Pediatric Femoral Shaft
-
Represent 1.6% of all fractures in the pediatric population.
-
Boys are more commonly affected at a ratio of 2.6:1.
-
Bimodal distribution of incidence: The first peak is from 2 to 4 years of age, and the second is in mid-adolescence.
-
There is also a seasonal distribution, with a higher incidence during the summer months.
-
In children younger than walking age, 80% of these injuries are caused by child abuse; this decreases to 30% in toddlers.
-
In adolescence, >90% of femoral fractures are caused by motor vehicle accident.
-
During childhood, remodeling in the femur causes a change from primarily weaker woven bone to stronger lamellar bone.
-
Up to age 16 years, there is a geometric
increase in the femoral shaft diameter and relative cortical thickness
of the femur, resulting in a markedly increased area moment of inertia
and strength. This partially explains the bimodal distribution of
injury pattern, in which younger patients experience fractures under
load conditions reached in normal play or minor trauma, whereas in
adolescence high-energy trauma is required to reach the stresses
necessary for fracture (Fig. 48.1).
-
Direct trauma: Motor vehicle accident, pedestrian injury, fall, and child abuse are causes.
-
Indirect trauma: Rotational injury.
-
Pathologic fractures: Causes include
osteogenesis imperfecta, nonossifying fibroma, bone cysts, and tumors.
Severe involvement from myelomeningocele or cerebral palsy may result
in generalized osteopenia and a predisposition to fracture with minor
trauma.
-
Patients with a history of high-energy injury should undergo full trauma evaluation as indicated.
-
The presence of a femoral shaft fracture
results in an inability to ambulate, with extreme pain, variable
swelling, and variable gross deformity. The diagnosis is more difficult
in patients with multiple trauma or head injury or in nonambulatory,
severely disabled children. -
A careful neurovascular examination is essential.
-
Splints or bandages placed in the field
must be removed with a careful examination of the overlying soft
tissues to rule out the possibility of an open fracture. -
Hypotension from an isolated femoral
shaft fracture is uncommon. The Waddell triad of head injury,
intraabdominal or intrathoracic trauma, and femoral shaft fracture is
strongly
P.579
associated
with vehicular trauma and is a more likely cause of volume loss.
However, the presence of a severely swollen thigh may indicate large
volume loss into muscle compartments surrounding the fracture.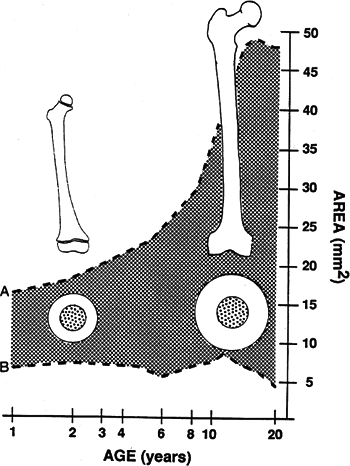 Figure 48.1. The shaded area
Figure 48.1. The shaded area
represents cortical thickness by age group. This rapid increase in
cortical thickness may contribute to the diminishing incidence of
femoral fractures during late childhood.(Redrawn from Netter FH. The Ciba collection of medical illustrations.
Vol. 8. Musculoskeletal system. Part I. Anatomy, physiology, and
metabolic disorders. Summit, NJ: Ciba-Geigy, 1987; in Bucholz RW,
Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.) -
Compartment syndrome is rare and occurs only with severe hemorrhage into thigh compartments.
-
The ipsilateral hip and knee should be examined for associated injuries.
-
Anteroposterior and lateral views of the femur should be obtained.
-
Radiographs of the hip and knee should be
obtained to rule out associated injuries; intertrochanteric fractures,
femoral neck fractures, hip dislocation, physeal injuries to the distal
femur, ligamentous disruptions, meniscal tears, and tibial fractures
have all been described in association with femoral shaft fractures. -
Magnetic resonance imaging and bone scans
are generally unnecessary but may aid in the diagnosis of otherwise
occult nondisplaced, buckle, or stress fractures.
-
Open versus closed
-
Level of fracture: proximal, middle, distal third
-
Fracture pattern: transverse, spiral, oblique, butterfly fragment
-
Comminution
-
Displacement
-
Angulation
-
Subtrochanteric
-
Shaft
-
Supracondylar
among age groups. The size of the child must be considered when
choosing a treatment method, as well as the mechanism of the injury
(i.e., isolated, low-energy versus high-energy polytrauma).
-
Pavlik harness or a posterior splint is indicated.
-
Traction and spica casting are rarely needed in this age group.
-
Immediate spica casting is nearly always the treatment of choice (>95%).
