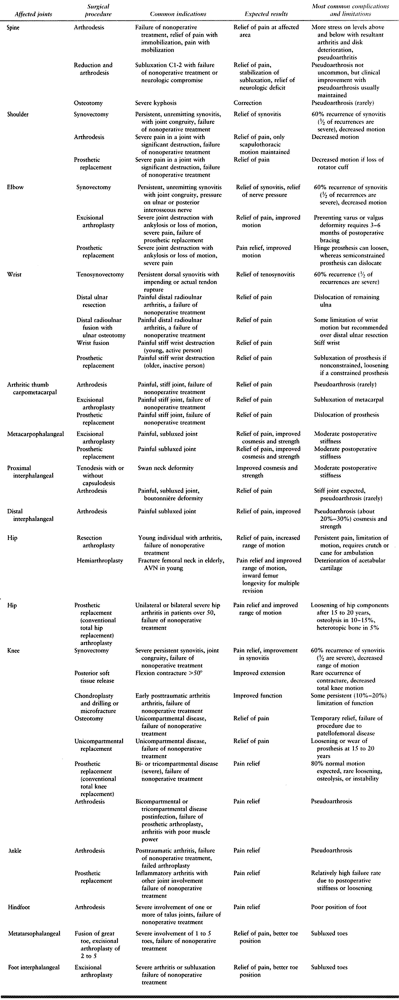 |
|
Table 99.4. Surgical Procedures Commonly Used in the Treatment of Arthritic Conditions
|
-
It is characterized by progressive loss
of articular cartilage, appositional new bone formation in the
subchondral trabecular bone, and formation of new cartilage and new
bone at the margins (osteophytes). -
Clinical features can include pain in the
involved joint, which is frequently aggravated by activity and relieved
by rest. Stiffness after periods of immobility is common. -
Advanced stages are characterized by enlargement of the joint, instability, limitation of motion, and functional loss.
from some degree of osteoarthritis. The prevalence increases with age,
and age is the most important predictive risk factor. Osteoarthritis is
a major cause of disability, and the knee is involved more commonly
than the hip. There are also racial differences, with whites having a
higher incidence than Chinese, South African blacks, East Indians, and
Native Americans.
of osteoarthritis have significant symptoms; therefore, treatment is
predicated on symptoms rather than on the degree of pathology. The
damaged joint may be due to degenerative joint disease due to wear and
tear, or it may be secondary to a previous traumatic episode. There is
some evidence that there is a genetic predisposition (42).
The presence of Heberden’s nodes signifies a predisposition toward the
development of osteoarthritis, and this may potentiate the effects of
local etiologic factors, such as trauma or instability. For example,
patients with Heberden’s nodes who have meniscal tears are more likely
to develop posttraumatic arthritis of the knee after meniscectomy (12). Other predictors of osteoarthritis are obesity, increased bone density, trauma, and repetitive stress (67).
an increase in thickness owing to increased water content (swelling)
and an increase in the net rate of synthesis of PG. This is an attempt
to repair articular cartilage, and may last for years in humans (62,63).
With disease progression, the joint surface thins and the PG content
decreases. Progressive fibrillation of the cartilage occurs, and
eventually, the underlying bone is exposed. There is increased bone
formation in the subchondral bone, and this leads to sclerosis that may
be seen radiographically. Appositional growth of bone at the joint
margins leads to osteophytes, or “spurs.” Spurs, along with thickening
of the joint capsule, leads to limitation of motion.
After the initial attempts at repair with increased synthesis of
collagen, PG, and hyaluronan, the catabolic activity at the biochemical
level becomes high. Lysosomal proteases (cathepsins) and neutral
metalloproteinase (such as stromelysin, collagenase, and gelatinase)
account for much of the loss of cartilage. The concentration of
collagenase increases with advancing disease, and matrix collagen
decreases. Similarly, despite an increase in hyaluronan synthesis,
there is a reduction in hyaluronan. A specific hyaluronidase has not
been identified in cartilage, but several lysosomal enzymes can lyse
hyaluronic acid and chondroitin sulfate. The cartilage loses aggrecan (49),
which results in a loss of compressive stiffness and elasticity as well
as an increase in fluid permeability. This may be due to a deficiency
in link protein. The cells in osteoarthritic cartilage divide more
actively than in normal cartilage, and the resultant cells are very
metabolically active. However, the new cells do not produce a normal
extracellular matrix due to biochemical deficiencies, which leads to
further cartilage deterioration. Tissue inhibitors of metalloproteinase
and plasminogen activator inhibitor can be secreted by chondrocytes to
inhibit the degenerative process, but the balance appears in favor of
the degradative enzymes.
the symptoms remain localized to a joint. Clinical correlation of
patient complaints with objective findings usually show a positive
correlation, but the discrepancy between symptoms and pathological
findings may be striking. The findings are usually local and may or may
not be bilateral. There is progressive loss of motion and pain in the
joint with physical activity, and the pain is usually relieved by rest.
