PRINCIPLES FOR RESTORATION OF MUSCLE BALANCE AFTER FOREARM AND HAND PARALYSIS
III – THE HAND > Conditions of Nerves > CHAPTER 54 – PRINCIPLES
FOR RESTORATION OF MUSCLE BALANCE AFTER FOREARM AND HAND PARALYSIS
new insertions. Therapists can help the patient to understand new
patterns of control of the hand. Only the patient can heal the wound
and make the hand work. In this process, one of the most important
variables is the attitude of the patient and her willingness to accept
the disciplines of recovery.
self-employed, has no one to blame but himself for the injury, and has
everything to gain by a speedy return to work. The poorest results
occur when a patient blames someone else for the injury, and is angry
and resentful. This problem is compounded when the patient expects to
obtain a larger financial reward if she has residual disability. The
outlook is still worse if the patient already has a poor self-image,
has been a failure, and now views the injury as a lasting excuse for
continued dependency.
until the patient’s own attitudes and personality have been evaluated
and until he has been brought fully into the picture. Before outlining
any program, the surgeon must encourage patients to talk and present
their own ideas about the future. It is important to know how the
patient has been influenced by others, including family, employer, and
attorney. If the patient has been fortunate enough to see a surgeon
before talking to a lawyer, it may be possible for the surgeon to
recommend a legal advisor who works for a fee rather than for a
proportion of any potential award and who understands the harm that is
done to the process of recovery by delays in the financial settlement
and by suggestions that it may be financially beneficial to the patient to maximize the disability.
with the patient or to get help for the patient to come to terms with
these emotions, enabling the process of rehabilitation to start with a
single-minded and uncomplicated determination to do well.
about the worth of any complex procedure. An operation that would be
obviously indicated for a young manual worker may be inappropriate for
a retired person who can manage what he needs to do with the ranges of
useful motion that remain.
between a simple procedure, using synergistic transfers, and one that
is more complex, requiring the retraining of nonsynergists. Age must be
taken into account. Children and young people can easily bring back
into their consciousness the mechanisms of control of any muscle in the
upper limb and can reprogram their nervous system to make it fit a
different pattern. This may, however, be almost impossible for some
elderly people of even the highest intelligence. Their neuronal
pathways have created “ruts” that have deepened over years of efficient
use. The ruts remain even when new pathways are established, and it is
not good use of mental concentration to direct it constantly away from
useful activity to control the new pathways. For these patients,
synergistic muscles should be used, and only one movement should be
restored at a time.
potential. The first is its capability for creating tension, and the
second is the distance, or excursion, through which its tension may be
sustained.
effect of her proposed actions should move muscles or tendons. I do not
suggest that a mathematical equation needs to be worked out in each
case. However, the surgeon and therapist should use approximate figures
that can inform them whether any given tendon transfer can provide
enough but not too much tension to restore balance and whether a given
muscle is capable of providing the range of motion needed by the joints.
