Radial Head Fractures: Open Reduction Internal Fixation
coincided with an increasing appreciation of the important
contributions of the radial head to the stability of the elbow and
forearm (2,3,4,5). As a result, and also due to the inadequacy and problems associated with the silicone rubber radial-head prostheses (2,6,7,8), it became popular to attempt to save even the most complex fracture of the radial head by operative fixation (9).
Early reports of open reduction and internal fixation (ORIF) of radial
head fractures were very positive, perhaps due to the prevalence of
isolated, partial, radial-head fractures for which good results would
be expected (10,11,12,13,14,15).
Some subsequent reports have stated that complex fractures of the
radial head are prone to early failure, nonunion, and poor forearm
rotation after operative fixation (9,16,17,18).
Combined with increased availability and use of more-predictable metal
radial-head prosthesis for complex fractures of the radial head (19,20), the role of ORIF is being redefined.
head was the only commonly used treatment for fractures of the radial
head (21,22), and
decision making was simple: excise or do not excise. If excision was
elected, the entire head was resected because the results of partial
head excision were usually poor (23,24,25,26).
In the 1980s, with the advent of techniques and implants for the
fixation of small fractures and articular fracture fragments, ORIF
became a more viable option (1).
of proximal migration of the radius after excision of isolated
radial-head fractures have long been a source of debate (24).
On the other hand, there is agreement on the value of retaining the
fractured radial head amidst complex combined injury with instability
of the forearm or elbow, such as an Essex-Lopresti injury (22,27)
(radial head fracture and rupture of the interosseous ligament of the
forearm) or a terrible triad injury (posterior dislocation of the elbow
with fractures of the radial head and coronoid process) (28,29,30,31). The radial head is increasingly recognized as an important stabilizer of the forearm and elbow (2,3,4,5,22,28,29,30,31,32,33).
Some authors even suggest that ulnohumeral arthrosis after elbow
fracture-dislocation is accelerated in the absence of a radial head (34).
focused primarily on isolated fractures involving only part of the
radial head (10,11,12,13,14,15).
The good results in these series, the popularity of the new techniques
for internal fixation of small fractures, and the increasing
recognition of the importance of the radial head led many to emphasize
the importance of preserving the native radial head. Unfortunately,
subsequent papers have reported unpredictable results after internal
fixation of more complex radial-head fractures (9,16,17,18), particularly very comminuted fractures with greater than three articular fragments (9).
focused on deciding whether to use fixation or prosthetic replacement
for radial head fractures associated with forearm and/or elbow
instability. Problems related to the articulation of a metal
radial-head implant with native capitular cartilage have been reported,
but the majority of these problems are related to an oversized
prosthesis (35). In general, results of prosthetic replacement of the radial head have been quite favorable (19,20), making it a useful alternative to ORIF.
rotation, compromise the stability of the forearm or elbow, and in
relatively rare cases, cause radiocapitellar arthrosis. The primary
goal of treatment is to ensure forearm rotation. Incongruity of the
radial head in the proximal radioulnar joint causes loss of rotation.
Painful arthrosis of the proximal radioulnar joint is not usually
observed. Although some studies dispute these observations, my training
and experience lead me to conclude that partial fractures of the radial
head that do not restrict forearm rotation are usually consistent with
excellent elbow and forearm function no matter the radiographic
appearance (13).
via implant prominence, scarring, or heterotopic bone formation. Some
patients with healed and apparently well-aligned fractures of the
radial head after operative fixation have substantial loss of motion
that is not attributable to implant prominence (9).
