NONUNIONS AND MALUNIONS OF THE HIP
II – FRACTURES, DISLOCATIONS, NONUNIONS, AND MALUNIONS > Malunions
and Nonunions > CHAPTER 29 – NONUNIONS AND MALUNIONS OF THE HIP
what is necessary to achieve union in the femoral neck, most recent
series continue to report an incidence of avascular necrosis that
ranges from 20% to 25% and about a 10% rate of nonunion (4,7,8,14,16,17,18,19 and 20,28).
These statistics show that union is possible in the presence of
avascular necrosis. The live bone from the femoral neck can grow into
the avascular bone of the femoral head or, in some cases, partial union
may occur between viable sections of the femoral head and the neck.
When union to an avascular femoral head occurs, complications generally
do not develop until resorption of the avascular bone in the head
occurs, resulting in segmental collapse (11).
nonunion of the femoral neck is loss of blood supply to the femoral
head. In developing countries, neglect of these fractures is common and
leads to nonunion in most cases. Disruption of the blood supply is most
likely to occur when the fracture displaces, resulting in tearing of
the vessels; consequently, there is an increased incidence of avascular
necrosis in displaced fractures (8). The
incidence of avascular necrosis and nonunion is increased in young
adults, probably because a greater force is required to break the
femoral neck in this population. The greater force leads to increased
displacement, which correlates with avascularity. Avascular necrosis is
common, occurring in 20% to 25% of all femoral neck fractures; its
incidence is greater with poor reduction (52%) and in young patients
(90%) (13,19,29).
A high index of suspicion for an avascular head should be accorded
patients with marked shortening of the femoral neck after surgery.
High-risk patients include those who have undergone pelvic irradiation
therapy, those with alcoholism, and those receiving large-dose
steroidal therapy. Patients with a great deal of initial displacement
may do well, and displacement at injury should not be used as the sole
reason for prosthetic replacement. Delay in treatment is associated
with avascular necrosis; the incidence is nearly 100% after a delay of
7 days.
pressure secondary to a hematoma may occlude the blood supply, leading
to avascular necrosis (30,31).
Currently, only two steps can be taken to improve the blood supply to
the fracture site and head immediately after injury. First, obtain a
reasonably good reduction by closed means as soon as possible to
minimize distortion of the vessels. Second, decompress the
intracapsular hematoma, either by aspirating the hip joint or by
incising the capsule at the time of internal fixation.
has been disrupted by a fracture, recent efforts have been aimed at
diagnosing avascularity early so as to permit either revascularization
of the head or, in older patients, immediate hemiarthroplasty (30).
of nonunion are inaccurate reduction and loss of fixation secondary to
inadequate technique or poor bone quality. In most displaced femoral
neck fractures, the fracture angulates into a varus position and the
head collapses posteriorly (5). This results in
posterior comminution of the femoral neck with loss of bone substance.
Medial comminution of the calcar femorale does not occur often;
however, the calcar may impact into the femoral head, crushing
cancellous bone there. When major displacement disrupts soft tissues,
reduction and maintenance of position can be extremely difficult. With
the posterior bone deficit, malposition is common. When this is
combined with severe osteoporosis, internal fixation is difficult. For
this reason, the standard of practice for displaced fractures of the
femoral neck (Garden type III or IV) in the elderly is immediate
hemiarthroplasty (4,6,22,32).
fixation usually has delayed union with motion at the fracture site and
loosening of the fixation. Pain from the fixation device itself is
highly unusual, unless it is prominent at the hip, producing a
trochanteric bursitis. Removal of the internal fixation device at this
time causes instability, loss of position, and nonunion. With
displacement, nonunion is fairly easy to diagnose by routine
radiographs. In undisplaced fractures, nonunion can be very difficult
to diagnose, particularly when a great deal of fixation hardware is
present. In obese and elderly patients, soft-tissue density and bone
porosis may make roentgenograms difficult to interpret. In addition,
overlap of bone secondary to settling at the fracture site can suggest
union when, in fact, a nonunion is present. The preoperative workup
must establish whether union is present and whether the head is
avascular.
with reconstruction or anteroposterior (AP) tomograms of the femoral
neck. The cuts must be spaced closely, must extend through the entire
femoral neck region, and must be taken with the hip in internal
rotation to place the femoral neck into maximum profile. Fluoroscopic
examination of the fracture site while oscillating it through 5° to 10°
of rotation or varus–valgus positioning may also reveal instability at
the fracture site. We have not found arthrography to be helpful in
diagnosing nonunion. Magnetic resonance imaging (MRI) is very sensitive
for detecting avascular necrosis and is very helpful in the diagnosis
of nonunions, particularly in cancellous bone.
fracture line on radiography, increasing displacement of the fracture,
any varus position, or any angulation of the femoral head of greater
than 20° in relationship to the neck indicates impending failure. Each
of these suggests a fracture that is not likely to heal and is an
indication for operative intervention. Because their prognosis is
otherwise good, this applies particularly to fractures that are
initially minimally displaced (Garden type I or II) and that have been
reduced incompletely or fixed insecurely.
to the femoral head before undertaking reconstruction. The viability of
the femoral head is best determined by technetium-99m sulfur colloid
bone scans (21). However, false-positive uptake
of contrast material may be seen after 1 month, as blood from the
creeping substitution process may be present, but on a scaffold of
necrotic bone so extensive as to be doomed to collapse. Although an MRI
scan is more reliable than a bone scan in determining whether the head
is viable and suitable for reconstruction, it cannot be used if there
is metallic fixation in the head unless the software can subtract the
artifacts from the fixation devices.
contemplated should undergo a sedimentation rate study, a joint
aspiration culture, and, if the latter is suspicious, a gallium
radioisotope study to rule out a septic process. In questionable cases
involving an elevated sedimentation rate, leukocytosis on joint
aspiration, or a positive gallium scan, an open biopsy and culture may
be necessary.
