Surgical Dislocation of the Hip for Fractures of the Femoral Head
IV – Miscellaneous Topics > 44 – Surgical Dislocation of the Hip for
Fractures of the Femoral Head
Anterior hip dislocations are less common but can also be associated
with femoral head fractures; according to one series, femoral head
fractures were seen in 15% of anterior hip dislocations (12), and in another, up to 77% of anterior hip dislocations involved femoral head fractures (3).
decrease the risk of avascular necrosis, which is secondary to ischemia
caused by tension on the blood supply of the femoral head (13,14,15,16). This treatment is preferably done within 6 to 12 hours from the time of injury (4,13,17).
Prior to attempting a closed reduction, the surgeon should exclude the
presence of a concomitant femoral-neck fracture. Postreduction, an
axial computed tomography (CT) scan with 2-mm cuts is necessary to
ensure concentric reduction (5,18,19). Typically, open reduction and internal fixation (ORIF) is required for definitive management of the femoral head fracture (4).
At the same time, the surgeon can address other associated
musculoskeletal injuries, which commonly include fractures of the
acetabulum as well as the femoral neck and shaft (4).
As these injuries are often seen in the setting of high-energy trauma,
the patient must be evaluated appropriately for associated abdominal,
thoracic, and craniofacial injuries (8).
presence of femoral neck fracture, postreduction hip-joint asymmetry,
progressive sciatic-nerve injury, or an intra-articular fragment
displacement of at least 2 mm or that renders the hip unstable (1,20,21,22). For
Pipkin type I or II femoral-head fractures, free or nonreduced
fragments that remain after reduction must be excised or reduced and
stabilized to avoid early posttraumatic arthrosis (5,11,14,17).
Historically, recommendations have included excision of large
fragments, including those that measure up to one third of the femoral
head (2,4,5,21). However, because the entire acetabulum is involved in weight bearing (23), any fragment that is amenable to fixation should be rigidly fixed. Smaller fragments may be excised (6,14,22,23,24,25,26,27,28), and avulsion fractures of the ligamentum teres can be treated conservatively.
optimal surgical approach for fixation of femoral head fractures.
Initially, the Kocher-Langenbeck approach was used. Through the
Kocher-Langenbeck approach, surgeons can address fractures of the
posterior acetabular wall but had only limited access to the articular
surface of the femoral head for fracture reduction and fixation. In
addition, some studies identified an increased incidence of avascular
necrosis of the femoral head when Kocher-Langenbeck was used instead of
the Smith-Peterson approach (26,27).
access to the anterior portion of the femoral head for debridement of
intra-articular debris. However, this approach does not allow complete
visualization of the femoral head, nor can the surgeon address
posterior acetabular-wall fractures. In addition, heterotopic
ossification has been shown to be a significant risk with the anterior
approach (24,27). While
combined anterior and posterior approaches would improve visualization
in the case of extensive femoral-head fractures, the risk of
complication is increased with such extensive dissection.
described a technique for surgical dislocation of the hip. It involves
a Kocher-Langenbeck approach with a trochanteric flip and anterior
dislocation of the hip. This approach allows visualization of the
entire femoral head as well as the full circumference of the
acetabulum. Using this exposure, the surgeon can obtain anatomic
reduction and rigid fixation of the femoral head fragments, as well as
a thorough debridement of the joint, without compromising the blood
supply to the femoral head (29,30,31).
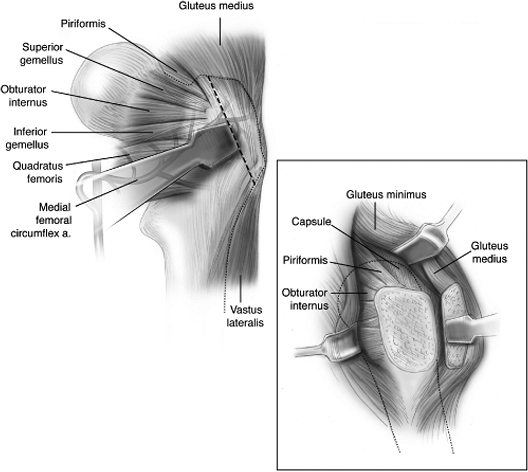
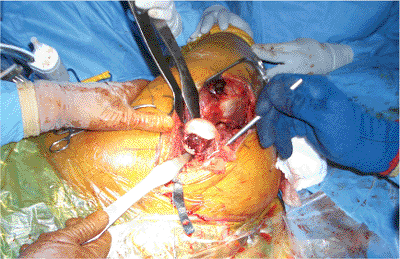
standard Kocher-Langenbeck incision is made through the skin,
subcutaneous tissue, and tensor fascia lata (Fig. 44.1).
