MISCELLANEOUS DISORDERS OF THE FOOT
the epiphysis of the metatarsal head, was first reported in six cases
in 1914 (3). It occurs in adolescence, mostly
affecting girls. The etiology is assumed to be traumatic insult causing
loss of vascularity. It usually involves the second metatarsal, and
less frequently the third and fourth. The second metatarsal head is
affected because it is the longest ray and is the least mobile, as it
is the keystone of the transverse arch of the foot.
There can be associated swelling and loss of motion. The pain
diminishes with rest and increases with activity. Physical examination
shows swelling, tenderness, and discomfort with movement of the joint.
If the osteophytes are large, they may be palpated.
of joint space and collapse of the metatarsal head in the late stage.
There can be new bone formed as the metatarsal attempts to heal.
Smillie’s classification is based on the anteroposterior and oblique
radiographs (20,21).
In stage I, there is a fissure fracture of the ischemic epiphysis; in
stage II, there is central depression of the head from bone resorption;
in stage III, there is further collapse of the head with residual
projections of the sides, and the plantar cartilage remains intact; in
stage IV, the plantar portion of articular cartilage separates into a
loose body; and stage V is the final stage, with arthritis, deformity,
and flattening of the metatarsal head (Fig. 119.1).
 |
|
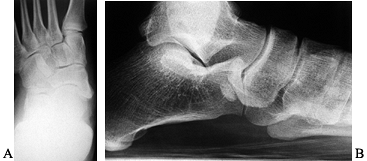
Figure 119.1. Radiograph showing the typical appearance of Freiberg’s infraction, with a large metatarsal head, flattening, and osteophytes.
|
radiographic appearance. In the early stages, cast immobilization for
4–6 weeks with protected weight bearing will decrease pain and
swelling. Later, pressure under the affected metatarsal head can be
reduced by a metatarsal pad, metatarsal bar, or a custom-molded
orthosis.
process begins, symptoms generally reduce. Sometimes the symptoms are
present after complete healing. There can be residual pain and loss of
motion from the bony prominence from the healed metatarsal head or the
presence of loose bodies. In these cases, surgery may be indicated.
treatment of symptomatic Freiberg’s infraction. These include
debridement, cheilectomy, osteotomy, resection arthroplasty, and
metatarsophalangeal joint implant (8,14).
joint may be helpful to remove the synovitis, loose bodies, nand
osteophytes. Excision of excess bone is indicated if the bony
prominence is symptomatic.
-
Make a dorsal hockey-stick incision over
the second metatarsophalangeal joint, and incise the extensor tendons
longitudinally to expose the joint. -
Perform a modified DuVries condylectomy (see Chapter 113).
-
Perform a synovectomy, and remove the excess bone of the metatarsal head.
-
Remove the dorsal one fourth to one third
of the metatarsal head with an osteotome, and use a rongeur to excise
any remaining sharp edges. -
Remove the medial and lateral osteophytes
to the level of the metatarsal diaphysis. Extend the second toe to 75°
to 80° to confirm that enough bone has been removed. -
Repair the extensor mechanism and the skin, and apply a firm compression dressing.
consider resection of the metatarsal head. This procedure is not
generally recommended because it will result in shortening of the toe,
possibly transferring pain to the third metatarsal head.
shoe. Remove the skin sutures at 2 weeks, and start the patient on
passive and active range-of-motion exercises. An ordinary store-bought
shoe may be worn once swelling has decreased. A metatarsal pad may be
helpful during the first few weeks after resection to decrease the
pressure under the metatarsal heads.
prior to the operative procedure and realistic expectations
established. The most common postoperative complaint is continuation of
some of the preoperative symptoms of pain and stiffness. Because the
metatarsal head is involved, it is likely that some pain and stiffness
will persist that may require shoewear modifications or possibly a
secondary procedure.
other possible complications. These may be prevented by limiting the
amount of resection, and by limiting motion of the toe for 3 weeks with
a K-wire, depending on the amount of dissection and excision. After pin
removal, tape the toe for 3 weeks, and have the patient continue to
wear the postoperative shoe.
transferring pressure to the third metatarsal head or even developing
an intractable plantar keratosis.
pediatric population. It is more commonly seen in male patients, and
the average age of onset is 5–6 years, during the time of ossification
of the navicular (11). The exact etiology of this disease is unknown, but it may be traumatic.
limping are the most common symptoms. There may be swelling and
tenderness of the medial midfoot, and discomfort with ranging the
transverse tarsal joints.
