Intertrochanteric Fractures
-
Intertrochanteric fractures account for nearly 50% of all fractures of the proximal femur.
-
Average patient age of incidence is 66 to 76 years.
-
The ratio of women to men ranges from 2:1 to 8:1, likely because of postmenopausal metabolic changes in bone.
-
In the United States, the annual rate of
intertrochanteric fractures in elderly women is about 63 per 100,000;
in men, it is 34 per 100,000. -
Some of the factors associated with
intertrochanteric rather than femoral neck fractures include advancing
age, increased number of comorbidities, increased dependency in
activities of daily living, and a history of other osteoporosis-related
(“fragility”) fractures.
-
Intertrochanteric fractures occur in the
region between the greater and lesser trochanters of the proximal
femur, occasionally extending into the subtrochanteric region. -
These extracapsular fractures occur in
cancellous bone with an abundant blood supply. As a result, nonunion
and osteonecrosis are not major problems, as in femoral neck fractures. -
Deforming muscle forces will usually produce shortening, external rotation, and varus position at the fracture.
-
Abductors tend to displace the greater trochanter laterally and proximally.
-
The iliopsoas displaces the lesser trochanter medially and proximally.
-
The hip flexors, extensors, and adductors pull the distal fragment proximally.
-
-
Fracture stability is determined by the
presence of posteromedial bony contact, which acts as a buttress
against fracture collapse.
-
Intertrochanteric fractures in younger
individuals are usually the result of a high-energy injury such as a
motor vehicle accident or fall from a height. -
Ninety percent of intertochanteric fractures in the elderly result from a simple fall.
-
Most fractures result from a direct impact to the greater trochanteric area.
-
Patients with nondisplaced fractures may be ambulatory and experience minimal pain.
-
Patients with displaced fractures are nonambulatory, with the injured lower extremity shortened and externally rotated.
-
Range of hip motion is typically painful.
-
Common associated injuries include fractures of the distal radius, proximal humerus, ribs, and spine (compression fractures).
-
Patients may have experienced a delay
before hospital presentation, time usually spent on the floor and
without oral intake. The examiner must therefore be cognizant of
potential dehydration, nutritional, and pressure ulceration issues as
well as hemodynamic instability, because intertrochanteric fractures
may be associated with as much as a full unit of hemorrhage into the
thigh.
-
An anteroposterior (AP) view of the pelvis and an AP and a cross-table lateral view of the involved proximal femur are obtained.
-
An internal rotation view of the injured hip may be helpful to clarify the fracture pattern further.
-
Technetium bone scan or preferably
magnetic resonance imaging may be of clinical utility in delineating
nondisplaced or occult fractures that are not apparent on plain
radiographs.
-
This is based on prereduction and
postreduction stability, that is, the convertibility of an unstable
fracture configuration to a stable reduction. -
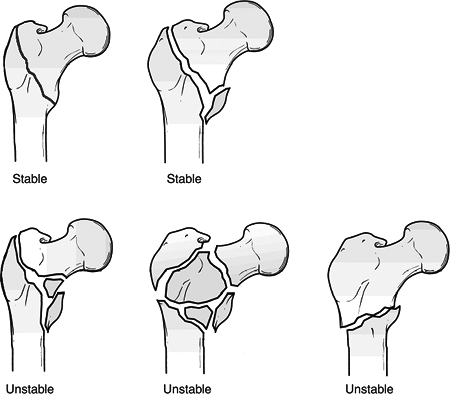
In stable fracture patterns, the
posteromedial cortex remains intact or has minimal comminution, making
it possible to obtain and maintain a stable reduction. -
Unstable fracture patterns are
characterized by greater comminution of the posteromedial cortex.
Although they are inherently unstable, these fractures can be converted
to a stable reduction if medial cortical opposition is obtained. -
The reverse obliquity pattern is inherently unstable because of the tendency for medial displacement of the femoral shaft.
-
The adoption of this system was important
not only because it emphasized the important distinction between stable
and unstable fracture patterns, but also because it helped define the
characteristics of a stable reduction.
-
Several studies have documented poor
reproducibility of results based on the various intertrochanteric
fracture classification systems. -
Many investigators simply classify
intertrochanteric fractures as either stable or unstable, depending on
the status of the posteromedial cortex. Unstable fracture patterns
comprise those with comminution of the posteromedial cortex,
subtrochanteric extension, or a reverse obliquity pattern.
 |
|
Figure
30.1. The Evans classification of intertrochanteric fractures. In stable fracture patterns, the posteromedial cortex remains intact or has minimal comminution, making it possible to obtain and maintain a reduction. Unstable fracture patterns, conversely, are characterized by greater comminution of the posteromedial cortex. The reverse obliquity pattern is inherently unstable because of the tendency for medial displacement of the femoral shaft. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
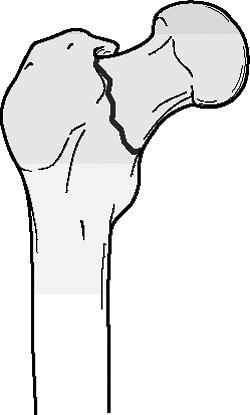
Basicervical neck fractures are located just proximal to or along the intertrochanteric line (Fig. 30.2).
