Pilon Fractures
substantial therapeutic challenges that confront the orthopaedic
traumatologist. Numerous features are responsible for this, but perhaps
none are as difficult as the accompanying soft tissue injury that is
frequently present. First described by the French radiologist Destot in
1911, ankle fractures that involve the weight-bearing distal tibial
articular surface are known as pilon fractures.54 The term pilon
is from the French language and refers to a pestle, specifically a
club-shaped tool for mashing or grinding substances in a mortar, or a
large bar moved vertically to stamp or pound. Later, Bonin would refer
to a similar fracture as a plafond fracture.22 Plafond, meaning ceiling
in French, likens the distal tibial articular weight-bearing surface to
the ceiling of the ankle joint. Though commonly used interchangeably
with the term plafond, a pilon fracture is a descriptive term
suggesting that the talus acts as a hammer, or pestle, that impacts and
injures the tibial plafond. Several key aspects of these poorly
understood injuries were elucidated 1968, when Ruedi published an
influential paper on this topic, describing the fracture, its treatment
principles, and a classification system.145
The surgical management of distal tibia fractures has evolved over the
past 30 years in large part because of an improved understanding of the
importance of the soft tissue envelope. Specifically, the restoration
of the osseous anatomy while ignoring the often-traumatized soft tissue
envelope frequently led to poor postoperative outcomes and high
complication rates. Although multiple treatment approaches and
protocols have been described, there is no consensus regarding the
optimal treatment of these challenging injuries. Similarly, long-term
outcome data from randomized comparative treatment methods remains
lacking. What does appear to be clear, however, is that the surgeon
must balance the extent of osseous reduction and stability,
particularly that of the articular surface, within the tolerances of
the soft tissue envelope. Although the severity of these injuries,
complexities of a variety of treatment methods, and limitations of
management having been well documented in the literature, excellent
long-term results of treatment continue to elude patients sustaining
these fractures.
plafond injuries, initially described in 1968, demonstrated
satisfactory and durable results with few complications.145 A subsequent paper in 1973 evaluating 54 of the initial 82 patients an average
of 9 years postinjury demonstrated the durability of the initial
results with an overall improvement of function and only exceptional
deterioration.144
These findings were in stark contrast to earlier published results that
shaped the existing fatalistic attitude of these injuries.23,50,66,70 Ruedi’s results were supported over the following decade, initially by the results Heim78 and later by those of Ovadia and Beals.129
The authors of these manuscripts noted that their best results were
obtained by open reduction and internal fixation according to the
Arbeitsgemeinschaft fur Osteosynthese (AO) technique used by Ruedi. In
part as a result of these publications, open reduction and internal
fixation of tibial pilon fractures became the North American standard
of care in the late 1980s and early 1990s. Nonetheless, the enthusiasm
for open treatment of these injuries soon became tempered by reports of
substantial rates of wound complications, particularly deep sepsis,
osteomyelitis, and, ultimately, poor outcomes.33,34,57,110,165,187
of injury in Ruedi’s initial patient population, a greater proportion
of North American injuries were noted to be the result of higher energy
axial-loading motor vehicle collisions. Additionally, the experience
with soft tissue handling techniques was potentially not as advanced as
those for treating the osseous injury. Wrysch noted, in contrast to the
skiing accident population reported by Ruedi, that a large percentage
of urban trauma center patients incurred their injuries from axial
compressive forces, resulting in severe articular comminution and an
increased soft tissue injury severity.187
Because of the severity of the soft tissue injury and the reported soft
tissue complication rate attributed to extensive surgical exposures and
bulky internal fixation devices approximating 40% to 50%, external
fixation emerged as a successful technique for decreasing significant
septic complications that had been previously attributable to open
surgical management.20 In a series
of high-energy tibial plafond fractures, Bone and colleagues reported
their results using combined internal and external fixation techniques.21
This consisted of open reduction and stabilization of the articular
surface with screws or small plate fixation and an ankle-spanning
external fixator was used to primarily neutralize the distal
metaphyseal fracture until union. There were three fractures with
delayed unions that required bone grafting, but there were no
significant infections in either the open or closed fracture groups.
The authors attributed the decrease in complications to improved soft
tissue management afforded by the external fixation. Other authors
similarly noted a comparable decrease in deep wound complications with
the use of external fixation when compared with open plating techniques.19,76,149
Tornetta described combined open stabilization of the articular injury
and neutralization of the metaphyseal fracture with the use of hybrid
external fixation without spanning across the ankle joint.171 The theorized benefits of this treatment were similar to those of Bone,21
with the added potential benefit of allowing cartilage nutrition
through the use of early ankle range of motion. Tornetta’s favorable
results demonstrated a substantial decrease in soft tissue
complications, with only one deep infection noted in 26 managed
fractures, and 71% of patients with intra-articular fractures followed
between 8 and 34 months demonstrating good and excellent results. These
results were supported by other authors using hybrid or fully circular
wire and ring external fixation devices.* However, in
separate reports, Pugh and colleagues and Anglen noted that the use of
external fixation was not a panacea, identifying increased rates of
malunion, nonunion, lower clinical scores, and a slower return to
function when compared with their own concurrent ORIF study groups, as
well as the results of previously published external fixation reports
in the literature.6,137
Subsequent investigations would demonstrate significant rates of pin
tract infections, tendon injury, and impalement of neurovascular
structures with the use of tensioned wire fixators.87,178
fixation techniques and an improved understanding of the associated
soft tissue injury gave way to the reconsidering of open treatment with
internal fixation but after a period of soft tissue recovery. In their
1996 textbook, Schatzker and Tile made a distinction between the soft
tissue envelope that is adequate for an immediate major surgical
procedure and the soft tissue envelope that is not suitable for surgery
because of the presence of marked swelling or fracture blisters.166
In this latter group, a 7- to 10-day delay prior to definitive fixation
was suggested, allowing for the skin and soft tissues to return to a
“reasonable” state. Until resolution of the soft tissue injury, it was
recommended that the limb undergo a closed reduction and plaster splint
immobilization, or some form of skeletal traction or external fixation.166
Before this, Mast had recommended that if definitive surgery cannot be
performed within 8 to 12 hours, that temporary treatment should be
rendered and the definitive procedure delayed for 7 to 10 days to allow
time for resolution of swelling.108
Mast recommended that length stable injuries could be temporized with
casting, but for those fractures with shortening, a period of calcaneal
traction was allowed that restored fracture fragment length or even
slight distraction.108 Hontzsch had
also noted the advantages of two-stage treatment in treating 50 tibial
pilon fractures, using external fixation as a temporizing device.83
tibial plafond fractures with open reduction and internal fixation
techniques, but with strict attention to the critical appreciation and
handling of the traumatized soft tissue envelope. This has led to the
popularization of the staged management of tibial pilon fractures,
championed in 1999 by two separate reports by Sirkin and colleagues,
and Patterson and Cole.135,156
of infection associated with open reduction and internal fixation of
pilon fractures may have been caused by attempts at immediate fixation
through swollen and compromised soft tissues. Although staged treatment
remains the current foundation for the management of these injuries,
the application of minimally invasive plating techniques,12,44,46,80 use of alternate exposures,7,77,81 the development of low profile and anatomically contoured plates,154 and a greater understanding of the osseous fracture anatomy169 has, in part, also been a response to the difficult soft tissue injury that accompanies these fractures.
understanding, and treatment of the concomitant soft tissue injury, the
liberal use of computed tomographic (CT) scanning, advances in implant
design including locking plate technology, and minimally invasive
application techniques, consistently satisfactory outcomes for the
management of these challenging fractures remains elusive.
|
TABLE 56-1 Characteristics of Rotational Compared with Axially Loading Fractures
|
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||
weight-bearing surface are the result of high-energy mechanisms that
occur during motor vehicle accidents, falls from heights, motorcycle
accidents, and industrial mishaps.122
Malleolar ankle fractures are typically the result of lower energy
indirect rotational forces, whereas the majority of intra-articular
fractures of the distal tibial weight-bearing surface are primarily the
result of axial loading forces in which the talus is forced proximally
into the distal tibia, producing the “explosion” fracture of the
articular surface.89,147
These two main mechanisms of injury result in significantly different
fracture patterns, soft tissue damage, associated injuries, and
prognosis. Compared with rotational forces, axial loads are typically
applied in a more rapid fashion. Because bone is viscoelastic, more
energy is absorbed before failure; at failure, the energy is released
and imparted to the soft tissue envelope. Even in the absence of direct
trauma to the soft tissue envelope, it is this release of energy that
results in the substantial swelling and blistering seen in these
injuries (Table 56-1). Clearly a spectrum of injury results, with predominantly axial or rotational forces evident in combined mechanisms.
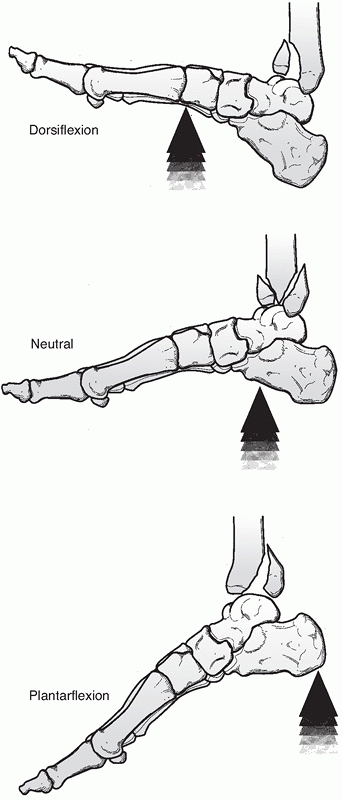
the ultimate fracture pattern depends on the direction and rate of
application of the injurious force, and the position of the foot at the
time of loading. Because of this, wide variations in fracture patterns
occur. A vertical impact while the foot is in dorsiflexion results in
cephalad and anterior force, resulting in significant anterior plafond
comminution, whereas impact with the foot in the neutral position
results in significant central comminution. These injury patterns are
much more common than those of the posterior plafond, which are thought
to occur during plantarflexion. The precise direction and position of
the foot at the time of impact, however, leads to wide variations in
fracture patterns (Fig. 56-1).
automotive restraint systems, and improved life-saving trauma care
systems have resulted in an increasing incidence of axial load-type
intra-articular distal tibia fractures that confront the orthopaedist.
The same forces that may have previously resulted in death of the
occupant are now neutralized by vehicle restraint systems; however,
these same forces are still applied to the lower extremities, resulting
in the increasingly frequent presentation of extremely severe injuries
of the distal tibia. Tibial plafond
fractures
may present in isolation but are also frequently seen in the
polytraumatized patient. Marked articular and metaphyseal comminution,
wide displacement, chondral impaction, associated fibular fractures,
and articular debris are commonly seen. Open wounds, deep abrasions,
fracture blisters, and accompanying osseous and soft tissue
devitalization are common and corroborate the high-energy mechanism.
 |
|
FIGURE 56-1
The position of the foot at the time of axial load determines which portion of the tibial plafond sustains the major impact of the talus. |
rotational forces have a spiral orientation, frequently without
significant fracture comminution. The articular injury is composed of
mildly or moderately displaced large articular fragments with minimal
chondral impaction or disruption. The soft tissue envelope is injured
to a lesser degree, although significant swelling may still be a
component. Open wounds with significant devitalization are not common
and the prognosis is more favorable.
motor vehicle collisions or falls from a height, create a variety of
associated injuries. In several large series of tibial plafond
fractures, other fractures and other major system injuries were present
in between 27% and 51% of patients.* The incidence of open
fracture varies according to whether higher or lower energy mechanisms
are reviewed. Ruedi noted the open fracture rate to be between 3% and
6%,144,146
where a high percentage of injuries occurred in skiers. Higher
incidences of open fractures ranging between 12% and 56% have been
reported in series in which most of the fractures resulted from higher
energy mechanisms such as motor vehicle collisions and falls from
heights.21,77,136,180
vascular injury and compartmental syndrome is relatively rare, with the
incidence ranging from 0% to 5%.34,100,171
Recently, however, LeBus and Collinge evaluated 25 consecutive patients
sustaining high-energy tibial plafond fractures with computed
tomographic angiography (CTA) noting vascular abnormalities in 52%.94
Of the 14 arterial lesions identified, 9 involved the anterior tibial
artery, 3 the posterior tibial artery, and 2 the peroneal artery. Fifty
percent of these arterial lesions demonstrated complete occlusion, and
a significant association was found between the presence of an open
fracture and an arterial abnormality. Interestingly, all of these limbs
demonstrated dorsalis pedis artery pulses or documented biphasic
Doppler tones and none were described as pulseless or clinically
ischemic. Although no sequelae regarding wound healing or fracture
union related to the arterial abnormality was identified, patients with
CTA-diagnosed vascular abnormalities tended to be treated with more
minimally invasive surgery than those without vascular abnormalities.
are extremely unusual; however, chondral injuries of the talus,
particularly gouges, scuffing, and frank chondral fractures are quite
common but are likely underreported.151
Although the definitive impact that these chondral injuries have
remains unknown, it is intuitive that they likely negatively affect
long-term outcome.
the magnitude of energy involved. This in turn allows the surgeon to
assess the likelihood of associated skeletal or other system injuries,
and the propensity for the development of significant soft tissue
swelling and blistering of the soft tissues of the fractured distal
tibia. Insight into the mechanism of injury allows the surgeon to begin
formulating a preoperative plan and counseling for the patient
regarding the prognosis of the injury. Medical comorbidities and
nicotine usage are particularly important and are detailed, as they may
modify the surgical tactic. Additional information that is obtained
from the history include the type of employment, family support
systems, level of education, and whether the injury occurred as the
result of a work-related accident, as these have been identified as
variables that appear to affect the functional outcome.136,184
The setting of injury should be identified, as this information may
have an impact on the type and degree of contamination in open
fractures and direct subsequent antibiotic treatment.
importance in the complete assessment of fractures of the tibial
plafond and should be performed in a logical, consistent, and
circumferential manner. The degree of swelling, severity of contusions,
and presence of abrasions, blisters, open wounds, and compartmental
syndrome are evaluated and noted. Not infrequently, widely displaced
fracture fragments may create excessive skin tension and jeopardize
local skin circulation. In these situations, manual correction of these
gross deformities must be performed expeditiously, before radiographic
examination, to minimize further vascular compromise to the local skin
and soft tissues. The circulatory status is evaluated by palpation
and/or Doppler ultrasound examination of the pedal pulses, and by
noting the color and temperature of the foot. The dorsal and plantar
aspects of the foot are examined for alterations in sensation. Open
wounds are treated with initiation of intravenous antibiotics, removal
of obvious foreign material and debris, sterile saline irrigation, and
coverage with a sterile bandage. Occasionally a fragment of bone
remains extruded through the skin, resulting in crushing of the
underlying skin and soft tissue envelope. Often this scenario occurs
when the distal portion of the tibial shaft is extruded through the
anteromedial skin of the distal tibia, putting the skin at the distal
portion of the wound in jeopardy. In this situation, reduction of the
extruded fragment should be attempted, with the goal of relieving
further injury to the anteromedial soft tissues. Once the limb has been
evaluated, it is realigned and placed into a provisional splint that
does not obscure radiographic detail.
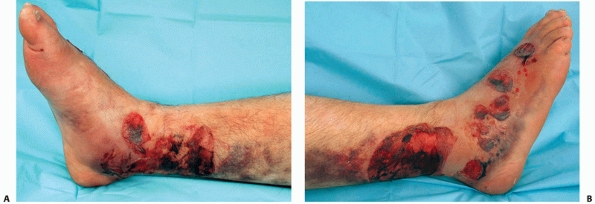
In a clinical and histologic study performed by Giordano and
colleagues, the authors identified two clinical types of fracture
blisters, clear filled and blood filled.73
Histologic evaluation demonstrated that both fracture blister subtypes
represented cleavage injuries at the dermal-epidermal junction. The
main difference between clear- and blood-filled blister types was the
retention of some degree of epidermal cells in the clearfilled
blisters, which the authors believed contributed to a more rapid
reepithelialization and was indicative of a more superficial
injury.
Conversely, the dermis of the blood-filled subtype was completely free
of epidermal cells, indicative of a deeper injury involving the
papillary vasculature, and which may have led to increased
reepithelialization time. Disruption of the dermal-epidermal junction
and the subsequent formation of fracture blisters appears to result
from high strain exposure in the skin as it is deformed by bony
displacement at the time the fracture occurs.74
Although reports in the orthopaedic literature concerning fracture
blisters and their management are limited, hemorrhagic blisters appear
to be associated with increased complication rates, scarring, and
delayed surgical intervention.72,159,176
Several methods are used to treat fracture blisters, including: (i)
sterile unroofing with the application of Silvadene and/or nonadherent
dressings, (ii) sterile aspiration with maintenance of the overlying
roof, and (iii) leaving the blister intact. There is no compelling
evidence to support any method over another.72,159
What does appear reasonable, however, is to avoid the placement of
incisions through a noneipithelialized blister bed, particularly a
hemorrhagic blister, if possible.72,159,176
 |
|
FIGURE 56-2 Clinical photographs of the right lower extremity from the medial (A), and lateral (B)
perspectives 5 days after sustaining a highly comminuted tibial pilon fracture. A number of drained hemorrhagic fracture blisters can be identified, the majority of which are still covered by the overlying epidermal layer. Initial treatment (spanning external fixation) was delayed secondary to associated life-threatening injuries. The severity of soft tissue injury laterally, particularly the need for reepithelialization of the hemorrhagic fracture blister bed, precluded fibular fixation for approximately 3 weeks. |
ankle anteroposterior (AP), mortise, and lateral radiographs.
Full-length images of the tibia and fibula complete the radiologic
examination of the injured leg and are used to diagnose more proximal
and potentially noncontiguous fractures of the tibia and/or fibula. The
diagnosis of a displaced fracture of the tibial plafond is invariably
made on these initial radiographs. Although CT scanning has become a
routine part of the radiographic assessment of tibial plafond
fractures, a careful review of the plain radiographs will demonstrate a
substantial amount of information. Key features to identify include the
direction and magnitude of talar displacement or talar subluxation, the
presence or absence of a fibular fracture, the degree of articular
comminution, areas of articular impaction, and disruptions of the
distal tibiofibular syndesmosis. Distally, associated injuries of the
hindfoot and proximally, diaphyseal extension can be assessed.
ability to assess the injury and formulate a preoperative plan before
definitive fixation.169,170
Thin cut axial images combined with coronal and sagittal reformatting
allow evaluation of major fracture planes, articular impaction, and
degree of comminution. The ability to accurately assess the location,
size, and displacement of the articular surface greatly helps to
determine the location and orientation of articular fixation,
particularly when using percutaneous techniques. The information
obtained from CT scans enables an accurate surgical plan, allowing the
surgeon to apply strategic fixation with minimization of soft tissue
dissection. For these reasons, axial CT scans with sagittal and coronal
plane reformations should be obtained routinely to assist with
definitive preoperative planning. In the author’s opinion,
three-dimensional reconstructions add little to the information
obtained using the axial images with sagittal and coronal reformations.
a provisional reduction is obtained, preferably with a spanning
external fixator. CT scans obtained with substantial shortening,
angulation, and significant displacements of the talus and fracture
fragments make the identification of fracture details more difficult
and formulation of a preoperative surgical plan suboptimal.
Occasionally, however, acute CT scanning of the distal tibia is
appropriate. This situation occurs when the plain radiographic
investigations demonstrate: (i) a “simple” and modestly displaced
articular injury with a soft tissue envelope that does not preclude
early ORIF, or (ii) the plafond injury is part of a seemingly
extra-articular distal tibia fracture with plain radiographic clues
that suggest an intra-articular extension. In this latter situation,
the CT scan is used predominantly as a diagnostic tool, rather than as
a method for further delineating the fracture anatomy already
identified on the plain radiographs. The distinguishing features of
both of these scenarios are that: (i) the interpretation
of
the CT scan is clear and understandable, and (ii) the operative
strategy may consist of a single-stage surgical procedure provided the
injury demonstrates a satisfactory soft tissue envelope.
magnetic resonance imaging of these injuries, and although angiography
has been described as a diagnostic tool for clinically silent vascular
abnormalities associated with fractures of the distal tibia,94 its routine use has not been supported.