This result may be due to articular incongruities, but based on
observations of my own patients and similar observations noted in the
literature (36), I suspect that many fractures
of the radial head are impacted in a way that expands the diameter of
the radial head. Healing of the radial head with this deformity might
contribute to loss of forearm motion. Loss of ulnohumeral motion is
usually related to capsular contracture and only rarely related to
interference from displaced fracture fragments.
the initial treatment must include restoration of contact between the
radial head and capitulum to prevent marked proximal migration of the
radius. Although restoration of the radial head does not guarantee good
function in this complex injury, failure to restore the radial head
will result in chronic forearm instability that currently has no good
solution (39). Attempts to save the radial head
at all costs might be unwise in this setting. For instance, many
chronic Essex-Lopresti lesions result from failure of attempted
operative fixation of the radial head. In this circumstance, where the
radial head is essential, tenuous fixation of a complex radial-head
fracture may be inadequate and prosthetic replacement might be
preferable.
fracture-dislocations. Particularly for unstable elbow injuries, such
as the terrible triad pattern of elbow fracture-dislocation (29),
secure reconstruction of the radial head is requisite. If the fracture
is too complex to achieve reconstruction, then radial head replacement
may be preferable. Many partial radial-head
fractures are difficult or impossible to repair securely and should also be considered for prosthetic replacement.
little data support them. The oft-repeated 2-mm limit for acceptable
articular alignment, derived from Knirk and Jupiter’s study of
intra-articular distal radius fractures (42),
may not apply to the radiocapitellar joint. Although displaced
fractures of the radial head are extremely common, radiocapitellar
arthritis is an uncommon presenting complaint about which very little
has been published (43).
They rarely block motion, cause pain, or lead to arthrosis. Although
radiographic criteria for operative treatment have been suggested, they
lack scientific support.
treatment of an isolated partial fracture of the radial head is a
fracture that blocks forearm rotation. Because it can be difficult to
assess forearm rotation in the setting of an acute, painful, elbow
hemarthrosis, it can be useful to aspirate the hemarthrosis and place a
local anesthetic in the elbow joint. Alternatively (perhaps preferably)
if the patient is evaluated in the office at least 4 or 5 days after
injury, the pain is sufficiently relieved to allow a reliable
examination. Without block to motion, crepitation with forearm rotation
does not seem predictive of problems, but this phenomenon deserves
further study.
[a minimum of 75% good results in long-term follow-up as measured
according to a very strict rating scale (45)],
the surgeon should not take too much credit for good elbow function
after operative treatment of isolated partial fractures of the radial
head. In addition, operative treatment provides an opportunity for
several complications and so should be undertaken with care.
slightly displaced are very uncommon (approximately 4% of all
radial-head fractures in an unpublished review of over 300 patients
treated at Massachusetts General Hospital). Among this small group of
patients, blocks to forearm rotation were uncommon. The surgeon should
therefore approach the management of the patient with an isolated
partial fracture of the radial head with the understanding that these
fractures rarely benefit from operative treatment.
fractures that are part of a complex injury pattern is entirely
different than in other cases. Such fractures are usually displaced and
unstable with little or no soft-tissue attachments; occasionally some
fragments are lost. Even a relatively small fracture can make an
important contribution to the stability of the elbow and forearm.
Usually, the anterolateral aspect of the radial head is fractured with
resultant loss of the anterior buttress of the ulnohumeral joint.
for ORIF because the majority of the head remains intact, they can be
very challenging to treat due to fragmentation, the small size of the
fragments, lost fragments, poor bone quality, limited subchondral bone
on the fracture fragments, and metaphyseal comminution and bone loss.
Early failure of fixation of these fractures is potentially
problematic, particularly in an Essex-Lopresti injury or a terrible
triad fracture-dislocation of the elbow. Therefore, many partial-head
fractures associated with complex injuries may be best treated with
prosthetic replacement even though this means removing a substantial
amount of uninjured radial head. ORIF is indicated when stable,
reliable fixation can be achieved.
among patients with posterior olecranon fracture dislocations; the
majority of these candidates are older, osteoporotic women. Some
authors believe that radial head excision is acceptable in these cases
as long as the ulnohumeral joint is stable (46).
In some cases, I have neglected or excised a small, partial,
radial-head fracture in these patients, with good results, but favor
retaining the
stability
and support of radiocapitellar contact in most cases. I believe that a
low-energy injury in an older patient is a relatively favorable
situation in which to consider neglecting or resecting the radial head;
however, retention of the radial head, either with operative fixation
or prosthetic replacement, would be preferable in healthy, active
patients injured in high-energy activities.
are almost always part of a more complex injury. Some older, low-demand
patients are best treated with resection of the radial head without
prosthetic replacement but only if the elbow and forearm are stable.
