SURGICAL TREATMENT OF ADULT SCOLIOSIS
VIII – THE SPINE > Spinal Deformity > CHAPTER 159 – SURGICAL
TREATMENT OF ADULT SCOLIOSIS
adolescent idiopathic curve. It may also develop secondary to
progressive degenerative collapse or neuromuscular disease. It may,
rarely, be attributable to a progressive idiopathic curve arising after
skeletal maturity, in which the curves tend to be more rigid than those
seen in adolescence.
problems (pain, neurologic signs and symptoms, progression of
deformity, and cosmetic concerns). Postsurgical complications are more
common, more severe, and less well tolerated than in younger patients.
Even though advances in diagnostic modalities and surgical technique
provide for more effective treatment options than in the past, the
treatment of adult scoliosis remains one of the most complex and
challenging disorders confronting the spinal surgeon.
progress past skeletal maturity. It is now well documented that large
curves continue to progress into adulthood. Curves less than 30° at the
end of growth rarely progress and do not need close observation, but as
Weinstein and Ponseti have shown, curves measuring greater than 50° at
skeletal maturity are at significant risk for progression (28). Thoracic curves are even more likely to progress than lumbar curves.
asymmetric disc space collapse is distinct from adolescent and adult
idiopathic scoliosis. The degenerative scoliosis is commonly a lumbar
curve of moderate severity characterized by less rotation at the apex
and more lateral listhesis
between adjacent segments. Degenerative scoliosis is discussed more fully in Chapter 160.
scoliosis. The pain tends to be mechanical in nature, worse in the
morning and late evening, exacerbated by strenuous activity and certain
bending or twisting activities, and characterized by limited sitting
tolerance. Pain along the convexity of the curve can also be due to
muscle fatigue or scapulothoracic incongruency. With advancing age and
curve severity, the pain tends to concentrate in the concavity of the
curve. Focal back pain across the concavity may be due to disc
degeneration, facet arthrosis, junctional disc degeneration, or
segmental instability (30).
of disc degeneration as seen in normal spines, but eccentric loads may
accelerate the degenerative process. Distortion of the outer annulus or
posterior longitudinal ligament could generate back pain localized to
the site of highest compressive load. The degenerating disc may release
pain mediators that sensitize local receptors or the nerve root itself.
The asymmetrically loaded facet joints could also be the source of pain
in some patients.
convexity of the curve can stimulate capsular receptors capable of
generating pain. Painful degeneration of the junctional disc may occur
at the end of a rigid structural segment, within a flexible
compensatory curve, or between opposing curves. In these areas,
exaggerated bending forces tend to break down normal restraints and
produce instability that may eventually result in coronal or sagittal
displacements, abnormal motion, or axial and radicular pain. Radicular
pain usually occurs on the concavity of lumbar or thoracolumbar curves,
where nerve root compression in the lateral recess or foramen is caused
by facet arthrosis and hypertrophy, disc herniation, or a combination
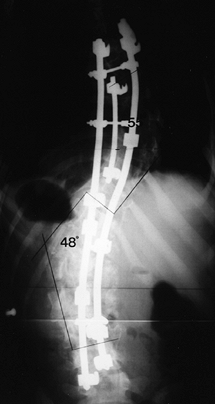
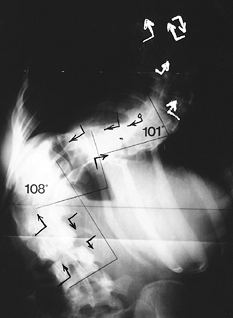
of the two (Fig. 159.1). Radicular symptoms may
also occur on the convexity when traction and kinking of the nerve root
occur as it passes around the pedicle and out of the foramen.
 |
|
Figure 159.1.
A 55-year-old woman with a large lumbar curve that was not progressing. She developed radicular pain in her lower left extremity that markedly limited her walking and standing tolerance. Back pain had not changed for years. Myelogram (A) and postmyelographic (B) CT scan demonstrated nonfilling of left L-5 nerve root and displacement of left S-1 nerve root secondary to facet hypertrophy and subarticular and foraminal stenosis. Limited decompression consisting of left hemilaminotomy, partial medial facetectomy, and internal foraminotomy provided relief of lower extremity radicular pain. The curve has not progressed in over 1 year since surgery. |
complaint. Patients may complain of a loss of height, an increase in
rib prominence, or changes in shoulder or waistline symmetry. In
general, scoliosis in the adult progresses slowly, in the range of 1°
per year (28). More rapid changes in posture may signal a more complex underlying
disorder (i.e., metabolic bone disease, associated neurologic
disorders, unrecognized congenital abnormalities) or may simply mean
that the patient is losing the ability to compensate for the
longstanding deformity.