there is a halo about the fixation device—operative intervention is
indicated, as further nonoperative care is unlikely to lead to fracture
union. Not only does delay prolong the healing period, but nail
penetration may destroy bone stock, blood supply, or acetabular
cartilage, preventing reconstruction. On the other hand, if the
radiographs are suggestive of delayed union or nonunion but the
fracture appears to be stable, well aligned, and well fixed continued
treatment with touch-down weight bearing on crutches may lead to
eventual union. If union does not
occur
within 6 months, a nonunion is likely. In young adults, avascularity of
the head with an impending nonunion may precipitate a decision for
early surgery. A muscle-pedicle bone graft may be considered in an
effort to revascularize the head if there is no segmental collapse of
the femoral head and no bone stock loss that would make stable fixation
unlikely (16,17,18,19,20 and 21). In the elderly, however, if the fracture is stable, it is best to wait, as a satisfactory clinical outcome may be achieved.
the patient’s physical condition, the status of the femoral neck,
degenerative changes in the hip joint, and the duration of the
nonunion. In sedentary patients who are elderly or disabled and who are
high-risk surgical candidates, it may be best to continue nonoperative
care, using assistive devices for walking and appropriate analgesics.
Disabling pain or deformity usually warrants surgery. Avascular
necrosis in the femoral head substantially lowers the likelihood of
success with internal fixation and bone grafting. In young, active
patients, it is worthwhile to try to salvage the femoral head. Elderly
patients, or those who cannot protect the injured hip because of
Parkinson’s disease, neurotrophic arthropathy, or other disabilities,
should be considered for a prosthesis. Prosthetic replacement is
indicated in patients who have less than a 15-year life expectancy and
who are not progressing normally after conventional techniques of
reduction and fixation. The operative timing of the hip replacement is
not as urgent as that of the reconstructive procedures, but if the gait
is unsatisfactory or if penetration of the metallic devices is likely,
which would cause additional destruction of the acetabulum, try to save
the acetabular surface.
walking with an unstable nonunion, crushing and resorption of the
femoral neck may occur. Loss of the femoral neck normally makes
internal fixation and bone grafting impossible. Once a nonunion is
diagnosed, it is important to move ahead with surgery to avoid
resorption of the femoral neck.
decision-making process. Longstanding nonunions are likely to be
associated with resorption of the femoral neck or associated
degenerative changes in the hip, and this must be taken into account.
by valgus osteotomy, internal fixation and bone graft, prosthetic
replacement, Girdlestone resection, or hip arthrodesis. Preserving the
femoral head is the primary consideration for younger patients (under
60 years old), very active patients, and obese patients (weighing more
than 200 pounds), all of whom have poorer long-term results with total
hip arthroplasty.
weight-bearing line medially and, most importantly, to place the
fracture plane more horizontally to reduce the shear stress on the
fracture (1,2). The
procedure is most successful when the fracture is undisplaced, when
there is no femoral neck resorption, and when the femoral head is
viable. An osteotomy can also be useful when the fracture line is
vertical and resistant to valgus reduction, as may occur in
high-velocity trauma. If healing has progressed but loss of leg length
and hip mechanics secondary to varus positioning is a problem,
osteotomy is indicated.
fracture, the asymmetric forces exerted on the femoral head and neck
lead to increasing displacement. Such a reduction is unacceptable. The
angulated fracture may be remanipulated and renailed if it is detected
within a few weeks of injury and the deformity is mild. If it is
detected later, at the time of initial healing, or if it is accompanied
by a severe deformity, a change in position will require force, or
dissection that is likely to interrupt the blood supply. These delayed
cases are more safely treated with an osteotomy. Since the procedure is
performed in the intertrochanteric region, the risk of avascular
necrosis is minimal.
the head and neck are placed in extreme valgus (greater than 150°), is
that the trochanteric lever arm is shortened. A greater abductor pull
is then required to counterbalance the body weight during the
single-leg stance phase. If the abductors are weak, a Trendelenburg
gait will result. If they are strong enough to avoid a Trendelenburg
gait, pressure on the femoral head will be increased, possibly leading
to early degeneration of the cartilage. For these reasons, the patient
may need to use a cane permanently. There is usually enough neck
resorption and shortening accompanying nonunion of the femoral neck for
the valgus osteotomy to compensate and for leg length to remain
relatively normal. Warn the patient, however, that a discrepancy in leg
length—either too long or too short—may be a permanent outcome.
occur after osteotomy, external immobilization is impractical.
Therefore, rigid internal fixation is essential so that the patient can
start touch-down weight bearing using crutches immediately after
surgery.
there are four types of valgus-transposition osteotomies: valgus
intertrochanteric wedge osteotomy, valgus wedge prop osteotomy, valgus
Y-shaped prop os- teotomy, and a variation described by Müller (Fig. 29.1, Fig. 29.2, Fig. 29.3 and Fig. 29.4). Weber and Cech (33) provide an exhaustive discussion of the treatment of femoral nonunion by osteotomy
in their excellent text. The most common osteotomy used is the valgus
intertrochanteric wedge osteotomy, the procedure for which is described
in the following section.
 |
|
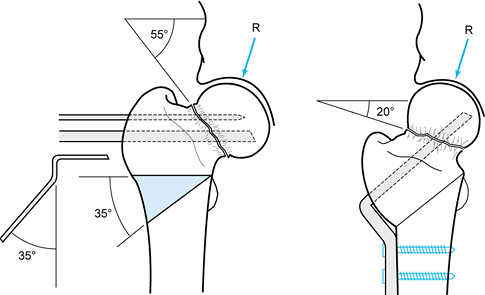
Figure 29.1.
A valgus intertrochanteric wedge osteotomy is performed to treat a nonunion of the femoral neck with a shear angle of 55°. A 35°, laterally based wedge is removed to place the nonunion 20° off horizontal. (From Weber BG, Cech O. Pseudoarthrosis. Bern: Hans Huber, 1976, with permission.) |
 |
|
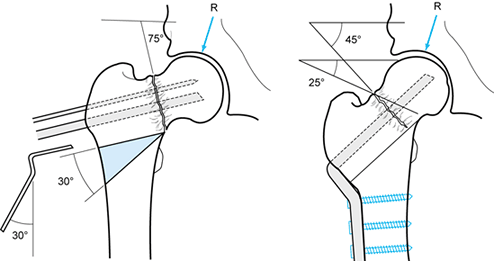
Figure 29.2.
