MANAGEMENT OF POLYTRAUMA
II – FRACTURES, DISLOCATIONS, NONUNIONS, AND MALUNIONS > General
> CHAPTER 14 – MANAGEMENT OF POLYTRAUMA
associated with blunt trauma. An isolated injury rarely poses any
threat to life, but, when associated with multiple injuries, a
musculoskeletal injury assumes greater significance. Trauma is the
leading cause of death in persons between the ages of 1 and 45 years.
It is estimated that there are 150,000 deaths annually from accidents
alone. The cost in lost years and dollars from death and disability
exceeds that of heart disease, stroke, and cancer combined (1). Trauma remains a major social and economic affliction (2). Proper management can greatly reduce the mortality and morbidity associated with these injuries (6).
field with initial contact by the emergency medical technicians. Their
job is to initially evaluate and, if necessary, resuscitate the
patient; to extricate the patient; and to safely transport him or her
to the appropriate facility. The emergency medical technicians should
obtain a history of the accident to better understand the mechanism of
injury and relate that information to the treating physician. They
should assess the airway and, when properly trained, perform
endotracheal intubation if needed. Although intravenous access is
beneficial, it should not be obtained at the expense of time in
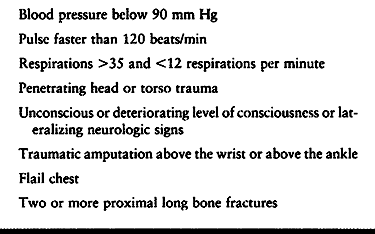
transfer of the patient from the scene to the trauma center (Table 14.1).
 |
|
Table 14.1. Criteria for Automatic Triage to a Trauma Center
|
are often placed in pneumatic antishock garments (PASG). When there is
life-threatening hemorrhage and severe loss of blood pressure, these
garments may be inflated to 100 mm Hg, and the patient is sent
immediately to the trauma center for resuscitation and gradual release
of the PASG. If prolonged use of the garments is necessary, do not
inflate to more than 30 mm Hg because of the increased risk for
compartment syndrome and soft-tissue loss with lower extremity injuries
(7). The PASG has been a good device for
initially stabilizing pelvic fractures, helping to tamponade hemorrhage
with some reduction and stabilization of the pelvic fracture or
separation (12).
the emergency room has been well studied, and protocols have been
developed by the Committee for Trauma of the American College of
Surgeons (6). Their courses on
advanced trauma life support (ATLS) have shown that assessment of the
patient in an orderly fashion has improved the care and reduced the
incidence of missed injuries. Patient management requires rapid primary
evaluation, resuscitation of vital functions, a more detailed secondary
assessment, and definitive care.
establish an airway for adequate oxygenation. In establishing and
maintaining an airway, it is important to control the cervical spine to
avoid iatrogenic neurologic injuries if the cervical spine is unstable.
Examine the trauma patient to be certain that the airway is cleared of
any obstructions, such as foreign objects, loose teeth, blood, mucus,
or vomitus. In the unconscious patient, protect the cervical spine with
longitudinal traction. Keep the mandible elevated to clear the airway
of the patient’s tongue. Take a cross-table lateral radiograph of the
cervical spine as soon as possible to rule out cervical injury that
could be exacerbated with motion. Quickly assess the patient’s ability
to oxygenate by inspecting an arterial blood gas sample to see whether
the arterial blood is red or dark, indicating the state of oxygenation.
exchange. Airway patency does not necessarily mean that the patient is
adequately exchanging oxygen; this can be determined through an
arterial blood gas sample. Inspect for evidence of a flail segment in
the chest with paradoxic movement. Cover and clean open chest wounds
with a Vaseline gauze dressing. If the patient does not appear to be
ventilating adequately (i.e., patient is using accessory muscles in the
neck to help breathe), and the arterial blood gas is dark, perform
endotracheal intubation. If you are not experienced in endotracheal
intubation, use a mask and bag valve device with an oral airway first
to oxygenate the patient. Endotracheal intubation in the trauma patient
can be difficult and should be performed by the most experienced hands.