Only the ossification center is affected. Because there are few, if
any, surgical pathologic specimens, the true etiology remains unknown.
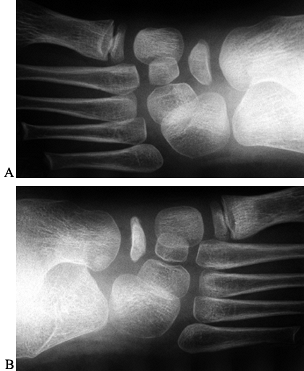 |
|
Figure 119.2. Radiographs (A,B) of a patient with unilateral Köhler’s disease show that the navicular on the affected side is flattened and sclerotic.
|
 |
|
Figure 119.3.
Lateral radiograph of a patient with Köhler’s disease showing preservation of the space for the navicular despite fragmentation and flattening of the bone. |
aimed at reducing symptoms. An arch support may be used, but cast
immobilization for 6–8 weeks is more effective (11),
especially when used initially with crutches. Follow-up radiographs are
not necessary as these lesions heal, and by 6–13 months after onset the
navicular has normal appearance and there are no known residual
symptoms in adults.
very common. Frequently seen in children, it is caused by ligamentous
laxity and is considered a variation of normal (22).
The medial longitudinal arch is determined by age and inheritable
traits; it develops with age as the ligamentous laxity resolves and the
subcutaneous fat decreases (23). Gould et al. (6)
followed 125 toddlers from 11–14 months of age until 5 years of age.
Initially, all the toddlers had pes planus, and arch development
occurred regardless of the type of footwear worn.
longitudinal arch is lost with weight bearing, but it reconstitutes
with non-weight-bearing. Generally, a flexible flatfoot does not cause
pain or disability. Even into adulthood, most patients do not develop
pain or stiffness or require treatment. A flexible flatfoot can be
associated with disability if there is an associated equinus
contracture.
medial arch. Their arch can “feel tired.” They may complain of
difficulty in finding comfortable shoes, or they experience abnormal or
excessive shoe wear. Inspect both lower extremities undressed to check
foot posture and function during gait, standing, and sitting. Assess
motion of the foot and ankle, and look for abnormal bony prominences.
Look for an Achilles tendon contracture by inverting the subtalar joint
and forefoot to lock the calcaneus under the talus while dorsiflexing
the ankle.
lateral view. Also, the angle between the longitudinal axis of the
talus and the first metatarsal is increased; 0° is normal, 0° to 15° is
a mild deformity, 15° to 30° is moderate, and more than 30° is severe.
The anteroposterior view may reveal abduction of the talonavicular
joint, leaving the medial portion of the talar head uncovered.
tried for flatfoot deformity, but the current recommended treatment is
observation in the asymptomatic child. The natural history of flexible
pes planus is not changed by corrective shoes, orthotic devices, or
exercises. Also, compliance was found to diminish with prolonged use of
corrective shoewear (over 3 years) (23).
functional improvement in a treated symptomatic patient, a supportive
medial arch may be used. If the Achilles tendon is tight, initiate heel
cord stretching exercises. Occasionally, sequential casting is needed
to treat a tight heel cord. Place the talonavicular joint in the
corrected position by placing the forefoot in varus (correct the
lateral subluxation), and apply the cast with the ankle in neutral.
Allow the patient to bear weight. Change the cast 2–3 weeks later;
usually three casts changes are required for correction (4).
planus in the past, it is unusual that a surgical procedure is
indicated. The operative options are a soft-tissue procedure,
osteotomy, and fusion (4). If the disability is
caused by an associated equinus contracture that does not respond to
nonoperative measures, then a tendo Achillis lengthening is performed.
