The Forearm and Elbow
origin but believed to involve nerve and muscle, possibly anterior horn
cells, occurring in approximately 1/3,000 live births. These children
have a predictable pattern of muscle weakness and joint contracture.
Although the elbow may present in a 90° flexed position, a typical
clinical presentation is shoulder girdle wasting, stiff extended
elbows, pronated forearms, and flexed wrists. The primary goal is to
provide these children with one elbow that will allow hand to mouth
while maintaining one arm extended, facilitating lower extremity or
perineal care.
instructed on manual stretching exercises in an attempt to achieve some
element of a supple elbow. Later during this initial treatment phase,
static elbow splints are worn to maintain passive range of elbow
motion. Once improved passive elbow motion is achieved, tendon
transfers about the elbow are considered following posterior elbow
joint release. Some prefer a two-staged operative approach while others
will perform
both
procedures at once. Muscle transfers accomplishing elbow flex can
include triceps transfer, pectoralis major muscle transfer, or a free
gracilis muscle transfer. Although surgical results are not ideal,
these children are typically of normal intelligence, respond well to
physical therapy, and can become independent.
remains speculative. Suggested origins include congenital,
developmental or posttraumatic. A commonly considered traumatic cause
is the “nursemaid’s elbow” or the pulled elbow of infancy.
Developmental causation can result from an ulnar aplasia, multiple
exostosis, and multiple enchondromatosis. Radiographic evidence of a
true congenital cause is hypoplasia of the capitellum, a rounded
appearance of the radial head articular surface and a thin radial neck.
Clinical evidence of a congenital origin for this condition is the
presence of bilateral involvement.
Disability from degenerative arthritis is seldom seen in patients
having congenital dislocation of the radial head. If degenerative
arthritis is seen, radial head resection in the adult patient is the
preferred treatment option. In a recent study, Sacher and Mih have
reported encouraging results in children having surgery for radial head
dislocation, but the long-term efficacy of such a procedure is unknown.
As many patients do well with this condition, supportive care may be
all that is necessary for congenital radial head dislocation,
irrespective of the cause.
 |
|
FIGURE 13-1. Congenital radioulnar synostosis involving proximal aspect of the radius and the ulna.
|
fetal development when the longitudinal separation of the forearm
anlage does not completely occur. The most common presentation is a
failure of proximal separation of the radius and ulna leaving a
coalition between these bones (Figure 13-1).
Other presentations of congenital elbow synostosis include radiohumeral
synostosis, ulnohumeral synostosis, or synostosis involving all three
bones about the elbow. Radioulnar synostosis is seen in patients with
fetal alcohol syndrome and is also seen in association with hip
dysplasia, clubfoot, and a variety of congenital hand anomalies.
become apparent until the child has difficulty with a simple task that
requires forearm rotation. Physical examination often finds a forearm
fixed in a midrange pronated position, which is often a functional
position. Patients with a forearm in the completely pronated position
likely suffer from notable functional disability. Fortunately, this
condition is unusual and patients generally adapt, through wrist
hypermobility, to the degree that little functional disability
persists. In the patients with disability, treatment can consist of a
derotational osteotomy either in the midforearm or at the level of the
synostosis. When extreme forearm positions are
corrected,
injury to nerve and arterial structures can occur as the forearm is
derotated to a more neutral position. Such injury can result in hand
ischemia or even compartment syndrome. Careful postoperative monitoring
is necessary following these procedures. Fortunately, most children
with congenital radioulnar synostosis are left with a forearm in a
functional position and surgery is not necessary.
elbow are much less common than carpal tunnel syndrome. Some have
reported that median nerve neuropathies about the proximal forearm and
elbow account for less than 1% of all entrapment neuropathies. Anterior
interosseous syndrome occurs due to fascial bands or aberrant blood
vessels compressing the anterior branch of the median nerve. Pronator
syndrome is caused from direct compression of the median nerve by the
pronator teres muscle. The site of compression is distal to the branch
of the anterior interosseous nerve.
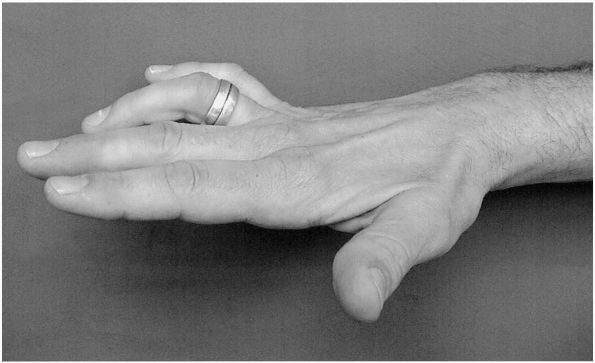
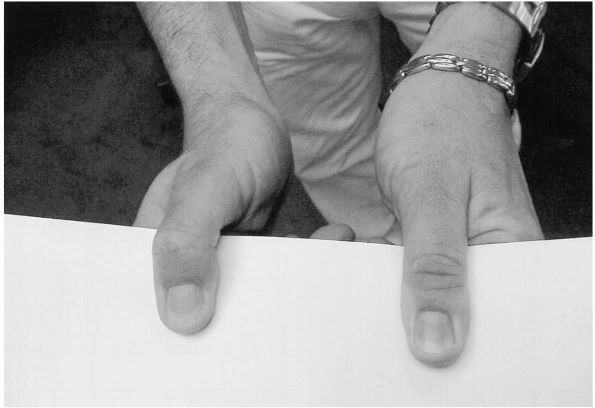
with weakness of the flexor pollicis longus muscle and the flexor
digitorum profundus to the index. Characteristic hyperextension
posturing of the distal interphalangeal joints of the index finger and
thumb are seen. Patients cannot make an “OK” sign due to FPL and FDPI
weakness. Sensory examination is normal and pain, paresthesias absent.
