Patella Fractures and Extensor Mechanism Injuries
improvements in both fracture fixation techniques and an improved
understanding of patellar function. Until the nineteenth century, the
vast majority of patella fractures were treated nonoperatively with
extension splinting. The critical structural and biomechanical
functions of the patella were not understood, such that excision of a
“vestigial embryological remnant” was thought to be a reasonable option.24 Brooke24
published results showing increased limb strength after patellectomy
compared with normal controls and advocated patellectomy as a viable
surgical option. Hey-Groves56 and Watson-Jones154
believed that the patella inhibited quadriceps function and concluded
that the strength of the knee was improved after patellectomy. Blodgett
and Fairchild19 and Thompson146
published additional clinical series describing excellent clinical
results with partial or complete patellar excision for fracture.
was tempered, however, by modest functional outcomes. Extension
splinting was associated with high rates of residual pain, nonunion,
and permanent disability.41 Furthermore, laboratory and clinical studies raised concern regarding outcomes after patellectomy. Cohn35 and Bruce and Walmsley74
demonstrated degenerative changes on the femoral articular surface
after patellectomy in a rabbit model. A high rate of patient
dissatisfaction, decreased quadriceps strength, residual pain, and
functional disability was also reported after total patellectomy.40,45,65,89,130,137,157
and others demonstrated the critical biomechanical function of the
patella and highlighted the importance of its preservation to optimize
function of the extensor mechanism. With advances in aseptic surgery
and techniques in fracture fixation, significant interest developed in
identifying alternative means of treatment for these injuries.
Malgaigne designed the griffe metallique in 1843, a metal claw connected to sliding plates designed to reapproximate fragments in displaced patellar fracture patterns.36,93
Sir Hector Cameron of Glasgow, Scotland, performed the first open
reduction and internal fixation of a patella fracture in 1877 with
interfragmentary wiring.28 Lister and Trendelenberg88
performed similar procedures in Germany using drill holes and wire
fixation. Numerous techniques of fracture reduction and fixation
emerged, but stable fixation was difficult to achieve.39,56,57,145 Materials used for fixation included percutaneous pins, metal loops, kangaroo tendon xenografts, fascial strips, and screws.39,56,57,145
however, occurred in the 1950s with presentation of the anterior
tension band technique by Pauwel.106
The Arbeitsgemeinschaft fur Osteosynthesefragen/Association for the
Study of Internal Fixation (AO/ASIF) subsequently modified and
advocated tension band fixation as a rigid construct that allowed for
early range-of-motion and rehabilitation of patella fractures.106 Weber et al.156
demonstrated superior biomechanical strength with modified anterior
tension banding and retinacular repair in a transverse patellar
fracture model compared with cerclage or interfragmentary wiring
techniques. Numerous clinical series have subsequently confirmed a high
rate of success with tension band wiring techniques.20,21,61,152 Currently, three forms of operative treatment for displaced patella fractures are most commonly used:
-
Open reduction and internal fixation, usually with a tension band wiring technique
-
Partial patellectomy
-
Total patellectomy
and dependent on the fracture pattern, patient activity level, and
functional expectations. Each procedure can achieve good to excellent
results with proper patient selection and application. Regardless of
the selected technique, the goals of surgical treatment are:
-
Restoration of the articular surface of the patella
-
Maximum preservation of the patella
-
Preservation of the functional integrity and strength of the extensor mechanism
all skeletal fractures and may result from direct, indirect, or
combined injury patterns. The patella is prone to injury from a direct
blow as a consequence of its anterior location and thin overlying soft
tissue envelope. Direct injuries may be low-energy, such as after a
fall from sitting or standing height, or high energy, as from a
dashboard injury in a motor vehicle collision. Comminuted fracture
patterns are often the result of high-energy, direct injuries. In these
cases, it is critical to survey for associated injuries of the
ipsilateral limb, including hip dislocation, proximal femur fractures,
or fractures about the knee.
generated through the extensor mechanism and typically result from
forceful contraction of the quadriceps with the knee in a flexed
position. The substantial force generated by a violent quadriceps
contraction fractures the patella and may propagate through the
adjacent retinaculum of the extensor mechanism. As a result, indirect
injuries frequently cause a greater degree of retinacular disruption
compared with direct injuries, and active knee extension is compromised
in most cases. The degree of fragment displacement is generally
representative of occult injury to the adjacent soft tissue envelope.
While transverse fracture patterns are associated with an indirect
injury mechanism, it is clear that fracture pattern is not solely
determined by injury mechanism and is also dependent on various other
factors such as patient age, bone quality, and the degree of knee
flexion. In reality, patellar fractures likely reflect a combination of
both direct and indirect forces—the culmination of a direct blow,
quadriceps muscle contraction, and secondary joint collapse.
fracture pattern resulting from excessive tensile forces through the
extensor mechanism. These may occur through the body, apex, or distal
pole of the patella. Small proximal or distal avulsiontype fractures
should not be ignored, as they are often associated with substantial
soft tissue injury to the quadriceps or patellar tendon. Vertical
fractures are typically the result of a direct blow to a partially
flexed knee and may be nondisplaced if the retinaculum and extensor
mechanism are intact. Comminuted, stellate fracture patterns are
typically the result of a direct blow with impaction against the
femoral condyles and can be associated with substantial injury to both
the femoral and patellar chondral surfaces.
patella, a fall from standing height, or a near fall with forceful
contraction of the quadriceps on a partially flexed knee. Correlation
of the fracture with the mechanism of injury will help the surgeon to
anticipate both the fracture pattern and degree of soft tissue injury.
Complaints of anterior knee pain, swelling, and difficulty ambulating
after a fall are also common and may reflect an injury to the extensor
mechanism. With high-energy injuries, the surgeon must have a low
threshold of suspicion for associated lower and upper extremity
musculoskeletal injuries.
typically present with an acute hemarthrosis and a tender, palpable
defect between the fracture fragments. The absence of a large effusion
in the presence of palpable bony defect should raise concern for
associated retinacular tears. Competence of the extensor mechanism must
be assessed by asking the patient to perform a straight-leg raise or
extend a partially flexed knee against gravity. A large hemarthrosis
may be very painful and limit the ability of the patient to comply with
this part of the examination. In these situations, aspiration of the
hemarthrosis followed by injection of a local anesthetic into the joint
may be helpful. It is critical to note, however, that the patient’s
ability
to
extend the knee does not rule out a patella fracture but rather it
suggests that the continuity of the extensor mechanism is maintained
via an intact retinacular sleeve.
patella are of particular concern and may reflect an occult open
fracture or communication with the knee joint. Any concern warrants
further investigation with a saline load test. A large-bore, 18-gauge
needle and syringe are used to perform a joint aspiration, followed by
infusion of 50 to 100 mL of saline into the knee joint. Any
communication between the knee joint and the wound is marked by egress
of the infused saline from the wound. Methylene blue may be added to
the saline infusion to facilitate detection. Open fractures or
arthrotomies warrant emergent irrigation and debridement in the
operating room.
should be splinted, iced, and elevated. The knee is typically
immobilized in a slightly flexed position for comfort until definitive
treatment is rendered.
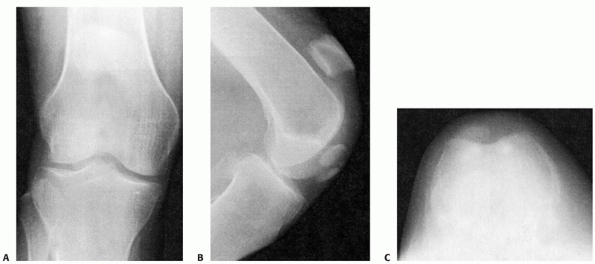
diagnosis of patellar fracture or injury to the extensor mechanism.
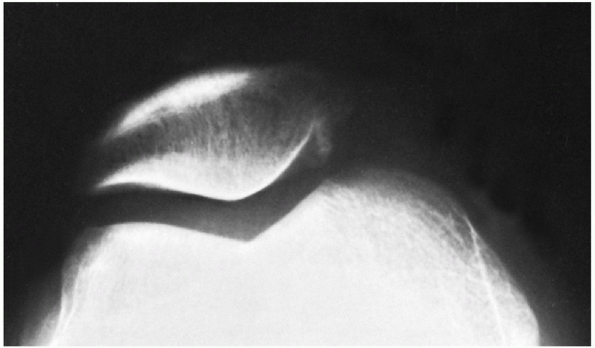
Anteroposterior (AP), lateral, and a tangential or axial view of the
patellofemoral joint should be obtained (Fig. 52-1).
Views of the contralateral knee are helpful for comparison and may
prevent the erroneous diagnosis of a normal anatomic variant as a
fracture.
should be taken with the largest cassette possible (typically 14 × 17
inches) placed behind the knee of the supine patient. If full knee
extension is not possible secondary to pain, the x-ray beam trajectory
must be adjusted accordingly. Leg rotation must be controlled so the
patella is pointing straight up and will be centered on the film. The
patella should lie within the midline of the femoral sulcus, and the
distal pole should be no higher than 20 mm above a tangential line
connecting the distal femoral condyles. Vertical and horizontal
fracture lines should be carefully noted. Typically, the degree of
fracture comminution is underestimated by the radiographically evident
fracture lines. The distal femur and proximal tibia should not be
ignored and must be carefully inspected for occult condylar or plateau
fractures.
 |
|
FIGURE 52-1 Anteroposterior (A), lateral (B), and axial (C) views of a displaced transverse patella fracture.
|
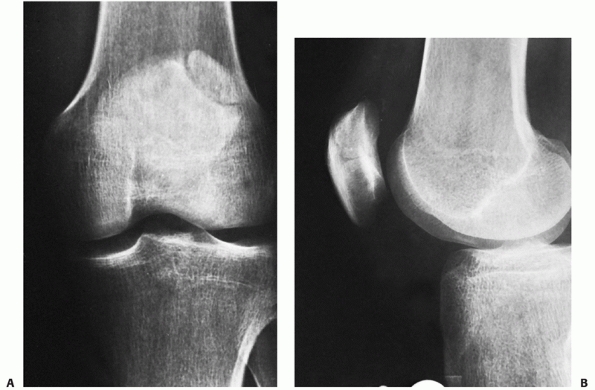
These anatomic variants reflect incomplete fusion of two or more
ossification centers. The opposing edges are usually smooth and
corticated on plain radiographs. The finding is typically bilateral,
and contralateral knee radiographs often confirm the diagnosis. The
most common bipartite pattern is located in the superolateral aspect of
the patella and is not associated with any pain, tenderness, or
functional compromise of the extensor mechanism on physical
examination. A true unilateral bipartite patella is extremely rare, and
may represent an old avulsiontype patellar fracture.
fracture pattern and associated extensor mechanism disruption.
Controlling limb rotation, however, is essential to obtain a true
lateral view that allows for reliable determination of patellar height
and identification of occult injuries. The distal patellar pole and
tibial tubercle should be carefully inspected for subtle avulsion
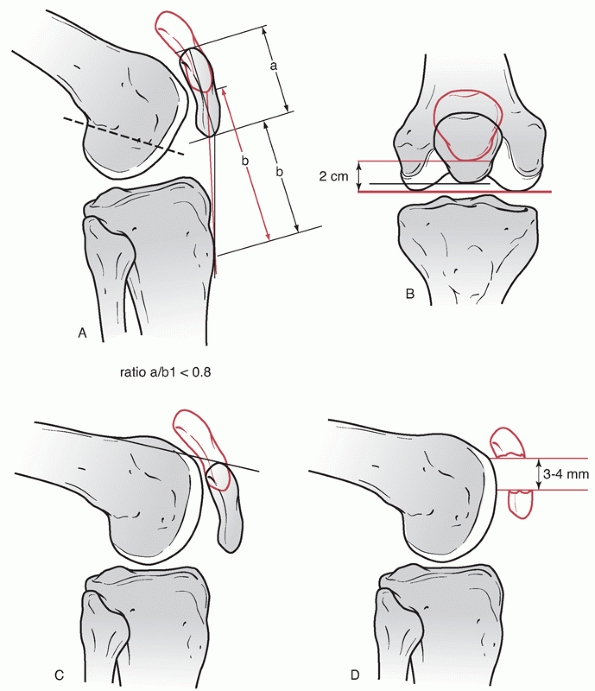
fractures. Patellar height should be assessed by the Insall-Salvati
ratio, which compares the height of the patella to the length of the
patellar tendon. In a normal subject, a ratio of 1.02 ± 0.13 is
expected.64 A ratio of less than 1.0
suggests patella alta and disruption of the patellar tendon. A ratio of
greater than 1.0 is associated with patella baja and quadriceps tendon
disruption.64 Other less sensitive
indices of patellar height can also be assessed on the lateral view.
With the knee flexed 90 degrees, the proximal patellar pole normally
rests at or below the level of the anterior cortex of the femur31,64 (Fig. 52-3).
With the knee flexed 30 degrees, the inferior patellar pole normally
projects to the level of the Blumensaat line (the distal physeal scar
remnant).31,64 Loss of this relationship is suggestive of extensor mechanism disruption.
is also useful. With patellar fractures, vertical or marginal fracture
lines
and associated osteochondral defects may only be visualized on this view. Merchant and associates103
described their technique for obtaining an axial view of the patella.
With the patient supine and the knees flexed 45 degrees over the edge
of the table, the x-ray beam is angled 30 degrees below horizontal with
the cassette placed approximately 6 to 12 inches below the knees and
perpendicular to the beam. This technique is easily performed in
patients with knee trauma, because supporting the knee in a partially
flexed position often confers maximal comfort in the setting of an
acute hemarthrosis.
 |
|
FIGURE 52-2 Anteroposterior (A) and lateral (B) radiographs of a bipartite patella. Note the superolateral fragment with well-defined cortical margins.
|
 |
|
FIGURE 52-3 A.
The length of the patellar tendon should approximate the midsagittal length of the patella and the inferior pole of the patella projects to the level of Blumenstaat line (dashed line). A ratio of less than 0.8 indicates possible injury to the patellar tendon (method of Insall). B. On the anteroposterior radiograph, the inferior pole of the patella should lie within 2 cm of a plane formed by the distal femoral condyles. C. At 90 degrees of flexion, the superior pole of the patella should lie inferior to the anterior surface of the femoral shaft. D. The lateral view gives the best view of the fracture pattern and of fragment separation. |
the evaluation and treatment of isolated patellar fractures.