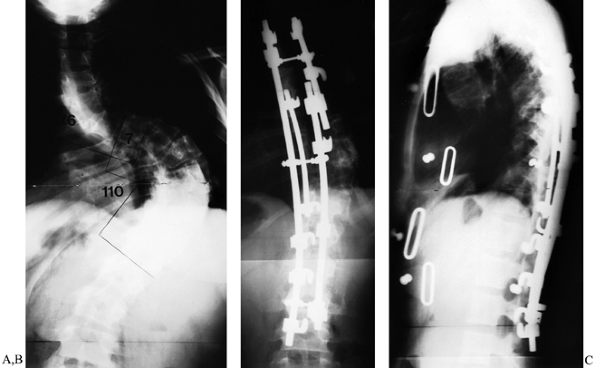
progressive adult scoliotic spine acts more like a leaning tower of
Pisa, in that the rigid spine cannot compensate for curve progression
to maintain sagittal or coronal balance. Since the primary curve
(thoracic, thoracolumbar, or lumbar) becomes rigid early in the curve’s
development, it can no longer compensate in the sagittal or coronal
plane as the compensatory curve progresses and eventually becomes
structural. Frequently, the patient notices progression of coronal and
sagittal imbalance as he or she falls farther and farther to one side (Fig. 159.2).
 |
|
Figure 159.2. Progression and decompensation. A:
Adult patient with longstanding thoracic curve. The curve is rigid but well balanced in coronal plane. The lumbar compensatory curve is low-grade and supple. B: Over time, the lumbar compensatory curve progresses. The ability of the spinal column to compensate is limited by the rigid thoracic curve. Degenerative changes, superimposed on the secondary curve, accelerate the curves’ progression. C: When the limits of spinal compensation are reached, the progressive lumbar curve begins to throw the thoracic curve out of coronal balance. The patient begins to lean or collapse to one side. Decompensation progresses rapidly because of the mechanical disadvantage, and the apparent deformity becomes dramatically worse in a short time. D: The final compensatory mechanism is postural; the patient stands with the left hip flexed and shoulders askew, trying to balance the head over the pelvis. |
treatment, but many patients are reluctant to raise this issue with
their doctors. Rib prominence, changes in the waistline, and lateral
postural imbalance all contribute to an undesirable appearance. While
the cosmetic aspects of spinal deformity are often downplayed by
physicians, they are often extremely important to the patient and
should be carefully considered in formulating a treatment plan.
scoliosis but is rarely the main reason the patient seeks treatment.
Large thoracic curves (greater than 100°) may cause restrictive
pulmonary disease, particularly when the chest is hypokyphotic (3).
Although most patients with large curves have pain as their major
complaint, the presence of deteriorating pulmonary function is an
additional indication for surgical intervention. Key features of
cardiopulmonary involvement include
-
Measurable losses in pulmonary function
that are first noted in curves greater than 60°; significant impairment
occurs where curves exceed 100°; -
Direct correlation between curve magnitude and loss of pulmonary capacity;
-
Complaints of fatigue and shortness of breath with minor exertion;
-
Neuromuscular disease that can amplify pulmonary compromise.
cord compression with myelopathy has not been reported in idiopathic
scoliosis. Occasionally, patients may have activity-related deficits
due to central stenosis. These deficits usually occur in older
patients, where degenerative changes have set in on top of the original
deformity. Lateral or sagittal translation can cause rapid progression
of stenosis symptoms.
-
Pain, focal or radicular
-
Documented curve progression
-
Curve greater than 60°
-
Severe cosmetic deformity
-
Flatback syndrome, sagittal or coronal imbalance
-
Vertebral translation or instability due to severe lumbar curve
modalities are ineffective in stopping it and surgical treatment should
be considered. Because of the high likelihood of progression, patients
with thoracic curves measuring 60° or more should generally consider
surgical treatment. Patients with lumbar curves of less magnitude may
sometimes require surgery because of pain and progression (4).
must decide if the symptoms are severe and limiting enough to justify
the risks of major surgery. The physician must be certain that the pain
is related to a structural spinal problem, since idiopathic back pain
is just as common in people with scoliosis as in the general
population. Discography may be helpful in determining whether
symptoms
of low back pain are related to disc degeneration or junctional
problems. The radiographic appearance of the discogram is not
important, but the reproduction of the patient’s pain pattern during
injection is diagnostic (13,26).
the goals of surgery and the treatment expectations to the patient. The
treatment recommendations must be tailored to the patient’s specific
complaints. In most cases, they represent a combination of pain,
neurologic symptoms, curve progression, and cosmesis. When pain is the
major complaint, the pain generator must
be identified and treatment targeted accordingly. The contribution of
sagittal and coronal imbalance to pain must be evaluated and treatment
planned to include the appropriate realignment procedure. If neurologic
symptoms are the major concern, the source of root or cord compression
must be identified and treated.
posterior decompression or may be alleviated by indirect decompression
through curve realignment. When curve progression is the most
significant concern, its rate and extent must be documented to provide
the correct treatment recommendation—fusion in situ
or curve correction. If cosmesis is the primary indication for surgery,
then the curve flexibility must be evaluated and the most appropriate
realignment technique utilized. Thoracoplasty may be needed to correct
the rib hump in patients with adult scoliosis.
indicate the location of implants and the application of corrective
forces to be used (Fig. 159.3). Side-bending
radiographs are crucial to the decision process. Measure bending films
to determine the best passive correction obtainable for each curve.