The diagnosis of anterior interosseous syndrome should be distinguished
from Parsonage-Turner syndrome, or brachial neuritis. In
Parsonage-Turner syndrome, a painful shoulder and arm prodrome exists
with paralysis of the anterior interosseous nerve occurring later.
Trauma, surgery, flu, or a vaccination may precede the diagnosis of
Parsonage-Turner syndrome. The cause of this peculiar syndrome is
uncertain.
diagnosing advanced anterior interosseous lesions, although
electrodiagnostic testing is often unreliable in the earlier stages of
the condition. Neurodiagnostic studies are not helpful for 6 weeks
following the onset of symptoms due to neurophysiologic equilibration
of the nerve.
instructed to avoid repetitive gripping and lifting. Long-arm splinting
and nonsteroidal anti-inflammatory drugs (NSAIDs) may prove helpful. If
no improvement in FPL and FDPI is seen in 3 to 4 months, surgical
exploration and decompression of the anterior interosseous nerve is
indicated. This decompression is accomplished through a generous
incision over the volar aspect of the proximal forearm, which often
leaves a rather unsightly scar. Treatment for Parsonage-Turner syndrome
is nonsurgical with return of function seen up to 2 years following the
onset of symptoms.
with pronator syndrome present with vague anterior forearm pain and
unpredictable sensory changes of the hand. The forearm pain is
exacerbated by repetitive activities such as hammering and forced
gripping. Decreased sensation may be found in the thumb, index finger,
long finger, and the radial aspect of the ring finger. The pattern of
sensory change can be distinguished from carpal tunnel syndrome by the
loss of sensation in the palm of the hand caused by involvement of the
palmar cutaneous branch of the median nerve. Patients with pronator
syndrome typically do not experience night paresthesias, further
distinguishing the condition from carpal tunnel syndrome.
Electrodiagnostic studies are helpful only in 40 to 50% of cases. The
diagnostic acumen of neurodiagnostic studies for pronator syndrome is
limited due to the proximal forearm median nerve conduction velocity
delays often seen in carpal tunnel syndrome. The diagnosis, then, is
clinical. Physical examination findings include tenderness over the
course of the median nerve in the forearm, a Tinel’s sign in the
proximal forearm, and a positive nerve compression test in the proximal
forearm. Much like the carpal tunnel compression test in the wrist, the
proximal forearm compression test is performed by applying firm, direct
pressure over the median nerve at the pronator arcade. The pressure is
held for 30 seconds. A positive test is elicited by pain in the forearm
or paresthesias in the median nerve distribution of the hand.
Hyperflexion of the elbow and pronation of the forearms may also elicit
symptoms.
treatment of pronator syndrome is nonoperative. Activity restriction
with goal-directed recovery under the supervision of a certified hand
therapist is, perhaps, the most effective nonoperative measure. NSAIDs
and removable long-arm splinting with the elbow in 90° flexion and the
forearm in neutral may prove useful. Failure to improve following 6
months of nonoperative therapy is an indication
for
surgical exploration and decompression of the median nerve in the
forearm. Sites of compression can not only include the interval between
the two heads of the pronator teres, the fibrous elements of the
lacertus fibrosis, or the proximal arch of the flexor digitorum
sublimus muscle.
into the superficial radial nerve and the posterior interosseous nerve
(PIN). The superficial radial nerve courses distally beneath the
brachioradialis muscle over the dorsal radial aspect of the forearm
before emerging to a subcutaneous position at the junction of its
distal third and middle third. The posterior interosseous nerve travels
around the radial neck and through the interval between the two heads
of the supinator muscle. This opening, which often has an overlying,
compressive fibrous arch, is known as the arcade of Frosche. The space
beneath the supinator muscle belly and where the PIN travels is known
as the radial tunnel. The sites of potential radial nerve compression
are the entrance to the radial tunnel (arcade of Frosche) and the exit
of the superficial radial nerve from beneath the brachioradialis muscle.
as it exits the brachioradialis muscle can result in Wartenberg’s
syndrome. This condition can occur following direct trauma along the
course of the superficial radial nerve or, possibly, as a result of
repetitive forearm movements as might be sustained in certain
occupations. Patients with compressive neuropathy of the superficial
radial nerve present with pain, paresthesias, or anesthesia over the
dorsum of the hand. Clinical examination may find tenderness over the
course of the nerve or a Tinel’s sign where the nerve lies in a
subcutaneous position. Initial treatment is nonoperative, including
splinting, NSAIDs, and activity avoidance or modification. In rare
instances, surgical decompression of the nerve may be necessary.
 |
|
FIGURE 13-2.
Dorsal aspect of the posterior forearm with posterior interosseous nerve (PIN) exposed following release of the supinator. Notice flattening and discoloration of the PIN. |
arcade of Frosche, potentially resulting in one of two different
syndromes. Posterior interosseous nerve syndrome causes a painless
paralysis of digital and wrist extension. External compression of the
PIN may also occur due to ganglion cyst formation from the elbow joint
or the development of other neoplasms. PIN syndrome may also result
from proliferative synovitis from the radiocapitellar joint in the
patient with rheumatoid arthritis. Electrodiagnostic testing may
localize the site of compression. A brief period of observation and
nonoperative treatment is indicated initially following the onset of
symptoms, but surgical exploration and PIN decompression is indicated
if symptoms do not resolve promptly (Figure 13-2).
condition characterized by volar forearm pain without muscle weakness.
Thought to occur as a result of PIN compression within the radial
tunnel, the condition is often confused with chronic lateral
epicondylitis. Some have suggested that lateral
epicondylitis
and radial tunnel syndrome may coexist, further complicating the
clinical picture. Others, however, have questioned the existence of the
condition altogether. Most patients respond to nonoperative treatment
of activity modification, splinting, NSAIDs, and rest. Surgical
decompression may be indicated in recalcitrant cases and is often
combined with lateral epicondylar release. Electrodiagnostic testing is
often of little diagnostic benefit in patients with radial tunnel
syndrome.
elbow within the fibro-osseous groove known as the cubital tunnel.