-
Perform tendo Achillis lengthening
through three small incisions along the length of the tendon, two
medial and one lateral. Expose the tendon at each incision and then cut
from the midline of the tendon outward. -
Repair the tendon sheath to help prevent scarring of the tendon to the skin.
-
Extend the knee, and bring the foot up to 10° to 15° of dorsiflexion, taking care not to overlengthen the tendon.
-
Repair the skin and place the limb in a short-leg cast with the ankle in neutral.
of stiffness from adaptive changes of soft-tissue or bone. The symptoms
can be from severe pronation and heel valgus. In the past, a triple
arthrodesis yielded the most reliable results. Currently, other
procedures can alleviate the symptoms without the dramatic loss of
motion by sparing the joints. These are osteotomies aimed at correcting
the hyperpronation.
column by placing a bone graft from the tibia into the anterior process
of the calcaneus. It was described by Evans (2)
as treatment of calcaneovalgus feet, in which the medial and lateral
columns are equalized in length. This procedure preserves the
calcaneocuboid joint and pushes the navicular bone medially in relation
to the talus. The procedure has been popularized by Mosca (15).
-
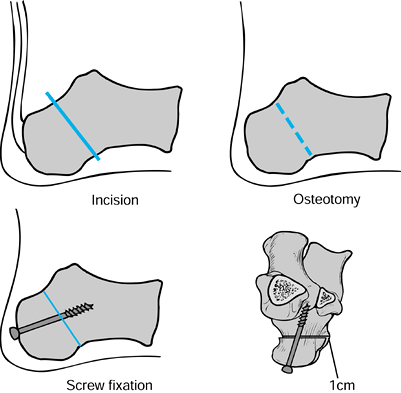
Perform the Evans procedure through a
longitudinal incision over the lateral calcaneus, just superior and
parallel to the peroneal tendons, and protecting the sural nerve.
Expose the anterior calcaneus and calcaneocuboid joint (Fig. 119.4).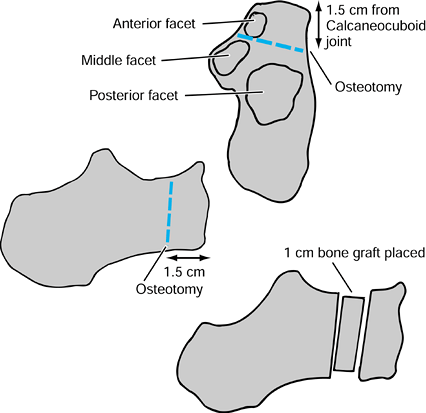 Figure 119.4. The Evans procedure.
Figure 119.4. The Evans procedure. -
Take a cortical bone graft from the
tibia, a bicortical iliac crest graft, or a piece of cortical allograft
measuring approximately 1 cm, depending on the desired amount of
correction. Place it between the osteotomized fragments so that the
hindfoot valgus deformity is corrected. -
Use 2 mm Kirschner (K) wires for fixation.
The procedure was successful in treating calcaneovalgus caused by
polio, painful rigid flatfoot, and idiopathic calcaneovalgus. It
slightly improved the shape of the foot and relieved pain in patients
with rigid flatfeet.
can be used to correct the deformity. The effect is to move the
proximal calcaneus medially, which improves the excessive valgus,
elevates the medial arch, and centralizes the motion of the subtalar
joint (17).
-
Make a lateral oblique incision over the
lateral calcaneus above the peroneal tendons. Retract the tendons
posteriorly and inferiorly with the sural nerve (Fig. 119.5).![]() Figure 119.5. Medial displacement osteotomy.
Figure 119.5. Medial displacement osteotomy. -
Cut the calcaneus perpendicular to the body between the posterior facet and the posterior tuberosity.
