Torticollis
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Torticollis
Torticollis
Barry Waldman MD
Andrew P. Manista MD
Description
-
A limitation of motion of the cervical spine that causes the head to be held in a tilted position
-
May result from muscular, skeletal, or neurologic abnormalities (1) (Fig. 1)
-
Classification (3):
-
Congenital abnormalities
-
Acquired abnormalities
-
-
Synonyms: Skeletal wry neck; Congenital
wry neck; Cock-robin deformity; Sandifer syndrome (torticollis
resulting from gastroesophageal reflux disease and hiatal hernia) (2)
General Prevention
The condition cannot be prevented, but prompt referral and treatment may preclude the need for surgery.
Epidemiology
-
The most common cause is rotatory subluxation of the atlantoaxial joint, an acquired condition.
-
Congenital muscular torticollis usually is evident in the first 6–8 weeks of life.
-
Other causes may appear throughout childhood or may become evident well into adulthood.
-
Males and females are affected equally.
Incidence
-
Because of the multiple causes, it is difficult to give a specific figure for incidence.
-
It affects an estimated 1 per 100 to 1 per 1,000 patients (4).
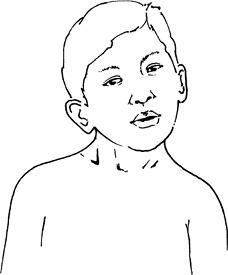 Fig. 1. Torticollis typically produces lateral flexion to 1 side and rotation to the other.
Fig. 1. Torticollis typically produces lateral flexion to 1 side and rotation to the other.
Risk Factors
-
Local trauma to the infant’s neck during delivery, especially during a difficult delivery
-
For atlantoaxial rotatory subluxation: Upper respiratory infection, pharyngitis, or trauma
Genetics
-
Multiple congenital causes of torticollis exist, of which a few have a genetic predisposition.
-
Skeletal dysplasias are the most common genetic syndromes associated with torticollis.
Etiology
-
Congenital muscular torticollis is caused by contracture of the sternocleidomastoid muscle.
-
Congenital bony torticollis may be secondary to occipitocervical abnormalities.
-
Acquired torticollis may result from neurogenic, traumatic, inflammatory, or idiopathic causes (see “Differential Diagnosis”).
-
Bony abnormalities: Atlanto-occipital
synostosis, basilar impression, odontoid abnormalities, cervical
hemivertebrae, or asymmetry of occipital condyles -
Atlantoaxial rotatory subluxation, the
most common bony abnormality, is characterized by rotatory displacement
of C1 on C2 and may be congenital or secondary to inflammation or
trauma.
Signs and Symptoms
-
Hallmark sign: Tilting of the head to 1 side with limitation of ROM
-
Usually the patient rotates the head away from the neutral (straight) position, but not toward it.
-
Patients may present with a neck mass (contracted sternocleidomastoid muscle).
-
Neck pain is a common complaint, but it usually occurs in adults.
-
Patients also may complain of occipital pain, vertigo, or dizziness aggravated by certain movements of the head.
-
If torticollis persists beyond infancy, secondary asymmetry of the cranium (plagiocephaly) may remain.
Physical Exam
-
The patient’s head is tilted, with the
ear toward the involved side and the chin rotated away, with limitation
of ROM toward the corrected position. -
In some cases of muscular torticollis, a
palpable mass may be present on the involved side (contracted
sternocleidomastoid muscle). -
Remodeling of the head or face may result from pressure while sleeping.
-
A short, broad neck with a low hairline may be seen in patients with bony abnormalities or Klippel-Feil syndrome.
Tests
Lab
-
No specific laboratory tests, unless an inflammatory or neoplastic origin is being considered
-
Ophthalmologic, audiologic, and gastroenterologic evaluations sometimes are needed if no obvious skeletal causes are seen.
Imaging
-
AP and lateral radiographs of the
cervical spine should be obtained for any patient with torticollis to
identify bony abnormalities. -
CT is used to evaluate rotatory subluxation, dislocation, or fracture.
-
MRI is used if a neurologic lesion of the brainstem or neck is suspected.
Pathological Findings
In congenital muscular torticollis, the
sternocleidomastoid muscle is fibrotic, replaced by scar tissue in a
nonspecific fashion.
sternocleidomastoid muscle is fibrotic, replaced by scar tissue in a
nonspecific fashion.