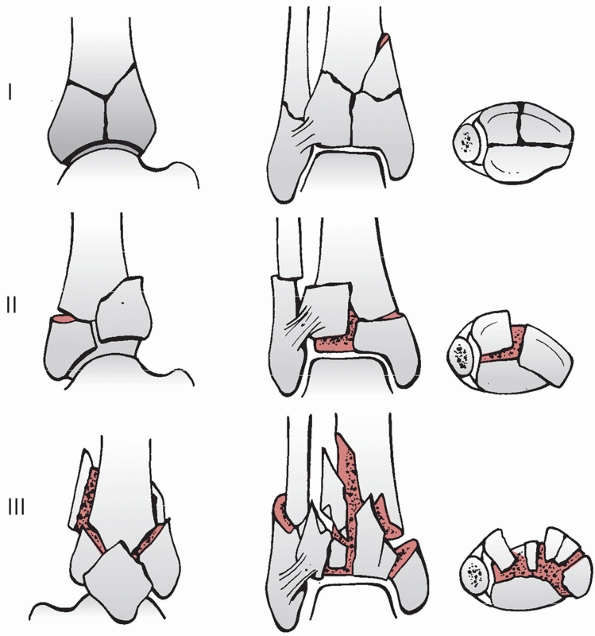
is moderately useful and divides fractures of the tibial plafond into
three types based on the displacement and degree of comminution of the
articular surface (Fig. 56-3). Type I fractures
are intra-articular fractures without displacement. Type II fractures
demonstrate displaced articular fragments without comminution. Type III
fractures demonstrate displacement and comminution of articular
fragments. Interobserver and intraobserver agreement has been shown to
be poor with the Ruedi-Allgower system.107
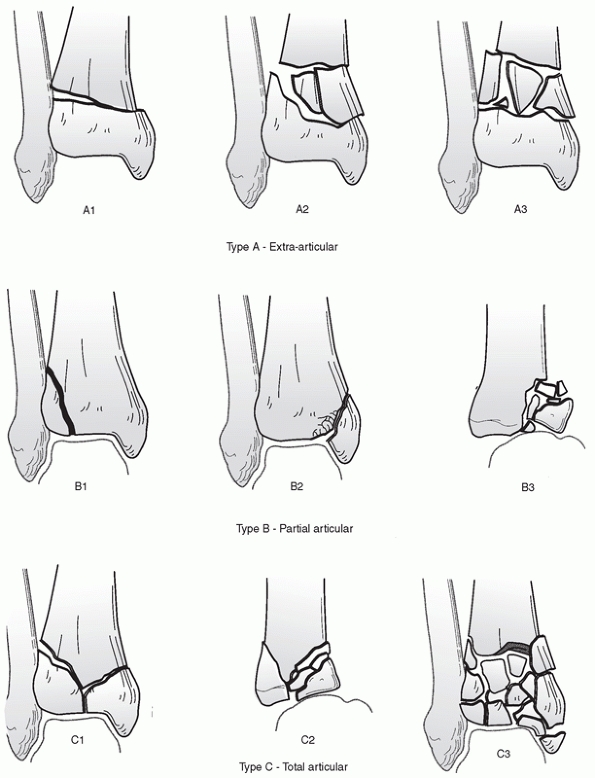
incorporating all fractures of the distal tibia, including
extra-articular fractures of the distal tibial metaphysis. Each bone is
assigned a unique numerical designation and fractures are classified
according to a consistent framework. The tibia is assigned the numeric
code of 43. Injuries of the tibial plafond are then categorized as
extra-articular (43 type A), partial articular (43 type B), or total
articular (43 type C) (Fig. 56-4). Each type is
then further divided into one of three groups depending on the amount
of fracture comminution. Each of these, in turn, can be further divided
into subgroups by other characteristics of the fracture, such as the
direction, description, or location of a fracture line; the presence or
absence of asymmetric metaphyseal impaction; and the location and
amount of comminution. As expected, the resultant 27 subgroups form a
fairly large and cumbersome classification system. Swiontkowski
demonstrated moderate observer agreement using the AO/OTA system,
particularly in the determination of the fracture type (type A, B, or
C), with poorer observer agreement noted with fracture grouping (e.g.,
C1, C2, or C3).164 Martin
demonstrated improved interobserver reliability when classifying
fractures into major types with the AO/OTA system (kappa = 0.60) than
with that of the Ruedi-Allgower system (kappa = 0.46).107
Nevertheless, for describing these injuries, and for the purposes of
developing a surgical tactic, the authors find that grouping the
fractures according to the AO/OTA system (e.g., C1, C2, or C3) can be
useful.
 |
|
FIGURE 56-3
Ruedi-Allgower classification of tibial plafond fractures. Type I: cleavage fracture of the distal tibia without significant displacement of the articular surface. Type II: significant fracture displacement of the articular surface without comminution. Type III: Impaction and comminution of the distal tibial articular surface. |
associated with tibial plafond fractures has resulted in the evolution
of their surgical treatment. Despite this being a critical therapeutic
consideration, a clinically useful classification system that guides
treatment still remains lacking. What has become apparent is
that classifying soft tissue injuries is even more difficult than classifying the fracture.37,85
Therefore, a thorough evaluation of the soft tissue envelope, and
individual surgeon experience and judgment remain the mainstay.
 |
|
FIGURE 56-4
The three major types of distal tibia fractures according to the AO/OTA classification system. Type A fractures are extra-articular. Type B fractures are partial articular. Type C fractures are complete articular. Subdivisions within each type are based on increasing amounts of comminution. |
and Goetzen is subjective and grades soft tissue injuries of closed
fractures into one of four categories, organized from 0 to 3.174
Closed fractures with no appreciable soft tissue injury are Grade 0 and
demonstrate an indirect fracture with a simple pattern. Grade 1 soft
tissue injuries have superficial abrasion or contusion of skin; simple
or medium-energy fracture patterns are evident with displaced fracture
fragments exerting pressure on the skin. Grade 2 injuries have deep
abrasions and local contused skin; medium to severe fracture patterns
are identified. Grade 2 injuries may also demonstrate imminent
compartmental syndrome. Finally, Grade 3 injuries have extensive
contusions or crushing, and significant muscle destruction and
subcutaneous tissue degloving. Compartmental syndrome, vascular
injuries, and severe fracture comminution and a high-energy mechanism
are often identified as part of Grade 3 injuries.
injury is widely discussed in the literature, the observer reliability
and reproducibility have not been evaluated. The extent of soft tissue
injury does not necessarily vary directly with the AO/OTA fracture
classification, and although higher energy injuries often demonstrate
increased fracture comminution and worse soft tissue injuries, the
reverse does not necessarily hold true. Therefore, although the
underlying fracture type may provide a clue to the amount of soft
tissue injury, it is important to evaluate and classify the soft tissue
injury separately from the fracture configuration.
expanded by the AO group to create a more objective system that
evaluates and grades each component of the soft tissue envelope,
including the skin, musculotendinous components, and neurovascular
tissue.120 This comprehensive system
is very complicated and not clinically practical, but does provide the
framework for the surgeon to systematically and critically evaluate the
associated soft tissue injury.
surgical approaches are frequently required. Therefore, a thorough
understanding of each approach and the associated anatomic structures
is necessary to properly care for these injuries. The choice of
surgical approach(es) is arrived at by an understanding of the fracture
anatomy, and balancing the need for accessing and manipulating
displaced articular segments, while minimizing further injury to the
soft tissue envelope. The most frequent approaches used include the
anterolateral, anterior, anteromedial, posteromedial, and
posterolateral. Because of the subcutaneous nature of the distal tibia,
direct medial approaches are associated with an unacceptably high rate
of soft tissue complications and should be avoided.
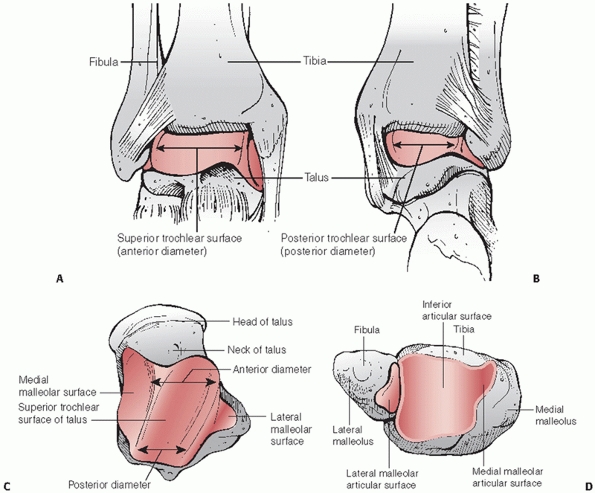
The distal ends of the tibia and fibula together form a deep socket or
boxlike mortise into which the superior dome of the talus fits.115
The articular surface of the distal tibia is rectangular in shape and
forms the roof of the mortise. Its surface is wider anteriorly than
posteriorly and slightly concave from anterior to posterior.115
The centrally concave distal tibial articular surface demonstrates
anterior and posterior extensions. The posterior tibial articular
surface extends more distally, making a posterior arthrotomy for joint
inspection impractical. Although the anterior tibia extends over the
dome of the talus, the entire articular surface of the tibia can be
viewed from any of the anteriorly based approaches. The medial
malleolus is a distal and slightly anterior projection from the medial
aspect of the weight-bearing surface. It presents a chondral surface
that is oriented approximately 90 degrees to the horizontal tibial
plafond and articulates with the medial aspect of the talar body. The
lateral malleolus is the terminal distal portion of the fibula that
articulates with the lateral aspect of the talus. Additionally, it
demonstrates an important articulation with the posterolateral aspect
of the distal tibia, the distal tibiofibular syndesmosis. Maximum
compressive strength of the tibial plafond occurs within approximately
3 cm from the articular surface, with virtually no resistance to
compression in the trabecular bone at a distance of more than 3 cm
proximal to the subchondral region.4 The strongest cancellous bone in the region of the distal tibia is located near the subchondral bone plate4
and may provide an optimal area for fixation devices. The relevant
anatomy of the talus includes those nonarticular portions of the talar
neck that are useful in the placement of Schanz pins to facilitate
talar manipulation and application of distraction across the ankle
joint. Laterally, there is substantially more area available at the
talar neck than that available medially. Relative to the anatomic axis
of the tibia, the orientation of the tibial plafond in the frontal
plane is slight valgus (approximately 2 degrees), and the
mid-diaphyseal line (or anatomic axis) of the tibia passes just medial
to the midline of the talus.132 In
the sagittal plane, the plafond is slightly extended (approximating 5
to 10 degrees), and the mid-diaphyseal line of the tibia passes through
the lateral process of the talus (center of rotation of the ankle
joint) when the foot is at 90 degrees to the tibia.132
Understanding these relationships is particularly important during the
application of external fixation devices and the use of indirect
fracture reduction techniques. In our experience, radiographs of the
contralateral ankle form the best reference for restoring each
patient’s unique osseous anatomy.
ankle joint is useful for appreciating fracture displacement patterns,
and when considering planes of safe surgical dissection (Fig. 56-6).
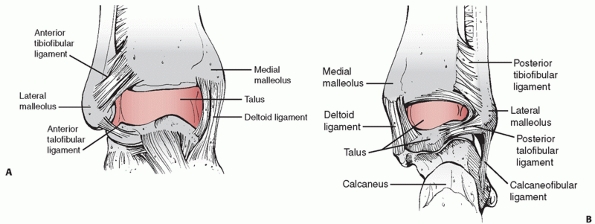
The distal tibiofibular syndesmosis is formed by the irregular convex
surface of the medial aspect of the distal fibula and the irregular
concave surface on the lateral aspect of the tibia. In its distal
portion, the fibula is effectively secured to the distal tibia by the
anterior tibiofibular ligament, posterior tibiofibular ligament, and
strong interosseous tibiofibular ligament. The flat and
triangular-shaped anterior tibiofibular ligament travels from the
anterolateral aspect of the distal tibia, usually referred to as the
tubercle of Chaput, laterally and distally to insert on the anterior
aspect of the distal fibula.133 The smaller and more horizontally oriented posterior tibiofibular
ligament is comprised of a superficial and deep component. The latter
is also known as the transverse tibiofibular ligament and projects
below the margin of the distal tibia to form a labral articulation for
the posterolateral talus.124
The deltoid ligament is a strong, flat, broad triangular band composed
of a superficial and deep set of fibers. The superficial fibers pass
distally from the anterior colliculus of the medial malleolus to the
navicular, sustentaculum tali of the calcaneus, and the anterior
portion of the medial tubercle of the talus.134
The clinically important deep portion of the deltoid consists of a
posterior band, the deep posterior talotibial ligament, originates from
the posterior colliculus and intercollicular groove and travels
posterolaterally and distally to insert into the entire nonarticular
medial surface of the talus.133,134
This deep portion of the deltoid ligament is the principal stabilizer
of the talus in the ankle mortise. Using MRI ankle arthrography, Lee
and colleagues have delineated the proximal capsular extension of the
ankle joint.95 The mean capsular
extension anterior to the distal tibia was 9.6 mm proximal to the
anteroinferior tibial margin and 3.8 mm proximal to the dome of the
tibial plafond. In the tibiofibular recess, the mean capsular extension
was 19.2 mm proximal to the anteroinferior tibial margin and 13.4 mm
proximal to the dome of the tibial plafond. These and other authors
have noted that these areas, therefore, are at risk for being traversed
with the use of fine wire external fixation techniques for distal
tibial plafond fractures.95,178
 |
|
FIGURE 56-5 Osseous anatomy of the right ankle joint. A. Anterior view. B. Posterior view. C. Superior view of the right talus. D. Undersurface view of the right tibial plafond.
|
 |
|
FIGURE 56-6 Important ligamentous structures around the ankle are illustrated. A. Anterior view. B. Posterior view.
|
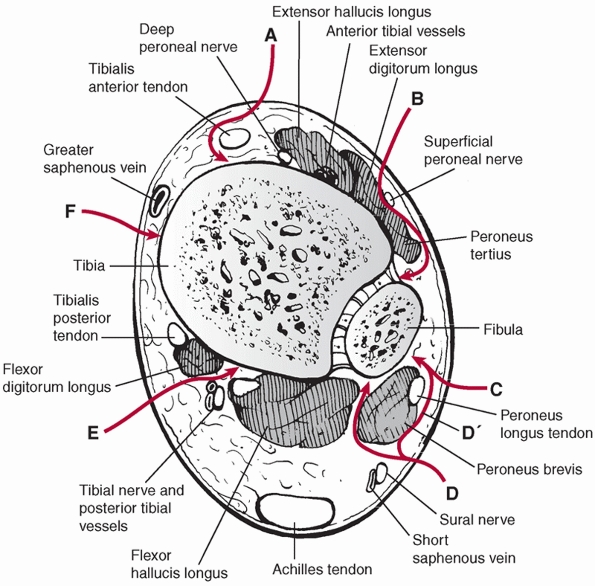
the distal tibia and ankle joint is necessary to allow for
uncomplicated approaches and dissections in safe planes (Fig. 56-7).
The anterior tibial compartment contains, from medial to lateral, the
tibialis anterior, extensor hallucis longus (EHL), extensor digitorum
longus (EDL), and peroneus tertius muscles. Because these muscles are
all innervated by branches from the deep peroneal nerve proximally in
the leg, distal approaches that are medial, lateral, and between these
muscles can be used. Distally, the continuation of the deep peroneal
nerve and the anterior tibial vessels are located between the EHL and
the EDL, requiring direct identification and protection in the direct
anterior approach. The lateral compartment of the leg contains the
peroneus longus and peroneus brevis muscles, both of which are
innervated proximally by the superficial peroneal nerve. The peroneus
brevis has a more distal muscle belly and is located posterior to the
peroneus longus. Both are firmly attached along the distal fibula by
the peroneal sheath. In the distal third of the leg, the superficial
peroneal nerve is purely sensory, pierces the lateral compartment
fascia, and travels in the subcutaneous tissue from posterior to
anterior, typically being encountered during the anterolateral surgical
exposure.
 |
|
FIGURE 56-7
Axial view of the distal tibia just proximal to the distal tibiofibular syndesmosis demonstrating the relevant local surgical anatomy and surgical approaches for management of distal tibial plafond fractures. A. Anteromedial. B. Anterolateral. C. Posterolateral (fibula). D. Posterolateral (tibia). D′. Posterolateral (fibula). E. Posteromedial. F. Medial. |
gastrocnemius, soleus, and plantaris muscles, all of which are
innervated by the tibial nerve. In the distal quarter of the leg, the
tendo Achilles is formed by the confluence of the soleus and
gastrocnemius tendons and their tendon sheath requires protection in
any posterior approaches. At the level of the ankle joint, the deep
posterior compartment muscles are largely tendinous and include the
posterior tibial, the flexor digitorum longus, and the flexor hallucis
longus (FHL) muscles. The FHL, however, has a very distal and large
muscle belly, and its identification is especially useful in the
posterolateral approach to the distal tibia. These muscles are
innervated by the tibial nerve, which passes with the posterior tibial
vessels deep to the tendinous arch of the soleus muscle in the proximal
quarter of the
leg.
The tibial nerve then descends deep to the soleus muscle and runs
distally on the tibialis posterior muscle along with the posterior
tibial vessels. The tibialis posterior, flexor digitorum longus,
posterior tibial artery, tibial nerve, and FHL travel along the
posteromedial aspect of the distal tibia within the tarsal tunnel.
These structures require protection and identification during
posteromedial surgical exposures.
The distal metaphyseal areas of the tibia have a rich extraosseous
blood supply that is primarily rendered by branches of the anterior
tibial and posterior tibial arteries. Distally, the anterior tibial
artery gives off several medial and lateral arterial branches that pass
onto the surface of the anterior distal tibial metaphysis. The
posterior tibial artery provides the majority of the extraosseous
vasculature to the medial and posterior aspects of the distal tibial
metaphysis. On the medial aspect of the distal tibia, these branches
anastomose with branches from the anterior tibial artery and form a
complex vascular network. Additionally, the posterior tibial artery
provides numerous extraosseous branches to the medial malleolar area
and the posterior aspect of the distal metaphysis just proximal to the
tibial plafond. This extraosseous blood supply is at risk for
disruption during the injurious process, but is also at risk during
plate applications to the distal tibia.28
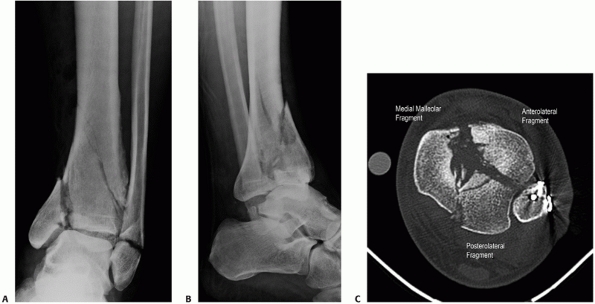
tibial plafond are nearly limitless, general fracture characteristics
have been observed. Frequently, the important ligaments of the ankle
often remain largely intact after a tibial plafond fracture and are
associated with the three commonly observed major fracture segments.
These three fracture fragments are the medial malleolar fragment, the
anterolateral (Chaput) fragment, and the posterolateral (Volkmann)15 fragment (Fig. 56-8).
In complete articular injuries (AO/OTA C-type fractures) these fracture
segments typically retain connections with portions of the deltoid
(medial malleolar segment), posterior tibiofibular ligament (posterior
malleolar segment), and anterior tibiofibular ligament (anterolateral
tibial segment). As the complexity increases, the number of fragments
and associated comminution increase. Often within these major fracture
segments central areas of comminution and impaction can be identified,
often corroborating the axial load and cephalad migration of the talus
within the distal tibial metaphysis at the time of injury. Partial
articular injuries may affect any aspect of the tibial plafond, but
most commonly involve the anterior plafond, medial malleolar segment,
or combinations thereof. It is critical in these partial articular
injuries to closely examine that portion of the intact tibial plafond
immediately adjacent to the fracture to identify subtle areas of
impaction. Clinically, the fractured edge of the intact segment
frequently demonstrates substantial chondral injury and small zones of
comminution that may frustrate an exact reduction. Using CT scanning,
Topliss has performed an extensive anatomic description of the major
fracture lines at the level of the tibial plafond, further delineating
the fracture morphology of the anterolateral, posterolateral, and
medial malleolar fracture fragments.169
 |
|
FIGURE 56-8 Anteroposterior (A) and lateral (B)
injury radiographs of a 42-year-old man after falling from a ladder. Initial displacement demonstrates varus angulation with anterior translation of the talus relative to the tibia. The associated transverse fibular fracture at the level of the tibial plafond indicates a tensile failure mechanism of the fibula. After fibular fixation and tibiotalar external fixation, the axial CT scan (C) demonstrates the three commonly identified major fragments: a medial malleolar fragment, an anterolateral (Chaput) fragment, and a posterior malleolar (Volkmann) fragment. Articular comminution is noted between all fracture fragments, most notably at the central intersection of all three fragments. |
consideration when managing fractures of the distal tibia. Unlike
rotational injuries of the ankle, axial-loading fractures of the tibial
plafond frequently demonstrate comminuted fibular fractures with
transverse and oblique fracture plane orientation. In a recent study,
fibular fractures appear to be more commonly associated with AO/OTA
C-type distal tibial plafond fractures than with partial articular
(B-type) patterns.14 Using a rank
order technique, this same study also determined that tibial plafond
injuries with fibular fractures appeared to be more radiographically
severe than those without fibula fractures.14
Compressive fibular failure is commonly seen with tibial plafond
fractures that present with valgus angulation, whereas tension fibular
failure is commonly identified with tibial plafond fractures that
present with varus angulation (Fig. 56-8). The
mechanism and inherent lack of stability associated with comminuted
fibular fractures that occur in the setting of tibial plafond injuries,
simple fixation devices, such as tubular plates, may be inadequate at
achieving the desired stability. Because a purely ligamentous failure
of the anterior and posterior distal tibiofibular ligaments is very
unusual,169 restoration of fibular
length, alignment, and rotation has a substantial impact on the
indirect realignment of the anterolateral and posterolateral tibial
plafond from their attachments to the anterior and posterior
tibiofibular syndesmotic ligaments. Any change in either the length or
the rotation of the distal fibula will be reflected in the
anterolateral and posterolateral segments of the distal tibia.
