Soft Tissue Tumors
– Evaluation and Management of Musculoskeletal Oncology Problems > 4
– Treatment Principles > 4.4 – Soft Tissue Tumors
by the diagnosis. Based on the pathology of the tumor, appropriate
treatment can involve observation, surgery, radiation and/or
chemotherapy. This chapter will discuss the general treatment
principles.
lesions. Often, the diagnosis of a benign tumor can be made based on
physical examination findings and imaging studies. If there is
confidence that a tumor is benign, treatment can be either observation
or excision.
-
Indications for excision of a benign lesion
-
Unacceptable symptoms from mass effect
-
Known aggressiveness of the tumor type (Box 4.4-1)
-
Uncertainty in the diagnosis (e.g., rapidly enlarging mass)
-
surgical excision. Widespread metastatic disease where local control
provides no benefit is a relative contraindication to surgery.
Historically, soft tissue sarcomas were treated with amputation.
Improvements in radiation, chemotherapy, and imaging and a better
understanding of surgical margins have made limb salvage possible in
the majority of cases. For limb salvage to be pursued, the excision
should give equal local control and function as good as or better than
that of an amputation.
-
Vascular involvement
-
If a major vessel is contained within the wide surgical margin, excision and reconstruction of the vessels are indicated.
-
-
Neural involvement
-
If major nerves are contained within the
wide surgical margin, necessitating resection of the nerve(s), the
functional result must be weighed against amputation. -
If the function of the residual limb is likely to be very poor, amputation may be a better option.
-
-
Osseous involvement
-
If cortical destruction is present, the bone must also be excised and reconstructed as indicated.
-
-
Dead-space management and soft tissue coverage
-
The defect should be closed to minimize
the space for fluid collections, which may impair wound healing.
Surgical drains are frequently used. -
Large defects may require rotational or free flaps for closure (Fig. 4.4-1).
-
Split-thickness skin grafts can be used when there is a skin defect over healthy muscle.
-
-
Extra-abdominal fibromatosis
-
Active hemangiomas
-
Atypical lipomatous tumors
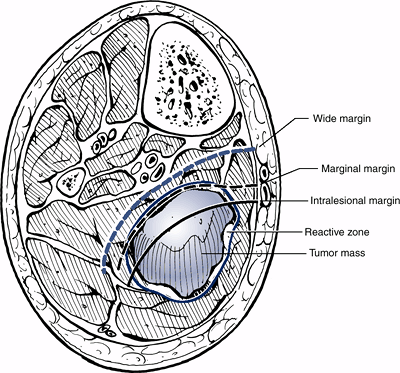
surrounded by a capsule, whereas a sarcoma is surrounded by a
pseudocapsule and a reactive zone. The types of surgical excisions are
defined as intralesional, marginal, wide, or radical according to the
relation of the excised tumor to the surrounding tissue (Fig. 4.4-2).
-
Definition: Dissection plane is carried directly into the tumor; removal is piecemeal
-
Recurrence rate: As gross tumor is left behind, results in 100% recurrence rate in malignancies
-
Indications
-
Often used for biopsy purposes
-
Rarely indicated in treatment of sarcomas
-
Can rarely be used for debulking to relieve mass effect of tumor in palliative surgery
-
-
Definition: Tumor is excised along with the pseudocapsule, with the dissection carried through the reactive zone
-
Recurrence rate: Recurrence rate for soft tissue sarcoma approximately 25% to 50%
-
Indications
-
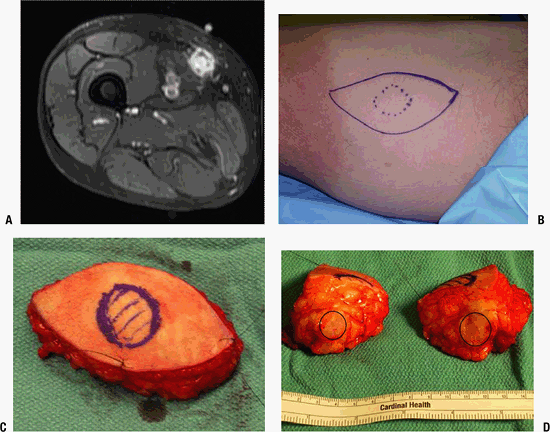
Used predominantly for treatment of benign lesions (Fig. 4.4-3)
-
Rarely used alone for sarcoma treatment, as tumor will extend to the margin of the resection
-
If necessary because of anatomic
limitations, marginal excision with radiation may potentially provide
equivalent local control as wide excision.