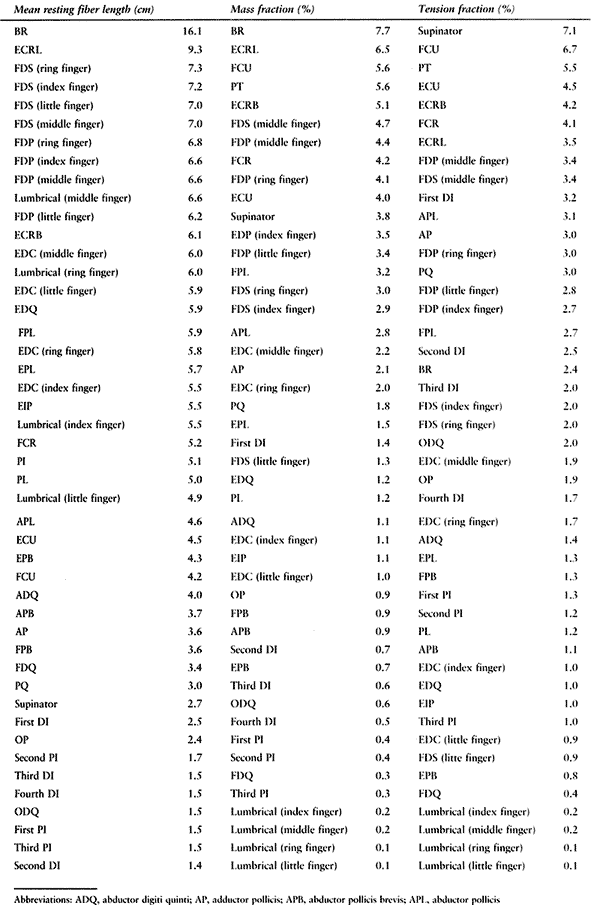
the forearm and hand is given in Fig. 54.1 Figure 54.1
shows the tension capability on the vertical scale and the potential
range of excursion on the horizontal scale. Both of these scales are
relative. The numbers for tension represent each muscle as a percentage
of the combined tensions of all muscles below the elbow. The excursions
are the average of the fiber lengths of each muscle in a medium-sized
forearm or hand, measured while all muscles are in their position of
physiologic rest.
 |
|
Table 54.1. Normal Mean Fiber Lengths, Mass Fractions, and Tension Fractions for Adult Muscles
|
 |
|
Figure 54.1. Using values from Table 54.1,
this diagram shows the relationship between fiber length and tension-producing capability. Some muscle groups are circled for clarity. (See Table 54.1 for a key to abbreviations.) (From data in Brand PW, Beach RB, Thompson DE. Relative Tension and Potential Excursion of Muscles in the Forearm and Hand. J Hand Surg 1981;6:209.) |
use only one half to two thirds of the excursions that are calculated
from the fiber lengths. Muscles whose tendons cross several joints more
often use their whole potential excursion, but even these muscles
manage to work within the central half to two thirds of their potential
most of the time by means of extending one of the joints while allowing
others to flex.
result in the classic pattern of muscle loss for that injury. There are
many patterns of innervation and of injury and disease, and the only
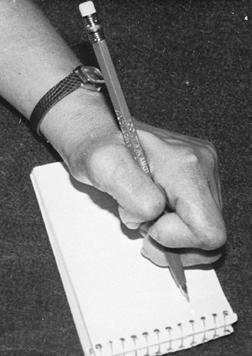
reliable way to evaluate patterns of paralysis is to have a hands-on
clinical test of every movement while the examiner’s fingers feel for
the tightening of the tendons. During surgery, some clinical testing
can be repeated while the tendons are exposed if the patient is awake,
or at least a needle electrode should be used to stimulate the muscles
that are about to be used to confirm their vitality, strength, and
potential for excursion.
to lose one grade of strength after transfer. This rule is based on the
Medical Research Council (MRC) system of grading of muscle tension,
which was developed in Britain during World War II and has been widely
used ever since. The grades are 0 to 5; 5 is normal, and 1 is a twitch
without movement of a joint. Three of the grades refer to the ability
of a muscle to oppose gravity: unable to move against gravity, able to
move against gravity, and able to move against gravity and resistance.
Because the effect of
gravity
on muscle varies depending on what limb segment has to be moved, and
because movement against gravity is a very small part of the work of
muscles in the upper limb, the MRC scale gives a much wider spread at
the lower end of the scale. For this and other reasons, Yahr and Beebe
suggested that it would be more reasonable to use a simple percentage
scale in which 100% is normal (3).
