NONUNIONS AND MALUNIONS OF THE FEMORAL SHAFT AND PATELLA
II – FRACTURES, DISLOCATIONS, NONUNIONS, AND MALUNIONS > Malunions
and Nonunions > CHAPTER 30 – NONUNIONS AND MALUNIONS OF THE FEMORAL
SHAFT AND PATELLA
neck. Both nonoperative and operative treatment methods have high rates
of union because of the excellent blood supply to the femur. The most
common cause of nonunion (other than in the femoral neck) is an open
fracture complicated by infection (15). The etiology of nonunion and the preferred methods of treatment for each section of the femur are quite variable.
from more than 2.5 cm distal to the lesser trochanter, to within 10 cm
of the knee joint. Supracondylar nonunions are discussed in the next
section of this chapter. See Chapter 29 for nonunions about the hip.
locked intramedullary nailing using closed techniques, nonunions of the
femoral shaft are unusual (46). The literature
up to 1979 reported an incidence of nonunion of 2.1% in open nailing of
the femur and 0.2% in closed nailing of the femur (11).
Today, the incidence in closed fractures remains less than 1%. Nonunion
is more likely to occur when an open fracture is complicated by
infection or when there is loss of bone substance. External fixation
is usually indicated for infected nonunions (3). Infected nonunions are discussed in detail in Chapter 133 and Chapter 135.
The incidence of nonunion is higher in nonoperative treatment of shaft
fractures than with intramedullary nailing. Nonunion is most likely to
be a complication of failure of plate fixation of the femur. Nonunions
of fractures treated nonoperatively are usually accompanied by
shortening, malrotation, and significant angulation. Nonunions
accompanying intramedullary fixation are usually in good alignment, but
a broken nail may be present. Nonunions with plate fixation are usually
accompanied by failure of fixation. Good cortical contact is usually
present, but angulation may be a problem.
can be treated, if the medullary canal is in reasonable alignment, by
removal of the original nail and closed reamed intramedullary renailing
(27). An open procedure is necessary when
alignment of the medullary canal is poor or there is hardware in place
that requires removal. With closed intramedullary nailing, bone
grafting is usually unnecessary (30). In open procedures, however, onlay cancellous bone grafting should be done routinely (21,36,37).
Intramedullary nailing is the preferred method of fixation, except
where distortion of the intramedullary canal makes nailing impossible (13).
In such cases, plate fixation is indicated, and the principles
described for plate fixation of supracondylar nonunions apply (35).
Nonunions with defects or severe shortening may need specialized
techniques such as allograft replacement, free microvascularized bone
grafts (45), newer bone inductive methods (23,24), or Ilizarov techniques (see Chapter 32).
shaft of the femur without bone grafting, follow the basic principles
of closed intramedullary nailing described in Chapter 11, Chapter 19, and Chapter 20.
-
Place the patient in a lateral decubitus
position on a fracture table or on a radiolucent regular table, with
the femur to be operated on uppermost. The supine position on a
fracture table can be used as well. -
Expose the trochanteric region through a gluteus maximus–splitting incision.
-
If an intramedullary nail is present,
remove it. If it is a cannulated design, first place a 3.5 mm reaming
guide pin. If the nail is broken, it is usually possible to remove it
by closed technique. First, remove the broken proximal piece of the
nail. Ream the proximal fragment until it is larger than the diameter
of the remaining distal portion of the nail. In most nonunions in
average-size patients, I use a 15 mm or larger nail. In large patients,
I advise a 16 or 17 mm nail. Thus, it is possible to ream up to 15 to
17 mm. -
The distal fragment of the nail can then
be removed by one of several techniques. It may be possible, under
fluoroscopic control, to grasp its proximal end with a strong
bronchoscopy forceps and pull it out. A set of specialized instruments
for removal of nails and nail fragments designed by Dr. Robert Winquist
is now available from Snap-On MPD (Kenosha, WI). In this set, one of
the most useful devices I have found for removal of nails is a series
of guidepins in various sizes with bullet tips, together with
associated guidepins with no bullet. To remove a cannulated broken
nail, insert (under fluoroscopy) the largest ball tip that will fit
through the end of the nail and locate the ball just outside the tip of
the nail. Then jam this guidepin by driving a non-ball-tip guidepin
beside it. Attach the Jacobs chuck T-wrench with flanges to the ball
tip guidepin and using a mallet, extract the broken segment. “Easy
outs” and other special tools for broken nail removal are also
available. If it is impossible to remove the distal section of the nail
by one of these techniques, or if the nail is solid, make a small
window in the bone distally and tap it out, or open the nonunion site
to extract the remaining portion of the nail. -
Once the canal is clear, carry out closed nailing by the usual technique (see Chapter 11, Chapter 19, and Chapter 20).
Use a nail at least 2 mm wider than the previous nail, if possible.
Ream sufficiently to obtain good cortical contact on both sides of the
nonunion, and use a nail that extends distally to within 1 cm of the
subchondral bone of the knee. I always use statically locked
interlocking nails. I prefer the Alta nail (Howmedica, Rutherford, NJ)
because its slap-hammer driver facilitates compression of the fracture.
In the vast majority of cases, I lock the nail distally first, impact
the fracture by reversing the slap-hammer or by applying an AO
distractor in compression, and then lock proximally (Fig. 30.1, Fig. 30.2, Fig. 30.3).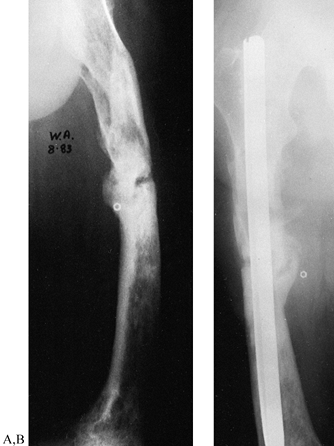 Figure 30.1. A:Radiograph
Figure 30.1. A:Radiograph
of a nonunion of the midshaft of the femur in a 47-year-old man who
sustained the fracture 29 years earlier. Treatment was complicated by
infection. Thirty previous operations had been performed. At this
point, the limb was 1 inch short, the patient had had no recurrence of
infection for 5 years, and he had a painful deformity of the femur. B:
Closed intramedullary nailing using a 17-mm-diameter nail was
performed. This AP radiograph shows early union 12 weeks after the
procedure. The patient was treated before locking nails were available.
Today, the fracture site would have been fixed in compression with a
statically locked nail.![]() Figure 30.2. A:
Figure 30.2. A:
AP radiograph of a subtrochanteric nonunion after blade plate fixation
of a comminuted subtrochanteric fracture with failure of the plate. B: AP radiograph showing treatment with an Alta rod connector combined with a hip screw and an autologous bone graft.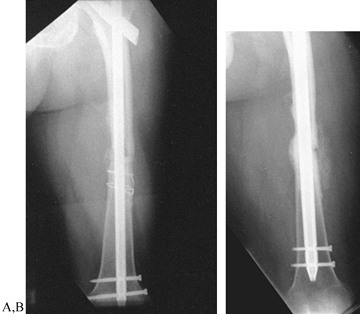 Figure 30.3. A:
Figure 30.3. A:
AP radiograph of a 45-year-old man 1 year after ipsilateral concomitant
fracture of the femoral neck and shaft treated with an Alta rod
connector. There was union of the femoral neck and nonunion of the
shaft fracture. B: The nonunion was
treated by removal of the rod connector and repeat closed nailing with
a larger nail with static locking in compression. This AP radiograph
shows union 9 months after repeat nailing.
union rate after repeat reamed closed nailing of femoral nonunions is
reported to be 53% to 78% after a single procedure and 87% to 95% after
a second procedure (16,19,43).
In my personal experience of 41 nonunions of the femoral shaft treated
by this technique between 1983 and 1999, the union rate was 78% after
one procedure and 95% after two procedures (16).
reconstruction nails that provide fixation into the femoral head are
usually necessary (2,47) (Fig. 30.2).
-
If an open technique is indicated, place
the patient in the lateral decubitus position on either a regular
operating table or on a fracture table, depending on your preference
and the technique to be used. Use a direct lateral
P.953
approach to dissect posteriorly to the vastus lateralis and expose the femur by subperiosteal dissection (see Chapter 3). Preserve the medial and posterior soft-tissue attachments. -
If plates and screws are present, remove
them. If an intramedullary nail is present, remove it as described
previously. If the nail is broken, it is possible to remove it directly
through the nonunion site rather than through the buttock incision.
Special techniques are not usually required.In most cases, it is necessary to take down the
nonunion, open the medullary canal, and freshen the ends of the
fracture. Reduce the fracture and carry out locked intramedullary
nailing. With an osteotome, petal the femur for 5 cm proximal and
distal to the nonunion site and place copious cancellous bone graft
around the nonunion site. Close in the usual fashion over a drain.
the nonunion site is in compression and the femur is statically locked
postoperatively. This provides solid fixation, which permits early
weight bearing and a full rehabilitation program to work on joint range
of motion and muscle strengthening. For the first 6 weeks after repair,
it is advisable to ask the patient to use assistive devices, but I
usually allow them to progress to full weight bearing as tolerated.