Causes of inadequate oxygenation must be found. If no flail segments
are visible, palpate the rib cage for tenderness or crepitus caused by
rib fractures.
bilaterally to help rule out a pneumothorax. If no cause is found for
the patient’s inadequate oxygenation, perform bilateral tube
thoracostomy to decompress potential bilateral pneumothoraces.
airway and provide adequate oxygenation for any patient with inadequate
or labored ventilation or flail chest and for patients who are
unconscious and unable to control the airway, those with facial
fractures, multiply injured patients, and those with deteriorating
blood oxygenation. If a cervical spine injury is suspected or has not
been ruled out, perform nasotracheal or fiberoptic intubation with
proper longitudinal control of the head and cervical spine. Oral
endotracheal intubation is preferred because a larger tube can be
placed. Rarely, a surgical cricothyroidectomy may be needed to obtain
access to the airway.
patient until proved otherwise. Shock is caused by and defined as
inadequate oxygen delivery to soft tissues. Assess cardiac output by
palpation of peripheral pulses and observe skin color and capillary
refill. As a general rule, if the radial pulse is palpable, the
systolic blood pressure is 80 mm Hg. The femoral pulse indicates a
pressure of 70 mm Hg, and the carotid pulse a pressure of 60 mm Hg.
Normally, capillary refill requires less than 2 s. A delay of longer
than 2 s indicates hypotension. Additional indicators of hypovolemia
are decreased bicarbonate and acidosis found in the arterial blood gas
samples. Hemorrhagic shock requires rapid fluid resuscitation.
Initially, insert two large-bore angiocaths and give a 2-L bolus of
lactated Ringer’s solution.
to nonhypovolemic shock. Rule out causes of myocardial dysfunction such
as cardiac contusion with arrhythmias or cardiac tamponade or
myocardial infarction. A history of direct blow to the sternum from a
deceleration injury suggests myocardial contusion. The combination of
distended neck veins, decreased arterial pressure, and muffled heart
sounds (Beck’s triad) is diagnostic of a cardiac tamponade.
Electrocardiographic changes may indicate an acute myocardial
infarction. In the patient with a history of cardiac injury, perform
cardiac monitoring and insert a Swan-Ganz catheter. In the patient with
the clinical suggestion of a cardiac tamponade, decompress the
tamponade emergently with pericardiocentesis. Monitor arrhythmias
secondary to myocardial infarction or contusion and manage with
appropriate medication.
pulse, blood pressure, and urine output. Repeat arterial blood gases as
necessary. The effectiveness of oxygenation is reflected through the
oxygen saturation (PO2), and the effectiveness of fluid
resuscitation through the pH and bicarbonate levels. Constantly
reassess the patient to be certain adequate resuscitation and
oxygenation are maintained. Prolonged shock contributes to pulmonary
distress syndrome, hepatic dysfunction, renal failure, gut-origin
septic state, and multisystem organ failure.
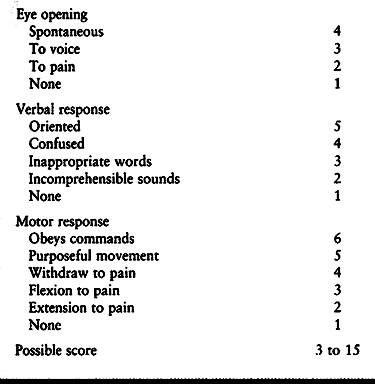
A score may range from 3 to 15, with a score of less than 8 signifying
serious neurologic injury. Repeat determinations of the Glasgow Coma
Scale are helpful in determining changes in the patient’s mental
status. In addition to the Glasgow Coma Scale, evaluate for focal signs
such as unequal pupils and doll’s eyes, which point to an expanding
intracranial lesion.