The rare young patient with an isolated injury involving the entire
radial head can also be considered for excision without prosthetic
replacement, but retention of the radial head may improve the function
and durability of the elbow, particularly with forceful use.
elbow with associated fracture involving the entire head of the radius,
ORIF should only be considered a viable option if stable, reliable
fixation can be achieved. There is a definite risk of both early
failure and later nonunion, both of which can contribute to recurrent
instability. Other factors, such as loss of fragments, metaphyseal bone
loss, impaction and deformity of fragments (36),
and the size and quality of the fracture fragments may make ORIF a less
predictable choice. In particular, if more than three articular
fragments are presented, the rates of early failure, nonunion, and poor
forearm rotation may be unacceptable (9). The
optimal fracture for ORIF will have three or fewer articular fragments
without impaction or deformity, each of sufficient size and bone
quality to accept screw fixation, and little or no metaphyseal bone
loss.
pattern of injury. In my experience in both patient care and research,
fractures of the radial head can occur either in isolation or in
association with one of several discrete injury patterns, including (a)
fracture of the radial head and rupture of the interosseous ligament of
the forearm (Essex-Lopresti and variants) (Fig. 9.1A) (27,37,38); (b) fracture of the radial head and rupture of the medial collateral-ligament complex and/or fracture of the capitulum (see Fig. 9.1B); (c) fracture of the radial head and posterior dislocation of the elbow (47,48); (d) posterior dislocation of the elbow with fractures of the radial head and coronoid process (18,29,48) [the so-called terrible triad (49)] (Fig. 9.1C); and (e) posterior olecranon fracture-dislocations (posterior Monteggia pattern injuries) (see Fig. 9.1D) (28,50,51,52). As has been emphasized by Davidson et al (36),
complex fractures of the radial head are nearly always associated with
a complex injury. Intraoperative evidence of ligament injury should
always be sought (53), particularly if simple excision is being considered (22).
are very useful for characterizing the fracture and planning surgery.
When facing a complex injury pattern, the surgeon should always be
prepared for prosthetic replacement of the radial head in case
operative fixation proves unfeasible or unwise (see Fig. 9.2C,D).
the patient supine on the operating table, under general or regional
anesthesia, with the arm supported on a hand table. To improve access
to the elbow, a sterile tourniquet is preferred to a nonsterile one.
Posterior olecranon fracture-dislocations are often best treated in a
lateral decubitus position with the arm supported over a bolster.
 |
|
Figure 9.1.
When evaluating a fracture of the radial head, one should consider the possibility of one of the following complex injury patterns: (A) an Essex-Lopresti lesion or variant; (B) fracture of the radial head and medial collateral-ligament injury; (C) an elbow fracture-dislocation; and (D) an olecranon fracture-dislocation. (Copyright © David Ring, MD.) |
 |
|
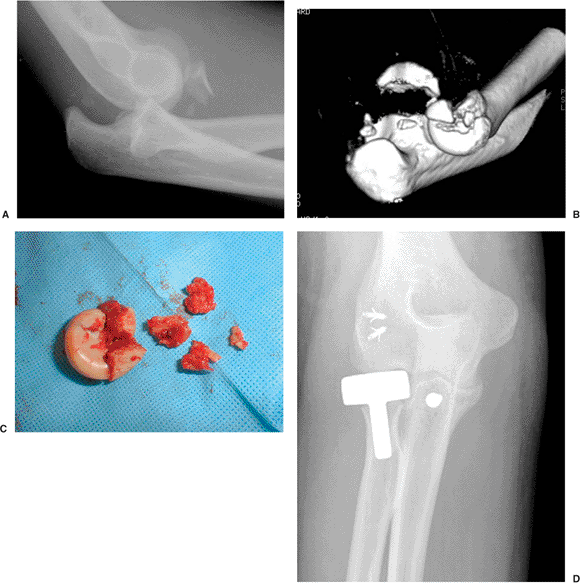
Figure 9.2. CT can help characterize a fracture of the radial head. A.