Thereafter, patients can usually progress to full weight bearing but
must avoid activities other than ordinary walking and nonimpact
activities such as swimming and stationary bicycling until healing of
the nonunion occurs, as heralded by bridging callus or disappearance of
the nonunion site seen on two views.
nonunions with exchanged reamed nailing using first-generation
nonlocking nails such as the Küntscher nail (7).
This resulted in union rates of 90% or better. The principle with this
technique was to allow full weight bearing on a nail, which would allow
compression of the fracture site. The same philosophy applies to
removing the cross screws from a locked screw to “dynamize” the
fracture, allowing weight bearing to cause compression and pulsatile
stimulus at the fracture site to promote union. This technique does
work and is most effective when the fracture pattern is such that with
impaction it becomes rotationally stable, such as in oblique nonunions.
In many nonunions, however, the configuration is such that either
excessive shortening will occur or rotational stability may ensue. I
have also found that the dynamization worsens some patients’ pain and
is not well tolerated. Currently, I dynamize only when there is no
comminution in the fracture site and an oblique pattern is present that
will stabilize with weight bearing. It is necessary to remove the cross
screws from only one end of the rod, and these should be at the end
farthest from the fracture site. This applies only to delayed union or
nonunions in the mid diaphysis. In all other fractures with delayed
union or nonunion, a much higher success rate will be achieved with
exchanged reamed locked nailing with compression across the fracture
site.
nails, it is possible to treat any nonunion that is sufficiently
proximal to the knee joint (a distal segment of 10 cm is required) by
placing two distal cross-locking screws. Modification of the nail by
cutting off part of its tip to allow it to be placed more distally may
permit the treatment of more distal nonunions, but this is a
specialized technique. Custom nails can be ordered as well.
through the intracondylar notch of the femur—these nails are specially
designed for this purpose—have been advocated for the treatment of
supracondylar nonunions. Experience with these nails, however, has not
proven successful (P. Tornetta III, personal communication 1999). The
nails apparently do not provide sufficient purchase in the distal
fragment because of disuse osteoporosis secondary to the nonunion. At
present, I do not advise the use of retrograde supracondylar nails for
supracondylar nonunions.
internal fixation using a variety of plates. Double-plate fixation
comparable to that described for the trochanteric region may be
indicated (see Chapter 29). Osteoporosis may
make solid screw fixation difficult to achieve. In elderly patients, in
cancellous bone, methacrylate can be inserted into the screw holes to
improve screw fixation. Cement is not advisable in younger patients
because if the appliance must be removed, considerable bone destruction
may be necessary to remove it. Consequently, methacrylate is used only
as a last resort. Back-up washers and nuts on the screws on the
opposite cortex are often helpful. Another useful technique is to take
a cortical or corticocancellous bone graft from the tibia or ilium, or
a femoral allograft, place it opposite the plate, and fix the screws
into this stronger bone. I believe this is more useful than dual-onlay
grafts. See the section on PERIPROSTHETIC FRACTURES in Chapter 20 for a discussion of this technique.
the distal femur, or destruction of the knee joint makes salvage of
knee joint motion impractical and internal fixation of the nonunion
extremely difficult. In such situations, consider immediate fusion of
the knee in combination with treatment of the nonunion. This can be
accomplished by double-plate fixation, or with a long intramedullary
nail traversing the femur and knee joint into the proximal tibia (4,30). In the series by Beall et al. (4),
fusion of the knee was not attempted, and after nail removal
preoperative range of motion of the knee was maintained or increased in
all cases.
arthritis of the knee, the morbidity of and low success rate with
internal fixation may not justify fixation. Total knee replacement with
a modular distal femoral component in some with acute fractures and in
difficult nonunions may be a better choice (18). Freedman et al. (18)
used the Kinematic rotating hinge knee (Howmedica, Rutherford, NJ cin
five patients with difficult distal femoral reconstructive problems
after fracture of the femur, and four were restored to ambulatory
status with good results on the Enneking rating system. One patient
required amputation as a result of deep infection.
-
If plate fixation and bone grafting are
necessary, use the basic techniques for fixation of the shaft or
supracondylar fractures of the femur (see Chapter 20 and Chapter 21). Place the patient in a supine position on a radiolucent operating table with a C-arm fluoroscope available. -
Use an anterolateral exposure (10)
because visualization of the condyles of the femur and knee joint is
often necessary. Try not to strip the medial and posterior surfaces. I
have never found release of the patellar tendon to be necessary. -
Remove any hardware and correct any
secondary deformity. A fibrous union in good position can be internally
fixed in position; otherwise, take down the nonunion, freshen the bone
ends, open the medullary canal, and refashion the bone ends to correct
any deformity and maximize bone contact. Fixation choices include the
AO 95° condylar blade plate, a dynamic compression screw and side
plate, or the Alta distal condylar plate or 95° screw or bolt and side
plate. I no longer use the AO condylar plate because it is difficult to
use and not as versatile as the newer devices. (See Fig. 30.4, Fig. 30.5). Chapter 21 describes the full operative technique.![]() Figure 30.4. A:
Figure 30.4. A:
AP radiograph of a 24-year-old woman 18 months after a T-type
supracondylar fracture of the femur treated with an AO T plate. She has
a painful nonunion with shortening and a varus deformity. B: AP radiograph of treatment with an Alta distal 95° condylar plate and screw combined with autologous bone graft. Figure 30.5. Supracondylar femoral nonunion. A: AP radiograph of the femur in a 35-year-old man who sustained a grade 3A open comminuted supracondylar fracture. B:
Figure 30.5. Supracondylar femoral nonunion. A: AP radiograph of the femur in a 35-year-old man who sustained a grade 3A open comminuted supracondylar fracture. B:
After irrigation, debridement, and plate fixation, the fracture became
infected and went on to a nonunion. This AP radiograph shows the
original internal fixation with antibiotic beads in place. C,D:
The plate and screws were removed and after resolution of the
infection, the original treating physician internally fixed the
fracture with a retrograde supracondylar nail. Unfortunately, this
failed as well, resulting in a persistent nonunion. E,F:
I first encountered the patient 18 months after the original fracture.
There had been no evidence of infection for 15 months. I removed the
nail and screws, and through an anterolateral approach applied an Alta
lateral plate assembly. I augmented this with a smaller anterior plate
and applied an iliac crest bone graft. The nonunion healed in 16 weeks
with no recurrence of infection. Knee motion was from full extension to
110° of flexion. -
If necessary, add a second anterior 3.5
or 4.5 mm narrow or reconstruction plate with six holes to place three
bicortical screws in each fragment. Make this plate shorter than the
side plate proximally. Obtain interfragmentary lag screw compression if
possible. -
Petal the bone about the fracture site, apply an onlay cancellous bone graft, and close over suction drainage.
advise wave plating when treating nonunions where there is a segmental
defect more than 5 cm in length, where there has been a history of
sepsis, or where the medullary canal is unsuitable for intramedullary
nailing. Wave plating involves molding the plate into a wave
configuration so that it stands out from the femur throughout the zone
of bone deficiency and nonunion. This permits the placement of a large
volume of bone graft, which promotes union, makes for a structurally
stronger union when it occurs, and permits the use of a free
microvascularized fibular transfer. Using the wave plate method, Ring
et al. (38) achieved union in 41 of 42
consecutive complex ununited fractures of the femoral shaft at an
average of 6 months after fracture. Three required a
second bone graft, and two had recurrence of infection; in one of these there was a persistent nonunion. Matelic et al. (31)
have promoted the use of an AO dynamic compression plate placed in an
intramedullary location to serve as a medial buttress in fresh
fractures and nonunions where there is medial bone deficiency. The
advantages of the intramedullary location are that less soft-tissue
stripping (and thus devascularization) of the bone is necessary; more
surface area at the fracture site is available for bone grafting; and
the screw fixation from the accompanying lateral plate can be inserted
through the intramedullary plate, increasing the strength of fixation
and buttressing the medial cortex. The primary disadvantage of
endosteal plating is that it is technically demanding, resulting in
long surgery times and increased blood loss. In seven patients with
complex nonunions of the distal femur, Cove et al. (14) achieved union in all with an average time to union of 19 weeks (Fig. 30.6).