A valgus wedge prop osteotomy is indicated when the fracture is nearly vertical, when there is minimal varus deformity, and when the femoral neck is fairly long. A 30° wedge is removed, reducing the fracture angle of 75° to 45°. This restores the normal anatomy of the neck–shaft angle. A 130° plate is then used to offset the shaft medially. This slides the distal femur beneath the femoral neck to support the nonunion site. (From Weber BG, Cech O. Pseudoarthrosis. Bern: Hans Huber, 1976, with permission.) |
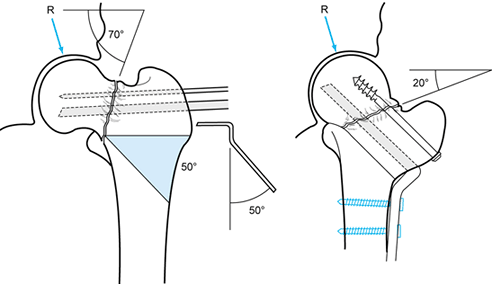 |
|
Figure 29.3.
A valgus Y-shaped prop osteotomy is indicated when there is significant varus deformity. This osteotomy can correct severe deformities with a valgus inclination of up to 70°. In this case, the nonunion is at a 70° angle, so a 50° wedge with its medial apex located at the fracture site is removed. A 50° blade plate is used. The lower cut of the osteotomy is placed to preserve the remnants of the calcar femorale. After correction and fixation, the nonunion is at 20°, the shaft is medially displaced, and the fracture site is supported by the medial shaft. Additional screws can be added to improve fixation. (From Weber BG, Cech O. Pseudoarthrosis. Bern: Hans Huber, 1976, with permission.) |
 |
|
Figure 29.4.
Transposition osteotomy, as described by Müller, permits correction of severe varus deformity with inferior subsidence of the femoral head. The femoral neck and head in this example are 30° below horizontal, and therefore in 65° to 70° of varus. To correct this, a 70°, laterally based wedge is removed. Note that the proximal cut preserves the remaining calcar femorale on the distal fragment, as does the inferior cut. Careful preoperative planning is necessary to make this osteotomy match up as well as the one depicted here. After repositioning, the fracture line is within 20° of horizontal, and the shaft supports the fracture site and is medially displaced. (From Weber BG, Cech O. Pseudoarthrosis. Bern: Hans Huber, 1976, with permission.) |
ensure that the head of the femur moves freely within the acetabulum.
If it does not, arthrotomy and lysis of adhesions may be necessary
before acceptable motion is achieved. A fibrous ankylosis of the hip is
usually accompanied by degradation of the articular cartilage, and it
may be a contraindication for osteotomy. The goal of the osteotomy is
to place the femoral neck fracture at an angle 20° to 30° off
horizontal (Fig. 29.1). Preoperative planning
must include a determination of the size of the bone wedge to be
removed, the position of the seating chisel (which will determine the
position of the blade plate in the proximal fragment), and the size and
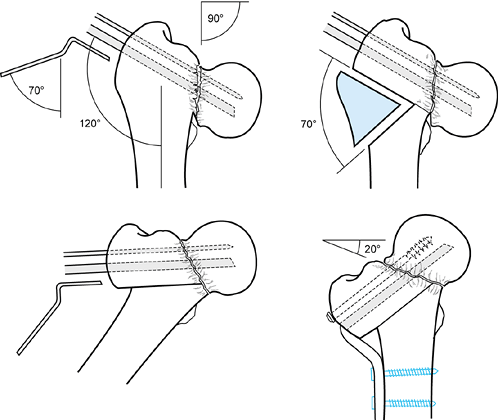
angle of the blade plate to be used (Fig. 29.5A, Fig. 29.5B, Fig. 29.5C, Fig. 29.5D, Fig. 29.5E and Fig. 29.5F).
 |
|
Figure 29.5. A:
This 42-year-old man sustained a femoral neck fracture in a bicycle accident. Note the high shear angle. Initial treatment was closed reduction and percutaneous multiple screw fixation in excellent position. This AP radiograph shows the hip at 2 months after surgery. B: Lateral view 2 months after surgery. C: AP radiograph at 8 months after fracture showing a nonunion with shortening and varus position. D: Preoperative planning drawing showing a reduction in the fracture angle from 60° to 30° off horizontal and a projected gain in length of 13 mm. E: Guide pin in place with 4.5 mm drill inserted through a triple drill sleeve to create a track for the chisel. F: Seating chisel in place. G: This 120° angled blade plate is in place with an independent 6.5 mm cancellous lag screw to gain further stability at the fracture site, as well as to compress it. Note the 4.5 mm cortical screw inserted through the impaction hole in the blade plate to secure the position of the blade. Place this after inserting the 6.5 mm lag screw. The illustration shows the location of the transverse osteotomy and the 30° wedge to be removed. H: Immediate postoperative AP radiograph. I: Immediate postoperative lateral radiograph. J: AP radiograph at 18-month follow-up showing union of the osteotomy and the fracture with no evidence of avascular necrosis or arthritis so far. K: Lateral radiograph at 18 months after osteotomy. |
best radiologic control but is technically difficult. I prefer to place
the patient in a semisupine position on a regular operating table (with
bolsters to raise the operative site about 25° to 30°), or in the full
lateral decubitus position. Use a Watson-Jones anterolateral approach.