The leg is then internally rotated to expose the posterior border of
the gluteus medius. Unlike the approach used in total hip arthroplasty,
no attempt is made to mobilize the gluteus medius or expose the
piriformis tendon. Electrocautery is used to mark the gluteus medius at
the posterior edge of the greater trochanter. The posterior border of
gluteus medius is then traced distally to the posterior ridge of the
vastus lateralis muscle, which is the point at which the deep branch of
the medial femoral-circumflex artery becomes intracapsular.
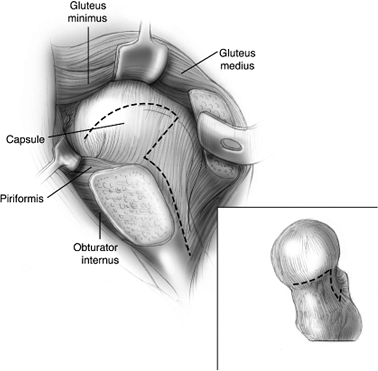
line traced by the electrocautery, is then performed with an
oscillating saw (Fig. 44.2). To protect the
deep branch of the medial femoral-circumflex artery, the surgeon is
careful to work anterior to the most posterior insertion of the gluteus
medius. In addition, the surgeon must keep a posterior shelf of bone
just behind the osteotomy to protect the insertion of the short
external rotators. At its distal end, the osteotomy should exit at the
level of the vastus ridge. The vastus lateralis is then released along
its posterior edge to the level of the gluteus maximus tendon, and the
greater trochanter is everted anteriorly. Release of the remaining
posterior fibers of gluteus medius allows free mobilization of the
trochanteric segment. Additional exposure can be obtained by the
elevation of the vastus lateralis and intermedius from the lateral and
anterior aspects of the femur respectively. With anterior retraction of
gluteus medius, the trochanteric
fragment,
and vastus lateralis, the tendon of the piriformis and the gluteus
minimus muscle should be visible. The gluteus minimus is then carefully
elevated off of the hip capsule. Gentle flexion and external rotation
of the hip allows visualization of the anterior, superior, and
posterosuperior hip capsule.
 |
|
Figure 44.1. Incision and division of the tensor fascia lata.
|
location of the sciatic nerve as it passes inferior to the piriformis
tendon. Flexion of the knee releases some of the tension on
the
nerve. In 12.7% of individuals, the peroneal branch of the sciatic
nerve passes either through the piriformis or superior to it (Fig. 44.3) (32).
In these individuals, the piriformis tendon should be released to
prevent stretching of the nerve during dislocation of the hip. To
protect the ascending branch of the medial femoral-circumflex artery,
the tendon should be released 1.5 cm from its insertion rather then at
its attachment to the femur.
 |
|
Figure 44.2. A. Sliding trochanteric osteotomy. B. Retraction of trochanter, gluteus medius, and gluteus minimus with exposure of joint capsule.
|
 |
|
Figure 44.3. Variations in relationship of the sciatic nerve to the piriformis muscle. (From
Agur AMR, Lee MJ. In: Kelly PJ, ed. Grant’s atlas of anatomy, 10th ed. Philadelphia: Lippincott Williams & Wilkins; 1999:329
, with permission.) |
 |
|
Figure 44.4. Outline of capsular incision.
|
anterolateral surface parallel to the long axis of the neck. At the
base of the neck, the incision curves anteriorly and inferiorly along
the reflection of the anterior capsule (Fig. 44.4).
The main branch of the medial femoral-circumflex artery lies superior
and posterior to the lesser trochanter; therefore, to avoid injury, the
capsular incision must remain anterior to the trochanter. The proximal
end of the anterolateral capsular incision is extended to the
acetabular rim. It then curves posteriorly, remaining parallel to the
labrum, until the surgeon encounters the retracted piriformis tendon.
Care must be taken not to damage the labrum when doing the capsulotomy.