 |
|
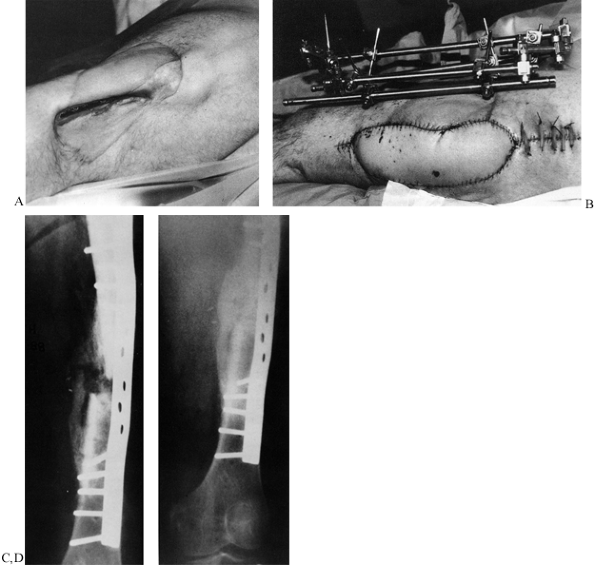
Figure 30.6. Wave plate: A: A 27-year-old man presented with an infected nonunion of 13 months duration. B:
Debridement was performed with application of an external fixator, using a latissimus free flap to cover the defect at a subsequent debridement 2 weeks later. C: Three weeks after soft-tissue coverage, the patient underwent stabilization using a 16-hole broad dynamic compression plate with wave configuration augmented with iliac crest bone graft. D: At 7 months, the fracture had consolidated, and the patient was fully weight bearing without pain. (From Cove JA, Lhowe DW, Jupiter JB, Siliski JM. The Management of Femoral Diaphyseal Nonunions. J Orthop Trauma 1997;11:513, with permission.) |
plate used as a medial buttress, combined with a 95° angled blade. The
technique of using a medial endosteal buttress plate is as follows (31):
 |
|
Figure 30.7.
Medial endosteal buttress plate. An AO broad plate is used as a medial buttress, combined with a 95° angled blade plate. (From Matelic TM, Monroe MT, Mast JW. The Use of Endosteal Substitution in the Treatment of Recalcitrant Nonunions of the Femur: Report of Seven Cases. J Orthop Trauma 1996;10:1, with permission.) |
-
Use an articulating tension device or a femoral distractor to distract the fracture.
-
Use a gouge and curet to make a trough in
the distal metaphysis on the medial aspect to allow the intramedullary
plate to be seated against the blade. -
Insert the plate into the intramedullary
canal in a retrograde fashion and then, using a curved impactor, drive
it into the prepared trough to abut against the blade. -
Then reduce the fracture by diminishing the distraction force and allowing the fracture surfaces to oppose.
-
Insert two or three screws into the lateral cortex only and impact them against the plate, pushing it medially.
-
Insert the other screws through the holes
in both plates. To accomplish this, use a 3.2 mm drill to drill the
lateral cortex with the appropriate drill guide. Then pass a 1.6 mm
Kirschner wire (K-wire) through the hole and use it to feel the holes
on the medullary plate. When you know the direction, direct the drill
in the same path toward the medial cortex, and penetrate it. Insertion
of these screws is frequently skewed so that the screws actually thread
the hole in the plate as they pass into
P.957P.958
the medial cortex. This ensures the blocking action of the plate. In Figure 30.7, the fifth screw from the top would have this effect. The medial plate is thus locked between the blade and the screws.
and improve knee range of motion. In most cases, continuous passive
motion can be started after drain removal and continued until the
patient can actively carry out range-of-motion exercises. Active
assistive exercises with a therapist are helpful. With good internal
fixation, external protection is usually unnecessary. Confirm the
presence of bone union with four-plane radiographs or anteroposterior
(AP) and lateral tomograms before beginning full weight bearing.
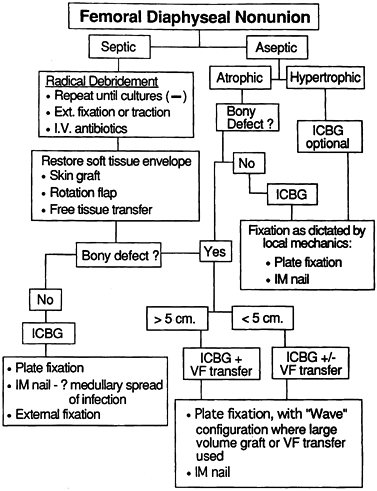
A few comments about the treatment of infected nonunions are pertinent
here. The general principles in the treatment of infected femoral
diaphyseal nonunions are well outlined in the algorithm advocated by
Cove et al. (Fig. 30.8) (14). In treating infected nonunions,
the first step in the vast majority of cases is eradication or control
of the infection, followed by restoration of the soft-tissue envelope (23).
Generally, this requires a radical debridement of the nonunion site,
removing all scarred soft tissues that are impairing revascularization
and all necrotic bone. Take cultures to identify the infecting
organisms. In the femur, stabilization to maintain alignment and length
is essential. Although traction can be used, in most cases the period
of time that stabilization in the absence of internal fixation will be
necessary is such that external fixation is best. If the infection can
be resolved and there are particular advantages in converting from
external to internal fixation, such conversion may occur, but
definitive treatment to union in external fixation may be necessary.
Usually, several debridements are necessary and treatment with
intravenous antibiotics for up to 6 weeks, with suppressive oral
antibiotics for longer, may be necessary.
 |
|
Figure 30.8.
Clinical algorithm for treating femoral nonunion. (From Cove JA, Lhowe DW, Jupiter JB, Siliski JM. The Management of Femoral Diaphyseal Nonunions. J Orthop Trauma 1997;11:570, with permission.) |
by having a well-vascularized muscular envelope completely around the
fracture. This is usually not a great problem in the femur because of
the large muscle envelope of the thigh, but skin grafts, rotation
flaps, and free tissue transfer may be necessary to provide an
appropriate environment for definitive treatment of the nonunion (40). Ilizarov techniques may be appropriate for the particular fracture (see Chapter 32 for details).
then iliac crest bone graft in external fixation usually suffices for
those nonunions without a major gap. Usually, conversion from external
fixation to intramedullary nailing is not appropriate because of the
high risk of infection, but conversion from the external fixator to
plates may be appropriate. In such cases, removal of the external
fixator to allow the pin tracks to heal prior to open plate fixation is
usually advisable. In the interim, stability and length can be
maintained with a cast-brace with intermittent traction if necessary.
For larger defects, iliac crest bone graft combined with a vascularized
fibula may be necessary (46).
Slätis and Paavolainen (41)
advocate one-stage treatment of infected nonunions of the femoral shaft
by excision of dead and infected tissue, resection of bone ends,
cancellous bone grafting, and external fixation. They were successful
in four of five cases. This small series, however, does not prove the
efficacy of this method, and I prefer the staged approach advocated by
Cove et al. (14) (Fig. 30.8).
nonunions treated between 1983 and 1997, using plating and bone graft,
I was able to achieve union in 95% (10). In most series, overall success rates for treatment of aseptic and septic nonunions of the femur are 70% to 97% (4,5,13,14,25,27,31,38,39,40 and 41).
experience, they occur most often after treatment with cast-braces,
which is rare today, or after treatment of unstable and/or open
fractures with small intramedullary nails. Almost all malunions of the
shaft show combined deformities of malrotation, angulation, and
shortening. Shortening of more than 2.5 cm necessitates a cumbersome
shoe lift and causes considerable inconvenience to active patients. It
generally requires correction either by lengthening the shortened femur
or by shortening the contralateral femur (12).
Malrotation is better tolerated in external rotation than in internal
rotation. As long as there is at least 10° to 15° of rotation beyond
neutral in either external or internal rotation, patients rarely have
functional problems. When they cannot rotate to neutral, significant
functional problems usually require correction of the malrotation.
Inability to rotate the extremity at least to a neutral position places
the knee and ankle joints out of the plane of progression for walking.
This produces an inefficient and unsightly gait and interferes with
sports activities.
significant malrotation or shortening. There are three indications for
correction of angulation: poor function, often accompanied by pain;
poor cosmesis; and the potential for late degenerative arthritis due to
abnormal stresses across the knee joint (26).
Decisions to undertake surgical correction for the first two complaints
depend not so much on the degree of angulation present as on the
patient’s complaints. Generally speaking, angulation of less than 10°
rarely produces significant functional or cosmetic impairment.
Angulation of more than 20° almost always creates problems for the
patient. The effect of angulation on joint function and possible late
degenerative arthritis is more difficult to judge. In most patients,
angulation of less than 10°, particularly in the middle third of the
shaft, rarely creates problems. The preexisting alignment of the
patient’s legs, however, has a major effect; for example, a patient
with preexisting genu varum may not tolerate an additional 10° of varus
angulation and may require surgical correction. Generally, angulation
of more than 15° requires correction in active patients. These are
multifactorial decisions that require close consultation with the
patient. The goal of restoration of the mechanical axis of the
extremity is discussed in Chapter 26 and Chapter 32.
of malunion of the femur depends on the degree of deformity, the
alignment of the medullary canal, and the location of the deformity.
From a technical viewpoint, open procedures are the easiest to perform,
but many deformities of the femur are correctable by closed
intramedullary osteotomy and nailing techniques. Ilizarov techniques
have added a whole new dimension to the treatment of malunions (see Chapter 32).