-
 |
|
Figure 4.4-1 A synovial cell sarcoma was treated with wide resection (A) and required a free tissue flap for coverage (B).
|
-
Definition
-
Tumor is excised along with pseudocapsule, reactive zone, and cuff of normal tissue.
-
Width of normal tissue that needs to be excised is variable and often dictated by anatomic location and aggressiveness of tumor.
-
-
Recurrence rate: Approximately 10% or less in general
-
Indications
-
The basis of surgical treatment for most soft tissue sarcomas (Fig. 4.4-4)
-
Used for aggressive benign lesions (extra-abdominal fibromatosis, active hemangiomas)
-
 |
|
Figure 4.4-2
Different types of surgical margins. (Adapted from Sim FH, Frassica FJ, Frassica DA. Soft-tissue tumors: diagnosis, evaluation, and management. J Am Acad Orthop Surg 1994;2:202–211.) |
-
Definition
-
Excision of the tumor and the anatomical compartment in which it is contained
-
Can be excision of a muscle compartment (i.e., anterior compartment of thigh) or amputation
-
Results in a larger functional deficit than lesser excisions
-
-
Recurrence rate: Leaves no potential for
local recurrence, but does not appear to provide any benefit over wide
excision in terms of overall survival -
Indications
-
Used if wide excision cannot be achieved otherwiseP.89
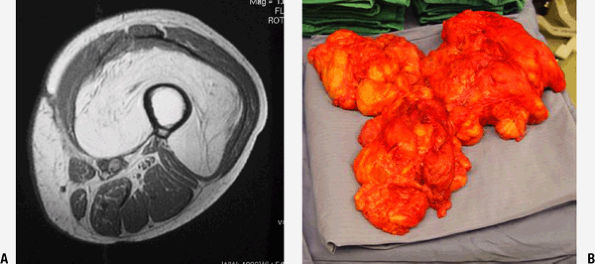 Figure 4.4-3 (A) Magnetic resonance image of a large, deep lipoma in the thigh. (B) Specimen after treatment with marginal excision.
Figure 4.4-3 (A) Magnetic resonance image of a large, deep lipoma in the thigh. (B) Specimen after treatment with marginal excision. -
Not as commonly performed as wide excision and radiation
-
Amputation, a form of radical excision, is often used to treat very aggressive disease.
-
 |
|
Figure 4.4-4 (A) Magnetic resonance imaging shows a soft tissue lesion in the medial thigh. (B) Skin markings showing the limits of the lesion (dashed line) and planned wide resection (solid line). (C) Tissue after wide resection showing sutures marking the orientation. (D) Specimen has been hemisected, showing the normal tissue margins around the tumor (circle).
|
treatment. Wide resection of sarcomas is often difficult to achieve
because of anatomic proximity of tumor to bone and major neurovascular
structures. Radiotherapy is an invaluable
adjunctive
treatment in these instances to augment surgical margins, to allow a
more conservative resection, and therefore to improve the residual
function of the salvaged limb. There is strong evidence that
radiotherapy improves local control rates in combination with
conservative surgery with negative, marginal, or minimal microscopic
positive margins.
-
Indications
-
In current practice, radiation therapy is commonly used as adjuvant therapy for most soft tissue sarcomas.
-
Soft tissue sarcomas that don’t always require radiotherapy
-
Low-grade soft tissue sarcomas
-
Small lesions with very wide surgical margins
-
-
-
Techniques
-
Radiation therapy can be delivered with
external beam, brachytherapy, or intraoperative methods. External beam
may be delivered before or after surgery (Fig. 4.4-5).