This radiograph of a terrible triad fracture-dislocation suggests that the radial head fracture is partial and relatively small. B. A CT scan demonstrates that at least one half of the radial head is involved and the fracture has created complex comminution. C. The fragments were not repairable. D. Because this portion of the radial head is critical to stability in the setting of a terrible triad injury, a metal prosthesis was used with a good result. (Copyright © David Ring, MD.) |
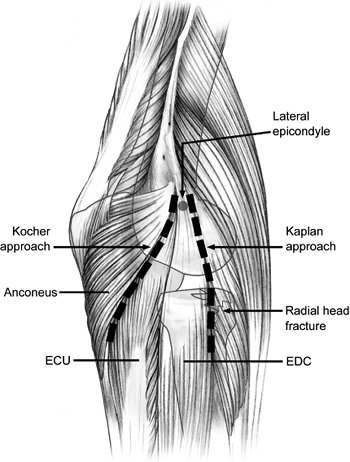
of the radial head is between the anconeus and extensor carpi ulnaris
(Kocher exposure) (Fig. 9.3) (54,55).
This interval is fairly easy to define intraoperatively. It represents
the most posterior interval and provides good access to fragments of
the radial head that displace posteriorly. It also provides greater
protection to the posterior interosseous nerve. However, attention must
be paid to protecting the lateral collateral-ligament complex. The
anconeus should not be elevated posteriorly, and the elbow capsule and
annular ligament should be incised diagonally, in line with the
posterior margin of the extensor carpi ulnaris (56).
collateral-ligament complex but places the posterior interosseous nerve
at greater risk (22). Some authors recommend identifying the nerve if dissection onto the radial neck is required (22). Kaplan described an interval between the extensor carpi radialis brevis and the extensor digitorum communis (54), whereas Hotchkiss recommends going directly through the extensor digitorum-communis muscle (see Fig. 9.3) (22).
I find these intervals difficult to define precisely based upon
intraoperative observations. A useful technique for choosing a good
interval and protecting the lateral collateral-ligament complex was
described by Hotchkiss (22): Starting at the
supracondylar ridge of the distal humerus, if one incises the origin of
the extensor carpi radialis, elevates it, and incises the underlying
elbow capsule, it is then possible to see the capitulum and radial
head. The interval for more distal dissection should be just anterior
to a line bisecting the radial head in the anteroposterior (AP) plane.
fractures that merit operative treatment are associated with
fracture-dislocations of the elbow. In this context, exposure is
greatly facilitated by the associated capsuloligamentous and muscle
injury (9,28,57).
When the elbow has dislocated, the lateral collateral ligament has
ruptured and the injury always occurs [or, according to some authors (57),
nearly always occurs] as an avulsion from the lateral epicondyle. Along
with a variable amount of muscle avulsion from the lateral epicondyle (57,58,59,60,61), these injuries leave a relatively bare epicondyle (Fig. 9.4). A frequently found split in the common extensor muscle can be developed more distally.
 |
|
Figure 9.3.
Several, lateral, muscle intervals have been described. The most commonly used interval is that of Kocher (between the anconeus and extensor carpi ulnaris). This interval is particularly good for retrieving posterior fracture fragments. The relatively anterior Kaplan interval places the lateral collateral ligament at less risk and provides good exposure to the more anterolateral aspects of the radial head that are typically fractured, but it puts the posterior interosseous nerve at greater risk. |
 |
|
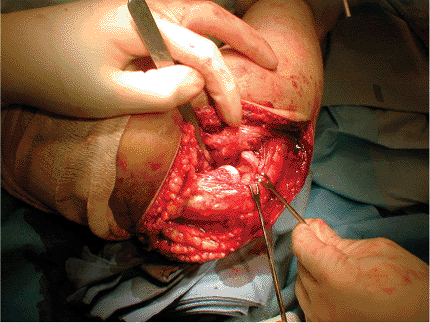
Figure 9.4.