In most cases, it is best to expose the fracture site, take down the
malunion, and restore the normal anatomy of the femur. Late malunions
with significant remodeling are difficult to take down through the
original fracture site, and various osteotomies are applicable.
technique that requires significant experience with closed
intramedullary nailing (9,17,44).
For this technique, the offset in the diameter of the medullary canal
must be less than 25%. Alignment must be good enough to allow the
passage of intramedullary instruments and a nail down the medullary
canal of the femur past the deformity. The technique is best suited for
correction of shortening of less than 5.0 cm and for correction of
malrotation. In some cases, angulation is correctable as well, but
often an open osteotomy to realign the femoral canal is necessary. In
malunions of the middle third of the shaft, internal fixation with
medullary nails rather than plates and screws is preferred because
failure is less likely and immediate weight bearing is possible in most
cases.
-
Place the patient in the lateral decubitus position on a fracture table with the extremity to be operated on uppermost (see Chapter 11 and Chapter 20).
Prepare and drape from buttocks to the tibial traction pin. Through a
gluteus-splitting incision, expose the piriformis fossa of the femur. -
If an intramedullary nail is already in
place, the procedure is greatly simplified; remove the nail and insert
a reaming guide pin. If a nail is not present, it is necessary to
reestablish the patency of the medullary canal. In some cases, a 3.5 mm
guide pin can be passed directly down the canal, and reaming can
proceed. In other
P.961
cases,
the medullary canal at the fracture site is blocked by callus and must
be reopened. To achieve this, a set of recently sharpened, heavy,
flagged Küntscher guide pins or hand reamers must be available. If
angular deformity is present, one of the guidepins will need a bent tip. -
First, place a reaming guide pin down to
the blockage and progressively ream the canal to the size required for
the nail to be inserted. For these osteotomies, larger-than-normal
nails are used; in the average-size man, I use at least a 16 mm nail.
Enlarging the proximal canal allows better working room for the guides
necessary to perforate the blockage. -
Insert a sharp-tipped guide pin of the
appropriate curvature and drive it with a mallet into the bone blocking
the canal. Take care to remain in the central axis of the canal. If a
straight-tipped pin is used, this can be attached to a power source and
the blockage drilled. If the bone is soft, direct penetration may be
possible. Otherwise, it will be necessary to withdraw the sharp-tipped
guide pin after penetrating 1 cm or so. Reinsert the reaming guide pin,
and with the end-cutting reamer open the canal in the perforated
portion. Alternate these two methods until the blockage is opened. If
the blockage is in the proximal half of the femur, the hand reamers
from the AO instrumentation are useful as well. This technique can be
difficult and time consuming. -
Rather than spending inordinate amounts
of time trying to open the canal by closed technique, I often open the
malunion site and perform an open osteotomy. Once the canal is open,
insert the reaming guide pin distally to the subchondral bone at the
knee, and progressively ream the canal to the desired diameter. -
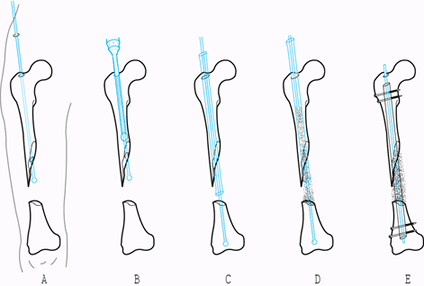
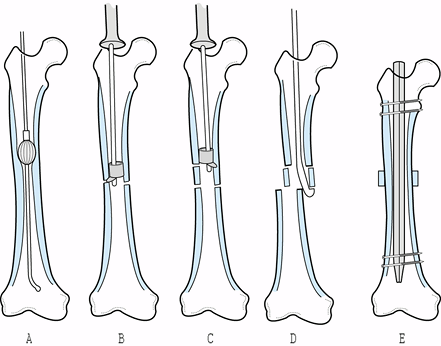
With closed technique, insert the Pearson intramedullary saw (Fig. 30.9)
and transect the femur at the appropriate level. In preoperative
planning, it is important to select an osteotomy site slightly proximal
or distal to the fracture site in normal bone. Closed osteotomies at
the old fracture site give the most precise correction, but an
incomplete cut due to asymmetry of the canal will require osteoclasis,
or percutaneous insertion of a 0.25-inch osteotome from the lateral
side of the thigh, to complete the osteotomy. Figure 30.9.
Figure 30.9.
Intramedullary saw for osteotomy of the femur using the closed
intramedullary technique. The cutting blade at the distal end works on
the principle of a cam and is available in diameters of 12 to 17 mm.
(Courtesy of Biomet, Bourbon, IL.) B: Saw with parts labeled. (From Winquist RA, Hansen ST Jr, Pearson RE. Closed Intramedullary Shortening of the Femur. Clin Orthop 1978;136:54, with permission.) -
When straightening an angular deformity,
drive the nail into the central portion of the distal femoral condyles.
This will correct any angular deformity. -
If malrotation is present, place two
Steinmann pins or Schanz screws, one above and one below the osteotomy,
for rotational control before performing the osteotomy. Place these
pins directly lateral, with one in the proximal fragment and one in the
distal fragment, through only the lateral cortex of the femur. Do not
penetrate the medullary canal proximally or the pin will interfere with
the saw. Place the pins in alignment with each other initially, and
then measure the angulation between the pins after correction of the
deformity. Before surgery, make a template by bending a K-wire or
cutting a piece of sheet aluminum to measure the rotational angle. A
commercially available goniometer can be used instead, but this is more
difficult to read. -
Maintaining rotational correction during
the drive of the medullary nail can be difficult. For this reason, I
prefer to use the Chick-Langren table (Kirshner Medical, Greenwood,
SC), where the extremity is controlled by a large, threaded Steinmann
pin through the proximal tibia or distal femur attached to the traction
apparatus of the table. This gives nearly absolute control during the
nailing. -
Then drive an interlocking nail, which
can be statically locked. If the limb is less than 2.5 cm short, this
discrepancy can usually be corrected at the same time by distraction
and closed intramedullary bone grafting (Fig. 30.10) (8).
Although length can be gained through the traction apparatus of the
fracture table, it is more effective, and safer, to use an AO femoral
distractor. Attach the two Schanz pins inserted as guides for
correction of rotation to the femoral distractor. Distract slowly over
15–20 minutes. To avoid excessive traction on the sciatic nerve, do no
soft-tissue releases and keep the knee flexed to 90° during the
lengthening. Although I have had no difficulty with the sciatic nerve
with acute lengthenings of less than 2.5 cm, it is advisable to use
sensory-evoked potentials to monitor function in the sciatic nerve
during lengthening. Johnson has performed acute lengthenings of 0.4–3.3
cm using an open technique with various bone grafting materials and has
achieved healing in 18 of 19 patients (22,23).![]() Figure 30.10. Closed intramedullary bone grafting and nailing. A: Insert a guide pin. B: Ream the proximal femur. Do not ream in the gap if it is necessary to ream distally. Save the reamings. C: Pass the guide pin into the distal fragment. Insert a large chest tube down to the fracture. D:
Figure 30.10. Closed intramedullary bone grafting and nailing. A: Insert a guide pin. B: Ream the proximal femur. Do not ream in the gap if it is necessary to ream distally. Save the reamings. C: Pass the guide pin into the distal fragment. Insert a large chest tube down to the fracture. D:
Push reamings and finely morcelized graft down the chest tube by hand,
using the flexible shaft from the AO medullary reamers. Overfill the
defect site. E: Insert an intramedullary
nail, which is statically interlocked. (From Chapman MW. Closed
Intramedullary Bone Grafting and Nailing of Segmental Defects of the
Femur. J Bone Joint Surg Am 1980;62:1004, with permission.) -
When lengthening is anticipated, save all
medullary reamings and bone marrow. For lengthenings of less than 2.5
cm, this will provide enough grafting material to fill the defect. If
insufficient graft is available, harvest cancellous bone from the
inside of the greater trochanter through the entry site for the nail.
If more is needed, obtain cancellous bone from the posterior ilium.