-
These fractures are usually extracapsular.
-
They are at greater risk for osteonecrosis than the more distal intertrochanteric fractures.
-
They lack the cancellous interdigitation
seen with fractures through the intertrochanteric region and are more
likely to sustain rotation of the femoral head during implant insertion.
-
Reverse obliquity intertrochanteric
fractures are unstable fractures characterized by an oblique fracture
line extending from the medial cortex proximally to the lateral cortex
distally (Fig. 30.3). -
The location and direction of the
fracture line result in a tendency to medial displacement from the pull
of the adductor muscles.
 |
|
Figure 30.2. Basicervical neck fractures are located just proximal to or along the intertrochanteric line.
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
This is indicated only for patients who
are at extreme medical risk for surgery; it may also be considered for
demented nonambulatory patients with mild hip pain. -
Early bed to chair mobilization is
important to avoid increased risks and complications of prolonged
recumbency, including poor pulmonary toilet, atelectasis, venous
stasis, and pressure ulceration. -
Resultant hip deformity is both expected and accepted.
-
This is associated with a higher mortality rate than operative treatment.
-
The goal is stable internal fixation to
allow early mobilization and full weight-bearing ambulation. Stability
of fracture fixation depends on:-
Bone quality.
-
Fracture pattern.
-
Fracture reduction.
-
Implant design.
-
Implant placement.
-
-
Surgery should be performed in a timely fashion, once the patient has been medically stabilized.
-
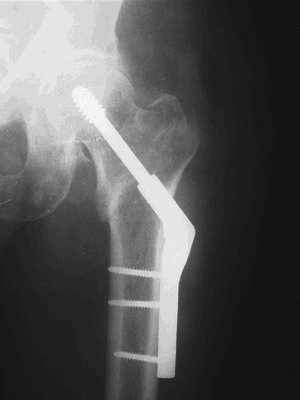
This is the most commonly used device for
both stable and unstable fracture patterns. It is available in plate
angles from 130 to 150 degrees (Fig. 30.4).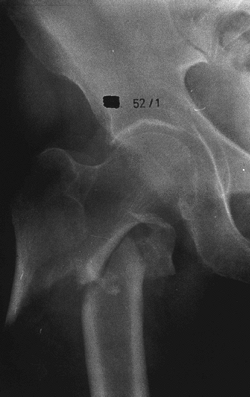 Figure 30.3. Anteroposterior x-ray demonstrating a reverse obliquity right intertrochanteric fracture.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 30.3. Anteroposterior x-ray demonstrating a reverse obliquity right intertrochanteric fracture.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)![]() Figure 30.4. X-ray of a sliding hip screw.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 30.4. X-ray of a sliding hip screw.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
The most important technical aspects of
screw insertion are (1) placement within 1 cm of subchondral bone to
provide secure fixation and (2) central position in the femoral head.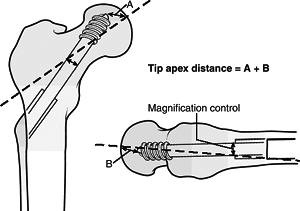 Figure
Figure
30.5. The tip-apex distance (TAD), expressed in millimeters, is the sum
of the distances from the tip of the lag screw to the apex of the
femoral head on both the anteroposterior and lateral radiographic views.(From Baumgaertner
MR, Chrostowski JH, Levy RN. Intertrochanteric hip fractures. In:
Browner BD, Levine AM, Jupiter JB, Trafton PG, eds. Skeletal Trauma, vol. 2. Philadelphia: WB Saunders, 1992:1833–1881.) -
The tip-apex distance can be used to
determine lag screw position within the femoral head. This measurement,
expressed in millimeters, is the sum of the distances from the tip of
the lag screw to the apex of the femoral head on both the AP and
lateral radiographic views (after controlling for radiographic
magnification) (Fig. 30.5). The sum should be <25 mm to minimize the risk of lag screw cutout. -
Biomechanical and clinical studies have shown no advantage of four screws over two to stabilize the sideplate.
-
At surgery, the surgeon must be prepared to deal with residual varus angulation, posterior sag, or malrotation.
-
A 4% to 12% incidence of loss of fixation is reported, most commonly with unstable fracture patterns.
-
Most failures of fixation are
attributable to technical problems of screw placement and/or inadequate
impaction of the fracture fragments at the time of screw insertion.
-
This implant combines the features of a sliding hip screw (SHS) and an intramedullary nail (Fig. 30.6).
-
Advantages are both technical and
mechanical: Theoretically, these implants can be inserted in a closed
manner with limited fracture exposure, decreased blood loss, and less
tissue damage than an SHS. In addition, these devices are subjected to
a lower bending moment than the SHS owing to their intramedullary
location. -
Use of the intramedullary hip screw limits the amount of fracture collapse, compared with an SHS.