The vast majority of complex radial-head fractures are associated with an elbow dislocation. Elbow dislocation results in avulsion of the lateral collateral-ligament origin and a variable amount of the common extensor musculature from the lateral epicondyle resulting in a relatively bare epicondyle. This damage should be used to enhance exposure to the radial head. (Copyright © David Ring, MD.) |
fracture-dislocation (posterior Monteggia pattern injury) the radial
head often displaces posteriorly through capsule and muscle. In such
cases, the surgeon will usually extend this posterior injury to
mobilize the olecranon fracture proximally to expose and manipulate the
coronoid fracture through the elbow articulation. This usually provides
adequate access to the radial head as well (Fig. 9.5).
Slight additional dissection between the radius and the ulna is
acceptable because of the usually extensive injury in this region, but
extensive new dissection in this area may increase the risk of proximal
radioulnar synostosis.
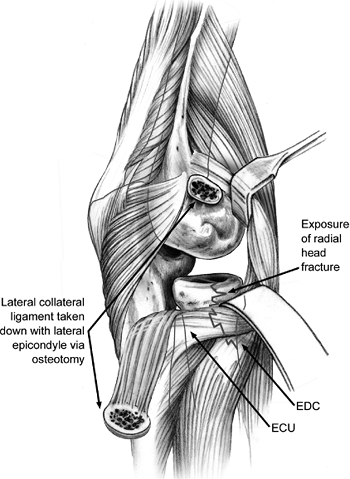
the lateral collateral-ligament complex intact (for instance an
Essex-Lopresti injury), it may be difficult to gain adequate exposure
without releasing the lateral collateral-ligament complex from the
lateral epicondyle. This can be done either by directly incising the
origin of the lateral collateral-ligament complex from bone or by
performing an osteotomy of the lateral epicondyle (Fig. 9.6) (1,11,17,62,63).
In either case, a secure repair and avoidance of varus stress (shoulder
abduction) in the early postoperative period are important.
neck, directly adjacent to the neck in some patients and separated by
some muscle fibers in others. It is at risk during ORIF. It can be
protected by pronating the forearm, by dissecting the supinator bluntly
with or without identifying the nerve, and by avoiding the use of
retractors placed over the radial neck (22). A
recent study showed that, with pronation, the posterior interosseous
nerve is an average of 3.8 cm distal to the articular surface of the
radius (64).
the Herbert screw) can be used. Standard screws placed in the articular
area of the radial head should be countersunk below the articular
surface. Some small fragments can only be repaired with small K wires.
Threaded wires are usually used because of the tendency for smooth
wires to migrate and potentially travel to various parts
of the body (65). Absorbable pins and screws are being developed for similar uses (66,67) but are still somewhat brittle and associated with an inflammatory response.
 |
|
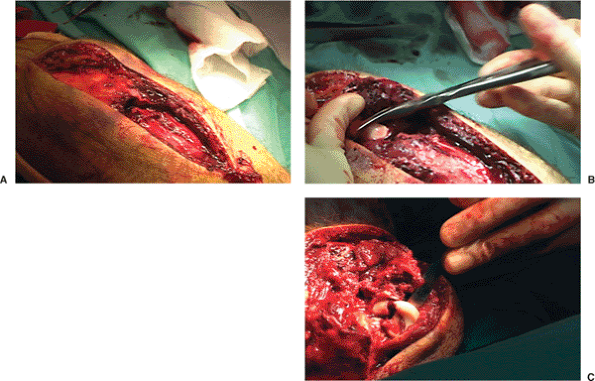
Figure 9.5. A.
Posterior olecranon fracture-dislocations (very proximal, posterior, Monteggia injuries) create posterior muscle injury that can be used to expose a fracture of the radial head. B. Mobilizing the olecranon fracture fragment proximally as one would do for an olecranon osteotomy exposure of the distal humerus provides access to the joint. C. Recreating the posterior subluxation of the radial head that occurred at the time of injury provides good exposure to the radial head. (Copyright © David Ring, MD.) |
 |
|
Figure 9.6.