-
Perform the osteotomy with a saw;
complete it with an osteotome at the medial cortex. Then bluntly strip
the medial periosteum of the calcaneus. -
Open the osteotomy site with a lamina
spreader, and then displace the proximal portion medially, one half of
the width of the calcaneus, and tilt it to correct the valgus. -
Insert a bone graft to fill the gap and
use two 2 mm K-wires (for a cannulated 7.3 mm screw), which are drilled
from posterior to anterior, for fixation.
short-leg walking cast in the neutral position and begin weight bearing
as tolerated for a total of 6 weeks.
bulky compression dressing and splints. Remove the sutures at 2 weeks,
and apply a non-weight-bearing cast for an additional 4 weeks. Allow
weight bearing in a walking cast at 4–6 weeks after surgery. Remove the
K-wires as an outpatient surgical procedure 8 weeks after surgery. Once
the osteotomy has healed and the cast is removed, progress weight
bearing with limitations on athletics. At 6 months, allow full activity.
procedure is rarely indicated in an adult because no growth potential
remains. The presence of a fixed deformity in the hindfoot or midfoot
or degenerative joint disease is a contraindication to a soft-tissue
procedure or osteotomy. Perform arthrodeses for correction of deformity
and alleviation of pain (see Chapter 115).
medial aspect to strip but not cut the medial periosteum of the
calcaneus, to avoid injury of the neurovascular structures and flexor
tendons, which lie just on the periosteum.
Usually, there is a bony abnormality, such as tarsal coalition,
congenital vertical talus, or arthritis. Of these, tarsal coalition is
the most common cause and can present as peroneal spastic flatfoot.
 |
|
Figure 119.6.
Lateral radiograph of an adult patient with rigid pes planus demonstrating adaptive bony changes. The patient also had a tight heel cord. |
mesenchymal segmentation, and the resulting connection of two tarsal
bones may be fibrous (syndesmosis), cartilaginous (synchondrosis),
or bony (synostosis) (10). Tarsal coalition was described as long ago as 1769 by Buffon and can involve any combination of the tarsal bones (5). The tarsal coalition is an inherited disease that is autosomal dominant.
The calcaneonavicular type becomes symptomatic when the coalition
ossifies at 8–12 years of age. The talocalcaneal coalition frequently
involves the medial facet, and it ossifies at 12–16 years of age. In a
study of 22 patients with suspected coalitions, Herzenberg et al. found
that 14 had a coalition documented by computed tomography (CT) scans,
of which six were bilateral (9). All of the
talocalcaneal coalitions involved the middle facet joint, and these
were composed of bony or mixed osteocartilaginous tissue.
Tarsal coalition should be suspected in adolescents with painful and
stiff pes planus. The most common age of presentation is the teen
years, but patients can develop initial symptoms in their twenties to
forties. Most patients complain of pain about the tarsal area, and
stiffness and tightness of the peroneal and toe extensor muscles. They
complain of difficulty with sports activities or even with standing and
walking. Physical examination shows a rigid hindfoot, loss of the
medial longitudinal arch, and fixed forefoot abduction. Spasm of the
peroneal tendons can be seen by placing the foot into inversion: The
result is contraction of the peroneus brevis or longus, or both.
They are superior to plain tomography and radiographs for visualizing
the three subtalar facet joints, as well as the size, nature, and
location of the coalition. To obtain coronal cuts of the subtalar
joint, position the patient supine with the hips and knees flexed, and
place the feet in maximum plantar flexion and flat on the table so that
the subtalar joint is perpendicular to the x-ray beam.
 |
|
Figure 119.7. Oblique radiograph showing a complete bony coalition between the navicular and calcaneus.
|
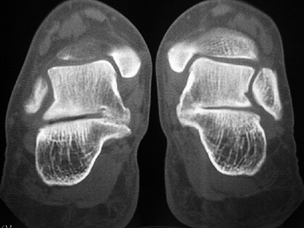 |
|
Figure 119.8. Computed tomography scan showing bilateral talocalcaneal coalition of the middle facet.
|
Rest, nonsteroidal anti-inflammatory medication, and cast
immobilization will be helpful to some patients. Use a cast for at
least 3 weeks; usually 6–8 weeks are required for relief of symptoms.
Later, a shoe modification, such as a heel cup, a medial arch support,
or a medial heel wedge, may allow patients to return to weight-bearing
activities.
in a child with a middle facet coalition or a posterior facet coalition
that comprises less than 25% of the joint surface and that is
symptomatic and unresponsive to nonoperative treatment. Once
symptomatic, the majority of patients do not respond to nonoperative
treatment. Contraindications to coalition resection include
degenerative arthritis, associated deformity, and involvement of
greater than 50% of the posterior facet.
