Talus Fractures
frequent incidence of serious complications, such as osteonecrosis,
associated with talus fractures leads to a high risk of unsatisfactory
results. Since the early descriptions by Anderson4
and others of the “aviator’s astragalus.” fractures of the talus have
earned a reputation as a problematic fracture. In Greek mythology,
Talos was a giant, grotesque bronze god with a singular large vein
coursing through his body. Because of this vulnerable vascularity, his
crucial weakness was the relative ease with which exsanguination might
occur.
evolved such that orthopaedic surgeons are now well aware of the
inherent dangers of this injury. Surgical techniques, timing, and
instrumentation have changed. Many of the surgical implants in common
use to stabilize talus fractures were not available just a decade ago.
The use of smaller implants and locking plates has improved the
surgeon’s ability to reconstruct problematic talar injuries. Similarly,
our understanding of the biology of bone repair and the vascular supply
to the talus has grown. Nonetheless, talus fractures remain among the
most interesting and difficult injuries in orthopedic trauma.
relatively uncommon. However, the talus is the second most commonly
fractured tarsal bone. In recent years, improved recognition has
resulted in an increased number of talar process fractures being
diagnosed. Coltart30 reviewed 228
talus fractures and noted that chip and avulsion injuries were most
common, followed by fractures of the talar neck.
injuries. Fractures of the talar neck are commonly the result of a
hyperdorsiflexion type injury. Following World War I, Anderson,4
the consultant surgeon to the Royal Flying Corps, described the
aviator’s astragalus. Pilots resting the sole of the foot on the rudder
bar at the time of impact commonly sustained a hyperdorsiflexion force,
resulting in a fracture of the neck of the talus. Flying accidents were
also common in the description by Coltart.30 Currently, motor vehicle collisions and falls from a height are more common mechanisms of serious talus fractures.
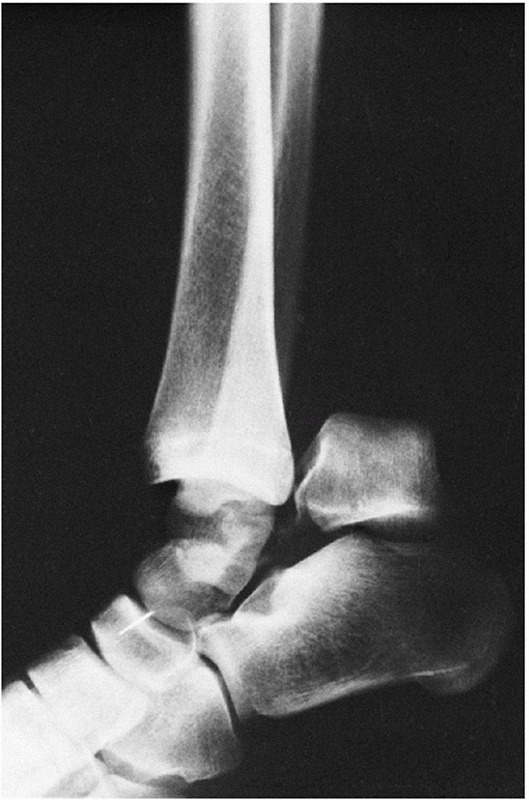
ligaments of the subtalar joint rupture, the neck of the talus impacts
against the leading anterior edge of the distal tibia, and a fracture
line develops at this point and enters the nonarticular portion of the
subtalar joint between the middle facet and the posterior facet. With a
continuation of the dorsiflexion force the calcaneus with the rest of
the foot and including the head of the talus subluxes forward. If there
is a concomitant inversion component to the force, the foot may sublux
or dislocate medially (if there is a concomitant eversion force, the
foot dislocates laterally). If the force subsides at this moment, the
foot recoils, the body of the talus tips into equinus and the fracture
surface of the neck comes to ride on the upper surface of the os
calcis. A continuation of the dorsiflexion force, however, produces
further rupture of the posterior ankle capsular ligaments, the strong
posterior talofibular ligament, and the superficial and posterior
aspects of the deltoid ligament… .The body of the talus is then wedged
posteriorly and medially out of the mortise and rotates around a
horizontal and transverse axis so that the fracture surface faces
upwards and laterally. This is a constant position for the body when
there has been dislocation of the body out of the mortise occurring
because of the direction of the posterior facet of the subtalar joint,
and because the talus pivots around the intact deep fibers of the
deltoid ligament and flexor hallucis longus tendon. The body of the
talus then comes to lie in the interval between the posterior aspect of
the medial malleolus and the anterior aspect of the tendo Achillis. It
may be tightly jammed behind the medial malleolus, which is often
concomitantly fractured, and the sustentaculum tali. The posterior
tibial neurovascular structures almost invariably evade injury by this
mechanism, lying anterior to and being protected by the flexor hallucis
longus tendon.
applied a dorsiflexion force to cadaver specimens and were unable to
produce a talar neck fracture. Rather, the typical pattern of talar
neck fracture was achieved by the application of an axial load to the
plantar surface of the foot when the body of the talus was fixed as a
cantilever between the tibia and the calcaneus.159
Fractures of the lateral and posteromedial processes of the talus and
subtalar dislocations can result from inversion and eversion mechanisms
and are commonly seen in sports injuries. The energy applied at the
time of the injury is often predictive of the ultimate result.
Typically, the midfoot progressively dorsiflexes relative to the body
of the talus, resulting in significant loss of ankle motion and
deformity of the hindfoot. The talar body can eventually become
prominent medially and even progress towards dislocation.
conjunction with one another. In this case, the proposed mechanism of
injury relates primarily to axial load. Fractures of the talar body are
commonly associated with fractures of the tibial plafond and fractures
involving the medial and lateral malleoli. Virtually all fractures of
the talar body as well as combined injuries of the neck and body are
high-energy injuries.
foot injuries involve fractures of the talus. Talus fractures
frequently occur in a young, active, and mobile population. Injuries
involving the talar processes can be initially misdiagnosed. A high
index of suspicion is required for the detection of talar process
fractures, in conjunction with ankle inversion or eversion injuries.
These injuries can be difficult to appreciate on routine radiographs,
and specialized views or cross-sectional imaging may be required.
Fractures of the talus can occur from relatively low-energy mechanisms
or major trauma and in all cases can be a disabling injury if not
treated expeditiously.
conjunction with high-energy talar fractures, such as Hawkins type III
injuries, in which the talar body can be extruded posteromedially and
wrapped around the deltoid ligament.72
Soft tissue compromise is common to talar fracture-dislocations,
although the injury does not always penetrate the skin. When the talus
fracture is open, the situation can be even more devastating. In some
cases, the talar body can be completely extruded as all soft tissues
can be detached from the bone.183
The talar body may even be left at the scene of the injury. Management
of the extruded or absent talus is especially challenging.
mandatory to minimize additional soft tissue injury and skin necrosis
and to reduce cartilage injury. Urgent reduction of the dislocated
talus is one of the key principles of management.
occur. Frequently, however, even when the talus is dislocated
posteromedially, relative protection of the neurovascular bundle is
afforded by the flexor hallucis longus tendon such that the posterior
tibial nerve and vessel are usually intact.23
Vascular injury to the talus itself, however, is frequently noted and
is the predisposing factor associated with osteonecrosis of the talus.
For example, when the talus is dislocated posteromedially, the arteries
of the tarsal sinus and tarsal canal are usually disrupted, as are the
dorsal neck branches such that the only remaining vascular supply to
the talar body may be through the deltoid ligament.
with severe soft tissue injury, neurovascular injury may be severe. An
accurate assessment of the vascular and neurologic status of the foot
is an important principle in the initial management of these injuries.
musculoskeletal injuries and systemic trauma. Management of the talus
fracture in the multiply injured patient can be difficult. An important
principle remains emergent reduction of dislocated joints whenever
possible. Stabilization of fractures and dislocations facilitates
management of the soft tissues.23,35,96
However, in some cases the multisystem injury is so severe that
treatment of the talus fracture is by necessity delayed. Nonetheless, a
good result for the talus fracture can still be achieved, even when
appropriate orthopaedic intervention is delayed.
assessment includes the Advanced Trauma Life Support (ATLS) protocols
for management. Where possible, an emergent reduction of dislocated
joints can be performed followed by application of an external fixator93,94 or internal fixation.173 Foot injuries are among the most commonly missed injuries in the multiply injured patient.200
In one series of talar fractures from a Level I trauma center, 31 out
of 70 fractures occurred in multiple trauma patients with an injury
severity score of greater than 16, and 41 of 70 fractures were
associated with other ipsilateral lower extremity injuries, confirming
the common association of multiple trauma and ipsilateral injuries in
patients with fractures of the talar neck.171
talus fracture-dislocations, particularly in patients who have fallen
from a height or sustained major motor vehicle trauma. High-energy foot
injuries should be managed in conjunction with the talus fracture such
that early reduction and stabilization of all dislocated joints can be
achieved.75,85
In many cases, the management of dislocated joints, as well as
management of soft tissue problems, may preclude further definitive
fixation or internal fixation of fractures; however, where possible,
early stabilization of the joints is preferred.147
High-energy foot injuries seem to be increasing in frequency related in
part to the increasing use of air bags in motor vehicles. With the
improved survival of patients who previously may have died from chest,
head, and visceral injuries, now serious trauma to the foot, ankle, and
lower extremity is more commonly noted. These foot injuries can be
devastating in terms of long-term outcome for the patient.
seen with fractures of the talar neck and body. In a recent study by
Vallier et al.,202 associated foot
and ankle fractures occurred in 44 of 100 patients. Talus fractures are
frequently associated with tibial plafond and malleolar fractures. The
incidence of associated malleolar injury has ranged from 19% to 28% in
prior studies.19,116
Fractures of the distal tibia and fibula can be addressed in
conjunction with the talus fracture and may even afford a means of
exposure of the talar body through the malleolar fracture site.
Tibiofibular diastasis has been found in conjunction with talar neck
fractures.63 A 10% incidence of calcaneal fractures has also been reported in conjunction with talar neck fractures.116
treated urgently, although the exact timing is controversial. Reduction
of dislocated joints is critical to maintain vascularity to the talar
body where possible and to reduce tension on the soft tissues and
neurovascular structures around the foot and ankle. Early reduction is
theorized to assist the restoration of blood flow and potentially
decrease the rate of osteonecrosis. However, clinical studies have, to
date, not demonstrated a significant effect of surgical timing on rates
of osteonecrosis. When delayed treatment is an unfortunate necessity
due to the condition of the patient, a prolonged delay in transfer, or
other reasons, immediate management should still include an attempt at
reduction of dislocations. Preferred surgical timing for talar neck
fractures is controversial. A recent survey of orthopaedic trauma
experts regarding the timing of surgical treatment for displaced talar
neck fractures revealed that 40% of respondents felt treatment should
occur within 8 hours, and 76% felt treatment should occur within 24
hours; the remaining 24% felt treatment after 24 hours was acceptable.153
reduction of the talar neck fracture and the associated joints and to
achieve sufficient stabilization to facilitate early motion. A variety
of surgical techniques have been described to accomplish these
principles. Emergent reduction of dislocated joints, precise fracture
reduction and stabilization, and protection of the remaining vascular
supply and soft tissue envelope provide the best probability of
regaining an excellent functional result.
variety of plain radiographic views are important to visualize the
talus. Standard anteroposterior, lateral, and mortise views of the
ankle are essential to assess fractures of the talar body, talar neck,
and the associated processes. However, in many cases, standard plain
radiographic views are inadequate to demonstrate relatively subtle
fractures of the talus and to give adequate visualization of
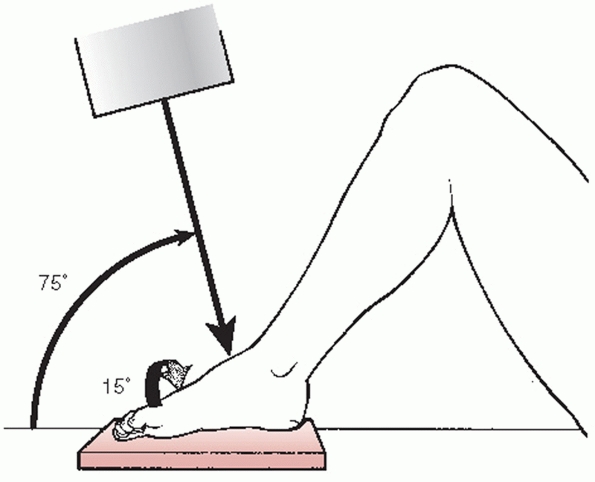
comminution and alignment. Canale and Kelly19,20
described a view of the talar neck achieved by internal rotation of the
foot by placing the foot plantigrade on an x-ray film and angling the
beam at 75 degrees to the perpendicular. Pronation of the foot or
internal rotation of the limb will achieve rotation of the talus such
that the medial aspect of the talar neck can be well visualized. This
view is particularly useful intraoperatively to assess the
reconstruction of a talar neck fracture with associated medial
comminution and to confirm that varus malalignment has been avoided (Fig. 58-1).
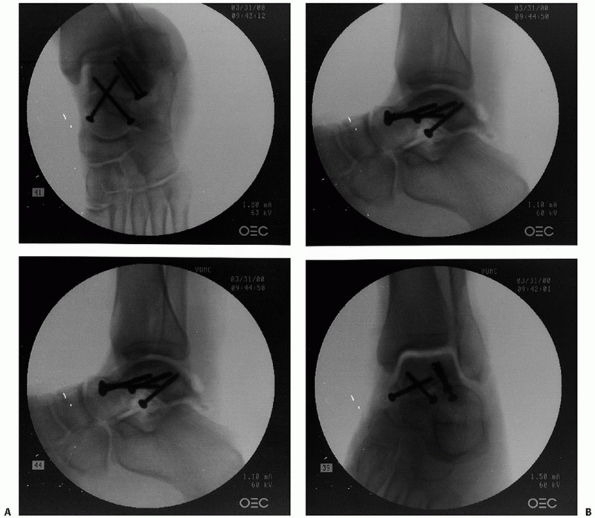
calcaneus, as associated fractures of the posterior facet can often be
seen. A true lateral view of the subtalar joint can be beneficial to
assess for comminution and subluxation (Fig. 58-2). Oblique views of the talus are helpful in diagnosing posterior process fractures.46
For example, an anteroposterior view obtained with the ankle externally
rotated 30 degrees brings the posteromedial process into profile.44
visualization of the congruity of the subtalar joint reduction and
provide superior detail compared with plain films. Comminuted fractures
of the talus as well as fractures involving its inferior aspect
extending into the subtalar joint benefit from the improved detail
noted with CT scans as these regions may be especially difficult to
visualize on plain films. Compared to plain radiographs and
radiostereometric analysis, CT imaging has greater accuracy in the
detection and characterization of displacement following fixation or
displacement associated with malunion.22
 |
|
FIGURE 58-1 Canale and Kelly view of the foot. The correct position of the foot for x-ray evaluation of the talus is shown.
|
 |
|
FIGURE 58-2 Intraoperative fluoroscopic evaluation of the talus. A. A Canale and Kelly view and lateral image of the subtalar joint. B. Lateral and anteroposterior views of the ankle in a talar neck fracture with an associated lateral process fracture.
|
fractures for congruency of reduction can be similarly useful to assess
subtalar dislocations. Subtalar dislocations are often associated with
small but significant fractures of the inferior aspect of the talus,
which are better appreciated on CT scans compared to plain films alone.
New technology includes C-arm based mobile CT. Although the image
quality of this method is still improving, mobile CT may prove to be a
significant advantage for intraoperative imaging.211
the assessment of talar fractures.95,141
MRI demonstrates osteonecrosis most effectively. Previously, MRI has
been subject to artifact from the placement of significant volume of
stainless steel screws. This problem is lessened when titanium implants
are used for fracture fixation. Recently, improved MRI technology has
lessened the effect of metallic artifact, such that MRI may provide
useful information even in the presence of metal hardware.
injuries. Varying in severity from devastating to trivial, these
injuries necessarily are grouped in several distinct classifications.
The most clinically useful general classification separates talus
injuries into fractures of the talar neck, the talar body, the talar
head, and the talar processes. Subtalar dislocations are usually
considered separately. Each of these anatomic regions may be
subclassified and will be discussed in the appropriate section of this
chapter.
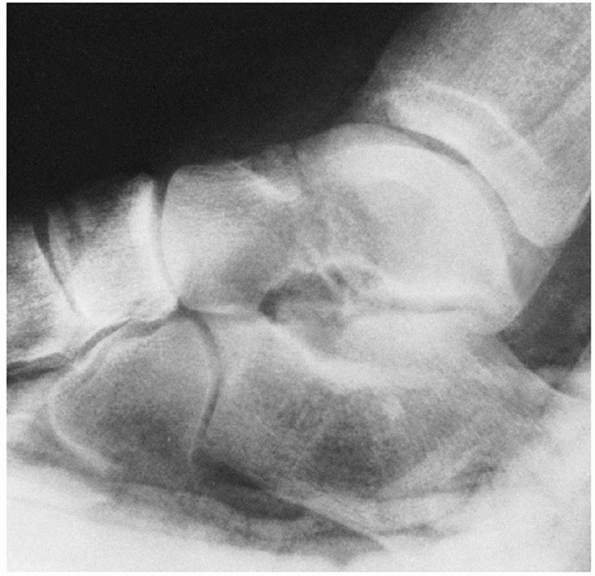
classification, type I refers to a fracture without associated joint
dislocation, that is, an undisplaced fracture of the talar neck (Fig. 58-3). As noted by Daniels, “There is no room for the term ‘a minimally displaced type I talar neck fracture.’”32
In equivocal cases, careful attention should be directed to the
subtalar joint alignment to confirm that there is in fact no degree of
subtle incongruity and to the clinical exam, as most slightly displaced
talar neck fractures are associated with deformity. Often the talar
head is rotated relative to the talar body, such that supination of the
midfoot and forefoot relative to the hindfoot can be noted.
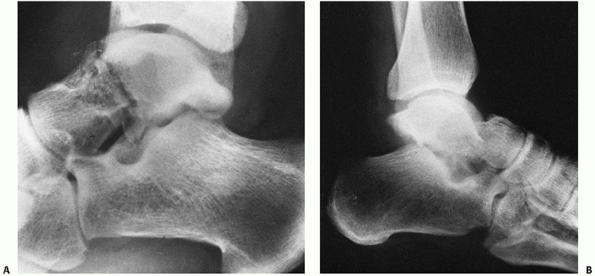
This is the most common type of talar neck fracture-dislocation and in
some cases is amenable to closed reduction. While osteonecrosis of the
body of the talus in Hawkins type I fractures is relatively rare, the
incidence of osteonecrosis in type II fractures ranges as high as 40%
to 50%.20
 |
|
FIGURE 58-3 Nondisplaced vertical fracture of the talar neck, Hawkins’ type I.
|
In this case, osteonecrosis is the rule rather than the exception with
rates of osteonecrosis of nearly 100% in both the Hawkins73 and the Canale and Kelly20
series. With Hawkins type III fractures, the body is most commonly
dislocated posteromedially. The talar body fragment can be rotated
around the deep fibers of the deltoid ligament and may lie posterior to
the long flexor tendons of the foot. These injuries are most commonly
irreducible by closed means.