Some may prefer to use a scale of 0 to 10, in which 10 is equal to
100%. Grade 1 on the MRC scale is about 5%; 2 is perhaps 10%; 3 is
approximately 25%; 4 is 60% to 70%; and 5 is 100%.
strength (MRC scale) on transfer was never a quantitative statement
but, rather, a warning to expect less tension out of a muscle after it
has been transferred than it had before. However, the basic concept of
loss of strength is wrong. A muscle has the same nerve supply, the same
blood supply, and the same number of sarcomeres after it has been
rerouted as it had before.
transfer. This change is due not to loss of active muscle tension but
to the increased passive drag on the muscle caused by the changed
elastic properties of passive soft tissue. All the soft tissue in and
around a muscle must be lengthened with the muscle as it moves and
exerts an elastic restraint. In the normal situation of a muscle, the
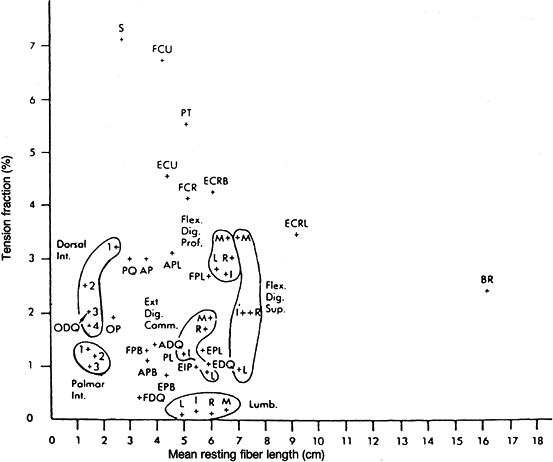
length-tension curve of this tissue is low (Fig. 54.2)
and becomes steep only toward extremes of movement. After a muscle is
moved to another part of the limb, it becomes surrounded by scar tissue
that binds it to the tissues along the new pathway. Scar tissue has a
short, steep length-tension curve and may severely limit the excursion
of a muscle after transfer. If great care is taken to pass the tendon
through yielding fatty tissue only, without using a large wound of
access, the postoperative scar will bind the tendon only to tissues
that can be easily moved and stretched and will have a low
length-tension curve. If an open wound of access cuts through fascia or
retinaculum, or if bone is scratched or periosteum is cut, the scar may
bind the tendon directly to an immovable structure and the
postoperative range of excursion will be very short. In either case,
the actual tension produced by the muscle is the same as it was before
repositioning. The change is that the tension will be useful only for a
shorter distance on either side of the position in which the muscle and
tendon rested while the wound was healing. When wider excursion is
attempted, part of the energy of the muscle is used in stretching or
attempting to stretch scar tissue.
 |
|
Figure 54.2. A:
Normal paratendinous material is shown. Resting length l requires almost no tension to lengthen up to 100% and then gradual increase until elastic limit, in this case at about 160%. B: Scar tissue replacing the paratendon. Resting length (l) requires tension to lengthen from the start. Elastic limit is between 10% and 20%. If the scar is short, the percentage of lengthening must also be short. |
should be cut in the same wound as a transferred tendon. This is why it
is wise to use only a small wound proximally where the muscle or tendon
is to change direction and only a small wound distally where the tendon
is to be attached. The tendon should be tunneled between the two
incisions with no open wound. First detach the tendon from its original
site of insertion. After the tendon has been freed from other tissues,
if necessary, pull it out through the proximal incision. Then pass
tendon-tunneling forceps from the incision of proposed insertion to the
proximal incision. Open the jaws to receive the tendon end, and
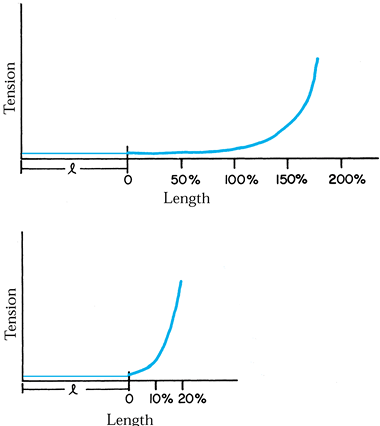
withdraw the forceps distally with the tendon following.
tendon-tunneling forceps should have a smooth, rounded nose, widening
to a viper head, quite close to the nose, and then narrowing back to a
straight shaft as far as the handles. This ensures that any resistance
that is felt during passage will be at or near the advancing end (Fig. 54.3).