Frequently, however, the patella may be incidentally imaged during the
evaluation of an ipsilateral distal femoral or proximal tibial
fracture. While CT allows for improved evaluation of articular
congruity and fracture comminution, it rarely provides additional
information that will alter the treatment plan that has been rendered
based on physical examination and plain radiographs.
demonstrated a 71% sensitivity of tomography in detecting stress
fractures in elderly, osteopenic patients, compared with 30% with bone
scans and 0% with plain radiographs alone. CT is also useful to
characterize trochlear anatomy and lower extremity rotational alignment
with patellofemoral tracking disorders.
increasingly to identify extensor mechanism injuries as well as
chondral or osteochondral injuries associated with patellar fractures.151,162
The normal quadriceps and patellar tendons have a laminated appearance
with homogeneous, low signal intensity on MRI. Trauma to the patella or
adjacent soft tissues results in hemorrhage and edema and is associated
with increased signal intensity on T2-weighted images. Furthermore,
loss of continuity of patellar or quadriceps tendon fibers can be
readily seen to define both partial or complete disruptions.151,162
gadolinium-enhanced imaging of articular cartilage (dGEMRIC) allow for
the identification of chondral injuries that may not be visualized on
plain radiographs.147 These lesions may be amenable to treatment at the time of patellar fracture fixation.
characteristic edema pattern on MRI that allows for confirmation of the
diagnosis even after spontaneous reduction following the injury. In
addition to a traumatic effusion, contusion of the lateral femoral
condyle and medial patellar facet with increased signal on T2-weighted
images, disruption of the medial patellofemoral ligament, retinacular
tears, and osteochondral loose bodies are frequently seen.151
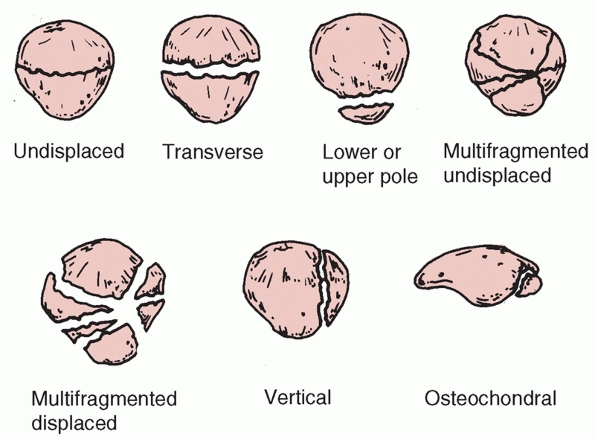
descriptive in nature and can be based on fracture pattern, degree of
displacement, or mechanism of injury. The Orthopaedic Trauma
Association classification system is universally accepted, but neither
this scheme nor any other classification system has been shown to
correlate fracture pattern with clinical outcome. For this reason, most
clinical series have reported outcomes based on the type of fixation
rather than fracture pattern.20,21,22,34,87,109,142
Practically, a treatment-based approach begins with classifying
patellar fractures as displaced or nondisplaced. Displaced patellar
fractures are defined by separation of fracture fragments by more than
3 mm or articular incongruity of more than 2 mm. After the fracture is
classified as displaced or nondisplaced, the injury can be further
categorized based on the geometric configuration of fracture lines (Table 52-1).
Described patterns include transverse or horizontal, stellate or
comminuted, vertical or longitudinal, apical or marginal, and
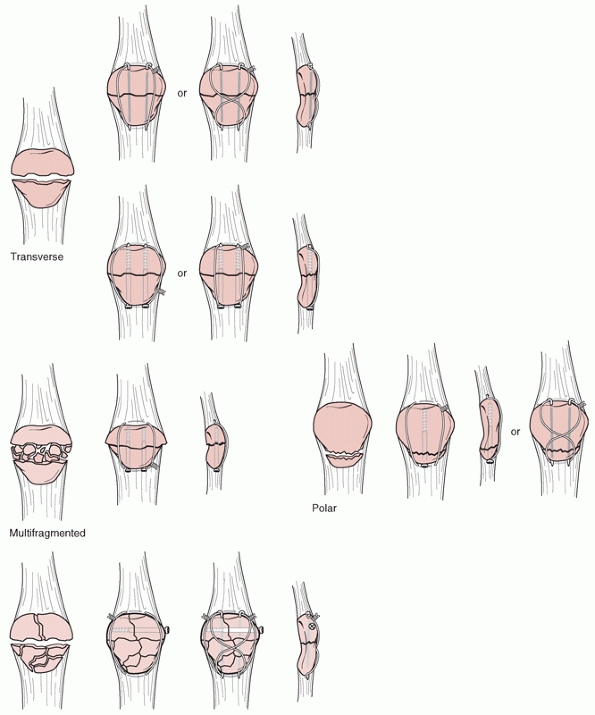
osteochondral (Fig. 52-4). In addition, a
special category of patellar sleeve fractures can occur in skeletally
immature patients in which a distal pole fragment with a large
component of the articular surface avulses from the remaining patella.
|
TABLE 52-1 Patellar Fracture Classification
|
||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||
forces that fracture the patella but are insufficient to tear the
medial and lateral patellar retinaculum. As a result, the extensor
mechanism remains competent. The preserved integrity of the soft tissue
envelope helps to maintain the reduction. Approximately 80% of these
fractures occur in the middle to lower third of the patella.111
 |
|
FIGURE 52-4 Descriptive classification of patellar fractures.
|
injuries to the patella with the knee in a partially flexed position.
Approximately 65% of these injuries are nondisplaced.11,22
Active knee extension is preserved, because the medial and lateral
patellar retinacula are usually not torn with the injury. Damage to the
patellar and femoral articular surface is not uncommon given the
mechanism of injury, and careful evaluation on tangential views or MRI
is necessary to identify occult osteochondral lesions.
uncommon and has been reported to account for 12% to 22% of patellar
fractures in several large series.18,42,111
The fracture line is most commonly seen involving the lateral facet and
lying between the middle and lateral third of the patella. Different
mechanisms of injury have been implicated. Bostrom et al.23 reported that lateral avulsion was the most common mechanism in 75% of their series. Dowd,42
however, reported that direct compression of the patella in a
hyperflexed knee is responsible for this pattern of injury. The
patellar retinacula are intact, preserving active knee extension by the
patient. The fracture pattern is easily missed on an AP radiograph,
emphasizing the importance of an axial view to identify this injury.
Evaluation of the integrity of the extensor mechanism is critical with
this pattern of injury. The fracture fragment separation (>3 mm) is
suggestive but not diagnostic of
retinacular and extensor mechanism disruption. A subset of these
fractures with fragment displacement but intact retinacula exists and
is characterized by preservation of full active knee extension. These
fractures may respond more favorably to nonoperative treatment. Bostrom
et al.22 has reported that preservation of the retinacula allows satisfactory healing without surgery. McMaster,101 however, has warned of a high risk of nonunion with nonoperative treatment in these patients.
high-energy, direct blow to the patella. These fractures typically
demonstrate a high degree of comminution. Anterior soft tissue
contusion and/or lacerations are not uncommon, and careful evaluation
for an open fracture or traumatic arthrotomy is warranted. Transverse
fracture lines with extensive comminution may result in propagation
into the retinaculum and disruption of the extensor mechanism. However,
even if the extensor mechanism is preserved, the significant articular
incongruity may warrant operative intervention.
typically bony avulsions of the quadriceps mechanism. Displacement is
rare and has been reported to be approximately 4% in large clinical
series.22,134
Active knee extension may be preserved if the medial and lateral
retinacula remain intact. The lateral radiograph may demonstrate
patella baja and a reduced Insall-Salvati ratio. Distal pole fractures
are bony avulsions of the patellar tendon. Displacement is much more
common with these injuries and has been reported to occur in up to
11.5% in large series.22,134
Retinacular disruption with loss of knee extension is virtually
universal with distal pole fractures. A lateral radiograph will
demonstrate patella alta and an increased Insall-Salvati ratio.64
seen in association with high-energy, stellate patellar fractures or
after patellar dislocation (Fig. 52-5). Plain
radiographs may not demonstrate these lesions. MRI with
cartilage-sensitive sequences can improve the detection of these
injuries.162 Osteochondral fracture
fragments can shear from the lateral femoral condyle or medial patellar
facet after patellar subluxation or dislocation and may warrant
surgical intervention. Kroner79 first reported on a series of these fractures after patellar subluxation in patients 15 to 20 years of age.
graft harvest for bone-tendon-bone anterior cruciate ligament (ACL)
reconstruction. An incidence of 0.2% has been reported in one series of
more than 1700 ACL reconstructions.82
While these may occur intraoperatively secondary to technical error,
the majority of cases have been attributed to postoperative trauma from
a fall or overly aggressive rehabilitation protocols. Both transverse
and vertical fracture patterns have been reported. Rigid fixation of
these fractures, even in the setting of minimal displacement, has been
advocated to allow for early motion and avoid delayed rehabilitation of
the ACL reconstruction.
variant and should not be misdiagnosed as a displaced patellar
fracture. A bipartite fragment typically presents as a well-corticated
fragment
in
the superolateral aspect of the patella and is the result of incomplete
fusion of ossification centers. The incidence of a bipartite patella is
approximately 8% and is almost always seen bilaterally.1,112 Radiographs of the contralateral knee will confirm the diagnosis.
 |
|
FIGURE 52-5
A minimally displaced osteochondral fracture of the medial facet after an acute patellar dislocation best demonstrated with a Merchant view. |
deep to the fascia lata within the tendon fibers of the rectus femoris.
Its proximal margin is termed the basis, and the rounded inferior
margin, the apex. Ossification centers typically appear at 2 to 3 years
of age. While its shape can vary considerably, the patella is typically
ovoid and flat anteriorly on its nonarticular surface.22
with thick articular cartilage, while the distal pole is entirely
devoid of articular cartilage. For this reason, most distal pole
fractures are extra-articular. The articular cartilage can be 1 cm or
greater in thickness in a normal patella.124
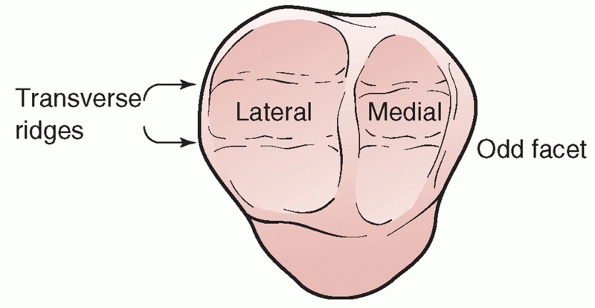
The proximal articular region is divided into medial and lateral facets
by a longitudinal ridge. A second, vertical ridge along the medial
border of the patella defines a small medial region termed the odd facet.124 Small, transverse ridges further subdivide the medial and lateral facets into superior, intermediate, and inferior facets (Fig. 52-6).
While the lateral facet is usually the largest, considerable variation
in the size and shape of patellar facets has been observed. Wiberg158 classified patellar osteology into three major groups based on the size of the medial and lateral facets:
-
Type I: medial and lateral facets are both concave and approximately equal in size
-
Type II: the medial, concave facet is smaller than the lateral facet
-
Type III: the medial, convex facet is smaller than the lateral facet
Type II and III patellas have a small, flat medial facet, while type IV
patellas have a small, steeply sloped medial facet with a medial ridge.
Type V, termed the Jaegerhut patella, is devoid of a medial facet or
vertical ridge.14
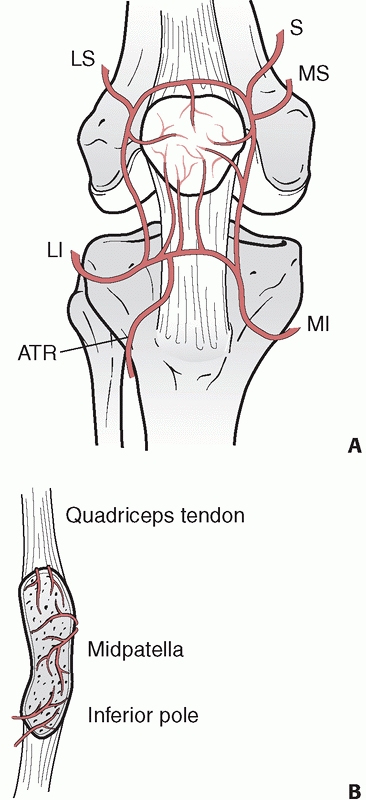
of blood vessels that can be separated into both an extraosseous and an
intraosseous vascular system (Fig. 52-7). Six
separate arteries contribute to this vascular plexus and help to
preserve fragment vascularity even in the setting of comminuted
fracture patterns.127,135
The supreme geniculate artery arises from the superficial femoral
artery at the level of Hunter’s canal, while the four geniculate
arteries take origin from the popliteal artery. The recurrent anterior
tibial artery is a branch of the anterior tibial artery, taking origin
approximately 1 cm below the proximal tibiofibular joint. The superior
portion of the plexus lies dorsal to the quadriceps tendon, while the
inferior aspect passes deep to the patellar tendon in the fat pad.
Scapinelli127 has shown that the
primary intraosseous blood supply of the patella enters through the
middle third of the anterior body and distal pole and perfuses in a
distal to proximal fashion. This pattern of retrograde perfusion is
important in understanding the risk of osteonecrosis after patellar
fracture.
 |
|
FIGURE 52-6 The articular surface of the patella.
|
 |
|
FIGURE 52-7 Arterial blood supply of the patella. A.