These injuries are relatively uncommon compared to the Hawkins type II
and III fracture-dislocations. The quoted rate of osteonecrosis remains
close to 100%. Some authors have grouped comminuted fractures of the
talus associated with high-energy foot injuries into the Hawkins IV
classification to imply a worse prognosis and because these injuries
are difficult to fit into the classification elsewhere. Pantazopoulos150
described a case in which the talar neck fracture was associated with a
dislocation of the talar head, but the body remained reduced. This
injury was also classified as a Hawkins type IV talar neck fracture.150
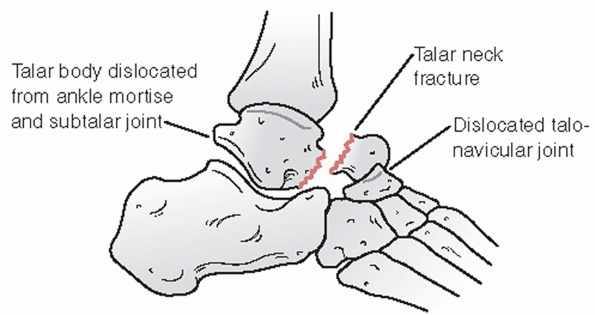
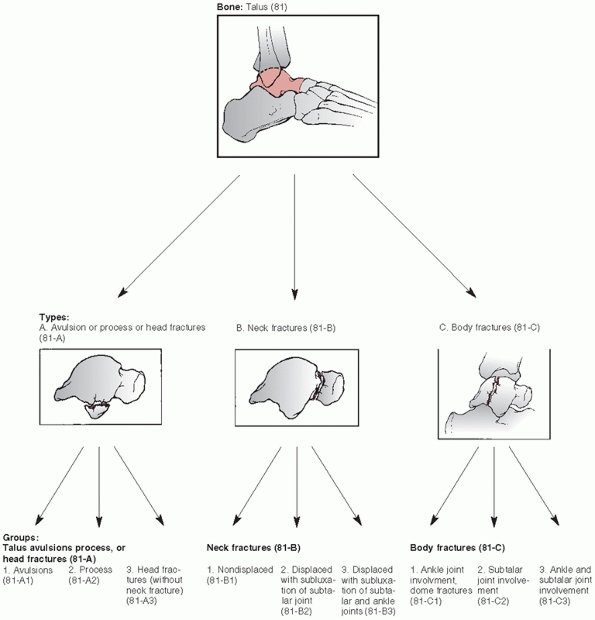
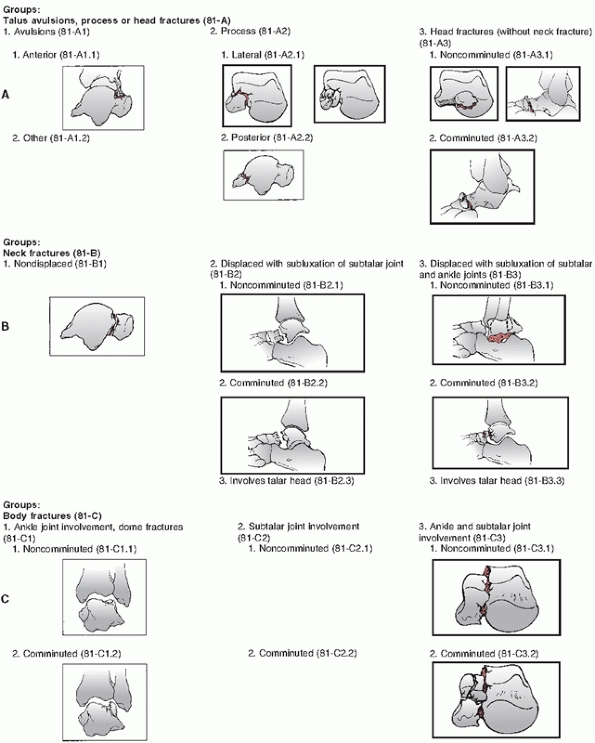
is described in the Orthopedic Trauma Association’s Fracture and
Dislocation compendium.148 Talus
fractures are divided into avulsion, process, or head fractures (81-A),
neck fractures (81-B), and body fractures (81-C) (Fig. 58-7).
Similar to Hawkins’ classification, neck fractures are subdivided into
nondisplaced fractures (81-B1), displaced fractures associated with
subluxation of the subtalar joint (81-B2), and displaced fractures
associated with subluxation of the subtalar and tibiotalar joints
(81-B3). Talar body fractures are divided into talar dome fractures
(81-C1), talar body fractures with subtalar joint involvement (81-C2),
and talar body fractures with subtalar and ankle joint involvement
(81-C3). For fractures of the talar head (81-A3), neck (81-B2 and
81-B3), and body (81-C1, C2, and C3) fractures are further classified
according to comminution.148 Comminution has been noted to be an important factor related to outcome in recent studies of talus fractures.171,202
to talar neck fractures and is predictive of rates of osteonecrosis,
another important prognostic factor is fracture comminution. In two
recent large series of talar neck fractures, comminution was predictive
of outcome independent of Hawkins’ classification.171,202 The presence of severe comminution implies more energy imparted to the fracture and may suggest a worse prognosis and outcome.
The blood vessels that enter the talus traverse regions of articular
capsule and synovial membrane in which they are vulnerable to trauma.
Because of the lack of muscular soft tissue
attachments
and the limited space available for vascular foramina, the talus is
predisposed to difficulties with blood supply, and osteonecrosis is a
well-recognized complication of trauma to the talus.
 |
|
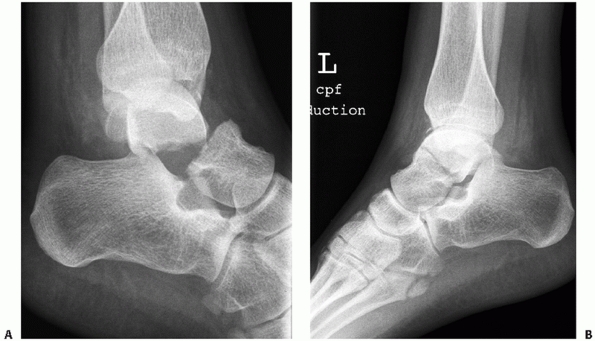
FIGURE 58-4 Displaced Hawkins’ type II fractures of the talar neck with subluxation (A) and dislocation (B) of the subtalar joint.
|
The trochlea is wider anteriorly compared to posteriorly such that the
medial and lateral sides of the trochlea converge in a posterior
direction. Medially and laterally, the articular cartilage extends
plantarward to articulate with the medial and lateral malleoli. The
inferior side of the talus is also predominantly covered by cartilage
to form the articulation with the posterior facet of the calcaneus.
 |
|
FIGURE 58-5 Displaced fracture of the talar neck with dislocation of both the subtalar and tibiotalar joints (Hawkins type III).
|
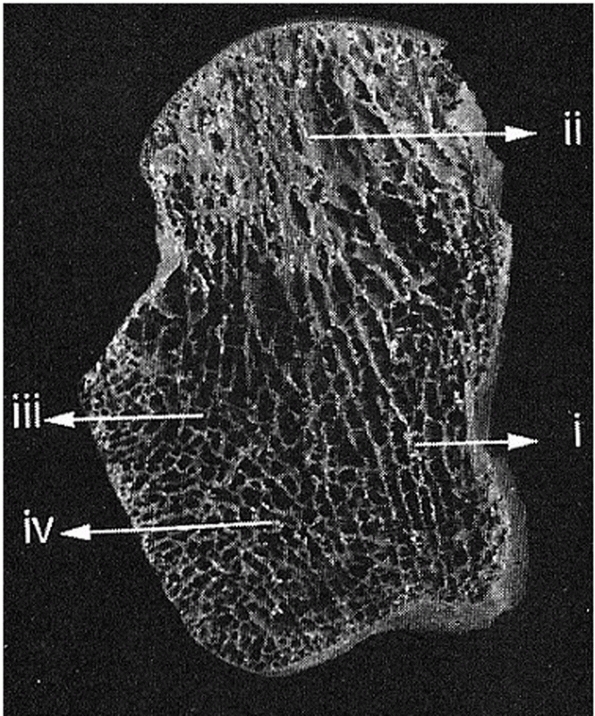
function in force transmission across the ankle. The cortex of the
talus is thicker around the posterior calcaneal facet, the malleolar
facets, the talar neck, and at the attachments of major ligaments.5 Swanson187
described an increase in bone density in the lateral aspect of the
talar head and in the inferolateral aspect of the talar body compared
with the medial bone (Fig. 58-9). The
cancellous bone is organized into two sets of stacked vertical lamellae
or plates which are organized primarily from the anteromedial trochlea
toward the talar head, and from the posterolateral trochlea inferiorly
toward the posterior calcaneal facet.5
This arrangement of lamellae facilitates force transmission. During
heel strike, weight is transmitted inferiorly toward the calcaneus, and
as the gait cycle progresses, an increasing amount of weight is
transmitted anteriorly toward the talar head.
 |
|
FIGURE 58-6 Hawkins type IV fracture of the talar neck with subluxation of the subtalar joint and dislocation of the talonavicular joint.
|
 |
|
FIGURE 58-7 The AO/OTA classification of talus fractures.148 (continues)
|
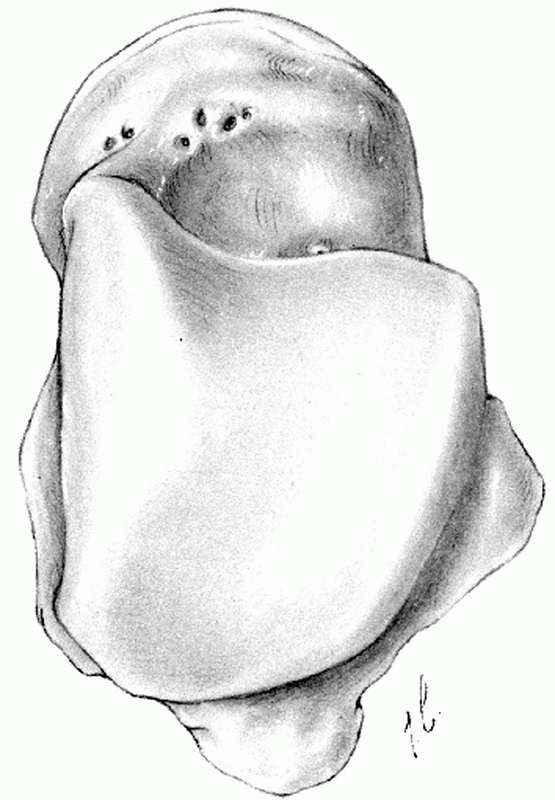
Multiple vascular foramina exist, particularly on the dorsal neck where
capsular and ligamentous attachments originate. The neck of the talus
deviates medially by about 15 to 20 degrees. The head of the talus has
rounded cartilaginous facets to articulate with the navicular
anteriorly. The spring ligament wraps around the inferior aspect of the
talar head and the deltoid ligament attaches to the medial aspect of
the talar body. There is a wide area of attachment for the deltoid
ligament extending from the talar body onto the medial aspect of the
neck.
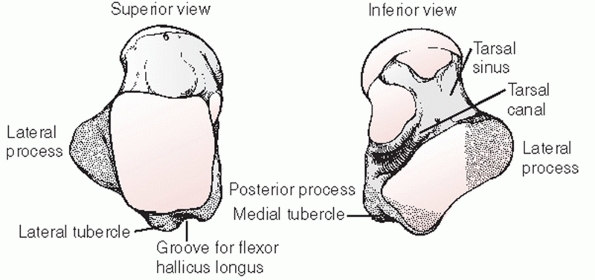
inferior medial surface forms the lateral third of the talar
articulation with the posterior facet of the calcaneus. Its superior
lateral surface articulates with the distal end of the fibula. It is
vulnerable to fracture as an isolated injury or associated with
fractures of the talar body. The posterior process of the talus is
derived from two tubercles. The medial tubercle and the lateral
tubercle
are
separated by a groove, within which courses the flexor hallus longus
tendon. The os trigonum may exist as a separate ossicle or be fused
with the lateral tubercle of the posterior process. The os trigonum is
present in 50% of normal feet.109 This small ossicle arises from a separate ossification center just posterior to the lateral tubercle.
 |
|
FIGURE 58-7 (continued)
|
 |
|
FIGURE 58-8 Superior and inferior views of the talus (stippling indicates the posterior and lateral processes).
|
Blood vessels enter the talus via the limited capsular and ligamentous
attachments and are vulnerable to injury such that osteonecrosis is a
well-recognized complication of talus fractures and dislocations.
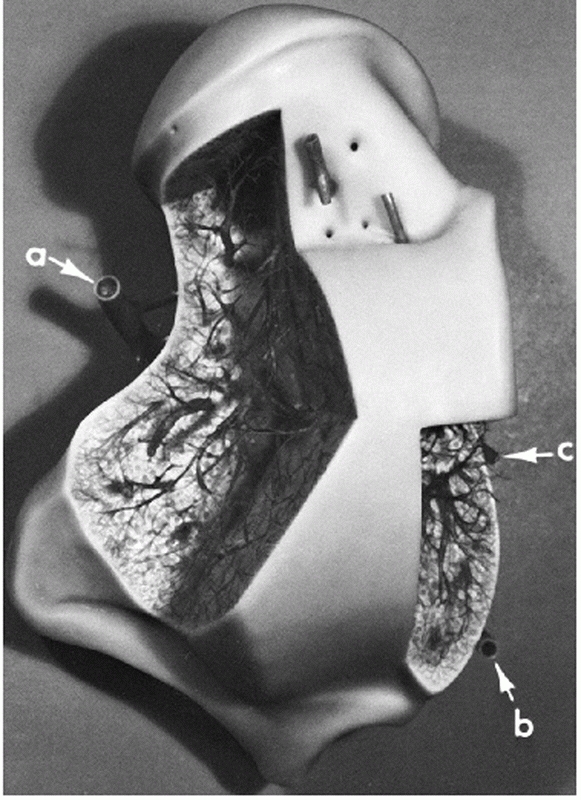
who described the critical anastomotic sling of vessels in the tarsal
sinus and tarsal canal, lying inferior to the neck of the talus. Within
the tarsal canal and the tarsal sinus, these important anastomotic
vessels perforate the inferior neck to form the primary source of blood
supply to the body of the talus. The tarsal sinus is bounded by the
calcaneus inferiorly, the body of the talus posteriorly, and the talar
head and neck anteriorly. The tarsal canal lies between the talus and
calcaneus just behind and below the tip of the medial malleolus. The
tarsal sinus and tarsal canal can be likened to a funnel. Kelly and
Sullivan91 compare the tarsal sinus to the cone of the funnel and the tarsal canal to the tube of the funnel (Fig. 58-11).
The artery to the sinus tarsi and the artery of the tarsal canal form
the anastomotic sling inferior to the talus from which branches arise
to enter the talar neck area.
artery just proximal to the origin of the medial and lateral plantar arteries.140 The deltoid branches arise from the artery of the tarsal canal and supply the medial third of the talar body.57
From the anterior tibial, or dorsalis pedis artery, come multiple
branches to the dorsal aspect of the talar neck. An additional branch
may provide a contribution to the artery of the sinus tarsi. From the
peroneal artery come branches to the posterior process and a branch to
form the artery of the sinus tarsi. Peterson and colleagues160
emphasized the important contribution of additional capsular and
ligamentous vessels adjoining the talus with the navicular, the
calcaneus, and even the tibia through capsular and ligamentous
attachments. Intraosseus communications between the major arterial
supplies to the talus have also been demonstrated.57
 |
|
FIGURE 58-9 Left talus horizontal section demonstrating internal lamellar architecture including sagittal plates in the medial body (i) curving toward the talar head (ii) and plates from the lateral process curving anterior (iii) and posterior (iv).
(Reproduced from Athavale S, Joshi S, Joshi S. Internal architecture of the talus. Foot Ankle Int 2008;29:82-86, with permission.) |
 |
|
FIGURE 58-10
Superior view of the right talus demonstrating the convergence of the sides of the trochlear surface and the vascular foramina on the neck. (From Giannestras NJ. Foot Disorders: Medical and Surgical Management. 2nd ed. Philadelphia: Lea and Febiger, 1973.) |
 |
|
FIGURE 58-11
The anastomotic sling of vessels that provides the blood supply to the body of the talus. Laterally, the artery of the tarsal sinus (A); medially, the artery of the tarsal canal (B). Additional arteries enter dorsally through the neck and on the medial surface of the body (C). (Kelly PJ, Sullivan CR. Blood supply of the talus. Clin Orthop 1963; 30:38.) |
the anastomotic sling in the tarsal canal and tarsal sinus. Many
branches of the sling enter the inferior aspect of the neck and course
posterolaterally. Additional blood supply originates from the deltoid
branches of the posterior tibial artery, contributing significantly to
the medial third of the talus. Branches of the peroneal artery may make
a minor contribution posteriorly, around the posterior process. The
talar head is supplied by branches of the dorsalis pedis arising from
the dorsal neck vessels and also from the artery of the tarsal sinus.
demonstrated that undisplaced fractures of the talar neck are
associated with intraosseus disruption of the branches of the arteries
of the tarsal sinus and tarsal canal. However, the major vascular sling
should remain intact. With increasing displacement, branches from the
dorsalis pedis artery as well as the artery of the tarsal canal and
artery of the tarsal sinus can be disrupted. These findings confirm the
clinical observation that the rate of osteonecrosis depends upon the
degree of fracture displacement.20,73
upon the development of complications. These include, in particular,
osteonecrosis of the talar body, osteoarthritis of the subtalar joint
and the ankle joint, delayed union, nonunion, malunion, and infection.
Treatment should be directed to an early anatomic reduction of the
talar neck fracture and, where possible, avoidance of complications.
Anatomic union, not associated with complications, frequently results
in an excellent outcome for the patient despite this devastating injury.171
of the talar neck. Nonoperative treatment should only be considered for
fractures in which there is no displacement of the fracture line and no
incongruity of the subtalar joint. According to the Hawkins
classification system, only type I fractures can be treated
nonoperatively. When nonoperative treatment is selected, confirmation
of the anatomically maintained reduction should be obtained with a CT
scan.22 Fractures that appear to be
slightly displaced are commonly associated with incongruity of the
subtalar joint. If subtalar incongruity is present, the injuries should
be classified as type II fractures and treated with anatomic reduction.
fracture includes immobilization and nonweight bearing until clinical
and x-ray signs of fracture healing are present, which can last up to
12 weeks. Nonweight bearing is usually required for at least the first
4 to 6 weeks of treatment.1,2,15,19,20,30,42,73,92,156,162
talar neck; however, achieving a closed reduction can be very
difficult. It is often preferable to proceed directly to open reduction
and internal fixation, thereby avoiding repeated failed attempts at
closed reduction. However, when operative intervention will be delayed,
and in type II fractures in particular, closed reduction can be a
helpful initial treatment step (Fig. 58-12).
firstly, adequate analgesia and sedation. The essential technique
involves bringing the foot, including the talar head, to the residual
talar body fragment. This requires the talar body to be reduced within
the ankle mortise. In the type II fracture with subluxation or
dislocation of the subtalar joint, a reduction is most likely to be
successful with the knee flexed and the foot flexed plantarward. This
relaxes the gastrocsoleus complex and brings the talar head fragment
into proper relation to the body. At that point, any varus or valgus
malalignment can be corrected as well. Once the reduction is achieved,
excessive dorsiflexion will cause a redisplacement of the head
fragment, and therefore radiographs to confirm reduction should be
performed with the foot in a comfortable position of equinus.
requires plantarflexion and varus positioning of the foot. In some
cases, closed reduction is aided by the use of a transverse pin placed
through the calcaneus to apply traction. However, direct traction also
increases the soft tissue tension around the ankle including the flexor
tendons, the posterior tibial tendon, and even the deltoid ligament. A
closed reduction may be more difficult if the tissues are overly
tensioned. Direct pressure on the talar body fragment is often required
to reduce it relative to the medial malleolus. However, direct
pressure, applied for too long or with too much force, can increase the
risk of complications particularly related to skin necrosis. Therefore,
this maneuver should be performed with care.
 |
|
FIGURE 58-12 Closed reduction of a talar neck fracture. Lateral radiograph demonstrating alignment prereduction (A) and postreduction (B) of a Hawkins type II fracture. Note some displacement persists.
|
reduction is achieved, one can consider percutaneous screw fixation to
stabilize the talar neck fracture. Cast treatment can also be
considered but requires positioning the foot in equinus for
approximately a month to maintain the reduction. Subsequent casting can
be performed to gradually bring the foot out of equinus as long as the
reduction is maintained. Nonweight bearing immobilization is usually
required until union is achieved.
standard treatment for all displaced talar neck fractures. Operative
treatment is indicated to achieve an anatomic reduction of the talar
neck fracture. Displacement of the talar neck is associated with
subluxation or dislocation of the posterior facet of the subtalar
joint. As noted by Adelaar,2
subluxation of the posterior facet of the subtalar joint results from
disruption of the interosseous talocalcaneal ligament. The talar body
assumes a plantarflexed, malaligned position usually also associated
with varus deformity. Sangeorzan et al.174
demonstrated the importance of even slight deformity of the talar neck.
In their biomechanic study, residual displacements of as little as 2 mm
altered the contact characteristics of the subtalar joint. Daniels et
al.33 performed a biomechanic study
using cadaver specimens and demonstrated that varus malalignment of the
talar neck is associated with forefoot adduction, calcaneal internal
rotation, and loss of subtalar motion. Severe displacement of the
fracture fragments can cause skin tenting and necrosis. When the skin
is at risk, prompt reduction of severe malaligment is critical to
lessen skin complications and infection.
neck fracture. Considerations for which approach to use include the
degree and location of comminution, the potential need for malleolar
osteotomy (for reduction and visualization purposes), and preservation
of the remaining vascular supply.
used. The incision is made directly over the talar neck and medial to
the anterior tibial tendon. For fractures that extend more posteriorly
into the talar body, the incision can be sited slightly posterior,
midway between the anterior and posterior tibial tendons, to facilitate
the creation of a medial malleolar osteotomy. When fractures of the
talar neck are associated with malleolar fractures, the use of a medial
incision will facilitate reduction and fixation of the medial malleolar
fragment. In some cases, open reduction is difficult, and the talar
body is rotated around the deltoid ligament which may be the only
remaining soft tissue attachment. In such instances, osteotomy of the
malleolus is preferable to cutting the deltoid ligament to achieve a
reduction. Osteotomy of the malleolus may preserve the deltoid ligament
and thereby protect what may be the only remaining source of
vascularity for the talar body.156
For the more distal talar neck fracture, an incision just medial to the
anterior tibial tendon is usually sufficient to provide direct access
to the fracture site to visualize and manipulate both fragments. The
anteromedial incision can be performed without exposing the anterior
tibial tendon and leaving it within its sheath. Subsequently, an
incision down to bone can be performed, elevating full thickness flaps
from the anteromedial aspect of the tibia to facilitate exposure of the
talar neck.
damage to the blood supply of the talus, and it provides adequate exposure of the fracture.156
In many cases, a cortical fragment is visible at the anterolateral
corner of the talar neck fracture at the anterior margin of the lateral
process, upon which one may base an anatomic reduction. Exposure of the
lateral aspect of the talus and the subtalar joint requires extra
caution to avoid injury to the blood vessels of the sinus tarsi.
additional option for reduction. It is often performed in conjunction
with an anteromedial incision to facilitate exposure of the subtalar
joint. This approach requires inferior mobilization of the extensor
digitorum brevis muscle. Caution should be exercised around the sinus
tarsi to protect the vessels therein. The direct lateral approach
facilitates good visualization of the subtalar joint especially in the
case of comminuted fractures with extension into the subtalar joint.