Acute inflammatory flares may be precipitated by trauma or exercise.
The entire joint will be swollen, tender, and stiff. After the acute
flare resolves, the tenderness will be localized to the area of maximum
joint space narrowing. The joints most frequently involved are the
hands, knees, hips, feet, and spine. The distal interphalangeal joints
of the hands have characteristic spurs and lateral deviations called
Heberden’s nodes.
are performed to rule out other arthritides. The erythrocyte
sedimentation rate is normal in most patients, and the synovial fluid
white cell count is less than 1000/mm3.
knee, with relatively minor changes seen at arthroscopy. The end-stage
changes are characterized by joint space narrowing, subchondral bony
sclerosis, marginal osteophyte formation, and cyst formation (Fig. 99.4
demonstrates a shoulder with ostoarthritis). A variant form of
osteoarthritis, erosive inflammatory arthritis, involves primarily the
distal or proximal interphalangeal joints of the hands (16). Painful inflammatory episodes lead to deformity and ankylosis, but the end-stage disease frequently becomes asymptomatic.
 |
|
Figure 99.4. A radiograph showing osteoarthritis of the shoulder. Note the subchondral sclerosis and marginal osteophyte formation.
|
straight forward, atypical presentations and osteoarthritis secondary
to other conditions can lead to diagnostic difficulties. Such atypical
presentations include the occurrence of osteoarthritis in joints
infrequently involved, such as the elbow; the presence of
osteoarthritis associated with a significant degree of inflammation,
such as erosive inflammatory arthritis of the hands; or osteoarthritis
associated with crystal deposition disease, such as the pyrophosphate
of pseudogout.
therapy that have been outlined earlier. Many patients are overweight
and require weight loss for successful treatment. Corticosteroids
should not be given on a long-term basis. The likelihood of fixed
deformity is much less in osteoarthritis than in the high-inflammatory
types of arthritis. The surgeries outlined for arthritis in general
apply to osteoarthritis (Table 99.4). The most
common operations performed for the hip and knee are total joint
replacements. Osteotomies to change the mechanical axis of weight
bearing are useful for unicompartmental arthritis in the knee (76).
Unicompartmental arthroplasty of the knee should be strongly considered
in these cases as well. Another joint that most commonly requires
surgery for osteoarthritis is the carpometacarpal joint of the thumb;
the procedure usually recommended is fusion, although interposition
arthroplasty is commonly performed (see Chapter 70).
It is characterized by chronic systemic erosive synovitis of peripheral
joints and is associated with an elevated rheumatoid factor in the
majority of patients. Associated nonarticular manifestations may
include subcutaneous nodules, vasculitis, pericarditis, pulmonary
nodules and interstitial fibrosis, mononeuritis multiplex,
episcleritis, and Sjögren’s and Felty’s syndromes.
the classification of the American Rheumatism Association, is 1% to 2%
of the population in every part of the world (67).
The incidence increases with age, with 0.3% of the population being
affected younger than 35 years of age and 10% over the age of 65 (67).
The incidence is higher in females than in males, with a ratio of 2.5
to 1. Genetic factors are clearly operative, but they also indicate
that disease penetrance is low and that environmental risk factors play
a significant role as well (54).
Investigations of the etiology have focused on interrelationships of
infectious agents, genetics, and autoimmunity. It is known that
rheumatoid arthritis has a higher incidence in those patients with an
HLA-DR4 locus containing the amino acid sequence common to the DR1,
Dw14, or Dw15 hypervariable region. It has been suggested that the
third hyperavailable regions of the beta chains of HLA-DR4 may
influence the susceptibility to disease by binding arthrogenic
peptides; that they trigger
disease by expanding or deleting particular T-cell populations; or both.
with the Fc portion of the IgG molecule. They are detected in about 3%
of the normal population but are common in high titers in rheumatoid
arthritis. Animal studies have shown that they are found when prolonged
hypergammaglobulinemia is found, such as in chronic infections. They
may help host defense mechanisms by cleaning small antigen-antibody
complexes, but they may secondarily harm host structures by increasing
deleterious inflammation. Certain polymorphysisms of the variable and
constant regions of the rheumatoid factor kappa light chain are
associated with an increased risk of rheumatoid arthritis, indicating
that immunoglobulin genes, in addition to the major histocompatability
locus DR4, may influence disease susceptibility.
tumor-like expansion of stromal connective tissue cells, primarily
fibroblast-like cells and new blood vessels. The fibroblast-like cells
are typically immature and highly invasive (forming a tissue called
pannus). They appear more like transformed cells and express activation
markers such as photo-oncogenes c-fos and c-jun and metalloproteinase
such as collagenase and transin/stromelysin (67,80).