It should be possible to open the jaws of the tunneling forceps without
increasing the width of the tunnel. It is essential that the surgeon
know the anatomy of the pathway, having passed forceps of the same
pattern along the chosen path previously, at least in a fresh cadaver
arm, so the feel of the structures is familiar.
 |
|
Figure 54.3.
A tendon tunneler is illustrated. A tendon tunneler must have a smooth blunt nose; its thickest point should be just behind the nose (the “viper” head); and it should be possible to open the jaws and the handles without stretching or tearing the tissues of the tunnel. (From Brand PW. Muscles—The Motors of the Hand. In: Rob C, Smith R, eds. Operative Surgery, 3rd ed. Stoneham, MA: Butterworth Publishers, 1977, with permission.) |
is felt. It must be withdrawn a little and probed until yielding tissue
is found. If a tendon or graft is to be passed
through
the carpal tunnel (often a good path), the nose of the tunneler must be
deep to all tendons and sheaths. The feel of the floor of the tunnel is
hard, irregular, and quite unmistakable; it is safe for the tunneler to
press on the floor. If passage of the tunneler pulls the fingers into
flexion, it means that the tunneler is in among the tendons. It must be
pulled back and rerouted more deeply on the floor. I have never known
adhesions to be a problem in this uninjured skeletal plane; this plane
also is clear of the median nerve.
original muscle it is to replace and if it is not blocked by adhesions,
it may eventually become stronger until it is able to match the
requirements of its new responsibilities.
interference, respond to repeated strong contractions by becoming
stronger. This is accomplished by the addition of sarcomeres in new
muscle fibrils in parallel with the old. The condition for this
hypertrophy is that the weak muscle must actually contract as strongly
as it is able, in phase with its new task. I have seen many transferred
muscles that have become progressively weaker after surgery and have
been regarded as failures. In a few cases, this has been because it has
become rigidly adherent in its new pathway; however, this has often
been because the muscle was never reeducated to contract in phase with
its new action. The hand therapist must not be content to see the
transferred muscle contracting on command or in the sequence of
postoperative exercises that are planned to involve contraction of that
muscle. The muscle must be seen to contract during activities of daily
living or at a work bench where the patient is thinking of work rather
than of the hand.
muscle that has short fibers to replace a muscle that had long fibers.
Assuming that the new muscle will have a shorter excursion, will it
eventually develop longer fibers to match the requirement of its new
task?
well and uses the muscle effectively, the result is gradual lengthening
of the paratendinous soft tissues to maximize available excursion.
However, the number of sarcomeres in series in each fiber remain the
same. The only way to lengthen a muscle fiber is to keep it on stretch
at rest. The only way to do this without shortening the fibers on the
opposite side of the limb is to operate and attach the tendon at a
higher relative tension. Muscle fibers respond to constant tension by
adding sarcomeres in series until normal resting tension is
reestablished.
high tension, because the muscle may respond by involuntary
contractions that cause avulsion at the suture line. The best way to
handle the problem is to make the attachment of a transferred tendon at
a tension just above normal resting tension (for a wrist-moving muscle,
this may be 1 cm of distal pulling of tendon from its relaxed
position), and to place the limb in the postoperative cast in a posture
to relax that tension until the wound has healed, usually in 3 to 4
weeks. After the posture is allowed to return to normal, the
transferred muscle tends to give electromyographic discharges for 1 or
2 weeks until new sarcomeres have grown and relaxed the tension. This
whole process brings the new muscle enough into consciousness to be of
some assistance in the process of reeducation.
moment or torque at a joint. This is the product of the tension of the
muscle and the lever arm or moment arm at the joint. A weak muscle may
produce a high torque at a joint if it crosses the joint far enough
from its axis to have a long lever. In so doing, however, it uses a lot
of excursion and may be able to produce only a limited range of motion
of the joint. A stronger muscle may produce the same torque by crossing
the joint nearer to the axis; it requires less excursion, thus allowing
a wider range of joint motion.