Other sites of potential ulnar nerve compression at the elbow or ulnar
include the arcade of Struthers, the medial intermuscular septum, and
the ligament of Osborne. The arcade of Struthers is a constrictive
condensation of fibrous tissue adjacent to the medial intermuscular
septum, located approximately 12 cm proximal to the cubital tunnel. The
intermuscular septum is a sheet of fibrous tissue separating the
triceps from the brachialis muscle. The ulnar nerve lies immediately
posterior to this structure and can be a source of impingement to the
ulnar nerve when treatment calls for anterior transposition of the
nerve. The ligament of Osborne is the fibrous tendinous arch of the
proximal origin of the two heads of the flexor carpi ulnaris tendon.
Ulnar neuropathy may develop idiopathically or as a late result of
trauma. The later is known as tardy ulnar nerve palsy and results from
a malunited distal humerus fracture or from posttraumatic growth arrest
of the distal humerus.
 |
|
FIGURE 13-3. Clawing of the ring and small finger due to ulnar nerve dysfunction.
|
(abnormal sensations) and dysesthesias (lack of feeling) in the small
finger and the ulnar portion of the ring finger. Burning ring and small
finger pain as well as hand weakness and clumsiness are also common
complaints. Physical examination may reveal exacerbation of the
paresthesias with light percussion over the ulnar nerve within the
cubital tunnel (Tinel’s sign). Additionally, the ulnar nerve may be
tender to touch in this region. In more active patients or patients
with a history of sporting activities, the ulnar nerve may be found to
slip in and out of the cubital groove (translocation) during flexion
and extension of the elbow.
weakness of the ulnarly innervated muscles may result. This most
notably manifests itself by clawing of the ring and small fingers (Figure 13-3).
Other signs of ulnar nerve paralysis include interosseous muscle
wasting, Wartenberg’s sign (inability to abduct the small finger in
against the ring finger due to weakness of the palmar interosseous
muscles), and Froment’s sign (substituting thumb IP joint flexion for
thumb adduction due to weakness of the adductor pollicis muscle) (Figure 13-4).
Findings can vary due to aberrations in ulnar nerve anatomy. For
instance, the intrinsic muscles in the hand are innervated by the
median nerve through the Martin-Gruber anastomosis in 7.5% of people.
Electrodiagnostic studies are helpful in confirming the diagnosis and
following recovery.
nonoperative. Queries are first made to identify in occupational or
activities of daily life that may have become an irritant to the ulnar
nerve at the elbow. Avoidance of these activities may be all
that
is necessary in some patients. Further nonoperative measures include
immobilization of the elbow in 30° of extension, followed by periods of
mobilization with elbow padding. An often-used protocol is the
fabrication of an orthoplast, anteriorly based nighttime splint with
the elbow at 30° flexion. The patient is instructed to remove the pad
during the day and wear an elbow pad in an effort to prevent direct
trauma to the nerve and to prevent the patient from applying direct
pressure on the ulnar nerve. A lack of response to these measures by 3
months is generally considered a failure of conservative treatment.
 |
|
FIGURE 13-4. Froment’s sign showing thumb IP joint flexion substituting for adductor pollicis weakness.
|
insertional activity on the electromyographic portion of the
neurodiagnostic studies are indicative of advanced ulnar neuropathy and
indicate the need for surgical treatment of the ulnar neuropathy. Other
indications for surgical treatment of ulnar neuropathy are clinical
signs of ulnar nerve paralysis and failure of nonoperative management.
Opinions vary on the best surgical procedure for treating ulnar
neuropathy. Options include in situ release, anterior ulnar nerve
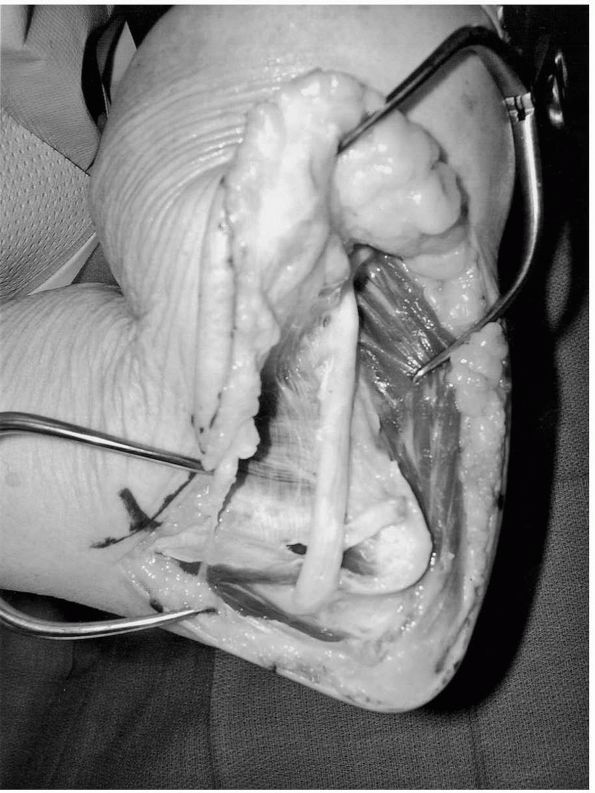
transposition (either subcutaneous, submuscular, or intramuscular) and
medial epicondylectomy. The in situ release is decompression of the
ulnar nerve by release of the cubital tunnel retinaculum and the
ligament of Osborne connecting the two muscle heads of the flexor carpi
ulnaris (FCU). Anterior transposition of the ulnar nerve requires
release of ulnar nerve compression sites and restraints as mentioned
earlier. The transposed ulnar nerve can be placed subcutaneous,
submuscular beneath the flexor-pronator mass, or intramuscular (Figure 13-5).