These cells are not malignant but are stimulated by factors such as
platelet derived growth factor (PDGF), fibroblast growth factor (FGF),
Interleukin-I (IL-1), and tumor necrosis factor (TNF) to express the
abnormal phenotype. It appears that the rheumatoid factor containing
immune complexes precipitate out in the superficial layers of cartilage
and stimulate further pannus invasion. The result of the multifaceted
process is continuous pain, progressive deformity and disability.
synovitis. This must be documented by synovial analysis showing a
leukocytosis of 2,000 cells/mm3 to 50,000 plus cells/mm3,
biopsy proven synovitis, or characteristic periarticular erosions on
x-ray study. Another diagnostic feature is the evolution of the disease
process to bilaterally symmetric arthritis.
radiographic finding that is definitive for rheumatoid arthritis.
Rheumatoid factor is present in 85% of patients with rheumatoid
arthritis, and is frequently a predictor of the severe and unremitting
form of the disease. The erythrocyte sedimentation rate is elevated
with flares of the disease, as is the C-reactive protein level.
the first and second year of the disease. The synovitis tends to come
and go following a sine wave pattern, but the structural damage tends
to follow a straight line related to the amount of prior synovitis.
Patients who undergo remission within the first year can become
virtually symptom free. However, once structural damage occurs, there
will be permanent disability.
symptoms due to the structural deformity and recurrent synovitis. It is
important to recognize the difference, because recurrent synovitis is
usually treated pharmacologically, whereas structural deformity
requires activity restriction, or reconstructive surgery. Morning
stiffness (lasting 1 hour or more) is present with inflammatory flares,
and usually disappears when a remission occurs. Structural damage is
characterized by pain that occurs with activity but is relieved by
rest, deformity, and joint space narrowing on radiographs in addition
to periarticular cysts and diffuse subchondral osteopenia (Fig. 99.2).
joints (knees, hips), the small joints of the hands
(metacarpophalangeal joints and proximal interphalangeal joints, but
not distal interphalangeal joints), and the carpal articulations. In
the hands, deformities due to erosion of ligaments are common
(swan-neck deformity, boutonniére deformity, hitchhiker’s thumb).
Shoulder involvement with rotation cuff tears and mechanical
instability are common. In the feet, clawing of the toes and dorsal
subluxations of the metaphalangeal joints are common. The subtalar
joint is also frequently involved, and an everted foot is common. In
the cervical spine, erosions of the transverse ligament of C-1 can
result in subluxation of C-1 on C-2, and eventually superior migration
of C2.
generalized malaise and fatigue are common. Significant involvement of
other organ systems, however, is usually limited to those patients with
rheumatoid factor in the serum. Awareness of complicating conditions
such as rheumatoid nodules and vasculitis, ocular manifestations,
interstitial lung disease, pericarditis, neuropathies related to
cervical spine instability, nerve entrapment, hyperchromic-microcytic
anemia, and Felty’s syndrome are important to be aware of, but
discussion of these conditions is beyond the scope of this chapter.
Further details can be found in larger rheumatoid texts (67).
and most long-term remissions occur within the first 2 years of the
disease. Factors that are predictors for the more severe chronic form
of the disease are the presence of rheumatoid factor, nodules, and the
HLA-DR4 phenotype. Close to 90% of joints ultimately involved in a
given patient are evident on clinical examination during the first year
of the disease (65).
previously outlined apply to rheumatoid arthritis. Soluble gold salts
and methotrexate often give some relief in rheumatoid
diseases but not in other arthritic processes (41).
Corticosteroids have an important place in the treatment of rheumatoid
arthritis. They are often helpful in low doses given over a long
period, a regimen that avoids most of the systemic side effects seen
with high doses. Biologics, such as tumor necrosis factor and receptor,
will be more and more applicable for the treatment of rheumatoid
arthritis. Prevent deformity by using splints on an alternating basis
with range-of-motion exercises. Prescribe rest in the position of
function during periods of acute inflammation and exacerbation of the
disease. The position of function for the upper extremity is with the
elbow at 90°, the forearm across the abdomen, with the wrist slightly
dorsiflexed and the finger joints slightly palmarflexed. The position
of function for the lower extremity is with the hip and knee fully
extended, and the ankle at 90° to the tibia.
erosion, and capsulotomy to increase motion, are used in rheumatoid
arthritis much more frequently than in other arthritic conditions (60).
To be effective, perform synovectomy before significant articular
cartilage damage has occurred. Synovectomy is usually performed in the
shoulder before rupture of the rotator cuff, in the wrist preferably
before and after rupture of the finger or thumb extensor tendons, and
in the knee before loss of articular cartilage and attenuation of the
knee ligaments. Capsulotomy is often used as an isolated procedure,
particularly about the knee to correct surgically joint deformities
that are resistant to bracing and other forms of physical therapy.
Capsulotomies are also used with arthroplasties.
