Tenosynovitis Epicondylitis
entities in the fingers, thumb, and wrist (stenosing tenosynovitis), as
well as medial and lateral epicondylitis of the elbow.
wrist, is commonly seen on a Hand and Upper Extremity Service and is
appropriately included in this text on the hand and wrist.
classified as inflammatory conditions that involve the respective
tendon sheaths and retinacular structures.
of the channel through which the respective tendons travel is the
common denominator in these conditions. There may not be agreement as
to the relative role of tendon, retinacular, or synovial tissues in
causing this narrowing, but perhaps all three play varying roles. The
fact that the problem may be relieved by rest, medication, or surgery
indicates that stenosis is a valid concept when discussing this
disorder.
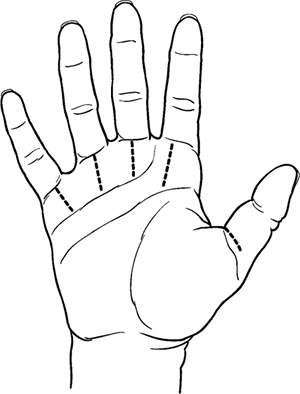
metacarpophalangeal (MCP) joint palmar plate and, to a lesser extent,
from the base of the proximal phalanx. It is located in the distal palm
and not the finger. In the thumb, the A1 pulley arises from the MCP
joint palmar plate and, to a lesser extent, from the base of the
proximal phalanx.
-
This condition is more common in women, with the peak incidence at 40 to 60 years of age.
-
The ring finger is most commonly involved, followed by the thumb and middle finger.
-
Single or multiple digits may be involved.
-
Patients give a history of a “clicking” sensation with motion of the affected finger or thumb.
-
Sometimes a “lump” is described in the palm, and anatomically this lump corresponds to the A1 pulley.
-
The clicking may progress to “locking” of the digit.
-
This “locking” is in the flexed position. Attempts at extension of the digit are often painful.
-
The locked position in a trigger digit is with both the MCP and proximal interphalangeal (PIP) joint flexed.
-
Sometimes the patient must use the other hand to passively extend, or “unlock,” the digit.
-
-
Repetitive use or overuse of the hand may be associated with the onset of the condition.
-
Commonly associated conditions are rheumatoid arthritis, diabetes mellitus, and gout.
-
Other reported causes of trigger digit
include localized enlargement of the flexor digitorum profundus (FDP)
in the region of the A3 pulley. In patients with rheumatoid arthritis,
the triggering may be due to proliferative synovium about the profundus
tendon and subsequent trapping at the flexor digitorum superficialis
(FDS) decussation. -
Stenosing tenosynovitis does not usually result in a fixed or permanently locked position.
-
If a “trigger finger” cannot be passively
extended, it is probable that true locking of the finger is present due
to a cause such as a spur from the metacarpal that is trapped in a
small fenestration in the palmar plate. -
The posture of true locking is with
varying degrees of flexion at the MCP joint, whereas the PIP joint is
in full extension and actively and passively mobile. -
The locked trigger finger is in a flexed posture at both the PIP and MCP joints (Figure 6-2).
-
-
In early or mild cases, crepitation with
flexion of the digit and tenderness over the region of the A1 pulley
may be the most prominent findings. -
As the condition progresses, definite locking and catching may occur. This is usually painful.P.89
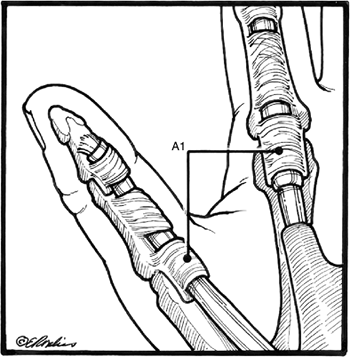 Figure 6-1 The arrangement of the finger and thumb flexor tendon sheath and pulleys.
Figure 6-1 The arrangement of the finger and thumb flexor tendon sheath and pulleys. -
The patient may become apprehensive when
asked to flex the finger, because the locking and release of the locked
digit are painful.
-
Conservative management in the form of
rest to the hand, splinting, and anti-inflammatory medication may be of
benefit in mild or early cases.![]() Figure 6-2 The clinical appearance of a typical “locked” trigger finger. Note that flexion is present in the MCP, PIP, and DIP joints.