Extraosseous geniculate arterial system. S, supreme geniculate; MS, medial superior geniculate; MI, medial inferior geniculate; ATR, anterior tibial recurrent; LI, lateral inferior geniculate; LS, lateral superior geniculate. B. Intraosseous arterial supply. |
fat pad receiving contributions from the inferior medial and lateral
geniculate arteries. The superficial surface of the tendon is supplied
by retinacular vessels that arise from the inferior medial geniculate
and recurrent tibial arteries.135
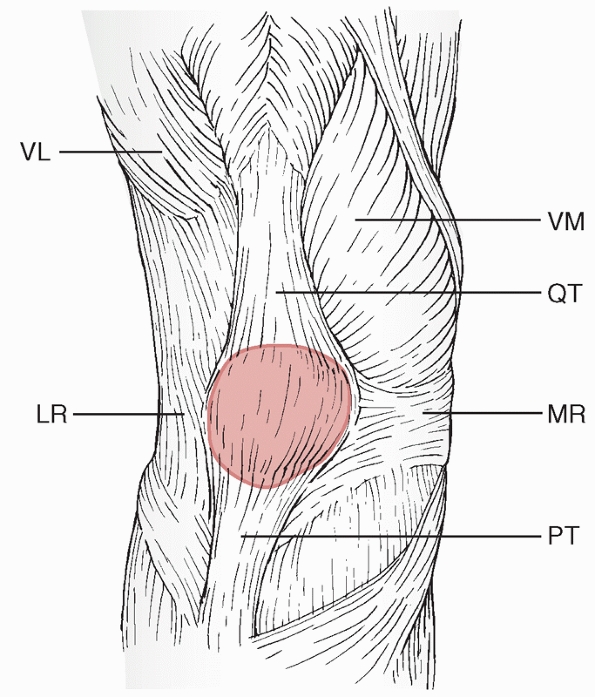
tendon deep to the fascia lata. The extensor mechanism, however,
collectively refers to the quadriceps tendon, medial and lateral
retinacula, patella, and patellar tendon (Fig. 52-8).
lateralis, vastus medialis, rectus femoris, and vastus intermedius. The
vastus lateralis originates from the femur and inserts
on
the patella at an approximately 30-degree angle relative to the
longitudinal axis of femur. Its most medial fibers insert on the
superolateral patella, and its most lateral fibers run lateral to the
patella to insert into the lateral retinaculum and the iliotibial tract.87,124
The vastus medialis consists of two distinct portions separated by
fascia and innervated by distinct branches of the femoral nerve.87,124
The vastus medialis longus inserts on the patella proximally at an
angle of 15 to 18 degrees relative to the long axis of the femur, while
the vastus medialis obliquus inserts more distally on the patella at an
angle of 50 to 55 degrees.87,124
The rectus femoris is a long, fusiform muscle that lies central and
superficial in the quadriceps complex. The fibers run 7 to 10 degrees
medially relative to the long axis of the femur in the coronal plane.
The vastus intermedius lies deep to the rectus femoris and inserts
directly into the superior pole of the patella.87,124
 |
|
FIGURE 52-8
Soft tissue anatomy of the patella. VL, vastus lateralis, LR, lateral retinaculum; VM, vastus medialis; QT, quadriceps tendon; MR, medial retinaculum; PT, patellar tendon. |
described. Previous studies have reported a trilaminar organization,
with the rectus femoris tendon superficial, the vastus medialis and
lateralis tendons in the middle, and the vastus intermedius fibers deep.87
In reality, however, the insertion reflects an intricate blending of
all tendon fibers at the insertion into the superior patella.124
secondary extensors of the knee. The retinaculum is formed by the
continuation of the deep investing fascia lata in the thigh and
reinforced by inserting aponeurotic fibers from both the vastus
medialis and lateralis. Both the medial and lateral retinacula insert
directly into the proximal tibia and can thereby allow for active knee
extension in the setting of an isolated patellar fracture.22
continuation of the deep retinacular surface of the vastus medialis
obliquus that extends from the superior medial border of the patella
and attaches to the medial epicondyle just anterior to the medial
collateral ligament.10,110 The medial patellofemoral ligament is accepted to be the major restraint to lateral patellar displacement10 and contributes 50% to 60% of the total restraining force of the medial patellar stabilizers.110
It has a fanshaped configuration that runs from the upper medial margin
of the patella to a femoral insertion posterosuperior to the epicondyle
and just distal to the adductor tubercle. Cadaver dissections have
revealed the ligament to be 58.8 ± 4.7 mm in length and 12.0 ± 3.1 mm
in width and inclined 15.9 ± 5.6 degrees proximally.110
patella proximally and inserts into the tibial tubercle distally. Its
average length is 5 cm. The patellar tendon is formed primarily from a
continuation of the central fibers of the rectus femoris tendon. The
tendon is reinforced medially and laterally by the extensor retinaculum
and the iliotibial tract as it inserts into the tibia.124
for active knee extension and the ability to maintain an erect
position. Numerous activities of daily living, including walking,
ascending stairs, or rising from a chair, depend on the extensor
mechanism to generate sufficient force to overcome gravity.71,133
During initial knee extension from a fully flexed position, the patella
functions as a link between the quadriceps and the patellar tendon. In
this capacity, it allows for transmission of torque generated by the
quadriceps muscle to the proximal tibia. For young men, these forces
can exceed 6000 N and can approach up to eight times body weight.60
At 135 degrees of flexion, linking occurs via transmission of forces
between the extensive contact area of the trochlea with the patellar
facets and the posterior surface of the quadriceps tendon.52
From 135 to 45 degrees of flexion, the odd facet engages the femur. The
odd facet is the only portion of the patella that articulates with the
tibial surface of the medial femoral condyle but not the trochlear.52 Albanese et al.3
studied knee extension mechanics after subtotal excision of the
patella. The quadriceps force as a function of knee flexion angle was
recorded for varying amounts of excision and compared with the results
for total patellectomy.3 Excision of
the proximal one half or less resulted in lower force requirements when
compared with total patellectomy. The effects of distal to proximal
excisions indicate a biomechanical advantage to maintaining a fragment
equal to at least three fourths the length of the proximal patella3.
critical from 45 degrees of flexion to terminal extension. Twice as
much torque is required to extend the knee the final 15 degrees as is
necessary to bring it from a fully flexed position to 15 degrees.87
The patella displaces the tendon away from the center of rotation of
the knee, increasing the moment arm and providing a mechanical
advantage that increases the force of knee extension by as much 50%
depending on the angle of knee flexion.71
It is this displacement action of the patella that provides the
additional 60% of torque necessary to gain the last 15 degrees of
terminal extension.
result in substantial patellofemoral contact forces. Compressive forces
as large as three to seven times body weight have been
recorded during squatting or climbing stairs.29,97
Given the small contact area of the patellofemoral articulation, it has
been estimated that the contact stresses generated are greater than in
any other weight-bearing joint in the body.97
with varying degrees of knee flexion. The patella engages the trochlear
sulcus at approximately 20 degrees of flexion. With increasing knee
flexion, a horizontal band of contact area across the patellar facets
moves proximally and reaches a maximum at 90 degrees of flexion. Beyond
90 degrees, the contact area on the patella shifts into two discrete
locations on the medial and lateral facets. Corresponding with the
proximal shift of contact on the patella, the contact zone on the femur
shifts distally on the trochlea and separates into two discrete zones
on the medial and lateral condyles with hyperflexion.2,52
the fracture classification and findings on physical examination, with
particular attention on the integrity of the extensor mechanism. Age,
bone quality, patient expectation, and the presence of associated
injuries may also influence surgical decision making. Regardless of the
treatment strategy, the goals of surgical intervention are as follows:
-
Maximal preservation of the patella to maintain its linking and displacement functions
-
Restoration of the articular congruity of the patella
-
Preservation of the functional integrity and strength of the extensor mechanism
|
TABLE 52-2 Patella Fracture Treatment Options
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
-
Nonoperative management
-
Open reduction and internal fixation, most commonly with a tension band or modified tension band wiring construct
-
Partial patellectomy
-
Complete patellectomy
fractures with less than 3 mm of fragment displacement or less than 2
mm of articular incongruity in which the extensor mechanism remains
intact. Almost any fracture pattern (transverse, stellate, or vertical)
may be addressed with closed treatment if the above criteria are
satisfied. Relative indications for nonoperative management, sometimes
even in circumstances of greater fragment displacement, include medical
conditions that are contraindications to anesthesia or elderly,
debilitated patients with severe osteopenia that precludes the ability
to achieve rigid internal fixation. In a series of 18 patients with
significant medical comorbidities and displaced patella fractures,
Pritchett et al.118 reported
satisfactory outcomes in 12 patients at 2-year follow-up, with 9 of
these 12 patients without significant limitations in daily activities
of living. Furthermore, Klassen and Trousdale76
reported on a retrospective series of delayed union or nonunion of
patella fractures and found that minimally symptomatic nonunions could
be successfully managed conservatively.
6 weeks of extension splinting or bracing. If patient compliance and
reliability are a concern, however, long leg cylinder casting may be
preferable. Molding carefully about the knee and above the ankle will
help to prevent displacement of the cast as edema resolves. Range of
motion is gradually initiated after there is evidence of callus
formation and fracture consolidation on plain radiographs. Straight leg
raises and isometric quadriceps exercises
are
initiated early in the cast or brace to minimize atrophy.
Recommendations on weight bearing are variable, although most modern
protocols allow for some degree of early weight bearing in full
extension. DePalma144 recommended early partial weight bearing in extension, while Bohler and Bostrom22 both recommended weight bearing as tolerated with crutches for support.
has been reported with good clinical outcomes. In a large series of 422
patellar fractures reported by Bostrom et al.,22
219 minimally displaced fractures were treated nonoperatively, and 98%
had good to excellent results at final follow-up. Only two failures
occurred with nonoperative treatment. Other series have reported low
failure rates of less than 5% with closed management of minimally
displaced fractures.124,137
fractures with preserved articular congruity and an intact extensor
mechanism. In patients with a large traumatic hemarthrosis, we will
consider aspiration of the joint and inject local anesthetic to
facilitate physical examination.
brace locked in full extension. The brace is lightweight and allows for
patient hygiene and monitoring of any abrasions or associated soft
tissue injuries of the extremity. Furthermore, controlled range of
motion may be initiated once fracture callus is radiographically
confirmed. In noncompliant patients or elderly patients who are at
significant risk for falls, we prefer to use a fiberglass cylinder cast
from the groin to just above the ankle, molded about the knee and above
the ankle with the knee in full extension. Care must be taken,
particularly in elderly or diabetic patients, to pad carefully and
avoid iatrogenic soft tissue injury from a poorly molded cast. In
patients with lower extremity venous stasis ulcers or compromised
circulation, an Unna boot can be applied before cast molding to protect
the soft tissues.
are initiated 1 week after immobilization to minimize quadriceps
atrophy. Partial weight bearing with crutch assistance is allowed
immediately with advancement to full weight bearing in extension as
tolerated. Follow-up radiographs are obtained at regular intervals to
confirm that reduction has been maintained. If fracture displacement
occurs early, surgical stabilization should be considered. After
fracture consolidation is radiographically confirmed, controlled range
of motion of the knee is initiated.
are often stable due to the preserved integrity of the soft tissues. In
these cases, cast or brace immobilization is often unnecessary, and
early, controlled range of motion with activity modification is
initiated as tolerated.
with greater than 3 mm of fragment displacement, or greater than 2 mm
of articular incongruity, osteochondral fractures with associated
intra-articular loose bodies, and/or a compromised extensor mechanism
with loss of active extension. Internal fixation, partial or total
patellectomy, with repair of the extensor mechanism are all surgical
interventions performed with the goal of achieving stable fixation and
a functional extensor mechanism that allows for early range of motion
and rehabilitation.
fracture stabilization have been described in the literature. The first
description of cerclage wiring for patellar fracture fixation was made
by Berger in 1892.5 Anderson5 discussed the use of an equatorial circumferential wire placed around the patella, and Magnuson and Payr92,114
described successful fixation with intraosseous wires passed through
vertical drill holes. Screw fixation for longitudinal and transverse
fracture patterns with large fragments has also been described.40,105,156
The potential concern of these fixation strategies, however, has been
(a) an inability to initiate early motion due to the risk of
displacement with large tensile forces from quadriceps contraction and
(b) lack of compressive forces at the articular surface. The AO/ASIF
popularized the technique of tension band wire fixation for patellar
fractures to address these concerns, based on biomechanical studies
demonstrating increased construct strength with wires placed on the
anterior, tension-side cortical surface of the patella.106
Fixation. The principle of tension band wire fixation for patellar
fractures is to convert the tensile forces generated from the
quadriceps complex at the anterior cortical surface of the patella into
compressive forces at the articular surface. With progressive knee
flexion, the passive tensile forces in the extensor mechanism in
addition to the pressure of the femoral condyles against the patella
increase interfragmentary compression at the articular surface.
compared the strength of four different fixation strategies (tension
band wiring, modified tension band wiring over Kirschner wires
[K-wires], Lotke and Ecker longitudinal anterior banding, and
circumferential cerclage wiring) in a transverse patellar fracture and
retinacular disruption model. Cerclage wiring provided the weakest
fixation strength, with up to 20 mm of gapping at the fracture site
with tensile stress. The modified anterior tension band technique of
transosseous K-wire fixation with anterior banding demonstrated
superior strength to all other constructs.15
Isolated screw fixation with 3.5- or 4.5-mm screws may be sufficient,
particularly in the setting of simple transverse or longitudinal
fractures in patients with good bone stock. Burvant et al.,27
however, also found tension banding with screws to perform
biomechanically superiorly to five other techniques of transverse
patellar fracture fixation, including screw fixation alone. Carpenter
et al.30 compared a modified tension
band, parallel 4.5-mm interfragmentary lag screws, and 4.0-mm
cannulated lag screws augmented with a tension band passed through them
in a transverse patellar fracture cadaver model. The highest
load-to-failure was seen with the modified tension band and the
cannulated lag screw technique.30 Regardless of which tension
band construct was selected, Baran et al.13
used MRI in a knee cadaveric model to advocate for placement of the
tension band wire as close to the bone as possible with minimal
interposing tendinous tissue.
 |
|
FIGURE 52-9 Fracture patterns and examples of internal fixation.
|
compared anterior tension banding with 1.0-mm wire versus 1.0-mm
braided cable. The braided cable allowed for less fragment displacement
with cyclical loading. In addition, tightening of the wire by twisting
at two different sites compared with a single site has been shown to
provide greater interfragmentary compression.128 John et al.66 demonstrated improved stability with cyclic loading if wire twists were placed at the corners of the figure-of-eight loop.
associated with subcutaneous wiring, braided suture tension banding has
also been evaluated. McGreal et al.99
demonstrated that braided polyester suture was 75% as strong as wire
and performed equivalent to cerclage wire with cyclical loading.