-
Make a lateral longitudinal or oblique
incision over the sinus tarsi. Make full-thickness skin flaps, and
identify and protect the sural nerve and peroneal tendons. Elevate the
extensor digitorum brevis from its origin from proximal to distal to
expose the coalition. -
Excise the coalition with an osteotome, ronguer, or motorized burr.
-
Once the bar is completely removed,
transfer the extensor digitorum brevis muscle into the defect of the
excised coalition, holding it there with absorbable sutures. A
convenient method is to use a pullout suture. -
Close the skin incision and apply a bulky dressing and well-padded splints.
-
Make a medial longitudinal curvilinear incision 6 cm long, just plantar to the posterior tibial tendon.
-
Develop the interval between the flexor
digitorum longus and the flexor hallucis longus tendons, retracting the
neurovascular bundle plantarward. -
Localize the coalition with two Keith
needles on either side using fluoroscopy. Then excise about 5–7 mm of
the bar with an osteotome or motorized burr until motion in the
subtalar joint is restored. -
Apply bone wax to the cut bony surfaces
to control bleeding. Then interpose fat harvested from the posterior
aspect of the calcaneus into the gap. -
Repair the flexor digitorum and hallucis
longus tendon sheaths, and then close the skin. Apply a bulky dressing
and short-leg splints.
recommended, although this is controversial. Excision alone is
definitely contraindicated if degenerative changes are present. Note
that talar beaking is a traction spur on the dorsum of the talus and
not degenerative arthritis. In young adults with no or minimal
degenerative changes or deformity, an excision may be attempted to
delay fusion. Some authors advocate this treatment initially. Scranton (19)
reported that of 14 feet that underwent resection of a talocalcaneal
coalition, 13 had a good result and 1 a satisfactory result. No patient
had a poor result. He found that once the coalition was excised, the
anterior and posterior facet joints appeared normal. Olney and Asher (16)
had satisfactory results in 8 of 10 feet after resection of
talocalcaneal coalition, and all patients appeared to have increased in
the range of motion in the subtalar joint.
deformity can be corrected by fusing the subtalar joint, the transverse
tarsal joints can be spared. This is my preferred method of surgical
treatment if there are no degenerative changes of the talonavicular and
calcaneocuboid joints. In the patient with severe deformity and
disabling pain, a triple arthrodesis is the procedure of choice. If
there is an associated equinus contracture, a tendo Achillis
lengthening may be needed to fully correct the deformity.
excision surgery, and begin range-of-motion exercises. Continue
non-weight-bearing until ranging the subtalar joint does not cause
pain, which is usually about 6 weeks. At that time, begin weight
bearing.
compression dressing and splints in the first 2 weeks, and then remove
the staples or sutures. Apply a non-weight-bearing cast, which is worn
for 4 weeks, followed by a walking cast for the next 6 weeks until bony
union occurs. After this, a well-cushioned wide shoe may be worn.
persist, especially if there are degenerative changes. If excision is
the initial treatment, a fusion later may be required. Talar beaking,
however, is not a contraindication to resection of the coalition alone,
and it may be resected at the time of surgery if symptomatic. Patients
who have good to excellent early results continue to do well even at 10
years follow-up (5).
also called the accessory scaphoid, prehallux, os tibiale, os tibiale
externum, naviculare secundarium, and navicular secundum.
It was initially described by Bauhin in 1605 (7). The accessory navicular sits posteromedial to the navicular (Fig. 119.9),
and it ossifies between 9 and 11 years of age. It is seen
radiographically with much variation, small to large, round to
triangular. Its connection to the navicular may be fibrous,
cartilaginous, or bony.
 |
|
Figure 119.9. (A) Anteroposterior and (B) lateral radiographs of a patient with a symptomatic accessory navicular.
|
determined by radiographic appearance. Type I is an ossicle that lies
within the posterior tibial tendon, type II is connected to the
navicular by a cartilaginous bridge, and type III is a cornuate-shaped
navicular from fusion of the accessory bone to the navicular. Accessory
navicular is quite common—2% to 14% of the population and is bilateral
in 77% to 100% of cases (7,8).
navicular can cause pes planus. Generally, the patient has a flatfoot
deformity and the accessory bone interferes with the normal mechanics
of the posterior tibial tendon. Kidner (12,13)
believed that removal of the accessory navicular would allow a
straighter pull of the tendon and thus improvement of the flatfoot
deformity.