The shoulder, elbow, hip, and knee are the most common joints
undergoing total joint arthroplasty, whereas fusion is most useful in
the wrist and ankle. See Chapter 101 (shoulder), Chapter 102 (elbow), Chapter 70 , Chapter 71 and Chapter 72 (hand and wrist), Chapter 105 (hip), Chapter 107 and Chapter 108 (knee), and Chapter 117 (foot). Distal ankle arthroplasty is becoming more accepted due to new prostheses.
The condition varies in symptoms and severity. The patient may be
asymptomatic and show only mild tenderness at the upper cervical spine
on physical examination, or he or she may have headaches and neck pain.
A cervical collar may give temporary symptomatic relief. Rarely, there
are patients with long-tract neurologic signs in whom spine fusion may
be indicated (see Chapter 154).
arthritis are defined by their extent at presentation: Still’s disease
(systemic onset), polyarticular onset, and pauciarticular onset (67).
All are characterized by chronic synovial inflammation, but the disease
must be present for more than 6 months before subclassification is
possible.
affects 65,000 tp 70,000 children in the United States. Juvenile
rheumatoid arthritis exhibits many of the radiographic features of
adult rheumatoid arthritis, including periarticular osteoporosis,
articular erosions, and joint deformities. Additional features that are
almost pathognomonic for this condition include a periosteal reaction
and joint ankylosis, particularly affecting the apophyseal joints of
the cervical spine. Growth retardation due to involvement of the
epiphysis is a major problem in children with rheumatoid arthritis and
is readily apparent on radiographs.
girls are equally involved, and the onset may be at any age. Spiking
temperatures associated with an evanescent, salmon pink rash may occur
at any time during the day but most often during the late afternoon.
Diffuse lymphadenopathy, hepatosplenomegaly, pericardial effusions, and
pleural effusions are common. Systemic attacks are usually self-limited
and rarely life threatening, and may recur after months to years,
unexpectedly. About 50% of patients develop severe, chronic arthritis,
which continues after systemic manifestations have subsided (19).
40% of children with juvenile rheumatoid arthritis. Malaise and weight
loss are common. Polyarticular involvement may occur at any time and
has a 3:1 predilection for girls. Three fourths of the patients have
systemic involvement.
juvenile rheumatoid arthritis. This group has arthritis affecting four
or fewer joints within the first 6 months of their disease, and about
50% only have one joint involved, usually the knee. Although synovitis
may be chronic, the prognosis for joint function is often good.
Iridocyliditis develops in 10% to 50% of children with pauciarticular
juvenile rheumatoid arthritis. An ophthalmology consult is important.
juvenile rheumatoid arthritis in younger patients. The presence of a
streptococcal infection and positive serologic
tests
for Streptococcus help in making the differential diagnosis. Rheumatic
fever usually is self-limited and has a relatively short course
compared with juvenile rheumatoid arthritis. Differentiating rheumatoid
arthritis from osteoarthritis is rarely a problem, because
osteoarthritis occurs in the older age group and the presence of
Heberden’s node is often helpful in making the diagnosis. The
sedimentation rate is rarely elevated in osteoarthritis. With septic
arthritis, there is usually a single joint involved, and high fever,
leukocytosis, and positive cultures are evident. Systemic lupus
erythematosus may present a difficult diagnostic problem, but the
positive ANA test and lupus erythematosus prep test are characteristic
of systemic lupus erythematosus and are not noted in the juvenile form.
In juvenile rheumatoid arthritis, the test for rheumatoid factor is
usually negative.
patients. ANAs are detected in 40% to 60%. Children who are
consistently rheumatoid factor positive have more erosions, nodules,
and vasculitis. Destructive arthritis occurs in about 50% of those with
rheumatoid factor positive disease as compared with 10% in rheumatoid
factor–negative disease. Radiographs show osteopenia about the affected
joints. There is diffuse narrowing of the joint surfaces, and
subluxation or dislocation may be evident.
relief of symptoms, maintenance of joint range of motion, and muscle
strength. Although juvenile rheumatoid arthritis is often chronic, the
prognosis for most children is good. At least 75% enter long remissions
and have no residual deformity (22).
syndrome (persistent vomiting and mental alterations), although this
usually occurs more commonly when treating a child for fever
accompanying viral infections. Ibuprofen, tolmetin, naproxen, and
fenoprofen are frequently used as alternative treatments. Gold and
hydroxychloroquine are occasionally used as slow-acting therapy in
resistant cases, but steroids are discouraged. An ophthalmology consult
for the treatment of iridocyclitis is important.
arthritis. Total joint replacement may greatly improve joint function
in longstanding diseases but must await full bone growth.