 |
|
Table 14.2. Glasgow Coma Scale
|
abnormal swelling, instability, or crepitus suggesting musculoskeletal
injury. Perform a careful neurologic examination. Check pulses
bilaterally for any decrease in peripheral blood flow. Perform
arteriography in any patient with major skeletal injury in whom the
distal pulses in the injured limb are weaker than those in the opposite
extremity. Be alert for vascular injury in patients with supracondylar
humerus fractures, supracondylar femur fractures, dislocations of the
knee, and crush injuries of the tibia. Reduce dislocations as soon as
possible, dress open fractures and extremity wounds, and splint
fractures immediately. Splint femur fractures with traction. Begin
appropriate bacteriocidal broad-spectrum intravenous antibiotics in
patients with open fractures.
patient’s level of consciousness with the Glasgow Coma Scale and
pupillary reflexes. Assess rectal tone and perianal sensation. Examine
and palpate the back for swelling and tenderness. Obtain appropriate
spine radiographs. Remember that the cervical spine should be assumed
to be injured and protected until radiographic evidence reveals
otherwise.
injury in the polytrauma patient is to obtain a stable skeleton as
early as possible, given the overall condition of the patient. Once the
patient is properly resuscitated and hemodynamically stable, then
stabilization of the skeleton can reduce the physiologic response to
trauma and lessen the risk of adult respiratory distress syndrome
(ARDS) and multiple system organ failure (2,3,11,17,21).
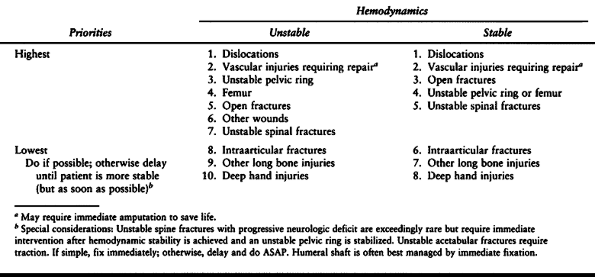
Priorities include external fixation of the anterior pelvis of
hemodynamically unstable patients, reduction of dislocations, repair of
vascular injuries, debridement of open fractures, stabilization of long
bone fractures (especially the femur), and stabilization of the
unstable spine (Table 14.3).
 |
|
Table 14.3. Priorities in the Operative Treatment of Musculoskeletal Injuries in the Multiply Injured Patient
|
external fixators until the soft tissue swelling subsides. Upper
extremity fractures, if not treated definitively at the initial
surgery, can be fixed at a later time.
 |
|
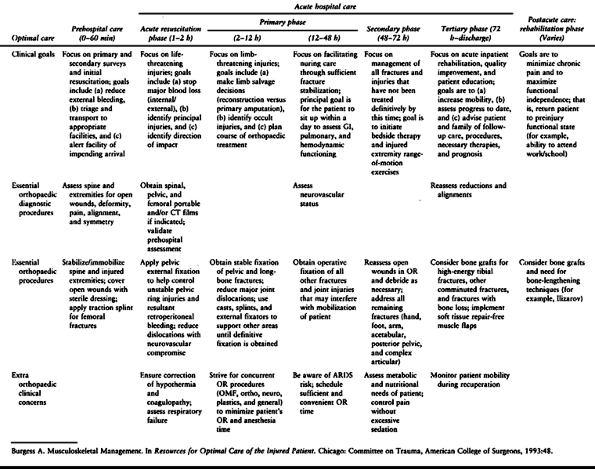
Table 14.4. Care of the Injured Patient with Musculoskeletal Trauma
|
 |
|
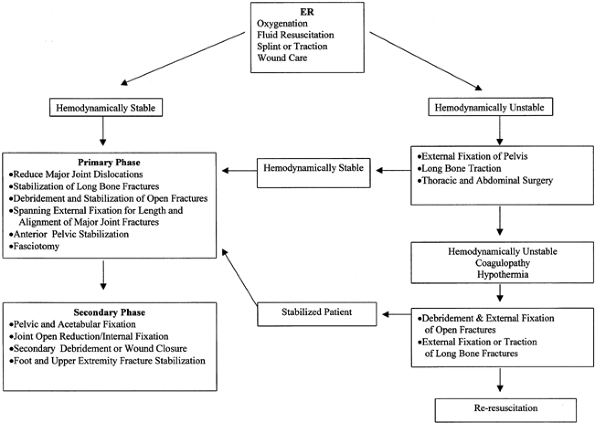
Figure 14.1. Multiple trauma algorithm.