Medial epicondylectomy removes the anterior bony barrier to nerve
anterior translation. Proponents of this procedure cite the advantage
of less
dissection about the nerve and, therefore, less interruption of ulnar nerve blood supply.
 |
|
FIGURE 13-5.
Anterior transposition of the ulnar nerve. Constraints of the ulnar nerve have been released and the ulnar nerve is prepared for subcutaneous placement. |
treatment are successful with a high degree of patient satisfaction
including nonoperative measures. In one Kaplan-Meier analysis, 80% of
patients with mild ulnar neuropathy were improved with nonoperative
treatment. For the more advanced lesions, submuscular transposition has
a higher patient satisfaction rate compared to the other methods of
treatment.
located between the olecranon process and the skin. This normal
structure may become inflamed and accumulate fluid once injured from
blunt or repetitive trauma. Other causes of olecranon bursitis include
gout, calcium pyrophosphate deposition, and rheumatoid arthritis.
Patients may or may not reveal a history of blunt trauma but repetitive
trauma is often identified with careful history taking. Patients
typically present with a notably swollen and fluctuant posterior elbow.
For nonseptic conditions pain and warmth are generally not elicited.
The diagnosis of the nonseptic olecranon bursitis is clinical and
treatment is conservative. The condition usually responds to a brief
period of activity modification and elbow protection. The elbow may be
protected with a posterior orthoplast splint or alternatively with a
pad. The condition should respond to nonoperative management in 3 to 4
weeks. If the condition does not respond and the bursitis becomes
chronic, infection must be considered and the bursa aspirated for
culture. Culture analysis should include aerobic, anaerobic, fungus,
and mycobacterium analysis. Nonseptic, chronic, long-standing olecranon
bursa unresponsive to conservative management occasionally requires
surgery. However, bursectomy is often complicated by wound-healing
problems and should only be considered after extensive nonoperative
therapy.
innocuous injury and must always be considered in immunocompromised
patients. These infections can progress insidiously leading to
devastating consequences. Abscesses can track proximally and distally
in the arm along fascial planes leading to a necritizing fasciitis,
particularly in the immunocompromised host. The most common organism is
Staphylococcus aureus. The isolation of methicillin-resistant S. aureus is becoming increasingly more common.
drainage, and debridement, leaving the wound open to heal by secondary
intention. Wound care of the open olecranon wound following incision
and drainage can be facilitated by use of a negative pressure wound
closure assist device. The negative pressure wound healing assist
device removes fluid, including proteolytic enzymes responsible for
inhibiting tissue angiogenesis. Healing by secondary intention can be
prolonged in these patients. Soft tissue pedicled muscle or
fasciocutaneous transfer can be considered in recalcitrant cases.
uncommon, accounting for fewer than 5% of patients receiving a total
elbow replacement. Additionally, primary degenerative arthritis of the
elbow has been reported to affect less than 2% of the population. Males
are more commonly affected than females. Patients complain of pain on
terminal extension of the elbow and less frequently pain with flexion.
On occasion, patients may be bothered by pain that awakens them from
sleep or locking of the elbow during daytime activities. The dominant
extremity is involved in greater than 80% of patients with bilateral
involvement occurring in up to 60% of patients. Characteristically,
these patients lose terminal extension, but elbow flexion and forearm
rotation may also be limited. Routine elbow radiographs often reveal
osteophytes of the sigmoid notch of the ulna as well as osteophytes of
the coronoid process (Figure 13-6A). Loose bodies may also be present.
intra-articular corticosteroid injections. The time from symptoms onset
until surgery may be several years. Operative procedures include
arthroscopic joint debridement, ulnohumeral arthroplasty (Outerbridge
procedure), and total elbow arthroplasty. Relief of pain and modest
improvement in motion can be anticipated following arthroscopic
debridement. Long-term results of this procedure are not known.
Ulnohumeral arthroplasty is an open procedure where osteophytes are
debrided from the ulnar and humeral periarticular surfaces. Through a
posterior approach to the olecranon, a trephine is used to remove
osteophytes from the olecranon fossa. Also through this approach, the
anterior aspect of the distal humerus can be reached and osteophytes
removed. Pain relief can be expected in 90% of patients. Modest
improvements in flexion and extension can also be expected.
Approximately 20% of patients experience recurrence of symptoms at 10
years postoperative.
 |
|
FIGURE 13-6. (A) Primary degenerative arthritis of the elbow. (B) and (C) PA and lateral elbow films showing total elbow arthroplasty for degenerative arthritis of the elbow.
|
Patients with degenerative arthritis of the elbow joint are often
relatively young and active. The combination of youth and higher
activity level often makes the patient with degenerative arthritis of
the elbow a poor total elbow arthroplasty candidate. Limited
information exists on the treatment of primary degenerative arthritis
of the elbow. Only small series have been published on the results of
total elbow arthroplasty in these patients and a higher rate of
complication has been reported. The semiconstrained, nonhinged surface
replacement variety of total elbow arthroplasty may theoretically be
better suited for the degenerative elbow because hinged components are
at risk for loosening due to stress imparted at the bone cement
interface. Ligament incompetence seen in the RA patient precludes the
use of surface replacement components in these patients. However, the
degenerative elbow would be expected to have ligamentous and capsular
integrity as well as intact subchondral humeral and ulnar bone stock,
thereby making surface replacement an option. Long-term results of
surface replacement arthroplasty in the degenerative elbow, however,
are lacking.
frequently affects adolescent boys in which elbow articular cartilage
and underlying bone separates from the articular surface. It is more
common in males than females, is more common in the dominant arm, and
appears in both elbows in 15% of patients. The most common presenting
complaint is pain and limited motion. Osteochondritis dissecans (OCD)
is a common cause of “Little League elbow.” Physical examination finds
loss of elbow extension and tenderness over the lateral aspect of the
elbow. Irregular ossification of the capitellum, or a discrete crater,
can be seen on plain radiography that should include PA, lateral, and
oblique projections. Loose bodies may also develop and may be best
visualized with CT scan. The actual cause of the condition remains
unknown although trauma is believed to be an important factor as well
as possibly ischemia and genetics.
radiographic stability of the fragment. Intact lesions generally
respond to nonoperative management, including rest, splinting, and
NSAIDs. Partially detached or unstable lesions can be reattached in
situ, but the ultimate outcome is unknown. Completely detached lesions
are best treated with simple removal. The role of arthroscopic
debridement of remaining craters following removal of unstable or
detached lesions remains unknown, but some successes have been
reported. An association between OCDs and the development of
degenerative arthritis may exist. In the skeletally mature OCD patient
with advanced capitellar irregularities, radial head resection may be
an option for treatment.