Obtain good exposure of the femoral head, neck, and shaft. Do not
disturb the soft-tissue attachments to the femoral neck superiorly or
posteriorly, to avoid injuring the blood supply to the femoral head. In
Figure 29.5A, Figure 29.5B, Figure 29.5C, Figure 29.5D and Figure 29.5E,
the femoral neck is at an angle of 60° in relation to horizontal;
therefore, a 30° valgus osteotomy is performed to place the neck at a
30° angle to horizontal. Use an AO blade plate with an angle of 120°
between the blade and the shaft portions and an angle of 30° between
the shaft portion and the trochanteric bend in the plate. Perform the
osteotomy as follows:
-
Insert a guide pin through the lateral
aspect of the greater trochanter, across the femoral neck, and into the
femoral head just proximal to where the blade plate will be inserted.
This must be parallel to the superior cut of the osteotomy and on the
lateral view must be in the center of the femoral head. Obtain a full
lateral view of the hip by rotating it into the frog position, with the
hip flexed to 90° and with the C-arm fluoroscope in the cross-table
position (Fig. 29.5E). -
Use the triple guide and 4.5 mm drill
points to predrill the path for the seating chisel. This avoids
deflection of the chisel by intramedullary callus and/or the dense bone
around the nonunion. Drive the seating chisel parallel to and in line
with the guide pin in the position determined by preoperative planning
using fluoroscopic guidance. Most likely, it will enter somewhat
proximal to the ridge of origin of the vastus lateralis. Place it in
the inferior half of the femoral head. Determine
P.940
the proper blade length for the blade plate by measuring off the chisel (Fig. 29.5F). Withdraw the chisel and insert the blade plate (Fig. 29.5G). -
With a water-cooled oscillating saw, make
the proximal osteotomy cut parallel to the blade and just proximal to
the lesser trochanter, as determined by preoperative drawings (Fig. 29.5G). -
With a template or goniometer, mark a 30°
angle for the distal osteotomy and cut it with the oscillating saw,
removing the appropriate-size wedge of bone from the distal fragment.
Note that in this patient the wedge stops at the mid femur, so that as
the osteotomy is closed more length will be gained to compensate for
the shortening. -
Reduce the osteotomy into position, apply
longitudinal compression, and secure the side plate to the femur with
screws of an appropriate size. Morcelize or place the removed wedge as
a structural graft medially in the osteotomy site. If desired, perform
supplementary fixation of either the fracture or the osteotomy using
cancellous screws with washers to achieve interfragmentary compression (Fig. 29.5H, Fig. 29.5I, Fig. 29.5J and Fig. 29.5K). -
Obtain hemostasis, place suction drainage, and close the wound in the usual fashion.
Maintain touch-down weight bearing until union occurs, usually in 3–6
months. Teach the patient to support the leg when making transfers, and
to avoid straight-leg-raising exercises. Active and active-assisted
range-of-motion exercises for the hip and knee, as well as light
resistive exercises with the thigh and hip supported on a table
surface, are permitted. Once union occurs, unrestricted rehabilitation
is possible.
neck pseudarthroses, 41 of whom were treated with transposition
osteotomy. Of 23 osteotomies performed in patients with pseudarthroses
but without femoral head necrosis, 21 healed, 1 failed as a result of
infection, and 1 failed because of faulty technique. Fourteen of the
patients so treated achieved normal function; 7 had good results but
some shortening or diminished range of motion, and in 3 patients,
partial avascular necrosis of the head occurred, leading to a poor
outcome. In 7 of 13 patients with associated avascular necrosis,
healing and revascularization of the femoral head occurred, producing a
good result; the other 6 patients had poor results. The other 5
osteotomies were done in adolescents younger than 20 years of age. Of
these patients, 1 achieved a normal hip, 3 had a good result, and 1 had
a failure.
-
The location of the apex of the wedge
osteotomy on the AP view determines how much length will be regained
with the osteotomy. This can be predicted from the preoperative
drawings (e.g., the case in Fig. 29.5). Having
the apex of the osteotomy at the medial cortex is technically the
easiest and results in the largest surface contact between the proximal
and distal fragments, thereby reducing the risk of nonunion. As the
apex is moved laterally, more length is gained but less surface contact
is available between the head/neck and shaft fragments. When the apex
is in the medial half, there is a tendency for the fragments to impact
when compressed, but if the apex is in the lateral half, a gap is left
medially, and it is important to fill this gap with a structural bone
graft. -
I observed Dr. David Helfet perform this
procedure at the Hospital for Special Surgery in New York. His
technique is quite attractive. He places the patient on a fracture
table and makes only a lateral approach, not exposing the hip. He
inserts the blade plate and performs the osteotomy in a similar manner
but often does not remove a wedge. Instead he simply forces the side
plate down to the shaft and then impacts the osteotomy. This impales
the distal fragment into the soft cancellous bone of the proximal
fragment, resulting in excellent correction and providing excellent
bone apposition. The only disadvantage of this technique is that it
does not allow for sliding of the osteotomy to provide support across
the fracture site (Fig. 29.2, Fig. 29.3 and Fig. 29.4).
In addition, the relationship between the fragments at the osteotomy
may not allow protrusion of the distal into the proximal fragment. -
When compression is applied across the
osteotomy site with the external compressor, there is a tendency for
the shaft to shift medially away from the plate, and for the blade
plate to pull out of the proximal fragment. I avoid this by placing a
4.5 mm corti- cal bone screw of appropriate length through the
compression hole just beneath the blade, which secures the blade into
the femoral head. I keep a Lowman bone-holding forceps on the plate on
the shaft to prevent the shaft from shifting away from the plate. -
In nonunions, it is always wise to
supplement fixation with an independent cancellous leg screw and washer
just superior to the blade plate. -
This procedure works best if the blade
plate is placed in the inferior half of the head. Be certain that the
square corner of the blade plate does not penetrate the femoral head.