|
hemodynamically unstable should have an anterior external fixator
applied to temporarily stabilize the pelvis and reduce the bleeding
into the pelvis (12). This is an emergency
procedure that should be done before angiography. It can be done in the
emergency department or in the operating room. If possible, it should
be performed on the unstable patient before a laparotomy.
requires prompt management. Although there is some debate about which
should be addressed first, vascular injuries or fractures, I strongly
believe that vascular repair should be performed first. This should be
performed after temporary stabilization of the fracture.
external fixator, a femoral distractor, or with the patient placed in
traction on a fracture table. This will place the fractured bone at
proper length and provide minimal stabilization to the limb for
vascular repairs. Reconstruction of the vascular repair has priority to
reduce the time of ischemic hypoxia to the limb.
develop a compartment syndrome because of systemic hypotension. A high
index of suspicion is needed. Limbs with crush injuries and/or vascular
injuries in patients subjected to prolonged shock with fluid
resuscitation may experience reperfusion injury and require
fasciotomies (20). Although the lower leg and
forearm are the most common places to develop a compartment syndrome,
any closed compartment is at risk. Open fractures as well as closed
injuries may be associated with compartment syndrome.
irrigation, and debridement of devitalized tissue are essential.
Perform immediate stabilization to reduce fracture motion and further
soft tissue damage. Use external fixation or, more commonly now,
unreamed or minimally reamed intramedullary nails to stabilize open
long bone fractures. Periarticular and intra-articular fractures can be
plated or stabilized with tensioned-wire external fixators. Delay soft
tissue closure of traumatic wounds. Grade IIIB injuries should have
soft tissue reconstruction (local or free flaps) within 72 h if
possible (20).
This allows the patient to be mobilized. Patients who exhibit
progressive loss of neurologic function on repeat neurologic
examination should be decompressed and stabilized acutely.
stable, additional fracture management can be addressed: fractures of
the acetabulum or posterior pelvis; closed upper extremity fractures;
and intraarticular fractures. Perform secondary evaluation of open
wounds at this time. Special care needs to be given to those patients
with continued respiratory insufficiency, febrile septic state, and
liver dysfunction. Patients with decreased platelets (less than
180,000), neutrophil elastase greater than 85 ng/dl, and C-reactive
protein greater than 11 ng/dl are at risk of secondary organ failure
with secondary surgery 72 h postinjury (22).
injuries presents a special problem. Most of these patients are
intubated in the field or in the emergency room because of their severe
injuries. It is important to rapidly reverse hypovolemic shock and to
maintain high oxygen transport to reduce further neurologic damage.
Physical examination followed by computed tomography of the head is
needed for diagnosis of the injury. The neurosurgeon treats the patient
with an intracranial lesion that needs decompression in the operating
room under general anesthesia. If neurosurgical decompression is
unnecessary, perform intracranial monitoring through an intracranial
bolt or ventricular catheter. Increased intracranial pressure can be
managed medically with fluid management and osmotic diuretics and by
decreasing the serum carbon dioxide (PCO2) with hyperventilation. If necessary, cerebral spinal fluid can be withdrawn to reduce intracranial pressure (16,19).