Morcelize this bone finely with a bone-cutting forceps or bone mill. -
With the reaming guide pin in place,
insert a large plastic chest tube down the medullary canal into the
defect site. Cut the chest tube to allow about 4 inches to protrude
from the top of the femur. Hold the chest tube in place with a Kocher
clamp on the top of the tube. It is possible to place the chest tube by
fluoroscopy using the radiographic marker in the chest tube. Insert the
morcelized bone graft into the chest tube; do not place too much at one
time because it may jam in the tube. Place the smaller, flexible AO
reamer shaft, without the reaming head, over the guide pin and use it
to push the graft into the defect site. Completely fill the defect site
with cancellous bone and reaming materials. This is a meticulous and
time-consuming technique. Overfill the defect site with graft. After
inserting the bone graft, ensure that length has been maintained, then
insert and statically lock an intramedullary nail.
occurred in all 15, and no refractures occurred after removal of the
nail. Substantial remodeling is necessary to achieve adequate strength,
so I advise leaving the nail in for no less than 24 months. In the two
cases for which lengthening of 4 cm or more was performed, supplemental
open cancellous bone grafting was later necessary due to inadequate
bone stock at the defect site (union had occurred, however).
femur caused by open fractures with bone loss. In the latter case,
irrigate and debride the wound, initially leave it open, and
subsequently close it. Maintain the length of the femur by skeletal
traction. At 21 days, when the wound has healed satisfactorily and
there is no evidence of infection, perform closed intramedullary bone
grafting.
fixator is usually necessary when the discrepancy is more than 2.5–3.0
cm. In these cases, an alternative technique to equalize leg lengths is
to shorten the contralateral femur using a closed intramedullary
technique. Shortening the
contralateral
femur is technically much easier and safer than lengthening. Although
originally described by Küntscher, this method was popularized by
Winquist et al. (44) (Fig. 30.9, Fig. 30.11).
Although the technique shortens the patient’s overall stature, and in
large corrections will affect overall body proportions, it is
technically a much simpler technique than lengthening, and it offers
the advantages of immediate weight bearing, early union, and early
return to function (Fig. 30.12).
 |
|
Figure 30.11. Closed intramedullary shortening of the femur. A: Ream the medullary canal to the appropriate size—usually 15–16 mm in the average-size male. Remove the reaming guide pin. B: Make the distal saw cut first, in the middle of the isthmus of the femur. C: Make the second saw cut proximally at the appropriate distance from the distal cut. D:
Insert the back-cutting chisel and split the intercalary fragment along the linea aspera. Manipulate the fragments outside the gap with the chisel, or push them out of the way with a small Küntscher nail. E: Insert the intramedullary nail over a driving guide pin and shorten the femur as the nail is driven. (Redrawn from Winquist RA, Hansen ST Jr, Pearson RE. Closed Intramedullary Shortening of the Femur. Clin Orthop 1978;136:54, with permission.) |
 |
|
Figure 30.12. A: Preoperative AP radiograph showing the planned osteotomy sites to equalize a leg-length discrepancy of 25 mm. B: Postoperative AP radiograph showing correction of the leg-length discrepancy with a locked Alta nail for fixation.
|
Determination of the actual leg-length discrepancy can be difficult. I
have not found scanograms to be consistently reliable, so I use them
only for confirmation of other measurements. The best technique is to
place blocks under the short leg of the standing patient to level the
pelvis. Rely on your judgment of the correction of the discrepancy and
the patient’s feelings about the correction. Try to obtain a level
pelvis and take into account any distortion of the pelvis that may be
present from old trauma or developmental or congenital abnormalities.
Then confirm the clinical measurement by taking an AP radiograph of the
pelvis with the patient again standing on enough blocks to correct the
leg-length discrepancy. Use either the film or a horizontal marker to
establish a level plane of reference. Take full-length AP and lateral
radiographs of the femur to be shortened to ensure that there is no
abnormality that would contraindicate shortening.
is to be performed on a previously fractured femur, the osteotomy must
be performed in an area of normal bone, preferably proximal to the
fracture site. Using the preoperative radiographs, plan the site of the
osteotomies and measure their distance from the tip of the trochanter,
taking into account x-ray magnification.
however, postoperative bleeding into the thigh can result in up to a
40% drop in the hemoglobin level. In young healthy patients,
transfusion is rarely required.
-
Place the patient in the lateral
decubitus position on a fracture table with the extremity to be
operated on uppermost, and expose the entry to the medullary canal in
the usual fashion (see Chapter 11 and Chapter 20). -
Insert a 3.5 mm reaming guide pin.
Progressively ream the medullary canal to the desired size. In closed
shortening, the saw is more likely to transect the femur if a larger
saw is used and the canal is reamed widely. With a reamer of known
diameter in the site of the proposed saw cut, visualize the femur on a
lateral view. The size of the reamer provides a guide to the size of
the saw needed to cut through the linea aspera. Take care in smaller
patients not to overream the femur. Overthinning of the anterior cortex
will result in comminution and inability to complete the osteotomy.
Intraoperative monitoring of the reaming process by fluoroscopy avoids
this problem. When reaming a closed intramedullary canal, make a 5 mm
or larger drill hole in the distal metaphysis of the canal to
decompress the canal to reduce the embolization of marrow contents.
Proceed slowly with reaming and progress by 0.5 mm increments. Although
it has been reported, I have never encountered fat embolism syndrome or
adult respiratory distress syndrome after closed intramedullary
osteotomy (Fig. 30.11A) (20). -
Set the medullary saw for the most distal cut first. Insert
P.964
the saw and verify by fluoroscopy that it is in the appropriate
position. Make the saw cut. Because of the teardrop cross-sectional
shape of the femur, if the saw used is too small, the cut may be
incomplete posteriorly. Either place a larger saw or complete the
osteotomy, either by osteoclasis or by placing a 5 mm osteotome
percutaneously from a lateral approach to cut the remaining bridge. In
most cases, sufficient reaming can be done to allow a large-enough saw
to make a complete cut (Fig. 30.11B). -
Carefully set the measuring device on the
saw for the second osteotomy, insert the saw, and verify correct
position by fluoroscopy. The cam of the cutter is 15 mm long, providing
a useful reference to verify the length between cuts. Make the second
cut. An incomplete cut can make displacement of the intercalary
fragment difficult. If only a small bridge of bone remains, insert a 12
mm Küntscher nail down to the proximal osteotomy and abduct the
proximal fragment. A firm blow to the tip of the fragment will often
break it free. If this does not occur easily, then percutaneously
insert a 5 mm osteotome from a lateral approach and transect the bone
bridge. Occasionally, bone spikes are left on the main shaft fragments,
which will prevent complete shortening; these can be removed by a
percutaneous osteotome if necessary (Fig. 30.11C). -
Next, split the intercalary fragment
using the back-cutting osteotome supplied with the medullary saw. Under
fluoroscopic control, insert the back-cutting osteotome and pull it
firmly against the distal surface of the intercalary segment at the
linea aspera. Hold it firmly in position and gently tap the handle of
the saw with the slotted mallet to cut the intercalary fragment. A
single cut usually splits the fragment into two halves (Fig. 30.11D). -
Displace the intercalary fragments out of
the osteotomy site. This can be done by pulling them to the side with
the back-cutting osteotome, or they can be pushed out into the soft
tissues with a small Küntscher nail inserted into the medullary canal.
As long as one end of the intercalary fragments lies outside the
femoral shaft, they will come to lie outside the osteotomy site and
adjacent to the femoral shaft when shortening is performed. The
preferred location for the intercalary fragments is medial, although
generally one fragment ends up medial and the other lateral. -
Insert a driving guide pin and drive an
interlocking medullary nail into position; the nail should be 1 mm in
diameter smaller than the canal was reamed. To accomplish shortening,
it is easiest to drive the nail until it just exits the proximal
fragment. Loosen the traction and manually shorten the femur to close
the osteotomy and bring the tip of the nail just into the distal
fragment. While manually holding the osteotomy closed and maintaining
proper rotation, drive the nail into position. If distraction occurs
during the drive, extract the nail until the osteotomy closes and then
redrive it while holding the osteotomy closed. I always interlock both
distally and proximally. Lock distally first, impact the osteotomy to
close it and achieve compression, and then lock proximally (Fig. 30.11E). -
Wash and debride the entry wound
thoroughly to help prevent heterotopic bone formation. Close the wounds
in layers. Do not use a drain.
can occur. Without blood replacement, I have seen a drop in the
hematocrit in some patients into the low 20s. Monitor the hemoglobin or
hematocrit
on
a daily basis until it stabilizes. Immediately apply a knee immobilizer
in the operating room, with good thigh coverage to compress the thigh;
this may help control hemorrhage. Because of the shortening, patients
lose some control of the quadriceps and hamstring muscles and will have
an unstable knee immediately after surgery. The knee immobilizer
controls the knee and allows immediate weight bearing. Start the
patient immediately on knee range-of-motion and thigh muscle
progressive resistance exercises. Patients can bear weight as tolerated
wearing the knee immobilizer and using crutches. With shortening of 2
inches or less, most patients gain sufficient quadriceps control that
the knee immobilizer can be abandoned after 6 weeks. Most patients will
switch from crutches to a cane at that time, and within a few
additional weeks will be fully weight bearing without assistive devices
(Fig. 30.12).