Most adult curves can be adequately treated with posterior techniques
alone, but larger, more rigid curves are better treated with a combined
approach of anterior release and interbody grafting followed by
posterior instrumentation and grafting. Anterior release and interbody
fusion should be considered when
 |
|
Figure 159.3.
Radiograph marked before surgery to indicate types and sites of hook placement in a 24-year-old woman with double major thoracic and lumbar curves. |
-
The thoracic and thoracolumbar curves do not correct to an angle of less than 50° on lateral-bending radiographs;
-
The primary curve cannot be corrected on
lateral-bending radiographs to match the corrected compensatory curve
(to achieve two balanced curves) (5); -
The patient has a higher than usual risk of pseudarthrosis (neurofibromatosis);
-
L-4 does not reach neutral on maximal side-bending radiographs and the surgeon wants to avoid fusion to L-5 or the sacrum;
-
Fusion to the sacrum is necessary.
pseudarthrosis in a posterior lumbosacral fusion. In painful curves,
discography can ensure that the fusion is not terminated at the level
of a symptomatic degenerative disc. If radicular symptoms are
prominent, magnetic resonance imaging (MRI) is indicated.
as a single surgical procedure. Preoperative autologous blood donation
is routine unless contraindicated. Perform pulmonary function tests,
measure nutritional parameters, and do a full medical workup before
undertaking a combined procedure. Although a single-stage operation is
physically taxing, complications for it are significantly less than for
two-stage procedures (19,20).
If blood loss during the anterior approach is excessive or the patient
is hemodynamically unstable, the posterior procedure may be postponed
for 5–7 days. In the interim, maximize pulmonary function, prevent or
treat urinary tract or wound infections, and maintain sound nutritional
status.
correction is the goal, consider a staged procedure incorporating 2 to
3 weeks of halo–femoral traction between the
anterior
and posterior surgeries. Most adults can tolerate this regimen
physically and psychologically. Pin site and skin care must be
meticulous. We recommend prophylaxis against deep-vein thrombosis.
Initiate physical therapy to encourage deep breathing and extremity
range-of-motion exercises. During traction, tilt the head of the bed up
15° to 20°. Attach the halo ring to the bed frame and apply 10–20
pounds of weight to each of the femoral traction pins. The patients may
be out of traction for bathing and may be up with a walking or
wheelchair traction frame as tolerated.
fixation in adult scoliosis. Greater curve correction and better
sagittal plane balance are possible with segmental instrumentation than
with traditional Harrington instrumentation. Modern segmental
instrumentation systems are based on a longitudinal member to which a
variety of hooks, screws, sublaminar wires, or connectors can be
attached. Stronger spinal fixation is afforded by multiple fixation
points along the rod and by using strategic combinations of screws,
sublaminar wires, and hooks to gain firm purchase on the pedicles,
laminae, and transverse processes.
implant stability, as adults fuse more slowly than adolescents, and
they have stiffer curves and often poorer bone stock. The rate of
pseudarthrosis and rod failure with segmental instrumentation is lower
than with Harrington instrumentation (18,22,24).
In addition, the prolonged postoperative immobilization necessary after
Harrington instrumentation is often unnecessary after segmental
instrumentation.
is controversial and does carry a theoretically greater risk of screw
misplacement because of the bony deformity. Pedicle screws do provide
superior fixation in adult patients, however, and their use can enhance
correction by harnessing the “force nucleus” (junction of pedicle
lamina and transverse process), as described by Steffee et al. (23) and others (27). Pedicle screws also allow for parallel, purely axial corrective forces between adjacent segments.
lordosis when distraction or compression forces are applied.
Specifically, pure distraction in the lumbar spine can produce a
painful flatback syndrome unless multiple hooks are used and rods are
carefully contoured to maintain lordosis. Sublaminar wires are most
valuable in lateral translation of the spine during correction. They
cannot control rotation or axial collapse and as such work best in a
combined construct with hooks or screws.
at the stable vertebra, which is the vertebra intersected by the
central sacral line (12) (see chapter 156).
With segmental instrumentation, the lower end of the fusion should be
the vertebra that becomes level on maximal side-bend radiographs.
Patients with a rigid lumbosacral curve who have significant residual
tilt of L-4 on bending films, and those with low back pain due to disc
degeneration at L-4–L-5 or L-5–S-1, require fusion to the sacrum. Avoid
fusion down to L-5 alone, as the incidence of subsequent low back pain
is high (6).
-
Coronal plane deformities can be corrected by longitudinal compression and distraction forces.