spleen, lacerated liver, or aortic arch rupture, the head-injured
patient must undergo general anesthesia. The patient should also
undergo early total care with management of the musculoskeletal system
for open fractures and long bone injuries and timely care of spinal,
pelvic, and acetabular fractures. With proper monitoring of
intracranial pressure, good fluid resuscitation, and oxygen transport,
the patient usually can tolerate the anesthetic for the musculoskeletal
care that is essential for stabilization and early mobilization (18,21).
patient has been shown to reduce the risk of adult respiratory distress
syndrome (ARDS) and respiratory dysfunction as well as to reduce time
on a ventilator, time in the intensive care unit, and cost of care (2,11,17).
Recent research has shown that manipulation of the femoral canal—that
is, entering the proximal canal, placement of a guide rod, reaming and
placement of an intramedullary nail—causes fat and marrow contents to
be released into the venous system and embolized to the heart and lungs
(9,23). There was some
concern that this embolization caused the development of ARDS in those
patients with already compromised oxygenation because of chest injury,
that is, pulmonary contusion (13,14).
How- ever, good animal and clinical studies have shown no increased
ARDS with acute intramedullary nailing of femur fractures in patients
with pulmonary contusion (5,24,25).
They need to be well hydrated and hemodynamically stabilized. Acute
fracture stabilization can be safely performed with intramedullary
nailing. Because there is less embolization with the unreamed femoral
nail, this is the recommended treatment of choice in patients with
pulmonary contusion or other compromise of pulmonary function (3,21).
If the patient is not well oxygenated or hemodynamically stable, then
temporary fracture stabilization with external fixation can be
performed.
surgery for life-threatening injuries of the chest or abdomen, or who
have a coagulopathy or hypothermia, should be taken to the intensive
care unit, resuscitated, warmed, and well oxygenated. With a stable
patient, fracture fixation can proceed as outlined. In critical
situations where the patient is systematically unstable, perform
temporary stabilization with external fixation.
the risk for life-threatening complications such as ARDS and multiple
system organ failure. Protocols need to be developed that include
management of general surgical and neurosurgical injuries, followed by
fracture stabilization. Special considerations have to be made for the
patient with pulmonary contusion or head injuries. These considerations
do not prevent proper stabilization of the skeleton.
early total care can be. (Case of Michael Chapman, M.D., University of
California, Davis, Department of Orthopaedic Surgery, Sacramento,
California.)
high-speed motor vehicle accident. After a prolonged extrication from
her vehicle, she was transported by helicopter to the University of
California, Davis, Medical Center. She was found to be unconscious at
the scene of the accident but subsequently regained consciousness and
had a score on the Glasgow Coma Scale of 15. On arrival in the
emergency room, she was complaining of left-sided chest pain and was
short of breath.
100 over 60, heart rate 158, and respiration 20. She was in shock and
hemodynamically unstable despite efforts at resuscitation. Her abdomen
was swollen and tender throughout. She was intubated in the emergency
room, and a left chest tube was placed for a hemopneumothorax. She had
obvious deformity of all four extremities with wounds on the left upper
and left lower extremities consistent with multiple open fractures. Her
wounds were dressed, and fractures splinted. Further orthopaedic
evaluation and x-rays were not possible because of the patient’s
unstable status. She was rushed immediately to the operating room for a
laparotomy.
liver, laceration of the colon, and a perinephric hematoma. The spleen
was removed, and a partial lobectomy of the liver was performed. The
laceration of the colon was repaired. After the laparotomy she was
hemodynamically stable. Because of the potential for a head injury, she
then had a CT scan of the head, which was negative. She was then
returned to the operating room for orthopaedic evaluation and
procedures.
multiple x-rays revealed a normal cervical, thoracic, and lumbar spine
and the following 10 fractures:
-
Grade II open, somewhat comminuted midshaft fracture of the left humerus (Fig. 14.2).
![]() Figure 14.2.
Figure 14.2.