-
-
Amputation through the tumor is intralesional.
-
Amputation through the reactive zone is marginal.
-
Amputation through normal tissue but leaving a portion of the involved compartment is wide.
-
Amputation involving the entire compartment(s) involved is radical.
-
Preoperative external beam radiation
-
Administration
-
Usually given as a daily fraction over 5 to 7 weeks
-
Surgical resection carried out 3 to 6 weeks following radiation treatment
-
Typical dose is 50 Gy in 2-Gy fractions.
-
Based on pathological findings, a postoperative boost of 10 to 15 Gy can be given.
-
-
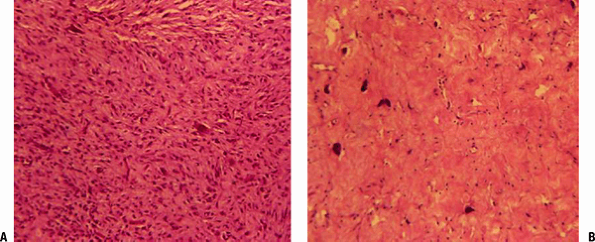
Rationale: In comparison to postoperative
radiation, has the potential benefit of improving the resectability of
lesions and decreasing treatment volumes and local recurrence rates for
large lesions -
Randomized prospective comparison to postoperative external beam:
-
Higher incidence of wound complications (short-term)
-
Lower incidence of edema and fibrosis (long-term)
-
-
-
Postoperative external beam radiation
-
Administration
-
Includes the entire surgical bed with a margin including biopsy site, drain site, and surgical scar
-
Often involves radiation to wider area of nontumor tissue than with preoperative radiotherapy
-
With negative margins, total radiation dose of 50 to 60 Gy
-
With residual tumor or intralesional margin, total dose of 65 to 70 Gy
-
Can combine therapy with a radiation sensitizer to decrease necessary dose
-
-
Rationale: Minimizes wound healing complications, but late adverse effects, including edema and fibrosis, are greater
-
 |
|
Figure 4.4-5 Histological slide of a sarcoma at the time of initial biopsy (A) and after a preoperative course of radiation (B), which resulted in cytoreduction of the tumor.
|
-
Administration
-
Local delivery of radiation through catheters placed at the time of surgery
-
If used alone, a typical dose is 40 to 45 Gy over 4 to 6 days in the perioperative period.
-
If used to augment external beam radiation, a typical dose is 15 to 20 Gy.
-
-
Rationale
-
Allows use of a lower dose because radiation is delivered in close proximity to tissues
-
Delivers radiation dose in shorter time period
-
-
Indications
-
Can be used as alternative or in addition to external beam radiation
-
No randomized trials comparing efficacy to external beam radiation, but appears to have equivalent efficacy
-
-
Administration
-
Treatment given at the time of surgery to the tumor bed
-
Typical dose: 10 to 20 Gy, which is equivalent to 20 to 40 Gy of external beam radiation
-
Can be given in two forms
-
High-dose brachytherapy
-
Catheters used intraoperatively to selectively deliver high-dose radiation to tissue of interest
-
Similar to standard brachytherapy, but higher doses given over a few minutes
-
-
Low-penetration beam (electron beam)
-
The penetration is limited to the first few centimeters of tissue based on energy of beam.
-
Allows use of lower doses than external beam radiation
-
-
-
-
Rationale: Can move vital structures out of the field of radiation
-
Common complications
-
Skin necrosis: the most common major complication
-
Wound dehiscence (Fig. 4.4-6)
-
Soft tissue fibrosis
-
Decreased range of motion
-
Decreased muscle strength
-
Edema
-
Bone fracture
-
Postirradiation sarcoma (very poor prognosis)
-
-
Techniques used to minimize soft tissue damage
-
Conformal radiation
-
Intensity-modulated radiation therapy
-
-
Factors affecting complication rate
-
Total dose of radiation
-
Dose per fraction
-
Relative volume of organ that is irradiated
-
Sensitivity of the specific tissue to radiation
-
 |
|
Figure 4.4-6 Wound breakdown after external beam radiation and surgical resection (single arrow). The margins of the irradiated field and subsequent skin changes can also be seen (double arrows).
|
sarcomas is not as well established as that of surgery or radiation.