-
Sagittal plane contours can be restored
by properly contouring the rods and avoiding strong distraction forces
in the lower lumbar segment. -
Finally, there is limited potential to improve rotational deformity through proper contouring of the rods.
of surgery can be improved, especially with regard to the thoracic rib
hump. The cosmetic correction possible in the adult is usually less
than what can be achieved in the adolescent, but it can be maximized by
a circumferential release of the spine including concave and convex
facetectomies. Severe rib-cage deformities may be improved through
thoracoplasty, but not without some additional pain and potential
morbidity.
rate of pseudarthrosis and fixation failure. For neuromuscular
scoliosis, the modified Galveston technique of Allen and Ferguson
achieves firm pelvic fixation and a high fusion rate (1).
For ambulatory patients, instrumenting across the intact sacroiliac
joints is not recommended and sacral fixation is needed. Single-level
hook or screw purchase into the sacrum is often inadequate when an
extended construct acts as a long lever arm above the sacrum. The two
options that can be considered are (a) additional pedicle screws into
S-2 and (b) an intrasacral rod technique. Any long construct
terminating at the sacrum should be augmented with an L-5–S-1 interbody
fusion using either an anterior or a posterolateral technique.
stabilize a curve until fusion is achieved. The Zielke instrumentation
is the prototype, but many useful systems are now available. Double-rod
anterior systems have recently been described (11)
and appear promising. Anterior instrumentation can be more advantageous
than posterior and may even preclude a posterior procedure.
instrumentation systems are better suited to correct deformity in the
coronal, sagittal, and axial planes (8,10,14), but
they have their limitations. If screws are not properly aligned,
anterior instrumentation may produce kyphosis in the thoracolumbar and
lumbar spine. Also, instrumentation extending to the low lumbar spine
may impinge on the vascular structures.
penetration of the spinal canal. Protect the spinal canal by
identifying landmarks and bluntly dissecting around the opposite side
of the vertebral body. Place a finger at the junction of the transverse
process, pedicle, and vertebral body to act as an aiming guide.
screw and rod breakage were common. With more modern, robust
instrumentation, breakage is far less common, but screw pullout at the
proximal or distal end of the construct remains a problem. To prevent
this problem, use a pullout-resistant nut on the opposite side of the
vertebral body (16), or extend the instrumentation to other levels to distribute the load.
-
Position the patient on an appropriate
spinal frame, ensuring that the abdomen hangs freely and that
compression of the inferior vena cava is minimized. If pedicle screws
will be needed, use a radiolucent table or frame; otherwise, use either
a Wilson frame or longitudinal bolsters. Take care during positioning
to make sure that the face is well padded and that there is no
P.4107
pressure on the eyes. Drape the back to provide access to the entire spine and to the iliac crest for graft harvest. -
Center a longitudinal midline incision
over the apical vertebra. After stripping the paraspinous musculature,
expose the spine subperiosteally to the tips of the transverse
processes. -
Identify levels radiographically by placing a towel clip through the transverse process of the selected vertebra.
-
After exposing the lamina at the levels
to be fused, identify hook and screw sites and prepare them for implant
placement. The technique of hook insertion is identical to that
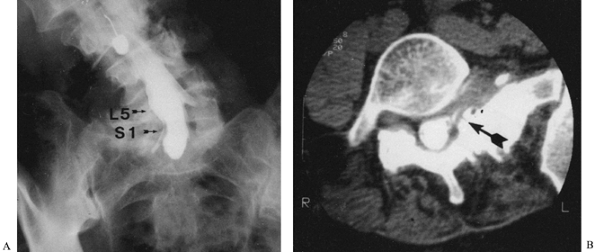
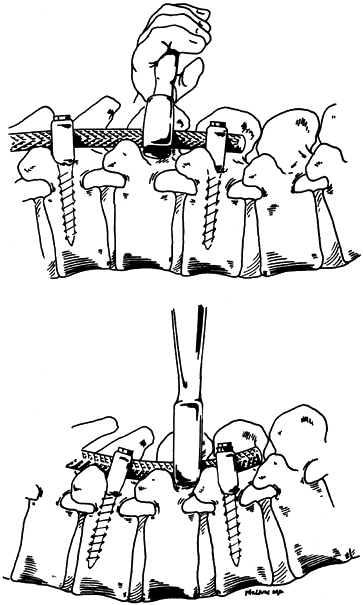
performed in adolescent patients (Fig. 159.4).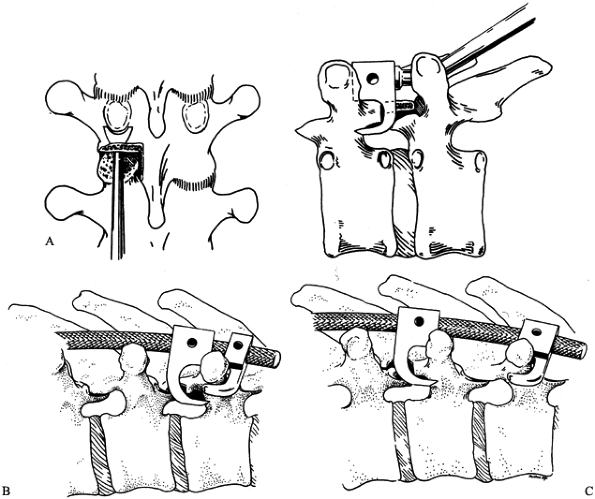 Figure 159.4. A: Insertion of the pedicle hook. B:
Figure 159.4. A: Insertion of the pedicle hook. B:
Construction of the upper claw. Two forms of transverse-pedicular claws
can be used to secure the upper end of the construct. A single-level
claw using a transverse process hook and standard pedicle hook is the
most common combination. C: For longer
constructs, a two-level claw may be easier to apply. Use standard
closed lumbar lamina and pedicle hooks. Either of these constructs can
be substituted for the other when a transverse process is fractured
during instrumentation. -
After excising the inferior facet with a
narrow osteotome, remove the articular surface of the underlying
superior facet with a straight curet. Locate the pedicle, which lies at
the level of the transverse processes, with the pedicle finder. With
the finder well seated on the pedicle, the vertebral body can be moved
side to side with the finder. If the two do not move as a unit, the
purchase is inadequate. -
Then insert the pedicle hook, taking care not to split the lamina during placement.