![]() Figure 30.6. Reverse obliquity fracture stabilized with a cephalomedullary nail.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 30.6. Reverse obliquity fracture stabilized with a cephalomedullary nail.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Most studies have demonstrated no
clinical advantage of the intramedullary hip screw compared with the
SHS in stable fracture patterns. -
Use of intramedullary hip screws has been
most effective in intertrochanteric fractures with subtrochanteric
extension and in reverse obliquity fractures. -
Use of older design intramedullary hip
screws has been associated with an increased risk of femur fracture at
the nail tip or distal locking screw insertion point.
-
This has been used successfully for
patients in whom open reduction and internal fixation have failed and
who are unsuitable candidates for repeat internal fixation. -
A calcar replacement hemiarthroplasty is needed because of the level of the fracture.
-
Primary prosthetic replacement for
comminuted, unstable intertrochanteric fractures has yielded up to 94%
good functional results. -
Disadvantages include morbidity
associated with a more extensive operative procedure, the internal
fixation problems with greater trochanteric reattachment, and the risk
of postoperative prosthetic dislocation.
-
This is not commonly considered for the treatment of intertrochanteric femur fractures.
-
Early experiences with external fixation
for intertrochanteric fractures were associated with postoperative
complications such as pin loosening, infection, and varus collapse. -
Recent studies have reported good results using hydroxyapatite-coated pins.
-
With use of an SHS, large posteromedial
fragments in younger individuals should receive fixation with cerclage
wires or a lag screw to restore the posteromedial buttress. -
With use of an SHS, greater trochanteric displacement should be fixed utilizing tension band techniques.
-
Basicervical fractures should be treated
with an SHS or IM nail with a supplemental antirotation screw or pin
during implant insertion. -
Reverse obliquity fractures are best treated as subtrochanteric fractures.
-
Ipsilateral fractures of the femoral
shaft, although more common in association with femoral neck fractures,
should be ruled out when the injury is caused by high-energy trauma.
-
Early patient mobilization with weight bearing as tolerated ambulation is indicated.
-
Loss of fixation: This most commonly
results from varus collapse of the proximal fragment with cutout of the
lag screw from the femoral head; the incidence of fixation failure is
reported to be as high as 20% in unstable fracture patterns. Lag screw
cutout from the femoral head generally occurs within 3 months of
surgery and is usually caused by one the following:-
Eccentric placement of the lag screw within the femoral head.
-
Improper reaming that creates a second channel.
-
Inability to obtain a stable reduction.
-
Excessive fracture collapse such that the sliding capacity of the device is exceeded.
-
Inadequate screw-barrel engagement, which prevents sliding.
-
Severe osteopenia, which precludes secure fixation.
-
Management choices include: (1)
acceptance of the deformity; (2) revision open reduction and internal
fixation, which may require methylmethacrylate; and (3) conversion to
prosthetic replacement. Acceptance of the deformity should be
considered in marginal ambulators who are a poor surgical risk.
Revision open reduction and internal fixation are indicated in younger
patients, whereas conversion to prosthetic replacement (unipolar,
bipolar, or total hip replacement) is preferred in elderly patients
with osteopenic bone.
-
-
-
Nonunion: Rare, occurring in less than 2% of patients, especially in patients with unstable fracture patterns. The diagnosis
P.337
should be suspected in a patient with persistent hip pain and
radiographs revealing a persistent radiolucency at the fracture site 4
to 7 months after fracture fixation. With adequate bone stock, repeat
internal fixation combined with a valgus osteotomy and bone grafting
may be considered. In most elderly individuals, conversion to a calcar
replacement prosthesis is preferred. -
Malrotation deformity: This results from
internal rotation of the distal fragment at the time of internal
fixation. When it is severe and interferes with ambulation, revision
surgery with plate removal and rotational osteotomy of the femoral
shaft should be considered. -
With full-length intramedullary nails,
impingement of the distal aspect of the nail on the anterior femoral
cortex can occur, secondary to a mismatch of the nail curvature and
femoral bow. -
With dual screw trochanteric nails,
failure can result from the “Z effect,” with the most proximal screw
penetrating the hip joint and the distal screw backing out of the
femoral head. -
Osteonecrosis of the femoral head: This is rare following intertrochanteric fracture.
-
Lag screw-sideplate separation.
-
Lag screw migration into the pelvis.
-
Laceration of the superficial femoral artery by a displaced lesser trochanter fragment.
-
Isolated greater trochanteric fractures, although rare, typically occur in older patients as a result of a direct blow.
-
Treatment of greater trochanteric fractures is usually nonoperative.
-
Operative management can be considered in younger, active patients who have a widely displaced greater trochanter.
-
Tension band wiring of the displaced fragment and the attached abductor muscles is the preferred technique.
-
These are most common in adolescence, typically secondary to forceful iliopsoas contracture.
-
In the elderly, isolated lesser
trochanter fractures have been recognized as pathognomonic for
pathologic lesions of the proximal femur.