In the uncommon circumstance that a complex fracture of the radial head is not associated with injury to the lateral collateral ligament (e.g., Essex-Lopresti injury), it may be necessary to take down the origin of the ligament to obtain satisfactory exposure of the radial head. This can be done by releasing the soft-tissue attachment or via an osteotomy of the lateral epicondyle. |
the entire head. Plate types include T-shaped and L-shaped plates with
standard screws, small (condylar) blade plates, and new plates designed
specifically for the radial head (many of which incorporate angular
stable screws that thread directly into the plate). The use of plates
that are placed within the radial head or countersunk into the
articular surface has also been described (62).
the proximal ulna or the distal humerus. Implants can be placed on the
small nonarticular area without impinging during motion, but implants
placed in other areas must be countersunk below the articular surface.
By simple visual inspection, the articular surface of the radial head
with the proximal ulna can be difficult to distinguish from the
nonarticular surface, particularly when the radial head is fractured.
Smith and Hotchkiss (68) characterized the
nonarticular portion of the radial head based upon reference points
made in the operative wound. If the radial head is bisected in the
anterior-posterior plane with the elbow in neutral, full pronation, and
full supination, the safe zone can be defined as half the distance
between the middle and posterior marks and half the distance plus a few
millimeters (roughly two thirds the distance) between the middle and
anterior marks (68). Caputo et al (69)
have approximated this zone according to landmarks on the distal radius
as lying between the radial styloid and Lister’s tubercle. In one
study, small plates were applied to the radial head with the forearm in
neutral rotation, and the results show that the procedure did not
result in impingement (70).
or Kaplan exposure is used, with the surgeon taking care to protect the
uninjured, lateral collateral-ligament complex. In these isolated
injuries, the anterolateral aspect of the radial head is usually
fractured, and the process to expose through these intervals is
straightforward (Fig. 9.7A,B). The fracture is usually only slightly displaced. In fact, it is usually impacted into a stable position (see Fig. 9.7D). The periosteum is
usually intact over the metaphyseal fracture line. Every attempt is
made to preserve this inherent stability by using a bone tamp to
reposition the fragment (see Fig. 9.7E,F). After the fragments have been realigned, one or two small screws are used to secure each fragment.
|
Figure 9.7. ORIF of a isolated fracture of the radial head. A. This impacted partial-head fracture blocked forearm rotation. B. There were no other apparent injuries. C. A lateral skin incision in line with the muscle interval is used. D.
In this case, the interval between the anconeus and the extensor carpi ulnaris was used, and the elbow capsule and annular ligament were incised anterior to the lateral collateral ligament. E. This patient had two large impact fragments. The periosteum was intact and the position of the fragments was quite stable. F. A bone tamp was used to realign the fragments without disrupting soft-tissue attachment and to attempt to preserve some of the inherent stability of this impacted fracture. G. A 1.5-mm drill was used initially. H. Careful screw-size measurement with a depth gauge is important. I. To provide interfragmentary compression, the near hole is overdrilled with a 2.0-mm drill. I often skip this step in poor-quality bone. J. A countersink is used to diminish screw prominence. K. It is particularly important to place the screw below the articular surface when it is within the area that articulates with the proximal ulna. L. The annular-ligament elbow capsule is sutured. M. In most cases, I suture this along with overlying fascia. N. In this patient, a subcuticular suture is used. O. Steri-Strips were applied. (Copyright © David Ring, MD.) |
elbow fracture-dislocation is straightforward because of associated
capsuloligamentous and muscle injury. In the absence of this
soft-tissue injury, most partial radial-head fractures can be treated
through a Kocher or Kaplan exposure. Reduction and screw fixation is
usually used, but if any metaphyseal bone loss or comminution is found,
a plate may be preferable (Fig. 9.8).
excellent exposure is requisite, and the surgeon should not hesitate to
release the origin of the lateral collateral-ligament complex to
improve exposure in the unusual situation where it is not injured (Fig. 9.9).