-
Perform closed intramedullary shortening
of the femur only in the lateral decubitus position on a suitable
fracture table. Full access for the instrumentation is critical and is
not really possible in many patients in the supine position. It may be
feasible to do this procedure in the lateral decubitus position on a
regular radiolucent operating table, but I have never attempted it. -
During preoperative planning, note how
much anterior bow the femur has on the lateral view, and the thickness
of the linea aspera. The saw is straight, so the cut needs to be
located where the saw will fit. A very bowed femur will make passage of
the saw very difficult distally. In addition, try to select an area for
the osteotomy where the linea aspera can be cut completely through by
an appropriate-size saw. -
Although routine intramedullary nailing
can be done through a fairly small proximal incision in the buttocks,
for this procedure I recommend an incision at least 10 cm in length
with good exposure of the posterior aspect of the greater trochanter,
because the need to repeatedly enter the canal with instrumentation
requires good exposure. In addition, the length of the cut is
determined by the placement of the measuring device of the
intramedullary saw against the tip of the greater trochanter. It is
necessary to reproduce this position when the saw is inserted for the
second cut. This necessitates having no soft tissues in the way. -
Protect and be gentle with the gluteus
musculature: One of the primary problems in rehabilitation is regaining
abductor muscle strength. -
The entry for the nail must be directly
above the medullary canal. An eccentric entry will complicate entry of
the medullary saw and nail. -
Entering the saw into the medullary canal
can be difficult. Reaming the entry hole several millimeters larger
than the saw is helpful. When placing the saw, enter from slightly
posterior to the long axis of the femur and screw the saw into place.
The saw is easily bent, so be gentle with it. -
When seating the saw for the first cut,
be certain that the measuring device is firmly implanted on the tip of
the greater trochanter and that all components of the saw are fully
closed. During the cut, be certain that this position is maintained.
Reproduce it for the second cut. Lack of attention to these details can
lead to incorrect shortening. -
When selecting the place for the two saw
cuts, pick a place where there is no pathology in the femur, where
there will be good purchase of the intramedullary rod with the inner
wall of the cortex in both the proximal and distal fragments, and where
the linea aspera is as narrow as possible. Be certain that you are
within the operating length of the saw. -
When cutting with the saw, always advance
it in a clockwise direction. Do not reverse it, as this may catch and
break off the blade. Once the saw breaks through the anterior cortex,
be careful not to advance it too much between cuts, as it may catch and
again break. Never force the saw. -
The linea aspera is always the last
section to be cut through. This can be enhanced by angulating the saw
gently within the canal to press it against the posterior aspect. Try
to avoid incomplete cuts, because subsequent completion of the cut is
complicated, as is closure of the osteotomy. -
When driving the nail, if difficulties
are encountered in keeping the osteotomy closed, use a nail that is
smaller in diameter and/or shorter, because this will facilitate
sliding of the bone on the nail. Recognize that this decreases the
stability of the nailing. -
Shortening becomes increasingly difficult
as the length of the intercalary segment removed increases. Little
difficulty is encountered in shortening up to 3 cm. The most I have
shortened at one time is 6.5 cm. Closure of the osteotomy in such
extreme shortenings is difficult because of bunching of the soft
tissues, and it may require use of an AO universal distractor placed
into compression to close the osteotomy. -
For closed shortenings, I prefer the Alta
system (Howmedica, Rutherford, NJ) because the versatility of the
location of the cross-locking holes permits more flexibility in
placement of the nail and the slap-hammer driver is very useful in
closing down the osteotomy (as described early in this chapter). -
In preoperative planning, be certain to
accommodate for the shorter nail that will be required once the femur
is shortened. In shorter patients, nail size can be a problem because
the large of amount of reaming necessary to use the saw requires a
large-diameter nail, which may not necessarily be routinely available
in short lengths. Be certain that nails of the appropriate length and
diameter are available. -
The only nonunions I have seen in closed
intramedullary shortenings have occurred when the osteotomy was not
fully closed down, and when the nail used had a diameter that was more
than 1 mm smaller than the saw. Be certain that the osteotomy is
absolutely closed down tightly on both AP and lateral views. Beware of
parallax, because if the central beam of the x-ray is not exactly at
right angles to the osteotomy, you can be fooled. Try to use a nail
that is no less than 1 mm in diameter smaller than the saw used. -
Finally, it is very important to
carefully examine the extremity on the operating table under anesthesia
after completion of the shortening, to be certain that leg length
equalization is appropriate. For shortenings of 2.5 cm or more, plus or
minus 5 mm will leave most patients satisfied, although I try to get
them exact. Verify that rotation has not changed because occasionally
the proximal fragment will rotate externally because of muscle pull,
which will result in nailing in too much internal rotation. In more
than 75 closed intramedullary shortenings, I have experienced this only
a couple of times. We corrected it by reprepping the knee, pulling the
distal cross-locking screws, rotating the femur to the correct
position, and then reinserting the screws.
intramedullary osteotomy of the femur can be avoided by following the
technical guidelines just discussed. Avoid inadequate correction of
deformity and inadequate fixation by good preoperative planning. Closed
intramedullary osteotomies are technically challenging and require
considerable experience with intramedullary nailing techniques. I
advise that the surgeon gain considerable experience with routine
fracture fixation using closed intramedullary nailing before attempting
these osteotomy techniques. Avoid comminution by not overreaming. I
have not had an infection or nonunion from closed shortening.
returns rather quickly. By Biodex measurement (Biodex Medical Systems,
Inc., Shirley, NY), most return to within a few percentage points of
normal (9). With shortening of more than 2.5
cm, at least 1 year is required to achieve 90% of normal muscle
function, and most patients are left permanently with about 5% of
residual weakness. In my patients, this has never been of functional
significance. Because union of the osteotomy is almost always present
by 6 weeks and quite mature at 12 weeks, the reestablishment of muscle
function and joint range of motion is the major determinant of return
to sports and vocational activities.
performed in active patients, most will want the nails removed.
Although I have removed them as early as 9 months after surgery, I
advise most patients that removal is best delayed to 1 year.
bone about the tip of the medullary nail that is symptomatic. Because
these patients are quite active, a nail that is left protruding will
also be symptomatic. In most cases, you can emphasize to patients that
you are operating on a normal extremity and that they will be left with
some residual disability, including a scar in the buttock, and that
some patients will have minor, long-term discomfort in the operative
site. This has discouraged none of my patients from having the surgery,
because the benefits of equal leg lengths far outweigh these minor
residuals.
osteotomy, but it has the disadvantage of slightly higher rates of
infection and nonunion. Before interlocking nails were available,
step-cut osteotomies were used to gain rotational control and better
stability. With locked nails, a step-cut osteotomy is not necessary. In
most instances, a straight transverse osteotomy can be used. When
angular deformity is present, a transverse osteotomy will result in an
open wedge-type osteotomy when the nail is driven.
Graft all osteotomies with the reamings and autogenous cancellous bone if necessary.
-
Place the patient on a fracture table as
you would for the closed intramedullary nailing technique. Prepare and
drape the entire thigh and buttocks area. Use a direct lateral approach
(see Chapter 3) and expose the fracture site by subperiosteal dissection. -
If length needs to be regained, take down the fracture site in a step-cut fashion (Fig. 30.13). Apply a femoral distractor or use traction on the fracture table to gain length.
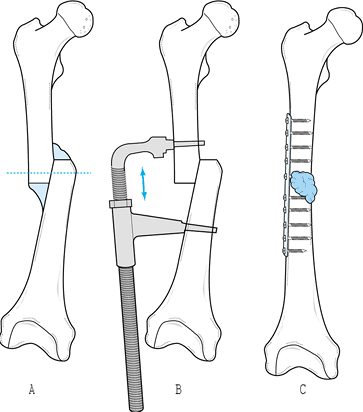 Figure 30.13. A:
Figure 30.13. A:
Malunion of a midshaft fracture of the femur with angulation and
overriding. Even a year after the original fracture, the original
cortex can be differentiated from the surrounding callus. To restore
length, shave off the callus and identify the original cortex. Take
down the malunion through the old fracture site. B: Apply an AO femoral distractor and restore alignment and length. Avoid excessive tension on the sciatic nerve. C:
Fix the osteotomy with a 10- to 12-hole broad dynamic compression
plate. Interfragmentary screw fixation is recommended. Apply the callus
removed earlier as a bone graft. Add additional graft if necessary.
(From Müller ME, Allgöwer M, Schneider R, Willenegger H. Manual of
Internal Fixation. New York: Springer-Verlag, 1979, with permission.) -
Align the femur and internally fix it
with a locked intramedullary nail. Apply the reamings and/or a
cancellous bone graft from the posterior ilium.
intramedullary nailing is the same as for osteotomies using the closed
technique, as outlined previously. The complications are also the same.
Because there is a somewhat increased risk of infection due to open
technique, be certain to administer perioperative antibiotics.
the shaft but is most commonly used for condylar or supracondylar
malunions (1,6,29,32,34,39,42).
