Rotator Cuff Impingement Syndrome: Diagnosis and Treatment
III – Shoulder Reconstruction > Part B – Evaluation and Treatment of
Shoulder Disorders > 37 – Rotator Cuff Impingement Syndrome:
Diagnosis and Treatment
complaint after back pain encountered by the medical profession. Since
Neer’s description in 1972, subacromial impingement syndrome has become
the most common shoulder diagnosis made by the orthopaedic surgeon.
Despite its frequency, care must be taken to ensure the proper
diagnosis is made and appropriate treatment instituted.
controversial. It is unclear if the spectrum of rotator cuff disease is
a direct result of mechanical impingement or if intrinsic factors lead
to cuff disease and secondarily cause changes within the coracoacromial
arch. Neer believed that the rotator cuff impinges on the overlying CA
arch, leading to repetitive microtrauma. Progressive extrinsic injury
leads to eventual rotator cuff tears. Bigliani et al. showed that
acromial morphology could worsen this extrinsic compression by
narrowing the subacromial space. Acromions were divided into type I
(flat), type II (curved), or type III (hooked). Hooked acromions were
associated with 73% of the rotator cuff tears in their cadaver study.
In a separate cadaver study, Flatow et al. showed that there was
contact between the rotator cuff and acromion. This occurred over the
supraspinatus and was more pronounced with type III acromions.
Extrinsic compression worsens with a decrease in the subacromial space.
This can occur from multiple additional causes such as
acromioclavicular spurs, primary bursal swelling, or a laterally sloped
acromion.
dynamic impingement, may worsen extrinsic compression. The rotator cuff
functions to keep the humeral head centered on the glenoid as the arm
is elevated. Several studies have shown that with an injured or
weakened rotator cuff, the humeral head moves superiorly abutting the
coracoacromial arch. Restoration of rotator cuff strength and function
should decrease this dynamic compression.
more important in the development of rotator cuff pathology. Ogata and
Uhthoff have described primary degenerative tendinopathy involving the
rotator cuff and suggested that this may lead to tendon tears. Several
studies have shown decreased vascularity in the area of the rotator
cuff where tears are commonly seen. One study showed a differential
pattern of vascularity between the bursal and articular side of the
rotator cuff. The articular surface showed a decrease in blood supply
relative to the bursal surface. This may help to explain why most
partial rotator cuff tears occur on the articular side of the cuff. If
extrinsic compression were the only or main cause of rotator cuff
tears, it would stand to reason that the tears would be predominately
bursal in origin. Although there is currently no consensus, it is
probable that a combination of these factors leads to the development
of rotator cuff disease.
stages consisted of increasing damage to the rotator cuff and appeared
age dependent. Further studies using MRI and ultrasound have confirmed
an increasing rate of rotator cuff disease as patients age. Stage I
consisted of edema and hemorrhage of the cuff and bursa. Stage II
consisted of fibrosis and tendonitis of the rotator cuff, whereas stage
III disease consisted of rotator cuff tearing. In practice, impingement
can be classified according to the status of the rotator cuff. For
those patients with intact rotator cuffs, nonoperative measures are
exhausted before surgery is indicated. In patients with rotator cuff
tears, surgical intervention should
be
discussed sooner, especially in patients younger than 65 years of age.
In these patients, prolonged nonoperative therapy may lead to
irreversible changes in the rotator cuff. These include muscle atrophy,
fatty degeneration, changes in tendon morphology, and degenerative
joint changes.
with a thorough history. Pain is the most common symptom. It is often
described as a dull ache of the anterolateral shoulder radiating to the
deltoid insertion. Pain is often worsened by overhead activities or
extension of the arm behind the back. Activities with the arm at the
side are usually pain free. Night pain often awakening the patient from
sleep is a common complaint. Complaints such as stiffness, crepitus, or
instability are less commonly associated with impingement syndrome and
should alert the physician to the possibility of an alternate
diagnosis. Older patients, in particular, should be evaluated for
osteoarthritis. Patients younger than 40 years of age with shoulder
pain often have instability leading to secondary impingement. Women
between the ages of 40 and 60 years, diabetics, and those with thyroid
disorders should be carefully evaluated for adhesive capsulitis.
pain. Pain radiating past the elbow, often associated with complaints
of numbness and tingling, should raise concern about this diagnosis. A
history of pain dependent more on neck than arm position also suggests
a cervical cause. In contrast to patients with impingement syndrome,
patients with cervical disc disease often state that their pain is
better with their arm over their head. Pain into the upper trapezius is
not necessarily related to the cervical spine. It is a common complaint
in patients with shoulder disorders and is secondary to abnormal
shoulder mechanics.
without a specific traumatic event. A recent onset of a new exercise
routine or greater than normal physical activity such as heavy yard
work often is described as the initiating event. Treatments initiated
by the primary physician or patient should be documented. Activity
modifications, medications, injections, and therapy are commonly tried
before seeing the orthopaedic surgeon. The effect of these treatments
is helpful in making the proper diagnosis. For example, a subacromial
injection of cortisone or local anesthetic that relieves the pain is
highly suggestive of impingement syndrome.
including the scapulas, can be examined. The initial evaluation of the
patient should include an examination of the cervical spine. Cervical
spondylosis and radiculopathy often mimic intrinsic shoulder pathology.