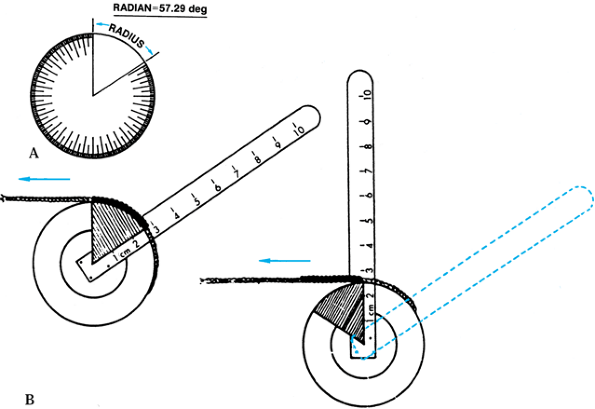
each joint that it crosses, the excursion needed at that joint may be
calculated by multiplying the moment arm in centimeters by the number
of degrees of required motion of the joint measured in radians (1
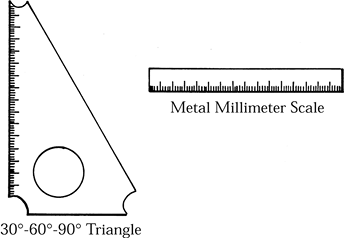
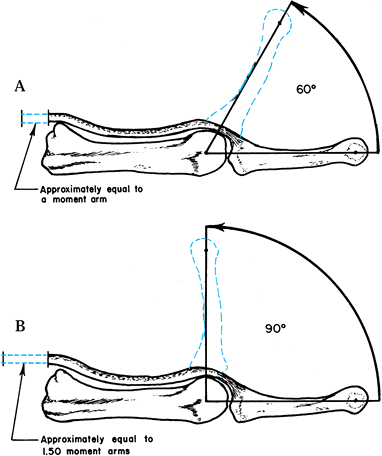
radian = 57.3°) (Fig. 54.4). This also may be
checked at surgery when a tendon is transferred. The joint is moved
through some multiple of 60° (approximately 1 radian), checked by a
geometric triangle (Fig. 54.5), and the
resulting motion of the tendon is measured on a millimeter scale. For
example, after performing a tendon transfer for intrinsic muscle
function
at the metacarpophalangeal joint of the middle finger, the surgeon may
hold the proximal part of the tendon, pulling it gently, while he
flexes the metacarpophalangeal joint through 90° (1.5 radians). If the
tendon moves 15 mm, it is lying 10 mm in front of the axis of the
metacarpophalangeal joint. By doing this, the surgeon is able to make
sure that the tendon is positioned correctly. If, with the same
metacarpophalangeal angular motion, the tendon moves only 8 mm, the
surgeon has inadvertently passed the tendon behind the metacarpal
ligament rather than in front of it; in that case, the tendon will be a
weak metacarpophalangeal flexor unless it is rerouted (Fig. 54.6).
 |
|
Figure 54.4. A: A radian is shown. The length of a radius, measured on the circumference, is joined to the center by two radii. B:
The way in which the lengthwise movement of a tendon may be used to measure the moment arm of a joint. If the joint moves 57.29°, the length of rope that runs off the pulley must be equal to its moment arm at the joint (i.e., radius of pulley). (From Brand PW. Clinical Mechanics of the Hand. St. Louis: CV Mosby, 1985, with permission.) |
 |
|
Figure 54.5.