Osteochondrosis is a growth disturbance involving a center of
ossification. The condition generally affects boys from the ages of 7
to 12 years, during the years of ossification of the capitellar
epiphysis. Patients usually present with a painful elbow, particularly
aggravated by throwing sports. Physical examination yields tenderness
over the lateral aspect of the elbow and limited motion of the elbow.
Radiographically, the capitellar epiphysis becomes fragmented in a
fashion similar to Perthes disease of the femoral head. In time as
growth progresses, the capitellar epiphysis reconstitutes. Treatment is
usually symptomatic as the symptoms and limitations of motion resolve.
of uncertain origin, although genetics is thought to play a role. The
prevalence of the condition is approximately 2%, affecting females
twice as commonly as males. Synovial biopsies of recently diagnosed
patients with RA show macrophages, T-cell and B-cell lymphocytes,
plasma cells, and polymorphonuclear lymphocytes. The resulting
inflammatory response invades normal tissue causing periarticular bony
erosions, cartilage destruction, and eventually joint destruction.
Patients generally experience pain and stiffness in multiple joints;
however, monoarticular involvement is recognized. Elbow involvement
affects approximately 50% of patients with RA. The hand and wrist are
the most commonly affected
joints.
Patients with RA affecting the elbow may experience loss of both
flexion and extension range of motion. Inspection of the posterior
surface of the elbow often finds loss of the normal bony contours due
to synovitis. This is perhaps most easily appreciated along the medial
border of the elbow, beneath the ulnar groove of the humerus or along
the lateral aspect of the elbow. Radiography will show periarticular
erosions as well as concentric cartilage shadow narrowing. The joint is
often warm to the touch during periods of active disease.
on the hand and wrist. Early nonoperative management can include a
corticosteroid injection, although relief of symptoms may be temporary.
It should also be remembered that the immunosuppressed status of these
patients puts them at a slightly increased risk of developing an
infection from a needle injection when compared to other patients.
Initial surgical management for RA affecting the elbow may include
synovectomy. Synovectomy combined with radial head excision is
indicated in patients with pain and stiffness following failure of
medical management. Radiographically, the ideal elbow synovectomy
candidate shows little if any alteration in subchondral architecture
despite cartilage shadow narrowing. Patients with gross deformity and
marked loss of motion are contraindicated for synovectomy. Elbow
synovectomy can be performed using an open technique or
arthroscopically. The later technique is demanding. Gendi et al.
has reported an 81% success rate at one year in 113 patients but noted
that this deteriorated over time with only 54% having pain relief at a
mean follow-up of 6½ years.
the patients with advanced, symptomatic RA of the elbow and are beyond
being considered for a synovectomy (Figure 13-7A-D).
These patients often seek medical attention due to constant pain and
profound functional limitations from compromised elbow motion. Surgery
is indicated in the patient older than 60 years who is relatively
inactive. These patients have failed medical management for their elbow
RA and understand that vigorous activity is not permitted once they
receive an elbow replacement. Contraindications include patients who
are mentally unstable or unreliable, patients with open elbow wounds,
or patients with prior or active elbow joint infection. Additionally
patients who are medically unstable or patients having current active
infections elsewhere are considered poor candidates for the procedure.
arthroplasty is the design most suitable for the RA patient. This
design does not rely on the capsuloligamentous structures nor
subchondral bone for elbow stability. In fact, generous portions of the
medial or lateral humeral condyles can be resected to facilitate
component placement, without compromising the overall result of the
elbow replacement surgery. The prosthesis lends immediate stability to
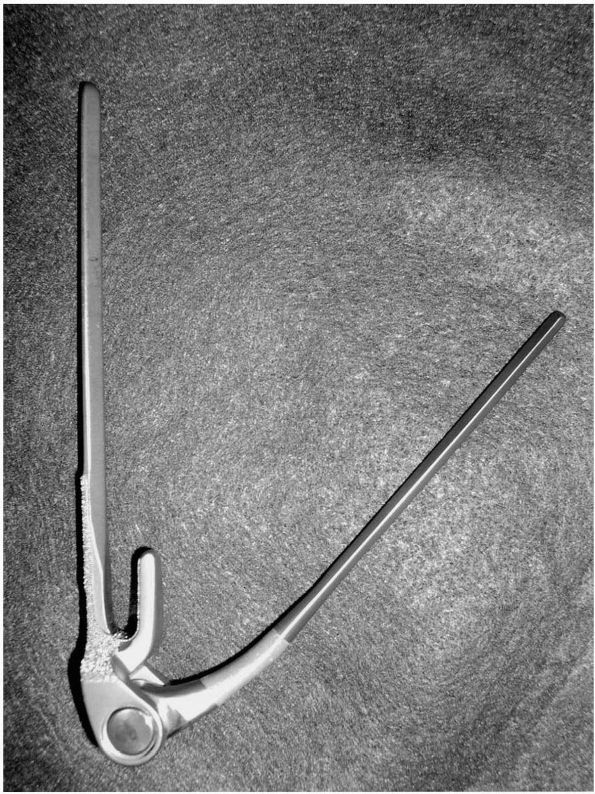
an otherwise unstable joint. Most constrained total elbow prosthetic
designs offer 5 to 10° of out-of-plane laxity of the ulnar component,
thereby unloading stress at the bone-cement interface. Otherwise,
stress at this location causes premature loosening and ultimate implant
failure. In one design, an anterior flange has been added to provide
rotational stability (Figure 13-8). The
procedure is performed through a triceps-sparing posterior approach
that facilitates early rehabilitation. Unlike other joint replacement
procedures, a major nerve must routinely be identified, mobilized, and
transferred to a new location. During the initial surgical exposure,
the ulnar nerve is identified, mobilized, and transposed anteriorly.