Anteroposterior x-ray of the left arm, elbow, and forearm showing
fractures of the midshaft humerus, medial condyle of the humerus, and
midshaft radius and ulna. -
Closed fracture of the medial condyle of the humerus (Fig. 14.2).
-
Grade II open transverse midshaft fractures of the left radius and ulna (Fig. 14.2).
-
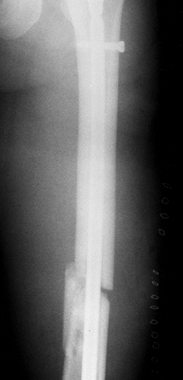
Closed midshaft fracture of the right humerus (Fig. 14.3).
 Figure 14.3. Fracture of the right humeral shaft.
Figure 14.3. Fracture of the right humeral shaft. -
Closed transverse fracture of the distal third of the right ulna (Fig. 14.4).
![]() Figure 14.4. Fracture of the right distal ulna.
Figure 14.4. Fracture of the right distal ulna. -
Grade II open, midshaft, slightly comminuted fracture of the left femoral shaft (Fig. 14.5).
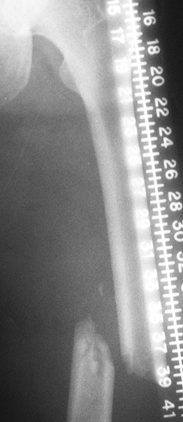 Figure 14.5. Fracture of the shaft of the left femur. Note that no fracture of the femoral neck can be seen.
Figure 14.5. Fracture of the shaft of the left femur. Note that no fracture of the femoral neck can be seen. -
Grade II open, severely comminuted pylon fracture of the left ankle involving the tibia and fibula (Fig. 14.6).
![]() Figure 14.6. Comminuted pylon fracture of the left distal tibia and fibula.
Figure 14.6. Comminuted pylon fracture of the left distal tibia and fibula. -
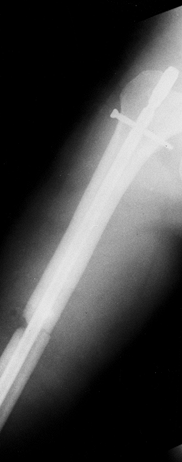
Closed transverse midshaft fracture of the right femur (Fig. 14.7).
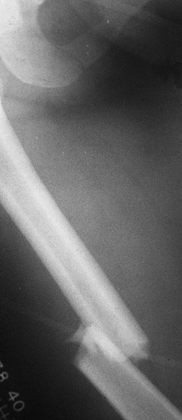 Figure 14.7. Midshaft fracture of the right femur.
Figure 14.7. Midshaft fracture of the right femur. -
Careful examination of both hips and AP
and lateral x-rays in internal rotation showed no evidence of fracture
of the femoral neck. In follow-up, an undisplaced fracture of the left
femoral neck was found and fixed with cannulated screws. -
Pelvic x-rays showed minor pubic rami fractures.
surgeon with a second-year resident and a trauma fellow with a
third-year resident. The patient was on a radiolucent operating table,
and a fluoroscope was available. The patient was rolled into the right
lateral decubitus position, and the left lower and left upper
extremities were operated simultaneously. All of the open fractures
were irrigated and debrided, and the wounds were left open. The
midshaft fracture of the left humerus was double-plated with a 3.7
titanium plating system. The left elbow was opened through a medial
approach, and
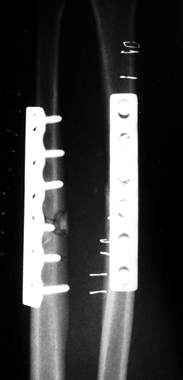
the medial condyle fracture was fixed with two interfragmentary screws (Fig. 14.8). The midshaft fractures of the left radius and ulna were compression plated (Fig. 14.9).
In the lower extremity, the open midshaft femur fracture was nailed
with a nonreamed antegrade femoral nail using open technique (Fig. 14.10).