-
Place additional hooks, if desired, to
increase the overall strength of the construct and to distribute forces
over a greater number of vertebrae (Fig. 159.5). Extra hooks may be especially helpful in patients with osteoporotic bone (Fig. 159.6).![]() Figure 159.5. Postoperative radiograph of patient in Figure 159.3,
Figure 159.5. Postoperative radiograph of patient in Figure 159.3,
treated with Cotrel-Dubousset segmental instrumentation. This
triple-rod technique distributes corrective forces over many spinal
segments using multiple fixation hooks. Combined with anterior thoracic
and lumbar releases, this approach provided 45% correction of the
thoracic curve (101° to 55°) and 55% correction of the lumbar curve
(108° to 48°).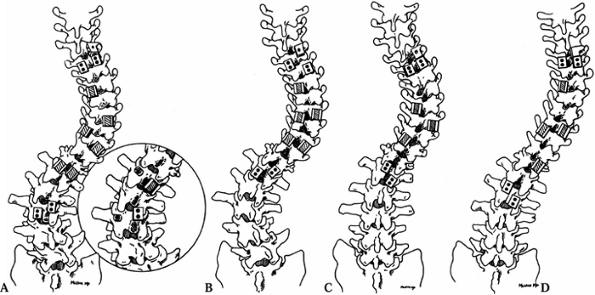 Figure 159.6. Hook patterns for specific scoliotic curves. A:
Figure 159.6. Hook patterns for specific scoliotic curves. A:
King type I curve—S-shaped curve with lumbar curve that is larger and
less flexible than the thoracic. This hook pattern uses the standard
thoracic pattern (see type III) but adds hooks distally to allow
compression of the lumbar convexity and distraction of the lumbar
concavity. (Inset) Pedicle screws may be
used in the lumbar segment and are most easily placed on the convexity.
Distal hooks or screws allow correction of any junctional kyphosis when
the curve is corrected. B: King type II
curve—S-shaped curve in which both thoracic and lumbar curves cross the
midline. In this curve, the lumbar curve is more flexible and does not
require full instrumentation. Correction of the thoracic curve using a
standard thoracic pattern is adequate to provide a satisfactory
anteroposterior (AP) contour. Add upper lumbar fixation to help prevent
decompensation and to restore sagittal balance. C:
King type III curve—typical right thoracic curve. Construct other
fixation patterns around this one. Instrument the concavity with
pedicle hooks at the upper end-vertebra and one level above the apex,
and sublaminar hooks downgoing at the lower end-vertebra and one level
below the apex. This pattern allows uniform distraction over the
concave side, along with some derotation. Provide compression over the
convex side with a transverse-pedicular claw at the upper end-vertebra,
an open pedicle hook at the level of the apex, and a sublaminar hook
under the lamina of the lower end-vertebra. Additional open hooks may
be added in patients with poor bone quality. D:
King type IV curve—long thoracic curve in which lower lumbar vertebrae
also tilt into the curve. Instrumentation of this curve is similar to
that of type III, with the distal hooks carried to the upper lumbar
spine to correct the longer curve. Attempt to spare the lower lumbar
segments and allow the patient to compensate spontaneously. If the
lumbar deformity is rigid, instrumentation and fusion may have to be
extended to the lower lumbar spine. -
Although rotational correction is
possible in reasonably flexible curves, derotation may not be possible
or safe in very stiff curves. Overzealous attempts to derotate or
translate vertebral elements may result in fractures of the laminae or
pedicles, and possible penetration of implants into the spinal canal (9). -
For stiffer curves, gain correction by
segmental distraction, along with appropriate sagittal contouring to
maintain or correct kyphotic or lordotic segments. Large, rigid
thoracic curves may be partially corrected with a short apical rod
placed in the concavity, before completing the construct with a long
distraction rod. The long rod can then be coupled to the short apical
distraction rod, and, after distraction, both can be coupled to the
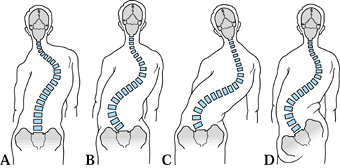
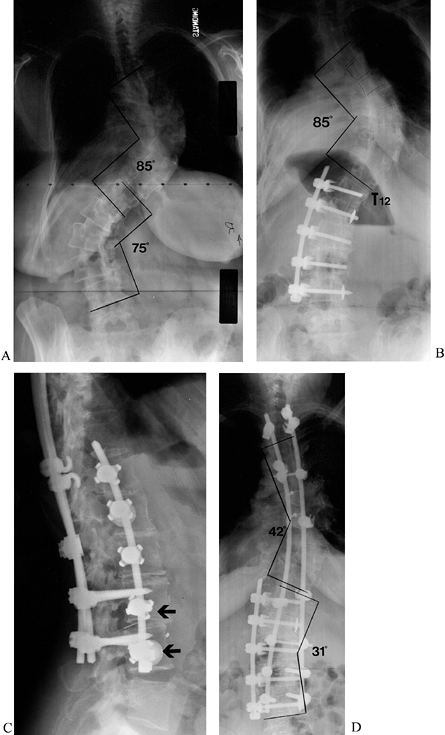
convex rod (Fig. 159.7).![]() Figure 159.7. A 28-year-old woman with a stiff King-type V thoracic scoliosis. A:
Figure 159.7. A 28-year-old woman with a stiff King-type V thoracic scoliosis. A:
Preoperative PA radiograph demonstrates double thoracic curve. Upper