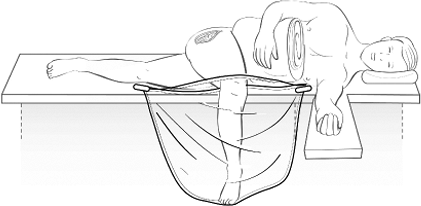
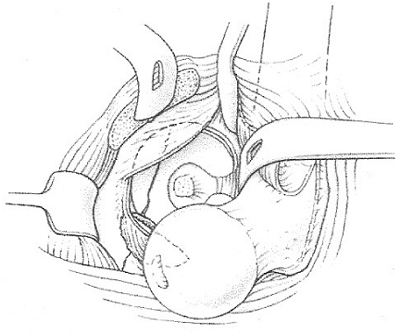
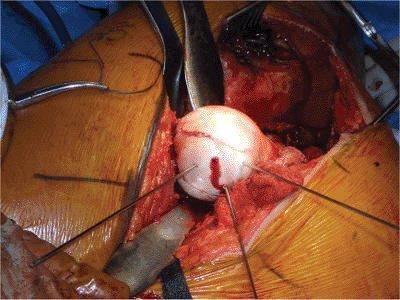
dislocated anteriorly. The leg is placed in a sterile bag over the
front of the table (Fig. 44.5). This positioning allows visualization of the entire femoral head (Fig. 44.6).
It also allows for inspection of the labrum, and with carefully placed
retractors, the entire articular surface of the acetabulum (Fig. 44.7).
surgeon may do a thorough irrigation and debridement of the femoral
head and acetabulum. The labrum and articular surfaces should be
inspected. Small comminuted fragments that are not amenable to fixation
may be excised. If a stump of the ligamentum teres remains attached to
the femoral head, or if it has avulsed a small fragment of the head, it
is also excised.
The aim of fixation is to achieve rigid subarticular fixation while
leaving a smooth articular surface on the femoral head. Common
strategies include burying pins or screws or capturing the fragment by
lag effect from a nonarticular entry point (25). Methods of fixation have included countersinking screws (33), using headless screws (34,35), utilizing bioabsorbable pins or screws (36), or completing suture fixation (21,22,27). Screws with threaded washers are contraindicated because a significant number have backed out of the hardware (26).
Headless screws provide less compressive force across the cancellous
bone of the femoral head than do standard, small, fragment screws (34).
Therefore, we prefer to countersink bioabsorbable or small fragment
screws with heads (Synthes, Paoli, PA) into the fragment. We often
augment the fracture fixation with the addition of a lag screw that is
entered from nonarticular regions.
 |
|
Figure 44.5. Positioning of patient for anterior dislocation: leg in flexion and ER suspended in a sterile bag.
|
 |
|
Figure 44.6. Dislocation of the hip with exposure of the articular surface of the acetabulum.
|
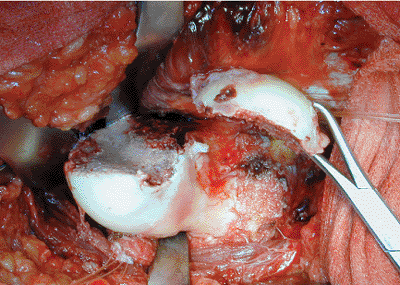
irrigation with saline can be used to prevent desiccation. Prior to
reduction of the hip, a 2.0-mm drill hole is made in the femoral head
to document preservation of the blood supply. Previous studies have
shown a high correlation between adequate blood supply and the presence
of a viable head (see Fig. 44.8) (37). Laser Doppler flowmetry is another proven method of documenting the vascularity of the femoral head prior to reduction (30). The hip is then reduced with manual traction on the flexed knee followed by internal rotation and extension.
meticulous hemostasis is achieved. The capsulotomy is then closed with
1-0 vicryl suture. The greater trochanter is secured using
two
3.5-mm cortical screws directed toward the lesser trochanter. Two large
Hemovac drains are placed deep to the tensor fascia lata.
 |
|
Figure 44.7. Dislocation of hip with exposure of femoral head and Pipkin fragment.
|
 |
|
Figure 44.8.
Dislocation of femoral head and temporary fixation of Pipkin fragment with Kirschner (K) wires. Active bleeding from the dislocated femoral head demonstrates that the blood supply remains intact. |
 |
|
Figure 44.9. Postoperative x-ray illustrating placement of screws for fixation of trochanteric osteotomy.
|
Crutch ambulation training with touch-down weight bearing of 20 pounds
is instituted for 6 to 8 weeks. Strengthening and motion exercises are
instituted and encouraged (22,38).
images are used to confirm fracture reduction, hardware placement, and
concentric hip reduction (Fig. 44.9).