Similarly, because of the intimate articulation between the tibia and
fibula at the distal tibiofibular joint, angular deformity of the
distal fibula in any plane will have implications on distal tibial
reduction. Additionally, anatomic realignment of the fibula also
indirectly reduces the talus beneath the anatomic axes of the tibia. It
is equally as important to appreciate then, that fibular malalignment
or residual shortening can therefore have a substantial negative
impact on: (i) the ability to reduce the articular surface of the
distal tibia, (ii) restoration of distal tibial alignment, and (iii)
final position of the talus beneath the tibia. Any surgical approach
chosen should respect any remaining ligamentous attachments to these
structures.
tissue condition, open wounds, patient comorbidities, and surgeon
comfort determines the surgical approach(es) to be used. Open wounds
may or may not be extended as a component of the surgical approach.
Frequently, the soft tissues are the most traumatized over the distal
tibia and avoidance of incisions in this region may prove prudent. One
of the most important factors in choosing the appropriate surgical
approach for a given injury is the location of the fracture lines and
associated comminution. The most frequently used approaches for
articular injuries are the anterolateral and anteromedial.
stabilized through a separate exposure than the tibial fracture, the
surgeon must be aware of where the subsequent tibial incisions may be
placed to preserve an appropriate skin bridge between the two
exposures. Although historically a 7-cm skin bridge was routinely
recommended,108,120,157
Howard recently demonstrated minimal soft tissue complications with
skin incision bridges between 5 and 6 cm when treating tibial plafond
fractures.86 It should be
recognized, however, that the surgeons involved in Howard’s study are
located at a tertiary referral center that manages a high volume of
these injuries.86 Although a
straight lateral incision is typically performed for fibular fractures
associated with rotational ankle fractures, the skin incision for
fibular fixation when associated with a tibial plafond fracture should
be performed in a relative posterolateral location; specifically,
slightly posterior to the palpable posterior border of the fibula. This
allows for the use of the same incision if a posterolateral tibial
approach is later chosen, and increases the soft tissue bridge if an
anterolateral exposure is required for tibial fixation (Fig. 56-9).
Additionally, a posterolateral incision is not directly located over
the subcutaneous fibula, which may help to minimize wound complications
in this location.122
the lateral approach to the fibula begins just posterior to the
palpable posterior border of the fibula. The incision is longitudinal
and centered over the fibula fracture. Dissection is carried directly
through the subcutaneous tissue and the fascia of the lateral
compartment is incised longitudinally along the entire length of the
skin incision. The anterior edge of the incised fascia is then
retracted anteriorly and the peroneal musculature is retracted
posteriorly. To preserve vascularity to the skin, care is taken to
minimize the creation of planes between the subcutaneous tissue and the
fascia over the lateral compartment. Depending on the location of the
fracture, the superficial peroneal nerve may be encountered within the
lateral compartment before exiting the fascia and traveling within the
subcutaneous layer.
fractures requires planning for subsequent procedures based on the
injury pattern, associated open wounds, and soft tissue swelling. If
open reduction is anticipated, reestablishment of the length of the
tibia and fibula is necessary. This assists with resolution of soft
tissue swelling, and it also ensures that the definitive open
reduction, particularly of the articular surface, will not require an
acute intraoperative lengthening. The choice of surgical approaches
depends on the location and displacement of the major fragments and
local soft tissue conditions. Surgical exposures to the distal tibia
for the operative treatment of tibial plafond fractures include an
anterolateral Bohler approach,81 a straight anterior approach,151 an anteromedial approach,108,120,157 a straight lateral approach,77 a posterolateral approach,16,91 and a posteromedial approach.58
Over the last several decades, a greater understanding of the fracture
anatomy and importance of soft tissue preservation has occurred.
Percutaneous adjuncts, limited arthrotomies, and indirect articular
reductions have been described and clearly have a role in the
management of these challenging injuries.*
 |
|
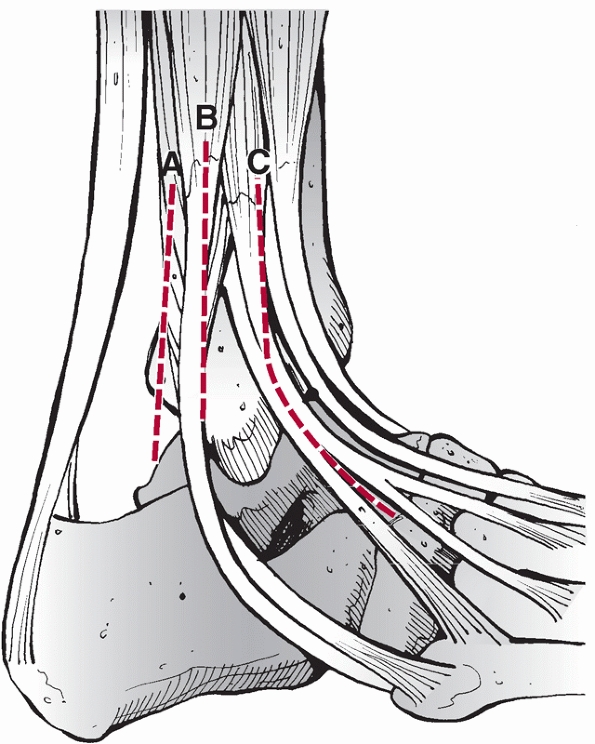
FIGURE 56-9
Schematic representation of the laterally based surgical approaches used for tibial plafond and associated fibular fracture management. The right ankle is viewed from the lateral vantage point. A. Posterolateral (tibia). B. Posterolateral (fibula). C. Anterolateral. |
anteromedial approach has been used for the open treatment of the
majority of comminuted tibial pilon fractures. This exposure is one of
the most extensile distal tibial exposures available, allowing adequate
visualization of a large percentage of the tibial plafond. It can be
used in virtually all complete articular fracture patterns, and is
especially useful in medial-sided partial articular injury patterns. In
particular, visualization and management of the central and medial
aspects of the tibial plafond is facilitated, as well as simultaneous
access to the medial malleolus, and the subcutaneous aspect of the
distal tibial metadiaphysis. The approach can be extended proximally to
address proximal fracture extension into the diaphysis if needed. The
obvious and main detraction from this exposure has been the reliance on
the survival of a large anteromedial skin flap that may already be
jeopardized from the injury. As a result, this exposure should only be
performed through a viable soft tissue envelope by a surgeon
experienced with the approach.
the traditional anteromedial exposure begins approximately 1 cm lateral
to the tibial crest and follows the course of the tibialis anterior
tendon. At the level of the ankle joint, the skin incision continues
distally and medially, ending at the distal tip of the medial
malleolus. The skin and subcutaneous tissue is elevated from the
underlying deep fascia only to a point at which the medial aspect of
the tibialis anterior tendon is identified. Immediately medial to the
tibialis anterior tendon, a full thickness incision directly to the
osseous surface of the anteromedial distal tibia is made. Ideally, the
deep dissection should not enter the tibialis anterior paratenon, but
this may be unavoidable as the dissection approaches the articular
surface as the periosteum begins to thin and the juxta-articular
metaphyseal fracture lines are encountered. Once the deep periosteal
layer is incised, the anteromedial skin, subcutaneous tissue, and
periosteum are elevated as a full thickness flap, akin to that
performed during the extensile lateral exposure for calcaneal reduction
and fixation. The anterior compartment is retracted laterally to allow
limited visualization of the lateral column of the distal tibia. The
joint is entered by longitudinally incising the capsule in the location
of the major anterior fracture line.
modification of the anteromedial approach has been recently described
by Assal that, in addition to allowing visualization of the anterior
and medial aspects of the distal tibia, facilitates improved
visualization of the lateral distal tibial metaphysis and lateral
articular surface.7 The main
disadvantage to this approach is similar to that for the standard
anteromedial approach. Additionally, because a more acute angle is
created at the level of the ankle joint, the skin of the tip of the
anteromedial skin flap may be more prone to necrosis.
the skin incision for the modified anteromedial approach begins
proximally approximately 1 to 2 cm lateral to the anterior crest of the
tibia and over the anterior compartment (Fig. 56-10).
This longitudinal component is continued distally to the level of the
tibiotalar joint at which point the incision curves medially to create
an angle between the vertical and the horizontal limbs of approximately
105 to 110 degrees. The horizontal incision extends to a point
approximately 1 cm distal to the tip of the medial malleolus, but
frequently terminates once the saphenous vein is identified. The medial
edge of the tibialis anterior tendon is identified and protected as the
extensor retinaculum and periosteum immediately medial to the tibialis
tendon sheath is incised sharply. A full-thickness skin, subcutaneous,
and periosteal tissue flap is then elevated from the distal tibial
metaphyseal region. Elevation of the anterior compartment with lateral
retraction allows improved access to the lateral aspect of the distal
tibia. Although sharing the same deep surgical dissection as the
standard anteromedial exposure, the modified anteromedial exposure
dissociates the course of the skin and subcutaneous incision from the
deep periosteal dissection, minimizing the skin and subcutaneous tissue
as a restriction to retraction of the anterior compartment,
facilitating visualization of the anterolateral distal tibia at the
level of the epiphysis.
approach avoids dissection over the tenuous soft tissue envelope of the
distal tibia and is an excellent alternative to the anteromedial
exposures. Although visualization of medial plafond comminution is more
difficult than with either of the anteromedial approaches, the
anterolateral approach otherwise allows excellent access to the vast
majority of the tibial plafond, particularly the lateral, posterior,
and central aspects. The exposure exploits the fracture involving the
anterolateral (Chaput) fragment, which, after the exposure is
performed, is manipulated and typically externally rotated on the
anterior tibiofibular ligament to allow access to the posterior and
central aspects of the plafond. Anterolateral plate application is
simplified with this exposure because the contents of the anterior
compartment are retracted medially. If needed, medial implants can be
placed percutaneously or through a separate medial malleolar approach.
The anterolateral approach for fractures of the tibial plafond is an
extension of the previously described Bohler approach.81
with the fourth ray and travels over the anterolateral aspect of the
distal tibia (Fig. 56-11). Because of the
origin of the anterior compartment musculature, the maximum proximal
extent of the incision is limited to approximately 7 cm. Distally, the
incision
terminates
at the predicted location of the talar head. Although its location is
variable, the superficial peroneal nerve and/or its arborizations are
almost universally identified immediately within the subcutaneous fat.
The nerve and its branches are mobilized to allow retraction either
medially or laterally. The distal extent of the fascia overlying the
anterior compartment and its confluence with the extensor retinaculum
are identified. With close observation, the tendons of the anterior
compartment musculature can be identified through the retinaculum,
allowing the superior and inferior extensor retinaculum to be incised
longitudinally, immediately lateral to the course of the long toe
extensor tendons and peroneus tertius. The longitudinal incision in the
retinaculum is carried proximally through the fascia of the anterior
compartment. The entire contents of the anterior compartment are then
retracted medially to expose the underlying anterolateral aspect of the
distal tibia and the capsule of the ankle joint. Care is taken when
inserting retractors below the anterior compartment as the anterior
neurovascular bundle (anterior tibial artery and vein, and deep
peroneal nerve) may be entrapped within anterior fracture fragments or,
after 1 to 2 weeks from the time of injury, adherent to this region. A
longitudinal capsulotomy is performed at the medial extent of the
Chaput fragment, thereby exposing the tibiotalar articulation.
Transversely oriented capsular vessels are often encountered and
require ligation or cauterization. The central and posterior aspects of
the tibial plafond are accessed by externally rotating the
anterolateral (Chaput) fragment on the anterior distal tibiofibular
syndesmotic ligaments. A summary of the relative placement of skin
incisions for anterior exposures of the distal tibia is demonstrated in
Figure 56-12.
 |
|
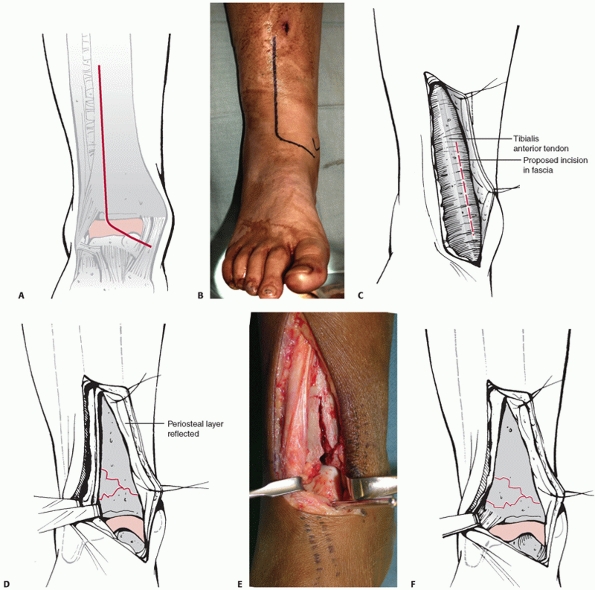
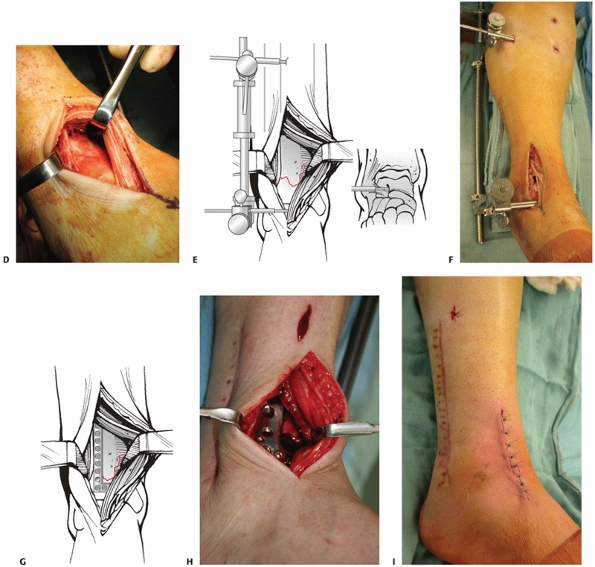
FIGURE 56-10 A. Illustration and (B)
clinical example of the modified anteromedial skin incision. Note the approximate 105- to 110-degree angle between the vertical and horizontal limbs of the incision. C. Illustration demonstrating the identification of the medial aspect of the tibialis anterior tendon. Care is taken to not undermine the medial skin flap significantly beyond this region. D. Illustrated and (E) clinical example demonstrating elevation of the medial skin, subcutaneous, and periosteal flap medially and retraction of the anterior compartment laterally allowing exposure of the anteromedial aspect of the distal tibia. F. Illustration demonstrating retraction of the anterior compartment laterally, with (continues) |
 |
|
FIGURE 56-10 (continued) (G) subsequent plate fixation applied to the anterolateral aspect of the distal tibia. H. Corresponding clinical example. I.
Illustration demonstrating relative positions of the anterolateral and medial plate fixations to the surgical incision. Note that the skin has been sutured using an Allgower-Donati technique with the knots tied at the periphery of the incision. |
 |
|
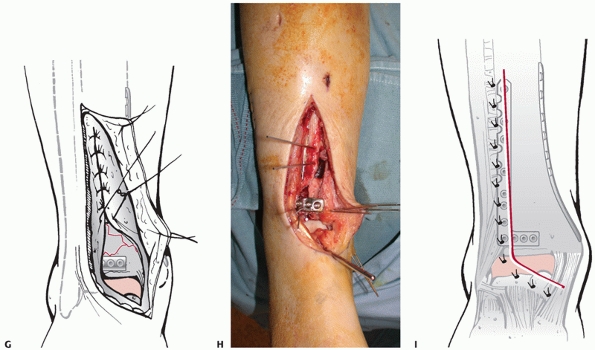
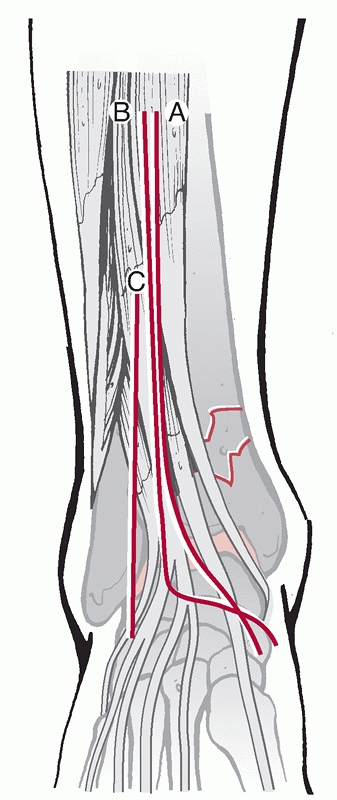
FIGURE 56-11 Illustration (A) and clinical example (B)
of the anterolateral exposure for a fracture of the tibial plafond. The incision is longitudinally oriented, in line with the fourth ray. Illustrated (C) and clinical (continues) |
 |
|
FIGURE 56-11 (continued) (D)
example of the anterior compartment mobilized medially. A laterally based universal distractor is applied to facilitate visualization of the articular surface (E,F). Note the course of the superficial peroneal nerve. Anterolateral plating is performed (G,H), and the wound is closed with an Allgower-Donati suture technique (I). |
approach is an extremely useful exposure to access and manipulate the
posterior aspect of the tibial plafond.16,91
It is most useful for those AO/OTA B-type tibial pilon fractures in
which the unstable articular segment is located posteriorly and has no
significant articular comminution. Although it is uncommonly used in
isolation for the management of AO/OTA C-type tibial pilon fractures,
it can be used in conjunction with anterior exposures to adequately
reduce and stabilize the entire articular surface. AO/OTA C-type
fracture patterns most amenable to this adjunctive approach include:
(i) those with complete dissociation of the posterolateral (Volkmann)
fragment from the fibula, especially those that remain substantially
displaced despite anatomic reduction of any associated fibula fracture,
and (ii) articular injury patterns that demonstrate a large but
minimally comminuted posterior plafond fragment that can be
anatomically reduced to the posterior metadiaphysis (Fig. 56-13).
In this latter scenario, a posterolateral approach can be used for
effectively converting a C-type tibial pilon fracture into a B-type
pattern.58 Because of the
orientation of the tibial plafond, once the posterior or posterolateral
portion of the tibial plafond is reduced, direct visualization of the
articular surface is extremely difficult if not impossible with this
exposure. The articular reduction is largely indirect, and is
accomplished by visual inspection of any available posterior cortical
interdigitations, and is confirmed radiographically. Fibular fixation
through the same skin incision is also possible. Because this exposure
can be performed in conjunction with operative fixation of the fibula,
it is imperative that the surgeon considers all anticipated subsequent
skin incisions when proceeding with the surgical management of these
fractures. A poorly positioned fibular incision may substantially
jeopardize the ability to use the posterolateral exposure.
 |
|
FIGURE 56-12 The relative placement of skin incisions for (A) the classic anteromedial, (B) modified anteromedial, and (C) anterolateral surgical exposures for the management of tibial plafond fractures is demonstrated.
|
patient in either the lateral or prone position. The longitudinally
oriented skin incision is placed midway between the lateral aspect of
the Achilles tendon and the posterolateral aspect of the fibula. Care
is taken to avoid injury to the sural nerve. The deep fascia is incised
and the peroneus brevis and longus musculature are retracted
anterolaterally. The flexor hallucis longus (FHL) muscle and its
overlying fascia are subsequently identified. The distal origins of the
FHL are then elevated from lateral to medial off the posterior aspect
of the fibula and interosseous membrane; the muscle belly is then
retracted posteromedially to expose the posterolateral aspect of the
distal tibia.84 During this
dissection, the peroneal artery and accompanying veins may be
encountered immediately posterior to the fibula, and require
coagulation. By simply retracting the peroneal musculature
posteromedially, an associated fibular fracture can be visualized,
reduced, and stabilized (see Fig. 56-7 D′).
uncommonly required for the management of tibial pilon fractures.
Occasional indications include posterior pilon variant fractures with
substantial central and/or posterior comminution with an intact
anterior plafond, or the tibial pilon fracture with an associated large
posteromedial fragment that can be accessed and secured at its
metadiaphyseal junction.58 The
posteromedial approach can be accomplished with the patient in the
supine or prone position. If the patient is in the supine position, a
small soft support is placed under the contralateral
buttock
and flank region, thereby facilitating external rotation of the injured
leg. Occasionally the prone position is used and allows an easier
trajectory for the insertion of screws and provisional stabilizing
wires. The incision is typically halfway between the medial border of
the Achilles tendon and the posterior aspect of the medial malleolus.