Immediately postoperative, the patients are placed in a sling and
encouraged to begin activities of daily living. Formal physical therapy
is not generally needed. The patients are instructed to never lift more
than 10 lbs with the operative elbow and to henceforth consider it a
“helper arm.”
population of 78 total elbow arthroplasties (TEA) at 10 years finding
that 97% are not painful and calculated a 92% survival with an 86%
having good or excellent results. Traditionally thought to have
infection rates of 7% or greater, the infection rate in this series was
2.6%. Ulnar neuritis is one of the more common postoperative problems.
In selected RA patients, TEA can be a life-altering procedure.
extensor pollicis brevis muscle (EPB)—the outcropper muscles of the
thumb—cross the extensor carpi radialis brevis (ECRB) and the extensor
carpi radialis longus (ECRL) in the distal forearm. At the point of
contact of these crossing structures, a bursa is present that may
become inflamed following repetitive wrist activities. This condition
is known as intersection syndrome of the forearm. Patients with
intersection syndrome of the forearm will complain of swelling and
acute pain with gripping and wrist extension. Also pain may be elicited
with isolated thumb movements. On physical examination, patients will
have point tenderness directly over the bursa and swelling will be
identified. In more advanced cases, warmth and erythema may be present.
Under certain circumstances, squeaking can be heard with wrist
movements.
 |
|
FIGURE 13-7. (A) and (B)
PA and lateral elbow film of patient with rheumatoid arthritis of the elbow. Notice concentric narrowing of the joint as well as osteopenia. (C) and (D) PA and lateral elbow film of total elbow arthroplasty for rheumatoid arthritis of the elbow. |
 |
|
FIGURE 13-8.
Coonrad-Morrey Total Elbow arthroplasty demonstrating the anterior flange of the humeral component, offering rotational stability. |
Generally, a specific activity can be identified that has incited the
condition. Restriction from this activity is the mainstay of initial
treatment. Patients also typically respond to static splinting of the
wrist in 15° for a period of 3 weeks combined with daily active, gentle
wrist range of motion exercises. NSAIDs, if tolerated, are included in
the nonoperative treatment regimen. A corticosteroid injection directly
into the intersection of tendons (approximately 4 cm proximal to the
radial styloid) can be performed if the condition proves refractory to
initial treatments.
failure of nonoperative treatment. The surgical approach is through a
longitudinal incision over the radial aspect of the dorsal surface of
the distal forearm. The APL and EPB tendons are elevated and the
underlying ECRB and ECRL are released from within their investing
fascia. Extensor tenosynovium is also debrided if identified.
Postoperatively, the wrist is splinted in extension and aggravating
activities are avoided for 4 weeks. After 4 weeks, patients resume
normal activities.
aspect of the elbow is often a result of the lateral epicondylitis.
This relatively common overuse injury may stem from a variety of
sporting activities that require repetitive use of the wrist and
forearm, or from occupational activities requiring similar movements.
The common age of onset is 35 to 50 years of age with an equal male to
female ratio. The common extensor origin consists of the tendons of
origin of the ECRB, ECRL, ECU, EDC, and EDQM. The pathologic process
begins with the microscopic disruption of the tendon fibers, which is a
degenerative process. Next, the tendon is invaded by fibroblasts,
vascular granulation tissue, and myofibroblasts. This degeneration and
repair process is termed angiofibroblastic hyperplasia.
The ordinary arrangement of the tendon fibers is disrupted. Of interest
is the absence of acute or chronic inflammatory tissues. Because of
this absence of inflammatory tissue, several authors have referred to
the condition as a “tendinosis” as opposed to “tendonitis.” The arcade
of Frohse is located just beneath the extensor carpi radialis brevis
(ECRB) tendon and radial tunnel syndrome may be associated with chronic
lateral epicondylitis.
functional limitations from lateral elbow pain. Patients complain of a
sharp pain localized to the lateral aspect of the elbow, exacerbated by
activities such as lifting, heavy gripping, or forearm supination and
pronation. Chronic conditions may find associated tenderness over the
arcade of Frohse, located two fingerbreadths distal to the lateral
epicondyle. This may indicate the presence of associated radial tunnel
syndrome, often confused with chronic lateral epicondylitis. Physical
examination may reveal one of several positive provocative maneuvers
for lateral epicondylitis. The resisted longer finger extension test is
the most commonly used test for
lateral
epicondylitis. Other tests include resisted wrist extension test and
the resisted supination test (also a test for associated radial tunnel
syndrome). Patients with long-standing symptoms may show a decrease in
grip strength.
nonoperative. Initial activity restriction is perhaps the most
effective, especially as it relates to racquet sports. For tennis
enthusiasts, careful evaluation of the size and weight of the racquet
should be evaluated and, most importantly, the the racquet’s string
pressure. A weight of 55 to 60 lb of pressure is preferred for most
amateurs. Greater string pressure may result in injury. Other issues
relate to proper tennis technique. For instance, greater reliance on
elbow and forearm motion to increase racquet speed (as opposed to more
proximal shoulder girdle muscles) may also result in injury. The
reliance on forearm and elbow motion for racquet speed is often caused
by deconditioned scapular stabilizer muscles, resulting in scapular
dyskinesis. Open chain shoulder rehabilitation is an effective means of
rehabilitating the tennis player following lateral epicondylitis. Other
rehabilitation includes forearm stretching exercises and gradual
strengthening. In the early phase, NSAIDs, wrist cock-up bracing, elbow
contour force bracing (Figure 13-9), and
steroid phonophoresis may prove beneficial for symptom relief. In most
instances, strict immobilization and repeated corticosteroid injections
are avoided. The use of corticosteroid injections in the absence of
inflammation seems counterintuitive. Some have suggested that the use
of corticosteroid on lateral epicondylitis may enhance the tendinosis
aspect of the condition.