Promising local control and recurrence rates have been reported for
preoperative chemotherapy combined with radiation and surgery in
certain series. However, limitations in study design, including small
sample size, variation in treatment protocols, tumor type, tumor stage,
and lack of control groups, have made it difficult to draw definitive
conclusions on the efficacy of chemotherapy protocols. Based on
building evidence in the literature, systemic chemotherapy in
combination with local control is used in situations where distant
metastases are likely or already present.
-
Relative indications
-
High-grade extremity sarcomas >5 cm
-
Intermediate-grade extremity sarcomas >10 cm
-
Locally recurrent disease
-
Known metastatic disease
-
Small cell sarcomas of any size (primitive neuroectodermal tumor/Ewing sarcoma, rhabdomyosarcoma)
-
-
Relative contraindications
-
Chemoresistant tumors
-
Poor general health that would not tolerate side effects
-
Low-grade nonmetastatic sarcomas
-
Small nonmetastatic sarcomas
-
potential treatments for soft tissue sarcomas. The two agents that show
the greatest activity are doxorubicin and ifosfamide. There is building
evidence that these agents improve local control and overall survival
in patients with extremity soft tissue sarcomas.
-
Cytotoxic anthracycline antibiotic that exerts its effect on malignant cells through two mechanisms of action:
-
Intercalates between nucleotide bases, blocking DNA synthesis and transcription
-
Interacts with topoisomerase type II, leading to formation of DNA cleavable complexes
-
-
Tumor response rate is dose-dependent.
-
Cardiac toxicity is a serious side effect and can lead to arrhythmias and congestive heart failure.
-
An alkylating agent that exerts its
effects through active metabolites that alkylate, or bind, many
intracellular molecules, including DNA and RNA -
Cytotoxic effect is thought to be secondary to cross-linking of DNA and RNA as well as inhibition of protein synthesis.
-
Tumor response is dose-dependent.
-
Used alone or in combination with doxorubicin
-
Side effects include myelosuppression, nephrotoxicity, and neurotoxicity.
JM, Lopez-Pousa A, Martin J, et al. Phase II trial of first-line
high-dose ifosfamide in advanced soft tissue sarcomas of the adult: a
study of the Spanish Group of Research on Sarcomas (GEIS). Ann Oncol 1999;10(1):123–124.
WG, Harris J, Spiro IJ, et al. Study of neoadjuvant chemotherapy and
radiation therapy in the management of high-risk, high-grade, soft
tissue sarcomas of the extremities and body wall: Radiation Therapy
Oncology Group Trial 9514. J Clin Oncol 2006;24(4):619–625.
PC, Tsokos M, Long L, et al. Adjuvant chemotherapy for the treatment of
advanced pediatric nonrhabdomyosarcoma soft tissue sarcoma: the
National Cancer Institute experience. Pediatr Blood Cancer 2005;45(2):226–227.
B, Davis AM, Turcotte R, et al. Preoperative versus postoperative
radiotherapy in soft-tissue sarcoma of the limbs: a randomised trial. Lancet 2002;359(9325):2235–2241.
SR, Vadhan-Raj S, Papadopolous N, et al. High-dose isofosfamide in bone
and soft tissue sarcomas: results of phase II and pilot studies—dose
response and schedule dependence. J Clin Oncol 1997;15(6):2378–2384.
PW. Preoperative chemotherapy and split-course radiation therapy for
patients with localized soft tissue sarcomas: home run, base hit, or
strike out? J Clin Oncol 2006;24(4):549–551.
Meta-analysis Collaboration. Adjuvant chemotherapy for localised
resectable soft-tissue sarcoma of adults: meta-analysis of individual
data. Lancet 1997;350:1647–1654.