After insertion, examine the femoral head under direct fluoroscopy,
rotating the hip to be certain accidental penetration has not occurred. -
Absorption of the femoral neck with
shortening, or drift of the femoral neck into a severe varus or
inferior position, requires modifications (Fig. 29.2, Fig. 29.3 and Fig. 29.4).
nonunions of the femoral neck treated by abduction intertrochanteric
osteotomy. Their union rate was 94%. At 7.1 years follow-up, 7 had
required prosthetic replacement—the result of persistent nonunion in 3,
fixation failure in 1, and avascular necrosis in 3.
and popularized for the treatment of fresh fractures when there is
extensive posterior neck comminution and a high risk of avascular
necrosis. It is also useful in cases of nonunion. Although the
technique is best suited for nonunion without significant displacement,
we have successfully used it for displaced nonunion by repositioning
the fracture through the old fracture site. Open reduction with a
pedicle graft or other graft (26) may be
necessary when a true synovial pseudarthrosis is present, or when there
is severe loss of bone substance posteriorly with substantial
retroversion of the head.
supine position on a fracture table with the limb in traction. Although
this works well, I have found it to be much more convenient if the
patient is placed in the lateral decubitus position with the leg draped
free.
-
Use a posterolateral approach to the hip (see Chapter 3).
Distortion of anatomy as a result of shortening may displace the
sciatic nerve into an unexpected position. Identify the nerve and
protect it throughout the procedure. If the nerve must be retracted for
exposure, keep the hip extended and the knee flexed to avoid putting
tension on the nerve. Consider using somatosensory evoked potentials to
monitor sciatic nerve function. -
Dissect the hip external rotator muscles,
except the quadratus femoris, free from the underlying joint capsule
with a Cobb elevator, and transect them at a bony level from the
greater trochanter. Take care not to injure the underlying lateral
epiphyseal vessels. Delineate the superior and inferior margins of the
quadratus femoris muscle. Free it from the underlying capsule and soft
tissues with a Cobb elevator, from its origin to insertion. The medial
circumflex femoral artery abuts the upper margin of the quadratus
femoris. As it is the source of the lateral epiphyseal vessels, avoid
injury to this vessel. -
With an osteotome, mark the margins of
the bone graft to be taken from the posterior ridge of the greater
trochanter with the quadratus femoris attached (Fig. 29.6).
To obtain a bone block of sufficient length, take the posterior margin
of the greater trochanter from its tip to 1.5 cm distal to the lower
edge of the insertion of the quadratus femoris. It is easiest to
outline this block with a 0.5-inch osteotome, cutting the
superiorposterior and inferior margins of the graft first. Pry the
osteotomy open. This delineates nicely the posterior cortex beneath the
quadratus femoris that needs to be cut. Cut this with the osteotome
extending from proximal to distal beneath the quadratus femoris. The
bone block should be at least 5.0–7.5 cm long, and 1.5–2.0 cm wide and
deep. The superior part of the bone should extend beyond the upper
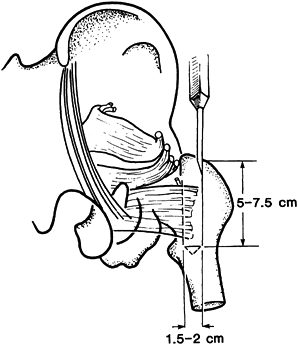
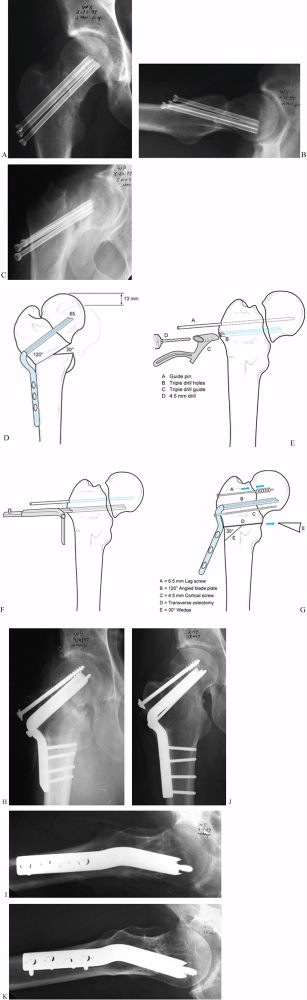
margin of the quadratus femoris by about 2 cm.![]() Figure 29.6.
Figure 29.6.
Meyers’s quadratus muscle pedicle bone graft. Remove the external
rotator tendons from the greater trochanter, taking care to avoid
injury to the medial femoral circumflex artery. Then harvest the bone
graft as is outlined with the attached quadratus muscle. -
Retract the bone graft and attached
quadratus femoris, freeing the underside of the muscle. Once mobilized,
it should easily swing superiorly to lie against the posterior aspect
of the femoral head and neck, without tension on the quadratus muscle. -
Incise the joint capsule using an H or T
pattern to expose the femoral neck, the site of nonunion, and the
posterior aspect of the femoral head. Identify the nonunion site and
remove all fibrous tissue. In longstanding nonunion, the bone surfaces
in the nonunion site may be quite sclerotic. If so, remove the
sclerotic bone with a curet. Drilling may be necessary as well. -
At this point, access to the fracture
site may be compromised by shortening and varus position. Achieve
reduction and anatomic position either by manual traction and
manipulation or by use of an AO femoral distractor with one Schanz pin
in the supra-acetabular area and the other in the greater trochanter.
The latter method is preferred. -
Fashion a site for the pedicle bone
graft. Using a curet, osteotome, or mortising chisel, make a hole in
the posterior aspect of the cancellous bone of the femoral head to
accept the proximal end of the bone graft. The hole should extend into
the femoral head at least 1–2 cm. Fashion the proximal end of the bone
graft so that it fits snugly into the hole, making certain that the
fracture is anatomically reduced and that there is good bone contact
anteriorly. Fashion the graft so that it fits snugly against the
posterior aspect of the femoral neck. If additional cancellous bone is
needed to pack the defect in the femoral neck, harvest a graft from
either the greater trochanter or the posterior ilium. Pack the
cancellous bone firmly into the defect in the femoral head so that
solid continuity between the head and neck fragments is achieved. -
In most cases, this step is followed by fixation of the femoral head and neck with three or four lag screws.