 |
|
FIGURE 13-9. Counterforce bracing for the treatment of lateral epicondylitis.
|
refractory symptoms following a year of nonoperative management. Many
surgical options exist. The most popular choice is accomplished through
a longitudinal incision over the lateral epicondyle, exposing the ECRB
tendon of origin. Devitalized, degenerative tissue is excised from the
tendon. Incomplete tears of the ECRB tendon of origin occur in
approximately 35% of patients according to Nirschl.
advancement of the ECRB tendon versus release. Some feel that repair or
advancement of the ECRB tendon may predispose to recurrence due to
applied tension. Others have recommended release of the entire extensor
origin with drilling of the lateral epicondyle to promote healing. More
recently described alternative techniques include percutaneous and
arthroscopic extensor origin release.
epicondylitis. However, when necessary, debridement with or without
repair of the ECRB tendon provides a good alternative. In one study,
85.3% of patients obtained good or excellent results with open surgery.
Similar results have been reported with arthroscopic and percutaneous
techniques. Surgical treatment should be reserved for a select patients.
medial elbow pain. Approximately one-third of patients with medial
epicondylitis develop the condition subsequent to an injury. The medial
condyle of the humerus gives origin to the flexor-pronator origin,
including the pronator teres, the flexor carpi radialis, the humeral
head of the flexor ulnaris, the palmaris longus, and the ulnar head of
the flexor digitorum superficialis. The pronator teres and the flexor
carpi radialis share a conjoined tendon that is regarded as the primary
site of origin of this condition. With repetitive stress loading of
this conjoined tendon, degenerative changes occur in the tendon leading
to pain.
activity-related medial elbow pain. Patients are more commonly males,
presenting in the third through the fifth decades. In over one-half of
cases, patients complain of associated ulnar neuropathy. This most
likely relates to localized inflammation about the ulnar nerve or
direct compression from the bulk of the flexor-pronator tendinopathy.
Tenderness over the medial humeral condyle can be elicited on physical
examination. Pain with resistive forearm pronation is also variably
present. Elbow range of motion is usually preserved but grip strength
may wane.
nonoperative management including activity restrictions, NSAIDs, and
active hand therapy. A forearm splint with the wrist is slight
extension may also prove helpful. Counterforce proximal forearm straps
are variably effective. If immobilization is chosen, daily active and
passive range of motion exercises of the wrist and elbow are
encouraged. Corticosteroid injections to the medial epicondyle may
provide temporary relief of symptoms. Injections can, however, cause
subcutaneous fat atrophy and localized skin depigmentation. Medial
epicondylar injections are best preformed with the elbow extended in
order to avoid injection into a potentially subluxed or dislocated
ulnar nerve.
epicondylitis can be considered for surgery. Surgical options include
debridement, repair, and reattachment (if needed) of the
flexor-pronator tendon origin, or medial epicondylectomy. Flexor origin
debridement, and repair and reattachment, is performed through a
longitudinal incision over the medial epicondyle. Branches of the
medial antibrachial cutaneous nerve are identified and must be
carefully protected. Some authors recommend detachment of the
flexor-pronator origin with debridement of the devitalized portions of
the tendon followed by reattachment. Others recommend simple
debridement. Less clear is the optimal treatment for associated ulnar
neuropathy. Patients with mild associated ulnar neuropathy generally
respond to simple ulnar nerve decompression while more advanced cases
of ulnar neuropathy are best treated with anterior submuscular
transposition. Results from surgical treatment of medial epicondylitis
are highly favorable unless moderate or severe ulnar nerve symptoms
exist. In one study, patients with more advanced ulnar nerve symptoms
achieved good results in only 40% of cases.
SN, Morrey BF, Bianco AJ Jr. Chronic posterior subluxation and
dislocation of the radial head. J Bone Joint Surg 1991;73A:392-396. Thirty-four
chronic posterior elbow dislocations in 27 patients were reviewed.
Follow-up consisted of examining 18 of the patients, 10 of whom
received treatment and 8 of whom did not. The authors conclude that
posterior displacement did not cause serious functional impairment,
although loss of forearm rotation was found. Deformity was noted as a
cosmetic problem.
JE, Omer GE Jr. Congenital proximal radioulnar synostosis. Natural
history and functional assessment. J Bone Joint Surg 1985;67A:539-545. Thirty-six
proximal radioulnar synostoses were evaluated in 23 patients. The
patients were reevaluated at a mean age of 23 years and were found to
be fixed in a mean position of 30° pronation. The patients had few if
any functional complaints and the position of the forearm was not found
to affect employment status. The authors conclude that operative
treatment is rarely indicated in the treatment of congenital proximal
radioulnar synostosis.
on an experience of 47 patients, the authors evaluated their results
and recommend early corrective surgery for arthrogryposis multiplex
congenita of the hand and wrist. Included in their surgery are a
proximal row carpectomy, wrist tendon transfers, and triceps to radius
transfer to improve elbow flexion. The authors conclude that the
optimum age for surgery is 3 to 6 months of age.
article reviews the topic of radial head dislocations. The authors
conclude that in their experience, early open reduction and ligament
reconstruction offers advantages over late radial head resection.
AL, Chiu DTW. Cubital tunnel and radial tunnel syndromes. In: Trumble
TE, ed. Hand Surgery Update. 3rd Ed. Chicago: American Society for
Surgery of the Hand, 2003:313-323. This is an
update and review on the subjects of cubital tunnel syndrome and radial
tunnel syndrome. Included in the book are data on the results of
treatment from the authors’ practice. Using a Kaplan-Meier analysis,
they report an 80% improvement rate in patients treated nonoperatively
for mild ulnar neuropathy.