Figure 6-2 The clinical appearance of a typical “locked” trigger finger. Note that flexion is present in the MCP, PIP, and DIP joints. -
The next level of treatment includes a steroid injection into the flexor sheath.
-
One injection (or a second 2 weeks later) may result in relief.
-
Patients with a discrete palpable nodule,
single digit involvement, and a short duration of symptoms appear to
have the best response to injections.
-
The site to be injected is prepped with
Betadine or a similar solution, and the skin at the injection site is
anesthetized with ethyl chloride spray. -
A short, 25-gauge needle attached to a
1-mL syringe with 0.5 mL of corticosteroid designed for intrasynovial
use (Kenalog-40 or similar agent) is introduced through the skin and
into the proximal synovial sheath. -
The ideal injection site is just proximal to the A1 pulley into the synovial sheath.
-
Entering at a slight angle aids in placement of the needle.
-
Marked resistance indicates that the
needle may be in the substance of the tendon, and the needle should be
withdrawn slightly or repositioned.
-
-
As the steroid is injected into the
sheath, the filling of the sheath may be palpated by the injector’s
finger positioned over the proximal or middle phalanx. -
Serial injections in the anatomy
laboratory by the author have demonstrated that a fluid volume of 0.5
mL is more than sufficient to fill the sheath in most digits. -
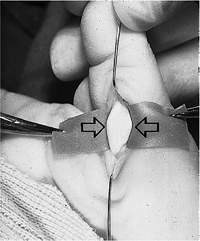
Figure 6-3 shows the injection technique.
-
The goal of surgical treatment is to incise (release) the first annular pulley through a transverse or longitudinal incision.
-
In general, the incisions should not cross a palmar or digital flexion crease at right angles.
-
Some suitable longitudinal incisions for the fingers and the recommended transverse thumb incision are depicted in Figure 6-4.
-
My preference for longitudinal finger
incisions is based on the ease of exposure. The line of incision
parallels the underlying tendons, nerves, and blood vessels (they are
less likely to be injured), and is oriented in a more suitable plane to
facilitate postoperative exercises. -
The proximal part of the incision over the middle finger is angled slightly, to parallel the distal palmar flexion crease.
-
Four digits may be released simultaneously with these incisions without compromise to the skin.
-
The soft tissues are retracted with two
vein retractors that protect the neurovascular bundles. The A1 pulley
is incised with a no. 15 blade under direct vision.P.90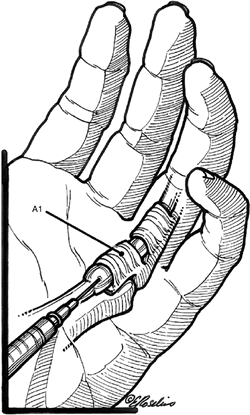 Figure 6-3 Injection technique for trigger fingers.
Figure 6-3 Injection technique for trigger fingers. -
All of the A1 pulley is incised and, if necessary, so are a few millimeters of the proximal portion of the A2 pulley.
-
The flexor tendons may be pulled up into
the wound to verify complete release. In the thumb, the radial digital
sensory nerve crosses the flexor pollicis longus (FPL) sheath from
ulnar to radial at or proximal to the A1 pulley and must be identified
and protected. -
The A1 pulley is incised, but the oblique pulley is preserved.
-
Percutaneous release has been developed
for trigger finger release and, in experienced, operators may be a
useful adjunct to the open technique.
-
These children are usually brought to the
pediatrician or other caregiver when the family notes that the thumb
interphalangeal (IP) joint is in a flexed posture and cannot be
passively extended. -
The child presents with a locked IP joint that cannot be actively or passively extended.
-
A prominent but nontender nodule is noted
in the region of the palmar aspect of the thumb MCP joint. It may be
bilateral in 25% to 33% of patients diagnosed. -
The wise practitioner will not attempt to
passively extend the IP joint with undue force, because such a maneuver
may be painful. -
The diagnosis is usually made by the clinical appearance and physical findings.
-
Other diagnoses may be considered, such as congenital clasped thumb, absent extensor tendons, arthrogryposis, or spasticity.