Braided No. 5 Ethibond has also been shown to be comparable to wire
fixation with anterior tension banding or Lotke-Ecker anterior
longitudinal banding procedures for displaced, transverse
fractures.160 In a clinical study, Chen et al.33
demonstrated equivalent clinical outcomes with wire versus
biodegradable tension band fixation of patellar fractures at a mean of
2 years of follow-up.
surgical emergency and warrant immediate irrigation, débridement, and
stable fixation. The consequences of a surgical delay are not
insignificant and can include septic arthritis and patellar
osteomyelitis. A thorough débridement includes removal of all
devitalized fragments and soft tissue, followed by serial débridements,
skin grafting, and local or free tissue flaps if necessary for wound
closure. Appropriate antibiotic coverage is also essential.
reported on a series of 79 open patella fractures with a mean of
21-month follow-up. Almost all fractures were displaced, with 22%
transverse patterns and 39% comminuted, stellate injuries. The majority
(53%) were Gustilo and Anderson Grade II injuries. Surgical
intervention consisted of a thorough irrigation and débridement
followed by open reduction and internal fixation in 57% and partial
patellectomy in 32% of cases. Outcomes were satisfactory in most cases
with only one case of revision internal fixation for failure and no
cases of deep infection. The Mayo Clinic’s retrospective review of open
patellar fractures also reported 77% good to excellent results, with no
infections in type I or II open injuries that were treated with
immediate internal fixation after irrigation and débridement.148 Anand et al.4
recently presented the long-term outcomes of 16 open patellar fractures
and compared their results to those of a matched group of patients with
closed injuries. The Injury Severity Score (ISS) and the incidence of
associated musculoskeletal injuries were significantly higher in the
open patellar fracture group. At a mean of 45 months of follow-up,
patients with open patellar fractures had a higher incidence of
complications, lower Knee and Osteoarthritis Outcome Scores (KOOS), and
higher visual analog scores for pain.4
Technique. The patient is positioned supine on a radiolucent table. A
tourniquet is applied high on the thigh, with care being taken to avoid
entrapment of the quadriceps complex by inflating it only after the
knee has been gently flexed beyond 90 degrees. A longitudinal, midline
incision is typically performed and allows for excellent visualization,
protects the medial cutaneous branches of the femoral nerve, and can be
extended proximally and distally along the extensor mechanism if
necessary. In the case of an open fracture or a traumatic arthrotomy,
the laceration should be incorporated into the incision if possible.
Superficial dissection should be avoided regardless of incision
orientation to preserve the blood supply and the viability of skin
flaps. After exposure of the fracture lines, all clots and devitalized
debris should be cleared. Before any fixation, the degree of injury
should be carefully assessed. The articular surfaces of the femur and
patella should be inspected, and any intra-articular loose bodies
flushed out of the joint. In addition, the integrity of the medial and
lateral retinaculum as well as the proximal and distal soft tissue
attachments of the patella must be evaluated. The fracture pattern
should be generally defined. Complex fracture patterns with moderate
comminution may be simplified with the use of interfragmentary lag
screws to create a transverse pattern that is then amenable to tension
band fixation. With the knee slightly flexed, the fracture should be
reduced and maintained with a pointed reduction forceps. The quality of
the articular reduction should be palpated through the defect in the
retinaculum. Occasionally, extension of the arthrotomy or retinacular
tear may be necessary to allow palpation of the articular surface.
Gardner et al.50 has developed a
technique for exposure and fixation of comminuted patellar fractures
using a lateral arthrotomy and eversion of the patella. This allows
direct visualization, permits reduction of articular surfaces without
soft tissue interposition, and facilitates confirmation of articular
congruity, compared with more traditional techniques that rely on
palpation alone.50 Intraoperative fluoroscopy with imaging in multiple planes may also be used to confirm an anatomic reduction.
across the fracture line to maintain the reduction, compress the
fracture site, and anchor the tension band wire. The K-wires can be
placed in an antegrade or a retrograde fashion. Using the antegrade
technique, the wires are advanced from proximal to distal at a level 5
mm below the anterior cortical surface and parallel to it. The wires
are spaced apart to divide the patella longitudinally into thirds. When
using the retrograde technique, the reduction is taken down and the
proximal fracture fragment is flexed 90 degrees to expose the fracture
surface. Starting 5 mm below the anterior cortical surface and dividing
the patella longitudinally into the thirds, the K-wires are advanced
proximally through the fracture site, exiting at the locations of the
starting points for the antegrade technique. The reduction is then
re-established and held with a pointed reduction forceps. The K-wires
are subsequently advanced from proximal to distal across the fracture
site until they exit distally at the inferior patellar margin.
complete the construct. To facilitate wire passage, a large-bore
angiocatheter (14- or 16-gauge) can be passed through the quadriceps
tendon directly adjacent to the superior patellar margin, and an
18-gauge wire is then passed through the catheter, after which it is
removed. The limbs of the wire are crossed over the anterior cortex of
the patella and one limb is passed below the patellar tendon
immediately adjacent to its inferior margin as described earlier. After
anatomic reduction is confirmed with direct palpation and fluoroscopy,
the wire is tensioned with slow twisting of the wire limbs. Twisting is
performed at two locations (one in each wire limb), as tightening at
only the ends of the wire may lead to asymmetric fracture compression
and excess slack on the contralateral side. Care must taken to avoid
overtensioning of the wires, which can result in wire breakage and loss
of reduction or malreduction secondary to iatrogenic fragment
comminution. After satisfactory wire tension is achieved, the K-wires
are cut at both ends and bent backward 180 degrees over the tension
band wire both proximally and distally. They are gently impacted and
buried into the patella to prevent migration. The arthrotomy is
copiously irrigated, and the retinacular tears and arthrotomy are
closed in a water-tight fashion with interrupted, figure-of-eight
nonabsorbable sutures. The wound is closed in a standard, layered
fashion (Table 52-3).
This allows for lagged interfragmentary compression and has been shown
to be biomechanically stronger than the K-wire construct.30 In this technique, guide wires are placed in an identical fashion to
K-wires as just described, followed by drilling and cannulated lag
screws advancement across the fracture over the wires. Eighteen-gauge
wire is then passed in a figure-of-eight fashion through the cannulated
screws and tightened after anatomic reduction of the fracture has been
confirmed.16
|
TABLE 52-3 Surgical Tips and Pearls
|
||||||||
|---|---|---|---|---|---|---|---|---|
|
 |
|
FIGURE 52-10 Modified tension band wiring through cannulated screws. Lateral view (A) of injury. Anteroposterior (B) and lateral (C) views of internal fixation.
|
patterns may present with more than one major fracture line, dividing
the patella into more than two major fragments. In these situations,
minor fragments can be reduced and fixed together to simplify the
fracture pattern into one that is amenable to anterior tension band
wire fixation. Lag screws, K-wires, and bioabsorbable pins all may be
used to hold together smaller fragments. We have typically used 3.5-mm
interfragmentary lag screws in these situations, although screw
fixation without lag compression may be
preferable with moderate or severe comminution to avoid excessive
shortening and malreduction. If the fragment is comminuted at the point
of entry, a washer can be used to anchor the screw head.
Lotke-Ecker Technique. Stellate fracture patterns that are not amenable
to a modified anterior tension band technique may be treated with
longitudinal anterior banding plus cerclage wire
fixation (the Lotke-Ecker technique).89
The fracture is exposed and the fracture fragments carefully identified
after the clot and devitalized debris are removed. Minimally displaced
fractures are fixed in situ, while severely comminuted and displaced stellate fractures are reduced through indirect techniques.89
In these cases, a cerclage wire is first placed around the
circumference of the patella immediately adjacent to the bone with the
assistance of a 14- or 16-gauge angiocatheter. Gross manual reduction
is performed without clamps, followed by articular surface reduction
with progressive tightening of the cerclage wire.
drilling two parallel tunnels 1 cm from the medial and lateral edges of
the patella respectively with Steinmann pins or 2.0-mm drill bits in an
antegrade fashion.89 A large-gauge
wire (18- to 22-gauge) is then inserted into both drill holes,
preserving a closed loop distally. The distal loop is brought
anteriorly and one free proximal end of the wire is passed through this
anterior loop. The wire is then secured to its other end and tightened
with progressive twisting. This fixation results in a hybrid of
anterior tension banding and interosseous wire fixation.89
The use of arthroscopy to assist with patellar fracture reduction and
fixation has been described. Appel and Siegel7
presented a limited series of cases with arthroscopic-assisted
reduction followed by percutaneous screw and wire fixation with
satisfactory outcomes. Theoretical advantages include direct
visualization of the articular surface during internal fixation,
limited dissection and soft tissue stripping, and the ability to
address associated intra-articular pathology in the knee including
osteochondral fractures. While this technique may have a role in
selected cases, we do not believe that it supplants open techniques,
which allow for anatomic fracture reduction, rigid fixation, and
retinacular and extensor mechanism.
|
TABLE 52-4 Outcomes after Internal Fixation of Patella Fractures
|
||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
recently presented a randomized series of 53 patients treated with
percutaneous patellar osteosynthesis (PPOS) versus standard open
reduction and internal fixation for closed, displaced transverse
patellar fractures. In the PPOS group, a special device was secured via
four percutaneous portals to maintain the reduction while an anterior
tension band was placed. In the group of patients treated with PPOS,
the authors reported shorter surgical times, less pain, less
complications, and improved functional outcome scores by Knee Society
Clinical Rating Scale (KSCRS) at 1-year follow-up. Clinical outcome
scores were not statistically different between the two groups by
2-year follow-up.116
standardized assessment scale limits the utility of reported outcomes
after operative fixation of patellar fractures. As a result, the
literature provides generalizations about “good” or “excellent”
outcomes based on subjective patient complaints of pain, loss or
motion, or limitations in daily activities. Based on the combined
results of many small series, open reduction and internal fixation has
produced a good to excellent result in 73% of 361 fractures (Table 52-4).
need to be interpreted with some caution, however, because series are
more often reported by repair construct rather than by fracture
pattern. A compilation of published series is shown in Table 52-4. Modified anterior tension band wiring has produced the best results, with 86% good to excellent outcomes reported.9 Bostman et al.21
reported significantly better results with anterior tension banding
compared with cerclage wiring, partial patellectomy, or
interfragmentary screw fixation. While small series have reported
excellent outcomes with cerclage wiring, a review of the combined
results reveals inferior performance to tension band wire fixation,
with only 70% good to excellent results. The anterior longitudinal
banding technique of Lotke and Ecker
can also be effective, with 81% excellent results reported in their small series.89
fractures because the fracture lines and comminution are not always
clearly visualized using standard imaging. It is imperative to have all
of the necessary equipment available in the operating room to perform
either internal fixation or a partial patellectomy. At minimum, a small
fragment implant set with 3.5-mm cortical screws for interfragmentary
fixation, 1.6- and 2.0-mm Kirschner wires, 18-gauge wire, and 14-or
16-gauge angiocatheters for wire passage are needed. A 4.0-mm
cannulated screw set can be made available as well to fix transverse
fracture patterns. Small- and medium-size pointed reduction forceps are
helpful for maintaining a provisional reduction. A power drill with
wire driver attachment and wire twisters should be available. If
significant distal pole comminution is encountered, a partial
patellectomy may be necessary. A Hewson suture passer may be helpful
for passing suture through bone tunnels if a partial patellectomy is
performed.
débridement of the fracture is performed followed by rigid internal
fixation for Grade I and II open injuries without gross contamination.
Appropriate antibiotic coverage is selected, and serial débridements
and/or soft tissue coverage are performed based on the contamination of
the wound and status of the soft tissues. If there is a question of an
open fracture or traumatic arthrotomy, a saline load test should be
performed in the emergency department. For closed fractures, the status
of the skin and soft tissues helps guide the timing of operative
intervention. Typically, we will wait 1 to 2 weeks in the setting of
significant soft tissue swelling or superficial abrasions to minimize
the risk of postoperative wound complications.
radiolucent table. Intraoperative fluoroscopy is used to obtain true AP
and lateral images. A high thigh tourniquet is applied, and the knee is
flexed to 90 degrees before inflation to avoid entrapment of the
quadriceps and facilitate reduction of the proximal fragment. The
fracture is approached through a longitudinal midline incision with
full-thickness skin flaps and minimal superficial dissection. This
extensile approach provides excellent exposure of the fracture as well
as the medial and lateral retinacular tears.
of clot and devitalized debris. In the setting of transverse fracture
patterns, we prefer a modified anterior tension band wiring and
cannulated screw construct (Fig. 52-10). With
more complex fractures in which the larger fragments have additional
fracture lines, we attempt to simplify the fracture into a transverse
pattern by securing the smaller fragments together with
interfragmentary screws or K-wires. Screws of various sizes may be
necessary based on fragment size and bone quality.
the assistance of a pointed reduction forceps and manual manipulation.
The reduction is assessed by both direct palpation of the articular
surface through the retinacular tear and multiplanar fluoroscopy. If
the retinacular tissues are intact, we create a small arthrotomy in the
medial retinaculum to allow direct palpation of the articular surface.
Guide wires for cannulated screws are placed in a retrograde fashion
via the fracture line into the proximal pole. We prefer this technique
to ensure a depth of 5 mm inferior to the anterior cortical surface.
After drilling, the parallel screws are placed over the guide wires,
conferring compression and rotational stability to the construct. The
18-gauge wire is then passed in a figure-of-eight fashion through the
cannulated screws and the free limbs twisted to achieve appropriate
tension. The ends are then cut and bent backward into the patellar bone
to minimize subcutaneous irritation from the wire.
in which anterior tension banding is not feasible, we will use indirect
reduction with cerclage wiring followed by the longitudinal anterior
banding technique of Lotke and Ecker.89
With severe inferior pole comminution that is not salvageable, we
perform a partial patellectomy while attempting to preserve as much of
the remaining patella as possible. Two locking Krackow sutures are run
in the patellar tendon, resulting in four core strands that are passed
through three tunnels in the residual patella. The drill holes are
placed at the articular margin to avoid iatrogenic patellar tilt. A
burr or rongeur is used to make a small trough at the inferior margin
of the patella to allow tendon apposition against bleeding, cancellous
bone. We typically protect the partial patellectomy with an 18-gauge
cerclage wire passed superior to the patella and through the proximal
tibia.
patella is extensive and cannot be stabilized with internal fixation, a
partial patellectomy should be performed. The surgical approach is the
same as for open reduction and consists of a longitudinal midline
exposure. Care is taken to preserve as many large, viable fragments as
possible. Retained fragments are anatomically reduced and secured to
one another with screws or K-wires. If the comminution primarily
involves the central patella with preserved proximal and distal
fragments, the central comminution can be excised and the remaining
fragments secured as congruously as possible with screw fixation.
fragments with patellar tendon reattachment can be performed. Most of
these fractures are extra-articular, as the distal pole is devoid of
articular cartilage. Three longitudinal drill holes are then placed
through the remaining patella to serve as tunnels for suture passage. A
tendon-grasping, woven or locking nonabsorbable suture (such as a
Krackow suture) is placed in the patellar tendon, and the sutures are
passed with a ligature passer through the tunnels and firmly tied over
bone bridges with the knee in hyperextension. Tantamount to the tendon repair, however, is a meticulous repair of the associated medial and lateral retinacular injury.15
Based on the energy of the injury and strength of the repair, the
construct may be protected with a cerclage wire, a tendon graft, or a
Mersilene tape that is passed immediately proximal to the superior pole
of the patella and inferiorly through the proximal tibia posterior to
the tibial tubercle.