10 to 20 ml per 8-hour shift. In the hospital, patients are maintained
on intravenous cefazolin for 48 to 72 hours. Our postoperative
anticoagulation regimen includes 6 weeks of warfarin in conjunction
with compression boots.
looked at three patients with Pipkin II fractures of the femoral head.
All three were treated with ORIF of the femoral head fractures through
the surgical dislocation technique. Follow-up ranged from 11 to 24
months. At the time of their latest follow-up, all three patients were
ambulating without difficulty and without a limp. None have pain with
ambulation or range of motion of the hip, nor do they have any
radiographic evidence of avascular necrosis or degenerative changes.
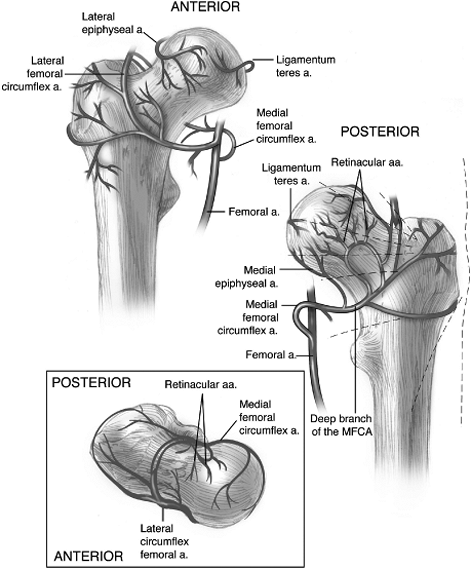
the hip-dislocation approach to fracture fixation is avascular necrosis
of the femoral head. The femoral head receives the majority of its
blood supply from the deep branch of the medial femoral-circumflex
artery (4,41,42,43,44,45).
This branch of the medial femoral circumflex artery (MFCA) is located
at the proximal border of the quadratus femoris muscle. It then courses
superiorly, crossing anterior to the conjoined tendon of the obturator
internus and the superior and inferior gemelli
muscles (Fig. 44.10).
It then perforates the hip capsule to supply the femoral head.
Preservation of the quadratus femoris and the short external rotators
of the hip protect this branch of the medial femoral-circumflex artery,
maintaining the critical blood supply to the femoral head.
 |
|
Figure 44.10. Blood supply to the femoral head and its relationship to the short external rotators.
|
traumatic dislocation of the hip; incidences range from 8.3% to 26.3%
of those treated for traumatic hip dislocation (8,10,14). When the dislocation is endured longer than 6 hours, the risk of avascular necrosis greatly increases (13).
The Ganz approach calls for use of a controlled anterior dislocation of
the hip for a short duration, minimizing the risk of injury to the
nutrient vessels. Ganz et al (29) looked at 213
patients treated with surgical dislocation of the hip for a variety of
pathologies. At 2 to 7 years follow-up, no evidence of avascular
necrosis of the hip has been found.
used a high-powered, laser, Doppler flowmeter to evaluate the changes
in blood flow to the head. They found that the dislocation resulted in
some impairment of blood flow, but it reversed completely with
reduction of the hip. They also found that the anterior capsulotomy
used in this approach did not alter the blood flow to the head despite
the disruption of the anterior intracapsular and extracapsular
anastomoses and the capsular branches of the lateral circumflex artery.
This result indicates that the vessels on the anterior aspect of the
femoral head are not critical to circulation to the femoral head.
Rather, preservation of the posterior extracapsular vessels is the
paramount concern.