-
Figure 6-5 shows the clinical appearance of bilateral congenital trigger thumbs.
reported in some series with or without conservative treatment, such as
splinting, massage, and passive extension exercises to the IP joint. It
is unknown how many of these thumbs spontaneously resolve without ever
being diagnosed. Conservative treatment may be tried based on the
perceived needs of the family and the age of the child. Little or no
harm will result from delaying the trigger thumb release should it be
required.
-
The first annular pulley is incised through a transverse incision that is centered over the nodule.
-
The neurovascular bundles are close by and must be protected.
-
In contrast to the adult trigger thumb, the FPL tendon has a prominent nodule (Notta’s node).
-
This nodule is not excised because it will resolve following release of the first annular pulley (Figure 6-6).
-
Trigger fingers in children are much less common than trigger thumbs.
-
Pathologic findings may include a nodule in the FDP and FDS, and a bunching up or buckling of one or more slips of the FDS.
-
In contrast to congenital trigger thumb
release, release of the first annular pulley in congenital trigger
finger may be inadequate. -
The incision should be extensile, because
correction, in addition to release of the A1 pulley, may require
excision of tendon nodules, one or both slips of the FDS, and release
of the A3 pulley. -
A Bruner zigzag incision is useful for this more comprehensive exposure.
 |
|
Figure 6-4
Suitable longitudinal incisions for trigger finger release, and the recommended transverse incision for release of the thumb A1 pulley. |
 |
|
Figure 6-5 Bilateral congenital trigger thumbs in a child. Note the flexed posture of the interphalangeal joints of the thumbs.
|
 |
|
Figure 6-6 Congenital trigger thumb. Intraoperative photo showing release of the first annular pulley, and the prominent nodule (arrows) in the FPL called Notta’s node.
|
 |
|
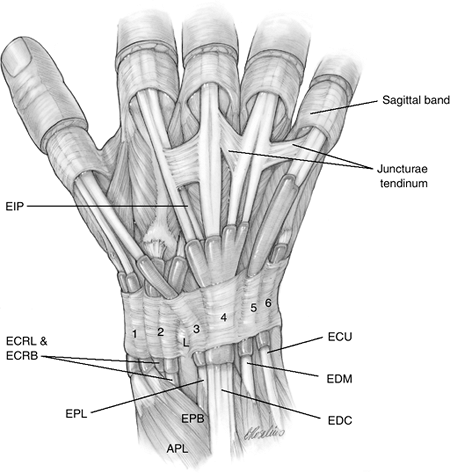
Figure 6-7 The six dorsal extensor compartments.
|
The wrist, thumb, and finger extensor tendons enter the hand beneath a
fibrous tissue retinaculum that contains six tunnels. Five of these
tunnels are fibroosseous and one (the fifth) is fibrous. This extensor
retinaculum (ER) is a wide fibrous tissue band that prevents
bowstringing of the tendons and improves their mechanical advantage. At
this level, the extensor tendons are covered by a synovial sheath. The
ER has two distinct layers: the supratendinous layer and the
infratendinous one. The latter is limited to the area deep to the ulnar
three compartments.
variable in their number of slips and tunnels. The APL may have two,
and up to four, tendon slips, whereas the EPB usually has only one and
may be absent in 5% to 7% of cases. Anatomic studies have revealed that
the first compartment may consist of two distinct compartments in as
many as 33% of patients. These two tunnels are an ulnar tunnel for the
EPB, and a more radial one for the abductor pollicis longus (APL). Even
a third tunnel containing an anomalous tendon has been reported.
Failure to recognize these variations may lead to treatment failure (Figure 6-8).
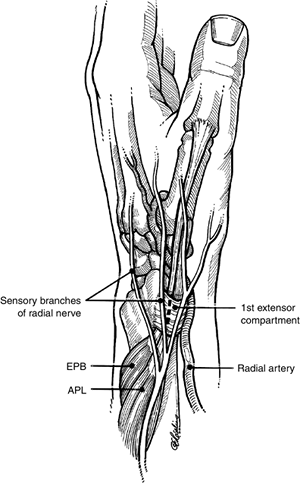
to this region must be recognized to prevent injury to these structures
(see Figure 6-8). The radial artery passes obliquely across the anatomical snuff box from the palmar aspect of the wrist deep
to the APL and the radial wrist extensors (extensor carpi radialis
longus [ECRL] and extensor carpi radialis brevis [ECRB]). Two or more
sensory branches of the radial nerve are immediately superficial to the first extensor compartment.