Like the anterolateral approach, visualization of the lateral process
facilitates placement of a “shoulder screw” or lateral plate to
stabilize the fracture.
fixation of the talar neck fracture. Directing the screws from
posterior to anterior facilitates their placement perpendicular to the
fracture line, thereby achieving compressive lag screw fixation. In
some cases, a posteromedial approach is performed to facilitate
reduction of a type III talar neck fracture. A malleolar osteotomy can
be performed through this approach in cases where the deltoid ligament
is intact and the talar body is rotated posteriorly between the
posterior tibial tendon and the medial malleolus. Reduction can be very
difficult and is facilitated through the use of a calcaneal traction
pin in addition to the malleolar osteotomy.
facilitate lag screw fixation. Posterior screw fixation involves some
removal of the posterior articular cartilage of the talus and may
increase the risk of neurovascular injury. Therefore, posterior screw
fixation or other posterior approaches should be used with care to
minimize surgical complications.
 |
|
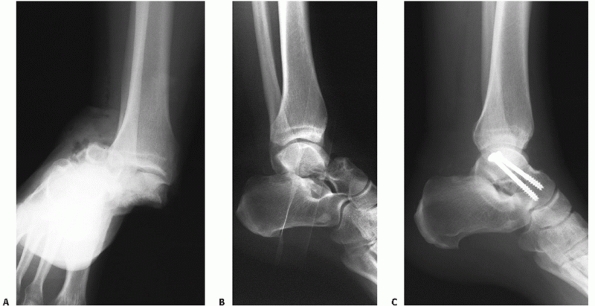
FIGURE 58-13
Closed reduction followed by posterior-to-anterior screw fixation of a noncomminuted type II fracture. The initial injury films are difficult to interpret but demonstrate a subtalar dislocation (A). An attempt at closed reduction partially reduced the subtalar joint but left residual subluxation (B). Formal closed reduction was accomplished in the operating room and stability was achieved with two posterior-to-anterior screws (C). |
In comminuted fractures, judgment of an anatomic reduction can be
difficult. The use of an anteromedial approach combined with a direct
lateral approach affords a slightly larger skin bridge between the two
incisions compared to the combined anteromedial and anterolateral
approach. Combined approaches should be performed with caution to
protect the tenuous blood supply to the talar body such that, in
particular, the arteries of the tarsal sinus and tarsal canal are
protected. The use of a combined approach facilitates preservation of
the blood supply through any remaining dorsal neck vessels by avoiding
excessive retraction on the anterior skin bridge.
in recent large series of talar neck fractures. Thirty eight out of 70
talar neck fracture-dislocations from one center were treated with dual
approaches.171 Four patients from
the group of 70 developed an early infection requiring reoperation. In
another series of 102 talar neck fractures from a large trauma center,
dual anteromedial and anterolateral approaches were used for 91
fractures. Of 60 fractures that were evaluated for complications, 5
developed skin complications of wound dehiscence and superficial or
deep infections.202
presents with confirmed anatomic alignment, percutaneous fixation can
be used to facilitate early range of motion as opposed to cast
treatment. The fixation can be inserted from posteromedial,
posterolateral, or anterior. Screws placed perpendicular to the
fracture line are used to lag the fracture fragments together. Due to
the proximity of the sural nerve posterolaterally and the neurovascular
bundle posteromedially, it is worthwhile to perform careful blunt
subcutaneous dissection to avoid neurovascular injury.52,149
stabilization has been accomplished, appropriate internal fixation can
be employed for definitive stabilization. Swanson et al.,188
using mathematical modeling, calculated that the theoretical maximum
shear force across the talar neck during active motion was 1129
Newtons. Internal fixation of the talus should ideally be sufficient to
withstand the theoretical forces involved with active motion until
healing has occurred.
fractures. They can be inserted from anterior to posterior or posterior
to anterior. Posterior screw insertion provides the advantage of
allowing screw placement perpendicular to the fracture line and,
therefore, perhaps improving compressive rigidity while avoiding shear
with screw placement. In the mechanical study of Swanson et al.,188
posterior screw fixation was sufficient to withstand the theoretical
shear forces of active motion. Cannulated screws are useful as the
direction of screw travel requires careful fluoroscopic visualization
and frequent redirecting of the guide wire is often necessary to
achieve the desired screw position. Only a limited window posteriorly
is available for correct screw insertion.45 Multiple cannulated screw sizes are available, and frequently a smaller screw is preferable. Thordarson et al.198
recommended the use of titanium screws to facilitate the later use of
MRI scans in the assessment of osteonecrosis of the talus.
many cases, it is not possible to insert anterior screws perpendicular
to the fracture site. Removal of a small amount of cortical bone using
a rongeur or a countersink adjacent to the screw head may allow
improved screw direction. Stabilization of comminuted fractures may be
performed with the use of noncompressive or “buttress” screw
techniques. Lag screw techniques can be employed for noncomminuted
fractures. On the anterolateral side, a shoulder of bone often exists
when the talar neck fracture extends into the lateral process directly
adjacent to the subtalar joint. In many instances, the inferior segment
of the lateral column of the talus fails in tension while the dorsal
and medial aspects of the talar neck are comminuted. The inferior
margin of the lateral column may therefore be noncomminuted. In this
area, a reduction can often be visualized and a compressive screw
inserted. This so-called “shoulder screw” runs from anterolateral to
posteromedial in areas of the talus where the bone is denser, and
compression along this axis does not cause varus malalignment (Fig. 58-14).45
plates has facilitated improved fixation of talar neck fractures. These
can be particularly useful for comminuted talar neck fractures in which
bridging of comminuted zones on the medial or lateral columns may be
required (Fig. 58-15). Use of plates around the
talar neck fracture often requires some caution as the hardware can
easily be prominent and potentially cause damage to the malleolar
cartilage. In some cases, countersinking of the plates is required, but
in general, careful placement of the hardware on the nonarticular
regions of the talus facilitates plate use. Lateral plate placement is
simpler than medial placement, as a large nonarticular region near the
inferior margin of the lateral surface extends from the talar head
cartilage to the lateral process. This area can often accommodate a
four-hole, contoured plate 2.4 or 2.7 mm in thickness. Medially, less
surface area is available but two- and three-hole plates may be
judiciously applied. Fleuriau Chateau et al.54
described a series of 23 patients with comminuted talar neck fractures
treated with medial, lateral, or combined medial and lateral plate
fixation. Four patients required hardware removal, but only two
patients developed a malunion.54 The development of appropriate sized implants has been critical to effective plate fixation in talar neck fractures.
In a cadaver study of comminuted talar neck fractures, the stiffness
and ultimate strength of an anteromedial blade plate was equivalent to
posterior screw fixation. In both techniques, the strength exceeded the
theoretical shear force across the talar neck and provided
approximately 25% greater strength compared to anterior-to-posterior
screw fixation.6 In a separate biomechanic study, Charlson et al.25 noted no mechanical advantage of lateral plate and medial screw fixation compared to posterior-to-anterior screw fixation.
indicated for talar neck fractures. The healing of the talar neck
occurs generally by creeping substitution and primary bone healing as
opposed to callus formation. As such, absolute stability with plate and
screw fixation is preferred. However, external fixation may have a role
in situations in which talar neck fracture fixation is delayed, as a
means of maintaining the reduction of the ankle and subtalar joints (Fig. 58-16).
As well, external fixation can have a role in the case of highly
contaminated open fractures to facilitate soft tissue management.
Finally, external fixation has a role following talectomy as a
temporary means to maintain length and alignment while further surgical
intervention is being determined.
commonly employed for talar neck fractures. As a rule, prompt reduction
and stabilization is preferred. However, it is sometimes a requirement
due to multisystem injury or severe soft tissue compromise to delay
reduction. In those cases, in which reduction must be delayed, open
reduction and internal fixation can still be accomplished with a
reasonable expectation of an acceptable outcome. In other words,
fracture healing can still be anticipated even when surgery is delayed.114 Huang et al.80
reviewed 9 patients treated between 4 months and 4 years after injury;
all 9 achieved union, although 1 patient developed osteonecrosis
requiring ankle arthrodesis. Whether complications are more frequent
following delayed surgery is unknown. Osteonecrosis may be more likely
when surgery is delayed; however, most studies in which early versus
late surgery were compared have been unable to detect a difference.50,114,171,202
situations of necessity. In some cases of open talus
fracture-dislocation, the talus is lost at the scene of the injury in
which case there is no possibility of talar repair. In other
situations,
the
bone is comminuted such that replacement of the talus within the ankle
mortise is considered impossible or unlikely to result in successful
outcome. The principles of talectomy include maintenance of length and
alignment with the use of spanning external fixation, followed by
tibiocalcaneal fusion. Isolated case series describe reasonable results
following talectomy. Gunal et al.66
described a technique of talectomy in 4 patients, including lateral
translation of the medial malleolus, and reported good results in 3 out
of 4 patients. Kharwadkar et al.98
describe a case of primary talectomy for a patient with a type III
talar neck fracture with full restoration of activity level and durable
results after 15 years of follow-up. In general, however, results of
talectomy are probably worse than the results of talus reduction and
stabilization. Therefore, in the case of a dislocated extruded talus or
talar body, it is reasonable to attempt to replace it within the
mortise, provided it is possible to achieve a clean surgical bed.
Irrigation and débridement of the bone and the soft tissue is
performed, followed by reimplantation of the clean talus. External
fixation is helpful to stabilize the joints and the associated soft
tissues and to facilitate wound care. Union can be obtained, even
through a completely avascular talar neck fracture, by creeping
substitution, although this may occur very slowly. It is not uncommon
to see evidence of complete sclerosis of the talus 4 to 6 months after
reimplantation, suggesting complete osteonecrosis. Smith et al.181
reviewed a large series of 27 patients with an extruded talus in whom
the strategy of preserving and reimplanting the talus was followed.
Nineteen patients attended review after a minimum of 1 year. Infection
complicated treatment in only two of the patients, one of whom had a
partial talar excision acutely. Secondary surgery was commonly
necessary. Ultimately, however, revascularization occurred in most
patients.181 Although osteonecrosis
with collapse might be expected in most, if not all, patients with a
reimplanted talus, it appears that some cases can successfully
revascularize without collapse. Brewster et al.16
reported on two cases of reimplanted extruded taluses which
revascularized without collapse. As such, wherever possible, treatment
of the completely dislocated talus will include replacement of the
talus within the ankle mortise, followed by appropriate fixation, wound
care, and rehabilitation to preserve the anatomy of the hindfoot.
 |
|
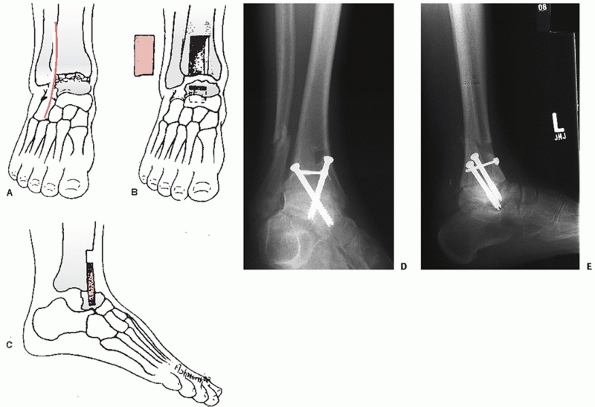
FIGURE 58-14
Intraoperative and postoperative views of a type II talus fracture treated with anterior-to-posterior screw fixation including a lateral shoulder screw. Anteroposterior (A), lateral (B), and Canale (C) views are shown following open reduction and internal fixation. Postoperative anteroposterior (D) and lateral (E) views 6 weeks later clearly demonstrate subchondral resorption of bone indicating vascularity of the talar body (Hawkins sign). |
 |
|
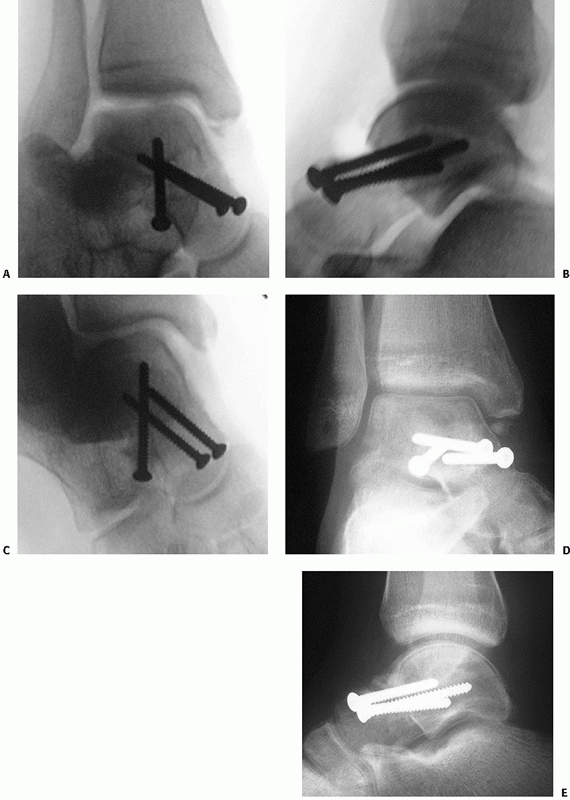
FIGURE 58-15 Anteroposterior (A) and lateral (B)
intraoperative views of talus fracture fixation. Periarticular lateral plate fixation is demonstrated, using a 2.4-mm plate extending from the anterior margin of the talar head to the lateral process. This plate is spanning a comminuted talar neck fracture with medial bone loss. An anteromedial screw was used to stabilize the medial column and a supplemental anterolateral screw was used to stabilize a large lateral process fragment. |
fractures. Undisplaced, Hawkins type I fractures can be treated well
with closed methods. A short leg nonweight bearing cast is applied
initially. I prefer a cast applied in neutral position followed by
repeat plain radiographs and CT scan to confirm maintenance of
reduction. If any displacement of the subtalar joint is noted, the
classification of the fracture should be reconsidered and open
reduction and internal fixation will be required. If cast treatment is
successful at maintaining the reduction, the patient is asked to remain
nonweight bearing for a period of approximately 6 weeks or until there
is some radiographic evidence of healing. Subsequently, patients are
converted to a removable brace to begin active range of motion
exercises. CT is useful at multiple intervals: to confirm the fracture
is undisplaced, to confirm that the reduction has been maintained, and
to confirm that union has occurred. Patients are warned against
excessive weight-bearing activity until revascularization appears to be
complete.
dislocations require prompt reduction. When possible, immediate closed
or open reduction of the dislocated joints is performed. An attempt at
a closed reduction of a type II fracture can be performed under
adequate anesthesia. Type III or IV fractures are usually not reduced
with closed techniques. If an anatomic closed reduction is
accomplished, internal fixation is inserted using percutaneous or open
techniques to achieve stability and facilitate early mobilization. If
percutaneous stabilization is performed, it is important to confirm
that the reduction is anatomic. I have been surprised on several
occasions that a reduction which appeared to be anatomic following
closed reduction was found to be malrotated upon surgical exposure.
Therefore, an open reduction should be performed if there is any doubt
about the quality of the reduction.
 |
|
FIGURE 58-16
Hawkins type III fracture treated with temporary spanning external fixation followed by definitive plate fixation. Anteroposterior (A) and lateral (B) images with the external fixator in place demonstrate residual displacement of the talar neck fracture. A clinical photo 10 days postinjury demonstrates resolution of soft tissue swelling with persistent deformity (C). Anteroposterior and lateral radiographs (D,E) 8 weeks following definitive open reduction, plate fixation, and an intercalary tricortical iliac crest bone graft demonstrate maintenance of alignment but sclerosis of the talar body, suggesting avascularity. The dorsal plate fixation used in this case required countersinking of the plate at the articular margin to avoid restriction of tibiotalar motion. |
I prefer an initial anteromedial approach to visualize the medial
aspect of the talar neck as a standard approach for noncomminuted
fractures. A slightly more posterior placement of the skin incision
facilitates the addition of a medial malleolar osteotomy, if required.
In the large majority of fractures, particularly if comminution is
noted, a second approach is performed to confirm an anatomic reduction.
A direct lateral or anterolateral approach is added to the medial
incision to facilitate visualization of the lateral aspect of the
fracture and for placement of hardware. The lateral side is often the
tension side of the fracture such that less comminution is present, and
therefore the surgeon’s ability to judge the reduction may be much
better on the lateral compared to the medial side. The lateral approach
is performed in all except the most simple of fracture patterns.
Dissection around the sinus tarsi and across the dorsal talar neck is
performed carefully to maintain any soft tissue attachments.
achieved, accomplishing a reduction is sometimes challenging. Useful
adjuncts include a calcaneal traction pin or distractor and the use of
a malleolar osteotomy, especially for type III or IV fractures.
Reflection of the medial malleolus distally facilitates a gentler
closed reduction compared to direct manipulation and is more likely to
preserve the talar blood supply via the deltoid ligament.
percutaneously, I prefer posterior to anterior screw fixation with an
associated small incision posterolaterally to facilitate visualization
of the corner of the subtalar joint and to avoid the sural nerve.
Percutaneous screw placement from posterolateral to anteromedial allows
screw insertion perpendicular to the primary fracture line, which may
avoid creating malalignment and improve stability.
compression screw techniques to address a noncomminuted fracture and
minifragment plates or their equivalent to address the comminuted
medial or lateral column. On occasion, dual plates are necessary for
highly comminuted talar neck fractures, and I have generally been
satisfied with the stability that has been achieved. Additional screws
can then be inserted perpendicular to the primary fracture line for
additional stability. The size of screws used depends upon the size of
the talar fragments. Usually 2.7- or 3.5-mm screws are used to
stabilize the primary fracture fragments, with smaller 2.0- or 2.4-mm
screws for comminuted fragments. Both 2.4- and 2.7-mm plates are
available and can be contoured to the medial or lateral column.
Placement of the plates inferiorly, close to the plantar surface of the
talus, allows a longer plate to be used. On the lateral side, a
four-hole plate beginning at the talar head cartilage can often be
contoured to extend to the anterior surface of the lateral process.
Screw insertion should be directed perpendicular to the plate. Good
fixation through the plate is usually achieved (see Fig. 58-15).
Medially, less surface area is available for plate placement, and
options may be restricted to a two- or three-hole plate. Adjuvant
anterior-to-posterior directed screws will further enhance the
stability of the construct.
|
TABLE 58-1 Fixation Options for Talar Neck Fractures: Pearls and Pitfalls
|
|||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
along the lateral shoulder of bone allows an ideal screw insertion
point and facilitates compression across the fracture line. The
anterolateral shoulder screw is useful to avoid malalignment and
facilitates compression of the fracture on the tension side.
comminution is noted, involving the subtalar joint. I visualize the
subtalar joint directly through the lateral approach to excise debris
and ensure an anatomic reduction of the subtalar joint.
immobilizing non-weight-bearing splint for the first month after a
talar neck fracture. Gentle range of motion exercises begin once the
incisions are definitely healed. However, nonweight bearing is usually
prolonged up to approximately 3 months following the injury. Patients
are counseled early about the importance of nonweight bearing to
protect the talar body during the revascularization phase. Where
evidence of revascularization with impending collapse is noted, I
discuss the use of a patellar tendon bearing brace with patients. This
may be worn until revascularization is complete.
In many cases, this is complicated by comminution, particularly when
the talar neck fracture is combined with a talar body fracture. In
these cases, the use of multiple surgical approaches is valuable; one
approach directed to the noncomminuted side (if one exists) is of
particular value to evaluate the reduction, and the second approach is
used to strut the comminuted
column
with a plate. The development of appropriately sized implants has
improved the surgeon’s ability to achieve stability in talus fracture
surgery. Reduction of the dislocated talus can be surprisingly
difficult. The simplest means of addressing this usually involves a
medial malleolar osteotomy. An extensile incision is similarly
beneficial because the soft tissues that normally lie posterior to the
medial malleolus are often displaced around the fracture trapping the
talar body in a dislocated position.