Once the tarsal tunnel is entered, the neurovascular bundle is
identified and protected. The specific deep interval depends on the
fracture type and the access needed, however, once the neurovascular
bundle is mobilized, dissection can proceed through any interval within
the tarsal tunnel. A modification of the deep exposure is to incise the
deep periosteum and origin of the tarsal tunnel sharply from the
posteromedial edge of the tibia. The entirety of the tarsal tunnel can
then be retracted posterolaterally without disturbing any of its
contents (see Figure 56-7).
 |
|
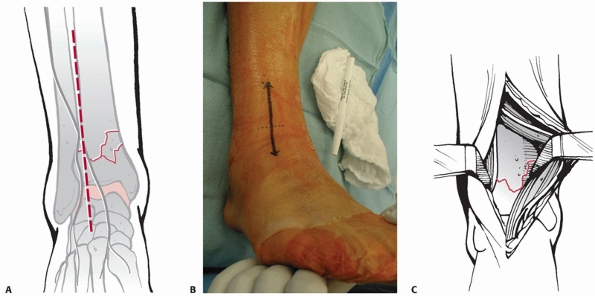
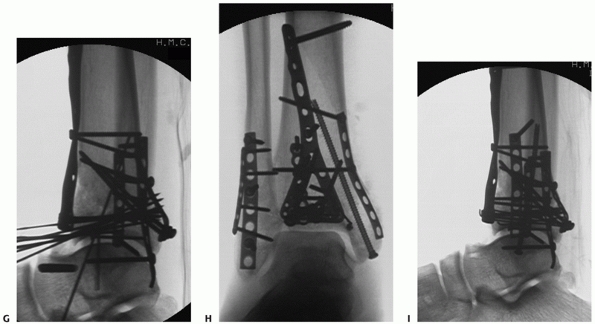
FIGURE 56-13 Injury anteroposterior (A) and lateral (B)
radiographs of a 32-year-old man involved in a moderate speed motor vehicle collision. The lateral radiograph demonstrates marked displacement of the posterolateral fragment from the distal tibia (C,D). Although markedly improved after fibular reduction via a posterolateral incision, substantial residual displacement of the posterolateral articular surface (*) remains. The white arrow denotes an impacted central plafond fragment. Provisional (E) and definitive (F) fixation of the posterolateral articular fragment performed using the posterolateral surgical incision. (continues) |
lateral approach has been advocated as a soft tissue-friendly technique
by which both the fibula and tibia can be exposed, reduced, and
stabilized through the creation of a single robust thick soft tissue
flap.77 Relative contraindications
to this approach are: (i) fractures lines that cannot be easily
accessed, particularly medial-sided impaction; and (ii) those injuries
that demonstrate wounds or soft tissue compromise that prevent
extensile incisions
from
safely being made along the anterior border of the fibula. The
reduction sequence is similar to that performed during the
anterolateral approach.
 |
|
FIGURE 56-13 (continued) At the conclusion of fixation, the distal tibia was managed with spanning external fixation (G-I).
After resolution of soft tissue swelling, the remainder of the tibial plafond was reduced and stabilized using a modified anteromedial approach. (continues) |
the most proximal fracture line (either fibular or tibial) and
extending 3 to 4 cm distal to the joint. The anterior border of the
fibula is identified, and the dissection is then carried posteriorly to
expose and posterior retraction of the peroneal musculature allow
subsequent fibular reduction and fixation. Tibial exposure is performed
by careful blunt dissection over the anterior edge of the fibula to the
interosseous membrane. The plane between the interosseous membrane and
the overlying contents of the anterior compartment is developed with a
periosteal elevator. The anteroinferior tibiofibular ligament is then
identified and followed medially to the anterolateral (Chaput) fragment.77
Depending on the fracture configuration, this fragment can be displaced
to allow visualization and manipulation of central and posterior
plafond fragments.
fractures that are truly nondisplaced or for those patients who have a
significant or absolute contraindication to surgical management.
Depending on the magnitude of articular injury and the degree of
fracture instability, patients treated using nonoperative methods can
be managed with closed manipulative reduction and cast immobilization.
Progressive weight bearing with ankle and subtalar range of motion is
initiated based on radiographic healing. Severely injured or ill
patients with marked fracture instability, displacement, and
substantial soft tissue injury can be treated with calcaneal pin
traction166 and transitioned into a
cast when the overall condition of the patient and limb allow.
Indications for nonoperative management of displaced intraarticular
fractures of the tibial plafond are extremely limited.
immobilization often did not prevent the talus from its natural
tendency to displace anteriorly and superiorly, recognizing that
maintaining the normal tibiotalar relationship was an important
component of restoring ankle function.147
Ayeni found that while closed treatment and casting gave good results
in minimally displaced fractures (Ruedi type I), a substantial number
of poor results occurred in displaced fractures, and felt that casting
was not even applicable in those with significant comminution.8
In a small comparative series, Kellam noted that, in both rotational
and compression types of tibial plafond injuries, the results of
operative treatment were superior to the results of nonoperative
treatment.89 The best results of
nonoperative treatment in that study occurred in those rotational
injuries that did not displace over the duration of closed management.
Bourne evaluated the results of 42 tibial pilon fractures classified
according to the Ruedi-Allgower system.33,34
In all fracture types, the authors noted worse results with closed
treatment compared with open treatment, with universally poor results
noted with increasing comminution and displacement (Types II and III).33,34
Collectively, the conclusion of these studies and others is that
casting is ineffective in maintaining limb length and reducing impacted
articular segments, particularly in axial loading injuries with
significant displacement and comminution. In those intraarticular
distal tibia fractures with an intact fibula, the persistent varus
tendency makes maintenance of limb alignment with nonoperative
techniques difficult. Similarly, displaced partial articular injuries
frequently demonstrate talar subluxation within the
mortise
that cannot be effectively managed with closed techniques. Despite the
shortcomings of closed treatment, this management method is preferred
in a small number of patients, such as those that are bedridden or that
have minimal ambulatory capacity or functional demands. Additionally,
patients with significant associated medical comorbidities,
particularly those that substantially affect bone and soft tissue
healing, may be candidates for closed treatment.
managed operatively; particularly those with displaced intra-articular
fracture fragments. Nevertheless, the ideal treatment has yet to be
determined.190 Unstable, displaced
extra-articular distal tibial fractures can be treated with numerous
techniques including external fixation,3,52 open or percutaneous reduction and plate fixation,* medullary nailing,90,119,123,141
and combinations thereof. The fracture pattern and conditions of the
local soft tissue envelope are the major determinants for the surgical
technique chosen. These same principles apply when managing
intra-articular fractures of the distal tibia.
displaced intra-articular distal tibial plafond fractures strongly
suggest that the tibiotalar joint poorly tolerates articular
incongruity and talar subluxation.8,34,89,128,147
The degree to which residual articular incongruity affects long-term
functional outcomes, posttraumatic arthrosis, and the need for further
surgical intervention, however, remains controversial.101,105
Although there are no strict guidelines for determining how much
articular step-off or gap can be tolerated, a visible incongruity at
the tibial plafond that is demonstrated on plain radiographs should be
considered an indication for operative reduction and fixation in
properly selected patients. Associated angular malalignment and/or
talar subluxation further jeopardize tibiotalar joint function,
especially with associated articular incongruity, and are strong
indications for operative management.
in the management of tibial pilon fractures, and can be used as a
definitive treatment method or in combination with staged open
reduction and internal fixation. In this latter scenario, external
fixation is used to temporarily maintain gross fracture alignment and
stability while awaiting soft tissue recovery and definitive ORIF; and
the external fixation device always crosses and immobilizes the ankle
joint by incorporating the foot into the construct. In the former
scenario, the most common rationale for the use of external fixation is
to obtain and maintain reduction of the distal tibial metaphyseal
fracture, obviating the need for plate stabilization of this area,
thereby decreasing the risk of significant wound complications
previously associated with open plate fixation. Although Bone reported
successful results with ankle spanning external fixation in severe
tibial pilon fractures,21 concerns
regarding prolonged bridging of the ankle joint gave rise to two
solutions: the use of hybrid or ring external fixation that allows
distal fixation to be terminated within the distal tibial segment, or
the use of an articulated external fixator with a hinge that allows
ankle motion but minimizes fracture motion. These devices have the
theoretical benefit of maintaining ankle joint motion during the
osseous healing phase. When using external fixation devices, the
surgeon has the option of managing the articular reduction with true
open reduction techniques via standard incisions and approaches or
using limited incisions combined with percutaneous screw insertions.
available that stabilize distal tibia fractures externally purely on
the tibial side of the tibiotalar articulation. Clinical utilization
has been reported using Ilizarov fine wire ring fixators,**
hybrid fixators that typically use bars to connect fine wire fixation
of the distal tibial segment to half pin fixation proximally,*** and pin only fixators.47
All of these fixators have successfully decreased wound complication
rates compared with older plating techniques. Although some infections
over the distal tibia are still reported, ranging from 4% to 13% in
several series,6,76,87,171
the union rate has been generally high, with 75% to 81% good and
excellent results being reported. Disadvantages of tibiotalar sparing
external fixation include the narrow safe corridors available for wire
placement may result in tendon impalement or neurovascular injury.125,178
Because stability of the distal tibial metaphysis is dependent on
stable fixation into the epiphyseal segment, certain comminuted distal
tibia fractures are not amenable to same-side external fixation, with
some authors suggesting that the presence of 2 cm of intact bone is
necessary to achieve adequate stability.76 Although less common than seen in the tibial plateau,87 septic arthritis of the ankle secondary to juxta-articular wires at the level of the tibial plafond have been reported.6,87
This indicates that there remains a risk of significant deep wound
complications when placing external fixator pins or wires in the zone
of injury to stabilize high-energy distal tibia fractures. Very distal
injuries, therefore, represent a therapeutic conundrum, because pins
placed within 2 cm of the joint line, particularly when traversing the
distal tibiofibular articulation, may be intracapsular and a subsequent
superficial infection of these pins can develop into septic arthritis.95,179
the clinical results of patients treated with either ankle joint
sparing external fixation or open reduction and internal fixation.6,11,137,180 Pugh and colleagues evaluated 60 patients with tibial pilon fractures, 15 of whom were treated with hybrid external fixation.137
Although no significant differences in patient characteristics were
noted between the external fixation group and the open plating group,
four of the patients with hybrid fixation developed malunions, and the
loss of the initial adequate reduction was independent of bone grafting
or fibular fixation. Watson and colleagues developed a staged treatment
protocol based on the severity of the soft tissue injury in 107
patients with tibial plafond fractures.180
In this study, all patients diagnosed with tibial pilon fractures
underwent immediate temporary stabilization followed by delayed
definitive stabilization. In those patients with closed fractures, the
initial treatment consisted of calcaneal traction and placement of the
limb into a Böhler-Braun frame. Those with open fractures,
compartmental
syndrome, or other injuries necessitating operative care, were
initially managed with a temporary two-pin quadrilateral spanning
external fixation frame using a proximal tibial transfixion pin and a
similar transcalcaneal pin. All tibial pilon fractures were
subsequently evaluated with a CT scan, and the soft tissue injury was
then classified using the Tscherne and Gotzen system for closed
fractures and the Gustilo and Anderson system for open fractures.
Patients with minor abrasions, contusions, and/or indirect soft tissue
injury (Tscherne grades 0 and 1) were treated with open plating
techniques using AO principles. Open fractures and those with higher
grade Tscherne closed soft tissue injuries were treated with limited
incision articular reduction and stabilization followed by definitive
stabilization with small wire circular external fixation. For all
fracture types according to the AO/OTA classification, 81% of those
treated with external fixation and 75% of those treated with open
plating procedures had a good or excellent result. Nevertheless, those
with more severe fracture patterns (AO/OTA C-type), regardless of which
treatment group they belonged to, demonstrated significantly poorer
results than patients with type A or B fractures. In this study,
patients with C-type fractures had higher rates of nonunion, malunion,
and severe wound complication rates in the open plating group than
those in the external fixation group. Anglen evaluated 63 patients
treated with either hybrid external fixation or open plating.6
The study noted that those patients treated with hybrid external
fixation demonstrated lower clinical scores, slower return to function,
and a higher rate of nonunion, malunion, and infection when compared
with patients treated with internal fixation. Despite the hybrid
fixation group being composed of subjectively worse injuries, the
author concluded that notwithstanding the optimistic results reported
in the literature, hybrid fixation did not seem to solve the problems
inherent in severe pilon fractures.6
Most recently Bacon performed a retrospective analysis of tibial
plafond fractures treated with either open plating or Ilizarov fixation.11
Based on their extensive review, the authors found no statistically
significant differences in overall complication rates, deep sepsis,
time to union, nonunion, and malunion. The authors concluded that no
clinical recommendation could be made as to which procedure is better
and safer for the patient, citing the need for future randomized trials.
method to temporarily stabilize the ankle, particularly in the setting
of a high-energy tibial plafond fracture and is typically applied soon
after the injury in an initial surgical procedure followed by a planned
second operation after a delay of days or even weeks.17,56,83,135,156
It is less commonly used, however, as the definitive method to
neutralize forces during fracture repair. One of the most significant
advantages of transarticular spanning external fixation is that it is
technically the easiest to apply. Additionally, because the zone of
injury is not typically violated during its application, it is also the
safest to apply since the fractured distal tibia and the surrounding
injured soft tissue envelope remain unviolated by the skeletal fixation
elements. Until a definitive treatment plan has been decided upon,
temporary transarticular spanning external fixation indirectly
maintains limb length, alignment, and rotation, which facilitates soft
tissue recovery and does not preclude other definitive treatment
methods, such as the later application of plates, screws, conversion to
hybrid or Ilizarov fixation, or combinations of these. Alternatively, a
spanning fixator may be used as the definitive method to stabilize the
distal tibia.17,21,56
The spanning fixator functions to neutralize the fracture, and the
articular surface is reduced and internally fixed, either
percutaneously or through limited open approaches or more extensive
open reduction. Cited disadvantages of definitive tibiotalar spanning
external fixation for tibial plafond fractures include ankle and
hindfoot stiffness, loss of reduction, malunion, and poor overall
outcome compared with open techniques.9,17,56,137
use a hinge that is approximated to the center of rotation of the ankle
enabling limited ankle movements during the treatment period. Initially
the fixator can be used to distract the tibiotalar joint to facilitate
articular visualization and reduction. The device is subsequently used
to maintain reduction of the distal metaphysis. According to Marsh, one
of the hindfoot pins is incorporated into the talus, allowing precise
control of the talar position beneath the tibia and also facilitates
partial reduction of the distal fibula, often eliminating the need to
fix the fibula internally.104
Nevertheless, because the neurovascular bundle and the subtalar joint
are in the immediate proximity, precise positioning of pins inserted
into the hindfoot is required. Inaccurate centering of the hinge
relative to the approximate axis of ankle rotations will limit the
amount of postoperative ankle motion. Additionally, because pins are
placed into both the talus and the calcaneus, the subtalar joint is
immobilized while the fixator is in place. Marsh prospectively examined
31 fractures at an average of 30 months after the injury treated with
medial articulated external fixation and minimal incision articular
reduction and stabilization.100
There were no deep infections, and although one third of patients
reported a satisfactory or excellent result, almost half were scored as
unsatisfactory.100 Additional
clinical experience with the articulated external fixator for tibial
plafond fractures has also demonstrated a low incidence of significant
complications, high union rates, and reasonable patient outcomes.**
successful results with the use of articulated external fixation,
particularly related to minimization of wound complications,55,100,149,172 the benefits of early ankle motion with this device remain inconclusive.102
Additionally, although cadaveric mechanical evidence has demonstrated
that during ankle movement through a well-aligned articulated hinge
results in minimal distal tibial segment motion,32,65
Marsh, in a randomized trial, identified three patients treated with
articulating external fixation that demonstrated delayed fracture
healing when compared with patients treated with similar but static
ankle spanning external fixation devices.102
The inference is that the delay to union in those patients may have
potentially been caused by motion occurring at the metaphyseal fracture
site rather than at the intended tibiotalar articulation.
for the management of distal tibial fractures is to maintain tibial
length, alignment, and rotation until union has occurred with minimal
additional
soft tissue injury from the surgical treatment. Reduction is obtained
indirectly using ligamentotaxis. The surgeon, however, has options
regarding the management of the articular injury. One technique is to
perform a true open reduction using standard surgical approaches. The
articular surface is visualized, secured with a series of screws, and
the external device is used to neutralize the metaphyseal injury.
Another technique is to perform limited or small incision reductions,
with fixation using screws or percutaneous wires. The technique for
limited incision reduction requires that the surgeon have a clear
understanding of the articular fracture morphology from the CT scan and
be able to subsequently plan the location and direction of lag screws
or tensioned small-diameter olive wires to achieve articular reduction
and interfragmentary compression. Having a thorough understanding of
the fracture morphology from the CT scan facilitates interpretation of
intraoperative fluoroscopic views of the quality of reduction. Last, in
certain situations, open reductions of the articular surface of any
sort are contraindicated because of soft tissue constraints or
associated injuries that prevent patients from undergoing a prolonged
operative procedure (Fig. 56-14).
In these situations, restoration of distal tibial alignment and
maintenance of the talus centered beneath the mechanical axis of the
tibia are the main objectives. Provided that union is achieved with
satisfactory alignment, subsequent reconstructive procedures in these
patients may be facilitated by the lack of prior surgical incisions and
implants.
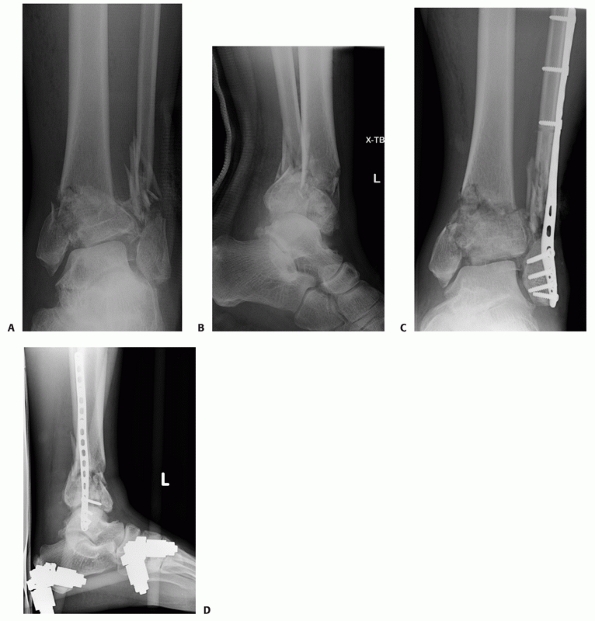 |
|
FIGURE 56-14 Injury anteroposterior (A) and lateral (B)
radiographs of a 68-year-old man involved in a motor vehicle collision. Associated comorbidities include hypertension and a smoking history. The physical examination demonstrated a severe closed soft tissue injury particularly along the anterolateral aspect of the distal tibia. He was treated acutely with open treatment of his comminuted fibula fracture and spanning external fixation of the tibial plafond fracture (C,D). (continues) |
the definitive management for a displaced fracture of the tibial
plafond, associated displaced fibula fractures are invariably managed
with operative stabilization. The importance of this was illustrated by
Ruedi, as he included the reconstruction of correct fibular length as
the first of the four sequential principles in the successful open
treatment of these fractures.144,145 The treatment of coexisting fibular fractures when using external fixation,
however, remains more controversial. Although many authors suggest that this step is beneficial in aligning the limb,69,76,99,121,126
Williams, in a study of tibial plafond fractures treated with external
fixation, noted significant complications associated with fibular
plating, including wound infections, nonunions, and malalignment.183
Late varus deformity, particularly with early frame removal, was noted
by French and Tornetta, who concluded that plating of the fibula is not
indicated when pilon fractures are treated with limited open reduction
and external fixation.67
 |
|
FIGURE 56-14 (continued) Two weeks after his injury, the severity of his soft tissue injury is still evident (E).
Open treatment would likely have required soft tissue transfer or coverage but his nicotine use, hypertension, and age precluded this as a realistic option. He was definitively treated with tibiotalar spanning external fixation, modifying the external fixator to incorporate the lateral column of the foot, and to insert a tibial pin closer to the metaphyseal fracture (F-H). At 9 months, his fracture and soft tissue envelope have healed. Substantial articular incongruity remains and the prognosis for long-term satisfactory joint function is guarded (I,J). |
for fractures involving the tibial plafond, Ruedi and Allgower
described the essential principles for successful open reduction and
internal fixation. The principles described over 20 years ago remain a
solid foundation and still continue to guide many current treatment
decisions.9,146
The original description of these four principles consisted of
restoration of anatomic fibular length, anatomic restoration of the
distal tibial articular surface, bone grafting of metaphyseal defects,
and stable fixation of the fracture with medial buttress plating.
Although some flexibility is required when managing these challenging
injuries, these basic principles remain the foundation for formulating
a surgical tactic. Although formal open reduction with internal
fixation can achieve optimal articular reduction and distal tibial
reconstruction, there is no question that wound complications and deep
infection have plagued this form of treatment.33,34,57,110,165,187
Nevertheless, when critically assessed, a consistent feature of the
failures of open reduction and internal fixation appears to be the
timing of the procedure relative to the injury. In their 5-year
experience with internal fixation of pilon fractures, McFerran reported
a 40% major complication rate, the majority caused by soft tissue
complications and infections.110 The
mean time delay between injury and definitive surgery was approximately
4.5 days, with 46% of patients operated upon within 36 hours. Teeny and
Wiss evaluated 60 tibial plafond fractures treated with open reduction
and plate fixation noting that poor results occurred in 50% of cases,
with a 37% deep infection rate in comminuted pilon fractures.165
This latter finding was strongly correlated with a surgical
postoperative wound infection, squarely placing the complication on the
shoulders of the treatment. In that study, closed fractures were
operatively managed an average of 6 days after injury. Wyrsch and
colleagues, in a prospective study, reported a near 40% soft tissue
complication rate in patients treated with primary ORIF.187
In that study, the average time to surgery in the closed fracture group
was 5 days. All of the preceding authors recognized that open reduction
and internal fixation techniques in a previously underappreciated
traumatized soft tissue envelope was a causative factor in the
development of significant wound complications and poor outcomes.
substantial reassessment of the optimal treatment for these injuries.
Although the concept of delayed definitive open reduction and internal
fixation to allow soft tissue recovery had been previously described,83,108 Sirkin’s influential study popularized staged treatment of these injuries.156
The authors acutely managed displaced tibial plafond fractures with a
closed manipulative reduction and the immediate application of
temporary transarticular external fixation. When fractured, open
reduction internal fixation of the fibula was also performed acutely.