-
A history of radial-sided wrist pain of
variable duration may be identified, in association with overuse of the
wrist and thumb. The condition may be associated with diabetes or
pregnancy. -
There is tenderness over the first
extensor compartment, and there may be swelling and redness over the
region of the radial styloid. -
Flexion and extension of the thumb is usually painful, and crepitation may be noted.
-
Finkelstein’s test is pathognomonic and is properly performed as described.
-
The thumb is grasped by the examiner, and the hand is quickly abducted (bent ulnarward).
-
The test is inappropriately performed by placing the thumb in the palm before wrist abduction, because this may produce pain even in a normal wrist (Figure 6-9).
-
A positive test is manifested by pain over the radial styloid due to stretching of the inflamed tendons.
P.93![]() Figure 6-8
Figure 6-8
Relevant anatomy for de Quervain’s tenosynovitis. The APL and EPB
ordinarily share a common fibroosseous canal, but in 33% of cases a
separate canal may be present that contains the EPB. Failure to
recognize and release this second compartment will result in an
incomplete release. Note the relationship of the radial artery and
radial nerve to the first extensor compartment. -
-
De Quervain’s tenosynovitis must be distinguished from arthritis of the trapeziometacarpal joint of the thumb.
-
Tenderness and swelling over this joint, along with pain and crepitation, are signs of arthritis.
-
This arthritic condition may co-exist with de Quervain’s tenosynovitis.
-
-
Rest to the thumb and wrist by means of a
splint that immobilizes both, along with anti-inflammatory medication,
may be useful in mild cases. -
If these simple measures are not successful, a steroid injection into the first extensor compartment should be considered.
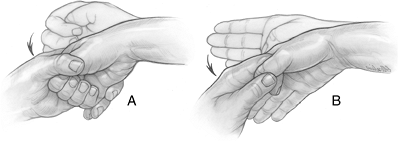 Figure 6-9 Finkelstein’s test. (A) The incorrect technique. (B)
Figure 6-9 Finkelstein’s test. (A) The incorrect technique. (B)
The correct technique. The test is appropriately performed by grasping
the patient’s thumb, and then ulnar deviating the hand. A
false-positive test may result if the thumb is flexed into the palm and
grasped by the patient’s fingers followed by ulnar deviation of the
wrist (see text).-
This is performed under sterile techniques and local anesthesia (1% Xylocaine without epinephrine).
-
Ethyl chloride spray is a suitable alternative to temporarily anesthetize the skin.
-
-
An intrasynovial steroid injection is placed into the first compartment using a short 25- or 27-gauge needle.
-
The injection site is about 1 cm proximal to the tip of the radial styloid.
-
The needle is guided by palpation of the
tendons in the first compartment. Needle placement may be verified by
noting enlargement of the sheath with instillation of the cortisone. -
The injection may be repeated in 4 to 6 weeks if symptoms are not relieved.
-
Water-soluble steroid preparations in
volumes of 1 mL or less are preferred. Informed consent prior to the
injection includes the possibility of depigmentation of the skin and
atrophy of the subcutaneous fat.
-
If conservative treatment fails, surgery by release of the first extensor compartment is performed.
-
A 2 cm transverse incision is made about 1 cm proximal to the tip of the radial styloid.
-
Branches of the radial sensory nerve are identified and carefully retracted.
-
The retinaculum is incised
longitudinally, all compartments released, and the respective tendons
are gently lifted from the wound to verify complete release. -
Traction on one of the unroofed tendons must result in extension of the MCP joint, indicating release of the EPB tendon.
-
If this does not occur, then a second compartment must be searched for and released.