The frequency of complications seems to be particularly dependent upon
the severity of the initial injury, such that Hawkins classification
continues to be very relevant. Recent reports171,202
have also highlighted the importance of fracture comminution as a
predictor of complications. Also notable is the comparatively good
function which can be achieved in the absence of osteonecrosis and
other complications.171
injured. Infection can be a problem in both closed and open fractures
of the talus. Deep infection is, without question, a devastating
complication. The older literature notes the severity of this
complication. Syme,189 in 1848,
described a series of 11 deaths in 13 patients with open
fracture-dislocations of the talus, all resulting from infection. He
recommended a trans-tibial amputation as appropriate treatment. Other
more recent reports have also noted the dangers of deep infection.20,58,150
extremely challenging. The avascular body of the talus acts as a large
necrotic sequestrum. Surgical débridement, including talectomy, may be
necessary to achieve control of the infection. Excision of the necrotic
talus combined with delayed tibiocalcaneal fusion can still achieve
reasonable results in terms of hindfoot alignment and stability.20,123,150,156
with a risk of 0% to 13%. In fracture dislocations, the risk increases
to 20% to 50% in type II fractures and to over 80% in type III
fractures. The incidence of osteonecrosis varies among published
reports and is somewhat dependent upon the diagnostic criteria used but
in general, the incidence correlates with the Hawkins classification.126 The overall incidence of osteonecrosis is between 21% and 58%, making it a common complication of talar neck fractures.20,73 The risk of osteonecrosis seems to be less in more recent reports171,202
compared to the older literature. This may be related to improved
surgical techniques for preserving blood supply to the talus or to
better implants that provide greater stability to facilitate
revascularization.
the talar body demonstrates increased density compared with the
surrounding bone, which is vascularized and undergoing disuse atrophy.
Later, as revascularization occurs, there is partial or complete
collapse of the subchondral bone, narrowing of the joint space, and
occasionally fragmentation of the talar body.
As noted by Hawkins, “The time to recognize the presence of avascular
necrosis is between the sixth and the eighth week after the
fracture-dislocation. By this time, if the patient has been
non-weight-bearing, diffuse atrophy is evident by roentgenogram in the
bones of the foot in the distal part of the tibia. An anteroposterior
roentgenogram of the ankle made with the foot out of the plaster cast,
reveals the presence or absence of subchondral atrophy in the dome of
the talus. Subchondral atrophy excludes the diagnosis of avascular
necrosis.”73,143
have pointed out that Hawkins’ sign has a high degree of sensitivity
but only moderate specificity. The extent of involvement of the talar
body can be quite variable.111 In
some cases, partial osteonecrosis is noted, particularly in type II
fractures. In many type III injuries, the entire talar body blood
supply is disrupted resulting in osteonecrosis of the entire talar
body. Tehranzedeh et al.194 describe
three cases of a partial Hawkins sign following fractures of the talus
and suggested the partial Hawkins sign may correlate with disruption of
end arteries within the body of the talus. The reliability of Hawkins’
sign was recently studied in 31 patients with displaced talar
fractures. No patient who developed osteonecrosis had a positive
Hawkins sign; however, the absence of Hawkins sign was not universally
associated with the development of osteonecrosis.195
include technetium bone scan and MRI. The use of bone scanning with a
pin-hole collimator158 can be
effective but has largely been replaced with MRI. MRI can be used as
early as 3 weeks postinjury and defines not only the presence but also
the extent of osteonecrosis, as well as the condition of the articular
cartilage (Fig. 58-17).2,180,196
treatment remain a source of controversy. Osteonecrosis does not
necessarily preclude a reasonable outcome. Union can occur in the
presence of osteonecrosis, provided the fixation is stable. Prolonged
periods of non-weight bearing have been recommended
because
the talus is revascularized slowly via creeping substitution of
necrotic bone with vascularized bone. This process may require up to 36
months.122,123
Such a long duration of non-weight bearing is unpredictable, relatively
impractical, and difficult to adhere to for patients. One alternative
solution is the use of a patellar tendon bearing orthosis. Saltzman et
al.169 evaluated the effect of
patellar tendon bracing in Charcot arthropathy and determined that
force transmission to the hindfoot was reduced by 37%. The brace also
reduces varus and valgus stresses to the hindfoot.
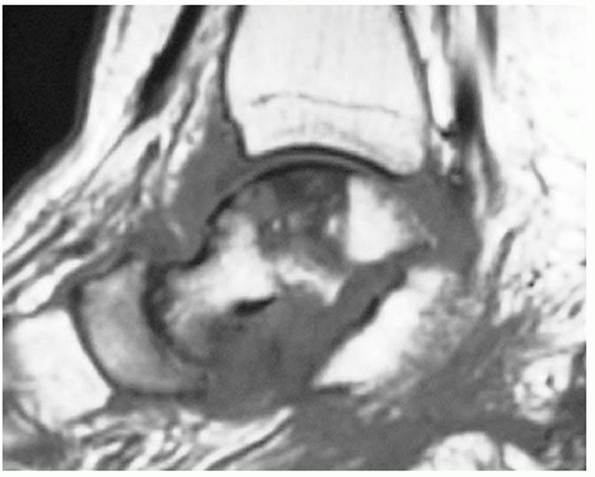 |
|
FIGURE 58-17
This T1-weighted MRI scan was obtained 6 months after a talar fracture-dislocation and demonstrates osteonecrosis of the talar body. The region of osteonecrosis corresponds to the distribution of the artery of the tarsal canal. The scan also demonstrates arthritis of the talonavicular and subtalar joints, subluxation of the subtalar joint, and extensive fluid accumulation around the talus in keeping with a diagnosis of infection. |
are numerous. Some authors have recommended immediate surgical
treatment. Options have included primary triple arthrodesis,123 total talectomy with tibiocalcaneal fusion,166 talectomy alone,15 subtalar fusion,103,104 pantalar fusion,64
and primary tibiotalar fusion. In most cases, however, the
recommendation is for a relatively conservative approach in which
osteonecrosis of the talus can be treated expectantly with preservation
of the talar body fragment. Anatomic reduction and fixation are
maintained, and primary arthrodesis is not indicated.
describe successful efforts to revascularize the necrotic talus. Hussl
et al.81 describe a technique using vascularized corticocancellous iliac crest bone graft to prevent collapse. Mont et al.135
performed a variation of core decompression of the talus in 17 ankles
with symptomatic nontraumatic osteonecrosis without collapse. Often,
however, the patient with osteonecrosis will present with associated
collapse, in which case the treatment is directed toward relief of pain
symptoms and restoration of alignment.
 |
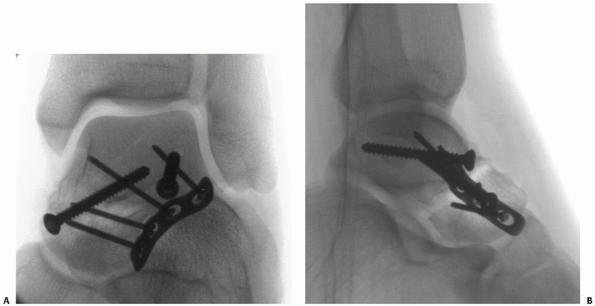
|
FIGURE 58-18 Blair fusion. Schematic drawing showing the anterolateral incision (A), sliding graft from the distal tibia (B), and the sliding graft embedded into the talar neck and head fragment (C).
Note the space left by removal of the talar body. (Blair HC. Comminuted fractures and fracture dislocations of the body of the astragalus: operative treatment. Am J Surg 1943;59:38.) D,E. Radiographs demonstrate a healed modified Blair fusion 2 years following a type III talar neck fracture with the sliding graft incorporated. The talar body has been retained and remains sclerotic, but appears to be healed to the distal tibia. |
instances, collapse of the entire talar body can occur while leaving a
relatively congruent ankle joint. The function of these ankles is not
normal, but may be acceptable to the patient. Partial collapse of large
segments of the talar body is often associated with severe hindfoot
malalignment and irregularities in the articular cartilage such that
further treatment is commonly necessary to relieve symptoms.
collapse of the talar dome and the development of symptomatic arthritis
of the ankle joint. For these patients, ankle arthrodesis is indicated.
Tibiocalcaneal arthrodesis and the Blair or modified Blair fusion have
been found effective. Blair12
described a technique of ankle fusion in 1943 specifically designed to
treat osteonecrosis of the talus. He recommended excision of the
avascular talar body and placement of a sliding corticocancellous graft
from the anterior distal tibia into the residual, viable talar head and
neck (Fig. 58-18). Modifications of this
technique include screw fixation of the sliding anterior distal tibial
graft, suggested by Lionberger et al.,115 and retention of the talar body. Authors such as Morris et al.137 and Dennis and Toulos37
have reviewed case series and recommend the modified Blair fusion as a
satisfactory reconstructive treatment after severe talar injuries.
Recently, Shrivastava et al.179
presented a series of eight patients who underwent primary Blair
tibiotalar arthrodesis for Hawkins type III fractures of the talar
neck, most of whom
presented
on a delayed basis. Although results were not uniformly good in this
challenging group of patients, 6 of the 8 patients were described as
achieving a good result.179
Benefits of the Blair fusion include a normal appearance of the foot,
minimal shortening, and potential retention of some subtalar function.
which fusion of the calcaneus to the distal tibia is performed.
Intercalary graft can be used to facilitate a hindfoot arthrodesis.166 Results have been noted to be superior to talectomy or ankle fusion by Canale and Kelly.20
Proponents of this procedure note that the fusion of the tibia to the
calcaneus may provide more stability compared to the sliding graft
technique. The use of intercalary material is required if the length
and appearance of the hindfoot is to be maintained.
complication. In many cases, however, the radiographic appearance of
osteonecrosis does not universally imply permanent disability. Current
recommendations are to reconstruct the talus at the time of injury with
an anatomic reduction and stable fixation. Weight bearing in the
presence of osteonecrosis can be facilitated with the use of a patellar
tendon bearing orthosis. Further surgical intervention should be
directed to the patient’s symptoms as many patients with osteonecrosis
do not require further surgery once healing is complete and
revascularization has proceeded. Treatment should be directed to
improve symptoms where necessary, and in these patients a Blair fusion
or tibiocalcaneal arthrodesis is most commonly indicated.
result following talar neck fractures. In one series of 46 patients,
Peterson et al.159 achieved better
results in type III fractures compared to type II fractures. The
critical variable was the adequacy of the initial reduction, with an
exact reduction being achieved more frequently in patients with type
III fractures.159 Miller felt that
“the ability to obtain and maintain an anatomic reduction (closed or
open) is the most important factor in predicting good results.”128 Hawkins73
noted that a good to excellent result is the expected outcome following
anatomic reduction of a talus fracture-dislocation not complicated by
osteonecrosis.
Obtaining an anatomic reduction can be difficult to assess,
particularly when using closed means. The use of lateral radiographs
and a Canale view are helpful to avoid achieving an inadequate
reduction. The fixation devices used should be carefully selected to
avoid creating a malreduction and to achieve adequate stability. For
example, in fractures with medial comminution, the use of compression
screw fixation on the medial aspect of the talar neck will inevitably
compress the medial column, leading to a varus malunion. In addition,
in patients in whom union is slow to occur, the progressive development
of a malunion is sometimes noted. Patients should therefore not
progress to full weight bearing until union is solid.
Commonly, malunion in varus occurs, often accompanied by a malrotation
resulting in a supination deformity of the foot. Daniels et al.,33
in a cadaver study, noted that removal of a medially based wedge of
bone from the talar neck resulted in varus deformity, internal rotation
of the hindfoot, adduction of the forefoot, and loss of subtalar motion.
noted that 14 of 30 patients with type II fractures treated in a cast
developed a varus malunion. More recent reports have also documented a
high incidence of varus malunion. In one study of patients with
high-energy fractures treated with screw fixation, a varus malunion
developed in 40% of patients.171 The use of plate fixation may be associated with a lower incidence of malunion,54,202
although there are currently no studies comparing the techniques.
Recognition of a malunion is important but can be difficult. A recent
study compared the accuracy of a variety of imaging techniques to
detect talar neck malunion. Chan et al.22
noted that investigators studying plain radiographs, radiostereometric
analysis, and CT scans all underestimated the degree of malunion of
talar neck fractures. Translational deformities were best measured by
CT, but rotational abnormalities were equally underestimated by all
three imaging techniques.22
Often, however, reconstruction of the malunion is more complicated.
Options include calcaneal osteotomy, calcaneal osteotomy combined with
midfoot osteotomy, direct osteotomy of the talar neck,133
and triple arthrodesis for severe malalignment associated with
degenerative changes. A recent series of 10 patients with malunion or
displaced nonunions reported good results by reconstruction of the
talar alignment and revision fixation in all patients, without the need
for arthrodesis of the adjacent joints.165
It is likely generally underdiagnosed, but clinically important. Varus
malunion results in subtalar stiffness, excessive weight bearing on the
lateral side of the foot, and it is frequently painful. Over time,
associated soft tissue structures become contracted such that these
contractures may need to be attended to at the time of reconstructive
osteotomy surgery (Fig. 58-19). Subtalar or triple arthrodesis is often required to achieve alignment and deal with secondary degenerative changes.
both can occur after fractures of the talar neck. The development of
subtalar arthritis is particularly common.171
Osteoarthritis may be noted in the presence or absence of
osteonecrosis. The causes of osteoarthritis, in addition to
osteonecrosis, include cartilage damage, joint stiffness, and
malalignment. In many cases, substantial damage to the inferior
articular margin of the talus articulating with the posterior facet of
the calcaneus is noted at the time of talar fracture-dislocation. This
may be a contributing factor to subtalar arthritis. In addition to
cartilage damage from the injury, the prolonged period of non-weight
bearing and cast immobilization can lead to arthrofibrosis, impaired
nutrition of the articular cartilage, and secondary osteoarthritis. As
such, the combination of injury, osteonecrosis, and immobilization
ensure a high likelihood of arthritis in the peritalar joints. Even
relatively undisplaced talar neck fractures have been noted to have
decreased motion in both the ankle and subtalar joints, require a
prolonged time off of work, and develop a high incidence of
unsatisfactory results.32
in 46% to 69% of patients.20,50,116,171,175,190
Hindfoot symptoms may also be common but are not always due solely to
the development of arthritis. It is frequently necessary to localize
the source of symptoms to the arthritic joint prior to proceeding to
surgical intervention. Selective joint infiltration with local
anesthetic can be useful as an assistive diagnostic modality. This may
require fluoroscopic localization to determine the exact needle
placement. An injection of local anesthetic into the symptomatic joint
which provides complete pain relief can be a useful indication for
arthrodesis.
 |
|
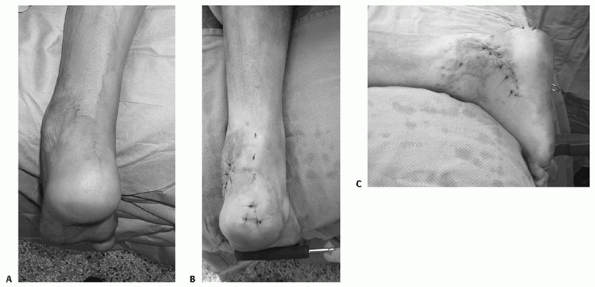
FIGURE 58-19 Reconstruction of talar neck malunion. A. Preoperative clinical photograph demonstrates varus deformity. B,C.
Postoperative clinical photographs following tendo-Achilles lengthening and a calcaneal osteotomy demonstrate restoration of neutral alignment. |
can begin. The use of anti-inflammatory medications, protected weight
bearing, and bracing may be helpful. Failure of these conservative
measures leads to surgical intervention, usually arthrodesis of the
involved joints. Subtalar and ankle fusion in the presence of a talar
neck fracture can be performed using standard techniques, although it
is often useful to confirm that the talar body is perfused prior to
proceeding to arthrodesis.
posttraumatic degenerative changes may be contraindicated after talar
neck fracture if osteonecrosis is present. However, if the talar body
is well perfused, ankle arthroplasty may be an alternative treatment
for selected cases of posttraumatic arthritis. At present, the use of
ankle replacement as a treatment option for posttraumatic arthritis in
young, active patients is a source of considerable controversy.28
uncommon injuries. Although a substantial body of literature exists
regarding treatment options, results, and outcomes, there are no
randomized trials comparing treatment strategies.
literature. Surgical timing is frequently discussed in the literature.
Since the classic articles of Hawkins,73 Canale and Kelly,20 Penny and Davis,156 and others,1,2,15,20,42,92,116,122,155,159
emergent treatment of talar neck fractures has been recommended. The
rationale for emergent treatment includes a reduction of osteonecrosis
rates related to earlier reduction and decreasing secondary soft tissue
injury. Recently, however, other authors have compared the results of
early and delayed treatment and found no difference. Lindvall et al.114
compared the results of surgery within 6 hours to delayed surgery in a
group of 26 isolated fractures of the talar neck and body, and found no
difference in the rates of union, osteonecrosis, or arthritis and no
difference in functional outcome. Other authors have had similar
findings.171,202
One should, however, consider that the power of a retrospective review
to detect differences in outcome related to surgical timing is very
limited by small numbers, differences in treatment techniques, and
variables in fracture and patient characteristics. Very large series of
talar neck fractures would be required to determine the benefit (if one
exists) of immediate versus urgent or delayed surgical treatment of
talar neck fractures.
plates as compared to screws for fixation and the use of biologically
active bone substitutes for grafting. These controversies are related
to the availability of new and better technologies. For example, the
use of small plates for stabilization has been a comparatively recent
phenomenon but seems to be evolving.54,202
Promising future considerations for talus fracture surgery include
improved technology in bone graft substitutes to potentially improve
union rates and perhaps eventually enhance revascularization. The use
of growth factors to enhance the vascular supply, in particular, may be
a promising area for further investigation.
minimally invasive techniques to reduce and stabilize talus fractures
and dislocations. The advantages of less invasive surgery include
improved maintenance of the soft tissue envelope around the fracture
and a more rapid, less painful recovery. However, the goals of surgery
must be respected, most importantly including
obtaining
an anatomic reduction. With respect to the talus, the irregular shape
of the bone and its articulations limits our ability to assess a
reduction using closed techniques in complex fractures. However, with
improvements in intraoperative imaging and percutaneous reduction
techniques, it may be possible to treat more talus fractures with less
invasive techniques in the future.
injuries. Complications following talar body fractures are similar to
those following talar neck fractures, including osteonecrosis,
arthritis of the ankle and subtalar joints, and prolonged disability.
Fewer reports in the literature exist related to fractures of the body
of the talus compared to talar neck fractures. Previously, this was
thought to be related to a much lower incidence of these type of
fractures compared to talar neck fractures. However, over the last two
decades, with the increase in survival following high-energy motor
vehicle collisions and the severe foot and ankle injuries that commonly
result, talar body fractures seem to be increasing in frequency.
Several recent reports in the literature have provided important
information related to these fractures.
compression of the talus between the tibial plafond and the calcaneus.
Common mechanisms of injury resulting in these fractures include motor
vehicle collisions and falls from a height. Depending upon whether the
force is more posterior or anterior and the relative plantarflexion or
dorsiflexion position of the ankle, the force may be directed through
the posterior or anterior aspect of the talar body. In many cases,
fractures of the talar body are associated with other fractures of the
foot and ankle.114 Combined talar neck and talar body fractures were noted in 40% of the talar body fractures in a recent study by Vallier et al.203
In that study, although falls were the most common mechanism of talar
body fractures overall, vehicular trauma was more common in combined
fractures of the talar neck and body.203
Other associated injuries include fractures of the malleoli, fractures
of the posterior and lateral talar processes, and fractures of the
calcaneus, particularly involving the sustentaculum.176
Because of the severe mechanism of injury, other associated injuries to
the lower extremities are also commonly noted in conjunction with
fractures of the talar body. Open talar body fractures are not uncommon
as well, occurring in approximately 20% of cases.203
intra-articular injuries in which the articular surfaces of the
tibiotalar and the subtalar joints are involved. Inokuchi et al.83
distinguished talar neck fractures from talar body fractures based upon
the location of the inferior fracture line relative to the lateral
process of the talus. Based upon the lateral radiograph, fractures
extending into or posterior to the lateral process of the talus are
defined as talar body fractures, whereas fractures anterior to the
lateral process are defined as talar neck fractures.
Fractures of the talar processes are considered separate from talar
body fractures; talar body fractures involve the articular surfaces of
the tibiotalar and subtalar joints. In general, the fractures can be
defined as shearing-type fractures or compression-type fractures. The
shearing-type fractures may occur either in the sagittal or the coronal
plane. The Orthopedic Trauma Association classification considers talar
body fractures according to the location of the fracture and the joints
involved (see Fig. 58-7). Talar body fractures
are divided into talar dome fractures (81-C1), talar body fractures
with subtalar joint involvement (81-C2), and talar body fractures with
subtalar and ankle joint involvement (81-C3). Subclassification is made
depending upon whether the fracture is comminuted.148
The location of the primary fracture line is important, particularly
when considering the surgical approach or a malleolar osteotomy for
exposure of the talar body.
with other life- and limb-threatening injuries, initial attention
should be directed to assessment and resuscitation according to the
ATLS guidelines. Obvious dislocations can be reduced and open wounds
treated appropriately. Once stabilization has occurred, the appropriate
diagnostic investigations can be performed, usually including
radiographs of the foot and ankle as well as CT scanning.
reported on a series of 31 patients with fractures of the talar body.