The physical exam includes motor and sensory testing of the entire
upper extremity. Specific tests such as the Spurling (extension with
rotation of the neck to the involved side) and Lhermitte (compression
and flexion of the neck) maneuver are performed. Any reproduction of
the patient’s symptoms suggests that the cervical spine is at least
partially involved. It must be remembered that both neck and shoulder
pathology can coexist in the same patient.
wasting, suggestive of a chronic rotator cuff tear or peripheral nerve
lesion, is documented. Range of motion is evaluated by standing behind
the patient. This allows for evaluation of scapular rhythm and winging
as active motion is evaluated. Forward elevation, external rotation in
90 degrees of abduction, external rotation at the side, and internal
rotation are recorded both actively and passively. Although there often
is a painful arc, the motion in patients with impingement syndrome is
usually well preserved. Long-standing cases may show a mild decrease in
motion, especially in internal rotation. A more profound loss of both
active and passive motion in the shoulder suggests the diagnosis of
adhesive capsulitis, assuming there is no significant glenohumeral
arthritis.
Supraspinatus strength is examined using the Jobe test. The patient
resists a downward force after the arm is placed in the plane of the
scapula elevated to shoulder level with the thumb pointed toward the
ground. The infraspinatus is tested with resisted external rotation
with the arms at the side and elbows flexed to 90 degrees. The arms
should be placed in internal rotation at the start of the test to
isolate the infraspinatus. The teres minor is isolated with use of the
horn blower’s test. The arm is brought into 90 degrees of abduction and
neutral rotation. The patient is then asked to rotate the shoulder
externally to 90 degrees with the thumb pointed posteriorly. The
subscapularis is tested either with the lift-off test or abdominal
compression test. Patients with impingement syndrome generally have
preserved strength although testing may elicit pain. This is especially
true with the Jobe test. If there is significant pain, the patient may
appear weak although the rotator cuff is intact.
The Neer and Hawkins tests are most commonly performed. The Neer sign
is performed by elevating the arm in the scapular plane while
stabilizing the scapula. The patient complains of pain as the
supraspinatus tendon impinges on the acromion usually above 70 degrees
of elevation. The Hawkins sign is performed by internally rotating the
arm with the arm in 90 degrees of forward flexion with the elbow flexed
90 degrees.
young patient, instability can cause secondary impingement. The
apprehension test is performed by bringing the arm into 90 degrees of
abduction with the patient supine. Progressive external rotation is
performed, trying to elicit apprehension as the patient feels the
humeral head sliding anteriorly. The relocation test is then performed
by applying a posteriorly directed force on the arm. The test is
positive if there is relief of pain and/or apprehension. If instability
is suspected as the cause of the impingement, the treatment will differ
from that for primary subacromial impingement syndrome. Failure to
appreciate mild instability is a leading cause of failed subacromial
decompressions.
 |
|
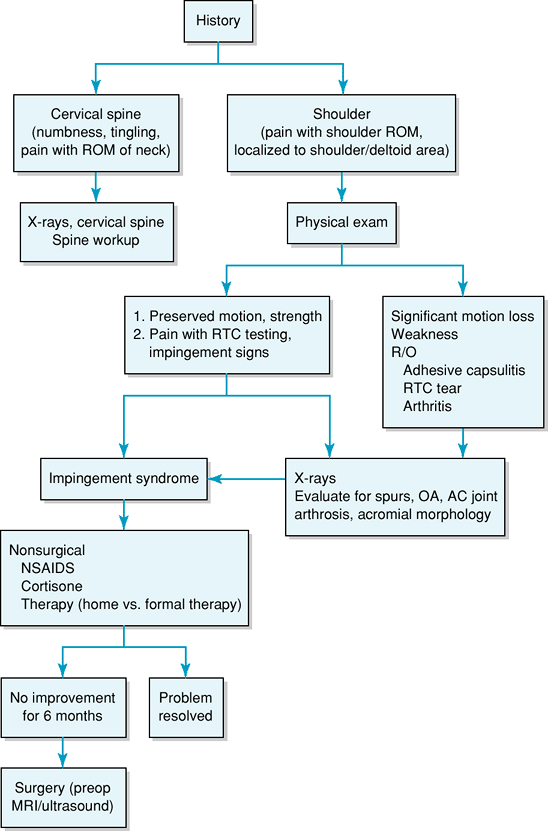
Figure 37-1 Diagnostic workup algorithm.