The
cerclage should be tightened with the knee flexed to 90 degrees, as
tightening in extension may constrain the postoperative flexion that is
achievable by the patient. The strength of the repair should always be
evaluated intraoperatively, observing for interfragmentary motion and
the integrity of the tendon-bone interface with progressive knee
flexion. Rigid constructs may allow for early, controlled motion of the
knee. Typically, extension bracing for ambulation and partial weight
bearing with crutch assistance is maintained for 6 weeks
postoperatively.
after partial patellectomy is important and has been debated in the
literature. Studies have suggested that the holes be placed near the
articular surface to avoid abnormal tilting of the patella and creating
increased patellofemoral contact forces.43 In 1958, Duthie and Hutchinson43
reported tilting of the patella in five of seven patients with
postoperative arthritis and attributed these changes to malalignment
from attachment of the patellar tendon to the anterior cortex. In
contrast, Marder et al.94 completed
contact pressure studies demonstrating improved mechanics with anterior
tendon reattachment for 20% and 40% partial patellectomy models.
Furthermore, Zhao et al.163 reported
an increase in the force required to extend the knee with tendon
attachment to the articular surface compared with the anterior cortex.
have been managed with partial patellectomy with satisfactory outcomes.
Recently, a technique for osteosynthesis of these fractures using a
novel basket plate device has been described.70,78,96,150
The basket plate is contoured to fit the geometry of the patellar apex
and is augmented with several anterior and posterior flanges to collect
the comminuted fragments. Fibers of the proximal patellar tendon are
spread apart by the flanges to allow positioning it at the inferior
pole without detachment. Four holes are provided to place parallel and
oblique screws that engage the opposite fragment and resist both
tensile and shear forces.78,96
Biomechanical studies have demonstrated an ultimate load-to-failure of
about 420 N for this construct, approximately 70% higher than a
separate vertical wiring fixation construct.78,161
reported 90% good to excellent outcomes at a mean 5-year follow-up for
51 patients who underwent basket plate osteosynthesis of comminuted
distal pole fractures. These data must be approached with caution,
however, as 61% of the study patients were lost to follow-up.96 A retrospective cohort study by Kastelec et al.70
compared 11 patients who had internal fixation of a distal pole
avulsion fracture to 13 patients who had a pole resection. At an
average follow-up of 4.6 years, average patellofemoral scores were
significantly better in the osteosynthesis group compared with the
resection group.70 Furthermore,
there was a significantly greater incidence of patella baja in the pole
resection group as assessed radiographically by the method of
Blackburne and Peel.70 Sample sizes
were small, however, and randomized control trials are necessary to
further define potential advantages of osteosynthesis compared with
resection in the surgical management of comminuted distal pole
fractures.
|
TABLE 52-5 Outcomes after Partial Patellectomy
|
||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
partial patellectomy can yield functional outcomes that are equivalent
to open reduction and internal fixation21,22,104,111,126,134 (Table 52-5).
Multiple authors have reported nearly normal functional outcome when
large fragments of the patella and articular congruity are preserved.
Retention of small, nonviable fracture fragments or those devoid of
cartilage did not improve function, while retention of large fragments
provided a lever arm for improved extensor mechanism function. Combined
results in 138 cases have shown a good to excellent outcomes in 72% of
cases. With extensive inferior pole comminution, superior results have
been reported with partial patellectomy compared with internal fixation.22 Bostrom et al.22
reported 88% good to excellent results with partial patellectomy for
transverse patellar fractures with inferior pole comminution, compared
with only 74% good to excellent results with internal fixation.
displaced, comminuted fractures in which stable fixation cannot be
achieved and when no large fragments can be retained. We have reserved
this as a salvage procedure in the rare setting of failed internal
fixation or patellar osteomyeltis. Retention of even a single fragment
is usually possible, and can substantially help to preserve the
biomechanical function of the extensor mechanism.3
are removed, with care being taken to preserve the retinacula and
restore the integrity of the extensor mechanism. Typically, an anterior
longitudinal incision is used, although a prior incision that will
preserve viability of skin flaps may be chosen in a revision setting.
Removal of the patella effectively lengthens the extensor mechanism,
such that end-to-end repair will result in an increased slack distance
and extension lag after surgery. This is avoided by imbrication or use
of a purse-string suturing technique that shortens the tendinous
repair. Tension should be evident on the repair at 90 degrees of
flexion when length has been adequately restored.
of soft tissue available for primary repair of the extensor mechanism.
In general, the absence of prepatellar soft tissues is addressed with
quadriceps turndown procedures. Absence of the quadriceps tendon,
however, usually requires fascia or tendon weaving procedures.
described the inverted V-plasty quadriceps turndown procedure. The
quadriceps tendon is exposed for approximately three inches, and a
full-thickness, V-shaped incision is made into the tendon with the apex
of the “V” located 2½ inches proximal to the former superior pole of
the patella. The V-limbs extend distally for 2 inches, creating a base
that preserves approximately ½ inch of tendon that is continuous with
the retinaculum on both the medial and lateral sides. The V-flap is
folded inferiorly, inserting it through the proximal patellar tendon
and suturing it in place with several interrupted sutures. The
quadriceps tendon defect is then closed in a side-to-side fashion with
multiple interrupted sutures.
have described a free fascia or tendon weave procedure. After nonviable
tendon remnants have been débrided, the length of the defect is
measured with the knee in full extension. This length is doubled and 2
inches added to harvest to the appropriate-size fascial graft. Through
a separate lateral incision, a 1½-cm-wide graft of fascia lata or
iliotibial band of appropriate length is harvested and tubularized
along its long axis. Alternatively, allograft tissue of appropriate
length can be used. The graft is then woven through the quadriceps
tendon and/or muscle, passed through the patellar tendon, and sewn back
onto itself. Tension should be evident on the repair at 90 degrees of
flexion when length has been adequately restored. Excess tissue is
excised and all edges firmly sutured down.
|
TABLE 52-6 Outcomes after Total Patellectomy
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
generally inferior to those reported after internal fixation or partial
patellectomy for fracture. However, these results are difficult to
interpret as fractures treated with total patellectomy likely reflect
higher energy, comminuted injuries. The combined results of 219 cases
showed 72% good to excellent results.
techniques, poor methods of achieving rigid internal fixation may have
justified total patellectomy in these early series. Recent studies,
however, have reported a higher rate of fair to poor outcomes with
total patellectomy (Table 52-6). Bostrom20 recommended total patellectomy only in the setting of severely comminuted fractures. Sutton and colleagues143
evaluated quadriceps strength and functional abilities in patients who
had undergone partial or complete patellectomy, with the contralateral
normal knee serving as a control. Total excision was associated with a
49% reduction in strength of the extensor mechanism and a mean loss of
18 degrees in range of motion. Functionally, there was a high incidence
of instability, with an inability of the patients to support their
weight on the loaded knee with stair climbing.143 Einola et al.45 reported on 28 patients with a mean 7½ years
of follow-up and reported a good result in only 6 patients. Quadriceps
power was within 75% of the contralateral knee in only 7 patients.
Scott et al.130
similarly reported a good outcome in only 4 of 71 patients, with 90%
complaining of chronic pain. Quadriceps atrophy, pain, and instability
in the knee during running or stair climbing were common complaints of
patients in both series. Wilkinson et al.159
evaluated 31 patients with up to 13 years of follow-up and reported an
excellent outcome in less than 25% of patients. Furthermore, Sorensen
et al.140 noted that no patients
regained full quadriceps strength after patellectomy and that none of
their operative reconstructions would have fared better with primary
excision. For these reasons, it is our recommendation to avoid total
patellectomy whenever possible. We have not encountered a patella so
comminuted that a single fragment could not be preserved acutely.
Maintaining even a single fragment provides a lever arm that
substantially improves the function of the extensor mechanism.71
operate acutely compared with a delayed fashion remains controversial.
Muller et al.107 retrospectively
reviewed their results of early (within 4 weeks) versus delayed
patellectomy and identified no differences in range of motion or
clinical outcome scores between the groups.
result of trauma without signs of a patellar fracture may have a
disruption of the extensor mechanism. Injuries to the extensor
mechanism can include quadriceps or patellar tendon ruptures, patellar
dislocations, or tibial tubercle avulsions. Demographic data suggest a
difference in the occurrence of quadriceps and patellar tendon ruptures
based on age.137 Patellar tendon
ruptures occur more commonly in patients younger than 40 years while
quadriceps tendon ruptures occur more commonly in patients older than
40 years.
including pain, atrophy, and tenderness around the distal or proximal
patellar pole and/or a history of Osgood-Schlatter disease or jumper’s
knee.73 Quadriceps tendon ruptures may occur more commonly in patients with systemic disease or degenerative changes.8,153
Numerous reports of simultaneous bilateral quadriceps tendon rupture
have been published and include patients with systemic illness and
obesity.75,91,117,138,142 Bilateral rupture of the patellar tendon can occur but is less frequent.53,67,123,155
Operative findings may suggest that the tendon was weakened or prone to
disruption from metabolic abnormalities, collagen disease, repetitive
microtrauma, or local steroid injections.69
in diagnosing a patellar or quadriceps tendon rupture. The patient has
usually sustained a forceful quadriceps contraction against a fixed or
sudden load of full body weight with the knee in a flexed position.
Pain with an associated tearing or popping sensation is typical, as is
the inability to bear weight. The key to diagnosing an extensor
mechanism rupture is the lack of active knee extension or the inability
to maintain the passively extended knee against gravity. Most commonly,
patellar tendon ruptures extend completely through the retinacular
tissue resulting in complete loss of knee extension. Quadriceps tendon
ruptures may not involve as much of the retinacular tissue, and as a
result some extension still may be possible. Typically some degree of
extensor lag is almost always present when compared with the uninjured
limb. Immediately after injury, a defect may be palpable at the level
of the rupture. However when the diagnosis is delayed the tendon defect
may not be palpable secondary to consolidation of the hematoma and
early scar formation.
mechanism injuries. Ice, compression, elevation, and anti-inflammatory
medications can be used to treat local symptoms. Although no studies
have shown a benefit for knee aspiration in these injuries, aspiration
of a tense hematoma may be considered to reduce pain and promote
recovery.
extensor mechanism injury is found in the translated writing of the
Greek physician Galen ca. 80 to 87 AD.48 In 1887, McBurney98
published the first case in the American literature. Conservative
treatment prevailed until the end of the nineteenth century, when Quenu
and Duval119 published a review of 26 cases treated surgically and recommended operative repair. In 1927, Gallie and LeMesurier49
described a technique using a fascia lata strip to repair a quadriceps
tendon rupture. Following these reports, surgical management became
increasingly accepted and numerous surgeons have subsequently published
their techniques and results.
conditions, tensile overload of the extensor mechanism usually leads to
fracture of the patella which is considered the weakest link in the
extensor mechanism.155 McMaster101
studied the tensile strength and location of tendon ruptures in a
rabbit model. Between 50% and 75% of the tendon fibers had to be
transected to result in a rupture under forces greater than those seen
under physiologic conditions. Patellar tendon ruptures secondary to
indirect trauma have been considered the end stage of long standing
chronic tendon degeneration secondary to repetitive microtrauma. Biopsy
specimens of spontaneously ruptured tendons reveal pathologic findings
that are degenerative in nature, including hypoxic tendinopathy, mucoid
degeneration, tendolipomatosis, and calcifying tendinopathy.69 A history of prodromal symptoms may be associated with tendon failure. Kelly73
reviewed 13 athletes with chronic jumper’s knee that resulted in tendon
rupture. In this series, younger patients had more severe symptoms than
older patients, leading Kelly to conclude that more advanced
degeneration is required to weaken younger, healthier tendons.
all patients with suspected injury to the knee extensor mechanism.
Plain radiographs are the most cost-effective radiographic means to
diagnose a patellar tendon rupture. The unopposed pull of the
quadriceps muscle will result in proximal migration of the patella.
Patella alta, defined as the position of the patella superior to the
Blumensaat line on the lateral radiograph, is consistent with rupture
of the patellar tendon. Additionally, if bone fragments are identified,
an avulsion injury may be suspected.74 Radiographic findings suggestive of a quadriceps tendon rupture
include obliteration of the quadriceps tendon shadow, a suprapatellar
mass, suprapatellar calcific densities, and an inferiorly displaced
patella. A study of 18 patients with known quadriceps tendon ruptures
identified at least three of these abnormalities in 17 of the 18
patients.68
an effective method of examining the patellar and quadriceps tendons in
both acute and chronic injuries.17,38 Raatikeinen120
reported on the successful use of ultrasound in diagnosing partial
quadriceps tendon ruptures. MRI is also an effective, albeit expensive,
method of diagnosing extensor mechanism injuries.80,162
It is not recommended in the evaluation of most suspected extensor
mechanism injuries but may be helpful in patients with neglected tears
or partial tendon injuries.
without surgical intervention if full active extension is present on
physical examination. The limb is initially immobilized with the knee
in full extension for 4 to 6 weeks, after which protected range of
motion and strengthening are begun. Initially, flexion of greater than
90 degrees is avoided to reduce stress on the tendon. Restrictions are
removed once the patient achieves good quadriceps muscle control and is
able to perform a straight leg raise without discomfort.
conjunction with a palpable defect above the superior pole of the
patella on physical examination confirms the diagnosis of a complete
quadriceps tendon tear. Nonsurgical management of a complete quadriceps
tendon rupture yields poor results with long-term disability in gait
and weakness.49,132
Untreated complete ruptures will result in ambulation with a stiff knee
gait or circumduction to allow the foot to clear the ground during the
swing phase of gait. Patients will also complain of knee buckling and
difficulty in climbing stairs. Surgical repair is the preferred
treatment for complete ruptures and is believed to result in the best
functional results. Many different repair techniques have been
described, with no single technique demonstrating superiority.85,100,132,137
of the patella can be treated by débridement of the tendon, followed by
the passage of three heavy nonabsorbable sutures into the tendon. Three
parallel drill holes are then created from superior to inferior through
the patella. The sutures are passed through the drill holes and tied at
the inferior patella, and the retinacular tissue is repaired (Fig. 52-11).