Differential Diagnosis
-
Neurogenic causes:
-
Spinal cord tumors of the cervical spine
-
Cerebellar tumors
-
Syringomyelia
-
Ocular dysfunction
-
-
Traumatic causes:
-
Subluxations
-
Fractures and dislocations of the occipitocervical junction
-
-
Inflammatory causes:
-
Cervical adenitis
-
Rheumatoid arthritis
-
-
Idiopathic causes:
-
Atlantoaxial rotatory subluxation or displacement
-
General Measures
-
Congenital muscular torticollis:
-
Responds to stretching exercises in nearly 100% of patients treated before 1 year of age (5,6)
-
Positioning of toys in the crib will encourage the child to stretch the involved side.
-
-
Atlantoaxial rotatory subluxation (7):
-
Patients usually recover with physical therapy if the condition is detected within the 1st week of onset.
-
Use of a soft collar and analgesics is for patients with atlantoaxial rotatory subluxation patients.
-
Patients with recalcitrant cases may require muscle relaxants and a hard collar or brace.
-
If treatment is delayed, traction or even surgery is required.
-
P.469
Activity
-
Contact sports and vigorous athletics should be restricted until the condition has been treated.
-
Specifics depend on the underlying cause.
Special Therapy
Physical Therapy
-
Stretching exercises may be beneficial in patients with muscular torticollis or recent-onset rotatory subluxation.
-
Specific instructions should be given to the therapist.
Medication
Analgesics (acetaminophen, ibuprofen)
Surgery
-
Congenital muscular torticollis that is refractory to stretching may require release of the sternocleidomastoid muscle.
-
Severe atlantoaxial rotatory subluxation or other severe bony abnormality may require fusion of C1 and C2.
Prognosis
Most cases resolve spontaneously or with treatment.
Complications
-
Fixed subluxation
-
Plagiocephaly (in late-treated muscular torticollis)
Patient Monitoring
-
Neurologic status should be followed closely.
-
Bony abnormalities, such as rotatory subluxation, may require repeated CT scans.
References
1. Nucci
P, Kushner BJ, Serafino M, et al. A multi-disciplinary study of the
ocular, orthopaedic, and neurologic causes of abnormal head postures in
children. Am J Ophthalmol 2005;140:65–68.
P, Kushner BJ, Serafino M, et al. A multi-disciplinary study of the
ocular, orthopaedic, and neurologic causes of abnormal head postures in
children. Am J Ophthalmol 2005;140:65–68.
2. Ramenofsky ML, Buyse M, Goldberg MJ, et al. Gastroesophageal reflux and torticollis. J Bone Joint Surg 1978;60A:1140–1141.
3. Cheng JCY, Tang SP. Outcome of surgical treatment of congenital muscular torticollis. Clin Orthop Relat Res 1999;362:190–200.
4. Cheng JCY, Au AWY. Infantile torticollis: A review of 624 cases. J Pediatr Orthop 1994;14:802–808.
5. Canale ST, Griffin DW, Hubbard CN. Congenital muscular torticollis. A long-term follow-up. J Bone Joint Surg 1982;64A:810–816.
6. Morrison
DL, MacEwen GD. Congenital muscular torticollis: Observations regarding
clinical findings, associated conditions, and results of treatment. J Pediatr Orthop 1982;2:500–505.
DL, MacEwen GD. Congenital muscular torticollis: Observations regarding
clinical findings, associated conditions, and results of treatment. J Pediatr Orthop 1982;2:500–505.
7. Phillips WA, Hensinger RN. The management of rotatory atlanto-axial subluxation in children. J Bone Joint Surg 1989;71A:664–668.
Codes
ICD9-CM
-
754.1 Congenital torticollis
-
847.0 Traumatic torticollis
Patient Teaching
-
Once the cause is known, anatomic models may be used to explain the cause of the torticollis to patients and families.
-
Patients and families should be made
aware of the usual course of the condition and the possible need for
different methods of therapy.
FAQ
Q: When is congenital torticollis usually 1st evident clinically?
A: In the first 6–8 weeks of life.
Q: What does a neck mass in a patient with torticollis often represent?
A:
A contracted sternocleidomastoid muscle. However, additional evaluation
may be required in some cases to rule out other causes.
A contracted sternocleidomastoid muscle. However, additional evaluation
may be required in some cases to rule out other causes.