Definitive open reduction and internal fixation of the tibia was then
performed an average of approximately 13 days later in the closed
fracture group, and 14 days later in the open fracture group.156
The time to definitive tibial fixation was predicated on resolution of
edema, and was a clinical determination. Using this technique a
dramatic decrease in early soft tissue complications, and later
problems of osteomyelitis and deep sepsis was noted. In a total of 46
fractures, the authors identified three deep septic complications, two
of which occurred in open fractures. Using a similar protocol,
Patterson and Cole had no cases of superficial or deep wound
complications in 21 patients followed an average of 22 months.135
Currently, definitive open reduction and internal fixation through
formal operative distal tibial exposures requires a critical assessment
of the soft tissue envelope. Although not all patients with tibial
plafond fractures will demonstrate significant soft tissue injuries,
many patients who present with high-energy tibial plafond fractures
have fracture blisters, deep contusions, and early onset of significant
edema. This patient group may also sustain other injuries that require
evaluation and treatment, often delaying operative orthopaedic
intervention to a point in time in which soft tissue swelling obviously
precludes definitive care. It is imperative therefore that the surgeon
recognizes the magnitude of any associated soft tissue injury and that
the development of a surgical tactic considers timing and soft tissue
recovery. Although the optimal time to surgery remains controversial,
surgery is often delayed for at least 10 days to allow wrinkles to
return, blisters to reepithelialize, and wounds to heal. At this
approximate time delay, the soft tissues enter the reparative phase and
are able to tolerate surgical intervention. Because of the typical
shortening, displacement, and instability seen with tibial plafond
fractures, particularly those considered to be associated with
high-energy mechanisms, simple splintage or casting of these fractures
for 10 to 21 days before operative intervention makes definitive tibial
reduction markedly more difficult and prolongs time to recovery of the
soft tissue envelope. Because of this, most surgeons who use formal
open reduction and internal fixation for these injuries currently favor
the two-stage treatment protocol described to promote recovery of the
traumatized soft tissue envelope before definitive fixation.135,156
wound complications with open reduction and internal fixation has been
entirely attributable to a delay in treatment, as improvements in soft
tissue handling,* the use of lower profile implants,93,154,186
the use of percutaneous and limited incision exposures, and a better
understanding of fracture and fixation mechanics were introduced
concurrently, and have all contributed to decreasing significant wound
complication rates. Although the bulk of unfavorable data used to
condemn open reduction and internal fixation have focused on wound and
soft tissue complications, the results of many of these studies are
also confounded by the inability to have achieved stable internal
fixation and/or anatomic reductions. Of 11 patients reviewed by Dillin,
only one had plate stabilization of the tibia, with the authors noting
that poor results in their series may be secondary to their
inexperience with the AO techniques described by Ruedi and colleagues.57 Similarly, of the 16 comminuted tibial
pilon fractures treated with open reduction and internal fixation,
Bourne noted that anatomic reduction and stable fixation were achieved
in only two.34
Teeny and Wiss noted that 37% of their Reudi type II and 30% of Reudi
type III tibial plafond fractures were unable to be anatomically
reduced.165 They also noted that
loss of fixation, fracture displacement, and implant failure were
present in 30% of Reudi type III fractures. Wrysch noted that an
increasing number of nonanatomic reductions occurred in fractures with
increasing comminution (Reudi type III).187
What is apparent from these studies is that open reduction and internal
fixation of comminuted tibial plafond fractures is difficult, and that
if one does not attain an anatomic reduction and stable fixation, and
is performed through an intolerant soft tissue envelope, the outcome
will likely be poor.
fractures of the tibial plafond with staged open reduction and internal
fixation, with the goals being anatomic articular reduction, and
anatomic restoration of length, alignment, and rotation of the distal
tibia. This treatment method requires strict attention to the
formulation of a surgical tactic at each intervention so as not to
compromise the final result and minimize the risk of deep wound
complications.
and stabilization, but primarily as it relates to stabilization of the
soft tissue envelope. This initial stage is performed as an urgent
surgical procedure as soon as the patient’s general condition permits.
In the author’s opinion, this component of treatment is as critical as
the definitive tibial reduction. In particular, fibular reduction
should be as exact as possible, as any malreduction will likely impact
the ability to obtain an anatomic reduction of the articular surface of
the tibial plafond. Additionally, because the talus typically tends to
follow the fibula, fibular malalignment may result in the talus not
being centered beneath the anatomic axis of the tibia, or distal tibial
metaphyseal malalignment. Poorly placed skin incisions or external
fixation pins can jeopardize the success of the subsequent stage (Fig. 56-15).
It is also the author’s opinion that, if possible, the surgeon
performing the initial stage should also perform the definitive stage,
or share a similar management philosophy. Decisions and treatments that
are rendered during this initial stage often have significant impact on
the final result, and should not be performed by an inexperienced
surgeon under the assumption that this stage is “simple” or only
“provisional.”
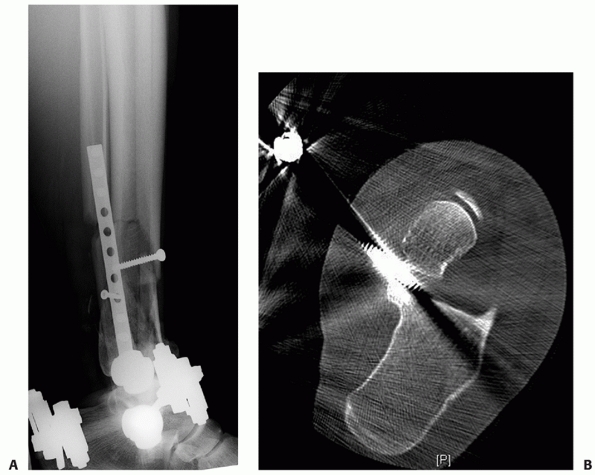 |
|
FIGURE 56-15
This patient sustained an open tibial plafond fracture with an associated fracture of the fibula. In addition to an operative débridement, open plating of the fibula and application of a spanning external fixator was applied before referral to our institution. A. The lateral radiograph demonstrates inadequate fibular reduction with apex posterior deformity. Note the obligatory anterior translation of the talus relative to the mid-diaphyseal line of the tibia. B. Axial CT scanning demonstrates an errant Schanz pin placed through the middle facet of the subtalar joint. |
anticipation of all skin incisions (for this and later stages),
débridement of any open wounds, a four-compartment fasciotomy if
required, open reduction and internal fixation of an associated fibular
fracture, and closed manipulative reduction and temporary spanning
external fixation of the tibial plafond fracture. Ankle and tibia plain
radiographs are assessed to determine the degree, magnitude, and
direction of displacement and angulation of the tibia and fibula.
Determining whether an associated fibula fracture failed predominantly
in compression, tension, or rotation aids in the selecting the type of
fibular fixation. Radiographs of the ipsilateral foot are useful to
ensure that there are no injuries of the calcaneus
or
midfoot that may compromise potential placement of an external fixator
pin. In a small subset of tibial plafond fracture patterns, extension
of the fracture may propagate into the diaphysis. Occasionally acute
reduction and stabilization of this fracture component during the
initial stage may facilitate the subsequent stage of definitive
articular and axial reductions and fixations.58
operating table with a radiolucent extension. A small soft supportive
bump or towel roll is placed beneath the ipsilateral buttock, flank,
and shoulder region to minimize the tendency for the entire limb to
externally rotate. A foam ramp or pillow is placed beneath the injured
leg to slightly flex the ipsilateral hip and knee, allowing easier
access to the posterolateral aspect of the fibula and to facilitate the
lateral fluoroscopic view of the foot, ankle, and tibia. The
ipsilateral arm is placed across the chest to avoid a traction injury
to the brachial plexus. All bony prominences should be padded,
particularly the fibular head and lateral malleolar regions of the
contralateral leg. A tourniquet is rarely used for this procedure.
lateral approach to the fibula already described. Placement of the
incision just posterior to the palpable posterolateral border of the
fibula ensures that access to the posterolateral aspect of the distal
tibia can be performed if needed, while still allowing ample access to
the fibular fracture.
integral part of the initial management of these injuries for several
reasons. First, restoration of accurate fibular length, alignment, and
rotation indirectly reduces the majority of tibial deformity secondary
to the ligamentous and other soft tissue attachments between the two
bones. Second, after fibular reduction and fixation, residual tibial
displacement can be managed with a medially based ankle joint-spanning
external fixator using the reduced and stabilized fibula as a fulcrum.
Third, anatomic reduction of the fibula
facilitates indirect reduction of the associated anterolateral (Chaput)
and posterior (Volkmann) tibial articular fragments via the anterior
and posterior distal tibiofibular syndesmotic ligaments, respectively.122
Fibular reduction usually neutralizes the tendency for valgus
angulation and/or lateral translation of the talus and associated
tibial pilon fracture fragments.
commonly fail in compression, and are frequently comminuted with
transverse and oblique fracture plane orientations. Because of this,
stiff precontoured periarticular distal fibular plates are
advantageous, in that they provide satisfactory stability and
facilitate indirect reduction techniques in comminuted fractures.
Although one third tubular plates are a common choice, stiffer
constructs such as stacked one third tubular plates, precontoured
distal fibular periarticular plates, and 2.7- or 3.5-mm dynamic
compression plates may be required. Those fibula fractures that occur
predominantly from rotational or tension mechanisms can be stabilized
with one third tubular plates.
techniques, or a combination thereof, and stabilizing implants are
typically applied to the posterolateral aspect of the fibula.127,185
It is imperative to avoid placing supportive bumps solely beneath the
posterior aspect of the hindfoot or ankle, as this will invariably
result in the undesired extension deformity of the fibula and tibia,
and ultimately result in the talus tending to translate anterior to the
anatomic axis of the tibia. If improved access to the fibula is
required, the entire leg should be elevated and supported on several
bumps to avoid creating this common angulatory deformity. Although
fibular reduction and fixation is typically performed before tibial
reduction and external fixation, there are occasions in which reversal
of this sequence may be advantageous. If limb shortening or instability
is significant, obtaining fibular reduction will be problematic. In
these situations, external fixation of the tibial component is
performed initially to obtain provisional restoration of length,
alignment, and rotation. Fibular reduction and fixation is then
performed and substantially simplified. Similarly, in the setting of a
comminuted fibula fracture in which a comparatively minimally
comminuted tibial fracture component exists, closed manipulative
reduction and external fixation of the tibia initially may more
accurately restore length, alignment, and rotation of the limb and
facilitate the subsequent fibular reduction.
external fixation of the tibial plafond is usually performed after
fibular stabilization (Fig. 56-16). External
fixation effectively stabilizes the tibial component of the injury,
maintains neutral talar tilt, and resists the tendency of the talus to
displace anteriorly out of the tibial plafond. Effective stabilization
of the reduced tibia and fibula provides a vital component to soft
tissue recovery. Closed manipulation and spanning external fixation
achieves these goals indirectly using ligamentotaxis. One of the most
powerful indirect reduction techniques for obtaining an accurate
restoration of tibial length and alignment, however, is an accurate and
stable fibular reduction. In the setting of an intact fibula or a
surgically stabilized fibula, a medially based frame is typically
employed. A 5-mm Schanz pin is placed from anteromedial to
posterolateral through the proximal tibial diaphysis. A second 5-mm pin
is placed from medial to lateral into the posterior aspect of the
calcaneal tuberosity and should avoid the numerous calcaneal sensory
branches from the tibial nerve.39
The knee is then flexed and supported with a radiolucent triangular
support commonly used for tibial nailing. This position facilitates
placement and fluoroscopic imaging of the subsequent midfoot Schanz
pin. A 4-mm Schanz pin is then placed from medial to lateral across the
three cuneiforms of the ipsilateral midfoot. To minimize the risk of
septic complications after definitive surgery, these pins are inserted well out of the anticipated location of plates, screws, and incisions.
Talar neck pins are specifically avoided, as these frequently
compromise anteromedial exposures of the distal tibia. Manipulation of
the calcaneal Shanz pin typically performs the vast majority of the
reduction. The usual reduction maneuvers applied to the hindfoot via
the calcaneal Schanz pin are traction (restoring tibial length), varus
or valgus correction (to achieve a horizontal talar dome), and
posterior translation (correcting the commonly seen anterior
displacement). Once tibial length, alignment, and rotation are
restored,
a
radiolucent bar is applied that connects the tibial pin to the
calcaneal pin. Placement of this initial bar stabilizes the vast
majority of the reduction. At this point, the talus should be centered
beneath the tibia on both the AP and lateral fluoroscopic images, and
the articular surface of the talus should be perpendicular to the
longitudinal axis of the tibial shaft. Accurate restoration of tibial
length is estimated by reestablishing the normal relationship of the
lateral process of the talus with the distal tip of the fibula.181
It is imperative that at the very least, the tibia is distracted to its
normal length, with slight overdistraction being preferred. Performing
delayed definitive open reduction becomes significantly more difficult
if the limb has been resting in a shortened position. Because the
radiolucent bar is located posterior to the anatomic axis of the tibia,
the talus is stabilized posteriorly beneath the tibial plafond and out
of the typical anterior displacement. A second radiolucent bar secures
the cuneiform pin to the tibial pin, maintaining neutral dorsiflexion
and plantarflexion of the tibiotalar joint. A third bar is used to
connect the calcaneal pin to the cuneiform pin neutralizing forefoot
adduction and increasing the rigidity of the external fixation
construct. A second 5-mm anteromedial to posterolateral Schanz pin is
then placed into the tibial diaphysis and connected to both of the
longitudinally oriented bars, completing the construct. Small amounts
of angulation and translation can be corrected before securing this
second tibial pin to the longitudinal bars.
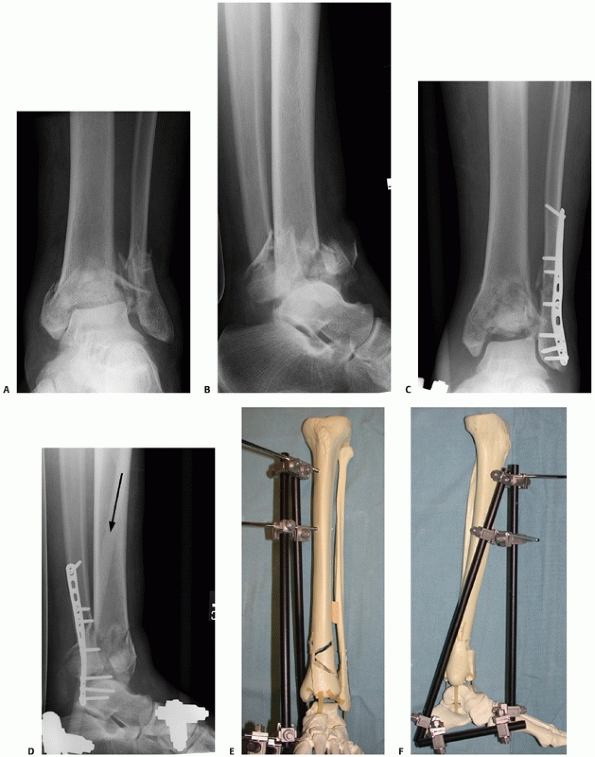 |
|
FIGURE 56-16 Anteroposterior (A) and lateral (B)
radiographs of a 52-year-old man involved in a motor vehicle collision. Provisional treatment consisted of open reduction and internal fixation of the comminuted fibula fracture and application of a medial transarticular spanning external fixator. The anteroposterior (C) and lateral (D) radiographs demonstrate satisfactory restoration of length with centering of the talus beneath the mid-diaphyseal line of the tibia on both views. Note the orientation of the tibio-calcaneal bar is marked with the black arrow. Sawbones models demonstrating the external fixation construct from the anterior (E) and lateral (F) vantage points. |
acute ORIF, a biplanar external fixator is placed. In addition to the
unstabilized fibula, the author’s main indications for the use of a
biplanar external fixation construct are: (i) tibial pilon fractures
with a delayed presentation (greater than 1 week postinjury), (ii)
tibial pilon fractures that demonstrate substantial valgus angulation
despite an intact or operatively reduced and stabilized fibula, or
(iii) marked tibial shortening with an intact fibula. In these
situations, the biplanar calcaneal Schanz pin markedly facilitates
restoration of tibial length and accurate coronal plane alignment of
the talus (Fig. 56-17). The essential features
that distinguish this external fixator construct from the medially
based frame described previously are: (i) the use of a transcalcaneal
Schanz pin and, (ii) the placement of tibial diaphyseal pins in a more
anterior to posterior direction rather than anteromedial to
posterolateral. The calcaneal Schanz pin can be manipulated from both
the lateral and medial aspects, resulting in excellent control of the
hindfoot, and via ligamentotaxis the talus and distal tibia,
substantially improving the ability to control the coronal alignment of
the distal tibia. Two radiolucent bars are used to secure the tibial
pin to the calcaneal pin: One bar connects to the medial portion of the
calcaneal pin, and one to the lateral portion. The remainder of the
construct is similar to that described for the medially based frame. At
the conclusion of the procedure, the fibular incision is closed using a
modified Allgower-Donati suture148
with the knots tied posteriorly, and the limb is placed into a
well-padded splint. A CT scan of the tibial plafond is then obtained to
aid in planning definitive fixation. Definitive reduction and fixation
is typically performed 7 to 21 days later and only after soft tissue
recovery has occurred (Table 56-2).135,156
routine postoperative antibiotic prophylaxis for 24 hours, parenteral
and oral analgesia, and the limb is splinted with a removable posterior
prefabricated support. Patients are instructed on the importance of
limb elevation, pin site care, and active motion of the toes is
encouraged. If there are no other significant injuries, the patient
receives deep venous thrombosis prophylaxis until they are mobilized
and discharged home. Before discharge, a thin cut axial CT scan is
obtained with sagittal and coronal reformations. The patient is
returned to the outpatient clinic for an assessment of soft tissue
swelling and to review the definitive operative plan.
fracture is challenging. Restoration of the articular surface along
with stable internal fixation allows early motion and has been felt to
be the most important predictor of satisfactory outcome,34,60,89,129,146 although this is controversial.101,184
Open management, however, must be carried out with meticulous attention
to preoperative planning, soft tissue handling, and the appropriate
timing of intervention. If soft tissue complications can be avoided,
anatomic articular reduction with stable fixation maximizes the chance
of obtaining a satisfactory outcome.165
from: (i) a thorough review of the postspanned CT scan to assess the
degree and displacement of the articular surface, (ii) the initial
injury radiographs to determine the optimum location for implants to
stabilize the metadiaphysis, and (iii) an assessment of the soft tissue
envelope to determine areas that are optimal or suboptimal for surgical
incisions. Because the ligamentous structures of the ankle remain
largely intact after a tibial pilon fracture, AO/OTA C-type injury
patterns commonly demonstrate three main fracture segments: the
anterolateral (Chaput) fragment, the posterior (Volkmann) fragment, and
the medial malleolar fragment.169
Each of these fragments, in turn, remains attached to the anterior
tibiofibular ligament, the posterior tibiofibular ligament, and the
deltoid ligament, respectively. Comminution and impaction are
frequently identified along the fracture lines separating the major
articular components, and are clearly seen with the CT scan. The
preoperative plan must include an assessment of the major fracture
components and how their manipulation will allow access to the areas of
comminution while respecting their soft tissue and ligamentous
attachments. A rational choice for stabilizing implants will allow the
reduced articular fragments to be secured, and to additionally
neutralize the major displacing forces that occur in the metadiaphyseal
region. All of this must be done within the limitations of the soft
tissue injury and within the limits that the available surgical
approaches offer.
extremely useful in the definitive management of these fractures.
Anterolateral and medial plates are now commonly available that provide
the ability to place multiple screws
into
the epiphyseal portion of the distal tibia, and allow the plate to
facilitate indirect reduction of the metaphyseal component. The
stiffness of these plates is particularly useful for unstable AO/OTA
C-type tibial plafond injuries. More malleable implants, such as distal
radius T-plates, quarter tubular, third tubular, and minifragment
plates, are occasionally useful, particularly in partial articular
injuries where neutralization of the metadiaphysis is unnecessary.
Additional equipment often includes a universal distractor, Schanz
pins, a large external fixation set, allograft or bone graft
substitute, headlamp illumination, Kirschner wires (K-wires),
minifragment screws, osteotomes, dental picks, and a variety of Freer
elevators and bone clamps.
 |
|
FIGURE 56-17 Injury anteroposterior (A) and lateral (B)
radiographs of a 42-year-old man who fell from a ladder sustaining a closed tibial plafond fracture with an intact fibula. Note the marked tibial shortening. C. Intraoperative lateral fluoroscopic view demonstrating transcalcaneal Schanz pin placement (white arrow). Final anteroposterior (D) and lateral (E) radiographs after closed manipulative reduction and application of a biplanar spanning external fixator. Satisfactory length and centering of the tibia is evident. Schematic representation of a shortened tibial plafond fracture with fibula restored to it’s anatomic length (F). (continues) |
managed with anterior-based exposures and the patient is typically
positioned supine, similar to that used for the initial stage.
Because
the surgical procedure may take several hours, a Foley catheter is
inserted, and care is taken to pad all bony prominences. A thigh
tourniquet is commonly used to facilitate visualization of the
articular surface. After the induction of anesthesia and positioning of
the patient, the limb is given a provisional scrub to remove loose skin
and debris. Provided the pin sites have been well maintained, the
entirety of the preexisting external fixator is prepped and drapped
into the surgical field. The surgeon is typically located at the distal
end of the radiolucent table and the C-arm is located contralateral to
the injured extremity.