In many cases, the surgeon will remove the fracture fragments from the
wound and reassemble them outside the body (on the “back table”). The
sacrifice of any small, residual, capsular attachments made in this
type of reassembly seems an acceptable trade-off to achieve the goal of
stable, anatomical fixation. This reconstructed radial head is then
secured to the radial neck with a plate. Consideration should be given
to applying bone graft to metaphyseal defects; sufficient bone can
often be obtained from the lateral epicondyle or olecranon.
 |
|
Figure 9.8. Partial radial-head fractures associated with relatively complex injuries are usually displaced and instable. A. This is a terrible triad injury with the coronoid fragment visible anterior to the coronoid. B. A lateral radiograph after manipulative reduction shows both coronoid and radial head fragments. C. The radial head fracture was a single small fragment that was repairable with a screw. D.
The coronoid was repaired with sutures through drill holes, and the lateral collateral ligament was reattached to the lateral epicondyle. (Copyright © David Ring, MD.) |
 |
|
Figure 9.9. Complex fractures of the entire head are very challenging to repair. A. This patient received a fracture-dislocation while playing hockey. The majority of the radial head is dislocated posteriorly. B. The complexity of the fracture is apparent on the AP radiograph. C.
A 2.0-mm blade plate and screws were used to repair the fracture, which consisted of two large head fragments and substantial metaphyseal comminution. D. The lateral collateral ligament was also repaired. (Copyright © David Ring, MD.) |
I recently reviewed the results of ORIF of a fracture of the radial
head in 56 patients. The 15 patients with isolated partial fractures of
the radial head experienced excellent results. Among the 15 patients
with displaced fractures of the radial head as part of a complex
injury, 4 (27%) recovered fewer than 100 degrees of forearm rotation,
and the results were considered unsatisfactory.
Thirteen
of the 14 (93%) patients with Mason type 3, comminuted, radial-head
fractures comprised of more than three articular fragments had
unsatisfactory results. Three had early failure of fixation, and so
required radial head excision; six had painful nonunions treated with
excision; four had 70 or fewer degrees of forearm rotation. In the 12
patients with a type 3 fracture in which the radial head was split into
two or three simple fragments, no one experienced early failures, two
had nonunion, and all achieved an arc of forearm rotation of 100 or
more degrees.
active exercises as soon as possible after injury and surgery.
Furthermore, elbow stability is enhanced by early, active, elbow
motion. For these reasons, the goal of surgery should be to create a
situation stable enough to allow active motion after a very short
period of comfortable immobilization.
shoulder abduction should be avoided for approximately 6 weeks
(so-called varus stress precautions). I have not found hinged braces
nor continuous passive motion useful or worth the added expense, and no
data are available to support their use.
interosseous nerve during ORIF of a radial head fracture is unusual.
This complication is most commonly experienced as a palsy related to
retraction or exposure and resolves over weeks to months. To limit the
potential for this complication, retractors should not be placed around
the radial neck, the forearm should be pronated during exposure of the
radial neck, and when relatively distal dissection and internal
fixation are needed, particularly when a more anterior muscle interval
is used for exposure, the nerve should be identified and protected.
leading to posterolateral, rotatory, elbow instability, is an uncommon
complication related to injury or inadequate repair of the lateral
collateral-ligament complex. Awareness of this potential complication
and the anatomic landmarks used to prevent it should help limit its
occurrence. This complication is treated by reconstruction of the
lateral collateral-ligament complex (71).
to the hemarthrosis and perhaps inadequate early movement of the elbow.
This could be exacerbated by the trauma of the operative dissection,
particularly if the fixation achieved was tenuous and the surgeon opted
to immobilize the elbow and forearm. Heterotopic ossification, usually
in the form of anterior heterotopic bone that blocks flexion or a
proximal radioulnar synostosis that blocks forearm rotation, is also a
risk of operative treatment. Stiffness, with or without heterotopic
bone, is treated with exercises, dynamic or static-progressive
splinting, or operative release (72).
In a recent series, 3 of 14 fractures involving the entire radial head
and more than three articular fragments had fixation failure within the
first month (9). Because it can contribute to
instability of the forearm or elbow, unstable or unpredictable fixation
is undesirable, and such fractures should probably be treated with
prosthetic replacement.