After repair, the limb is placed into a knee brace for 48 hours. The
patient is allowed to bear weight as tolerated with a hinged brace or
long leg cast with the knee held in extension. Range of motion and
strengthening exercises are gradually started after 4 to 6 weeks of
immobilization. The brace or cast is removed when the patient has good
quadriceps control and can perform a straight leg raise. Good range of
motion can be expected by 12 to 16 weeks postoperatively.
approximation of the tendon rupture. If the repair is tenous, the
Scuderi technique or quadriceps turndown flap has been described as a
method to reinforce the surgical repair.132
A partial-thickness triangular flap is developed from the anterior
surface of the proximal tendon that is 2 inches along the base and 3
inches along each side. The flap is folded distally over the
rupture/repair and sutured into place (Fig. 52-11D).
Immobilization in a long leg cast for 6 weeks is recommended to protect
a midsubstance repair. Several authors have suggested techniques for
reinforcing the repair using wire or Dacron tape.81,137,142 However, most repairs for tendon avulsions are sufficiently strong that secondary stress-relieving devices are not required.
wound. A knee immobilizer is applied initially and transitioned to a
locked hinged knee brace and the patient is allowed to bear weight as
tolerated. For the first 2 weeks, the leg is maintained in extension.
After the wound has healed, knee range of motion is permitted from 0 to
40 degrees and increased at biweekly intervals by 20 to 30 degrees with
the goal of obtaining 90 degrees of flexion by 6 to 8 weeks. The
patient is instructed in active assisted and passive range-of-motion
exercises during this time period. Active range of motion and
strengthening are begun 6 to 8 weeks postoperatively. The brace is used
until the patient has good quadriceps control and is able to perform a
straight leg raise.
knee from the inferior patella to 5 cm proximal to the quadriceps
tendon rupture. Full-thickness flaps are elevated medially and
laterally to identify the apex of the retinacular tears, if present.
The joint is irrigated to remove hematoma, allow identification and
assessment of the tear, and examination of the patellar and distal
femoral articular surfaces. The edges of the quadriceps tendon are
sharply débrided of grossly degenerated tissue, providing a fresh
surface to approximate to the patella. Absorbable sutures are placed
into the medial and lateral retinacular tissues but left untied until
after the tendon repair has been completed. Two heavy nonabsorbable
sutures (No. 5 Ticron or Fiberwire) are placed using a running Kessler
suture, leaving four strands of suture at the distal quadriceps stump.
A trough is created in the superior patella using a small burr or
rongeur.
along the longitudinal axis of the patella from superior to inferior. A
Hewson suture passer is passed from the proximal patella through the
drill hole. A No. 2 nylon suture is looped and placed into the suture
passer, which is then pulled out proximally. The nylon suture is used
as a shuttle or relay to pass the tendon sutures through the bone
tunnels. The two central sutures are passed through the middle drill
hole and retrieved at the inferior margin of the patella. The two
remaining sutures are passed in a similar fashion through each of the
peripheral drill holes and retrieved distally. Each of the central
strands is passed under the patellar tendon and retrieved with its
match so that the knots when tied will lie against the patella and not
on top of the tendon. The sutures are tied with the knee in full
extension. A drain is placed in the joint at this time as the joint can
still be accessed through the retinacular defect. The retinacular
sutures are then tied.
If
used, the tourniquet is deflated. Hemostasis is obtained. The hip is
flexed and the knee is allowed to bend passively into flexion. A range
of motion from 0 to 90 degrees is ideal. Patellar tracking and tension
on the repair are also assessed. The repair is reinforced with 0
nonabsorbable sutures. The wound is closed with absorbable suture and
the skin with nylon suture.
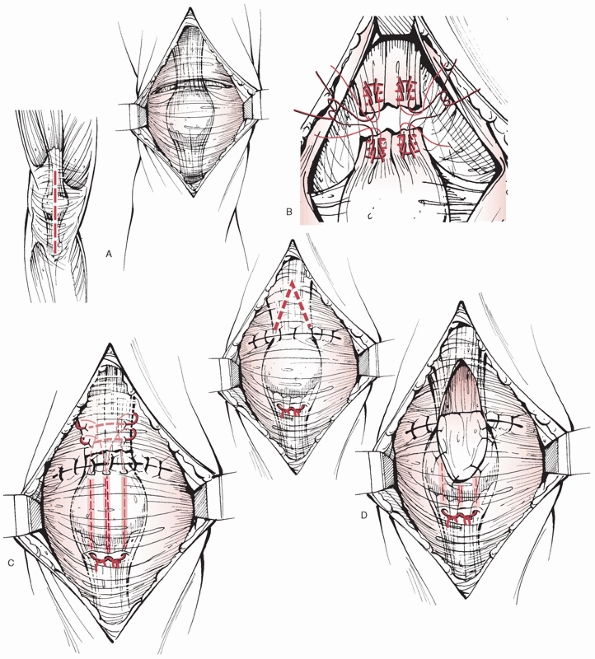 |
|
FIGURE 52-11 Acute quadriceps tendon repair. A. Approach is through a midline longitudinal incision. B. Acute repair using a Krackow suture technique. C. Repair through three parallel drill holes in the patella. D. Scuderi technique with a turndown flap reinforcement.
|
Many different techniques of primary repair have been described, and no
single technique has demonstrated superiority. In early series, primary
end-to-end repair was performed with cast immobilization, while in more
recent series, heavy nonabsorbable sutures have been passed through
bone
tunnels
and early rehabilitation undertaken. The only factor that has been
associated with inferior results is delay in timing of surgical repair
of greater than 2 to 3 weeks.125,137 Scuderi132 reported good to excellent results in 85% patients treated using the turndown flap. Siwek and Rao137
evaluated 36 ruptures and found that the 30 patients who underwent
early treatment obtained good to excellent results, while the 3
patients treated after 4 weeks had unsatisfactory results. Larsen and
Lund81 reported good to excellent
results in 15 of 18 patients. This study attempted to correlate
radiographic patellofemoral congruence with clinical outcome. Thirteen
of the 18 patients demonstrated incongruence compared with the
contralateral knee. All patients with residual pain had patellofemoral
incongruence. However, it is unclear what this finding means because 9
of the 13 patients with patellofemoral incongruence were asymptomatic.
They concluded that patellar congruence was not the only factor
contributing to persistent pain after repair. Rougraff125
reviewed 53 ruptures treated with multiple surgical techniques and
postoperative regimens and found no differences based on repair
technique or postoperative protocol. Patients with delayed surgery had
poorer functional outcome and decreased satisfaction scores. Konrath77
reviewed 51 quadriceps tendon ruptures in 39 patients treated with
heavy nonabsorbable suture placed through bone tunnels using functional
surveys and objective testing. Ninety-two percent were satisfied and
84% returned to previous occupations. However, 51% were unable to
return to their presurgery level of recreational activity. Objective
testing demonstrated a 12% strength loss in the quadriceps muscle and
14% strength loss in the hamstrings as well as an 8-degree loss of
range of motion.
|
TABLE 52-7 Outcomes after Acute Quadriceps Tendon Repair
|
|||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
significant treatment challenges. When the tendon end can be
approximated to the patella, a primary repair can be performed.
However, a large defect may be present between the end of tendon and
the patella, preventing tendon apposition. Patients with a quadriceps
tendon rupture older than 2 weeks may have muscle retraction of up to 5
cm.86 If the tendon has retracted
proximally resulting in a gap, the quadriceps muscle can be elevated
from the femur and adhesions released in an attempt to gain length. If
the tendon ends still cannot be opposed, a Codivilla lengthening
procedure should be considered.131 A
full-thickness inverted V is created in the proximal segment of the
quadriceps tendon. The lower margin of the V should be 1.3 to 2.0 cm
proximal to the site of the rupture. The ends of the ruptured tendon
are approximated and repaired with heavy nonabsorbable suture. The
triangular flap is turned down distally and sutured into place. The
open upper portion of the V is repaired in a side to side fashion.
Scuderi132 described a variation of
this technique for late reconstruction. After the tendon is exposed, a
Codivilla or Bennett lengthening is performed. An inverted V-cut is
made through the tendon proximal to the rupture. The triangular flap is
then divided into two flaps. One-half-thickness flap is incorporated
into the Y-plasty and the other is folded distally to reinforce the
tendon repair. Scuderi and Schrey131 reported good to excellent results in 7 of 9 patients treated with this technique. Oni113
described the medial transposition of a 2- to 5-cm strip of vastus
lateralis to bridge a large defect in five chronic quadriceps tendon
ruptures. Ramsey and Muller121
reported that four of seven delayed repairs lost between 10 and 20
degrees of full active extension at final follow-up. Overall, the
reported results for chronic quadriceps tendon repairs are less
satisfactory than those reported after repair of an acute tear with
residual functional deficits present in most patients.105,125,132
The majority occur as unilateral injuries during athletic
participation. The injury is commonly seen in the setting of
recreational athletics, and the patient will describe a pop or tearing
sensation after a sudden eccentric contraction resulting in immediate
pain and the inability to bear weight. Patellar tendon injuries are
often associated with cumulative microtrauma and patients may report
prodromal symptoms and a history of jumper’s knee.73
ineffective and results in significant functional deficits. Incomplete
tears with a functionally intact extensor mechanism can be treated with
cast immobilization with the knee in extension for 4 to 6 weeks.
Surgical repair of the extensor mechanism is indicated in nearly all
cases of complete patellar tendon rupture to allow for optimal return
to function. The site of the tear (proximal, midsubstance, or distal)
will dictate the preferred surgical repair technique. Most patellar
tendon ruptures occur at the insertion on the inferior pole of the
patella as an avulsion. This is believed
to
be the result of a relative decrease in the collagen fiber stiffness at
the insertion site and the greater tensile strain occurring at the
inferior pole fibers than the midtendon.69
of the patella can be treated by débridement of the tendon, followed by
the passage of three heavy nonabsorbable sutures into the tendon. Three
parallel drill holes are then created from inferior to superior in the
patella. The sutures are passed through the drill holes and tied at the
superior pole of the patella. The medial and lateral retinacular tears
are identified and repaired. A cerclage or reinforcement suture or wire
is recommended for most cases (Figs. 52-12 and 52-13).
A transverse drill hole is made 1 cm posterior to the tibial tubercle.
A heavy nonabsorbable suture, umbilical tape, or wire is passed through
the hole, brought proximally, and passed under the quadriceps tendon
close to the superior border of the patella and tied to itself. The
knee is flexed to 90 degrees to test the integrity of the repair. The
patellar tendon suture line is reinforced with absorbable sutures the
wound is closed in layers, and a well padded dressing is applied. A
hinged knee brace is applied with the knee in full extension.
the quality of tissue may be compromised and caution should be observed
to prevent shortening of the tendon and creating patella baja with
placement of the sutures. The most common method of repair involves
simple end-to-end repair, with or without a reinforcing cerclage suture
of wire or nonabsorbable suture material or tape. A distal patellar
tendon rupture from the tibial tubercle is the least common pattern. A
suture repair through bone tunnels with semitendosus and gracilis
augmentation as described for late reconstruction is recommended.44
surgeon’s assessment of the repair strength. A repair with poorquality
tissue should be immobilized for 4 to 6 weeks in a cylinder cast with
weight bearing as tolerated restrictions. A sturdy repair with
reinforcement can be started on early range of motion within 7 to 10
days postoperatively with active and active assisted exercises.
Initially full flexion is not allowed, but range of motion is started
at 0 to 45 degrees and advancing 30 degrees every 2 weeks. Active knee
extension is permitted at 6 weeks. The rehabilitation program should
stress closed chain eccentric strengthening to avoid possible reinjury.
Weight bearing is allowed immediately and crutches are used for at
least 6 weeks. The hinged knee brace and crutches are discontinued when
the patient is able to ambulate with good quadriceps control.
Competitive sports should not be allowed for 4 to 6 months until the
majority of isokinetic strength has been regained.
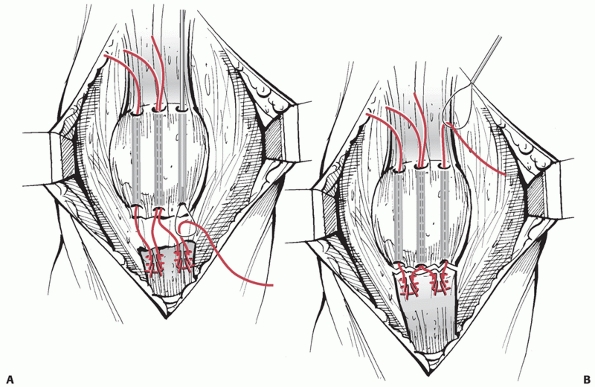 |
|
FIGURE 52-12 Suture technique of patellar tendon repair. A. A suture passer is used to guide the core sutures through the drill holes. B. The suture is retrieved and tied at the superior margin of the patella.
|
to the tibial tubercle. Full-thickness skin flaps are created to expose
the ruptured tendon and retinacular tissue. The edges of the patellar
tendon are sharply débrided of grossly degenerated tissue, providing a
fresh surface to approximate to the patella. If there are small loose
bone fragments, they can be excised. The extent of the medial and
lateral retinacular tears must be identified. These tissues are
sutured, but not tied, with No. 1 nonabsorbable suture (Ethibond). Two
No. 5 nonabsorbable sutures (Ticron, Fiberwire) are woven in a running
Bunnell stitch, resulting in one medial and one lateral suture strand
and two central strands. A trough is created in the inferior patella
with a small burr or rongeur to obtain a fresh cancellous bed to allow
tendon to bone healing.
along the longitudinal axis of the patella from inferior to superior. A
Hewson suture passer is passed from the distal patella through the
drill hole. A No. 2 nylon suture is looped and placed into the suture
passer, which is then pulled out distally. This technique shuttles the
nylon suture through the hole so that the core tendon sutures can be
passed easily and retrieved proximal to the patella. The two central
sutures are passed through the middle drill hole and retrieved at the
superior margin of the patella. The two peripheral sutures are each
passed through a drill hole in a similar manner. Each of the central
strands is then passed under the quadriceps tendon so that the knots
when tied will lie close to the patella and not on top of the
quadriceps tendon. Tension is applied to the sutures, which are clamped
but not tied. A lateral radiograph is obtained to assess the patellar
height in relation to the Blumensaat line and in comparison to the
contralateral knee. Suture tension can be increased or decreased to
control the patellar tendon length. The sutures are then tied. A drain
is placed deep and the retinacular tissue sutures are tied.