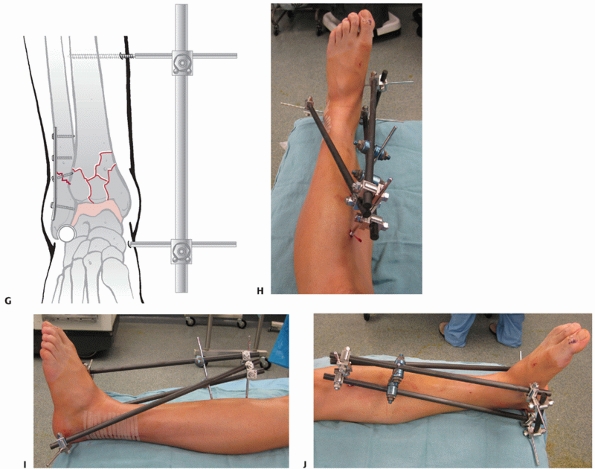 |
|
FIGURE 56-17 (continued) Restoring the “dime sign” indicates satisfactory reduction of relative fibular and tibial lengths (G). Clinical example of a biplanar provisional external fixator from the anterosuperior (H), lateral (I), and medial (J)
perspectives. Note that the Schanz pins have been placed out of the zone of anticipated surgical incisions or implants. The posterolateral fibular incision is identified from the lateral vantage (I). |
|
TABLE 56-2 Pearls and Pitfalls for Stage 1 Treatment of Pilon Fractures: Fibular ORIF and Spanning Tibiotalar External Fixation
|
|
|---|---|
|
approach is indicated, the patient is placed in the lateral position,
which facilitates a posterolateral exposure of the distal tibia.
Externally rotating the limb and tilting the operating table slightly
can subsequently allow supplemental anterior or medial exposures.
fracture varies according to the specific fracture pattern, state of
the local soft tissue envelope, as well as the experience and technical
abilities of the surgeon. In the author’s opinion, reduction of the
articular portion of a tibial plafond injury remains the most critical
aspect of surgical care and, therefore, typically dominates the
surgical tactic. The reduction sequence, choice of exposure(s), and
application of stabilizing implants are therefore all geared toward
achieving an accurate articular reduction. Initially, the
posterolateral fragment is critically assessed as the starting point
for the majority of C-type fracture patterns. After the exposure is
performed, articular visualization is facilitated with the use of an
external fixator or universal distractor. If an anteromedial exposure
is performed, a medial to lateral talar neck pin is inserted; if an
anterolateral exposure is performed, a lateral to medial talar neck pin
is inserted. In either situation, the talar neck pin is typically
connected to a preexisting tibial pin that was part of the initial
spanning external fixator. By removing the cuneiform to tibial bar that
was originally placed with the application of the spanning external
fixator, the talus is allowed to plantar flex in the mortise improving
the visualization. By leaving the tibial to calcaneal portion of the
external fixator in place, the talus maintains its posterior position
relative to the anatomic axis of the tibia. Reduction of the
posterolateral tibial articular fragment is frequently accomplished
with anatomic reduction and stabilization of the fibula fracture. If
satisfactorily reduced, the reduction sequence commonly involves
reducing the posterior aspect of the medial malleolar fragment to the
posterolateral fragment. Impacted central comminution is then reduced
and secured to the posterior plafond. The medial malleolar fragment is
secured using the medial shoulder chondral interdigitations, followed
by reduction of the anterolateral (Chaput) fragment. At each step of
the reduction process, provisional fixation is accomplished with the
use of strategically applied clamps and small (0.045-inch) Kirschner
wires (K-wires).
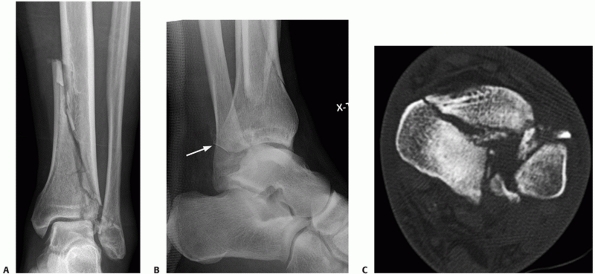 |
|
FIGURE 56-18 A,B.
Injury radiographs of a 49-year-old man after falling from a 10-foot height. Note the displaced posterolateral plafond fragment (white arrow). After application of a spanning external fixator, axial (C), (continues) |
“starting point” for the tibial reduction, it is imperative to ensure
that it is appropriately reduced to the fibula at the level of the
syndesmosis (Fig. 56-18). Occasionally, the
posterolateral plafond demonstrates a dorsiflexion impaction injury
that can be appreciated by critically assessing the sagittal CT
reformations. In this situation, subsequent reductions to the posterior
plafond result in an extension deformity of the articular surface and
altered contact pressures affecting the anterior plafond. It is
imperative that the surgeon identifies this posterolateral impaction
injury and rotates the affected plafond segment into a reduced position
before proceeding with the remaining reduction maneuvers (Fig. 56-19).
 |
|
FIGURE 56-18 (continued) and sagittal (D)
CT scans demonstrate significant articular injury, with dislocation of the posterolateral plafond relative to the talus and the fibula. With the patient in the lateral position, the operative tactic included a posterolateral approach with direct reduction and stabilization of this fragment initially (E). The leg was then externally rotated and a small anterolateral exposure was performed to reduce and secure the large coronal plane fracture separating the plafond into two halves (F). The metadiaphyseal fracture was then stabilized with a percutaneous medial plate (G,H). |
as well as that of the metadiaphysis is to identify a fracture fragment
that contains some amount of articular surface distally while
demonstrating a minimally comminuted metaphyseal or metadiaphyseal
proximal extension. In this situation, anatomic reduction of the
proximal metadiaphyseal component essentially converts the C-type
tibial pilon fracture into a partial articular (B-type) injury, greatly
facilitating the reduction of the remaining articular surface, and
providing a basis for reduction of axial alignment. Large medial
malleolar fragments, posterior osteochondral fragments, or large
posterolateral fragments are typically those that are sought for this
reduction strategy (Fig. 56-20).
success of the procedure. In addition to numerous small diameter
Kirschner wires and clamps, minifragment plates and screws are also
very useful in accurately and more rigidly maintaining a provisional
reduction. These devices should be placed out of the zone of definitive
implants and therefore a preexisting knowledge of the definitive
implants, reduction sequence, and choices of surgical approaches is
required.
stabilization of tibial plafond fractures were placed on the
anteromedial surface of the tibia. Their bulkiness, nonanatomic design,
and limited areas for strategic screw placement limited their
usefulness. Contemporary implants demonstrate a
more
anatomic-based lower profile design, facilitating percutaneous and
indirect plate reduction techniques. The goals of definitive internal
fixation should include absolute stability and interfragmentary
compression of reduced articular segments, stable fixation of the
articular segment to the tibial diaphysis, and restoration of coronal,
transverse, and sagittal plane alignments. The location, rigidity, and
number of these implants are based on each individual fracture. Factors
to consider include the degree of comminution, the ability to achieve
cortical contact and intrinsic fracture stability, the bone quality,
the direction of the initial failure of the bone (varus, valgus,
flexion, extension), the status of the soft tissue envelope, and any
associated bone loss, among others.122
It is important to recognize that the majority of implant placements
onto the proximal metadiaphyseal segment of the tibia can be performed
indirectly, using a submuscular plate insertion along the anterolateral
aspect of the tibia proximal to the anterolateral approach, and by
using a percutaneous medial plate placement. Ideally the thickness of
the plate should balance the need for an implant that has adequate
stiffness to counter the anticipated loads, while minimizing plate
prominence and soft tissue injury, particularly along the anteromedial
surface of the tibia. When neutralizing C-type injuries, at least one
stiff (e.g., 3.5-mm compression plate) implant is usually required to
maintain metadiaphyseal alignment (Figs. 18-20). B-type injuries do not
require metadiaphyseal neutralization, and can commonly be managed with
lower profile implants that simply allow neutralization of the partial
articular injury.
 |
|
FIGURE 56-19 Injury anteroposterior (A) and lateral (B)
radiographs of a 28-year-old man involved in a motocross accident. Note that his fibula is intact. After spanning external fixation, the lateral fluoroscopic view (C) demonstrates a dorsiflexion deformity of the articular surface of the posterior plafond. The axial CT scan demonstrates a large posterior plafond fragment with central and posteromedial comminution (D). The sagittal reformation corroborates the dorsiflexion deformity (E). Using a modified anteromedial exposure, the reduction sequence consisted of first clamping the metadiaphyseal fracture (F). (continues) |
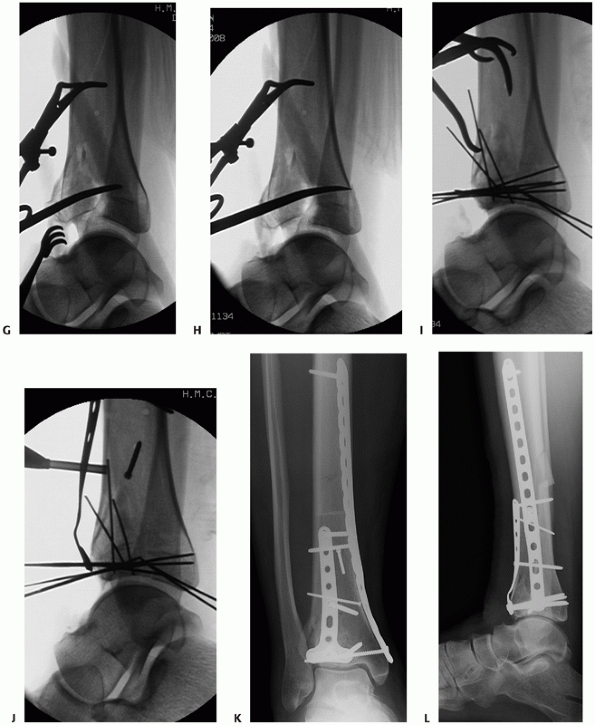 |
|
FIGURE 56-19 (continued) An osteotome is introduced proximal into the posterior fragment proximal to physeal scar (G). Downward pressure applied to the osteotome, correcting the impaction injury (H).
The reduced posterior fragment is secured to the fibula with percutaneous Kirschner wires, and the remainder of the plafond is reduced and provisionally secured (I). An undercontoured low profile T-plate is secured to the anterior aspect of the distal tibia, effectively stabilizing the articular reduction (J). A stiff medial plate is applied to neutralize the varus tendency of this fracture pattern. Final anteroposterior (K) and lateral (L) images. |
intra-articular fractures of the distal tibia, and current
evidence-based recommendations are lacking. Relative indications
include poor bone quality, anticipated prolonged time to union
(particularly in those with metaphyseal bone loss),
or
in those situations in which the ideal choice of implants cannot be
performed secondary to local soft tissue conditions. C-type injuries
with substantial metadiaphyseal comminution are often best stabilized
with anterolateral and medial distal tibial implants. In situations
with poor medial skin quality, isolated anterolateral locking implant
can be used to decrease the need for a medial internal implant.
Similarly, fractures best suited for buttress plate fixation that
cannot be treated in this fashion secondary to poor local skin
conditions can be stabilized with a locking plate placed 180 degrees
opposite from the fragment that requires buttressing. In this
situation, rather than being buttressed by a plate placed directly on
top of the fragment, several locking screws terminating into the
fragment provide its stability (Fig. 56-21).
The majority of tibial pilon fractures at the author’s institution,
however, continue to be managed with nonlocking screwplate devices (Table 56-3).
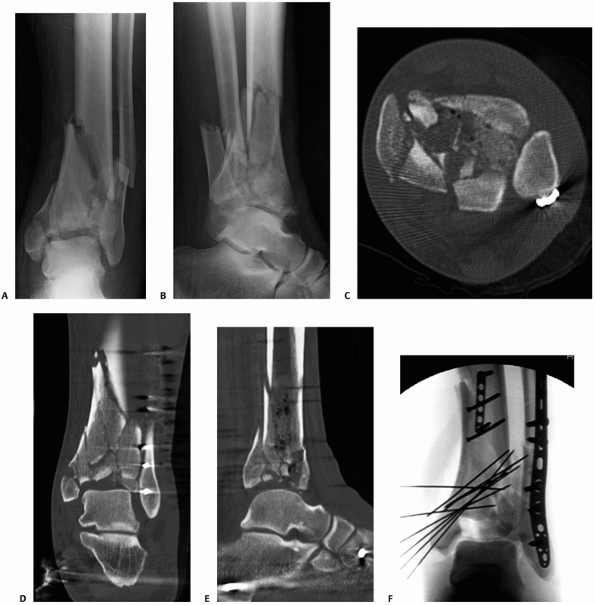 |
|
FIGURE 56-20 Injury radiographs (A,B)
of a 46-year-old man involved in a motor vehicle collision. After operative fixation of his fibula fracture and spanning external fixation of the tibial component, his axial (C), coronal (D), and sagittal (E) CT scans demonstrate substantial articular comminution. The medial malleolus was reduced initially and secured with K-wires (F). (continues) |
are placed into a well-padded plaster splint with the foot in neutral
position. In addition to patient controlled anesthesia
devices,
peripheral nerve blockades are commonly employed for pain control
during the first 24 to 48 hours, and are inserted at the conclusion of
the procedure while the patient is still under a general anesthetic.
Patients are discharged from the hospital on a long- and a short-acting
narcotic medication. Although controversial, the author prefers to
withhold nonsteroidal anti-inflammatory medications until approximately
3 months, to minimize the theoretical risk of delayed or nonunion.38,51,71,75,139
The wound is typically examined in the outpatient clinic area
approximately 4 to 5 days later. Splinting with the foot in neutral is
continued until the sutures are removed at the 2- to 3-week mark. A
supervised physical therapy program consisting of active,
active-assisted, and passive range of motion of the ankle, subtalar and
metatarsophalangeal joints are subsequently initiated. To avoid equinus
contracture, a removable nighttime and resting splint is recommended.
Partial progressive weight-bearing in a removable boot is usually
initiated approximately 12 weeks after definitive surgery. The physical
therapy focus at this point consists of maximization of motion,
strengthening, gait training, and the weaning of ambulatory devices
such as crutches, canes, and external supports. Postoperatively, edema
may be substantial and persist for several months after injury. In
addition to patient education regarding this normal phenomenon, an
elastic stocking is provided to help decrease dependency-related
swelling.
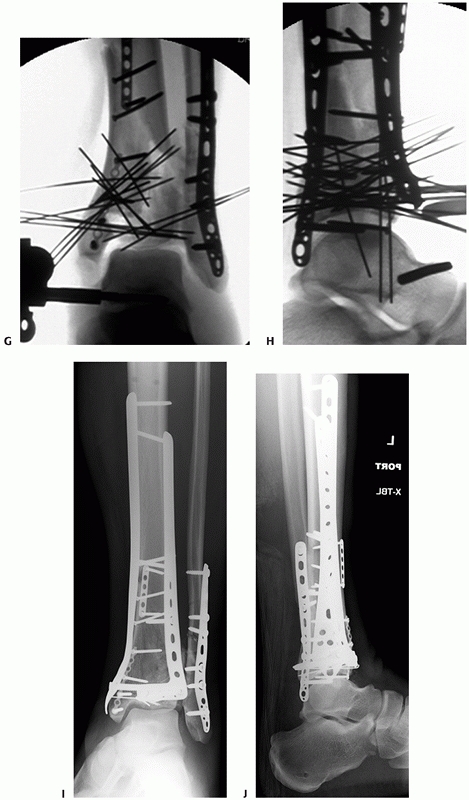 |
|
FIGURE 56-20 (continued)
A small maxillofacial implant was then used to securely stabilize the medial malleolar reduction to the distal tibia, allowing distraction to further visualize the articular surface (G). Once the provisional reduction of the articular and metaphyseal components was secured, definitive plate stabilization was applied (H). Final immediate postoperative radiographs demonstrate satisfactory articular and metadiaphyseal reductions (I,J). |
 |
|
FIGURE 56-21 Anteroposterior (A) and lateral (B)
injury radiographs of a 77-year-old woman involved in a motor vehicle collision. She was treated acutely with biplanar spanning external fixation (C,D). Severe full thickness hemorrhagic blisters over the lateral malleolus precluded operative treatment of her fibular fracture. Axial (E) and sagittal (F) CT imaging confirms a partial articular B-type posterior tibial pilon variant fracture with central articular impaction. (continues) |
 |
|
FIGURE 56-21 (continued)
A modified anteromedial exposure was performed 3 weeks after the injury. The sagittal fracture adjacent to the medial malleolus was used to facilitate reduction of the posterior plafond (G). The articular surface was secured with K-wires and, because of her anticipated poor bone quality, a distal radius locking plate and mini-fragment T-plate were used to support the articular surface (H,I). Despite the 3-week delay, the skin of the lateral malleolus still precluded safe open reduction methods for the fibula fracture, and the lateral malleolus was simply secured with percutaneous medullary K-wires after the plafond was reduced and plated (J). One year later, the patient reports a very satisfactory outcome with adequate maintenance of reduction (K,L). Although this particular injury pattern may have better been stabilized using a posteriorly applied buttress plate, the poor condition of the posterolateral soft tissue envelope was a relative contraindication for the exposure required for posterior buttress plate application. Because of the anticipated poor bone quality, and the inability to use a plate to stabilize the posterior plafond, an anterior fixed-angle screw/plate device was used to achieve stability of the posterior plafond fracture fragments. |
|
TABLE 56-3 Pearls and Pitfalls for Stage 2 Treatment of Pilon Fractures: Definitive Tibial Open Reduction and Internal Fixation
|
|
|---|---|
|
tibial plafond fractures can be grouped as septic and nonseptic. As
evidenced by the soft tissue envelope having been a primary driver in
the evolution of the operative care of these injuries, the most
significant complications after operative management of tibial plafond
fractures involves those of the soft tissue envelope.
slough, is the most common wound complication after open reduction and
internal stabilization of tibial plafond fractures. Using staged
protocols and formal open exposures, contemporary partial-thickness
skin necrosis rates have ranged from 5% to 17%,86,156
although this figure is likely underreported in studies that are not
particularly evaluating this as a complication. Partial-thickness skin
necrosis typically develops a dry eschar that will slowly elevate and
slough revealing an underlying epithelialized layer. Treatment is
typically supportive, with local wound care and patience resulting in
resolution. Occasionally wet-todry dressing changes are required if the
eschar is débrided or removed prematurely. Often these wounds are
accompanied by mild surrounding cellulitis with an erythematous margin,151
which represents an appropriate inflammatory response, not an
infection. At this point, the limb is placed at rest and motion across
the ankle joint is stopped to allow maturation of the eschar and
underlying skin. Close clinical follow-up is warranted to ensure
adequate healing. Antibiotics are initiated, however, if the
surrounding erythema that is present as an inflammatory response to the
necrotic skin devolves into cellulitis secondary to superficial
bacterial infection. Wound cultures are not indicated because the
surface of the leg is contaminated by normal skin flora and is not
representative of a causative organism. Failure to respond to this
treatment requires consideration for inpatient therapy and intravenous
antibiotics guided by an infectious disease consultant.
dehiscence should be regarded as an urgent situation that requires
hospital admission and operative treatment. The goal of operative
treatment in this situation is to convert the contaminated surgical
field into a sterile wound that can undergo soft tissue closure,
and
to obtain deep tissue cultures to guide antibiotic treatment. In all of
these significant wound complications, the author strongly recommends
obtaining radiographs to ensure that there has not also been a subtle
or obvious loss of fixation or implant failure. Irrigation and
débridement should be performed as soon as possible to remove all
necrotic tissue and cleanse the wound. Stable implants are left in
place, but loose implants should be removed, as they are of no benefit
to facilitating fracture union and simply represent a contaminated
foreign body. Often a small dehiscence can undergo primary suture
repair, but most often skin retraction prevents closure. In these
cases, the remaining wound is covered with a vacuum-assisted closure
device (VAC) to seal the open wound from the hospital environment,
eliminate the formation of wound seromas or hematomas, and facilitate
granulation and wound contraction.82,158
Culture-specific antibiotics are administered and, once the wound is
free of necrotic tissue and clean, a plan for definitive closure of the
wound is required. In small wounds without exposed metal, bone, or
tendon, a period of VAC changes then closure by secondary intention is
performed. If the area is larger, skin grafting can be performed to
expedite closure. Larger wounds, however, or those with exposed
tibialis anterior tendon or metal, require formal soft tissue coverage,
and a surgeon trained in microvascular techniques should be consulted.
Occasionally local fasciocutaneous flaps are sufficient, but because of
the limited tissue availability in the distal tibial region free tissue
transfer may be required.173 Despite
a clean-looking wound at the time of coverage or closure, a delayed
septic process may still occur, particularly if the implants that have
been left in situ have become colonized with bacteria.
wound infections, as evidenced by purulent open wound drainage,
elevated inflammatory markers, and clinical signs of deep sepsis,
treatment decisions become extremely complex. Similar to the goals
described in the preceding, operative débridement is urgently performed
to decrease the bacterial load, obtain deep tissue cultures to guide
antibiotic treatment, and remove devitalized tissue. In the setting of
an acute fracture and stable fixation, the goal of treatment is to
suppress the infectious process until there is fracture union, at which
point the implants can be removed.140
In these cases, draining wounds are packed and definitive soft tissue
coverage is typically delayed until the fracture is healed and implants
are removed. In patients with an acute infection and grossly unstable
implants and fracture, the treatment strategy is similar to that of an
infected nonunion, with staged reconstruction of the distal tibia.
fracture is a complex management problem. In situations in which there
has been an acute wound infection, the septic process is suppressed and
implant removal occurs when there is radiographic and clinical union.