Most patients were treated with closed reduction and casting, and
complications were common with high rates of malunion, osteonecrosis,
and arthritis. Ninety-five percent of their patients had moderate or
severe complaints. They concluded that more aggressive treatment is
indicated for displaced fractures and recommended “exact reduction and
stable fixation whenever possible.”184
In some cases, percutaneous techniques or arthroscopic techniques may
be employed, with the potential benefit of preserving the blood supply.132,170
However, the goals of treatment should be respected, including anatomic
restoration of alignment and achieving congruity of both the tibiotalar
and subtalar joints.
talar body fractures is preferred. In open fractures or irreducible
dislocations, treatment by necessity should be performed emergently.
However, in many talar body fractures, definitive treatment can be
delayed to facilitate improvement in the patient’s overall condition
and to permit resolution of severe soft tissue swelling.
and combined approaches. Débridement of the subtalar joint and fragment
fixation can also be accomplished using a lateral approach. The
anteromedial approach is commonly used. It is generally wise to site
the incision more posteriorly than usual, particularly if a medial
malleolar osteotomy is contemplated, to facilitate the osteotomy. In
addition, one should avoid disrupting
the
blood supply to the talus in the region of the tarsal canal by limiting
plantar dissection. Finally, it is often not necessary to dissect into
the talar head region, and the talonavicular joint capsule can often be
preserved in its entirety.
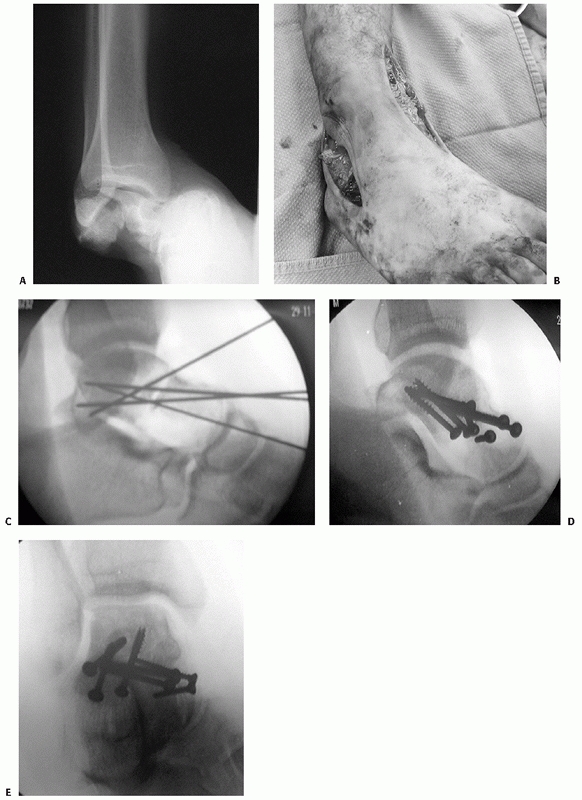 |
|
FIGURE 58-20 Talar body fracture with associated subtalar dislocation and comminution. A. Preoperative anteroposterior radiograph demonstrates dislocation and fracture comminution. B.
Combined lateral and anteromedial surgical approaches were used. Intraoperatively, Kirschner wires achieved provisional fixation (C) followed by definitive screw fixation (D,E). |
anteromedial exposure. Again, a fibular osteotomy is occasionally
necessary, and the incision may need to be redirected accordingly. The
use of combined anterolateral and anteromedial approaches is often
required, especially in comminuted fractures and those fractures with
displacement of the coronal fracture line. Isolated, noncomminuted
sagittal plane fractures can often be treated with a single incision
either medial or lateral, depending upon the location of the primary
fracture line.204
utilized a medial malleolar osteotomy in 16 patients and a fibular
osteotomy in the treatment of 3 of 57 fractures of the talar body. An
osteotomy is particularly required for fractures of the posterior
aspect of the talar body. Anterior fractures can frequently be
visualized well without an osteotomy. When a malleolar osteotomy is
required, predrilling and tapping prior to creating the osteotomy
facilitates later reduction and fixation of the osteotomy, once the
talar body has been reduced and stabilized.216
Care should be taken to ensure that the osteotomy is of sufficient size
to facilitate visualization and implant placement. Furthermore, when a
medial malleolar osteotomy is performed, reflecting the malleolus
inferiorly may allow preservation of the blood supply to the talar body
via the deltoid ligament branches.
for fragments of bone and cartilage large enough to stabilize.
Depending upon the size of the fragment, cortical screws ranging from
2.0 to 4.0 mm in diameter can be used (Fig. 58-21).
The availability of screws of sufficient length is also valuable, as
displaced fragments can range in size up to the width of the talar
body, usually approximately 35 to 40 mm across. Care should be taken to
avoid prominent hardware, and for that reason, countersinking of screws
or the use of headless screws is advantageous. Compression screw
fixation may be used in noncomminuted fractures. Alternative fixation
devices include Herbert screws,119
Kirschner wires, and threaded wires, all of which may be useful
depending upon the size of the fragments to be stabilized. Small plates
can also be used to span comminuted segments medially or laterally; in
some cases a portion of the plate can be countersunk to lessen the risk
of hardware impingement.
especially those which do not contribute to ankle or subtalar joint
stability. Although no criteria exist for which fragments to stabilize
or excise, the removal of small osteochondral fragments which do not
contribute to joint stability seems to be well tolerated.
appropriate treatment for fractures of the talar body with associated
dislocations. Limited case reports are available in the literature,
describing various techniques of arthrodesis. The length and alignment
of the ankle and hindfoot should be retained (Fig. 58-22).
The technique of primary arthrodesis offers the potential advantage of
earlier return to function compared to unsuccessful attempts at open
reduction and internal fixation.28,30,155,163
However, most talar body fractures can be successfully treated with
retention of intact ankle and subtalar joints, such that primary
arthrodesis is only rarely required. Experimental studies also exist
with talar body replacement in the setting of severe crush fractures of
the talus.71
following talar body fractures requires a prolonged period of
non-weight bearing. When stable fixation has been achieved, early
motion may help to prevent joint stiffness. Weight bearing is usually
restricted until union has occurred, often 3 months after the initial
injury and surgery.
development of complications, including osteonecrosis, malunion, and
arthritis.30,92,123,130
Although it is thought that improvements in surgical techniques and
fixation implants may decrease the incidence of complications, recent
reports continue to demonstrate very high rates of osteonecrosis and
arthritis. In one study, 88% of the patients had radiographic evidence
of osteonecrosis and/or posttraumatic arthritis at a follow-up period
of 33 months.203 Other complications include flexor tendon entrapment in scar tissue,144 superficial and deep wound infections, and skin necrosis. Lindvall et al.114 reported that in their series, complication rates and outcomes were equivalent between talar neck and talar body fractures.
Treatment is similar to that noted above, following fractures of the
talar neck. The combined fractures of the talar neck and body may be
more predisposed to osteonecrosis.203
Talar body fractures with associated fractures of the malleoli may have
a lower risk of osteonecrosis, as the combination of talar body
fracture and malleolar fracture is thought to preserve the soft tissue
attachments to the body fragments.136
Radiographic findings suggesting tibiotalar arthritis were noted in 65%
of patients, and subtalar joint changes were noted in 35% of patients
at the time of follow-up in the study of Vallier et al.203
All of the patients with open fractures developed arthritis. These
authors also noted that functional outcomes were worse in patients with
radiographic signs of osteoarthritis compared to patients without
arthritis in their series.
are common sequelae of talar body fractures. Functional outcome scores
demonstrate significant disability and are substantially higher
compared to patients with other hindfoot injuries.51,203
require emergent reduction and stabilization. As with talar neck
fractures, early reduction of dislocations may offer some advantages.
However, due to the relative rarity of these injuries, many surgeons
may be uncomfortable treating difficult talar body fractures, and
therefore, referral to a center with the appropriate expertise should
be performed. When transfer is selected, an attempt should be made to
achieve a closed reduction prior to transfer to minimize skin necrosis
and potentially improve vascular supply. Preoperative imaging including
a CT scan is essential, although in many cases the marked displacement
of the fragments makes interpretation difficult.
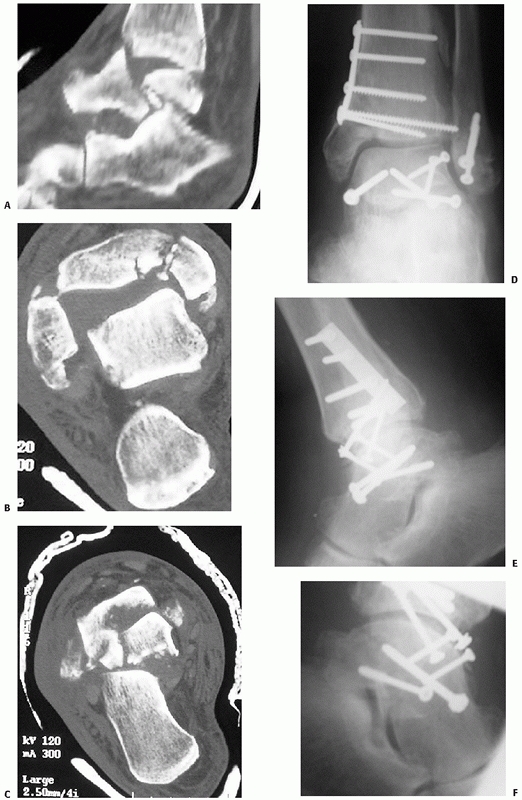 |
|
FIGURE 58-21
A talar body and associated tibial plafond fracture treated with open reduction and internal fixation in a 82-year-old farmer. Coronal and reconstructed CT views demonstrate the talar body fracture with subtalar subluxation (A), plafond impaction and malleolar fracture (B), and talar body comminution (C). Three-month postoperative images demonstrate restoration of alignment (D-F) with multiple screw fixation. There is evidence of sclerosis of the talar body. |
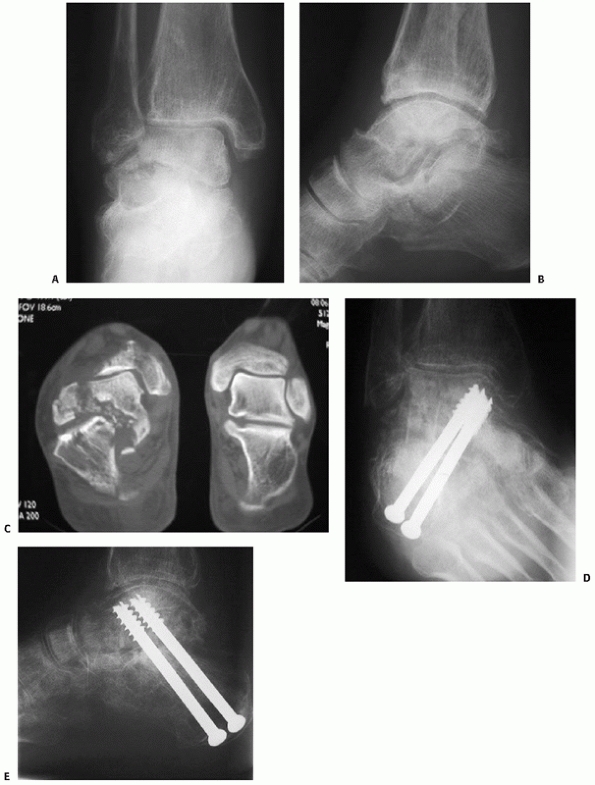 |
|
FIGURE 58-22
Treatment of a talar body fracture with primary subtalar arthrodesis in a 72-year-old woman with osteoporosis. Anteroposterior and lateral radiographs at the time of the injury demonstrate subtalar subluxation (A,B) but the fracture, with associated comminution, is better demonstrated on CT scan (C). Treatment in this case included a primary subtalar arthrodesis with intercalary bone graft (D,E). |
may be difficult. Because many fractures involve the anterior talar
body or are associated with malleolar fractures, a formal malleolar
osteotomy is often not required. In general, I perform an osteotomy for
fractures with involvement of the posterior half of the talar body. I
prefer a medial malleolar osteotomy, reserving a fibular osteotomy for
fractures with lateral side comminution. It is helpful to predrill the
screw fixation holes for the osteotomy prior to making the cut. I
prefer an oblique osteotomy, angled approximately 30 degrees inferior,
intersecting with the articular margin 1 to 2 mm lateral to the medial
edge of the articular surface of the plafond. An osteotome is used to
complete the cut through the articular surface. This technique seems to
facilitate good interdigitation of the fragments at the articular
surface; position screws are then used for fixation to avoid
overcompression at the nonarticular margin. Thordarson et al.198 and Alexander et al.3 describe a step-cut medial malleolar osteotomy for exposure of the talar body which has resulted in uncomplicated healing.
talar body fractures is dictated by the nature and personality of the
fracture. For anterior fractures, I prefer a medial or anteromedial
approach with an additional direct lateral approach to visualize the
subtalar joint. For posterior fractures, the incision is necessarily
more posterior to facilitate medial malleolar osteotomy. Reduction
requires a variety of direct and indirect techniques, including
calcaneal traction, placement of a distractor, and direct fragment
manipulation. In most cases, even relatively small fragments can be
stabilized with the appropriate size of screw. I prefer to insert
hardware from the medial side, where an area devoid of cartilage exists
at the superior margin of the deltoid ligament insertion on the talus.
When this is impossible or additional fracture fragments require
fixation, countersinking of the screw head or the use of headless
screws is required.
initial radiographs; efforts at reduction and fixation are often
extremely satisfying. In one study, an anatomic reduction was achieved
for 81% of talar body fractures.203
Range of motion exercises are instituted once the wounds have healed
and weight bearing is delayed for 3 months or until union has occurred.
understanding the tricks inherent in surgical treatment can be helpful.
The first pearl is to not rush into surgery without adequate
preparation. CT scanning can give valuable information regarding the
appropriate surgical approach and whether a malleolar osteotomy is
required. It is reasonable to delay surgery until soft tissue swelling
has settled, provided the tibiotalar joint is not dislocated.
osteonecrosis.” Avoid stripping the medial and plantar aspects of the
talus, where the primary blood supply enters, and avoid stripping any
more of the dorsal neck than is necessary. Consider a malleolar
osteotomy as a better option compared to any violation of the deltoid
ligament. In general, the osteotomy is only required when the fracture
line extends posterior to the midpoint of the talus. Visualization and
fixation in more anterior fractures can usually be achieved with
plantar flexion of the ankle.
appropriate sized screws is essential. I generally use 2.0-, 2.4-,
2.7-, and occasionally 3.5-mm cortical screws. The screw length varies,
but lengths upwards of 4.0 mm may be required. Placing the implants on
the medial side is somewhat easier and less likely to be irritating to
the patient. There is a bare area at the superior margin of the deltoid
ligament insertion on the talus, which is well suited to accept three
or four small screws. Otherwise, countersinking of the hardware is a
necessity. Intraoperative fluoroscopy is similarly an important
necessity, and the surgeon should be familiar with obtaining a Canale
view to assist with the determination of alignment.
techniques, complications occur and are best dealt with promptly.
Hardware removal is a common necessity, as is treatment of arthritis
and occasionally malunion or nonunion. Counselling the patient that
their injury is demanding and problematic at the time of initial
consultation saves countless hours and headaches in follow-up.
injury with a lower incidence than talar neck or body fractures. These
fractures may be seen in conjunction with neck and body fractures, as
well as fractures elsewhere in the foot. In most cases, the fracture
line involves the articular surface of the talar head such that the
talonavicular joint is involved. The injury is often associated with
talonavicular subluxation and may be complicated by talonavicular
arthritis.
to the talar head through the navicular bone. The fracture is often
described as a compression fracture and may result in significant
impaction to the articular surfaces of the navicular and the talar
head. Coltart30 described six cases
of which four occurred as a result of flying accidents, presumably due
to a “rudder bar” injury. He theorized the force of impact was
transmitted along the longitudinal axis of the foot through the
metatarsals and navicular, with the foot held in extreme
plantarflexion, such that a compression force was applied to the talar
head.30 The navicular may also fracture as a result of the compressive force.15
Fractures of the talar head are associated with varying degrees of
comminution. In some cases, the fractures are associated with midfoot
injuries, particularly divergent tarsometatarsal joint injuries.
extremely subtle, commonly missed injuries to a markedly swollen
midfoot with apparent major injury. Tenderness to palpation is usually
noted at the talonavicular joint region. Careful examination is useful
to demonstrate the findings of an associated midfoot injury.
foot demonstrate the fracture. Often, the displaced fractures are
associated with varying degrees of talonavicular joint subluxation.
Fractures of the talar head can be associated with other hindfoot
injuries, including talar neck and body fractures and peritalar dislocation.154
Careful inspection of the radiographs may demonstrate shortening of the
medial column of the foot due to the displaced fracture. Usually, the
displaced fracture fragment involves the dorsomedial aspect of the
talar head, with subluxation of the talonavicular joint occurring in a
similar dorsomedial direction.
alignment of the dorsomedial arch of the foot, prevention of
talonavicular joint incongruity and instability, and reduction of the
displaced talar head fragment. Occasionally, a talar head fracture may
present without displacement. In these cases, a well molded short leg
cast may be used. In most cases, weight bearing can be instituted at
approximately the 6-week mark, provided a well-fitting shoe with
appropriate arch support is used.
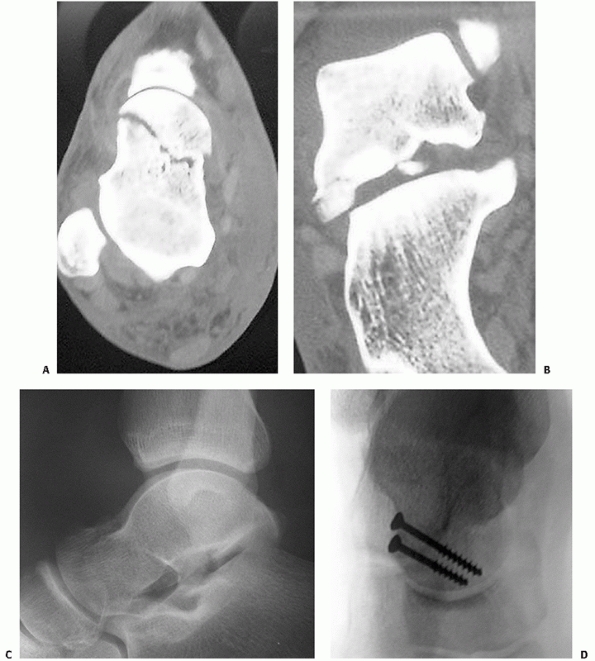 |
|
FIGURE 58-23
Talar head fracture treated with primary open reduction and internal fixation. Axial and coronal CT images demonstrate the fracture (A) and associated subtalar subluxation (B) better than plain radiographs (C). Open reduction and internal fixation was performed with compression screws (D). |
Small comminuted segments can be excised, but larger fragments can
usually be reduced and stabilized with small or mini fragment screws or
Kirschner wires. I use a dorsomedial approach, taking care to protect
the tibialis anterior tendon, and makes an effort to preserve portions
of the intact
talonavicular
capsular and ligamentous supports. Displaced fragments are reduced and
stabilized, usually with screws ranging from 2.0 to 3.5 mm in diameter.
Bone grafting is rarely necessary. Following surgery, patients are
placed in a short leg non-weight-bearing splint until wound healing
occurs. Early motion may be instituted depending upon the stability of
the fixation and the talonavicular joint. If the talonavicular joint is
stable, I prefer to begin mobilization in a removeable splint after 2
weeks. If, however, the talonavicular joint remains unstable following
fixation of the talar head fracture, I prefer to immobilize the joint
in a short leg cast for approximately 6 weeks.