|
responsible for the pain. The Neer impingement test consists of an
injection of local anesthetic into the subacromial space. If the
patient’s pain is relieved or decreased, it is assumed that the
subacromial space is a source of pain. If an injection of local
anesthetic and/or cortisone into the subacromial space does not relieve
a patient’s symptoms, the diagnosis of impingement syndrome is
questioned. In this setting, injections into the acromioclavicular
joint or into the glenohumeral joint are helpful in evaluating other
possible sources of pain.
anteroposterior (AP) in internal rotation, scapular AP in external
rotation, axillary, and supraspinatus outlet view. These films may
reveal other causes of shoulder pain such as calcific tendonitis,
osteoarthrosis of the glenohumeral or acromioclavicular joint, or an os
acromiale. The supraspinatus outlet view is a lateral view with a
10-degree caudal tilt, affording a better view of acromial morphology.
Typically there will be few abnormalities found in a patient with
isolated subacromial impingement. Acromial spurring, sclerosis of the
greater tuberosity, and subchondral cysts may be present.
and ultrasound. These tests are often ordered to evaluate for tears of
the rotator cuff. MRI gives the most additional information, allowing
for evaluation of the labrum, AC joint, and biceps tendon. In
well-trained hands, ultrasound is an inexpensive alternative for
evaluation of the cuff. Although not
needed
for the diagnosis and management of impingement syndrome, additional
imaging is often obtained if nonoperative measures fail (Fig. 37-1).
successful for subacromial impingement. Success rates of 70% to 80%
have been seen across several studies. Options include activity
modification, nonsteroidal anti-inflammatory drugs (NSAIDs),
rehabilitation exercises, cortisone injections, and modalities such as
ultrasound. Although these options are well established, few controlled
trials have been done proving their efficacy.
properties, are an integral part of most nonsurgical protocols. With
the recent concern about cardiovascular side effects with these
medications, it is advisable to try to limit their use to short periods
(1 to 3 months) at the smallest effective dose. Acetaminophen can be
tried as the first line of medication. If the pain is not well
controlled with these medications, the use of cortisone injections into
the subacromial space is indicated. Because of their deleterious
effects on normal tissue, cortisone injections are used judiciously. In
general, cortisone should be limited to three injections spaced at
least 3 months apart. Steroid injections are particularly helpful in
patients experiencing significant night pain.
therapy. After rest and medication have reduced the acute inflammation
and pain, stretching and strengthening exercises can begin. The goal of
stretching exercises is to restore a full range of motion through long,
slow stretches with minimal pain. After range of motion is improved,
strengthening of the rotator cuff and surrounding musculature can
begin. Opinions differ as to the need for supervision by a physical
therapist. Physical therapists may help those who need more
encouragement and guidance. They also have the ability to use
modalities such as ultrasound, phonophoresis, and iontophoresis to
improve pain control. Despite these potential advantages, studies have
shown no difference between supervised and unsupervised therapy.
despite appropriate nonsurgical treatment, operative intervention is
indicated. Surgery consists of an anterior acromioplasty, bursectomy,
and resection of the coracoacromial ligament. Routine resection of the
distal clavicle is not recommended. Distal clavicle resection is
indicated for patients with tenderness on exam or in those with
inferior spurring of the AC joint that is thought to aggravate
impingement. The goal of a subacromial decompression is to remove
sufficient bone from the anterolateral acromion to create a type I, or
flat, acromion. Similar results have been obtained using both open and
arthroscopic techniques. Good to excellent results are seen in
approximately 90% of patients with either method. The open
acromioplasty remains an effective operation and is less likely to
result in insufficient bone removal. An arthroscopic decompression
allows inspection of the glenohumeral joint for additional pathology
and decreases iatrogenic injury to the deltoid. The decision ultimately
depends on surgeon experience. Postoperatively, NSAIDs and therapy are
important to reduce residual inflammation and maximize return of
function. The stretching and strengthening exercises used for
nonoperative treatment are instituted in the early postoperative
period. These should commence in the first few days after surgery.
made by the practicing physician. Proper diagnosis depends on a
thorough history and physical exam. Nonsurgical management is extremely
successful and consists of both relief of inflammation and
rehabilitation. An arthroscopic or open acromioplasty is performed only
after failure of a 3-to 6-month course of nonsurgical treatment.
S, Uhthoff HK. Acromial enthesopathy and rotator cuff tear: a
radiologic and histologic postmortem investigation of the
coracoacromial arch. Clin Orthop. 1990;254:39–48.