This scenario is simplified because the fracture has united. The
surgical goals after union has occurred are the removal of all
potentially contaminated material, including stabilizing implants and
devitalized soft tissue and bone, deep tissue cultures, and secure
closure of the soft tissue envelope if needed. Adequate bone
débridement is facilitated with a high-speed burr, with decortication
guided by the occurrence of bleeding bone. Laser Doppler flowmetry has
been advocated as an adjunctive technique for the determination of
viable and nonviable bone in the treatment of osteomyelitis.59,160,161,162
Often patients may need soft tissue coverage to eliminate a densely
scarred area, or a previous sinus tract that is not amenable to primary
closure. A course of antibiotic treatment is then administered, guided
by an infectious disease specialist and the deep culture results.163
Treatment principles include radical débridement of infected and
nonviable tissue, bony reconstruction, soft tissue reconstruction, and
medical therapy.168 In these
situations, therefore, formal débridement, with implant removal,
medullary débridement, and cortical débridement of nonviable bone must
be performed. If necessary, repeated débridements are performed to
ensure that all necrotic and infected tissue is removed. Bone defects
are filled with nonbiodegradable drug delivery systems, such as
antibiotic-impregnated beads or cylinders. Soft tissue defects are
covered with local, or more commonly distant, tissue transfer, and the
skeleton is stabilized with external fixation. Culture-specific
antibiotics are administered according to an infectious disease
specialist, with the duration of treatment typically between 6 and 12
weeks, depending on the virulence of the organism, health of the host,
and available antibiotic regimens. Once the soft tissue healing has
stabilized, with complete epithelialization of muscle flaps
reconstruction is directed at achieving union with bone grafting,
consideration of definitive treatment with continued external fixation
or conversion to internal fixation. An important factor to consider is
whether the articular surface of the distal tibia is involved or not,
and whether ankle joint function is expected to be satisfactory. If the
articular surface is involved and the ultimate function of the
tibiotalar joint is anticipated to be poor, then reconstruction efforts
are directed toward achieving well-aligned tibiotalar arthrodesis. In
recalcitrant situations, those patients that are not candidates for
soft tissue transfer, or those patients who choose not to proceed with
repeated surgical interventions in the hopes of obtaining a functional
lower extremity, a well-timed below-knee amputation remains an
important therapeutic option.
fracture of the tibial plafond occur within the metaphysis or the
metadiaphyseal junction. Rates of nonunion range from 0% to 16%.11,77,96,135,153,156
Intra-articular nonunions are extremely rare. The preoperative workup
should include an assessment of the soft tissue envelope, particularly
the location of previous surgical incisions or traumatic wounds, ankle
and subtalar range of motion, clinical malalignment, and an evaluation
of potential causes for the nonunion, such as medications, infection,
poor osseous vascularity, fracture instability, or other factors that
may have been technique related. Distal tibial metaphyseal nonunion can
be managed with medullary nails, plates, or external fixation,
depending in part on the location of the nonunion relative to the
articular surface, local soft tissue conditions, previous treatment
methods, coexisting malalignment, and the biologic potential of the
region. In most cases, especially with broken plates, the original
incision should be used to retrieve the failed
implant and access and treat the nonunion according to current methods.151
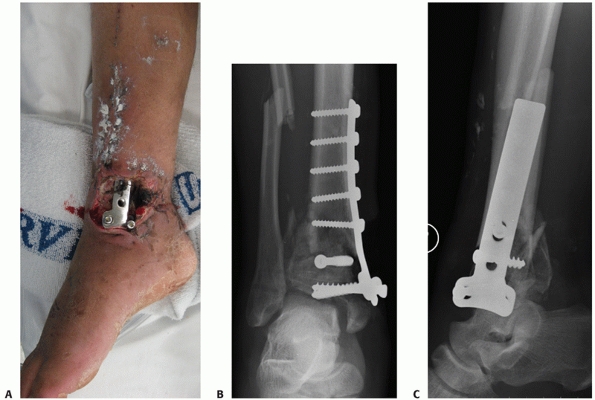 |
|
FIGURE 56-22 Clinical photo (A) and anteroposterior (B) and lateral (C)
radiographs of the ankle of a 38-year-old man 6 weeks after open treatment of a tibial plafond fracture at an outside facility. Gross purulence, loss of fixation, malalignment, and deep sepsis are evident. |
frontal, sagittal, and transverse plane alignment is required. A
typical scenario is the varus, extended, malaligned nonunion.
Restoration of appropriate alignment often requires the use a medially
based universal distractor or external fixator, followed by plate or
nail stabilization. Because correction of this deformity will result in
the creation of a bone defect, the surgeon must be prepared for the use
of bone graft. Additionally, the surgeon must carefully evaluate the
status of the soft tissue envelope before repair, as acute correction
of the varus and extension may substantially compromise the medial soft
tissue envelope, particularly if there has been significant scarring
secondary to the initial trauma and/or previous surgical interventions.
In these situations, preoperative consultation with a microvascular
surgeon will facilitate their understanding of the soft tissue coverage
possibilities that may arise, and importantly, the patient will
understand these possibilities preoperatively. Last, the surgeon and
patient should appreciate that once limb alignment is restored, the
location of the arc of motion of the ankle may be substantially altered
compared with that preoperatively. In particular, those patients who
present with an extension deformity of the distal tibia may require a
tendo-Achilles lengthening or gastrocnemius recession procedure to
eliminate the preexisting equinus contracture that will be made evident
with accurate sagittal plane realignment of the distal tibia. Severely
malaligned nonunions may be best managed with circular ring fixation
that allows gradual restoration of alignment and concomitantly creating
a gradual accommodation of medial soft tissue envelope.64,142,143 By incorporating the foot into the frame, the potential equinus contracture can also be managed with gradual realignment.
arthritis are common after fractures of the tibial plafond, but because
of the lack of significant long-term follow-up and the varied criteria
for diagnosis, exact incidences remain unknown. Marsh noted that the
majority of ankles in his study demonstrated radiographic arthrosis
changes such as joint space narrowing, but only weak correlations were
noted with clinical outcome.105
Although the foundation of open reduction and internal fixation is, in
part, to obtain an anatomic articular reduction, posttraumatic
arthrosis may still develop despite an anatomic reduction secondary to
chondral injury of the tibia, the talus, or both.* Many
patients can be successfully treated with anti-inflammatory
medications, activity modification, and periodic bracing. Provided that
the distal tibia is well aligned and the fracture is healed, treatment
for severe posttraumatic end-stage ankle arthritis is best treated with
an in situ arthrodesis (Fig. 56-23).151 Marsh reported an arthrodesis rate of 13% in 40 ankles after a minimum follow-up of 5 years.105 Chen noted a 4.7% arthrodesis rate in plated tibial plafond fractures followed an average of 10 years.41
Historically, reported arthrodesis rates with operative management of
tibial plafond fractures have ranged from 5% to 26%, with most of this
data being obtained
in patients followed for less than 5 years.17,34,129,144,146,153
In patients with significant erosions or juxta-articular deformity,
custom-shaped tricortical allograft or autograft shims should be used
to place the hindfoot in the proper position.118
Numerous arthrodesis techniques have been reported with successful
results, including the use of blade plates, hindfoot fusion nails, and
circular external fixators.* Total ankle replacement is a
relatively new alternative to arthrodesis for posttraumatic ankle
arthrosis. Despite the intuitive reconstruction of joint mechanics,
total ankle replacement remains unproved in this patient population,
and may be associated with substantially higher rates of complications
and revision procedures.42,53,152
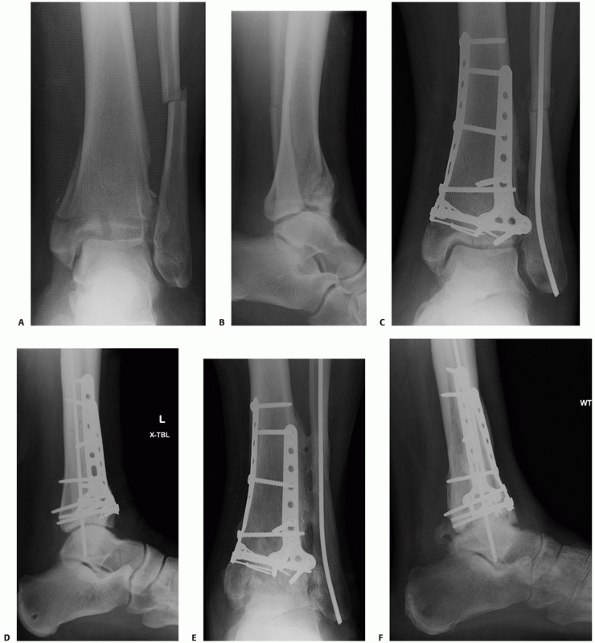 |
|
FIGURE 56-23 Injury anteroposterior (A) and lateral (B)
radiographs demonstrating a displaced tibial plafond fracture in a 53-year-old man who fell from a ladder. His fracture was treated in a staged fashion with definitive open reduction and internal fixation performed using a modified anteromedial exposure (C,D). His early postoperative course was complicated by a deep wound infection, ultimately resulting in significant ankle arthrosis (E,F). (continues) |
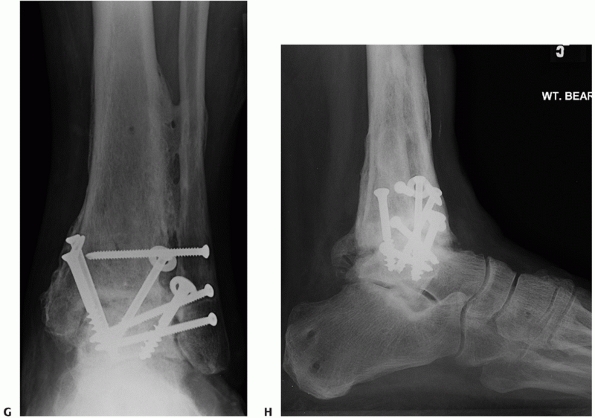 |
|
FIGURE 56-23 (continued) He was successfully treated with a single-stage tibiotalar arthrodesis (G,H).
|
plafond fractures with anatomic articular reconstruction, restoration
of distal tibial alignment, and avoidance of surgical complications,
the outcome is not always favorable. The irreversible injury that
occurs to the chondral surface and other supporting structures
continues to be delineated and likely represents important variables in
patient outcomes.29,30,31,111,112,113,167
Although the factors that most predictably affect patient outcome after
high-energy fractures of the tibial plafond have yet to be entirely
determined, validated outcome instruments for ascertaining disability
after musculoskeletal injury have demonstrated the significant impact
that fractures of the tibial plafond have on patient health.
management suggests that the surgical goals for treating tibial plafond
fractures are anatomic articular reduction and restoration of distal
tibial alignment. Unfortunately, at least with fractures of the tibial
plafond, proving that this has any substantial impact on the final
patient outcome has been exceedingly difficult.101 Many clinicians have considered that the severity of articular injury is the most critical determinant of outcome.48,60,100
On the other hand, others have contended that if an anatomic reduction
of the articular surface is achieved, then a good outcome can be
expected.135,144
Interestingly, DeCoster demonstrated that neither injury severity nor
quality of reduction consistently correlated with clinic ankle scores,
but that the quality of reduction did correlate with arthrosis.49
Discerning the effect that each of these preceding variables has on the
final outcome becomes even more problematic because of the inherently
close association between more severe injuries and the inability to
obtain an accurate articular reduction.184
The obvious inference is that poor results in patients with severe
injuries may be attributed to inadequate reduction when in fact the
patients with poor reductions usually have the most severe articular
injuries.184 Williams performed a
review of 32 tibial plafond fractures at a minimum of 2 years after
injury treated with ankle spanning external fixation and limited
internal fixation.184 Similar to the findings of DeCoster,49
the authors noted that the severity of injury and accuracy of articular
reduction as assessed on preoperative and postoperative radiographs
strongly correlated with the radiographic presence of arthrosis, but
that the presence of arthrosis had no correlation with the clinical
ankle score. These authors also found that neither the injury, the
quality of reduction, nor measurements of soft tissue injury correlated
with any of their patient-derived outcome scores. It should be noted,
however, that several reports have suggested that the accuracy and
reproducibility of plain radiographic measurements of articular
congruity may be suboptimal.27,43,92,106
Regardless, a preponderance of socioeconomic factors did correlate with
the clinical ankle score, with females, college graduates, and patients
with injuries not associated with workplace injury claims all having
better scores. The ability to return to work was also affected by type
of work and level of education, as those with higher levels of
education performed in less physically demanding jobs and were
therefore not as limited by their ankle injury.
patients with tibial plafond fracture managed with either open
reduction and internal fixation or external fixation with or without
limited internal fixation after a mean of 3.2 years.136
A majority of patients (74%) who were enrolled had sustained AO/OTA
C-type tibial plafond fractures. Although the cohort treated with open
reduction and internal fixation had significantly better outcomes that
the external fixation group with regard to pain, walking, and ankle
range of motion, ultimate outcomes for both groups were less than
optimal. As reflected by the SF-36 scales, patient scores were
significantly lower than age-matched controls, especially for role
disability owing to physical health problems and physical function. In
fact, SF-36 scores after pilon fracture were worse than after pelvic
fracture or with chronic illness such as AIDS, diabetes, or coronary
artery disease. Forty-three percent of previously working individuals
remained unemployed at the time of follow-up, and 68% of those patients
attributed their inability to work to the sequelae of their tibial
plafond fracture. As noted by others,2,10,63,184
patients with a lower income level or lower level of education were
significantly more likely to report and/or demonstrate poorer health
and function than were patients who had more financial resources and
education.
In their cohort of 64 patients treated with open reduction and internal
fixation of their tibial plafond fractures, the SF-36 demonstrated
significant negative differences when compared with age-matched general
population and patients with tibial plateau fractures in the physical
functioning and the role of physical functioning categories.
treatment with a monolateral hinged transarticular external fixator
coupled with screw fixation of the articular surface.105
Using validated outcome measures, the authors found that tibial plafond
fractures have a long-lasting negative effect on ankle function, work,
recreation, and health-related quality of life. Despite arthrosis being
evident in the majority of ankles, the effect on clinical outcome was
not clear, as the presence of arthrosis had only weak correlations with
clinical outcome as measured with the Iowa Ankle Score, the Ankle
Osteoarthritis Scale, and the SF-36. Despite this long-lasting negative
impact, few ankles in this series required late arthrodesis, or
subsequent ankle surgical procedures. The protracted time to
improvement (2.4 years postinjury) is similar to the results of Ruedi,144
who noted that most patients improved or had a stable outcome after
being evaluated at a longer follow-up interval. Chen evaluated 128
tibial plafond fractures treated with open reduction and internal
fixation at a mean of 10 years postinjury.42
The authors noted that posttraumatic arthrosis was a progressive
disease, with increasing incidence evident on plain radiographs, but
still demonstrated that rather few of these patients required later
arthrodesis. The authors similarly noted that patients with worse soft
tissue injury at presentation had poorer clinical outcomes.
challenging injuries, the outcome of tibial plafond fractures remains
problematic, with approximately one third of patients reporting
difficulty with ankle stiffness, swelling, or pain.136
Major physical and psychosocial health problems are evident long after
the initial injury. Although accurate surgical reconstruction with
minimization of iatrogenic complications should remain the goal in the
treatment of these fractures, certain factors outside of the surgeon’s
control appear to have substantial influence on patient outcomes after
these injuries.
the most challenging and controversial injuries that we treat. Much of
the controversy resides in treatment techniques and balancing the
benefits of surgical restoration of anatomy versus the potential risk
of further soft tissue injury and iatrogenic complication. The
development of staged open reduction and internal fixation has
recognized the important role of the soft tissue envelope, and the
problems that are faced with performing extensive surgical dissections
during the time of maximal soft tissue swelling. An appreciation of
surgical timing, however, continues to evolve and the role of immediate
fixation is an area for continued study. As more validated clinical
patient oriented outcome data have become available, the surgical
community is understanding that a number of factors that affect the
final outcome in these patients are out of our control; however, those
factors that are within our control still need considerable evaluation.
fixation remains an area that, although the foundation of fracture
care, continues to be controversial. In part, this is owing to the
inability to accurately assess the adequacy of reduction. Methods that
demonstrate high observer agreement in the accurate assessment of the
quality of reduction will greatly help in teasing out the relative
contributions that injury severity and surgical reduction have to
patient outcome. Based on the findings of Pollak136 and others,49,105,153,184
clinical research should be devoted to understanding improved methods
of pain control, minimization of stiffness, and understanding the
microscopic injury of the cartilage and other supportive ankle tissues.
It is likely that the frontier for the management of these injuries
will be less focused on the technical apparatus than on the
regenerative sciences and biological alternatives.
and dislocation compendium. Orthopaedic Trauma Association Committee
for Coding and Classification. J Orthop Trauma 1996;10 Suppl 1:v-ix,
1-154.
AK, Nagi ON. Hybrid external fixation in periarticular tibial
fractures. Good final outcome in 56 patients. Acta Orthop Belg
2006;72(4):434-440.
GK, Bourne RB, Finlay JB, et al. Indentation stiffness of the
cancellous bone in the distal human tibia. Clin Orthop Relat Res
1985(201):264-270.
K, Ozsoy MH, Yensel U. Treatment of displaced pylon fractures with
circular external fixators of Ilizarov. Foot Ankle Int
1998;19(4):208-216.
M, Ray A, Stern R. The extensile approach for the operative treatment
of high-energy pilon fractures: surgical technique and soft-tissue
healing. J Orthop Trauma 2007;21(3):198-206.
GC, Vayanos ED, Papaioannou N, et al. Results of surgical treatment of
tibial plafond fractures. Clin Orthop Relat Res 1997(341):99-105.
E, Sorlie PD, Johnson NJ. A comparison of the relationships of
education and income with mortality: the National Longitudinal
Mortality Study. Soc Sci Med 1999;49(10):1373-1384.
S, Smith WR, Morgan SJ, et al. A retrospective analysis of comminuted
intraarticular fractures of the tibial plafond: open reduction and
internal fixation versus external Ilizarov fixation. Injury
2008;39(2):196-202.
S, Lenehan B, Khan H, McElwain JP. Minimally invasive percutaneous
plate fixation of distal tibia fractures. Acta Orthop Belg
2007;73(5):635-640.
R, Schenk R, Koval K, et al. Hybrid external fixation in the treatment
of tibial plafond fractures. Clin Orthop Relat Res 1996(332):16-22.
DP, Nork SE, Bellabarba C, et al. Is the absence of an ipsilateral
fibular fracture predictive of increased radiographic tibial pilon
fracture severity? J Orthop Trauma 2006;20(1):6-10.
T, Crichlow R, Gobezie R, et al. Complications associated with the
posterolateral approach for pilon fractures. J Orthop Trauma
2006;20(2):104-107.
M, Bastian L, Krettek C, et al. Surgical options for the treatment of
severe tibial pilon fractures: a study of three techniques. J Orthop
Trauma 2001;15(3):153-160.
L, Stegemann P, McNamara K, et al. External fixation of severely
comminuted and open tibial pilon fractures. Clin Orthop Relat Res
1993(292):101-107.
O, Kloen P, Richmond J, et al. Minimally invasive treatment of pilon
fractures with a low profile plate: preliminary results in 17 cases.
Arch Orthop Trauma Surg 2006;8:573-582.
T, Larsson S, Lindsjo U. Percutaneous plating of distal tibial
fractures. Preliminary results in 21 patients. Injury
2004;35(6):608-614.
J Jr, Goldfarb C, Catalano L, et al. Assessment of articular fragment
displacement in acetabular fractures: a comparison of computerized
tomography and plain radiographs. J Orthop Trauma 2002;16(7):449-456;
discussion 446-447.
J Jr, Prickett W, Song E, et al. Extraosseous blood supply of the tibia
and the effects of different plating techniques: a human cadaveric
study. J Orthop Trauma 2002;16(10):691-695.
J Jr, Silva MJ, Zaegel MA, et al. Single high-energy impact load causes
posttraumatic OA in young rabbits via a decrease in cellular
metabolism. J Orthop Res 2009; 27(3):347-352.
J Jr, Tinsley K, Ricci WM, et al. Induction of chondrocyte apoptosis
following impact load. J Orthop Trauma 2003;17(9):635-641.
M, Marsh JL, Brown TD. Articulated external fixation of the ankle:
minimizing motion resistance by accurate axis alignment. J Biomech
1999;32(1):63-70.
RB, Rorabeck CH, MacNab J. Intra-articular fractures of the distal
tibia: the pilon fracture. J Trauma 1983;23(7):591-596.
V, Thordarson DB, Hertz J. Ankle fusion for definitive management of
nonreconstructable pilon fractures. Foot Ankle Int 2008;29(9):914-918.