curve (apex T-5) measured 76°. Lower curve (apex T-10–T-11) measured
110°. B: Following right anterior thoracic
release, a short, apical distraction rod used to correct the uppermost
curve. A longer rod spanning the convexity of the lower thoracic curve
was connected to the first rod in bayonet fashion with a double-barrel
“domino.” Both these rods combine to make the third member of a
triple-rod construct using a short reduction rod at the apex of the
lower thoracic curve. C: Lateral view shows restoration of thoracic kyphosis and neutral thoracolumbar alignment. -
Always crosslink rod constructs to increase the torsional stiffness of the construct (2).
-
Before completing the instrumentation,
excise all facet joints and thoroughly decorticate the exposed spine.
Although segmental instrumentation offers rigid fixation, strict
adherence to these principles is crucial to obtain a consistent fusion
in adult patients. During decortication, preserve the integrity of the
laminae and transverse processes on which hooks are to be placed. -
We advocate the use of autogenous iliac
bone graft, particularly if wide laminectomy has been performed in the
lumbar spine, in cases of pseudarthrosis, or with fusion to the sacrum. -
Radicular pain resulting from foraminal
or lateral recess stenosis often resolves with curve correction and
stabilization. Medial facetectomies and foraminotomies, however, may be
carried out if there is documented foraminal or lateral recess stenosis
consistent with the lower extremity symptoms. If the curve is stable,
and not progressive, root compression may be treated with decompression
alone. Partial medial facetectomies and foraminotomies may be carried
out through a limited laminotomy, taking care to preserve the pars
interarticularis and dorsal facet joints. -
Achieve posterior releases by performing
an osteotomy at each of the rigid periapical segments. Beginning in the
midline, open the ligamentum flavum, and then use Kerrison rongeurs to
excise the ligamentum flavum. In longstanding deformities, the
ligamentum flavum may be ossified and will need to be taken down with a
burr
P.4108P.4109
and
Kerrison rongeurs. Proceeding laterally on both sides, excise the
facets and enter the neural foramen. These osteotomies will
significantly increase the mobility of the curve.
-
Treat rigid, high-degree curves by
anterior release and interbody grafting before proceeding with
posterior instrumentation, correction, and grafting. Carry out the
traditional anterior release as described in Chapter 155,
with two particular precautions: First, because vascular supply to the
cord is less robust in adults, and particularly tenuous in kyphotic
segments, exercise caution when approaching those segments anteriorly.
It may be wise to preserve segmental vessels in these regions, or at
least to temporarily occlude large segmentals with a vascular clamp and
observe for changes in the somatosensory evoked potentials. -
Second, very rigid curves may require an
extensive release, including excision of the posterior longitudinal
ligament, before correction can be obtained. In order to shorten the
vertebral column (to restore thoracic kyphosis and avoid stretching the
neural elements) during correction, partial vertebrectomy may be
necessary at apical levels. -
Anterior instrumentation may improve
curve correction and may allow the surgeon to spare lower lumbar
segments in some patients with thoracolumbar and lumbar curves. Place
vertebral body screws as far posteriorly as possible on the convex side
of the spine, traversing each body in an anterolateral direction,
slightly
P.4110
away
from the canal. In a badly rotated specimen, this orientation can be
difficult to obtain. By placing the end-vertebral screws slightly more
anterior to the periapical screws, instrumentation and correction will
naturally tend to rotate the lumbar curve and restore lumbar lordosis. -
Because the vertebral cortex in the
midbody is thin, create the starting hole with a hand-held awl.