-
Finally, screw the pedicle graft into place (Fig. 29.7).
The order of placement of the screws depends on the stability of the
fracture. Verify the accuracy of the reduction and placement of the
fixation devices with the C-arm monitor.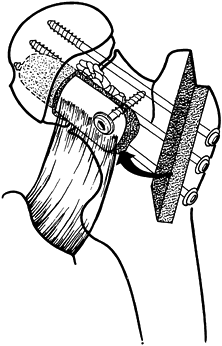 Figure 29.7.
Figure 29.7.
A completed Meyers’s quadratus pedicle bone graft. Note that the graft
is inserted into the posterior femoral head through a hole in the
posterior nonarticular aspect of the head. Secure the graft to the
distal femoral neck with a single bicortical screw. Overdrill the graft
to produce a lag effect. Use a washer on all screws. Pack cancellous
bone graft into remaining areas of bone defect. Then fix the fracture
with multiple cancellous screws. -
Close the hip joint capsule and reattach
the external rotators to the greater trochanter by suturing them to the
insertion of the gluteus medius. Place a suction drain and proceed with
routine closure.
intertrochanteric osteotomy. Full weight bearing must be delayed until
complete consolidation of the fracture occurs. In most cases, the
immediate postoperative radiographs appear to show union because of the
density of bone created by the bone-grafting procedure. An AP tomogram
or CT scan is often necessary to confirm that union has occurred. Figure 29.8 illustrates a typical case.
 |
|
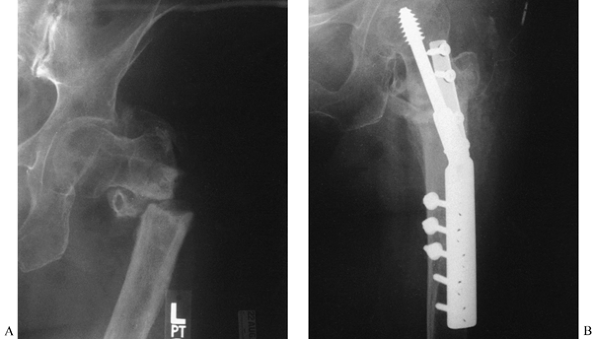
Figure 29.8. A:
Three months after intramedullary nailing of a femoral shaft fracture, a 39-year-old woman continued to have hip pain. This AP radiograph shows early healing of the shaft fracture but a nonunion with displacement of a femoral neck fracture. B: The lateral radiograph shows 90° of angulation in the fractured femoral neck. C: The intramedullary nail was removed and a Meyers’s pedicle bone graft combined with multiple screw fixation was performed. This AP radiograph 5 months after the graft shows union of the fracture. D: Lateral radiograph shows excellent restoration of alignment with union of the fracture. |
neck occur after internal fixation. In underdeveloped countries,
however, lack of access to medical care frequently results in neglected
fractures of the femoral neck in young adults going on to nonunion in
poor position. Nagi et al. (26) in India
treated 52 cases by open reduction, fixation by compression hip screw,
and a free fibular graft, at a mean of 5 months after the initial
fracture. Of 40 fractures available for evaluation at 59 months mean
follow-up, 38 were healed. Seven of 8 hips that showed avascular
necrosis before surgery revascularized without collapse, while 7 others
developed postoperative avascular necrosis. There were a considerable
number of later failures, including collapse of the femoral head in 5,
coxa vera in 11, fracture of the graft in 4, and penetration of the hip
by the screw or graft in 9. Of the 40 fractures, satisfactory
functional results were achieved in 35 and poor results in 5. I suspect
that a microvascularized graft will provide superior results to a
fibular graft, therefore in these cases, a Meyers’s pedicle graft or
free microvascularized fibular graft is worth consideration.
hemiarthroplasty or total hip arthroplasty—is limited to cases of
nonunion of the femoral neck that are not salvageable by osteotomy or
internal fixation and bone grafting (3).
Avascular necrosis with segmental collapse is the most common reason
for prosthetic replacement. Extensive resorption of the femoral neck,
making reconstruction impossible, is also an indication. In some cases,
even after successful union has been achieved, degenerative arthritis
may intervene, in which case arthroplasty would be indicated.
Hemiarthroplasty is adequate for hips without degenerative changes in
the acetabulum. Total hip arthroplasty is indicated when degenerative
changes are present in the acetabulum. The patient’s age and activity
level must be considered when determining whether to proceed with
arthroplasty or to perform a hip fusion. Arthroplasty is reserved for
patients who are physiologically older than 70 years of age, or in
younger patients whose lifestyle is sedentary. Young adults (those
physiologically younger than 50 years of age) who can continue to
participate in sports are better candidates for arthrodesis because of
the risk of prosthetic loosening. The techniques for hemiarthroplasty
and total hip arthroplasty are described in Chapter 105.
Because of the absence of the femoral head and neck, fusion is
difficult. The technique for fusion after removal of a total hip
prosthesis is applicable to this group as well. To maintain length,
ischiotrochanteric fusion may be necessary. Internal fixation of the
proximal femur into the old acetabulum, combined with subtrochanteric
osteotomy, is an alternative technique but usually results in
unacceptable shortening (see Chapter 109).
to treat, often because of multiple resistant organisms. The femoral
head is often totally avascular, and severe bone
stock
loss precludes arthrodesis or arthroplasty. Salvage by osteotomy or
bone grafting and internal fixation is rarely, if ever, possible. If
the fracture is superficially infected, debride all necrotic tissue and
place at the fracture site polymethylmethacrylate beads (not yet
approved by the U.S. Food and Drug Administration) containing an
appropriate antibiotic—usually 1.2 g of tobramycin and 1 g of
vancomycin in 10 g of bone cement. Close the wound, eliminating all the
dead space. Plan to internally fix when the patient’s wound heals,
usually within 3–4 weeks. Infection cannot be cleared if the nail
penetrates the hip, causing infection within the hip joint. The
presence of septic arthritis requires resection of the head and neck
fragment, insertion of antibiotic beads, and subsequent total hip
reconstruction. Final treatment involves removal of all internal
fixation hardware and necrotic bone, which usually leads to Girdlestone
resection of the hip. After debridement, leave the wound open and treat
with appropriate antibiotics. Secondary closure of the wound may be
possible, but often healing by secondary intention becomes necessary,
particularly when there is significant pelvic or acetabular involvement.