It has been associated with a variety of clinical conditions, such as
Gaucher’s disease, steroid therapy, alcoholism, decompression sickness
(Caisson’s disease), hip dislocation, and fractured femoral neck, but
the exact etiologic mechanism is unknown. There is also a certain group
in which there is no predisposing factor; it is truly idiopathic. The
femoral head is the most common site, but it may occur in the epiphysis
of any long bone. Other terms are avascular necrosis and aseptic
necrosis. The conditions and treatments are discussed in detail in Chapter 125.
crystals of monosodium urate results in one or more clinical
presentations including:
-
Gouty arthritis, which is characterized by recurrent attacks of acute severe or chronic articular and periarticular inflammation
-
Accumulation of gouty tophi in the articular, osseous, and soft tissues
-
Gouty nephropathy, which can lead to renal impairment
-
Uric acid stones in the urinary tract
incidence in the fifth decade. It is the most common inflammatory
arthritis in men over the age of 30 years. It rarely occurs in men
before adolescence or in women before menopause. Hyperuricemia occurs
in approximately 13% of hospitalized adult men (67), but fewer than one in five will develop clinically evident urate crystal deposits.
lack of the enzyme uricase, which makes uric acid soluble in body
fluids, can lead to the crystalline deposition of uric acid. There are
many environmental and genetic influences on uric acid formation,
transport and disposal, including: body weight, diet, lifestyle, social
class, and hemoglobin level. The familial occurrence of gout is well
known. Hyperuricemia occurs in 25% of first-degree relatives of
patients with gout.
joint tissues. The decreased solubility of sodium urate at lower
temperatures explains the predilection of the toes and ears for
deposition. The histopathology of tophi shows a chronic foreign body
granuloma surrounding monosodium urate crystals. The inflammatory
reaction consists primarily of mononuclear cells and giant cells.
asymptomatic hyperuricemia, acute gouty arthritis, and chronic
tophaceous gout. Acute arthritis is the most common early clinical
presentation. The metatarsal phalangeal joint of the great toe is
involved most often and is affected at some time in three quarters of
patients. Other common joints involved include the ankle, tarsal
joints, and knee. Gout usually begins with abrupt onset in a single
joint, often at night so that the patient awakens with severe
unexplained joint pain and swelling. Attacks tend to dissipate
spontaneously in 3 to 10 days without treatment, resulting in
desquamation of the skin over the affected joint. Subsequent episodes
may occur more frequently, involve other joints and persist longer.
the periarticular tissues of the hands and feet. Secondary degenerative
arthritis can develop as a result of erosion of the cartilage and
subchondral bone. Tendons and the carpal tunnel may be involved.
soft-tissue swelling surrounding the affected joint. Later, irregular,
asymmetric soft tissue swelling and calcification of tophi can occur.
Bony erosions tend to be round or oval in shape with a sclerotic margin
and interarticular or periarticular erosions showing a thin overhanging
edge of displaced bone at the margins of the articular cartilage.
which rod- or needle-shaped crystals 3 to 20 µ in size are seen. Under
a polarizing microscope, these show birefringence and bright yellow
crystals parallel to the axis of slow vibration. Synovial fluid
leukocyte counts can vary from 20,000 to 100,000. Serum uric acid
levels may or may not be elevated.
its use remains controversial due to its side effects. Up to 80% of
patients can be expected to experience significant relief of pain
within 48 hours when treated with oral colchicine. Gastrointestinal
toxicity consisting of nausea, vomiting, diarrhea, and cramping
abdominal pain can occur in up to 80% of patients and can be severe,
leading to dehydration and electrolyte imbalance. Intravenous
colchicine avoids the gastrointestinal symptoms and can result in
response within 30 minutes, however, improper use of colchicine has led
to serious toxicity and death.
should not exceed 3 mg and the total cumulative dose for a given attack
should not exceed 4 mg in a total 24-hour period. Do not administer
oral colchicine for at least 7 days after a full intravenous dose.
Reduce the dose in older patients and those with renal or hepatic
disease. Intravenous colchicine is contraindicated in combined renal
and hepatic disease, when the glomerular filtration rate is less than
10 mm per minute or there is extra hepatic biliary obstruction.
first sign of an attack may be successful and are less toxic than
colchicine, but they are not without their gastrointestinal side
effects as well. Many physicians prefer indomethacin for acute gout.
Oral corticosteroids and adrenocorticotrophic hormone can be effective
when colchicine and NSAIDs are contraindicated. Administer 20 to 40 mg
doses of prednisone or its equivalent daily for 3 to 4 days and then
gradually taper over 1 to 2 weeks.
indicated until an established pattern of frequency occurs. One 0.5 mg
colchicine tablet twice daily effectively lowers the frequency of
attacks. Efforts to reduce hyperuricemia are indicated in some
patients. Limit foods with high purine content. Uricosuric drugs such
as probenecid can be given at a dose from 0.5 g per day up to 1 g twice
daily, until a targeted urate level is reached. Common side effects are
rash and gastrointestinal upset. Xanthine oxidase inhibitors such as
allopurinol are useful in patients in whom there is urate
overproduction, nephrolithiasis, or other contraindications to
uricosuric therapy.
the excision of tophi that are interfering with function, threaten to
rupture tendons or erode through the skin, or which have eroded through
skin and become infected. Because of infiltration of the tophaceous
material throughout the connective tissues, excision can be difficult.