Nonunion of talar head fractures is relatively uncommon. The treatment
options for symptomatic talonavicular arthritis include the use of
longitudinal arch supports with increased arch rigidity or a long steel
shank in the shoe. If conservative measures fail, arthrodesis of the
talonavicular joint may relieve symptoms. Because isolated
talonavicular arthrodesis substantially alters hindfoot and midfoot
mechanics, triple arthrodesis may also be considered.42
fragments which remain displaced may result in residual talonavicular
joint subluxation. Verhaar207
reported on a case of late talonavicular subluxation secondary to
malunion. Anatomic restoration of alignment of the talar head fragment
eliminated the subluxation.207
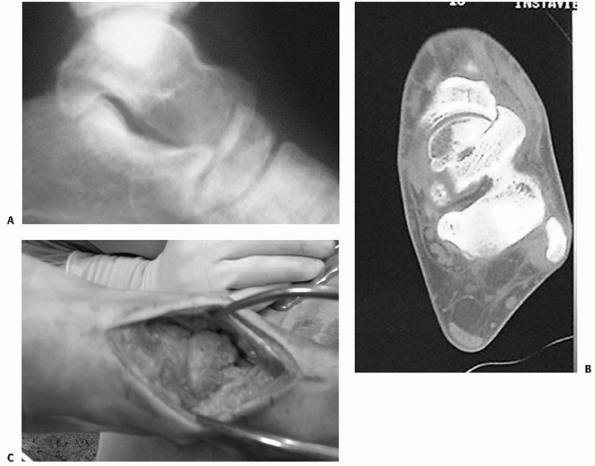 |
|
FIGURE 58-24 Missed talar head fracture with talonavicular subluxation. Lateral radiograph demonstrates the talonavicular subluxation (A) confirmed by CT scan (B) and intraoperative visualization. Following osteotomy and reduction (C), the talonavicular joint is congruent.
|
relatively common but frequently overlooked. The orthopaedic literature
includes little information regarding fractures of the talar processes
in general. The injury was described by Dimon39
in 1961. Recently, the association between snowboarding and lateral
process fractures has been recognized, leading to the term
“snowboarder’s fracture.” Most surgeons recognize that nonunion of
displaced lateral process fractures is relatively common. Similarly,
large lateral process fractures with extension into the subtalar joint
may lead to subtalar pain, arthritis, and loss of motion. The
literature related to lateral process fractures emphasizes two key
points: that the injuries are commonly misdiagnosed and that early
treatment improves functional results.
broad-based, wedges-haped prominence of the talar body. The lateral
process includes two articular surfaces. Dorsolaterally, it articulates
with the fibula; inferomedially, the lateral process articulates with
the
anterior portion of the posterior facet of the calcaneus. The lateral
talocalcaneal ligament originates from the tip of the lateral process
(see Fig.58-8).129
received increasing attention in recent years because of the
association between this fracture and snowboarding.145 Kirkpatrick et al.102
reviewed over 3000 snowboarding injuries from 12 Colorado ski resorts
and noted 74 lateral process fractures. It has been suggested that the
fracture results from a combination of ankle inversion and
dorsiflexion. However, in a cadaver study, Funk et al.55
noted that eversion of a dorsiflexed and axially loaded ankle was more
likely to result in a lateral process fracture. Similarly, Boon et al.14
combined external rotation with dorsiflexion, inversion, and axial
loading and reproduced lateral process fractures in 75% of the
specimens. It is likely that both avulsive and axial loading mechanisms
may occur and result in different types of lateral process fracture. A
patient with bilateral lateral process fractures was described, in whom
the mechanism of injury was predominantly axial loading. The fractures
occurred when the patient landed a jump on his dirtbike with both feet
planted on the foot-pegs.8 Stress fractures of the lateral process may also occur particularly in running athletes.11,138
fractures of the lateral process into three groups: a nonarticular chip
fracture, a single large fragment involving the talofibular and
subtalar articulations, and a comminuted fracture involving both
articulations. In some cases, the fracture may be associated with
subtalar joint incongruity or have marked displacement.
physical findings of a lateral process fracture may mimic those of an
inversion ankle sprain. Swelling and ecchymosis are commonly localized
to the lateral aspect of the ankle. Point tenderness is localized to
the lateral process, and most patients retain the ability to bear
weight. As a result, the injuries may be commonly overlooked or
misinterpreted.199 Mukherjee et al.139
reviewed 1500 sprains and fractures of the ankle region and found 13
cases of lateral process fracture. The diagnosis of lateral process
fracture should be considered in patients with acute findings similar
to an ankle sprain, patients previously diagnosed with an ankle sprain
who do not appear to be recovering in the usual time course, and those
who present with chronic lateral ankle pain.
radiographs are often insufficient to detect and fully diagnose a
lateral process fracture. On the lateral view, overlap of the malleoli
and the sustentaculum tali may make detection of the injury difficult.
The fracture can best be seen on careful inspection of the mortise view
because the fracture line is most commonly in the sagittal plane.
Because of the difficulty in detecting and defining the extent of a
lateral process fracture, a CT scan is frequently necessary to fully
understand the injury. CT will allow an accurate assessment of the
size, degree of displacement, and comminution of the fractured process
as well as joint involvement, tendon pathology, and any associated
injuries.46,146 MRI will similarly detect and define fractures of the lateral process and associated injuries.172
size of the fracture fragment, displacement of the fragment, degree of
comminution, associated injuries, and joint congruity. In general,
small fracture fragments and undisplaced fractures are appropriately
treated without surgery, with a period of immobilization followed by
progressive weight bearing and motion exercises. In contrast, large
fractures associated with significant displacement and involving
substantial portions of the subtalar joint are treated with open
reduction and internal fixation.76,129
Weight bearing is usually avoided for a period of approximately 4 to 6
weeks. Following mobilization, physical therapy is often required to
assist with rehabilitation of both the ankle and subtalar joints.
Preoperative CT is helpful in determining if fragments are large enough
to consider fixation. Although the lateral process can be a large
fragment, the amount of comminution and the small size of fragments are
often worse than is apparent on plain radiographs. For comminuted
fractures, primary excision of fragments is indicated to avoid the
later development of arthritic changes in the subtalar joint.76 Langer et al.108
studied the effect of excision of a 1-cm fragment of the lateral
process on ankle and subtalar stability. Although slight increases in
anterior translation, talar tilt, and subtalar motion were noted, the
increases were well below the traditional radiographic thresholds used
to define instability. The authors concluded that excision of a 1-cm3 fragment should not cause ankle or subtalar instability.108
Open reduction or fragment excision may be performed through a direct
lateral approach using an incision over the sinus tarsi. When open
reduction is performed, screw fixation can often be accomplished with
the screw inserted from the tip of the process and extending
posteriorly and superiorly into the talar body. Screws ranging from 2.0
to 2.7 mm in diameter are typically sufficient for fixation of lateral
process fractures.
Pain in the region of the subtalar joint seems to be common following
fractures of the lateral process, in particular when the diagnosis is
delayed. Nonunion of unreduced fractures and residual malalignment of
the subtalar joint cause persistent symptoms.39,72,139
Several authors have noted that earlier treatment may be associated
with better results. In one review of the literature, it was noted that
earlier treatment resulted in a low rate of nonunion and generally good
outcome.199 Heckman et al.,76
in a review of nine patients, found the best results when patients were
diagnosed and treated early compared to a high proportion of patients
with pain when treatment was delayed. Therefore, whether casting,
fragment excision, or open reduction and internal fixation is
necessary, it seems that the proposed treatment is best performed early.
noted generally favorable outcomes in 23 snowboarders with lateral
process fractures. Sixty-five percent of the patients regained their
preinjury activity level, and outcome scores were excellent in
virtually all patients. Those with nondisplaced fractures fared
slightly better compared to patients with displaced fractures.208 Similar results were reported by Valderrabano et al.201
in whom 16 of 20 snowboarders with lateral process fractures returned
to full sports activities. In both of these series, degenerative
changes were noted in the subtalar joint in several patients
approximately 3 years after the injury.
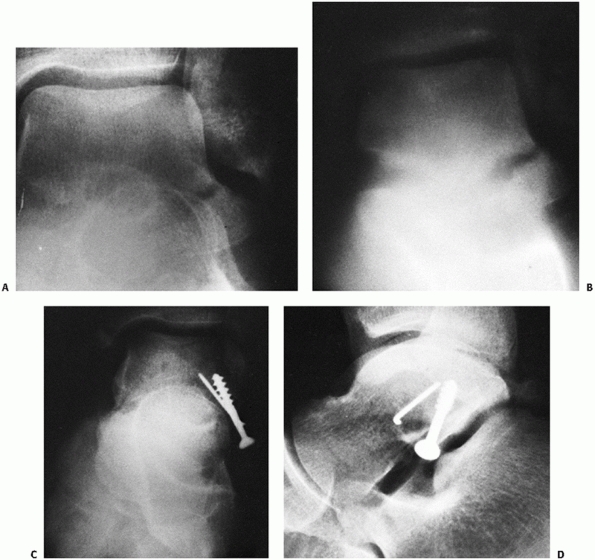 |
|
FIGURE 58-25 A lateral process fracture demonstrated on an anteroposterior radiograph of the ankle (A) and confirmed by CT (B). Open reduction and internal fixation was performed with a cancellous screw and Kirschner wire (C,D).
|
more frequently than is commonly recognized. Treatment of nonunions is
usually restricted to excision of ununited fragments. Attempts at
obtaining union of established nonunions are unlikely to succeed.
Nonunions associated with subtalar joint subluxation frequently develop
subtalar arthritis, often requiring arthrodesis.152
interesting injuries. The anatomy is deceptively complex. Together, the
medial and lateral tubercles comprise the posterior talar process (Fig. 58-26).
The lateral tubercle is larger, projects more posteriorly, and is the
tubercle usually seen on a lateral radiograph of the ankle. The
posterior talofibular ligament is attached to the lateral tubercle.
Between the lateral and medial tubercles is a groove for the flexor
hallucis longus tendon. The medial tubercle projects medially and
inferiorly from the groove for the flexor hallucis longus. The
posterior third of the deltoid ligament is attached to the medial
tubercle.
by articular cartilage, and the posterior 25% of the posterior
articular facet of the subtalar joint is formed by the posterior
process.
McDougall121
described the development of the posterior process of the talus. It is
thought that the posterior process arises from a secondary ossification
center that fuses with the body of the talus around age 12.121
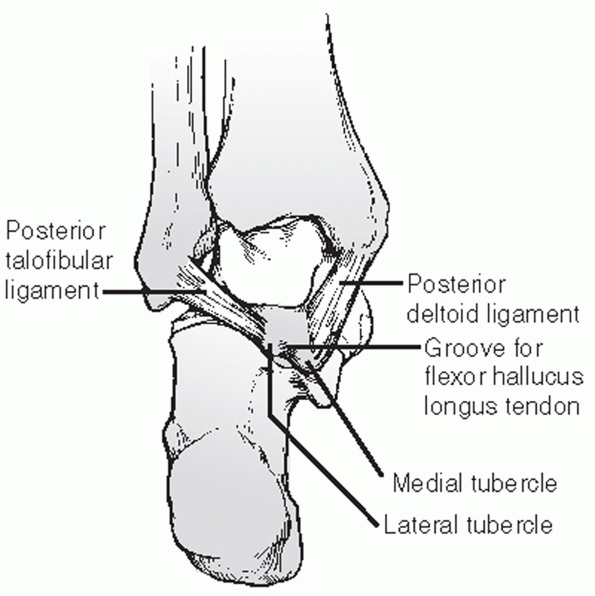 |
|
FIGURE 58-26
Posterior view of the talus demonstrating that the posterior process has two tubercles, separated by the groove for the flexor hallucis longus tendon. The posterior fibers of the deltoid insert into the medial tubercle, and the posterior talofibular ligament inserts into the lateral tubercle. |
the talus can be difficult, in part relating to the presence of an os
trigonum. The os trigonum is an accessory bone of the foot located just
posterior to the lateral tubercle of the posterior process. Burman and
Lapidus18 found a separate os
trigonum in 64 of 1000 feet examined by radiograph, and noted a fused
os trigonum in 429 of 1000 feet. These authors defined the fused os
trigonum as an elongated lateral tubercle. While Burman and Lapidus18 described a significant degree of symmetry in the anatomy of the posterior talus between the two feet of any person, McDougall121
described the os trigonum as a possible unilateral occurrence. The os
trigonum is usually distinguished from a fracture of the lateral
tubercle based upon its radiographic appearance. The shape of the os
trigonum varies, including round, oval, and triangular shapes. The
edges are well corticated and smooth, unlike an acute fracture. A high
index of suspicion is necessary to rule out an acute fracture.
Giuffrida et al.59 describe a series
of six patients with posteromedial talar facet fractures, in whom four
were misdiagnosed as having an os trigonum. Kim et al.100
described three of five patients in whom fractures of the medial
tubercle of the posterior process were misdiagnosed as an os trigonum
or an ankle sprain. In both series, patients with delayed diagnoses
presented with chronic posteromedial ankle pain.
process of the talus was described in 1844 by Cloquet. In 1882,
Shepherd described the fracture in the English literature.178 The fracture is often referred to as the Shepherd fracture.109
process may occur as a result of avulsion mechanisms or as a direct
compression injury. Inversion of the ankle may avulse the tubercle via
the posterior talofibular ligament.104
Direct compression injuries occur when the lateral tubercle is
compressed between the calcaneus and the posterior lip of the tibia
with the ankle in extreme equinus.69,79,104,121,127,164
Repetitive trauma may lead to fracture in kicking athletes, such as
football or rugby players, in whom pain may develop related to the
forced equinus position of the foot upon impact.121,209
A stress fracture may result in a similar presentation. Alternatively,
pain may result from a failure of fusion of the secondary ossification
center of the posterior process with the body of the talus, especially
in adolescents exposed to repetitive stress to the hindfoot.209
frequently present with symptoms comparable to an ankle sprain.
Tenderness can be elicited over the posterolateral ankle and motion of
the ankle and subtalar joints is painful. Active flexion of the great
toe may produce pain, as the flexor hallucis longus tendon moves over
the fracture site. The fracture can be difficult to see on plain
radiographs but is best demonstrated on the lateral radiograph (Fig. 58-27).
Comparison views of the contralateral foot are useful to identify and
contrast the appearance of an os trigonum. Any rough or irregular
surfaces visible should be interpreted as potentially indicative of a
fracture of the lateral tubercle of the posterior process, in contrast
to the smooth and well-corticated surfaces of the os trigonum. The
variability of the anatomy of the posterior process should be
considered. CT scanning may be useful when the diagnosis is not
apparent on plain radiographs.
posterior process of the talus should be directed toward achieving
union. Multiple reports in the literature describe ununited and
symptomatic fractures requiring surgical intervention. Patients should
be prevented from inversion and plantarflexion of the ankle to avoid
displacement. Protection from full weight bearing and the use of a
short leg cast or ankle brace is continued for 4 to 6 weeks or until
some radiographic signs of union are present.
 |
|
FIGURE 58-27 Lateral radiograph of the ankle showing a fresh fracture of the lateral tubercle of the posterior process of the talus.
|
excision of the fragment. Patients complain of pain with
plantarflexion, pain with physical activity, and often there is
restriction of ankle and subtalar joint motion. Making the diagnosis
can be difficult: if the fragment has developed a rounded appearance on
radiographs, distinguishing an ununited fragment from an os trigonum
can be challenging. In addition to the fragment, radiographs may show
degenerative changes adjacent to the fragment and in the subtalar
joint. Bone scan may demonstrate increased uptake in the area of the
fragment; however, an MRI scan will demonstrate the nonunion as well as
edema around the fragment suggestive of inflammation.
flexor hallucis longus tendon may develop. Partial rupture or
tenosynovitis of the tendon may occur without fracture, and is usually
noted in athletes such as soccer players or ballet dancers. Inokuchi et
al.84 reported a case of complete
rupture of the flexor hallucis longus tendon following a nonunion of a
Shepherd fracture, requiring tendon grafting to restore tendon function.
accomplished by excision of the fragment. Excision may be accomplished
via a posterolateral206 or posteromedial approach,214 and usually achieves relief of pain and improved motion.100,121,209
and is sometimes referred to as Cedell’s fracture. Although limited
case series exist regarding this injury, the literature notes problems
with this fracture related to delayed diagnosis and the subsequent
development of ankle pain.
fracture of the medial tubercle occurs via an avulsion injury of the
posteromedial talar facet. The foot is suddenly forced into combined
pronation and dorsiflexion, and the posterior deltoid ligament avulses
the medial tubercle of the posterior process.21,90,100,101,185 Alternate mechanisms include direct trauma to the posteromedial talar facet,212 impingement of the sustentaculum tali in supination,29 and forced dorsiflexion in high-energy trauma.40
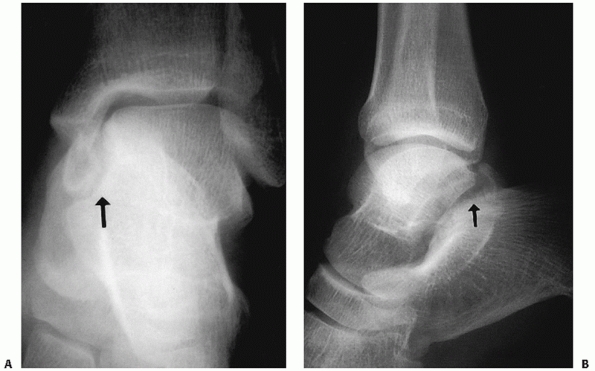 |
|
FIGURE 58-28 Anteroposterior (A) and lateral (B) radiographs of an acute fracture of the medial tubercle of the posterior process of the talus. The arrows identify the fracture line.
|
visualize on plain radiographs. Accordingly, injuries are often missed
and patients frequently present late. Common presenting symptoms are
posteromedial ankle pain and tenderness. Dougall and Ashcroft40
described an interesting patient with entrapment of the flexor hallucis
longus tendon in the fracture. In this instance, the patient presented
with an inability to extend the great toe as well as posteromedial
ankle symptoms.40 On occasion, the
fragment can be seen on the lateral projection of plain radiographs or
may be visualized as a small flake fragment off the medial wall of the
talus in the anteroposterior projection (Fig. 58-28).
However, plain radiographs often do not demonstrate the fracture well.
CT is perhaps most helpful at documenting the extent and severity of
these fractures (Fig. 58-29).
treated two patients with these fractures with open reduction and
internal fixation. In both cases, the fragment was found to be much
larger than initially suspected.90 Other authors have successfully treated the fracture with simple orthotic insoles.205 Cedell21 surgically excised three persistently symptomatic ununited fragments. Stefko et al.185 excised a malunited fragment to relieve a secondary tarsal tunnel syndrome. Kim et al.100
reported on two patients diagnosed early who were successfully managed
with cast immobilization, and three patients who presented late who
were successfully managed with fragment excision. In general, excision
of ununited or malunited fragments seems to relieve local irritative
symptoms in patients who present with posteromedial ankle pain secondary to a posterior medial tubercle avulsion.
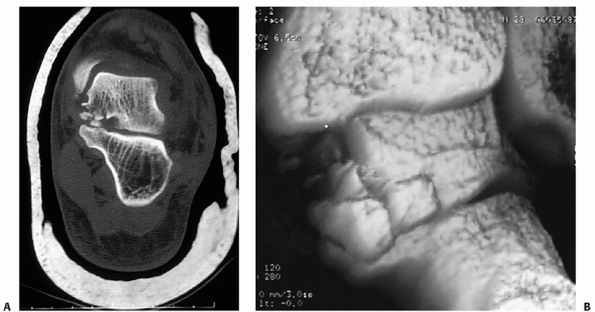 |
|
FIGURE 58-29 Coronal CT scan (A) and CT reconstruction (B) demonstrating the medial process fracture depicted in radiographs in Fig. 58-28.
|
an uncommon injury. Foster described a case in a 20-year-old woman who
sustained a displaced fracture of the posterior process as a result of
an inversion injury (Fig. 58-30). The process
was displaced and was compressing the posterior tibial neurovascular
bundle. Open reduction and internal fixation was performed. Nasser and
Manoli142 also described a case that required open reduction and internal fixation to restore congruity of the ankle and subtalar joints.
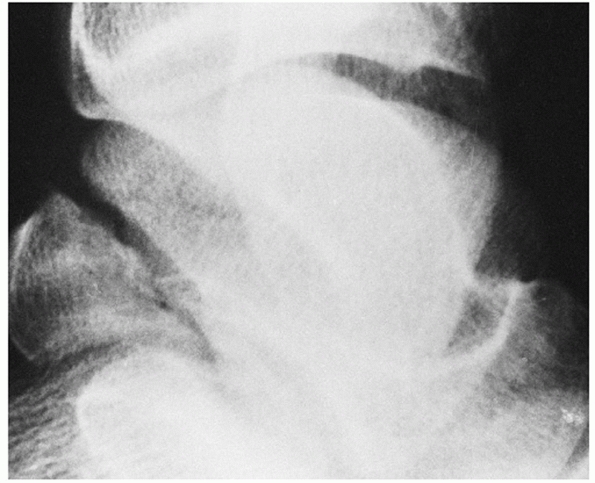 |
|
FIGURE 58-30
Oblique view of the ankle mortise demonstrating fracture of the entire posterior process of the talus. (Courtesy of Robert R. Foster, MD.) |
conjunction with major talus fractures, as described above. However,
dislocations can also occur with no associated bony injury or with
relatively minimal appearing fractures. These injuries can be
considered in two broad categories: subtalar dislocation and total
talar dislocation.
refers to the simultaneous dislocation of the distal articulations of
the talus at the talocalcaneal and talonavicular joints. Although first
described by Judcy89 and Dufaurets41 in 1811, the dislocations are uncommon, and the clinical literature related to subtalar dislocation is limited. Smith182 noted only seven dislocations in a review of 535 dislocations of all types. Leitner112 noted only 42 among 4215 dislocations. Fifteen percent of all talar injuries in Pennal’s155 series were subtalar dislocations. Most commonly, the injuries occur in young adult males, although Bibbo et al.9 noted 36% of subtalar dislocations in their series of 25 patients occurred in patients over 40 years of age.
Significant deformity is always present. Medial dislocations are
thought to be more common, comprising up to 85% of subtalar
dislocations (Fig. 58-31).36,62,77,134,162
The calcaneus, with the rest of the foot, is displaced medially while
the talar head is prominent in the dorsolateral aspect of the foot. The
navicular is medial and sometimes dorsal to the talar head and neck.