It may be necessary in malunions of the shaft where malalignment of the
medullary canal makes intramedullary nailing impossible. Many osteotomy
techniques are possible, including opening wedge, closing wedge,
step-cut, dome, and various types of oblique osteotomies. In most
cases, shortening, angulation, and malrotation must be corrected with a
single osteotomy. Closing-wedge osteotomies have the advantages of
simplicity and good stability. The disadvantages are that they result
in further shortening, and osteotomy site apposition is a problem when
correction of significant rotation is also required. Opening-wedge
osteotomies have the disadvantage of much less stability after fixation
and require structural bone grafting. Union is slower than with closing
wedge osteotomies, and remodeling of the graft is required. See Figure 30.13 for an illustration of open technique.
combination deformities, and the dome osteotomy for isolated varus or
valgus angulation in the metaphysis (33). An
oblique osteotomy has the advantages of excellent stability, broad bone
surfaces for union so that bone grafting is usually not required, and
correction of all components of the deformity. Disadvantages are that
considerable exposure of bone is required and meticulous preoperative
planning and surgical execution are necessary for it to work. In about
20 osteotomies in the distal femur, I have had one failure due to
nonunion, probably the result of overlengthening and devascularization
of the bone ends. The technique described next is an AO oblique
osteotomy for a supracondylar malunion (Fig. 30.14).
 |
|
Figure 30.14. A:
AP radiograph of a malunion of the distal third of the femur in a 26-year-old athlete with 13° of varus, 15° of external rotation, and 1.5 cm of shortening. B: Preoperative lateral radiograph. C: Tracing of the contralateral normal femur, and the osteotomy and fixation planned for the malunion. A 12-hole plate and at least two interfragmentary screws are planned for fixation. D: Lateral tracing of the contralateral normal femur and the planned correction for the malunion. Notice that the osteotomy is at 60° to the transverse axis of the femur, which permits sliding to gain length. (The wedge removed to correct the malrotation is not illustrated.) E: Intraoperative AP radiograph of the completed osteotomy. F: Lateral radiograph of the completed osteotomy. |
in most cases the former is better. Make tracings of the preoperative
radiographs to determine the angular deformity to be corrected. Use
clinical measurements to determine the amount of malrotation to be
corrected. Use both clinical and radiographic assessments to determine
the length to be corrected. Make a drawing of the proposed
postoperative construct with internal fixation in place (Fig. 30.14A, Fig. 30.14B, Fig. 30.14C and Fig. 30.14D).
-
Place the patient in the supine position on the operating table. Prepare and drape the extremity to be operated
P.968P.969
on. In distal osteotomies, a tourniquet can be used. It is often useful
to prepare and drape the contralateral normal extremity as well because
this permits intraoperative comparison. Be certain that the pelvis is
level so that leg-length determinations are accurate. -
Expose the distal femur through an anterolateral approach (see Chapter 3).
Place K-wires as guide pins in the proximal and distal segments. In the
frontal plane, insert one K-wire in the distal fragment parallel to the
knee joint. Insert a second wire into the proximal fragment at right
angles to the shaft of the femur. Verify correct position by
fluoroscopy or radiograph. Place a second set of K-wires in the
sagittal plane, entering the anterior aspect of the femur. These are
used to measure correction in the AP plane and can also be used to
ascertain rotation. Place the wires at right angles to the knee joint
distally and at right angles to the long axis of the femur in the
proximal fragment. Put them in direct alignment with each other
rotationally. Both of these sets of wires must be proximal and distal
to the osteotomy site. Measure the distance between the anterior
K-wires; this will be used to determine length. -
Through the middle of the fracture site
in the frontal plane, make an oblique osteotomy at 60° to the long axis
of the femur. Begin distally on the anterior surface of the femur and
exit posteriorly. Open the osteotomy site with bone-holding forceps or
retractors. Next, remove a wedge of bone from the distal fragment. The
base of the wedge will determine correction of rotation and any
deformity in flexion or extension. Experienced surgeons can remove this
with a single cut. Otherwise, take the wedge for correction of
deformity in the sagittal plane first and then take a side-based wedge
to correct rotation. Do not remove too large a wedge. It is better to
take too small a wedge initially and then have to cut further. Accurate
preoperative measurement, taking into account x-ray magnification, is
necessary. Approximate the osteotomy site and slide the distal and
proximal fragments against each other to correct varus or valgus
angulation. -
At this point, overall axial alignment of
the femur is corrected and only shortening remains. Apply a Lowman
bone-holding clamp or other bone-holding forceps to the osteotomy site
to hold it in loose apposition. Apply a femoral distractor and slowly
distract the osteotomy site to gain length. Keep the knee flexed and
use other precautions to avoid excessive traction on the sciatic nerve,
as described earlier in this chapter. Once enough length has been
obtained, temporarily fix the osteotomy site with two or three large
Steinmann pins. Carefully assess the correction clinically and
radiographically to ensure it is adequate. -
Begin internal fixation by inserting two
or three anterior-to-posterior interfragmentary lag screws (either 6.5
mm cancellous screws or cortical screws with gliding holes). Fixation
depends on the location of the osteotomy and bone quality. The
osteotomy will now be stable, which simplifies plate fixation. With an
osteotome or saw, remove excessive bone from the edges of the osteotomy
to restore the normal contours of the femur. Then apply a broad plate
on the lateral surface of the femur and obtain at least eight cortices
of screw fixation in both fragments (Fig. 30.14E, Fig. 30.14F).
If the osteotomy is very distal, a condylar blade plate or
distal-compression screw device may be necessary. Morcelize the bone
removed from shaping the femur and pack it about the osteotomy site. -
Release the tourniquet, if used, and secure hemostasis. Place two suction drains and close in the usual fashion.
patient is comfortable, remove the dressing and begin rehabilitation.
Continuous passive motion may be helpful in restoring knee motion.
During this period, progressive resistance exercises are possible as
long as the thigh is supported on the exercise table. Avoid excessive
weights. Because of the broad surfaces and intimate contact of the
osteotomy, union occurs rapidly. It may be difficult to document union
radiographically, however, because the osteotomy often appears healed
on the immediate postoperative film. Four routine views, as well as AP
and lateral tomograms, are often necessary to ascertain that union has
occurred. When it does occur, begin full weight bearing.
 |
|
Figure 30.15. Crescentic (dome) osteotomy. AP radiograph (A)
of the right knee of a 42-year-old woman who has had moderately severe genu valgum since she was a child. She was having significant lateral compartment pain that interfered with her activities of daily living. Bilateral radiographs showed moderately advanced arthritis of the lateral compartment. She was treated with bilateral dome osteotomies; this shows the right side. The black vertical line on the lateral aspect of this radiograph shows the mechanical axis between the center of the femoral head and the center of the ankle joint, which here lies completely lateral to the joint. Note the tibial femoral angle of 16° of valgus. AP (B) and lateral (C) radiographs taken at the time of surgery show a dome osteotomy in the distal femur with excellent correction of her deformity and restoration of the mechanical axis to slightly medial of normal in order to unload her lateral compartment. Note that the “cog wheel” edges of the osteotomy are impacted and the osteotomy fixed with two interfragmentary screws through a lateral plate. If any micromotion exists in the osteotomy after this fixation, a small anterior plate can be added as well. AP (D) and lateral (E) radiographs taken after hardware removal approximately 2 years after the initial osteotomy show good maintenance of alignment and good preservation of the lateral joint space, with no evidence of progression of her arthritis. At the 8-year follow-up, she continues to do well with some evidence of progression of her arthritis. A similar osteotomy was done of the opposite leg with an equally good result. |
-
In the preoperative planning, be certain
that a dome osteotomy will restore the normal mechanical axis of the
knee, or if treating unilateral arthrosis that it will result in an
appropriate shift of the mechanical axis. -
Use a direct anterior midline incision by
either an anteromedial or anterolateral approach depending on the
deformity to be corrected and the fixation planned. -
Perform the dome osteotomy using multiple drill points and an osteotome as described in Chapter 26.
Make the osteotomy as distal as possible because this provides a larger
area for the arc of the dome, which is technically easier and provides
a broader surface area for union. Be certain to leave enough length in
the distal fragment so that solid internal fixation with a lateral
plate providing three bicortical screws of fixation in the distal
fragment is possible. -
After completing the osteotomy, correct
the deformity, impact the osteotomy, and secure initial fixation with
one or two interfragmentary screws across the osteotnomy.
P.970
Apply a broad plate laterally to provide neutralization, securing bicortical fixation with three screws distally and proximally. -
Prior to closure, repeat mechanical axis
determination with the fluoroscope to be certain that the goals of the
osteotomy have been met. -
Do a meticulous closure of the joint
capsule and muscle, and apply a sterile dressing and knee immobilizer.