-
Skeletal traction followed by spica
casting may be needed if one is unable to maintain length and
acceptable alignment; a traction pin is preferably placed proximal to
the distal femoral physis. -
External fixation may be considered for multiple injuries or open fracture.
-
Flexible intramedullary nails placed in a retrograde fashion are frequently used in this age group.
-
External fixation or bridge plating may be considered for multiple injuries or open fracture.
-
Some centers are using interlocked nails inserted through the greater trochanter (controversial).
-
Spica casting may be used for the axially stable fractures in this age group.
-
Intramedullary fixation with either flexible or interlocked nails is the treatment of choice.
-
Locked submuscular plates may be considered for supracondylar or subtrochanteric fractures.
-
External fixation may be considered for multiple injuries or open fracture.
-
Length
-
Angulation
-
Sagittal plane: Up to 30 degrees of recurvatum/procurvatum is acceptable.
-
Frontal plane: Up to 10 degrees of varus/valgus angulation is acceptable (varus commonly seen with spica casting).
-
This varies with pattern, age, and location of fracture along the femur.
-
-
Rotation
-
Up to 10 degrees is acceptable; external rotation is better tolerated than internal rotation.
-
|
Table 48.1. Acceptable angulation
|
||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||
-
Multiple trauma, including head trauma
-
Open fracture
-
Vascular injury
-
Pathologic fracture
-
Uncooperative patient
-
Body habitus not amenable to spica casting
-
Intramedullary nailing
-
Flexible nails: These are inserted retrograde proximal to the distal femoral physis.
-
Reamed, locked intramedullary nails:
These are placed antegrade through the piriformis fossa or greater
trochanter. The distal physis should not be traversed. A piriformis
entry point is not recommended for patients <12 years old (proximal
femoral physis open), because proximal femoral growth abnormalities and
osteonecrosis of the femoral head owing to disruption of the vascular
supply are possible complications. A trochanteric entry point
theoretically reduces the risk of osteonecrosis.
-
-
External fixation
-
Lateral, unilateral frame: This spares the quadriceps mechanism.
-
This approach is useful in multiple
trauma, especially in those who are hemodynamically unstable, have open
fractures or burn patients.
-
-
Plate fixation
-
This may be accomplished using a 3.5 or
4.5 mm compression plate, with interfragmentary compression of
comminuted fragments; it is less desirable because of the long incision
necessary, significant periosteal stripping, quadriceps scarring,
frequent need for plate removal, and infection. -
Submuscular locking plates are useful for
supracondylar and subtrochanteric fractures in which intramedullary
devices have limited fixation. Less soft tissue stripping needed, but
infection and plate removal remain concerns.
-
-
Malunion: Remodeling will not correct
rotational deformities. An older child will not remodel as well as a
younger child. Anteroposterior remodeling occurs much more rapidly and
completely in the femur than varus/valgus angular deformity. For this
reason, greater degrees of sagittal angulation are acceptable. -
Nonunion: Rare; even with segmental
fractures, children often have sufficient osteogenic potential to fill
moderate defects. Children 5 to 10 years of age with established
nonunion may require bone grafting and plate fixation, although the
trend in older (>12 years) children is locked intramedullary nailing. -
Muscle weakness: Many patients
demonstrate weakness, typically in hip abductors, quadriceps, or
hamstrings, with up to a 30% decrease in strength and 1 cm thigh
atrophy as compared with the contralateral, uninjured lower extremity,
although this is seldom clinically significant. -
Leg length discrepancy: Secondary to
shortening or overgrowth. It represents the most common complication
after femoral shaft fracture.-
Overgrowth: Overgrowth of 1.5 to 2.0 cm
is common in the 2- to 10-year age range. It is most common during the
initial 2 years after fracture, especially with fractures of the distal
third of the femur and those associated with greater degrees of trauma. -
Shortening: Up to 2.0 cm (age dependent)
of initial shortening is acceptable because of the potential for
overgrowth. For fractures with greater than 3.0 cm of shortening,
skeletal traction may be employed before spica casting to obtain
adequate length. If the shortening is unacceptable at 6 weeks after
fracture, the decision must be made whether osteoclasis and distraction
with external fixation are preferable to a later limb length
equalization procedure.
-
-
Osteonecrosis: Proximal femoral
osteonecrosis may result from antegrade placement of an intramedullary
nail owing to the precarious vascular supply. This is of particular
concern when the proximal femoral physis is not yet closed, because the
major vascular supply to the femoral head is derived from the lateral
ascending cervical artery, which crosses the capsule at the level of
the trochanteric notch. Recently, intramedullary nails with a
trochanteric starting point have been advocated to reduce the risk of
osteonecrosis. Radiographic changes may be seen as late as 15 months
after antegrade intramedullary nailing.