Lateral dislocation occurs less often. In a lateral dislocation, the
calcaneus is displaced lateral to the talus and the talar head is
prominent medially (Fig. 58-32). The navicular
lies lateral to the talar neck. Rarely, a subtalar dislocation is
reported to occur in an anterior or posterior direction, but these are
usually associated with medial
or lateral displacement as well.87,105,162
The direction of subtalar dislocation has important effects with
respect to management and outcome. The method of reduction is different
for each type of injury. In addition, lateral dislocations are
associated with higher-energy mechanisms and a worse long-term
prognosis compared to medial subtalar dislocations.
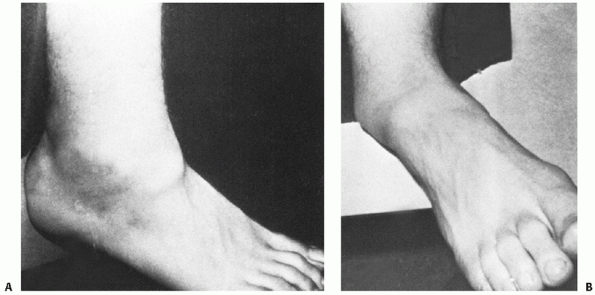 |
|
FIGURE 58-31 In this medial subtalar dislocation, the head of the talus (A) is palpable on the dorsum of the foot. The heel (B) is displaced medially. (Buckingham WW Jr. Subtalar dislocation of the foot. J Trauma 1973; 13:754.)
|
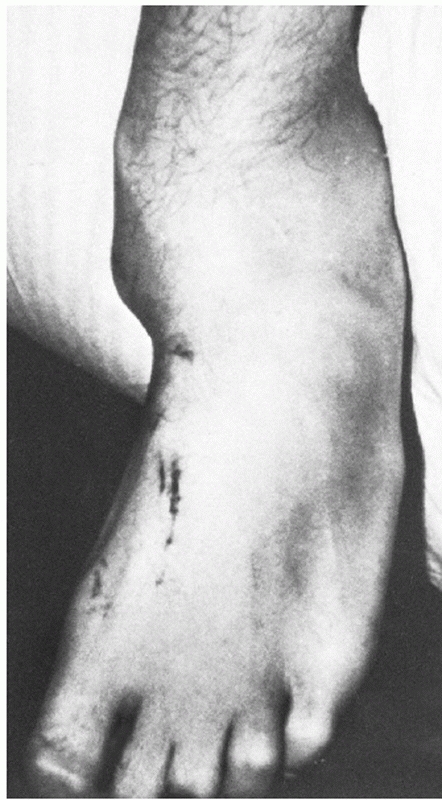 |
|
FIGURE 58-32
In this lateral subtalar dislocation, the head of the talus is prominent medially while the rest of the foot is dislocated laterally. (Buckingham WW Jr. Subtalar dislocation of the foot. J Trauma 1973;13: 757.) |
dislocation, while eversion produces a lateral subtalar dislocation.
The calcaneonavicular ligament resists disruption,17
while the inversion or eversion force is dissipated through the weaker
talonavicular and talocalcaneal ligaments such that the calcaneus,
navicular, and all distal bones of the foot are displaced as a unit
either medially or laterally. With a medial subtalar dislocation, the
sustentaculum tali acts as a fulcrum about which the foot rotates to
lever apart the talus and calcaneus; in the lateral dislocation, the
foot pivots about the anterior process of the calcaneus, again causing
the talus and calcaneus to separate.186
or low-energy mechanisms. The distinction is important because outcome
has been correlated with the severity of the initial injury. In the
series of Bibbo et al.,9 high-energy
mechanisms such as motor vehicle trauma and falls from height accounted
for 68% of subtalar dislocations. Other common mechanisms include
sports injuries, usually related to a fall from a jumping height.
Grantham62 coined the term
“basketball foot” to describe a medial subtalar dislocation because
four of the five patients in his series sustained the injury on the
hardwood. Usually, the dislocation occurs when landing from a rebound.
Open subtalar dislocations and lateral subtalar dislocations are more
common with a high-energy mechanism. Medial dislocations are more
common, suggesting that the forces required to produce it are less than
those required to produce a lateral dislocation.
other injuries, either regional or involving other body systems. One
series described associated foot and ankle injuries in 88% of patients
with subtalar dislocations.9 Regional fractures include talus, ankle, calcaneus, navicular, cuboid, cuneiform, and metatarsal fractures.26
Osteochondral shearing injuries to the articular surface of the talus,
the calcaneus, or the navicular are common. These injuries occurred in
45% of patients in one large
series, and were difficult to detect on plain radiographs.36
Injuries remote from the foot and ankle may occur as well. In a series
of subtalar dislocations from a major Level I trauma center, other
musculoskeletal injuries occurred in 48% of the patients, and 12% of
the patients had injuries to the head, abdomen, or chest.9
of deformity. The medial dislocation has been referred to as an
“acquired clubfoot” (Fig. 58-33), while the lateral has previously been described as an “acquired flatfoot” (Fig. 58-34).186
Additionally, many of the injuries are open, particularly when
associated with a high-energy mechanism. Up to 40% of subtalar
dislocations may present with an open wound.125
The head of the talus may protrude through the open wound in a lateral
dislocation. In closed dislocations, the skin is usually distorted and
markedly tented over the prominent head of the talus. Swelling occurs
rapidly and may mask the bone deformity. Evaluation for neurovascular
impairment should be performed prior to and following reduction of the
dislocation.
to interpret. The severity of the deformity makes it difficult to
obtain true anteroposterior and lateral images of the foot, and
standard ankle radiographs do not reveal the foot pathology.65
The relationship between the talus and tibia and fibula may be normal
or demonstrate positional talar tilt only because the point of injury
is distal to the ankle joint.
navicular is an important diagnostic key. On the lateral projection,
the head of the talus usually lies superior to the navicular and cuboid
for a medial dislocation and appears to be displaced inferior in a
lateral dislocation (see Figs. 58-33 and 58-34).
Usually, interpretation of the plain radiographs provides enough
information to determine the direction of the dislocation, such that
the physician can proceed with an attempt at reduction. However, plain
radiographs should be interpreted with caution. Associated fractures
can be missed on plain radiographs, and postreduction films may not be
adequate in all cases to determine whether residual subluxation is
present.
 |
|
FIGURE 58-33 Medial subtalar dislocation. The head of the talus is directed inferior to the navicular.
|
present and is sensitive enough to rule out talo-calcaneal subluxation.
Bohay and Manoli13 described four
cases of subtalar dislocation with associated fractures or residual
subluxation not documented on plain radiographs. Merchan125 reported associated fractures in 64% of his series of 39 cases, and Bibbo et al.9
reported associated injuries to the foot and ankle in 88% of patients.
In another study, in which a CT scan was performed in all cases, CT
identified additional injuries missed on initial plain radiographs in
all patients, and in 44% of the patients, new information gathered by
CT dictated a change in treatment.10
gentle and timely reduction. In most cases, reduction can be
accomplished closed. Often, the injury presents with skin tenting such
that a prompt reduction will reduce the possibility of skin necrosis.
Open peritalar dislocations require a formal irrigation and débridement
in addition to the reduction followed by wound closure.49
provision of adequate relaxation and sedation first. A forceful
manipulation may be necessary to accomplish the reduction, and patients
are often disturbed by the sight of their markedly deformed extremity,
such that general anesthesia may be required to achieve sufficient
relaxation. Second, the tension on the Achilles tendon should be
relaxed by flexing the knee. Next, longitudinal traction on the foot is
applied with countertraction on the leg.
“unlock” the calcaneus. Inversion is therefore applied for a medial
dislocation, and eversion for a lateral dislocation. Once the calcaneus
is unlocked, reversal of the deformity can be applied. Successful
reduction is usually accompanied by a satisfying clunk.
applied to aid in reduction. However, it should be applied with
caution. The calcaneus is ideally unlocked with inline traction and
accentuation of the deformity before digital pressure is applied.
Although digital pressure over the talar head can aid in the reduction,
it may also cause further skin necrosis and potentially displace an
osteochondral fracture.
confirmed by clinical examination and radiographs. On clinical exam,
the foot should demonstrate a restoration of normal alignment and range
of motion of the subtalar and midtarsal joints. Plain radiographs
confirm the reduction and should be closely inspected for associated
fractures that may have been missed on the radiographs of the distorted
foot. In many cases, a subtalar dislocation is stable following closed
reduction. This is particularly the case when there are no associated
osteochondral or other fractures. Clinical assessment of stability can
be performed following closed reduction. If the dislocation is
clinically stable, no internal fixation is necessary. A CT should be
performed following reduction to confirm that no displaced
intra-articular fragments are present, and to confirm that a congruent
joint reduction has been obtained. The foot can then be temporarily
immobilized in a short leg posterior splint. For stable reductions,
immobilization
until edema has settled and pain is controlled is adequate. Less than 2 weeks of immobilization may be necessary.
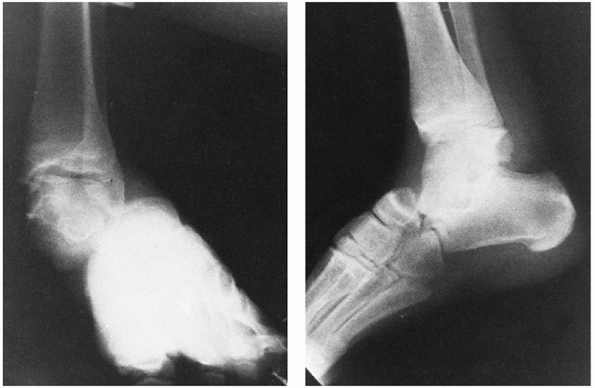 |
|
FIGURE 58-34 Radiographs of a lateral subtalar dislocation. (Buckingham WW Jr. Subtalar dislocation of the foot. J Trauma 1973;13:758.)
|
therapy is instituted to regain subtalar and midtarsal mobility. The
outcome following simple dislocations treated with closed reduction
seems to be favorable.36 In a series of 30 patients with closed isolated subtalar dislocations, de Palma et al.34
report that only three patients went on to require subtalar arthrodesis
after a minimum of five years of follow-up. Seventy percent of patients
scored either good or excellent on joint-specific functional outcome
measures.34 Recurrent dislocations are reported but are uncommon,86,110,215 and it is reasonable to proceed with early mobilization to avoid potential problems related to joint stiffness.
most series, the need for open reduction seems to be associated with
higher-energy subtalar dislocations. In some series, as few as 10% of
patients with medial dislocations and 15% to 20% of lateral subtalar
dislocations required open reduction.67,77,112,192 Garofalo et al.56
reviewed a series of 18 patients with peritalar dislocations in whom no
open reductions were required. Recent series, particularly from trauma
centers, have noted the need for open reduction to be more common, with
up to 32% of patients requiring open reduction.9
entrapped, resulting in a block to closed reduction. These impediments
require open manipulation or release to facilitate reduction. With
medial dislocations, the talar head can become trapped by the capsule
of the talonavicular joint, the extensor retinaculum or the extensor
tendons, or the extensor digitorum brevis muscle. Heck et al.74
studied the irreducible medial subtalar dislocation in a cadaver model.
Entrapment of the talar head in the extensor retinaculum, talonavicular
impaction, and impingement of the deep peroneal nerve and dorsalis
pedis branches between the talus and navicular were implicated as
causes of irreducible subtalar dislocation.74 Talonavicular impaction is often implicated as an obstruction to closed reduction (Fig. 58-35).
The extreme medial displacement of the foot at the moment of injury is
followed by recoil toward the normal position, causing the lateral edge
of the navicular to impinge on the medial talus. An impaction fracture
is produced and the articular surfaces become interlocked.
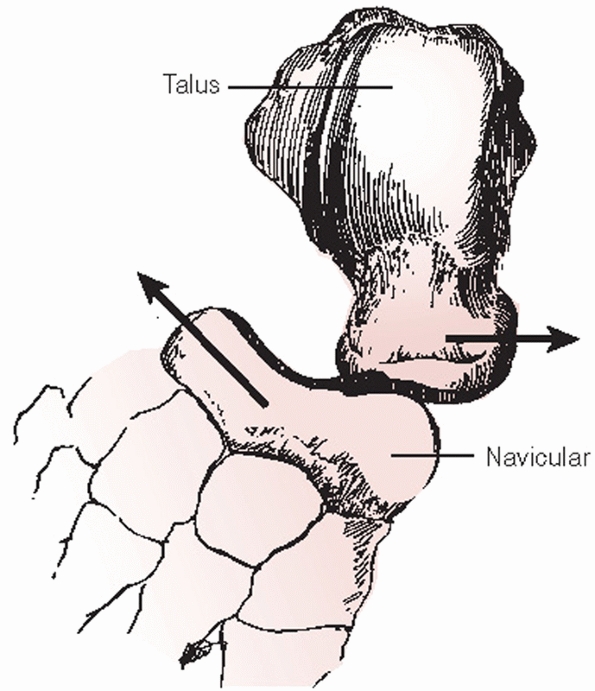 |
|
FIGURE 58-35
Line drawing of a medial subtalar dislocation, irreducible by closed means, due to impaction of the talus and navicular with interlocking of the articular surfaces. (Buckingham WW Jr. Subtalar dislocation of the foot. J Trauma 1973;13:757.) |
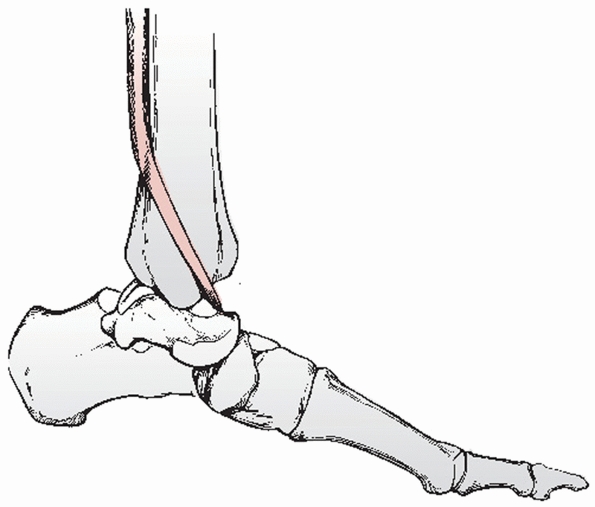 |
|
FIGURE 58-36
Lateral subtalar dislocation with interposed posterior tibial tendon preventing closed reduction. (Leitner B. Obstacles to reduction in subtalar dislocations. J Bone Joint Surg 1954;36A:299.) |
of a lateral subtalar dislocation. The posterior tibial tendon has also
been implicated as a barrier to closed reduction, as it can be
displaced and wrapped around the head of the talus (Fig. 58-36). Woodruff et al.213
presented a case in which the musculotendinous junction of the tibialis
posterior muscle allowed the extreme tendon excursion required to
displace the tendon around the talar head. Alternatively, the flexor
retinaculum may be torn such that the talar head can buttonhole between
the flexor tendons.213
performed through a longitudinal anteromedial incision. This approach
allows access to the structures that may be incarcerating the head of
the talus and allows visualization of an interlocked impaction fracture
of the talus and navicular. With a lateral peritalar dislocation, the
incision may be sited more medially to facilitate manipulation of the
posterior tibial tendon.
bone or soft tissue that is preventing closed reduction. Osteochondral
shear fractures may block reduction, and fragments should be removed if
small and nonstructural.117 It is
often possible to repair displaced bone fragments with small screws or
to elevate and bone graft impacted fragments. Entrapped soft tissue can
usually be gently distracted and the reduction achieved (Fig. 58-37). However, the extensor retinaculum in particular may require transection to facilitate a reduction.
when entrapped may present a substantial barrier, even to open
reduction, as it may become very firmly entrapped. Extreme varus and
plantarflexion of the hindfoot is necessary to relax the tendon, along
with extending the incision through the flexor retinaculum. Even so, in
some cases it has been necessary to transect the posterior tibial
tendon to achieve a reduction.110 This should be done as a last resort only, and it should be repaired and protected following reduction.
assessed for congruency radiographically and for stability. If an open
reduction was required because of soft tissue interposition, the
reduction is usually stable. However, if large or multiple bone
fragments required removal, stability may be less than ideal. Internal
fixation with smooth wires across the subtalar and talonavicular joints
may be necessary to maintain the reduction.56
Following 4 to 6 weeks of immobilization, the internal fixation can be
removed and weight bearing and active physiotherapy instituted.
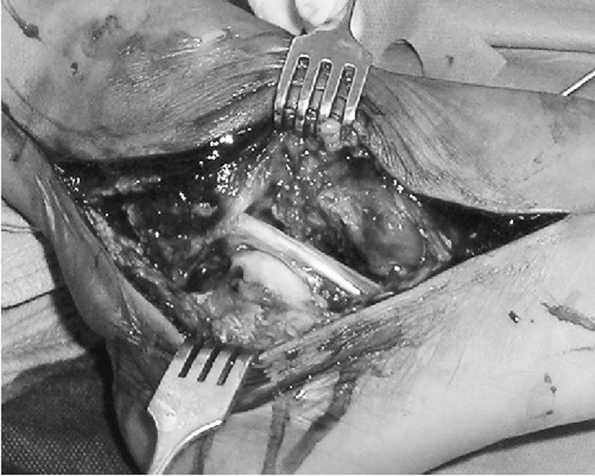 |
|
FIGURE 58-37
Clinical photograph of a complex lateral peritalar dislocation with entrapment of the peroneal tendons between the calcaneus and cuboid. Removal of the peroneal tendons was required to facilitate reduction. |
initially treated by an attempted closed reduction. Once reduced, the
dislocation is usually stable and no internal fixation is necessary. I
obtain a CT scan for all subtalar dislocations once the reduction has
been attempted. If the closed reduction has been unsuccessful, CT scan
provides useful information regarding any bony obstacles to reduction.
Following reduction, the CT scan confirms that an anatomic reduction
has been achieved and is also useful to assess whether associated
osteochondral fractures require further intervention.
dislocation, I prefer the use of a well-padded splint until swelling
has receded, followed by the application of a short leg removable
brace. Patients are encouraged to actively move the ankle, subtalar,
and midtarsal joints after approximately 2 weeks but are advised to
continue to wear the brace while weight bearing for approximately 4 to
6 weeks. As a result, the goals of early motion are achieved while
maintaining protection from sudden and unexpected inversion and
eversion forces.
not achieve a congruent joint. I have found the need for open reduction
to be more common than the 10% to 15% often quoted in the literature. I
perform an anteromedial approach in most cases and try to avoid
incisions through
any
region of impending or potential skin necrosis (usually localized
directly over the talar head). Impaction fractures are usually treated
by disimpaction and reduction, followed by elevation and grafting of
the fragments. Soft tissue entrapments are carefully inspected for
interposed neurovascular structures, then distracted and released as
necessary. The posterior tibial tendon should be protected as much as
possible in a lateral dislocation, but despite efforts to preserve the
tendon, it may not function normally after the reduction, leading to
problems later. Smooth Steinmann pins are sometimes necessary to
immobilize the hindfoot when the reduction is not stable due to
associated bone fragments. When internal fixation is necessary, I
immobilize the foot until the pins are removed (usually 6 weeks later)
and then recommend active motion physiotherapy.
their prognosis. Uncomplicated subtalar dislocations, stable following
a closed reduction, have an excellent prognosis with minimal symptoms
at long-term follow-up. Limitation of subtalar joint motion is a
consistent abnormal finding and may be associated with pain when
walking on uneven ground or pain with weather changes.17,62,110,182 Perugia et al.157
reported on 45 patients with subtalar dislocations followed for a mean
of 7.5 years in whom the mean ankle and hindfoot functional outcome
score was in the good to excellent range. Only 1 patient in their study
required a subtalar arthrodesis.157
studied 25 patients from a Level I trauma center. Of the 18 patients
who were available for review at a mean of 5 years, 89% demonstrated
radiographic changes of ankle arthritis, 89% demonstrated subtalar
arthritis, and 72% demonstrated midfoot arthritis. Functional outcome
scores were much lower than in the study of Perugia et al.,157 and 8 patients required an arthrodesis of the ankle or subtalar joints.9
in a review of the literature, noted that associated injuries and
complications were associated with a worse result. In particular, soft
tissue injury, extra-articular fracture, intra-articular fracture, and
osteonecrosis were associated with a worse outcome.107 Open fractures are undoubtedly associated with the poorest results. Goldner et al.60
reviewed 15 patients at a mean of 18 years following an open subtalar
dislocation. Associated injuries were noted to the tibial nerve in 10
patients, to the posterior tibial tendon in 5, and to the posterior
tibial artery in 5. Seven patients ultimately required arthrodesis due
to osteonecrosis or posttraumatic arthritis.
The mechanism of injury is an important factor in predicting long-term
outcome. Inversion dislocations resulting from a low-energy mechanism,
such as the “basketball foot,” rarely result in long-term morbidity.