A 30° to 60° to 90° triangle. The corners are cut off to allow the triangle to be tucked into web spaces, where the actual joint axis is deep in tissue. (From Brand PW. Clinical Mechanics of the Hand. St. Louis: CV Mosby, 1985, with permission.) |
 |
|
Figure 54.6. A: For 60° of joint movement, tendon movement is approximately equal to a moment arm. B: For 90° of joint movement, the tendon moves a distance approximately equal to 1.5 moment arms. (From Brand PW. Clinical Mechanics of the Hand. St. Louis: CV Mosby, 1985, with permission.)
|
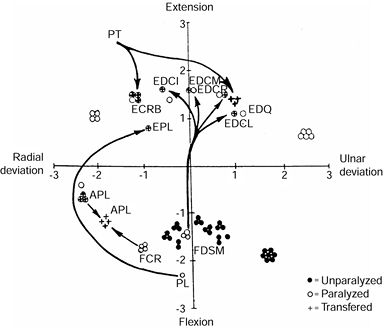
section of the wrist, based on mechanics rather than anatomy. It shows
the relation of each tendon to the axes of flexion and extension, and
of radioulnar deviation of the wrist. The number of dots marking each
tendon indicates the tension fraction of the muscle. It is possible to
calculate the torque available for each movement of the wrist by
multiplying the available tension by the measured distance from the
relevant axis. While planning tendon transfers, it may be good to
sketch
diagrams like Fig. 54.7 and Fig. 54.8 to demonstrate the new balance that will be achieved after paralysis and after tendon transfers.
 |
|
Figure 54.7.
This is not an anatomic diagram; it is a simplified mechanical statement of the capability of each muscle to affect the wrist joint. The positions of the tendons in relation to the axes of flexion and extension and of radioulnar deviation represent their moment arms at the wrist. The number of dots in each cluster is an indication of the tension capability of that muscle-tendon unit rounded off to the nearest whole number. (See Table 54.1 for a key to abbreviations.) (From Brand PW. Clinical Mechanics of the Hand. St. Louis: CV Mosby, 1985, with permisson.) |
 |
|
Figure 54.8.
My preferred pattern of transfer for radial palsy. When normal muscle • is transferred to a site of paralyzed muscle ○, the symbol [circled plus] indicates activation of paralyzed tendon, while the original tendon becomes ○. (See Table 54.1 for a key to abbreviations.) (From Brand PW. Clinical Mechanics of the Hand. St. Louis: CV Mosby, 1985, with permission) |
different tendon insertions, the surgeon must make sure that the
excursion required of each tendon is the same for each range of motion.
Otherwise, the tendon with the bigger moment arm will fall slack and
exert no tension, because it is linked to a tendon that moves less,
having a smaller moment arm. For example, in radial palsy, a pronator
teres attached to both extensor carpi radialis longus and extensor
carpi radialis brevis is effective for extension only through the
extensor carpi radialis longus insertion, which is the least effective
extensor. The pronator should be attached only to the extensor carpi
radialis brevis or to a better balanced pair of insertions.
tissues in close proximity to each other exhibit sharply contrasting
responses to imposed mechanical stress. Tendons, tendon sheaths, and
ligaments respond to repetitive tensile stress by a steep elastic curve
of resistance before 10% of elongation has occurred. Paratenon and
areolar tissue between tendons respond to repetitive tensile stress by
allowing
more
than 100% lengthening with minimal elastic resistance. Skin occupies an
intermediate position, and muscle allows about 100% of passive
lengthening from its fully relaxed position. The last 50% of muscle
lengthening requires significant tension, the energy of which is stored
and used to supplement the active contraction of the stretched muscle.
repetitive stress, all of these tissues have a rather constant response
to long-term changes in their resting tension.
stretched position for several days at a time, the tissue begins to
undergo structural change to adapt to the new length and to restore the
resting tension that was characteristic of the tissue before the
change. A continuously stretched muscle fiber begins to add sarcomeres
to increase its resting length and reduce tension. Collagen bands
become progressively absorbed and are replaced by new collagen that is
no longer under tension. Skin cells in the germinal layer show many
mitotic figures, and growth reduces the slight tension that had been
imposed on it.
in a totally slack and loose position, the tissue elements begin to be
absorbed and reoriented in a shortened position. Muscle fibers lose
sarcomeres until normal physiologic resting tension is restored in the
new posture.