Drain the knee and osteotomy site.
first postoperative day. As soon as the drain is removed, begin knee
range-of-motion and muscle rehabilitation exercises. These osteotomies
are very stable and most patients can begin 50% weight bearing with
assistive devices using a knee immobilizer immediately. Until the
osteotomy heals, avoid straight-leg raising and excessive stress across
the osteotomy site. Healing usually occurs in 6–8 weeks, at which time
progression to full weight bearing without assistive devices and afull
rehabilitation program can be instituted (Fig. 30.15A, Fig. 30.15B, Fig. 30.15C and Fig. 30.15D).
condyles is difficult. It is best to identify malposition early and
correct the deformity before remodeling takes place. Once remodeling
has occurred, it becomes exceedingly difficult to realign the articular
surfaces of the knee joint. Malunions of epiphyseal fractures in
children involving the condyles are even more difficult because the
malunion may be accompanied by growth arrest, and corrective osteotomy
often threatens the integrity of the physis. Specialized techniques are
necessary in children (see Chapter 168, Chapter 169, and Chapter 171).
in valgus, external rotation, and flexion deformity. Malunion of the
medial condyle produces a similar deformity, but in varus. Most
disabling is the malrotation that interferes with the articular surface
of the patellar groove and produces malalignment of the patellar
mechanism. Comminuted fractures with a transverse component produce a
step-off in the articular surface that can interfere with patellar or
tibial motion on the femur. Although patients can walk fairly well with
the knee straight, function is impaired in flexion and during sports
activities.
articular surface is very difficult, and the amount of soft-tissue
stripping of the fragments necessary to restore them to proper position
risks avascular necrosis. Surgical techniques for medial and lateral
condyles are similar.
-
Place the patient in a supine position on
the operating table and prepare and drape the entire extremity. As
recommended previously, it may be advisable to drape the normal
extremity as well for comparison. A tourniquet can be used. -
Use an anteromedial or anterolateral
parapatellar incision long enough so that the articular surfaces of the
femur can be easily seen and complete access to the fracture site
gained. To achieve good alignment, it is often necessary to dislocate
the patella. -
Maintain the soft-tissue attachments of
the collateral ligaments, and as much joint capsule as possible, as
well as the cruciate ligaments. In some distal femoral malunions, the
femoral artery and vein are fibrosed to the posterior aspect of the
femur. Dissect carefully in a subperiosteal manner along the posterior
aspect of the femur, staying intimately against bone to avoid injury to
the neurovascular structures. Keep the knee flexed
P.972P.973
to 90° during this dissection and when the osteotomy is made. -
Identify the fracture site at the
articular surface. With osteotomes, take down the malunion. Progress
from the articular surface proximalward, attempting to stay in the old
fracture site. A similar technique is used for transverse malunions. -
With the condyle mobile, restore the
alignment of the articular surface. Often this results in incongruity
in the osteotomy or fracture site and requires some carpentry to obtain
good alignment of the articular surface with good closure and
apposition of the fracture and osteotomy site. Most difficult to
correct is rotational malalignment. -
Achieve temporary fixation with K-wires
and obtain radiographs to ensure the correction is satisfactory.
Internally fix the osteotomy with three or more interfragmentary 6.5 mm
cancellous lag screws. In malunions, lag-screw fixation alone often is
inadequate, and adding a plate to buttress the malunion is important. -
When closing, ensure that the patella is
in good alignment. Use suction drains and apply a bulky soft dressing
with splints. A typical case is illustrated in Fig. 30.16![]() Figure 30.16. A:
Figure 30.16. A:
AP radiograph of the left knee in a 28-year-old man with a healed
fracture of the lateral tibial plateau and an intra-articular malunion
of the lateral femoral condyle. B: Lateral radiograph showing a 15 mm offset in the articular surface of the lateral condyle of the femur due to the malunion. C:
The malunion was taken down through the old fracture site with an
osteotome inserted from the articular surface. This radiograph taken 2
years after repair shows fixation with interfragmentary screws and a
buttress plate. A bone graft was not necessary. D:
Lateral view at 2-year follow-up. The articular surface is nearly
anatomic. At 7-year follow-up, the patient was doing well and
radiographs showed no degenerative changes.
and bulky dressing, and begin rehabilitation using continuous passive
motion. With solid internal fixation, an active rehabilitation program
is possible. Keep the patient on touch-down weight bearing until union
occurs. Again, multiplane radiographs and tomography may be necessary
to confirm union.
changes in the knee that arthrodesis may be a better choice.
Arthrodesis of the knee is so disabling, however, that I usually advise
correction of the deformity followed by total knee arthroplasty.
due to nonoperative treatment of widely displaced fractures or failure
of fixation, particularly as a result of infection. Treatment is
unnecessary unless the patient has symptoms. A fibrous union can have
acceptable function with minimal symptoms. Klassen and Trousdale (28)
treated 20 patients with patellar nonunions, of whom seven were treated
nonoperatively. They achieved an average knee range of motion of 120°
with a Knee Society score of 83 with a function score of 75. Pain, lack
of knee stability, or mechanical problems may require surgical
treatment. Therapeutic choices are total patellectomy, partial
patellectomy with repair of the quadriceps mechanism, or reconstruction
of the patella. In nonunions, it is difficult to correct the
irregularities in the patellar articular surface, so some type of
patellectomy is generally indicated. Reconstruction uses the same
principles of fixation and resection as described for patellar
fractures in Chapter 22. Use compression screw
fixation and a tension band wire. Bone graft is rarely necessary or
possible, but a sliding inlay graft can be used in some cases. Of the
13 patients Klassen and Trousdale (28) treated
operatively, all but one healed, achieving Knee Society scores of 94, a
function score of 93, and an average knee range of motion of 109°.
articular surface. As with condylar fractures, correction is possible
but difficult. Joint-surface irregularity often persists. Total or
partial patellectomy may be the best choice. In active patients,
preservation of the patella is worthwhile, but do not allow persistent
incongruity of the articular surface to precipitate patellofemoral
arthritis or perhaps generalized arthritis in the knee.
-
The surgical technique is similar to that described for femoral condyle malunions. Use a long, medial parapatellar approach.
-
Invert the patella. Take down the malunion with osteotomes, working from the articular surface.
-
Realign the patella. Obtain solid fixation with interfragmentary lag screws and a tension band wire.
passive motion and active assisted exercises. Judicious isometric
muscle exercises are beneficial. Avoid straight-leg raising. Permit
weight bearing with a knee immobilizer. Union will occur in 6–12 weeks.
Thereafter, institute a full rehabilitation program and allow gradual
return to normal activities.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
AR, Shorkey RL. Blade-Plate Fixation in Nonunion and in Complicated
Fractures of the Supracondylar Region of the Femur. J Bone Joint Surg Am 1949;31:312.
A, Silva R, Massaferro J, Dubra A. The AO Tubular External Fixator in
the Treatment of Open Fractures and Infected Nonunions of the Shaft of
the Femur. Injury 1988;19:415.
MS Jr, Nebel E, Bailey RW. Transarticular Fixation in the Treatment of
Nonunion of Supracondylar Fractures of the Femur: A Salvage Procedure. J Bone Joint Surg Am 1979;61:1018.
PK, Naranja RJ, Heppenstall RB, et al. Results of Treatment of 111
Patients with Nonunion of Femoral Shaft Fractures. Univ Penn Orthop J 1999;12:56.
HB, Lipinski SW, Wiley JH. Observations on Nonunion of the Shafts of
the Long Bones, with a Statistical Analysis of 842 Patients. J Bone Joint Surg Am 1961;43:159.
JL Jr, Brighton CT, Heppenstall RB, et al. Technetium and Gallium
Scintigraphic Evaluation of Patients with Long Bone Fracture Nonunion. Orthop Clin North Am 1984;15:125.
D. Closed Shortening of the Femoral Shaft. Presented at the 39th annual
meeting of the Association of Bone and Joint Surgeons, Charleston,
South Carolina, 1987.
EL, Hak DJ, Johnson EE, Eckardt JJ. Total Knee Replacement Including a
Modular Distal Femoral Component in Elderly Patients with Acute
Fracture or Nonunion. J Orthop Trauma 1995;9:231.
DJ, Lee SS, Goulet JA. The Success of Exchanged Reamed Intramedullary
Nailing for Femoral Shaft Nonunions. Presented to the Orthopaedic
Trauma Association, Vancouver, BC, Canada, October, 1998.
EE, Urist MR, Finerman GA. Bone Morphogenetic Protein Augmentation
Grafting of Resistant Femoral Nonunions. A Preliminary Report. Clin Orthop 1988;230:257.
JL, Ratcliffe SS, Weber JK, Hansen ST Jr. Corrective Osteotomy of
Femoral Shaft Malunion Causing Complete Occlusion of the Superficial
Femoral Artery: A Case Report. J Bone Joint Surg Am 1980;62:303.
TM, Monroe MT, Mast JW. The Use of Endosteal Substitution in the
Treatment of Recalcitrant Nonunions of the Femur: Report of Seven
Cases. J Orthop Trauma 1996;10:1.
DB. Treatment of Ununited Fractures by Onlay Bone Grafts without Screw
or Tie Fixation and without Breaking Down on the Fibrous Union. J Bone Joint Surg 1947;29:946.
MJ, Hakanson R, Stover M, et al. The Failure of Reamed Intramedullary
Exchange Nailing for Aseptic Ununited Femoral Shaft Fractures.
Presented to the Orthopaedic Trauma Association, Louisville, KY,
October, 1997.