Reinforcement is often necessary with a patellar tendon repair to
counteract the force of the quadriceps muscle contraction. A transverse
2.5-mm drill hole is made 1 cm posterior to the tibial tubercle. An
18-gauge wire is passed through the hole, brought proximally, and
passed under the quadriceps tendon close to the superior border of the
patella and twisted until it is tight. The reinforcement wire is
tightened with the knee in some flexion to avoid shortening the tendon.
The knee is flexed to 90 degrees to test the integrity of the repair.
The patellar tendon suture line is then reinforced with absorbable
sutures. The wound is closed in layers and a well-padded dressing is
applied. A hinged knee brace is applied with the knee in full
extension. Active flexion and passive extension are begun by 2 weeks
postoperatively starting at 0 to 45 degrees and advancing 20 to 30
degrees every 2 weeks. Active knee extension is permitted at 6 weeks.
Weight bearing is allowed immediately and crutches are used for at
least 6 weeks. The hinged knee brace and crutches are discontinued when
the patient is able to ambulate with good quadriceps control.
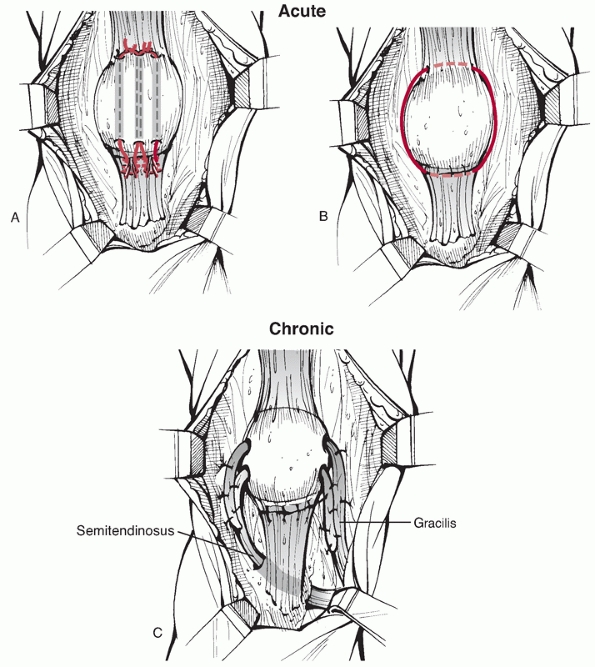 |
|
FIGURE 52-13 Patella tendon repair. A. Direct repair to the inferior pole of the patella through three parallel drill holes. B. Addition of a cerclage wire for protection of the tendon repair. C. Use of hamstring tendons placed through bone tunnels for repair of a chronic rupture.
|
The majority of patients who undergo early primary repair achieve a
functional range of motion and normal quadriceps strength. Persistent
quadriceps muscle atrophy commonly occurs but has not been correlated
with loss of strength.58,137 No relationship has been demonstrated between the configuration of the rupture, the method of repair, and
clinical outcome.77,81,122,137 An early repair within 2 to 3 weeks of injury is the only factor that has been associated with improved outcomes. Siwek and Rao137
reviewed 25 patients treated within 7 days and found that 96% had good
to excellent results while only one third of the six patients with a
delayed repair had excellent results. They also noted a greater degree
of persistent quadriceps atrophy in patients treated with delayed
repair. Hsu et al.58 reviewed 35
traumatic patellar tendon ruptures treated acutely with primary repair
and a neutralization wire. They reported 20 excellent (57%) and 10
(29%) good results. The majority of the patients in this series had
sustained the injury on a motorcycle and one third of the patients had
multiple injuries, which the authors concluded may have contributed to
the slightly lower success rate observed. Larsen and Lund81
performed a radiographic analysis of patellar congruence in a series of
patients who underwent operative repair of acute patellar tendon
ruptures. Seven of 10 patients demonstrated incongruity on the Merchant
and lateral radiographs. Patients with residual patellofemoral symptoms
all had incongruity, but the majority were asymptomatic. They concluded
that articular incongruity may not be the only cause of persistent knee
pain in patients who undergo patellar tendon repair.
|
TABLE 52-8 Outcomes after Acute Patellar Tendon Repair
|
||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
significant operative challenges. The unopposed pull of the quadriceps
muscles can result in significant contraction of the extensor
mechanism. Early series recommended preoperative traction to overcome
the contracted quadriceps tendon muscle so that the tendon ends could
be reapproximated.72,137
There have been no large series evaluating the outcomes after
reconstruction of a chronic patellar tendon rupture. Isolated case
reports have described different techniques and grafts including
autogenous or allogenic grafts when local tissue is unavailable.26,44,47,49,55,72,84,144
described a technique of preoperative traction used in the treatment of
three of five chronic patellar tendon ruptures. Preoperative traction
was used in the following circumstances: neglected rupture of the
patellar tendon with marked radiographic or clinical displacement and
inability to move the patella manually distally. A Steinman pin was
placed transversely through the proximal portion of the patella, and 5
lb of traction was applied from 4 days to 2 weeks preoperatively. Knee
range of motion was initiated after the traction procedure. All repairs
were augmented with a fascial graft or Bunnel wire. They reported 90%
good to excellent results in five patients.
first to describe a case using the semitendinosus tendon to augment a
chronic patellar tendon rupture. In this technique, a staged surgical
procedure was performed with skeletal traction applied until the
patella descended to a level 1 inch proximal to the articular surface.
Then, through a proximal incision, the semitendinous tendon was divided
at its musculotendinous junction. A longitudinal paramedian incision
was performed and a drill hole made in the tibial tubercle and the
distal patella. The free end of the tendon was passed from medial to
lateral through the tibial tunnel and then from lateral to medial
through the patella. The tendon was then brought down and sutured on
itself. A cylinder cast was applied for 6 weeks.
four patients who underwent late reconstruction of the patellar tendon
with semitendinosus and gracilis tendons. Preoperative traction was not
used in this series. Intraoperatively, a Steinmann pin was placed
transversely through the patella and traction was applied distally. The
Insall/Salvati ratio was used to determine the correct height of the
patella. The semitendonous and gracilis were harvested, leaving the
distal insertion at the pes anserinus intact. Three large drills holes
were made to accommodate the tendon: an oblique drill hole through the
tubercle beginning proximally on the lateral aspect and extending
distally to the medial aspect and two parallel transverse holes through
the patella. The semitendinosus tendon was then inserted from medial to
lateral through the oblique hole in the tibial tubercle and then from
lateral to medial through one of the transverse holes in the patella.
The gracilis tendon was then passed from medial to lateral through the
remaining transverse hole in the patella (Fig. 52-13C).
A heavygauge wire was placed through the tubercle and the distal hole
of the patella. While the patella was maintained in a normal position
with the traction pin, the wire was tightened to hold the position of
the patella. The tendons were then sutured to each other. The wound was
closed and a cylinder cast was applied for 6 weeks. The knee was
manipulated and the wire removed at 6 weeks. Satisfactory results were
reported with all four patients returning to work and achieving full
active extension and 100 degrees of flexion.
of extensor mechanism injuries. Treatment concepts are similar to those
used in the treatment of distal pole patellar avulsions. If the bone
fragment is large enough, internal fixation with 3.5-or 4.5-mm screws
should be performed with the addition of a stress-relieving cerclage
wire to the protect repair. If the tubercle fragment is too small for
screw fixation, the tendon should be reapproximated to the proximal
tibia through bone tunnels similar to the treatment used in other
tendon avulsion injuries.
average annual incidence of 5.8 per 100,000, increasing to 29 per
100,000 in the 10- to 17-year age group.102 Lateral patellar dislocations occur most commonly and conservative treatment is usually recommended.10,12,102,141
The majority of patients experience no further instability, but the
reported recurrence rates after conservative treatment range from 15%
to 44%.102 Osteochondral fractures
at the medial inferior edge of the patella are highly suggestive of
this injury pattern. Treatment of an acute lateral patellar dislocation
typically consists of closed reduction and the use of an extension
brace or cast for three weeks with immediate weight bearing. Range of
motion in flexion is increasingly permitted over the following 3 to 4
weeks. Atkin et al.12 prospectively
studied 74 patients with primary acute patellar dislocations treated
initially with a knee immobilizer for comfort, allowing them to bear
weight as tolerated with crutches. As soon as patient comfort allowed,
patellar stabilizing braces were used and resisted close-chain
exercises and passive range of motion in the brace were permitted.
Return to sports was allowed when full passive range of motion was
regained, no effusion was present, and quadriceps muscle strength had
achieved 80% of the contralateral side. No recurrences were seen at 6
months with this protocol.
controversy regarding the management of these injuries, particularly
with respect to operative indications. Most authors support operative
fixation of a large displaced osteochondral fracture.10,12,102,141
The presence of a hemarthrosis increases the likelihood that a
significant osteochondral fracture has occurred. Articular cartilage
injuries are common and have been reported to occur in up to 95% of
first-time dislocations.110 This
reported high rate of articular cartilage injury has led some authors
to advocate routine arthroscopy to evaluate this injury.10,37
However, a consensus statement issued by the International
Patellofemoral Study Group recommended that patients at high risk
(i.e., those with large hemarthrosis) undergo MRI to detect
osteochondral fractures.102 MRI is
also helpful in assessing the medial soft tissues and identifying
injuries of the medial retinaculum, the medial patellofemoral ligament,
and the vastus medialis obliquus.46
This recommendation was made based on the observation that while
articular injuries are common, not all require treatment. A second
controversy is whether a patient who has sustained a primary patellar
dislocation should undergo acute surgical management to decrease the
risk of future instability. While there are many reports in the
literature, there are only three studies that directly compare
operative and nonoperative management.25,102,108
None of these studies were able to identify any difference in outcome
between the two treatment groups with regard to recurrent dislocation.
Relative indications for early surgical treatment have included
concurrent osteochondral injury, palpable disruption of the medial
patellofemoral ligament-vastus medialis obliquus-adductor mechanism,
MRI findings of a large complete avulsion or midsubstance tear of the
medial patellofemoral ligament, patellar subluxation on a Merchant
view, and failure of nonoperative management with subsequent
redislocation.141
after an extensor mechanism injury are the loss of knee flexion and
quadriceps weakness.21 In general,
these complications are more closely associated with the injury itself
than with the technical aspects of the surgical procedure. An
aggressive postoperative program emphasizing early range of motion and
quadriceps strengthening is recommended. To achieve this goal, it is
paramount to achieve an operative repair that is strong enough to allow
early postoperative rehabilitation. Most patients will ultimately be
able to achieve 90 degrees of flexion. This is critical as it allows
for sitting in tight places and also helps with arising from a sitting
position. If 90 degrees of flexion is not obtained by 8 weeks
postoperatively, a closed manipulation under anesthesia may be
considered. However, caution should be used to avoid iatrogenic
re-rupture of the tendon. Arthroscopic débridement and manipulation may
be considered to treat a flexion contracture or more severe flexion
loss. Persistent quadriceps atrophy is noted in many patients but does
not appear to compromise final function. Siwek and Rao137
reported that 75% of their patients who underwent acute quadriceps
tendon repair had persistent quadriceps atrophy of 2 to 4 cm. However,
despite the marked atrophy, most had strength that was adequate for
normal knee function. The treatment for an extensor lag secondary to
weakness or atrophy is a vigorous rehabilitation program.
mechanism results in a high incidence of prominent or symptomatic
hardware. The problem is more common with the addition of a cerclage or
tension band wire. Symptoms are related to irritation of the capsule
and tendons by the implants. A 15% incidence of soft tissue irritation
from hardware that necessitated removal was reported in two series.61,139
Removal of prominent cerclage or K-wires usually alleviates symptoms
and can be performed on an elective basis. The use of nonabsorbable
suture as a reinforcing material has become more popular in an attempt
to avoid this complication.33,99
closed injuries and often related to patient specific conditions and
the subcutaneous positioning of heavy sutures or wires used in surgical
repair. Sutures should not be placed directly in line with the incision
to prevent delayed wound healing. Placing the skin incision lateral to
the tibial tubercle may provide better soft tissue coverage. A
postoperative hematoma can result in pain and an increased risk of
wound dehiscence and infection. The use of closed suction drainage is
recommended to avoid hemarthrosis formation.
injuries is relatively uncommon, postoperative infection following open
patella fractures has been reported to be as high as 10.7%.148
Surgical débridement of nonviable tissue (soft tissue or bone) and
evaluation of the stability of fixation remain the standard tenets of
care. After thorough irrigation and débridement, stable fixation can be
retained. Intraoperative cultures should be used to guide an
organism-specific, 6-week course of intravenous antibiotics. In the
vast majority of cases, early recognition of infection and aggressive
débridement of nonviable tissue will allow for preservation of the
patella. A total patellectomy, however, rarely may be necessary in
situations of intractable osteomyelitis and secondary nonunion.
internal fixation of patellar fractures has been reported to range from
0% to 20% in clinical series.21,61,139
Inadequate fixation, severe comminution, early aggressive
rehabilitation, and patient noncompliance have all been implicated as
risk factors. Smith et al.139 noted
11 cases of lost reduction in a series of 51 patients. Five cases were
attributed to technical errors in tension band wire placement, five to
patient noncompliance, and one to sequelae of infection. Nine cases had
symptomatic hardware that ultimately required removal. Nonoperative
management with a period of immobilization may be acceptable with
minimal displacement (2 mm or less) or incongruity after loss of
reduction. However, reoperation is warranted if the extensor mechanism
is compromised or separation of fragments or incongruity of more than 3
to 4 mm has developed.
who return to activities too early before the bone-tendon junction has
healed. Timely diagnosis and revision are usually successful in
reestablishing knee motion and strength. Competitive sports should not
be allowed for 4 to 6 months to allow time for sufficient tendon
healing and remodeling. Isokinetic strength should be regained before
resuming high-risk activities.