The proximal cross-locking screw was placed, but distal cross-locking
was not carried out in order to save time. The pylon fractures of the
left distal tibia and fibula were reduced after debridement of the
wound, and the leg was placed in a delta-frame-type external fixator (Fig. 14.11).
 |
|
Figure 14.8. Left humerus and elbow after fixation.
|
 |
|
Figure 14.9. Left forearm after fixation.
|
 |
|
Figure 14.10. Left femur after initial nailing.
|
 |
|
Figure 14.11. Left pylon fracture of the tibia and fibula after external fixation.
|
decubitus position, and simultaneous surgery was carried out on the
right upper and right lower extremities. The humerus fracture was
internally fixed with an antegrade intramedullary nail utilizing closed
technique. The right femur was fixed with an intramedullary nail,
nonreamed, inserted antegrade, with a small exposure of the fracture
site to permit reduction and passage of the nail. Distal cross-locking
was not carried out (Fig. 14.12).
 |
|
Figure 14.12. Right femur after initial nailing.
|
the general surgical procedures until completion of the last
orthopaedic procedure and transfer to the surgical intensive care unit
was 20 h, including the time required to take her to the CT scanner for
examination of her brain.
was extubated on her second postoperative day. Her chest tube was
removed on the third postoperative day. On the fifth day after injury,
she was returned to the operating
room,
where all of her open wounds were redebrided, irrigated, and closed.
Because of segmental deficiency in the left humerus, a bone graft from
the left iliac crest was placed. The distal cross-locking was carried
out on both femoral nails, and the pylon fracture was reduced, closed,
and fixed with two percutaneously inserted cannulated screws (Fig. 14.13).
 |
|
Figure 14.13. Anteroposterior view of left tibia at 6 weeks, at time of removal of external fixator.
|
and rehabilitation on all of her extremities. She was discharged from
the hospital on her ninth postoperative day, transferring from bed to
wheelchair.
her extremities until at least 6 weeks postoperatively. Apparently
through a misunderstanding, the patient began full weightbearing on
both lower extremities and her left upper extremity at about 4 weeks
postinjury. Because of that, she bent the plates in the left humerus
and bent her right femoral nail.
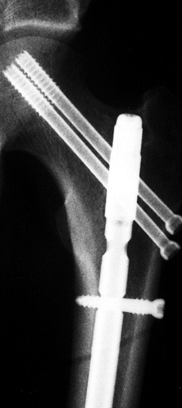
operating room, where plates on the left humerus were converted to a
locked intramedullary nail. The right femoral nail was exchanged for a
statically locked reamed nail. At that time she was complaining of pain
in the left hip. X-rays revealed an undisplaced fracture of the left
femoral neck. This was fixed with percutaneous cannulated screw
fixation anterior to the femoral nail (Fig. 14.14).
There was excellent early callus around the pylon fracture; therefore,
her external fixator was removed, and she was placed in a cast.
 |
|
Figure 14.14. Left femoral neck fracture after screw fixation at 6 weeks, anteroposterior view.
|
extremities and rehabilitating nicely. At 20 weeks she showed delayed
union of the right femoral fracture; therefore, her
nail was dynamized by removing the distal cross-locking screws.
and subsequently married and returned to work. She has excellent
function in all of her extremities with no limitations other than some
minor loss of motion in her left hip and about 50% loss of motion in
her left ankle.