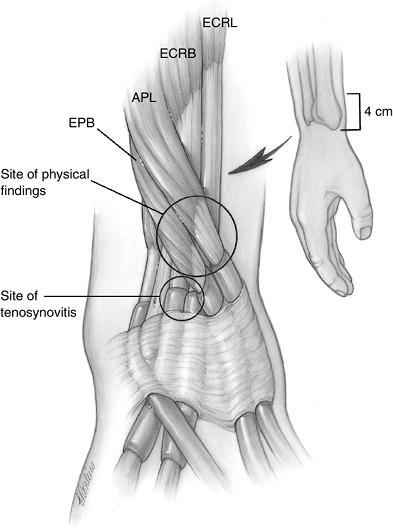
dorsal compartment. The APL and EPB muscle bellies cross over the
tendons of the ECRL and ECRB, and this is the
site
of physical findings. The pathology, however, is located distally in
the synovial sheath of the second compartment. The ECRL and ECRB are
encased in a tight compartment, and the symptoms and the physical
findings of swelling and tenderness do not present at this site. Rather
they present about 4 cm proximal to the radial styloid. Surgical
release of the second compartment distal to the area of symptoms and
findings reveal characteristic synovitis (Figure 6-10).
 |
|
Figure 6-10
Intersection syndrome. Although the symptoms of swelling and tenderness present in the crossover area 4 cm proximal to the radial styloid, the true pathology is distal in the second extensor compartment. |
-
Pain and swelling about the muscle
bellies of the APL and EPB at the dorsal and radial aspect of the wrist
are characteristic of this syndrome. -
This area is about 4 cm proximal to the radial styloid.
-
It may be seen after overuse of the wrist, and is often associated with sports activities such as rowing or weight lifting.
-
If conservative measures including
splinting and/or steroid injections into the second compartment fail,
then surgical release of the second dorsal compartment is performed
through an incision centered over the radial wrist extensors (ECRL and
ECRB). -
The extensor pollicis longus (EPL) tendon
and sensory branches of the radial nerve are in the area and are
identified and protected.
relatively small (8 to 10 mm wide) fourth compartment when the wrist is
flexed. This produces relative occlusion or compromise of the already
limited space. Hypertrophy of this muscle, or synovitis of the
surrounding tendon sheath, may be implicated.
-
This condition may manifest itself as
swelling and tenderness in the radial side of the fourth extensor
compartment, which is most noticeable in wrist flexion. -
With the wrist in full flexion, the patient is asked to extend the index finger against resistance.
-
The production of pain that is adjacent to Lister’s tubercle represents a positive test for EIP syndrome.
-
Partial release of the extensor
retinaculum or partial excision of a hypertrophied EIP muscle belly may
be indicated if conservative measures fail.
extensor compartment. Its movement is through a relatively long osseous
groove and Lister’s tubercle acts as a “turning fairlead” to change its
initial course that is parallel to the long axis of the forearm to an
oblique axis to reach the thumb. Any condition that compromises the
osseous groove or inflames the surrounding synovial sheath will result
in pain, swelling, and tenderness.
-
EPL tenosynovitis is often seen following
a Colles fracture, and its tendency to rupture may be related to local
ischemia in an unyielding fibro-osseous groove. -
Tenderness, swelling, and crepitation may be noted along the course of the tendon.
-
Attritional rupture of the EPL may occur in these circumstances, and steroid injections are not advised.
-
Re-routing of the tendon radial to its anatomic tunnel is recommended.
-
Release of calcium salts into the synovial and peritendinous space results in acute pain, swelling, redness, and tenderness.
-
The onset is sudden and is not usually associated with a precipitating incident.
-
The redness and swelling may mimic infection.
-
Gouty tenosynovitis may present in a similar fashion and may be diagnosed by history or laboratory studies.
-
A high index of suspicion and a radiograph more often than not lead to the diagnosis of acute calcific tendonitis.
-
The lesions may occur anywhere in the
hand or wrist, and the region of the flexor carpi ulnaris (FCU) and
pisiform bone is the most common site (Figure 6-11).
-
This condition is usually self-limited and may resolve in a matter of days.