Violent mechanisms such as a fall from a height or a motor vehicle
collision are much more likely to cause long-term problems. Lateral
subtalar dislocations may have a worse outcome compared to medial
dislocations, but it is likely that the energy of the mechanism is more
important than the direction.36 Associated fractures and articular cartilage damage may also be more common with lateral dislocations.
peritalar dislocations. Overall, osteonecrosis is uncommon and
generally only noted with high-energy and open injuries. Theoretically,
the talus is not displaced from the ankle mortise and, therefore, at
least some of the blood supply should be preserved. However, Goldner et
al.60 noted osteonecrosis in 5 of 15 patients with type III open subtalar dislocations, and Bibbo et al.9 noted osteonecrosis in 3 patients.
The subtalar and talonavicular joints have a substantial degree of
intrinsic stability such that early mobilization can usually be
undertaken safely and effectively. However, repeat subluxation has been
noted when immobilization was discontinued early215 and in patients with generalized joint laxity.86 Subluxation which occurs early may be treated with repeat closed reduction with good results.77
dislocation. The causes of arthritis include associated fractures,
cartilage damage, and potentially unrecognized instability. Arthritis
can be noted in the ankle or the midfoot, but is most common in the
subtalar joint itself. Reports on the incidence of subtalar arthritis
range from as low as 25% to as high as 89%.9,36,77,125,215
While the radiographic appearance of subtalar changes are not always
symptomatic, progression to severe and painful arthritis can only be
treated with an arthrodesis.
resulting from an extension of the forces causing a subtalar
dislocation. An extension of the supination force causing medial
subtalar dislocation will result in a total lateral talar
dislocation,and an extension of the pronation force causing a lateral
subtalar dislocation will result in a total medial talar dislocation (Fig.58-38).113
The injury is usually associated with some degree of associated
fracture in the hindfoot but has been reported without fracture in a
rare case of posterior dislocation.162
complete dislocation of the talus is a devastating injury. Results are
complicated by infection, osteonecrosis, and posttraumatic arthritis.
Most of the injuries are open. Detenbeck and Kelly38
reported a series of nine cases of complete dislocation of the talus.
Eight of nine eventually required talectomy for control of persistent
infection.38
early and thorough débridement of contaminated and nonviable tissue is
performed, as well as an urgent reduction of the talus to reduce skin
tension. In the limited number of available series, most authors
recommend reduction and preservation of the native talus, with
arthrodesis and talectomy reserved for treatment of complications.78,99,118,131,143,167,177 Based upon their results, Detenbeck and Kelly38 recommended excision of the talus and primary tibiocalcaneal arthrodesis. However, Taymaz et al.193
report a case treated simply with closed reduction and 6 weeks of
immobilization in which the patient had an essentially normal ankle at
9 years of follow-up, demonstrating that the outcome is not universally
poor.
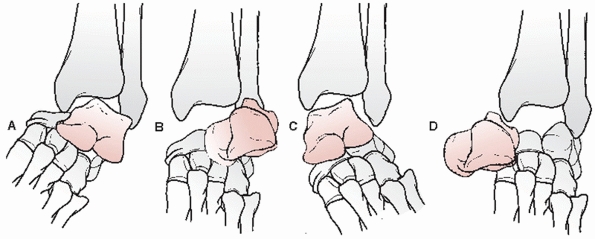 |
|
FIGURE 58-38
More extreme application of the same forces that produced subtalar dislocation can result in total talar dislocation. Supination produces medial subtalar dislocation (A) followed by subluxation and finally complete lateral dislocation of the talus (B). Pronation initially produces lateral subtalar dislocation (C), followed by talar subluxation, and eventually total medial dislocation of the talus (D). (Leitner B. The mechanism of total dislocation of the talus. J Bone Joint Surg 1955;37-A:93.) |
dislocated talus is required. Aids to reduction include a calcaneal
traction pin or distractor. An anteromedial or anterolateral arthrotomy
can be used. Blocks to reduction include the extrinsic tendons,
associated fracture fragments, and capsular soft tissues.124
The reduction is frequently unstable, requiring transfixion of the
subtalar or talonavicular joints. Immobilization should be continued
until soft tissue healing has achieved stability, which is usually at
least 6 weeks. Osteonecrosis can be anticipated such that early
treatment with a patellar tendon bearing orthosis may be considered.
Due to the anticipated development of complications, including
osteonecrosis and arthritis, patients should be counseled that
reconstructive surgery is likely to be required in the future in the
form of arthrodesis of involved and symptomatic joints.
RS. Surgical treatment of fractures of the talus. In Gould JS, ed.
Operative Foot Surgery. Philadelphia: WB Saunders, 1994:377-398.
IJ, Watson JT. Step-cut osteotomy of the medial malleolus for exposure
of the medial ankle joint space. Foot Ankle 1991:11:242-243.
M, Sanders DW, Valdivia G, et al. Comminuted talar neck fractures: a
mechanical comparison of fixation techniques. J Orthop Trauma
2007;21:47-51.
C, Anderson RB, Davis WH. Injury characteristics and the clinical
outcome of subtalar dislocations: a clinical and radiographic analysis
of 25 cases. Foot Ank Int 2003;24:158-163.
C, Lin SS, Abidi N, et al. Missed and associated injuries after
subtalar dislocation: the role of CT. Foot Ankle Int 2001;22(4):324-328.
KP, Ehlert KJ. A stress fracture of the lateral process of the talus in
a runner: a case report. J Bone Joint Surg 1994;76A:441-443.
HC. Comminuted fractures and fracture-dislocations of the body of the
astragalus: operative treatment. Am J Surg 1943;59:37-43.
MS, Lapidus PW. The functional disturbances caused by the inconstant
bones and sesamoids of the foot. Arch Surg 1931;22:936-975.
ST, Kelly FB Jr. Fractures of the neck of the talus: long-term
evaluation of 71 cases. J Bone Joint Surg 1978;60A:143-156.
CA. Rupture of the posterior talotibial ligament with the avulsion of a
bone fragment from the talus. Acta Orthop Scand 1974;45:454-461.
G, Sanders D, Yuan X, et al. Clinical accuracy of imaging techniques
for talar neck malunion. J Orthop Trauma 2008;22:415-418.
JM. Sur Quelques Arthropathies qui paraissent pendre d’une lesion
cerveau ou de la moelle epiniere. Arch Physiol Normale Pathol
1868;1:161-178.
MD, Parks BG, Weber TG, et al. Comparison of plate and screw fixation
and screw fixation alone in a comminuted talar neck fracture model.
Foot Ank Int 2006; 27:340-343.
AP, Conroy JL, Giannoudis PV, et al. Impingement fractureof the
posteromedial process of the talus—a case report. Acta Orthop Scan
2000;71:642-644.
TR, Smith JW, Ross TI. Varus malalignment of the talar neck. Its effect
on the position of the foot and on subtalar motion. J Bone Joint Surg
Am 1996;78:1559-1567.
Palma L, Santucci A, Marinelli M, et al. Clinical outcome of closed
isolated subtalar dislocations. Arch Orthop Trauma Surg
2008;128(6):593-598.
TW, Ashcroft GP. Flexor hallucis longus tendon interposition in a
fracture of the medial tubercle of the posterior process of the talus.
Injury 1997;28:551-552.
M. Luxation du pied en dehors, compliquee de l’issue de l’astragale a
travers la capsule et les tegumens dechires. J. Corvisart Leroux Boyer
1811;22:348-355.
NA, Karkare N, Gehling D, et al Use of a 30-degree external rotation
view for posteromedial tubercle fractures of the talus. J Orthop Trauma
2007;21:579-582.
NA, Mekhail AO, Salpietro BJ, et al. Talar neck fractures: anatomic
considerations for posterior screw application. Foot Ankle Int
1996;17:541-547.
NA, Patil V, Frisch NC, et al. Diagnosis of medial tubercle fractures
of the talar posterior process using oblique views. Injury
2007;38:1313-1317.
NA, Sabry FF, Nadim Y. Internal architecture of the talus: implication
for talar fracture. Foot Ankle Int 1999;20:794-796.
NA, Skie MC, Podeszwa DA, et al. Evaluation of process fractures of the
talus using computed tomography. J Orthop Trauma 1994;8(4):332-337.
H, Ebraheim NA, Tile M, et al. Fractures of the talus: experience of
two-level 1 trauma centers. Foot Ankle Int 2000;21:1023-1029.
R, Martin DP, Agel J, et al. Development of a musculoskeletal extremity
health status instrument: the musculoskeletal function assessment
instrument. J Orthop Res 1996;14:173-181.
O. Fracture of the lateral process of the talus: supination-dorsal
flexion fracture. Acta Orthop Scand 1968;39:407-412.
Chateau PB, Brokaw DS, Jelen BA, et al. Plate fixation of talar neck
fractures: preliminary review of a new technique in 23 patients. J
Orthop Trauma 2002:16: 213-219.
JR, Srinivasan SC, Crandall JR. Snowboarder’s talus fractures
experimentally produced by eversion and dorsiflexion. Am J Sports Med
2003;31(6):921-928.
R, Moretti B, Ortolano V, et al. Peritalar dislocations: a
retrospective study of 18 cases. J Foot Ankle Surg 2004;43:166-172.
AY, Lin SS, Abidi N, et al. Pseudo os trigonum sign: missed
posteromedial talar facet fracture. Foot Ank Int 2003;24:642-649.
JL, Poletti SC, Gates HS 3rd, et al. Severe open subtalar dislocations.
Long-term results. J Bone Joint Surg Am 1995;77A:1075-1079.
J, Berkowitz RD, Whitelaw GP, et al. Hawkins type III
fracture-dislocation of the talus and diastasis of the tibiofibular
joint without concomitant fracture of the malleoli: a case report. Clin
Orthop 1992;279:254-257.
I, Atilla S, Arac S, et al. A new technique of talectomy for severe
fracture-dislocation of the talus. J Bone Joint Surg Br 1993;75:69-71.
RA, Sullivan CR, Kelly PJ, et al. The extraosseous and intraosseous
blood supply of the talus. J Bone Joint Surg 1958;40A:1115-1120.
WG. Stenosing tenosynovitis of the flexor hallucis longus tendon and
posterior impingement upon the os trigonum in ballet dancers. Foot
Ankle 1982;3:74-80.
H, Al Sayed H, Barghash I. Primary ankle fusion using Blair technique
for severely comminuted fracture of the talus. Med Princ Pract
2003;12:47-50.
BE, Ebraheim NA, Jackson WT. Anatomical considerations of irreducible
medial subtalar dislocation. Foot Ankle Int 1992;17:103-106.
Ovejero AM, Garcia Mata S, Heras Izaguirre J, et al. Posteromedial
dislocation of the talus: a case report and review of the literature.
Acta Orthop Belg 1991;57: 63-67.
H, Sailer R, Daniaux H, etal. Revascularization of a partially necrotic
talus with a vascularized bone graft from the iliac crest. Arch Orthop
Trauma Surg 1989;108: 27-29.
S, Ogawa K, Usami N. Classification of fractures of the talus: clear
differentiation between neck and body fractures. Foot Ankle Int
1996;17:748-750.
S, Usami N. Closed complete rupture of the flexor hallucis longus
tendon at the groove of the talus. Foot Ankle Int 1997;18:47-49.
K, Kubota H, Hasegawa A, et al. Fracture of the posterior medial
tubercle of the talus treated by internal fixation: a report of two
cases. Foot Ank Int 1995;16: 164-1665.
JE, Edwards CC, Browner BD, et al. Acute management of major trauma
invoving the foot and ankle with Hoffman external fixation. Foot Ankle
1981;1: 348-361.
AY, Shelton ML. Primary internal fixation of open fractures: a
retrospective study of the use of metallic internal fixation in fresh
open fractures. J Trauma 1972; 12:756-763.
N, Nand S, Walker AP. Primary talectomy for severe fracture-dislocation
of the talus with a 15-year follow-up: case report. Foot Ank Int
2007;28(2):272-275.
GN, Gautam VK, Kochhar VL. Locking of posterior process of talus in the
sulcus calcanei in a case of peritalar dislocation. Injury
1989;20:49-50.
DH, Berkowitz MJ, Pressman DN. Avulsion fractures of the medial
tubercle of the posterior process of the talus. Foot Ank Int
2003;24:172-175.
DH, Hrutkay JM, Samson MM. Fracture of the medial tubercle of the
posterior process of the talus: a case report and literature review.
Foot Ankle Int 1996;17: 186-188.
EH, Lindenmaier HL, Munst P. Talus Fractures. In: Tscherne H, Schatzker
J, eds. Major Fractures of the Pilon, the Talus, and the Calcaneus.
Current Concepts of Treatment. New York: Springer-Verlag, 1993:71-85.
P, Nickisch F, Spenciner D, et al. In vitro evaluation of the effect of
lateral process excision on ankle and subtalar joint stability. Foot
Ank Int 2007:28:78-83.
RL, Sullivan CR, Janes JM. Trauma, Surgery, and Circulation of the
talus—what are the risks of avascular necrosis? J Trauma 1961;1:13-21.
E, Haidukewych G, DiPasquale T, et al. Open reduction and stable
fixation of isolated displaced talar neck and body fractures. J Bone
Joint Surg Am 2004;86-A: 2229-2234.
WJ, Wombwell JH, Nunley JA. Intra-articular talar fractures: repair
using the Herbert bone screw. Foot Ankle 1989;10:88-92.
BP, Girgis I, Moriarty RV. Irreducible talar dislocation with
entrapment by the tibialis posterior and the flexor digitorum longus
tendons: a case report. Clin Orthop 1993;286:222-224.
WE. Operative intervention for fracture of the talus. In: Bateman JE,
Trott AW, eds. Foot and Ankle. New York: BC Decker, 1980:52-63.
MA, Schon LC, Hungerford MW, et al. Avascular necrosis of the talus
treated by core decompression. J Bone Joint Surg Br 1996;78:827-830.
I, Zych A. An unusual fracture of the talus associated with a
bimalleolar ankle fracture: a case report and review of the literature.
Clin Orthop 1986;208:278-281.
SK, Pringle RM, Baxter AD. Fracture of the lateral process of the
talus: a report of thirteen cases. J Bone Joint Surg 1974;56B:263-273.
PL, Vellet AD, Levin MF, et al. Current status of magnetic resonance
imaging of the ankle and the hindfoot. Can Assoc Radiol J 1992;43:19-30.
R, Hadley J, Paul C, et al. Snowboarder’s fracture: fracture of the
lateral process of the talus. J Am Board Fam Pract 1994;7:130-133.
J, Royle SG. Fracture of the lateral process of the talus: computed
tomographic scan diagnosis. Br J Sports Med 1992;26:245-246.
GE Jr, Pomerantz GM. Initial management of severe open injuries and
traumatic amputations of the foot. Arch Surg 1972;105:696-698.
Trauma Association Committee for Coding and Classification. Fracture
and Dislocation Compendium—2007. J Orthop Trauma 2007;21 Suppl:S90-S91.
G, Vecsei V, Reddy B, et al. Treatment of talar neck fractures:
clinical results of 50 patients. J Foot Ankle Surg 2000;39:365-375.
T, Kapetsis P, Soucacos P, et al. Unusual fracture-dislocation of the
talus: report of a case. Clin Orthop 1972;83:232-234.
SJ. Relation between the occurrence of bony union and outcome for
fractures of the lateral process of the talus: a case report and
analysis of published reports. Br J Sports Med 2003;37:274-276.
R, Van Bergeyk A, Pinney S. Are displaced talar neck fractures surgical
emergencies? A survey of orthopaedic trauma experts. Foot Ank Int
2005;26:378-381.
L, Goldie IF. The arterial supply of the talus: a study of the
relationship to experimental talar fractures. Acta Orthop Scand
1975;46:1026-1034.
AJ. Immediate tibiocalcaneal arthrodesis with interposition fibular
autograft for salvage after talus fracture: a case report. J Orthop
Trauma 1999;13:589-592.
S, Winkler J, Heineck J, et al. Anatomical reconstruction of malunited
talus fractures: a prospective study of 10 patients followed for 4
years. Acta Orthop 2005; 76:588-596.
Valdivieso T, de Miguel Vielba JA, Hernandez Garcia C, et al. Subtalar
dislocation. A study of nineteen cases. Int Orthop 1996;20(2):83-86.
CL, Johnson KA, Goldstein RH, et al. The patellar tendon brace as a
treatment for neurotrophic arthropathy: a dynamic force monitoring
study. Foot Ankle 1992;13: 14-21.
CL, Marsh JL, Tearse DS. Treatment of displaced talus fractures: an
arthroscopically assisted approach. Foot Ankle Int 1994;15:630-633.
DW, Busam M, Hattwick E, et al. Functional outcomes following displaced
talar neck fractures. J Orthop Trauma 2004;18:265-270.
TG, Ptaxzek AJ, Morrison WB. Fracture of the lateral process of the
talus: appearance at MR imaging and clinical significance. Skeletal
Radiol 1999;28(4): 236-239.
BJ, Wagner UA, Harrington RM, et al. Contact characteristics of the
subtalar joint: the effect of talar neck misalignment. J Orthop Res
1992;10:544-551.
H, Sajadi K, Silver CM, et al. Total dislocation of the talus: a case
report of a 4-year follow-up. Orthop Rev 1980;9:65-68.
M, Shah R, Singh R. Treatment of fracture dislocation of talus by
primary tibiotalar arthrodesis (Blair fusion). Injury 2005;36:823-826.
A, Potchen EJ, Moore J, et al. High-field magnetic-resonance imaging of
aseptic necrosis of the talus: a case report. J Bone Joint Surg
1966;68A:927-928.
WL. The astragalus: a case of dislocation, excision and replacement: an
attempt to demonstrate the circulation in this bone. J Bone Joint Surg
1925;7:384-399.
RM, Lauerman WC, Heckman JD. Tarsal tunnel syndrome caused by an
unrecognized fracture of the posterior process of the talus (Cedell
fracture). A case report. J Bone Joint Surg 1994;76A:116-118.
TV, Bray TJ, Holmes GB Jr. Fractures of the talar neck. A mechanical
study of fixation. J Bone Joint Surg Am 1992:75:544-551.
R, Reschauer R, Seggl W. Eighty-five talus fractures treated by ORIF
with 5 to 8 years of follow-up: study of 69 patients. Clin Orthop
1985;199:97-107.
R, Seggl W, Wildburger R. Late results of fractures and
fracture-dislocation after ORIF. In: Tscherne H, Schatzker J, eds.
Major Fractures of the Pilon, the Talus, and the Calcaneus. Current
Concepts of Treatment. New York: Springer-Verlag, 1993: 103-112.
J, Stuffman E, Ross SD. Partial Hawkins sign in fractures of the talus:
a report of three cases. Am J Roentgenol 2003;181:1559-1563.
M, Dumont C, Sturmer K. Prognostic reliability of the Hawkins sign in
fractures of the talus. J Orthop Trauma 2007;21:538-543.
DB, Triffon MJ, Terk MR. Magnetic resonance imaging to detect avascular
necrosis after open reduction and internal fixation of talar neck
fractures. Foot Ankle Int 1996;17:742-747.
DJ, Feder JM, Boylan JP. Fractures of the lateral process of the talus:
two case reports and a comprehensive literature review. Foot Ankle Int
1998;19:641-646.
DC, Schemitsch EH, McKee MD, et al. Do foot injuries significantly
affect the functional outcome of multiply injured patients? J Orthop
Trauma 1999;13:1-4.
V, Perren T, Ryf C, et al. Snowboarder’s talus fracture: treatment
outcome of 20 cases after 3.5 years. Am J Sports Med 2005;33:871-880.
HA, Nork SE, Benirschke SK, et al. Surgical treatment of talar body
fractures: surgical technique. J Bone Joint Surg Am 2004;86A(Suppl 1 Pt
2):180-192.
Tongel A, Matricali GA. Fracture of the posterior medial tubercle of
the talus: a case report and review of the literature. Acta Orthop Belg
2007;73(6):804-806.
BL, Heckman JD, Galindo MJ, et al. Excision of ununited fractures of
the posterior process of the talus: a treatment for chronic posterior
ankle pain. Foot Ankle 1991;12:453-457.
Knoch F, Reckford U, von Knoch M, et al. Fracture of the lateral
process of the talus in snowboarders. J Bone Joint Surg Br
2007;89:772-777.
SL, Bonfiglio M. Unusual accessory (bipartite) talus simulating
fracture: a case report. J Bone Joint Surg 1975;57A:1161-1163.
S, Euler E, Linsenmaier U, et al. C-arm-based mobile computed
tomography: a comparison with established imaging on the basis of
simulated treatments of talus neck fractures in a cadaveric study.
Comput Aided Surg 2004;9:27-38.
RS, Heckman JD. Case report: fracture of the posterior medial tubercle
of the talus secondary to direct trauma. Foot Ankle Int 1998;19:255-258.
MJ, Brown JN, Mountney J. A mechanism for entrapment of the tibialis
posterior tendon in lateral subtalar dislocation. Injury
1996;27:193-194.
BH, Abidi NA, Scheel MJ. Medial malleolar osteotomy for exposure of
complex talar body fractures. J Orthop Trauma 2001;15:513-518.