A, Andrews K, Lille S et al. The management of cubital tunnel syndrome:
a meta-analysis of clinical studies. Plast Reconstr Surg
2000;106:327-334. This analysis of previous
clinical series of cubital tunnel treatment reports that the success of
surgery is related to the initial degree of ulnar nerve compression.
The authors report that the best results for more advanced cubital
tunnel syndrome were found in patients who had anterior submuscular
transposition.
this study, the authors examine the anatomic relationships of the
cubital tunnel in 27 cadaver elbows. Variations in the anatomy of the
cubital tunnel at the elbow were classified into four types: type 0 =
no cubital tunnel retinaculum; type 1a = cubital tunnel retinaculum
taut in flexion; type 1b = cubital tunnel retinaculum was taut in a
position short of full elbow flexion; type 2 = the retinaculum was
replaced by an anomalous muscle, the anconeus epitrochlearis. The
authors conclude that the variations in cubital tunnel retinacular
anatomy may account for the development of ulnar neuropathy in some
patients.
authors review 39 limbs in 36 patients in which surgical decompression
of the median nerve was performed in the proximal forearm.
Electrodiagnostic testing was abnormal in 12 of the 37 patients who
received the studies. The nerve was found compressed at the flexor
digitorum superficialis in 22 arms and at the pronator teres in 13
arms. Overall 30 patients had partial or complete relief of their
symptoms.
a review of 42 patients surgically treated for radial tunnel syndrome,
37 were followed up at an average of 24 months. Seventy-four percent
had improvement following surgery but one-third still had symptoms.
Electrodiagnostic studies were not helpful in making the diagnosis.
Radial tunnel block was helpful in establishing diagnosis.
R. Entrapment and compression neuropathies. In: Green DP, Pedersen W,
Hotchkiss RN, eds. Operative Hand Surgery, 4th Ed. St. Louis: Churchill
Livingstone 1998;1417-1446. This is a
comprehensive review on the subject of compression neuropathies of the
forearm and elbow. Included are detailed discussions on pronator
syndrome, anterior interosseous nerve entrapment syndrome, ulnar
neuropathy, posterior interosseous nerve syndrome, and radial nerve
syndrome.
BF. Primary degenerative arthritis of the elbow. Treatment by
ulnohumeral arthroplasty. J Bone Joint Surg 1992;74B:409-413. Fifteen
patients were reviewed at an average of 33 months follow-up after
ulnohumeral arthroplasty. Fourteen of the 15 patients had good relief
of pain. Elbow extension and flexion had improved 11° and 10°
respectively. Overall, 87% of patients felt they had been improved by
the operation.
TE, Andrews JR, Satterwhite YE. The arthroscopic classification and
treatment of osteochondritis dissecans of the capitellum. Am J Sports
Med 1998;26:520-523. Seventeen elbows in 16
patients were evaluated with an average follow-up of 48 months. Each
patient underwent arthroscopic abrasion arthroplasty and removal of
loose bodies. The average flexion and extension contracture decreases
following treatment. Six of the 9 patients active in sports returned to
their preoperative level of activity. The authors conclude that
arthroscopic abrasion chondroplasty is an effective form of treatment
for osteochondritis dissecans.
NS, Axon JM, Carr AJ et al. Synovectomy of the elbow and radial head
excision in rheumatoid arthritis. Predictive factors and long-term
outcome. J Bone Joint Surg 1997;79B: 918-923. Synovectomy
with radial head resection was performed in 171 patients. Eighty-three
percent of the patients were satisfied at one year. These results
deteriorated with time at a rate of 2.6 % per year. Poor preoperative
elbow range of motion was a predictor of failure. The authors conclude
that the long-term results of this procedure are poor.
DR, Morrey BF. The Coonrad-Morrey total elbow arthroplasty in patients
who have rheumatoid arthritis. A ten- to fifteen-year follow-up study.
J Bone Joint Surg 1998;80A:1327-1335. Seventy-eight
original total elbow replacements in 69 patients were followed. At
follow-up 46 total elbow replacements in 41 patients were still alive
and had at least 10 years of follow-up. At follow-up, 97% of the elbows
were not painful. The mean arc of flexion and extension was 28 to 131°,
an improvement in 13° over preoperative. Complications included
infections, ulnar fractures, and triceps avulsion. Calculated survival
rate of the implanted prostheses was 92%. At final follow-up, 86% of
the patients had a good or excellent result.
GT, Morrey BF. Operative treatment of medial epicondylitis. Influence
of concomitant ulnar neuropathy at the elbow. J Bone Joint Surg
1995;77A:1065-1069. The results of operative
treatment of medial epicondylitis in 30 elbows were reviewed. At an
average of 7 years follow-up, debridement and ulnar nerve
decompression/transposition resulted in good or excellent results in
87% of patients. The patients that had moderate or advanced
preoperative ulnar neuropathy had a significantly worse surgical result.
basic anatomy and pathoanatomy of intersection syndrome is discussed.
Thirteen patients received operative treatment for the condition. The
authors conclude that the basic pathologic abnormality is stenosing
tenosynovitis of the radial wrist extensor tendons.
BS, Nirschl RP. Tendinosis of the elbow (tennis elbow). Clinical
features and findings of histological, immunohistochemical, and
electron microscopy studies. J Bone Joint Surg 1999;81A:259-278.
1,213 elbows with lateral epicondylitis treated nonoperatively, seven
percent failed and underwent operative treatment. At the time of
surgery, 93% of the elbows (82 of the 88 operatively treated patients)
were observed to have gross involvement of the ECRB tendon of origin.
Seventy-five of the 88 operatively treated patients obtained good or
excellent results with tendon debridement and ECRB repair.