M, Ocguder DA, Ugurlu M, et al. Tibial pilon fracture repair using
Ilizarov external fixation, capsuloligamentotaxis, and early
rehabilitation of the ankle. J Foot Ankle Surg 2008;47(4):302-306.
RJ, Jones AL. Interobserver agreement in the classification of open
fractures of the tibia. The results of a survey of 245 orthopaedic
surgeons. J Bone Joint Surg Am 1994;76(8):1162-1166.
TA, Hughes MS, Anglen JO. Heterotopic ossification prophylaxis with
indomethacin increases the risk of long-bone nonunion. J Bone Joint
Surg Br 2003;85(5):700-705.
D, McConnell T, Parekh S, Tornetta P 3rd. Percutaneous pin placement in
the medial calcaneus: is anywhere safe? J Orthop Trauma
2002;16(1):26-29.
L, O’Shea K, Early JS. The use of medial and lateral surgical
approaches for the treatment of tibial plafond fractures. J Orthop
Trauma 2007;21(3):207-211.
RJ, Bindra RR, Evanoff BA, et al. Radiographic evaluation of osseous
displacement following intra-articular fractures of the distal radius:
reliability of plain radiography versus computed tomography. J Hand
Surg [Am] 1997;22(5):792-800.
C, Kuper M, Larson K, et al. Minimally invasive plating of high-energy
metaphyseal distal tibia fractures. J Orthop Trauma 2007;21(6):355-361.
C, Sanders R, DiPasquale T. Treatment of complex tibial periarticular
fractures using percutaneous techniques. Clin Orthop Relat Res
2000(375):69-77.
CM, Walker C, Garg A, McQueen MM. Half-ring external fixation in the
management of tibial plafond fractures. J Orthop Trauma
1999;13(3):200-206.
EH, Seligson D, Henry SL, Warnholtz A. Tibial pilon fractures: a
comparative clinical study of management techniques and results.
Orthopedics 1995;18(7): 613-617.
TA, Willis MC, Marsh JL, et al. Rank order analysis of tibial plafond
fractures: does injury or reduction predict outcome? Foot Ankle Int
1999;20(1):44-49.
M, Rapoff AJ, Zdeblick TA. Posterolateral fusion for isthmic
spondylolisthesis in adults: analysis of fusion rate and clinical
results. J Spinal Disord 1998;11(6): 459-464.
B, Atesalp AS, Bozkurt M, et al. Spiral and oblique fractures of distal
one-third of tibia-fibula: treatment results with circular external
fixator. Ann Acad Med Singapore 2007;36(4):267-271.
JK, Ware AW. Salvage technique for treatment of periplafond tibial
fractures: the modified fibula-pro-tibia procedure. Foot Ankle Int
2003;24(3):228-232.
D, Riemer BL, Butterfield SL, Burke CJ 3rd. Pilon fractures treated
with an articulated external fixator: a preliminary report. Orthopedics
1996;19(12): 1019-1024.
KF, Montgomery S, Field J. High-energy plafond fractures treated by a
spanning external fixator initially and followed by a second stage open
reduction internal fixation of the articular surface—preliminary
report. Injury 2001;32 Suppl 4:SD92-98.
L, Slabaugh P. Delayed wound healing, infection, and nonunion following
open reduction and internal fixation of tibial plafond fractures. J
Trauma 1986;26(12): 1116-1119.
RP, Barei DP, Kubiak EN, et al. Early limited internal fixation of
diaphyseal extensions in select pilon fractures: upgrading AO/OTA type
C fractures to AO/OTA type B. J Orthop Trauma 2008;22(6):426-429.
PJ, Schmidt AH. Assessment of bone viability in patients with
osteomyelitis: preliminary clinical experience with laser Doppler
flowmetry. J Orthop Trauma 1992; 6(3):327-332.
C, Ganz R. Long-term results of tibial plafond fractures treated with
open reduction and internal fixation. Arch Orthop Trauma Surg
1991;110(6):277-283.
RJ, Uhthoff HK. [Primary Ilizarov ankle fusion for nonreconstructable
tibial plafond fractures]. Oper Orthop Traumatol 2005;17(4-5):457-480.
JS. The relationship between socioeconomic status and health: a review
of the literature. Milbank Q 1993;71(2):279-322.
DS, Shin SS, Madan S, et al. Correction of tibial malunion and nonunion
with six-axis analysis deformity correction using the Taylor Spatial
Frame. J Orthop Trauma 2003;17(8):549-554.
DC, Marsh JL, Brown TD. Articulated external fixation of pilon
fractures: the effects on ankle joint kinematics. J Orthop Trauma
1995;9(1):76-82.
H, Zhang CQ, Luo CF, et al. Fractures of the distal tibia treated with
polyaxial locking plating. Clin Orthop Relat Res 2009;467(3):831-837.
PV, MacDonald DA, Matthews SJ, et al. Nonunion of the femoral
diaphysis. The influence of reaming and nonsteroidal anti-inflammatory
drugs. J Bone Joint Surg Br 2000;82(5):655-658.
SD, Rose SM, Dimar JR, et al. The effect of postoperative nonsteroidal
anti-inflammatory drug administration on spinal fusion. Spine
1998;23(7):834-838.
GP, Thordarson DB. Tibial plafond fractures: limited internal fixation
and a hybrid external fixator. Foot Ankle Int 1996;17(8):444-448.
A, Gardner MJ, Hettrich C, et al. Open reduction and internal fixation
of tibial pilon fractures using a lateral approach. J Orthop Trauma
2007;21(8):530-537.
U, Naser M. [Operative treatment of distal tibial fractures. Technique
of osteosynthesis and results in 128 patients (author’s transl)]. Arch
Orthop Unfallchir 1976; 86(3):341-356.
DL, Suk M. Minimally invasive percutaneous plate osteosynthesis of
fractures of the distal tibia. Instr Course Lect 2004;53:471-475.
D Jr, Sanders RW, Infante A, et al. Bohler incision: an extensile
anterolateral approach to the foot and ankle. J Orthop Trauma
2000;14(6):429-432.
D Jr, Sanders RW, Scaduto JM, et al. Vacuum-assisted wound closure (VAC
therapy) for the management of patients with high-energy soft tissue
injuries. J Orthop Trauma 2003;17(10):683-688.
D, Karnatz N, Jansen T. [One- or two-step management (with external
fixator) of severe pilon-tibial fractures]. Aktuelle Traumatol
1990;20(4):199-204.
S, deBoer P. Surgical Exposures in Orthopaedics: the Anatomic Approach.
3rd ed. Philadelphia: Lippincott Williams & Wilkins, 2003.
BD, Rettig ME. Interobserver reliability in the Gustilo and Anderson
classification of open fractures. J Orthop Trauma 1993;7(4):357-360.
JL, Agel J, Barei DP, et al. A prospective study evaluating incision
placement and wound healing for tibial plafond fractures. J Orthop
Trauma 2008;22(5):299-305; discussion 305-306.
JJ Jr, Zych GA. Infections in periarticular fractures of the lower
extremity treated with tensioned wire hybrid fixators. J Orthop Trauma
1998;12(3):214-218.
KW, Biert J, van Kampen A. Treatment of distal tibial fractures: plate
versus nail: a retrospective outcome analysis of matched pairs of
patients. Int Orthop 2007; 31(5):709-714.
JF, Waddell JP. Fractures of the distal tibial metaphysis with
intra-articular extension—the distal tibial explosion fracture. J
Trauma 1979;19(8):593-601.
G, Moed BR, Watson JT, et al. Intramedullary nailing of unstable
diaphyseal fractures of the tibia with distal intraarticular
involvement. J Orthop Trauma 1997; 11(3):200-205.
GA, Hopkins G 2nd. Posterolateral approach for tibial pilon fractures:
a report of two cases. J Orthop Trauma 1999;13(8):586-589.
HJ, Hanel DP, McKee M, et al. X-ray film measurements for healed distal
radius fractures. J Hand Surg [Am] 1996;21(1):31-39.
WF, Uhl RL, Purcell D. Use of a distal radius plate for treatment of a
tibial plafond fracture. Orthopedics 2006;29(11):989-990.
GF, Collinge C. Vascular abnormalities as assessed with CT angiography
in high-energy tibial plafond fractures. J Orthop Trauma
2008;22(1):16-22.
PT, Clarke MT, Bearcroft PW, et al. The proximal extent of the ankle
capsule and safety for the insertion of percutaneous fine wires. J Bone
Joint Surg Br 2005;87(5): 668-671.
M, Magill P, Khayyat G. Minimally invasive treatment of high velocity
intraarticular fractures of the distal tibia. Int Orthop 2008;25.
A, Stein H. Hybrid thin wire external fixation: an effective, minimally
invasive, modular surgical tool for the stabilization of periarticular
fractures. Orthopedics 2004; 27(1):59-62.
M, Marchetti S, Restuccia G, et al. Combined percutaneous internal and
external fixation of type-C tibial plafond fractures. A review of 22
cases. J Bone Joint Surg Am 2002;84-A(Suppl 2):109-115.
JL, Bonar S, Nepola JV, et al. Use of an articulated external fixator
for fractures of the tibial plafond. J Bone Joint Surg Am
1995;77(10):1498-1509.
JL, Buckwalter J, Gelberman R, et al. Articular fractures: does an
anatomic reduction really change the result? J Bone Joint Surg Am
2002;84-A(7):1259-1271.
JL, Muehling V, Dirschl D, et al. Tibial plafond fractures treated by
articulated external fixation: a randomized trial of postoperative
motion versus nonmotion. J Orthop Trauma 2006;20(8):536-541.
JL, Rattay RE, Dulaney T. Results of ankle arthrodesis for treatment of
supramalleolar nonunion and ankle arthrosis. Foot Ankle Int
1997;18(3):138-143.
JL, Saltzman CL. Ankle fractures. In: Bucholz RW, Heckman JD,
Court-Brown C, eds. Rockwood and Green’s Fractures in Adults. Vol 2.
6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006,
2147-2247.
JL, Weigel DP, Dirschl DR. Tibial plafond fractures. How do these
ankles function over time? J Bone Joint Surg Am 2003;85-A(2):287-295.
J, Marsh JL, Nepola JV, et al. Radiographic fracture assessments: which
ones can we reliably make? J Orthop Trauma 2000;14(6):379-385.
JS, Marsh JL, Bonar SK, et al. Assessment of the AO/ASIF fracture
classification for the distal tibia. J Orthop Trauma 1997;11(7):477-483.
MA, Smith SW, Boulas HJ, et al. Complications encountered in the
treatment of pilon fractures. J Orthop Trauma 1992;6(2):195-200.
TO, Rudert MJ, Tochigi Y, et al. Incongruity-dependent changes of
contact stress rates in human cadaveric ankles. J Orthop Trauma
2006;20(10):732-738.
TO, Tochigi Y, Rudert MJ, et al. Instability-associated changes in
contact stress and contact stress rates near a step-off incongruity. J
Bone Joint Surg Am 2008; 90(2):375-383.
TO, Tochigi Y, Rudert MJ, et al. The effect of incongruity and
instability on contact stress directional gradients in human cadaveric
ankles. Osteoarthritis Cartilage 2008;16(11):1363-1369.
R, Matthews SJ, Zavras DT, et al. Management of ipsilateral pilon and
calcaneal fractures: a report of two cases. J Foot Ankle Surg
2004;43(2):123-130.
TJ, Prince R, Pochatko D, et al. Retrograde intramedullary nailing for
ankle arthrodesis. Foot Ankle Int 1995;16(7):433-436.
SJ, Thordarson DB, Shepherd LE. Salvage of tibial pilon fractures using
fusion of the ankle with a 90 degrees cannulated blade-plate: a
preliminary report. Foot Ankle Int 1999;20(6):375-378.
BF, Wiedeman GP Jr. Complications and long-term results of ankle
arthrodeses following trauma. J Bone Joint Surg Am 1980;62(5):777-784.
R, Safran O, Segal D, et al. The unreamed tibial nail in the treatment
of distal metaphyseal fractures. Injury 1999;30(2):83-90.
ME, Allgower M, Schneider R. Manual of Internal Fixation: Techniques
Recommended by the AO-ASIF Group. 3rd ed. New York: Springer-Verlag,
1991.
CP, D’Ambrosia R, Dabezies EJ. The small pin circular fixator for
distal tibial pilon fractures with soft tissue compromise. Orthopedics
1991;14(3):283-290.
SE. Distal tibia fractures. In: Stannard JP, Schmidt AH, Kregor PJ,
eds. Surgical Treatment of Orthopaedic Trauma. New York: Thieme,
2007:767-791.
SE, Schwartz AK, Agel J, et al. Intramedullary nailing of distal
metaphyseal tibial fractures. J Bone Joint Surg Am 2005;87(6):1213-1221.
JK, Lee JJ, Jung DY, et al. Hybrid external fixation of distal tibial
fractures: new strategy to place pins and wires without penetrating the
anterior compartment. Arch Orthop Trauma Surg 2004;124(8):542-546.
G, Aktuglu K. Intra-articular fractures of the tibial plafond. A
comparison of the results using articulated and ring external fixators.
J Bone Joint Surg Br 2004;86(6): 868-875.
MH, Tuccar E, Demiryurek D, et al. Minimally invasive plating of the
distal tibia: do we really sacrifice saphenous vein and nerve? A
cadaver study. J Orthop Trauma 2009;23(2):132-138.
AM, Shivaram MS. Anatomical basis of variability in injuries of the
medial malleolus and the deltoid ligament. I. Anatomical studies. Acta
Orthop Scand 1979; 50(2):217-223.
MJ, Cole JD. Two-staged delayed open reduction and internal fixation of
severe pilon fractures. J Orthop Trauma 1999;13(2):85-91.
AN, McCarthy ML, Bess RS, et al. Outcomes after treatment of
high-energy tibial plafond fractures. J Bone Joint Surg Am
2003;85-A(10):1893-1900.
KJ, Wolinsky PR, McAndrew MP, et al. Tibial pilon fractures: a
comparison of treatment methods. J Trauma 1999;47(5):937-941.
H, Pechlaner S, Benedetto KP. [Long-term results after conservative and
surgical treatment of fractures of the distal end of the tibia].
Aktuelle Traumatol 1986;16(3): 117-123.
SS, Ablett D, Kaye R. High-dose nonsteroidal anti-inflammatory drugs
compromise spinal fusion. Can J Anaesth 2005;52(5):506-512.
E, Zurakowski D, Vrahas M. Acute infections after fracture repair:
management with hardware in place. Clin Orthop Relat Res
2008;466(2):466-472.
CM, McLauchlan GJ, McLean IP, et al. Distal metaphyseal fractures of
the tibia with minimal involvement of the ankle. Classification and
treatment by locked intramedullary nailing. J Bone Joint Surg Br
1995;77(5):781-787.
SR, Fragomen AT, Ilizarov S. Correction of tibial deformity with use of
the Ilizarov-Taylor spatial frame. J Bone Joint Surg Am 2006;88(Suppl
4):156-174.
SR, Pugsley JS, Fragomen AT, et al. Repair of tibial nonunions and bone
defects with the Taylor Spatial Frame. J Orthop Trauma 2008;22(2):88-95.
T. Fractures of the lower end of the tibia into the ankle joint:
results 9 years after open reduction and internal fixation. Injury
1973;5(2):130-134.
TP, Allgower M. The operative treatment of intra-articular fractures of
the lower end of the tibia. Clin Orthop Relat Res 1979(138):105-110.
HC, Papp S, Dipasquale T. The effect of suture pattern and tension on
cutaneous blood flow as assessed by laser Doppler flowmetry in a pig
model. J Orthop Trauma 2008;22(3):171-175.
M, Shanahan MD, Fern ED. Intra-articular fractures of the distal tibia:
surgical management by limited internal fixation and articulated
distraction. Injury 1993;24(1): 37-40.
KH, Kinzl L, Schmelz A. Ankle arthrodesis using Ilizarov ring fixators:
a review of 22 cases. Foot Ankle Int 2006;27(10):764-770.
R, Walling AK. Pilon fractures. In: Coughlin MJ, Mann RA, Saltzman CL,
eds. Surgery of the Foot and Ankle. Vol II. 8th ed. Philadelphia:
Mosby, 2007:1941-1971.
RW, Gorman RR, Walling AK. Replacement versus arthrodesis for
posttraumatic ankle arthritis. Paper presented at: Orthopaedic Trauma
Association 20th Annual Meeting, 2004; Hollywood, FL.
A, Grujic L, Byck DC, et al. Clinical and functional outcomes of
internal fixation of displaced pilon fractures. Clin Orthop Relat Res
1998(347):131-137.
B, Wullschleger ME, Kim H, et al. Fit assessment of anatomic plates for
the distal medial tibia. J Orthop Trauma 2008;22(4):258-263.
M, Sanders R, DiPasquale T, et al. A staged protocol for soft tissue
management in the treatment of complex pilon fractures. J Orthop Trauma
1999;13(2):78-84.
C, Ruedi T. Tibia: distal (pilon). In: Colton CL, Fernandez Dell’Oca A,
Holz U, et al., eds. AO principles of fracture management. New York:
Thieme; 2000:539-557.
JP, Robinson JT, Anderson ER, et al. Negative pressure wound therapy to
treat hematomas and surgical incisions following high-energy trauma. J
Trauma 2006; 60(6):1301-1306.
EJ, Petrucelli G, Bong M, et al. Blisters associated with
lower-extremity fracture: results of a prospective treatment protocol.
J Orthop Trauma 2006;20(9):618-622.
MF. Surgical approaches in osteomyelitis. Use of laser Doppler
flowmetry to determine nonviable bone. Infect Dis Clin North Am
1990;4(3):501-512.
MF, Hagan K, Shack RB. Adjunctive use of laser Doppler flowmetry for
debridement of osteomyelitis. J Orthop Trauma 1989;3(1):1-5.
MF, Hanel DP, Vedder NB, et al. A comparison of short- and long-term
intravenous antibiotic therapy in the postoperative management of adult
osteomyelitis. J Bone Joint Surg Br 1999;81(6):1046-1050.
MF, Sands AK, Agel J, et al. Interobserver variation in the AO/OTA
fracture classification system for pilon fractures. Is there a problem?
J Orthop Trauma 1997;11(7):467-470.
SM, Wiss DA. Open reduction and internal fixation of tibial plafond
fractures. Variables contributing to poor results and complications.
Clin Orthop Relat Res 1993(292):108-117.
M. Fractures of the distal tibial metaphysis involving the ankle joint:
the pilon fracture. In: Schatzker J, Tile M, eds. The rationale of
Operative Fracture Care. 2nd ed. New York: Springer-Verlag, 1996.
Y, Rudert MJ, McKinley TO, et al. Correlation of dynamic cartilage
contact stress aberrations with severity of instability in ankle
incongruity. J Orthop Res 2008; 26(9):1186-1193.
P 3rd, Weiner L, Bergman M, et al. Pilon fractures: treatment with
combined internal and external fixation. J Orthop Trauma
1993;7(6):489-496.
JR, Fallat LM. Dynamic unilateral distraction fixation: surgical
management of tibial pilon fractures. J Foot Ankle Surg
1994;33(5):438-442.
TE, Benirschke SK, Vedder NB. Use of radial forearm flaps to treat
complications of closed pilon fractures. J Orthop Trauma
1992;6(3):358-365.
HA, Le TT, Bedi A. Radiographic and clinical comparisons of distal
tibia shaft fractures (4 to 11 cm proximal to the plafond): plating
versus intramedullary nailing. J Orthop Trauma 2008;22(5):307-311.
MJ, Abidi NA, Ishikawa SN, et al. Soft tissue injuries with the use of
safe corridors for transfixion wire placement during external fixation
of distal tibia fractures: an anatomic study. J Orthop Trauma
2001;15(8):555-559.
AM, Haddad SL, Kadakia A, et al. Extracapsular placement of distal
tibial transfixation wires. J Bone Joint Surg Am 2004;86-A(5):988-993.
JT, Moed BR, Karges DE, Cramer KE. Pilon fractures. Treatment protocol
based on severity of soft tissue injury. Clin Orthop Relat Res
2000(375):78-90.
BG. Lengthening osteotomy of the fibula to correct a widened mortice of
the ankle after fracture. Int Orthop 1981;4(4):289-293.
TM, Marsh JL, Nepola JV, et al. External fixation of tibial plafond
fractures: is routine plating of the fibula necessary? J Orthop Trauma
1998;12(1):16-20.
TM, Nepola JV, DeCoster TA, et al. Factors affecting outcome in tibial
plafond fractures. Clin Orthop Relat Res 2004(423):93-98.
JC, van Laarhoven CJ, van der Werken C. The posterior antiglide plate
for fixation of fractures of the lateral malleolus. Injury
1992;23(2):94-96.
P, Lee M. The distal approach for anterolateral plate fixation of the
tibia: an anatomic study. J Orthop Trauma 2008;22(6):404-407.
B, McFerran MA, McAndrew M, et al. Operative treatment of fractures of
the tibial plafond. A randomized, prospective study. J Bone Joint Surg
Am 1996;78(11): 1646-1657.
C, Atesalp AS, Demiralp B, Gur E. High-velocity gunshot wounds of the
tibial plafond managed with Ilizarov external fixation: a report of 13
cases. J Orthop Trauma 2003;17(6):421-429.
BA, Bhandari M, Espiritu M, et al. Treatment of distal tibia fractures
without articular involvement: a systematic review of 1125 fractures. J
Orthop Trauma 2006; 20(1):76-79.