largely depends on the harmony between active muscle contraction and
the viscoelastic changes in the passive soft tissues. For example, a
stretched muscle uses elastic recoil to provide most of the force when
it begins to contract; most of the active contractile force of a
muscle, as it nears its limit of shortening, is consumed in stretching
out its opposing muscles and is not available for its primary function
of moving the joints. Similarly, the elastic stretching and recoil of
skin and connective tissue participates in all joint motion, and the
feedback of its sensory nerves provides the best monitor of joint
position and pro- prioception.
the hand. This results in a collapse of joints toward the posture in
which the unparalyzed muscles are shortened and in which the soft
tissues on the paralyzed side are stretched to the point at which their
elastic tension equals the diminished tonus of the shortened
unparalyzed muscles.
unparalyzed muscles rest at a tension below their normal resting
tension and begin losing sarcomeres to restore tension in the shortened
position. The stretched skin and other soft tissues begin to grow to
reduce their unnatural state of tension.
destabilization of the equilibrium until some joints reach a point
beyond which they cannot move. This process is seen in ulnar palsy, in
which there may be minimal clawing soon after injury but severe
deformity after several months. It is also seen in radial palsy if the
wrist is not supported night and day. And this process is seen in the
thumb in median palsy, in which the dorsal tissues of the thumb web
become progressively narrower and the ligaments at the base of the
thumb change their length and density; after 1 or 2 years it may become
impossible to oppose the thumb fully even after effective tendon
transfers.
often neglected. A recognition of its importance results in a greater
insistence on maintaining a normal functional position of the hand at
rest as well as during activity until muscle balance is restored. This
discussion should also stimulate the surgeon to operate earlier to
restore muscle balance.
active person to get things done despite the limitations of paralysis.
It is the good patient who finds a way around her disability, and it is
only a foolish surgeon or therapist who decries these efforts unless
there is a serious reason for preventing their use.
never be done if the hand were normal. When the normal way to hold an
object or to perform an action is no longer possible, some people react
passively and wait for the doctor to do something. Others are
determined to move ahead and find a way to do the job with whatever
resources remain in the hand. These unorthodox patterns of movement
indicate that the will to work is maintained. When patients succeed in
accomplishing objectives, they gain confidence and maintain personal
pride. These are assets beyond price. The quality of muscles, skin, and
joint motion are maintained in better condition than if the limb is
passive in a splint.
The tissues may become stretched or contracted as a result, and the
trick may persist after tendons have been transferred. Tissue changes
have already been mentioned, and examples have been given from
paralysis of each of the three main nerve paralyses. Of the trick
movements that may be troublesome as a habit after tendon transfer, one
of the worst is the lateral squeeze pinch that is developed by almost
every patient who has a low ulnar median palsy (Fig. 54.9).
These patients cannot easily use their thumbs except by simultaneous
contraction of the extensor pollicis longus and flexor pollicis longus.
Each of these muscles, although opposing each other at the
interphalangeal and metacarpophalangeal joints, has a common vector for
adduction at the carpometacarpal joint of the thumb. To make this work,
the two muscles must contract
together.
The flexor pollicis longus overcomes the extensor pollicis longus at
the two distal joints where its moment arms are greater, and the
extensor pollicis longus keeps the carpometacarpal joint in extension
for which it has a better leverage than the flexor pollicis longus has
for flexion. The resulting ugly pinch is strong and becomes frequently
used.
 |
|
Figure 54.9.
The lateral squeeze pinch, which is used by patients who have low median and ulnar paralysis of the thumb. The thumb squeezes with all joints in flexion except the carpometacarpal joint, which is in extension and supination. (From Brand PW. Clinical Mechanics of the Hand. St. Louis: CV Mosby, 1985, with permission.) |
interphalangeal joint and shortening of the dorsal skin and fascia of
the web. Even if these deformities are corrected by surgery, the habit
of using the extensor pollicis longus for pinch tends to persist. It is
most difficult to get rid of if it has been used for many months or
years and by older patients. The problem of this abnormal pinch is that
it is the opposite of the new pattern that the surgeon uses to restore
normal pinch. The newly transferred abductor-opponens transfer may be
hard to reeducate, but the extensor pollicis longus is easy to use by
force of habit. The extensor pollicis longus also has a better moment
arm to pull into supination than the new transfer has for pronation.