Transverse fractures may have a higher incidence, but nonunions can be
seen in comminuted fractures without stable fixation. If delayed union
is noted on radiography, a period of immobilization may be beneficial
to allow time for fracture consolidation. Elderly patients may tolerate
a nonunion well with minimal functional deficits, including persistent
muscle weakness and an extensor lag. However, reoperation should be
considered if there is a large separation between the bone fragments,
or pain in a younger patient. Revision surgery with rigid internal
fixation and autogenous bone grafting should be considered. Weber et al.156 achieved a 100% union rate in their series of patellar fracture nonunions using these techniques. Uvaraj et al.149
recently presented outcomes of the surgical management of 22 patellar
nonunions treated at a median of 3 months after injury. Nineteen cases
were treated with tension band wiring with or without cerclage, and
three cases were managed with patellectomy. At a median of 5½-year
follow-up, 91% good to excellent results were reported using the
Bostman criteria.149
Intraoperatively, if extensive cartilage injury is noted or the
fragment appears to have a poor blood supply, a partial patellectomy
may be considered. Whether revision internal fixation or partial
patellectomy is undertaken, reconstruction of the extensor mechanism
should be performed whenever possible. For long-standing nonunions, a
shortened and contracted quadriceps tendon may necessitate tendon
mobilization and quadricepsplasty.59,63
patellar fractures. The etiology is likely multifactorial and may
include (a) articular cartilage damage at the time of injury, (b)
inadequate reduction and restoration of articular congruity, and (c)
excessive callus formation and secondary articular incongruity. Nummi111
reviewed more than 700 patellar fractures and found radiographic
evidence of patellofemoral arthritis in 56.4% of the patients. Most
patellofemoral pain can be managed conservatively with rest, physical
therapy, and nonsteroidal anti-inflammatory medications. Severe
debilitating patellofemoral arthritis can be treated with a
patellectomy.51 Nonanatomic
attachment of the patellar tendon to the patellar remnant after partial
patellectomy can lead to abnormal patellar tilt and has been implicated
as a cause of patellofemoral arthritis. In 1958, Duthie and Hutchinson43
reported tilting of the patella in five of seven patients with
postoperative arthritis, and attributed these changes to malalignment
from attachment of the patellar tendon to the anterior cortex of the
patella.
JD, Leonard RD. A developmental anomaly of the patella frequently
diagnosed as fracture. Surg Gynecol Obstet 1925;41:601-604.
SA, Livermore JT, Werner FW, et al. Knee extensor mechanics after
subtotal excision of the patella. Clin Orthop Relat Res
1992;285:217-222.
MH, Seigel H. Treatment of transverse fractures of the patella by
arthroscopic percutaneous pinning. Arthroscopy 1993;9:119-121.
MT, Sanders R. Patella fractures and extensor mechanism injuries. In:
Browner JLT, ed. Skeletal Trauma: Basic Science, Management, and
Reconstruction. Philadelphia: WB Saunders, 2003:2013-2044.
M, Shields C, Karmy J. Diagnosis of osteochondral fractures in acute
traumatic patellar dislocations using air arthrography. J Trauma
1975;15:1032-1033.
DM, Fithian DC, Marangi KS, et al. Characteristics of patients with
primary acute lateral dislocation and their recovery within the first 6
months of injury. Am J Sports Med 2000;28:472-479.
O, Manisali M, Cecen B. Anatomical and biomechanical evaluation of the
tension band technique in patellar fractures. Int Orthop. Epub 2008.
J, Bried J, Dohm M. Biomechanical evaluation of various forms of
fixation with transverse patella fractures. J Orthop Trauma
1987;1:219-222.
E. Open reduction internal fixation of displaced transverse patella
fractures with figure-eight wiring through parallel cannulated
compression screws. J Orthop Trauma 1997;11:573-576.
S, Zwass A, Abdelwahab IF, et al. Diagnosis of tears of the quadriceps
tendon of the knee: value of sonography. AJR Am J Roentgenol
1994;162:137-1140.
W, Fairchild R. Fractures of the patella. Results of total and partial
excision of the patella for acute fractures. JAMA 1936;106:2121-2125.
O, Kiviluoto O, Santavirta S, et al. Fractures of the patella treated
by operation. Arch Orthop Trauma Surg 1983;102:78-81.
M, Baudendistel B, Sabo D, et al. Acute traumatic primary patellar
dislocation: long-term results comparing conservative and surgical
treatment. Clin J Sport Med 2005;15:62-66.
J, Thomas K, Alexander R, et al. Evaluation of methods of internal
fixation of transverse patella fractures: a biomechanical study. J
Orthop Trauma 1994;8:147-153.
J, Kasman R, Patel N, et al. Biomechanical evaluation of current
patella fracture fixation techniques. J Orthop Trauma 1997;11:351-356.
J, Iannacone W, Marczyk S, et al. Open fractures of the patella:
long-term functional outcome. J Orthop Trauma 1995;39:439-444.
A, Hou C, Bao J, et al. Comparison of biodegradable and metallic
tension-band fixation for patella fractures. Acta Orthop Scand
1998;69:39-42.
R. A new technique for the treatment of comminuted, transverse
fractures of the patella. Surg Gynecol Obstet 1977:909-912.
C. The history of fracture treatment. In: Browner B, Levine A, Jupiter
J, et al., eds. Skeletal Trauma. Philadelphia: WB Saunders, 2003.
S, Baudouin C, King J, et al. Ultrasound, computed tomography and
magnetic resonance imaging in patellar tendinitis. Clin Radiol
1991;43:52-56.
DA, White LM, Fithian DC. Acute lateral patellar dislocation at MR
imaging: injury patterns of medial patellar soft tissue restraints and
osteochondral injuries of the inferomedial patella. Radiology
2002;225:736-743.
P, Pritchard G, Jenkins D. Carbon fibre used in the late reconstruction
of rupture of the extensor mechanism of the knee. Injury Br J Accid
Surg 1987;18:57-60.
W, Lemesurier A. The late repair of fractures of the patella and of
rupture of the ligamentum patellae and quadriceps tendon. J Bone Joint
Surg Am 1927;9A:47-54.
MJ, Griffith MH, Lawrence BD, et al. Complete exposure of the articular
surface for fixation of patellar fractures. J Orthop Trauma
2005;19:118-123.
A, Difiore RJ, Tippens JK. Bilateral simultaneous rupture of the
infrapatellar tendon: a case report and literature review. Orthopedics
1983;6:1472-1474.
P, Reinders J. Transposition of the sartorius muscle for reconstruction
of the extensor apparatus of the knee. J Trauma 1986;26:90-92.
K, Wang K, Ho W, et al. Traumatic patellar tendon ruptures: a follow-up
study of primary repair and a neutralization wire. J Trauma
1994;36:658-660.
YC, Wu CC. Modified Thompson quadriceps plasty to treat extension
contracture of the knee after surgical treatment of patellar fractures.
Chang Gung Med J 2007;30:263-269.
HH, Hayes WC, Stone JL, Shybut GT. Force ratios in the quadriceps
tendon and the ligamentum patellae. J Orthop Res 1984;2:49-54.
L, Chan K, Chow Y, et al. Fractured patella: operative treatment using
the tension band principle. Injury Br J Accid Surg 1985;16:343-347.
L, Lee S, Leung K, et al. Partial patellectomy for patellar fracture:
tension band wiring and early mobilization. J Orthop Trauma
1993;7:252-260.
R, Miles J, Garlick N, et al. A conservative approach to
quadricepsplasty: description of a modified surgical technique and a
report of three cases. J Knee Surg 2008;21:39-42.
J, Wagner WW, Kuiper JH. Tension band wiring of transverse fractures of
the patella. The effect of site of wire twists and orientation of
stainless steel wire loop: a biomechanical investigation. Int Orthop
2007;31:703-707.
K, DeMouy EH, Brunet ME, et al. Radiographic diagnosis of quadriceps
tendon rupture: analysis of diagnostic failure. J Emerg Med
1994;12:225-229.
M, Veselko M. Inferior patellar pole avulsion fractures: osteosynthesis
compared with pole resection. J Bone Joint Surg Am 2004;86A:696-701.
H, Riashi E, Gleason J. Restoration of quadriceps function in neglected
tear of the patellar tendon. Surg Gynecol Obstet 1957;102:200-204.
D, Godfrey K, Johanson P, Whiting M. Quadriceps rupture in association
with the roentgenographic “tooth” sign: a case report. Orthopedics
1980;3:1206-1208.
P, Shanker SJ, Burke T, et al. Bilateral simultaneous rupture of the
quadriceps tendons: a report of four cases and review of the
literature. Clin Orthop 1988;234: 139-141.
M, Bombac D, Balazic M, et al. Modified precurved patellar basket
plate, reconstruction of the proper length, and position of the
patellar ligament: a biomechanical analysis. Knee 2007;14:188-193.
TE, Brems JJ. Diagnosis of acute rupture of the quadriceps tendon by
magnetic resonance imaging: a case report. Clin Orthop Relat Res
1991;262:236-241.
E, Lund P. Ruptures of the extensor mechanism of the knee joint:
clinical results and patellofemoral articulation. Clin Orthop
1986;150-153.
GH, McCulloch P, Cole BJ, et al. The incidence of acute patellar tendon
harvest complications for anterior cruciate ligament reconstruction.
Arthroscopy 2008;24: 162-166.
M, Goldstein J, Rosner M. A method of repair for quadriceps tendon or
patellar ligament (tendon) ruptures without cast immobilization. Clin
Orthop 1987;297-301.
DW. Extensor mechanism disruptions. In: Siliski JM, ed. Traumatic
Disorders of the Knee. New York: Springer-Verlag, 1994:169-174.
AG, Plewes JL. Bilateral simultaneous spontaneous rupture of the
quadriceps tendon: five case reports and a review of the literature. J
Bone Joint Surg Br 1984; 66B:81-83.
R, Swanson T, Sharkey N, et al. Effects of partial patellectomy and
reattachment of the patellar tendon on patellofemoral contact areas and
pressures. J Bone Joint Surg Am 1993;75A:35-45.
A, Smiljanic B, Bekavac-Beslin M, et al. The basket plate in the
osteosynthesis of comminuted fractures of the distal pole of the
patella. Injury 2006;37:525-530.
G, Reidy D, Joy A, et al. The biomechanical evaluation of polyester as
a tension band for the internal fixation of patellar fractures. J Med
Eng Technol 1999;23:53-56.
PE. Tendon and muscle ruptures: clinical and experimental studies on
the causes and location of subcutaneous ruptures. J Bone Joint Surg
1933;15:705-722.
VM, Inoue M, Nomura E, et al. An algorithm guiding the evaluation and
treatment of acute primary patellar dislocations. Sports Med Arthrosc
Rev 2007;15:2-78.
A, Mercer R, Jacobsen R, et al. Roentgenographic analysis of
patellofemoral congruence. J Bone Joint Surg Am 1974;56A:1391-1396.
DBW, Pearson RL, Pankovich AM. Mersilene strip suture in repair of
disruptions of the quadriceps and patellar tendons. J Trauma
1980;20:867-872.
ME, Allgower M, Schneider R, et al. Manual of Internal Fixation.
Techniques Recommended by the AO Group. Berlin: Springer-Verlag,
1979:248-253.
R, Nietosvaara Y, Aalto K, et al. Operative treatment of primary
patellar dislocation does not improve medium-term outcome. Acta Orthop
Scand 2005;76:699-704.
H, Hakek M. Boutonniere-type deformity of the knee following
patellectomy and manipulations. J Bone Joint Surg Am 1984;66A:137-138.
E, Inoue M, Osada N. Anatomical analysis of the medial patellofemoral
ligament of the knee, especially the femoral attachment. Knee Surg
Sports Traumatol Arthrosc 2005;13:510-515.
O, Ahmad S. The vastus lateralis derived flap for repair of neglected
rupture of the quadriceps femoris tendon. Surgery, Gynecol Obstet
1985;385-387.
DL, Amato D, Arellano F, et al. Comparison of a technique using a new
percutaneous osteosynthesis device with conventional open surgery for
displaced patella fractures in a randomized control trial. J Orthop
Trauma 2006;20:529-535.
T, Karpakka J, Orava S. Repair of partial quadriceps tendon rupture:
observations in 28 cases. Acta Orthop Scand 1994;65:154-156.
CD, Wilde AH, Phalen GH. Bilateral rupture of the infrapatellar tendon
in rheumatoid arthritis. Clin Orthop 1973;91:158-161.
C, Goulet J, Matthews L, et al. Results of treatment of displaced
patellar fractures by partial patellectomy. J Bone Joint Surg Am
1990;72A:1279-1285.
T, Grantham J, Prayson M, et al. Biomechanical comparison of fixation
methods in transverse patella fractures. J Orthop Trauma
1998;12:356-359.
S, Leung G. Blood supply of the knee joint: a micoangiographic study in
children and adults. Clini Orthop Relat Res 1956;208:1196.
S, Cramer K, Karges D, et al. Early complications in the operative
treatment of patella fractures. J Orthop Trauma 1997;11:183-187.
C. Uber die Grosse der Unfallfolgen bei der blutigen und unblutigen
behandlung der einfachen (subcutanen) querbruche der kniesheibe. Verh
Dtsch Ges Chir 1905; 34:374-393.
JEM. Fracture of the patella treated by removal of the loose fragments
and plastic repair of the tendon. Surg Gynecol Obstet 1942;74:860-866.
CJ, Svensson J, Leander P, et al. dGEMERIC (delayed gadolinium-enhanced
MRI of cartilage) indicates adaptive capacity of human knee cartilage.
Magn Reson Med 2004;51:286-290.
M, Kastelec M. Inferior patellar pole avulsion fractures:
osteosynthesis compared with pole resection surgical technique. J Bone
Joint Surg Am 2005;87S:113-121.
T, Kuusela T. Fixation of large osteochondral fractures of the patella
with fibrin adhesive system. Am J Sports Med 1989;17:842-845.
LG, glick H. Bilateral spontaneous quadriceps tendon ruptures: a case
report and review of the literature. Orthop Rev 1989;18:867-871.
L, Toby E. Bilateral rupture of the patella tendon in an otherwise
healthy male patient following minor trauma. J Trauma 1986;26:1045-1048.
M, Janecki C, McLeod P, et al. Efficacy of various forms of fixation of
transverse fractures of the patella. J Bone Joint Surg Am
1980;62A:215-220.
P, Johnson R. A study of quadriceps excursion, torque, and the effect
of patellectomy on cadaver knees. J Bone Joint Surg Am 1985;67A:726-732.
K, Byun Y. Separate vertical wiring for the fixation of comminuted
fractures of the inferior pole of the patella. J Bone Joint Surg Br
2003;85B:1155-1160.
J, Wu X, Peng X. Biomechanical experiment and clinical report of
modified patellectomy for polar fracture of the patella. Chin J
Traumatol 1999;2:122-124.