(including 2 of 12 fractures with three or fewer fragments and 6 of 14
fractures with more than three articular fragments) were classified as
nonunions.
performed to improve forearm rotation and not for painful arthrosis of
the radiocapitellar joint (73,74). Incongruity of the
proximal radioulnar joint presents as stiffness rather than pain or
arthrosis, and incongruity of the radiocapitellar joint inconsistently
and unpredictably leads to radiocapitellar arthrosis, which seems to be
an uncommon problem.
 |
|
Figure 9.10. Early failure of fixation is common a complex fracture of the radial head is treated. A. This fracture of the entire head created several small fragments. B. There was an associated elbow dislocation. C. The radial head was repaired with a plate and screws. D.
Within 3 weeks, some of the screws were loose and a few fragments had escaped from the fixation. There was crepitation and a block to forearm rotation. E. The radial head was excised. F. The elbow remained stable and the elbow regained good function; however, it would be unwise to go without radiocapitular contact if there was also a coronoid fracture. (Copyright © David Ring, MD.) |
 |
|
Figure 9.11. Nonunion is a frequent complication of complex fractures of the entire head of the radius. A. After reduction of fracture-dislocation of the elbow, a fracture of the entire head of the radius is apparent. B. The elbow remains well aligned. C. Operative fixation with a plate and screws was performed. D. The lateral collateral ligament was reattached to the epicondyle with sutures through drill holes. E. Six months later, the plate is broken and the fracture remains a nonunion. F. The patient has nearly full forearm rotation with crepitation and some pain. (Copyright © David Ring, MD.)
|
 |
|
Figure 9.12.
Partial radial-head fractures can also fail to heal. This seems to be more common in association with complex injury patterns and metaphyseal bone loss. (Copyright © David Ring, MD.) |
RS, Morrey BF, Melberg MW, et al. Inflammatory arthritis after failure
of silicone rubber replacement of the radial head. J Bone Joint Surg 1994;76B:78–81.
JK, Werier J, MacDermid JC, et al. Arthroplasty with a metal radial
head for unreconstructable fractures of the radial head. J Bone Joint Surg 2001;83:1201–1211.
JO, Ovesen J, Gundorf CE. The stability of the elbow following excision
of the radial head and transection of the annular ligament. Arch Orthop Trauma Surg 1987;106:248–250.
J, Romanillos O, Garay EG. Results of acute excision of the radial head
in elbow radial head fracture-dislocations. J Orthop Trauma 2000;14:354–358.
RM, Hotchkiss RN, Slater RR. The use of frozen-allograft radial head
replacement for treatment of established symptomatic proximal
translation of the radius: preliminary experience in five cases. J Hand Surg 1997;22A:269–278.
BF, Schneeberger AG. Anconeus arthroplasty: a new technique for
reconstruction of the radiocapitellar and/or proximal radioulnar joint.
J Bone Joint Surg 2002;84A:1960–1969.
P, Josefsson PO, Hasserius R, et al. Uncomplicated Mason type II and
III fractures of the radial head and neck in adults: a long-term
follow-up study. J Bone Joint Surg 2004;86A:569–574.
PO, Gentz CF, Johnell O, et al. Surgical versus non-surgical treatment
of ligamentous injuries following dislocation of the elbow joint. J Bone Joint Surg 1987;69:605–608.
T, Botte MJ, Abrams RA. Anatomical considerations regarding the
posterior interosseous nerve during posterolateral approaches to the
proximal part of the radius. J Bone Joint Surg 2000;82:809–813.
K, Hirvensalo E, Bostman O, et al. Treatment of radial head fractures
with absorbable polyglycolide pins: a study on the security of fixation
in 38 cases. J Orthop Trauma 1994;8:94–98.
AE, Mazzocca AD, Santoro VM. The nonarticulating portion of the radial
head: anatomic and clinical correlations for internal fixation. J Hand Surg 1998;23:1082–1090.
AD, Nowotarski PJ, Kelso TB, et al. Optimal position for plate fixation
of complex fractures of the proximal radius: a cadaver study. J Orthop Trauma 1998;12:291–293.