Care must be taken to maintain the function of affected structures.
crystals in synovial fluid and on cartilage characterize the condition
called pseudogout. Pathologic surveys indicate that 4% of the adult
population have articular pseudogout at the time of death and that the
incidence increases with age. The incidence of clinically symptomatic
disease is about one half that of classic gout. The male to female
ration is about 1.4:1.
sporadic (idiopathic), or associated with trauma. The hereditary form
is an autosomal dominant variety.
Frequently inflammation will occur early and later manifest as
degeneration. The knee is the most frequent joint presenting with an
acute attack. Trauma may preclude the attack as well as surgery,
similar to gout. About 50% of patients will have progressive
degeneration of multiple joints, with the knees most frequently
involved, followed by the wrists, metacarpophalangeal joints, hips,
shoulders, and elbows. However, most joints with radiologically evident
CPPD calcification are not symptomatic.
densities in articular hyaline or fibrocartilaginous surfaces is
helpful and is called “chondrocalcinosis.” In the early phases, there
is no joint space narrowing or degeneration. The inflammatory response
appears to be related to a dose related response to crystals being shed
from the joint surface. The joint aspirate will show rod-shaped
crystals, frequently in leukocytes, and they will test out with
positive birefringence.
removed from joints. Acute attacks can be treated by aspiration of the
joint and injection of steroids. Whether or not crystalline removal
over time would prevent chronic degenerative joint disease is not known
at this time.
is an arthritic condition characterized by primary involvement of the
sacroiliac joints and spine, leading to a full-blown bony ankylosis of
the entire spine at the end stage of the disease. In approximately 25%
of patients, there is involvement of the proximal joints of the limbs.
It is predominantly a disease of young men, and the cause is unknown.
(about 95%) in patients with the disease, there may be a genetic
predisposition. Making the correct diagnosis is often difficult in the
early stages of the disease, but it is rarely difficult in the end
stage. In the early stages, it may present as a lower lumbar disc
degenerative condition, and there is usually sacroiliac joint
involvement. Another diagnostic feature during early disease is a
decreased chest expansion (<3.8 cm). In end-stage disease, the
sacroiliac joints are fused, and the radiographic appearance of the
spine is that of a complete fusion with a bamboo spine appearance. The
patient often walks in a stooped position and has essentially no motion
in the spine. Rheumatoid factor and serologic tests for other types of
arthritis are usually negative.
iritis, cardiac conduction defects, aortic incompetence, spinal cord
compression, and amyloidosis. The radiographic hallmarks of ankylosing
spondylitis include squaring of the vertebral bodies and the
development of delicate syndesmophytes.
advise patient to sleep flat (without the use of pillows) to help
prevent seriously flexed fusions of the neck. Pharmacologic treatment
is essentially nonspecific, using anti-inflammatory drugs such as
salicylates and NSAIDs. The orthopaedic surgical procedures involve
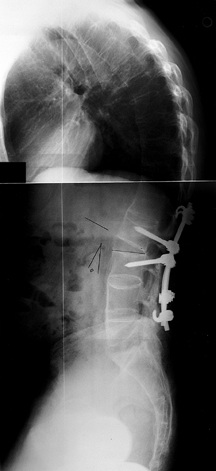
spinal osteotomy in the cervical region and the lumbar region to
correct severe flexion deformities of the spine (Fig. 99.5). These operations are major surgical procedures with considerable risk, and should not be undertaken lightly (see Chapter 153). Hip arthroplasty often is necessary if there is severe hip disease (see Chapter 105).
The possibility of spinal fracture should be excluded in any patient
with advanced ankylosing spondylitis who complains of neck or back pain
after even mild trauma. Computed tomography is helpful in making the
diagnosis.
 |
|
Figure 99.5.
A lateral roentgenogram of the spine after spinal osteotomy in a patient with ankylosing spondylitis. The vertebrae are squared off, and the spine is completely fused (Complements of Munish Gupta, M.D.). |
Fractures involving the joint surfaces that do not heal in an anatomic
position can produce arthritis. If ligamentous injuries do not heal in
a satisfactory manner, a chronically unstable joint results, and the
joint frequently develops degenerative arthritis as a result of chronic
subluxation. In addition, many heritable disorders and developmental
disorders can lead to mechanical malalignment and eventual arthritis
(multiple epiphyseal dysplasia, slipped capital femoral epiphysis,
congenital dislocation of the hips, neuropathic arthropathy,
hemophiliac arthropathy, acromegalic arthropathy, and Paget’s disease
of bone) (68). The histologic changes are
similar to those described for degenerative arthritis. These conditions
can be relatively mild, and conservative measures, such as decreased
activity and decreased mechanical stress, are satisfactory. The
symptoms also frequently occur in the thirties and forties after an
injury in the twenties, but the disability may not be severe at any age.
arthritis, and considerable improvement can be gained.