Both patients recovered within 6 months. Of note, both of these
patients had undergone previous surgery, and scarring around the
sciatic nerve is thought to have contributed to the neurapraxia.
 |
|
Figure 44.11. Anteroposterior (AP) pelvis radiograph (A) and axial CT scan image (B) show fracture dislocation of the femoral head with large Pipkin-II fragment.
|
failure of trochanteric fixation. These results compare favorably with
the 98% union rate described in the literature for the extended,
trochanteric, slide osteotomy in total hip arthroplasty (46).
was 37%. Most of the ectopic bone formation occurred at the tip of the
greater trochanter, and 86% were classified as Brooker grade I. Two
patients required excision of the ectopic bone to improve their range
of motion.
 |
|
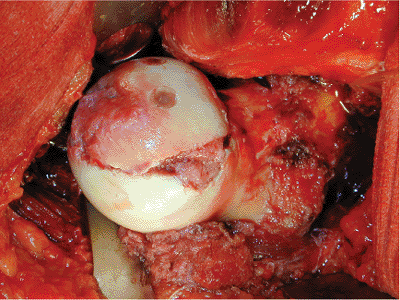
Figure 44.12. Intraoperative photo of femoral head fracture.
|
 |
|
Figure 44.13. ORIF of femoral head fracture. The two bioabsorbable screws are well visualized.
|
 |
|
Figure 44.14. Postoperative AP radiograph.
|
“saddleback” deformities of the subcutaneous fat due to insufficiency
of the subcutaneous sutures. Five of these patients underwent plastic
surgery to improve the cosmetic appearance.
vehicle accident. He was riding a bicycle and was struck by a sports
utility vehicle traveling at approximately 45 mph. He rolled over the
hood of the vehicle and onto the ground. He was initially evaluated at
an outside hospital and found to have an isolated, right, femoral-head
fracture dislocation. At the time of presentation, the hip remained
hinged on the posterosuperior wall of the acetabulum (Fig. 44.11).
femoral head. A surgical dislocation was performed. He was found to
have a sagittal split involving one third of the weight-bearing surface
of the femoral head (Fig. 44.12). The
incarcerated fragment remained attached to the ligamentum teres. This
surgical approach provided excellent visualization of the femoral head
and allowed for anatomic reduction of the Pipkin fragment. Fixation was
obtained using a 3.5-mm cortical screw in the fovea and two countersunk
bioabsorbable screws placed anteriorly and posteriorly (Fig. 44.13).
demonstrates excellent reduction of the femoral-head fracture and a
congruent hip joint (Fig. 44.14). At the
3-month follow-up, the fracture was healed, and the patient was full
weight bearing on the affected leg. At the 6-month follow-up, the
patient remained pain free with excellent range of motion in his hip.
No radiographic evidence of avascular necrosis was found at latest
follow-up.
K, Thomsen PB. Traumatic posterior dislocation of the hip: prognostic
factors influencing the incidence of avascular necrosis of the femoral
head. Arch Orthop Trauma Surg 1986;106(1):32–35.
JP, Harris HW, Volgas DA, et al. Functional outcome of patients with
femoral head fractures associated with hip dislocations. Clin Orthop 2000;377:44–56.
MF, Thorpe M, Seiler JG, et al. Operative management of displaced
femoral head fractures: case-matched comparison of anterior versus
posterior approaches for Pipkin I and Pipkin II fractures. J Orthop Trauma 1992;6(4):437–442.
TR, Rowe SM, Chung JY, et al. Clinical and radiographic outcome of
femoral head fractures: 30 patients followed for 3–10 years. Acta Orthop Scand 2001;72(4):348–353.
R, Gill TJ, Gautier E, et al. Surgical dislocation of the adult hip: a
technique with full access to the femoral head and acetabulum without
the risk of avascular necrosis. J Bone Joint Surg 2001;83(8):1119–1124.
HP, Siebenrock KA, Hempfing A, et al. Perfusion of the femoral head
during surgical dislocation of the hip: monitoring by laser Doppler
flowmetry. J Bone Joint Surg 2002;84(2):300–304.
KA, Gautier E, Woo AK, et al. Surgical dislocation of the femoral head
for joint debridement and accurate reduction of fractures of the
acetabulum. J Orthop Trauma 2002;16(8):543–552.
K, Partio EK, Hirvensalo E, et al. Absorbable fixation of femoral head
fractures: a prospective study of six cases. Ann Chir Gynaecol 1998;87(1):44–48.
RB, Simmonds DF, Malcolm BW, et al. The biological effect of continuous
passive motion on the healing of full-thickness defects in articular
cartilage: an experimental investigation in the rabbit. J Bone Joint Surg 1980;62(8):1232–1251.
TA, Lowry KJ, Anglen JO. Indomethacin compared with localized
irradiation for the prevention of heterotopic ossification following
surgical treatment of acetabular fractures. J Bone Joint Surg 2001;83(12):1783–1788.