The source symptoms in an accessory navicular are not absolutely clear.
Inflammation of the surrounding soft tissues from the prominence or
trauma to the cartilaginous bridge may cause pain. Repetitive stresses
on a cartilage bridge may result in a painful stress fracture (7).
mid-medial arch aggravated by weight bearing. In adults, initial
symptoms may appear after a severe twisting injury, often occurring in
sports.
the proximal medial border of the navicular with tenderness over the
accessory bone. There can be associated local edema and erythema.
radiographs of the foot. A bone scan may help to localize and
differentiate the pathologic cause of medial arch pain, but it is
rarely necessary.
consists of rest from activity, nonsteroidal anti-inflammatory
medication, and shoewear modification. A wider shoe will relieve the
pressure over the bony prominence. With a flatfoot deformity, a medial
arch in a custom orthotic device may reduce the stress on the medial
longitudinal arch.
sprain, can be treated with a short course of cast immobilization for
3–6 weeks. After casting, usual activities can be resumed as symptoms
allow.
nonoperative treatment, excision of the accessory bone is indicated.
Excision of the accessory bone with advancement of the posterior tibial
tendon is known as the Kidner procedure. However, there is little
advantage to advancing the tendon, and I do not recommend it. Bennett
et al. (1) reported on 75 feet that were
treated with excision of the accessory navicular only and simple
reefing of the tibialis posterior tendon. Fifty-eight feet had
excellent results, and 12 had good results. Grogan et al. (7) had excellent results in 16 of 17 patients by simple excision of the accessory navicular.
-
Make a 3–4 cm medial longitudinal
incision over the insertion of the posterior tibial tendon, incise the
tendon longitudinally, and visualize the accessory navicular. -
Excise the accessory navicular. The
remaining navicular tuberosity is usually prominent, so use a ronguer
to create a smooth surface. Apply bone wax to the cut surface to
decrease postoperative bleeding. -
Repair the posterior tibial tendon with
interrupted absorbable sutures. If the defect is large, repair the
tendon and advance it through a drill hole in the navicular; bring it
out the dorsum and suture it onto itself.
inversion in a bulky compressive dressing with splints. Remove the
sutures at 2 weeks, and place the foot in the same position in a
fiberglass cast until 3 weeks. Continue immobilization in a removable
cast for an additional 3 weeks, and then begin weight bearing as
tolerated.
removal of the cast, and prescribe a custom orthotic device with a
molded arch if necessary.
pressure against shoewear may persist. Sometimes tenderness persists
over the medial eminence area, especially in adults. To prevent this
problem, remove sufficient bone and smooth the remaining surface with a
rongeur.
including symptomatic flatfoot, equinus contracture, or a tarsal
coalition, the treatment must address these problems as well.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
P, Kumar SJ. Calcaneonavicular Coalition Treated by Resection and
Interposition of the Extensor Digitorum Brevis Muscle. J Bone Joint Surg Am 1990;72A:71.
JE, Golner L, Martinez S, Silverman PM. Computerized Tomography of
Talocalcaneal Tarsal Coalition: A Clinical and Anatomic Study. Foot Ankle 1986;6:273.
VS. Calcaneal Lengthening for Valgus Deformity of the Hindfoot. Results
in Children Who Had Severe, Symptomatic Flatfoot and Skewfoot. J Bone Joint Surg Am 1995;77:500.
LT, Chew DE, Corbett M. The Longitudinal Arch: A Survey of Eight
Hundred and Eighty-two Feet in Normal Children and Adults. J Bone Joint Surg Am 1987;69:426.