Anti-inflammatory medication is also important and should be used for
short periods when the joint is relatively symptomatic.
obtaining significant relief for a short period of time (6 months to 1
year). It is recommended as a temporizing procedure until more
definitive procedures are required. Debridement may also be considered
in the older patient who is medically unable to undergo a total joint
replacement, but in whom short term improvement is desired.
debridement and drilling or microfracture through the subchondral bone
of chondral defects. It is the procedure of choice after failed shaving
or abrasion chondroplasty. Many patients gain long-term improvement and
do not require osteotomy, open biologic resurfacing, or total joint
replacement. The commitment is a major one, however, because the
postoperative regimen requires 2 to 3 months of partial weight bearing
and continuous passive motion (CPM) for 6 to 8 hours per day. After the
initial rehabilitation, it is best if the patient gives up running,
cutting, and jumping sports and concentrates on an isometric anaerobic
exercise with bicycling or swimming for aerobic exercise. The surgery
is relatively atraumatic compared with the demanding postoperative
regimen, but only with such a rehabilitation program can a long-term
durable repair be expected.
A modification of the periosteal graft has been described, in which
autologous cultured chondrocytes are injected under the periosteum (6).
Normal joint cartilage is necessary on the other side of the joint if
osteotomy is considered. If the lesion is small or involves a small
joint in the hand, a perichondral autograft or periosteal autograft may
be appropriate. Osteoarticular shell autograft plugs are also
reasonable for small lesions, although their efficiency is not well
proven. This is best in locations where there is little joint space
narrowing or mechanical collapse. The subchondral bone must be intact;
otherwise, an osteoarticular allograft should be considered.
asymmetric mechanical collapse of the joint, an osteochondral allograft
is a good consideration (17,52,53)
This is particularly useful if multiple defects must be grafted in a
joint, requiring a fairly large graft surface. In addition, when the
subchondral bone is disrupted (for example, after a tibial plateau
fracture), an allograft is quite useful. When multiple defects occur in
a joint that is malaligned, then an osteotomy should be performed in
combination with the allograft procedure (see Chapter 9).
knee, and occasionally in the ankle to shift weight-bearing forces from
arthritic areas of the joint to more normal areas. If there is
significant subchondral bone loss in the joint then a shell allograft
should be performed together with the osteotomy, or a prosthetic
arthroplasty performed.
resurfacing procedures for their chondral defects, but their symptoms
are severe. It is not advisable to do a total joint replacement in
young patients, however, a total joint replacement is a predictable
means of providing a joint with minimal pain and adequate stability.
Therefore, it is one reasonable alternative for a patient to choose, as
long as he or she understands that the joint replacement will most
likely wear out or become loose in 10 to 15 years. The patient should
also understand that the scenario of multiple
joint
revisions involves increased risks of surgery and that the longevity of
the subsequent joint revision will decrease. The patient should be
advised that a joint replacement is not an end to the multiple biologic
resurfacing procedures that he or she has been considering, but rather
it is an opportunity to have a decent joint for 10 to 15 years before
having a revision or salvage procedure. The patient is “buying” a good
joint for his or her younger years but accepting the disability of a
fusion or resection arthroplasty during the older years. A second
alternative—and usually the one advised by the surgeon—is to use a cane
and live with the disability during the young and middle years, and put
off having a total joint replacement until the patient is retired. A
third alternative is to have a fusion or resection arthroplasty after
the failure of one or two biologic resurfacing procedures.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
M, Atkinson M, Lussier A, et al. The Role of Viscosupplementation with
Hylan G-F 20 (Synvisc) in the Treatment of Osteoarthritis of the Knee:
A Canadian Multicenter Trial Comparing Hylan G-F 20 Alone, hylan G-F 20
with Non-steroidal Anti-inflammatory Drugs (NSAIDs) and NSAIDs Alone. Osteoarthritis Cartilage 1995;3:213.
Foundation Committee on Evaluation of Synovectomy. Multicenter
Evaluation of Synovectomy in the Treatment of Rheumatoid Arthritis.
Report of Results at the End of Three Years. Arthritis Rheum 1977;20:765.
M, Lindhal A, Nilsson A, et al. Treatment of Deep Cartilage Defects of
the Knee with Autologus Chondrocyte Transplantation. N Engl J Med 1994;331:889.
R, Bayliss MT, Maroudas A, et al. The Composition of Normal and
Osteoarthritic Articular Cartilage from Human Knee Joints. J Bone Joint Surg 1984;66-A:95.
M, Nguyen M, Listrat V, Amor B. High Molecular Weight Sodium
Hyaluronate (Hyalectin) in Osteoarthritis of the Knee: A 1 Year
Placebo-controlled Trial. Osteoarthritis Cartilage 1993;1:97.