The patient’s instinctive tendency to contract the extensor pollicis
longus on attempted pinch is the cause of many failures of opponens
transfers.
thumb may be splinted forward or held out by a C-splint. If a tendon
transfer is to be delayed many months, however, it is not likely that a
patient will agree to remain restrained. If the pattern is already
firmly established at the time surgery is planned, consider using the
habit, rather than fighting it, by transferring the extensor pollicis
longus through the distal forearm between radius and ulna to be
attached to the stump of its own tendon to serve as an
abductor-extensor of the thumb. The attempt to use the trick movement
then enhances the true opponens action. This transfer leaves the thumb
with inadequate thumb supination and should be used only in older
patients or if there is likelihood of failure of regular transfers.
balance operation in any case of irreparable nerve loss is as soon as
possible after wounds have healed and after there is tissue
homeostasis. This approach allows no time for harmful secondary
stretching or contractures or for the development of trick movements or
habitual patterns.
skin mobility, joint mobility, hand volume, and skin temperature. I
suggest the use of a skin thermometer for comparing the affected side
with the normal side. A hand volumeter is also a useful instrument for
monitoring the resolution of any inflammatory state in the tissues of
the hand. The patient should notice the progress in the graph of these
records, which can also be used after surgery to mark progress in
recovery from the operation and the mobilizing of joints and tendons.
The patient learns to associate raised temperatures with inflammation
and notices how his hand volume increases when the hand is hanging down
and how it decreases after a period of elevation and moderate exercise.
tissue inflammation as marked by lack of free skin mobility, elevated
local temperature, and hand volume, the postoperative inflammation is
likely to be more severe and the adhesions around transferred tendons
more difficult to resolve.
and understand the implications of the operation and to identify the
muscle and tendon to be transferred, so that there may be no loss of
time in the critical period after the postoperative cast is removed.
nerve has been repaired and is in process of recovery. Too many
surgeons assume that they have to wait until they are absolutely
certain that no recovery is possible before
they
decide to operate for restoration of muscle balance. They are afraid of
some recovery occurring after they have performed a tendon transfer and
of being told that their operation was unnecessary and possibly harmful.
lawsuits than by the good of the patient. The correct approach to this
problem is first to make a realistic estimate of the probability of
good recovery of the involved muscles, recognizing that muscle recovery
is good if the nerve repair is accurate and without tension, and is in
the same limb segment as the affected muscle. The likelihood of good
recovery is fair if the nerve injury and repair is in the limb segment
proximal to the muscle, and it is poor if the injury is two segments
proximal. An ulnar nerve division above the elbow, for example, rarely
results in good recovery of the intrinsic muscles in the hand. A median
nerve above the elbow has a slightly better likelihood of recovery, but
the secondary stiffness and contracture that results from the necessary
1- to 2-year wait to make sure is more harmful than any disability that
may result from an early transfer followed 1 or 2 years later by
recovery of the thenar muscles.
recovery is possible, it is wise to select a tendon for transfer that
will not leave a significant defect by its loss from the donor site.
For example, in a high median palsy, although the thumb is fully mobile
passively, it is appropriate to use the extensor indicus proprius
around the ulnar border of the wrist to restore abduction to the thumb.
This muscle might be inadequate if it had to oppose contracted tissues
and a negative pattern of use after 1 or 2 years. Similarly, a palmaris
longus, extended by free grafts through the carpal tunnel, is
appropriate for a new case of intrinsic palsy of the fingers before the
support of the volar plates and other tissues is lost by being
stretched and before the interphalangeal joints become stiff in flexion.
patient and the pros and cons offered in writing so that the patient
may understand and choose between the possible harm of operating early
and the more probable harm of waiting until much later.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