Bicortical purchase is desirable, particularly at end vertebrae. If
posterior pedicle screw instrumentation is planned, place the anterior
vertebral body screws below the midpoint of the vertebral body. -
With the advent of endoscopic techniques,
thoracotomy and thoracolumbotomy may be avoided and the anterior
release and interbody grafting performed in a minimally invasive
fashion. Using endoscopy, the anterior and posterior procedures may
even be performed simultaneously with the patient in the prone position
(17).
surgery, and walking within 3–5 days. If bone quality is good and
implant purchase is thought to be secure, no brace is needed. If there
is any concern about the security of internal fixation, use a
thoracolumbosacral orthosis (TLSO) for 4 to 6 months. Bracing is also
commonly used in patients fused to L-3 or L-4, as there is greater
stress on the lower lumbar implants. Bracing to neutralize lower lumbar
or lumbosacral curves should include a thigh cuff with a drop-lock
hinge.
brace. Walking is recommended from the outset. A walking program,
progressing to 1 mile daily, provides regular exercise during fusion
consolidation.
-
Blood-loss-induced anemia
-
Pulmonary compromise
-
Pseudarthrosis
-
Failure of instrumentation
-
Flatback syndrome
-
Neurologic compromise
-
Continued pain
-
Infection
instrumentation are not yet known, these will probably be lower than
with older systems due to the more rigid fixation. Hook displacement
and cutting-out of lumbar hooks have been reported with
Cotrel-Dubousset instrumentation (9). “Claw”
hook configurations on a single lamina may predispose to lamina
fracture, and an inferior claw spanning two laminae is recommended to
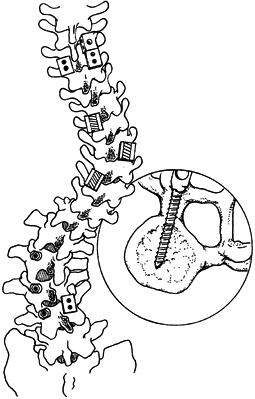
help prevent pullout. The use of pedicle screws in lower lumbar
vertebrae may improve purchase in osteoporotic patients and those with
stiff lumbar curves. The surgeon may use multiple pedicle screws or a
pedicle–laminar claw for maximum fixation (Fig. 159.8).
 |
|
Figure 159.8.
Lumbar fixation can be maximized by using pedicle screws in stiff thoracolumbar and lumbar curves. The rotation of the vertebra leaves the convex pedicle oriented in the AP plane, allowing easy placement of screws. Place a sublaminar hook on the concave side to allow distraction. |
since the introduction of segmental systems. This disabling condition
causes back pain, forward tilt of the trunk, and severe sagittal
imbalance (15).
It can be avoided in segmental fixation systems by carefully contouring
the rods to the normal lumbar lordosis and avoiding excessive
distraction in the lumbar spine. Preventing this complication is
critical, as surgical correction of the established condition is
fraught with complications and often gives a poor result.
fusion, but, if a discreet pain generator has been identified,
improvement can generally be expected (18,22). Even though the curve has been stabilized, patients may continue to experience back pain.
loss and neurologic injury, are more common in adults than in
adolescents. Neurologic complications with Harrington instrumentation
have been uncommon; the risk of spinal cord injury is primarily related
to overdistraction of a rigid curve. The same risks are present during
distraction using segmental instrumentation and may be magnified by the
increased mechanical advantage provided by segmental systems. Attempts
to derotate a rigid curve in an osteoporotic spine may cause a concave
pedicle hook to fracture the pedicle and penetrate the spinal canal.
Gurr and McAfee reported such a case, which resulted in a Brown-Séquard
syndrome (9). Rigid curves, especially in the
presence of osteoporosis, should be treated with distraction and
compression, avoiding derotation or strong translation forces. Remember
that the primary goal of surgery in the adult with scoliosis is to
stabilize the curve and halt progression; correction is a secondary
objective.
this allows recognition of subtle neurologic changes, permitting the
surgeon to take prompt action to reverse them (29).
scoliosis; each curve has its own “personality,” and each patient
presents with his own confounding variables (Fig. 159.9).
The presenting complaint, level of deformity, and rigidity of the
curves dictate the specifics, but a general approach can be proposed.
 |
|
Figure 159.9. A 46-year-old woman with severe, progressive thoracolumbar scoliosis. A:
Preoperative PA radiograph demonstrates high-degree thoracic and lumbar curves. Bending films revealed little correction of either curve. Occiput was 4.0 cm left of the central sacral line. B: After anterior lumbar release and instrumentation, the lumbar curve was improved but the thoracic curve was no better and out of balance. C: Thoracic release and posterior instrumentation were performed 7 days later, under one anesthetic. Lateral view shows pedicle screws properly placed in the lumbar pedicles, passing above the vertebral body screws that were placed low in each vertebral body. Thoracolumbar kyphosis has been improved to mild lordosis. Custom-designed pullout nuts (lower arrow) improve pullout strength of the vertebral body screws. D: Anterior thoracic release, combined with posterior segmental instrumentation, provided 50% correction of the thoracic curve. The combined approach to the lumbar curve provided correction of almost 60%. |
-
If both thoracic and lumbar curves must
be addressed, carry out the lumbar retroperitoneal approach at the
initial operation. Perform an anterior release, interbody fusion, and
anterior instrumentation. -
Give the patient 5–7 days to recover before performing the definitive second procedure.
release and full-length posterior instrumentation as staged or
simultaneous procedures.