-
Symptomatic treatment is indicated in the form of splints, mild anodynes, and anti-inflammatories as needed.
the ECRB muscle and its fibrous tissue origins from the lateral
epicondyle. It arises from the common extensor origin from the lateral
epicondyle, radial collateral ligament of the elbow joint, and the
intermuscular septum. Various entities have been implicated, and
include such conditions as an inflamed synovial fringe, fibrositis of
the annular ligament around the radial head and neck, periostitis of
the ECRB origin, and angiofibroblastic hyperplasia of the ECRB tendon
of origin. Most now agree that some form of noninflammatory
degeneration of the ECRB tendon is responsible, because acute
inflammatory cells are not often present in the specimens removed.
edematous ECRB origin and rupture of portions of the ECRB origin in
about one-third of the patients treated. Specialized stains of these
abnormal tissues have demonstrated myofibroblast cells that are not
normally found in tendons.
 |
|
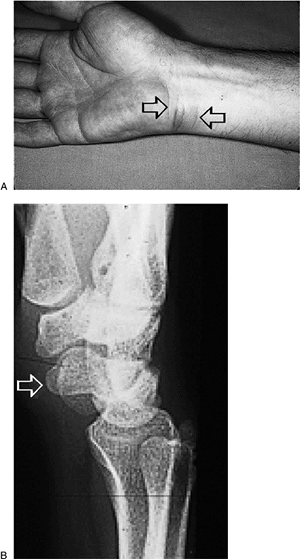
Figure 6-11 Acute calcific tendonitis. (A) This young reporter noted the sudden onset of pain, swelling, and redness on the flexor aspect of his wrist (arrows). (B) Radiographs demonstrated a calcium deposit in the region of the FCU tendon and pisiform bone (arrow).
|
-
Patients with this condition present with
the insidious onset of pain on the outer aspect of the elbow that may
radiate into the extensor surface of the forearm. -
Racket sports have been implicated, especially in those that play often or have faulty technique.
-
Repetitive use of the wrist and finger
extensor muscles is often noted. Swelling is not a usual feature, but
point tenderness over the lateral epicondyle and the tendon of origin
of the ECRB is present. -
Symptoms are reproduced by resisted dorsiflexion of the wrist with the elbow extended.
-
Differential diagnosis may include
cervical disc disease, radial tunnel syndrome, posterior interosseous
nerve syndrome, radiocapitellar arthritis, or osteochondral injury. -
Radiographs should be obtained to rule out bone pathology.
-
Initial treatment is conservative in the form of activity modification, rehabilitation exercises, ice, and anti-inflammatories.
-
Some patients will benefit from a
so-called tennis elbow brace that applies pressure to the extensor
tendon origin on the proximal forearm. -
Steroid injection, directed to the osseous origin of the ECRB tendon, may be beneficial.
-
Surgery is indicated for those patients
that have failed to improve after several months of conservative
treatment, and who, for a variety of reasons, cannot or chose not to
live with the condition. -
Most current surgical approaches to this
problem are extra-articular, and consist of debridement of the abnormal
tissue on the deep or underside of the ECRB and adjacent tendons. -
In open techniques, the interval between the ECRL and ECRB is exposed through a lateral incision.
-
Diseased tissue is removed from the ECRB after detaching it from its epicondylar origin.
-
Other sites of diseased tissue are looked for and removed from the ECRL or common extensor origin.
-
Reattachment of these tendons is facilitated by roughening of the adjacent bone or by mini-epicondylectomy.
-
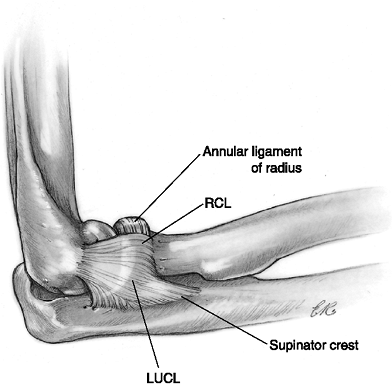
The collateral ligament is protected
during the procedure to avoid the postoperative complication of
posterolateral rotatory instability of the elbow (Figure 6-12). -
Arthroscopic debridement of the ECRB has also shown favorable results.
medial epicondyle and supracondylar ridge, and include the pronator
teres (PT), flexor carpi radialis (FCR), palmaris longus (PL), flexor
digitorum superficialis (FDS), and the FCU. The PT (humeral head) and
FCR share a common tendon origin from the epicondylar ridge, and are
the usual muscles involved. The anterior elements of the medial
collateral ligament (A-MCL) are the major ligamentous stabilizers of
the medial aspect of the elbow, and must be protected during any
surgical releases in this area. The A-MCL originates from the inferior
and anterior aspect of the medial epicondyle (Figure 6-13).
 |
|
Figure 6-12 The lateral elbow ligaments. LUCL, lateral ulnar collateral ligament; RCL, radial collateral ligament.
|
-
Medial epicondylitis is the most common cause of medial elbow pain, but it is much less common than lateral epicondylitis.