requires the use of a lift, and persistent instability nearly always
warrants the use of a cane or single crutch for ambulation. Subsequent
conversion to an arthrodesis is a consideration, but this is
technically difficult, and infection may recur.
can be manifested by a loss of fracture reduction, fracture of the
fixation device, varus collapse of the fracture, or pulling of the
screws from the shaft. Nails currently in use are strong at the
nail–plate junction; therefore, failures occur more often in bone than
in the plate.
by failure of fixation, with drifting of the fracture into a varus
position and external rotation. Normally, this leads to good apposition
of the bone fragments and union in malposition. The likelihood of
nonunion is increased when hardware interposition, major bone loss, or
excessive prolonged traction results in lack of good bone contact
across the fracture site.
patient to nonunion. Since infection can also cause the fixation device
to loosen, in any patient with an apparent nonunion, rule out infection
with a sedimentation rate, aspiration of the hip, wound culture, and if
necessary a biopsy of the fracture site.
intertrochanteric nonunion, as the former is the highest stress area of
the femur. Nonunion occurs after both operative and nonoperative
treatment. The overall incidence of nonunion in the trochanteric and
subtrochanteric region is about 1.5%. The most common cause of nonunion
after internal fixation of subtrochanteric fractures is the use of a
compression hip screw or blade plate device when the medial buttress is
not established and bone graft has not been used. Early activity causes
excessive bending motion of the unsupported plate, resulting in
mechanical failure and subsequent nonunion.
nonunion requires operative intervention. Externally applied or
semi-invasive methods of electrical stimulation are not indicated, as
the incidence of true synovial pseudarthrosis in subtrochanteric and
trochanteric nonunion is high, and the prolonged immobilization in a
spica cast that is required for electrical stimulation is unacceptable
if operative intervention is feasible.
unacceptable pain, unacceptable instability, or malposition that
interferes enough with function to justify operative intervention. In
sedentary or elderly patients in whom a stable, fibrous union has been
achieved without pain, surgery may not be necessary as long as the
malposition is acceptable. The treatment of intertrochanteric nonunion
and high (within 1 inch of the lesser trochanter) subtrochanteric
nonunion is nearly identical. Alternatives include AO condylar
blade-plate fixation, compression hip screw with or without anterior
plating, and intramedullary nails of the third-generation or
reconstruction type. Subtrochanteric nonunions are best treated with
intramedullary nails of the reconstruction type. The technique does not
differ much from that used for fresh fractures (see Chapter 19 and Chapter 20). A sample case is illustrated in Figure 29.9.
Contraindications to this approach include coexisting infection and
osteopenic bone that is incapable of providing good fixation.
 |
|
Figure 29.9. A:
AP radiograph of the femur of a 50-year-old man who was treated for a chondrosarcoma of the femur 9 months earlier. The tumor in the mid shaft was resected; the shaft was autoclaved and reconstructed. There is a nonunion at the subtrochanteric junction, with subsidence into varus. B: The postoperative radiograph shows reconstruction by replacement of the dead diaphysis with an allograft and fixation with an Alta rod connector using a dome in the hip. The graft junction sites were grafted with autologous bone. |
intertrochanteric or subtrochanteric nonunion can be performed on a
fracture table, I prefer to use a radiolucent operating table with the
patient in the lateral decubitus position. The purpose of the fracture
table is to use traction to correct the deformity; it also improves
radiographic control. However, the same goals can be met by using an AO
femoral distractor to correct malposition. A C-arm fluoroscope
placed over the top of the patient, using a frog-leg position for the lateral view, is sufficient for radiologic control.
-
Prepare the skin and drape the hip and affected lower extremity free.
-
Use a Watson-Jones exposure (see Chapter 3). Adequate anterolateral exposure of the femoral neck and the adjacent proximal shaft is essential.
-
If a fibrous nonunion is in good position, internal fixation in situ
is possible; otherwise, the nonunion must be taken down, the medullary
canal opened, and the fracture ends freshened. Correct shortening,
malrotation, and varus malformation using an AO femoral distractor if
necessary. A useful supplemental technique involves placing a hip screw
and side plate into correct position in the proximal fragment and then
reducing the proximal fragment, along with the side plate, to the shaft
of the femur. The AO outrigger compression device can be placed in
distraction to help gain length. -
If length of more than 15 mm is gained,
maintain the hip in extension and the knee in flexion to avoid
excessive traction on the sciatic nerve. Gaining more than 2.5 cm is
technically challenging, and in some cases preoperative traction may be
useful. In repositioning the fracture, try to reestablish medial
contact between the femoral head/neck and shaft fragments. If good
apposition is attained and interfragmentary screw fixation is possible,
an anterior plate may not be necessary. If the medial buttress is not
reestablished, place a medial bone graft and use an anterior plate. -
Once satisfactory position is achieved,
fix the fracture internally with an appropriate-size compression hip
screw with a side plate or other heavy-duty appliance. Screw fixation
in at least eight cortices of the distal fragment is necessary. Attain
interfragmentary screw fixation across the fragments if possible (Fig. 29.10).