-
In the staged procedure, place the
patient in a lateral decubitus position with the curve convexity up.
Through the anterior approach, release as many levels as can be
reached, removing as much of the concave soft tissues as is necessary
to allow motion when pressure is applied to the vertebral body. -
Once the convex release is completed,
lightly pack the morcelized rib into the intervertebral spaces, close
the wound, and turn the patient prone on the spinal frame. -
Perform posterior instrumentation, incorporating all of the thoracic and lumbar curves.
-
Place multiple hooks to correct both
coronal and sagittal alignment. Place pedicle screws distally to obtain
the most stable foundation for the rest of the construct. -
Contour the rods to impart more normal
thoracic kyphosis and lumbar lordosis, and then lock them into the
lumbar screws distally. -
Sequentially reduce the rods into remaining hooks, taking time to allow viscoelastic forces to dissipate.
curves may reflect the existing scoliotic curves, and rod placement may
be easier if the rods are placed in an off-axis, rotated position (Fig. 159.10).
 |
|
Figure 159.10.
Correction of junctional kyphosis is crucial to sagittal plane balance. Derotation of a contoured fixation rod using hooks or pedicle screws allows the surgeon to restore thoracolumbar lordosis and thoracic kyphosis at the time of curve correction. |
-
After loosely affixing the hooks and screws to the rod, apply C-rings to prevent hooks from displacing.
-
Slowly rotate the rods back into normal
orientation, placing the kyphotic and lordotic curves back in the
sagittal plane. This “derotation” maneuver simply uses rod contours to
apply translational forces to correct the coronal deformity. There is
no actual derotation of the vertebrae.
and prep anteriorly to the midaxillary line on the side of the
concavity. A thoracoscopic approach can then be used to release
multiple disc spaces through a few periapical portals. Carry out the
posterior instrumentation without changing the patient’s position.
requiring thorough patient evaluation and careful preoperative
planning. An accurate assessment of spinal pain and curve progression,
and knowledge of the natural history of scoliosis are essential
components in formulating an appropriate treatment plan. With more
advanced surgical techniques, patients once thought to be untreatable
may now be effectively managed. Although surgery is a major
undertaking, with a significant complication rate, the results of
surgical treatment of adult scoliosis can be extremely gratifying.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
T, Irtam L, Nachemson A. Long-Term Anatomic and Functional Changes in
Patients with Adolescent Idiopathic Scoliosis Treated by Harrington Rod
Fusion. Spine 1983;8:576.
K, Shono Y, Satoh S, Abumi K. Anterior Correction of Thoracic Scoliosis
with Kaneda Anterior Spinal System. A Preliminary Report. Spine 1997;22:1358.
IH, Khazim R, Woodside T. Anterior Vertebral Body Screw Pull-out
Testing: A Comparison of Zielke, Kaneda, Universal Spine System, and
Universal Spine System with Pull-out Resistant Nut. Spine 1998;23:908.
IH, Orr RD, Salo PT, Kraetschmer BG. The Results of Simultaneous
Endoscopic Anterior Release and Posterior Instrumentation for Spinal
Deformity. Orthopaedic Proceedings. J Bone Joint Surg Br 1998;80(supp 1):5.
RC, Dickson JH, Harrington PR, Erwin WD. Results of Harrington
Instrumentation and Fusion in the Adult Scoliosis Patient. J Bone Joint Surg Am 1975;57:797.
DN, McLain RF, Benson DR. Luque Galveston Instrumentation in
Neuromuscular Scoliosis: Surgical and Functional Outcomes. Proceedings of the Scoliosis Research Society, 32nd Annual Meeting, St Louis, MO, September 1997.
AD, Biscup RS, Sitkowski DJ. Segmental Spine Plates with Pedicle Screw
Fixation. A New Internal Fixation Device for Disorders of the Lumbar
and Thoracolumbar Spine. Clin Orthop 1986;203:45.
Dam DE, Bradford DS, Lonstein JE, et al. Adult Idiopathic Scoliosis
Treated by Posterior Spinal Fusion and Harrington Instrumentation. Spine 1987;12:32.
RG, Thompson GH, Shaffer JW, et al. Postoperative Neurological Deficits
in Segmental Spinal Instrumentation. A Study Using Spinal Cord
Monitoring. J Bone Joint Surg Am 1984;66:1178.