-
The onset, like lateral epicondylitis, is insidious in the majority of cases.
-
The patients often describe
activity-related pain associated with repetitive and forceful forearm
pronation and/or wrist flexion. -
Many cases are associated with occupational activities.
-
Sports-related activities such as throwing and golfing are often associated with this condition.
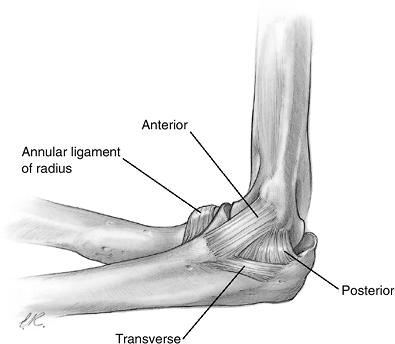 Figure 6-13 The medial elbow ligaments.
Figure 6-13 The medial elbow ligaments. -
The sites of maximum tenderness are over
the medial epicondyle and just distal at the tendinous origin of the
flexor-pronator muscles. -
Resisted pronation and wrist flexion often reproduce the symptoms.
-
Symptoms of cubital tunnel syndrome may
also be present, and are manifested by tenderness and a positive
Tinel’s sign over the ulnar nerve in the cubital tunnel. -
Additional differential diagnostic
entities include ulnar nerve subluxation, subluxing medial head of the
triceps, medial collateral ligament insufficiency (especially in
throwers), elbow arthritis, and cervical radiculitis.
-
Conservative treatment is represented by activity modification, ice, and anti-inflammatory medication.
-
A steroid injection deep to the site of the origin of the flexor-pronator group may also be tried.
-
If symptoms resolve in a timely fashion, flexor-pronator stretching exercises are performed.
-
Surgery is indicated for those patients
that have failed to improve after several months of conservative
treatment, and who, for a variety of reasons, cannot or chose not to
live with the condition. -
The commonly recommended treatment is
debridement and reattachment of the flexor-pronator origin through an
incision just anterior to the medial epicondyle. -
A small cuff of tissue may be left proximally to facilitate reattachment.
-
Pathological tissue on the underside of the PT or FCR, or elsewhere in the flexor-pronator origin, is excised.
-
Some surgeons perform a limited epicondylectomy to facilitate reattachment of the flexor-pronator muscles.
-
The ulnar nerve in the cubital tunnel,
and the branches of the medial antebrachial cutaneous nerve, must be
identified and preserved during the procedure.
CL Jr, Murphy KP, Gottlob CA, Curd DT. Arthroscopic classification and
treatment of lateral epicondylitis: two-year clinical results. J
Shoulder Elbow Surg 2000;9:475–482.
J, Stern PJ, Von Kuster LC. Transection of radial digital nerve of the
thumb during trigger release. J Hand Surg 1989;14A:198–200.
JR. The Elbow. In: Doyle JR, Botte MJ, Surgical anatomy of the hand and
upper extremity. Philadelphia: Lippincott, Williams & Wilkins:
2002:371–402.
JR. Palmar Hand. In: Doyle JR, Botte MJ, Surgical anatomy of the hand
and upper extremity. Philadelphia: Lippincott, Williams & Wilkins:
2002:532–641.
GT, Morrey BF. Operative treatment of medial epicondylitis: influence
of concomitant ulnar neuropathy at the elbow. J Bone Joint Surg
1995;77A:1065.
DS, Sotereanos DG. Tenosynovitis, de Quervain’s syndrome and
epicondylitis, In: Trumble, TE, ed. Hand surgery update-3, hand, elbow,
shoulder. Rosemont, IL: American Society for Surgery of the Hand,
2003:271–284.
S. Tenosynovitis. In: Green DP, Hotchkiss RN, Pederson WC, eds. Green’s
operative hand surgery. 4th Ed. New York: Churchill Livingstone,
1999:2022–2044.