results that can be achieved but also illustrates some of the pitfalls
and complications that can occur in these challenging patients. This
patient was cared for in the early 1990s. Today she would be managed in
the supine position on a radiolucent table with the femur fractures
fixed with retrograde nails and the upper extremity injuries managed
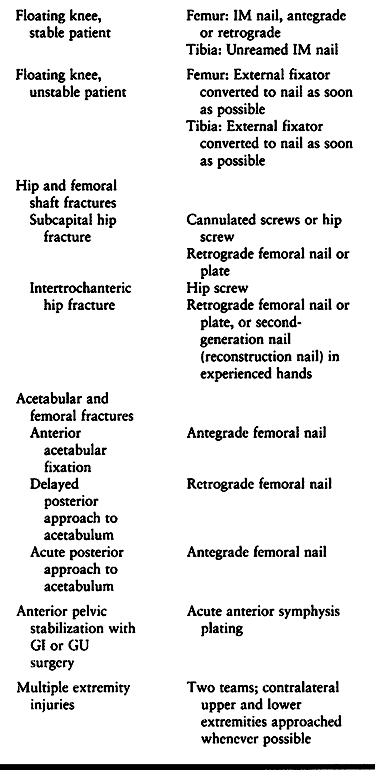
simultaneously by two teams (Table 14.5).
 |
|
Table 14.5. Management of Combined Injuries
|
could also have found her to be hemodynamically unstable, with a
coagulopathy and hypothermia. The patient would then have been best
managed either with temporary external fixation of her femur and tibia
fractures or, generally more appropriately, with temporary skeletal
traction, then taken to the intensive care unit and reresuscitated.
Once her vital signs were stable and oxygenation was adequate, and she
was rewarmed and no longer coagulopathic
(generally
within 12 to 24 h), she could be returned to surgery where, again, two
teams could be used to perform the surgery as described.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
MJ, MacKenzie EJ, Riemer BL, et al. Adult Respiratory Distress
Syndrome, Pneumonia, and Mortality Following Thoracic Injury and a
Femoral Fracture Treated Either with Intramedullary Nailing with
Reaming or with a Plate. J Bone Joint Surg 1997;79-A:799.
A. Musculoskeletal Management. In: Resources for Optimal Care of the
Injured Patient. Chicago: Committee on Trauma, American College of
Surgeons, 1993:48.
KD, Cadambi A, Seibert GB. Incidence of Adult Respiratory Distress
Syndrome in Patients with Multiple Musculoskeletal Injuries: Effect of
Early Operative Stabilization of Fractures. J Trauma 1985;25:375.
HC, Auf’m’Kolk M, Paffrath T, et al. Primary Intramedullary Femur
Fixation in Multiple Trauma Patients with Associated Lung Contusion: A
Cause of Post-traumatic ARDS? J Trauma 1993;34:540.
HC, Regel G, Sturm JA, Tscheim H. Influence of Thoracic Trauma and
Primary Femoral Intramedullary Nailing on the Incidence of ARDS in
Multiple Trauma Patients. Injury 1993;24(Suppl 3):S82.
JM, Becker DP, Miller JD, et al. Traumatic Acute Subdural Hematoma:
Major Mortality Reduction in Comatose Patients Treated Within Four
Hours. N Engl J Med 1981;304:1511.
SR, Hollingworth-Fridlund P, Cooper GF, Eastman AB. The Effect of
Regionalization upon the Quality of Trauma Care as Assessed by
Concurrent Audit Before and After Institution of a Trauma System: A
Preliminary Report. J Trauma 1986;26:812.
C, Nast-Kolb D, Trupka A, et al. Posttraumatic Inflammatory Response,
Secondary Operations, and Late Multiple Organ Failure. J Trauma 1996;40:624.
K, Runkel M, Degreif J, et al. Pathogenesis and Clinical Relevance of
Bone Marrow Embolism in Medullary Nailing—Demonstrated by
Intraoperative Echocardiography. Injury 1993;24(Suppl 3):S73.
GE, Simon P, Redl H, et al. Intramedullary Pressure Changes and Fat
Intravasation During Intramedullary Nailing: An Experimental Study in
Sheep. J Trauma 1994;36:202.
GE, Thurnher M, Redl H, Schlag G. Pulmonary Reaction During
Intramedullary Fracture Management in Traumatic Shock: An Experimental
Study. J Trauma 1994;37:249.