A, Bignamini AA, Rovati AL. Therapeutic Activity of Oral Glucosamine
Sulfate in Osteoarthrosis: A Placebo Controlled, Double-blind
Investigation. Clin Ther 1980;3:260.
Y, Masuhara K, Shiomi S. The Effect of High Tibial Osteotomy on
Osteoarthritis of the Knee: An Arthroscopic Study of 54 Knee Joints. Orthop Clin North Am 1979;10:585.
Treatment of Osteoarthritis of the Knee: Glucosamine/chondroitin
Sulfate, Hyaluronic Viscosupplementation, Cortisone Injections. Proceedings of the Knee Society, Interim Meeting, Scottsdale, 1998.
L, Kirsh G, Karpati Z, et al. Arthroscopic Autogenous Osteochondral
Mosaicplasty for the Treatment of Femoral Condylar Articular Defects: A
Preliminary Report. Knee Surg Sports Traumatol Arthrosc 1997;5:262.
ED, Jr. Mechanisms of Disease: Rheumatoid Arthritis Pathophysiology and
Implications for Therapy. N Engl J Med 1990;322:1277.
C, Goldie I, Ryba W. Intertrochanteric Osteotomy for Osteoarthritis of
the Hip: A Radiological Evaluation. Clin Orthop 1972;86:63.
DL, James SL, Larson RL, et al. Proximal Tibial Osteotomy in Patients
Who are 50 Years Old or Less: A Long Term Followup Study. J Bone Joint Surg Am 1988;70:977.
GN, Van der Lindent TJ, Terwindt-Rouwenforst EAW, et al. Repair of the
Articular Defects by Perichondral Grafts: Experiments in the Rabbit. Acta Orthop Scand 1989;60:326.
A, Pattrick M, Doherty S, Doherty M. Intra-articular Hyaluronic Acid
Compared to Intra-articular Triamcinolone Hexacetonide in Inflammatory
Knee Osteoarthritis. Osteoarthritis Cartilage 1995;3:269.
V, Ayral X, Patarnello F, et al. Arthroscopic Evaluation of Potential
Structure Modifying Activity of Hyaluronan (Hyalgan) in Osteoarthritis
of the Knee. Osteoarthritis Cartilage 1997;5:153.
LS, Dalen N, Englund G, et al. Intra-articular Hyaluronan Injections in
the Treatment of Osteoarthritis on the Knee: A Randomized,
Double-blind, Placebo Controlled Multicenter Trial. Hyluronan
Multicentre Trial Group. Ann Rheum Dis 1996;55:424.
Vaz AC. Double-blind Clinical Evaluation of the Relative Efficacy of
Ibuprofen and Glucosamine Sulfate in the Management of Osteoarthrosis
of the Knee in outpatients. Curr Med Res Opin 1982;8:145.
HJ, Dorfman H, Lipiello L. Biochemical and Metabolic Abnormalities in
Articular Cartilage from Osteoarthritic Human Hips II: Correlation of
Morphology with Biomechanical and Metabolic Data. J Bone Joint Surg 1971;53A:523.
LS, Goldstein SA, Malvitz TA, et al. Proximal Tibial Osteotomy: Factors
that Influence the Duration of Satisfactory Function. Clin Orthop 1988;229:193.
AG, Langer F, Pritzker KP, et al. Fresh, Small Fragment Osteochondral
Allografts: Long-term Followup Study of First 100 Cases. Clin Orthop 1985;197:96.
DM. Epidemiology; Rheumatoid Arthritis Etiology, Diagnosis, and
Treatment. In: Utsinger PD, Zvaifler NJ, Erlich GE. Philadelphia: JB
Lippincott Co., 1985:133.
P, Manopulo R, Galati M, et al. Comparison of the Antiinflammatory
Efficacy of Chondroitin Sulfate and Diclofenac Sodium in Patients with
Knee Osteoarthritis. J Rheumatol 1996;23:1385.
J, Llavore E, Ylescupidez F. Double-blind Clinical Evaluation of Oral
Glucosamine Sulfate in the Basic Treatment of Osteoarthrosis. Curr Med Res Opin 1980;7:110.
RB, Hamilton HW, Wedge JH, et al. Clinical Application of Basic
Research on Continuous Passive Motion for Disorders and Injuries of
Synovial Joints. A Preliminary Report of a Feasibility Study. J Orthop Res 1984;1:3.
LS, Weaver AL, Graham DY, et al. Anti-inflammatory and Upper
Gastrointestinal Effects of Celecoxib in Rheumatoid Arthritis: A
Randomized Controlled Trial. JAMA 1999;282:1921.
S, Aoyagi F, Maruyama Y. Free Perichondral Grafting in the Treatment of
Temporomandibular Joint Ankylosis: Preliminary Report. Plast Recontr Surg 1978;61:876.