In both intertrochanteric and subtrochanteric nonunions treated with a
hip screw, an anterior plate is useful. Use a 3.5 or 4.5 mm
reconstruction plate. With an intertrochanteric nonunion, the plate
must extend onto the base of the femoral neck, and proximal fixation
may have to be achieved with only two screws. In subtrochanteric
fractures, it is usually possible to place a six-hole plate with three
screws in each major fragment. Distally, the anterior plate should be
at least 2.5 cm short of the end
P.949
of the side plate to avoid a stress riser at the end of the plate![]() Figure 29.10. A:
Figure 29.10. A:
A 55-year-old woman 3 years after an intertrochanteric fracture of the
left hip. She was originally treated with a Smith-Peterson nail and
Thorton side plate. This was complicated by infection with a
penicillin-sensitive Staphylococcus aureus. Now she has painful nonunion with 1½-inch (3.75 cm) shortening. B:
This was treated with reduction, autologous bone graft, and double
plate fixation with a hip screw and semitubular plate. She healed and
regained her lost leg length and function. -
Harvest a copious bone graft from the posterior ilium and apply it to the nonunion site.
-
Place two deep suction drains and close
the wound in the usual fashion. Balanced suspension will make the
patient more comfortable in the immediate postoperative period.
weight of the leg with crutches or a walker. If good internal fixation
has been achieved, active-assisted joint range-of-motion exercises can
normally be started immediately. With the thigh supported, resistive
exercise to muscles is also possible. Delay straight-leg-raising and
resistive exercises across the hip joint until healing occurs.
immediate postoperative radiographs may show obliteration of the
fracture. The time of postoperative bone union can, therefore, be
difficult to judge. AP and lateral tomograms can be necessary to
confirm union. In any case, the minimal amount of time required for
union is 12 weeks; often 6 months is needed.
bone defect, a proximal femoral replacement total hip or hemiarthplasty
may be indicated. However, a prosthesis that preserves the trochanter
is preferred. Prosthetic replacement of trochanteric bone usually
results in poor muscle reattachment and consequent dislocation. The
type of prosthetic reconstruction to use is quite variable and depends
on many factors (see Chapter 105 and Chapter 106).
-
If there is marked osteoporosis in the
femoral head, supplemental fixation with methylmethacrylate may be
necessary. Make a nail track that does not enter the hip joint. Inject
cement into the nail track before replacing the device in the neck.
This procedure is, however, rarely necessary in fresh fractures treated
with a sliding nail that reaches the center of the head, near the
articular surface. If the purchase of screws in the femoral shaft is
inadequate, remove some of them, pack methylmethacrylate into the
medullary canal, let it set, and then drill and reinsert the screws. Do
not allow methylmethacrylate to enter the fracture site. Always use a
copious circumferential bone graft when methylmethacrylate is used.
trochanteric region is associated with varying degrees of varus and
shortening. External rotation is usually present as well, but
occasionally internal rotation occurs. It is important to correct these
deformities in children, as further shortening secondary to disuse may
occur if the deformity is not corrected and normal function restored.
Altered mechanics about the hip, which influence bone remodeling, may
contribute to further shortening. Most cases of malunion in this region
are treated with intertrochanteric or subtrochanteric osteotomy, using
techniques similar to those described in the section on nonunion. With
simple valgus osteotomy, it is easy to correct malrotation through the
osteotomy site. Correction of the varus position and malrotation will
also resolve a substantial amount of the shortening in most cases.
Further length can be gained by sliding an intertrochanteric or
subtrochanteric osteotomy, using the femoral distractor for distraction.
nerve, to attempt to gain more than 2.5 cm in leg length at the time of
surgery. Patients with leg-length discrepancies of more than 2.5 cm may
have residual shortening. A secondary procedure, to lengthen the
affected extremity or shorten the contralateral extremity, may
subsequently be necessary to equalize leg lengths.
disjunction between the femoral head/neck fragment and the shaft, it
may be necessary to take down the malunion, placing the patient either
in traction or in an external fixator to regain length before fixation.
Skeletal traction is preferred in most cases, as it is least invasive
and does involve placement of pin tracks in the hip region, which might
otherwise be a source of contamination with subsequent surgery.
axis for a subtrochanteric nonunion is an intramedullary nail. The
first choice is an interlocking or reconstruction nail (Fig. 29.9).
An advantage of nails is the closed reaming process that provides bone
graft to the fracture site and stimulates callus formation.
Additionally, the nail provides lasting protection at a time when the
partially avascular comminuted fragments are brittle and subject to
refracture.
subtrochanteric nonunion associated with a long, oblique fracture
surface that is suitable for lag-screw fixation. The bone must be in
good contact to carry compression forces. This oblique configuration
may be relatively unstable with intramedullary nailing and tends to
gap. Nail plates are also an alternative treatment for two-part
nonunion with a transverse component. Accurate reduction, restoration
of the medial buttress, and medial bone grafting are necessary. Limited
weight-bearing until union occurs is essential.
Comfort, who, prior to his untimely death, was a coauthor of this
chapter and a highly respected orthopaedic traumatologist.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
TD, Ferguson AB Jr. The Development of a Computational Stress Analysis
of the Femoral Head: Mapping Tensile, Compressive, and Shear Stress for
the Varus and Valgus Positions. J Bone Joint Surg Am 1978;60:619.
MH, Harvey JP Jr, Moore TM. Treatment of Displaced Subcapital and
Transcervical Fractures of the Femoral Neck by Muscle-Pedicle Bone
Graft and Internal Fixation. J Bone Joint Surg Am 1973;55:257.
MH, Harvey JP Jr, Moore TM. The Muscle-Pedicle Bone Graft in the
Treatment of Displaced Fractures of the Femoral Neck: Indications,
Operative Technique, and Results. Orthop Clin North Am 1974;5:779.
MH, Telfer N, Moore TM. Determination of the Vascularity of the Femoral
Head with Technetium-99m Sulfur Colloid: Diagnostic and Prognostic
Significance. J Bone Joint Surg Am 1977;59:658.
ON, Dhillon MS, Goni VG. Open Reduction, Internal Fixation, and Fibular
Autografting for Neglected Fracture of the Femoral Neck. J Bone Joint Surg Br 1998;80:798.
F. Der Schenkelhalsbruch ein Mechanisches Problem: Grundlagen d.
Heilungsvorganges, Prognose und Kausale Therapie. Beilageheft zor
Zeitschrift Für Orthopaedishe Chirogie, Ferdinand Enke, Stuttgart, 1935.