Köhler Disease
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Köhler Disease
Köhler Disease
Paul D. Sponseller MD
Description
-
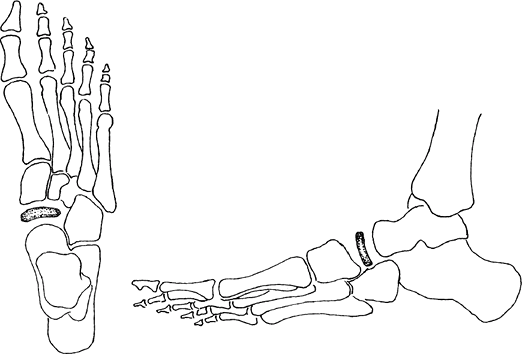
Köhler disease is an eponym for osteochondrosis of the tarsal navicular (scaphoid) bone (Figs. 1 and 2).
-
Pain in the medial midfoot in a young boy (aged 3–7 years) is the typical clinical presentation.
-
The condition usually is worsened with activity and relieved with rest.
-
Clinical outcome usually is good after healing.
-
Classification:
-
This disorder is 1 of multiple disorders
termed “osteochondroses,” which are characterized by transient vascular
impairment of developing bones. -
Others in this category include Legg-Calvé-Perthes disease and OSD
-
-
Synonyms: Osteonecrosis; Osteochondrosis; Osteochondritis of the tarsal navicular
General Prevention
Prevention is not effective or practical in this rare disease.
Epidemiology
A male predominance exists; it is 2–3 times more common in males than in females (1).
Incidence
This disease is uncommon.
 |
|
Fig. 1. Köhler disease is AVN of the tarsal navicular, which usually produces compression of this bone (stippled).
|
Risk Factors
-
Male gender
-
High activity level
-
Sports involving running and kicking
Genetics
No known genetic transmission of this disorder
Etiology
-
The most likely cause is mechanical compression of the navicular, thus impairing vascularity.
-
The navicular, which forms the apex of the longitudinal arch of the foot, is subject to constant compression during walking.
-
These forces appear to compromise the
circulation within the bone during a critical phase early in the
ossification of the navicular.
Associated Conditions
A slight association seems evident with Legg-Calvé-Perthes disease (childhood osteonecrosis of the femoral head) (1).
Signs and Symptoms
-
Medial midfoot pain worsening with activity
-
Tenderness to palpation
-
Limp
-
Walking on the outside of the foot to avoid stress on the navicular
Physical Exam
-
Look for tenderness over the navicular with soft-tissue swelling about the navicular and an antalgic gait.
-
Some patients walk on the outer border of the foot to minimize compression of the navicular.
Tests
Imaging
-
Plain films are sufficient to make the diagnosis during the established phase.
-
The normal navicular begins to ossify at age 2–3 years.
-
It may start normally from several small ossification centers that eventually coalesce.
-
In Köhler disease, the navicular is flattened in its AP diameter and may show irregular sclerosis.
-
It may be bilateral.
-
-
If the suspicion is high in spite of normal radiographs, MRI may be used to look for abnormal circulation within the navicular.
-
With healing, increased ossification and resumption of normal growth occur.
Pathological Findings
-
Pathologic specimens are not obtained routinely nor are they necessary for diagnosis.
-
Some specimens reported in the literature
show areas of necrosis, resorption of dead bone, and formation of new
bone, which are general findings of healing osteonecrosis.
Differential Diagnosis
-
Ankle fracture
-
Ankle sprain
-
Navicular fracture
-
Accessory navicular
-
Soft-tissue infection
 Fig. 2. Radiographic appearance of Köhler disease. Note the relative sclerosis and collapse of the navicular.
Fig. 2. Radiographic appearance of Köhler disease. Note the relative sclerosis and collapse of the navicular.
P.225
General Measures
-
Rest, arch support, and/or casting, depending on the level of symptoms:
-
For minimally symptomatic patients, the
use of an arch support or refraining from strenuous activities may be
all that is needed. -
For more pronounced symptoms, a below-the-knee cast with a well-molded arch, worn for 4–8 weeks, usually provides relief.
-
If the symptoms are severe, the patient may need to avoid weightbearing in the cast.
-
After casting, if tenderness is minimal, use of an arch support and gradual resumption of activities are advised.
-
-
Return to activity is based on physical examination.
Activity
-
The patient should avoid activities that produce the pain, including sports involving running, jumping, and kicking.
-
After symptoms resolve, the patient may resume those activities gradually, with use of an arch support.
Special Therapy
Physical Therapy
-
Physical therapy is not needed.
-
Parents may be put in charge of timing the return to activities, based on the child’s symptoms.
Medication
Acetaminophen or NSAIDs as needed
Surgery
-
Surgery rarely is needed.
-
Some persistent symptoms after maturity have required fusion of the talonavicular joint (1).
Prognosis
-
Prognosis is good.
-
In 2–3 years, the radiographic appearance of the navicular usually returns to normal, and the patient’s symptoms resolve (2).
Complications
-
Rarely, ache or tenderness may persist.
-
These symptoms may be treated in the same fashion, by rest, arch support, or (rarely) surgery.
Patient Monitoring
The course of the disease should be followed by clinical examination (tenderness, limp), rather than by radiography.
References
1. Kasser
JR. The foot. Acquired conditions. In: Morrissy RT, Weinstein SL, eds.
Lovell and Winter’s Pediatric Orthopaedics, 6th ed. Philadelphia:
Lippincott Williams & Wilkins, 2006:1311–1321.
JR. The foot. Acquired conditions. In: Morrissy RT, Weinstein SL, eds.
Lovell and Winter’s Pediatric Orthopaedics, 6th ed. Philadelphia:
Lippincott Williams & Wilkins, 2006:1311–1321.
2. Ippolito E, Ricciardi Pollini PT, Falez F. Kohler’s disease of the tarsal navicular: long-term follow-up of 12 cases. J Pediatr Orthop 1984;4:416–417.
Codes
ICD9-CM
732.5 Juvenile osteochondrosis of foot
Patient Teaching
Activity
Patients should be counseled about the benign,
self-resolving nature of this condition and its relation to activity so
they may moderate activities accordingly.
self-resolving nature of this condition and its relation to activity so
they may moderate activities accordingly.
Prevention
Prevention is not effective or practical in this rare disease.
FAQ
Q: Does Köhler disease lead to arthritis of the foot?
A: No evidence exists of long-term sequelae after the process heals.
