Pathologic Reflexes
responses not generally found in the normal individual. Some are
responses that are minimally present and elicited with difficulty in
normals but become prominent and active in disease, while others are
not seen in normals at all. Many are exaggerations and perversions of
normal muscle stretch and superficial reflexes. Some are related to
postural reflexes or primitive defense reflexes that are normally
suppressed by cerebral inhibition but become enhanced when the lower
motor neuron is separated from the influence of the higher centers.
Others are responses normally seen in the immature nervous system of
infancy, then disappear only to reemerge later in the presence of
disease. A decrease in threshold or an extension of the reflexogenic
zone plays a role in many pathologic reflexes.
modulate the activity at the local, segmental spinal cord level to
insure efficient muscle contraction and proper coordination of
agonists, antagonists, and synergists. Disease of the descending motor
pathways causes loss of this normal control so that activity spills
from the motor neuron pool responsible for a certain movement to
adjacent areas, resulting in the recruitment into the movement of
muscles not normally involved. Some pathologic reflexes may also be
classified as “associated movements,” related to such spread of motor
activity. Whether a certain abnormal response would be best classified
as a reflex or an associated movement is not always clear. Responses
that are more in the realm of an associated movement are sometimes
referred to clinically as reflexes (e.g., the Wartenberg thumb
adduction sign, an associated movement, is sometimes called a
Wartenberg reflex).
involving the corticospinal tract and associated pathways. They also
occur with frontal lobe disease and occasionally with disorders of the
extrapyramidal system. There is a great deal of confusion regarding
names of reflexes and methods of elicitation, and in many cases there
has been significant drift away from the original description. Many of
the responses are merely variations in the method of eliciting the same
responses, or modifications of the same reflex. The typical reflex
pattern with lesions involving the corticospinal tract, the upper motor
neuron syndrome, is exaggeration of deep tendon reflexes (DTRs),
disappearance of superficial reflexes, and emergence of pathologic
reflexes (Table 28.3).
normally present in the developing nervous system, but disappear to a
greater or lesser degree with maturation. While normal in infants and
children, when present in an older individual they may be evidence of
neurologic disease, although some may reappear in normal senescence.
Many of these are exaggerations of normal reflex responses. Responses
often included as FRS include the palmomental reflex (PMR), grasp,
snout, suck, and others.
severe dementias, diffuse encephalopathy (metabolic, toxic,
postanoxic), after head injury, and other states in which the pathology
is usually diffuse but involves particularly the frontal lobes or the
frontal association areas. The significance and usefulness of some of
these release signs or primitive reflexes has been questioned. The PMR
is commonly seen in normal individuals. The Hoffman finger flexor
reflex and its variants, which are sometimes classified as FRS and
sometimes as corticospinal signs, are similarly present in a
significant proportion of normal individuals. Clearly, these reflexes
are a normal phenomenon in a significant proportion of the healthy
population. They must be interpreted with caution and kept in clinical
context. Even when such reflexes are briskly active in an appropriate
clinical setting, the primitive reflexes do not have great localizing
value, suggesting instead the presence of diffuse and widespread
dysfunction of the hemispheres.
constant, more easily elicited, more reliable, and more clinically
relevant than those in the upper limbs. The most important of these
responses may be classified as (a) those characterized in the main by
dorsiflexion of the toes, and (b) those characterized by plantar
flexion of the toes. The most important pathologic reflex by far is the
Babinski sign, and a search for an upgoing toe is part of every
neurologic examination. Searching for upper-extremity pathologic
reflexes is much less productive and often omitted.
plantar surface of the foot is followed by plantar flexion of the toes (Figure 29.2).
In the normal plantar reflex, the response is usually fairly rapid, the
small toes flex more than the great toe, and the reaction is more
marked when the stimulus is along the medial plantar surface. In
disease of the corticospinal system there may be instead extension
(dorsiflexion) of the toes, especially the great toe, with variable
separation or fanning of the lateral four toes: the Babinski sign or
extensor plantar response (Figure 30.1). The Babinski
sign has been called the most important sign in clinical neurology. It
is one of the most significant indications of disease of the
corticospinal system at any level from the motor cortex through the
descending pathways.
 |
|
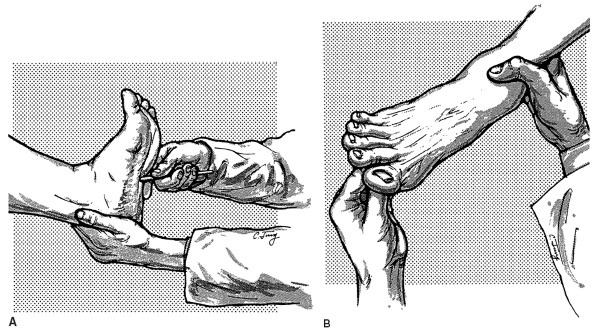
FIGURE 30.1 • Method of eliciting the Babinski sign.
|
surface of the foot with a blunt point, such as an applicator stick,
handle of a reflex hammer, a broken tongue blade, the thumbnail, or the
tip of a key. Strength of stimulus is an important variable. It is not
true that the stimulus must necessarily be deliberately “noxious,”
although most patients find it at least somewhat uncomfortable even if
the examiner is trying to be considerate. When the response is strongly
extensor only minimal stimulation is required. The stimulus should be
firm enough to elicit a consistent response, but as light as will
suffice. Some patients are very sensitive to plantar stimulation and
only a slight stimulus will elicit a consistent response; stronger
stimuli may produce confusing withdrawal. If the toe is briskly
upgoing, merely a fingertip stimulus may elicit the response. If no
response is obtained, progressively sharper objects and firmer
applications are necessary. Although some patients require a very firm
stimulus, it is not necessary to aggressively rake the sole as the
opening gambit. Both tickling, which may cause voluntary withdrawal,
and pain, which may bring about a reversal to flexion as a nociceptive
response, should be avoided.
in the S1 root/sural nerve sensory distribution. More medial plantar
stimulation may fail to elicit a positive response when one is present.
Far medial stimulation may actually elicit a plantar grasp response
causing the toes to flex strongly. The stimulus should begin near the
heel and be carried up the side of the foot at a deliberate pace, not
too quickly, usually stopping at the metatarsophalangeal joints. The
response has usually occurred by the time the stimulus reaches the
midportion of the foot. If the response is difficult to obtain, the
stimulus should continue along the metatarsal pad from the little toe
medially, but stopping short of the base of the great toe. The most
common mistakes are insufficiently firm stimulation, placement of the
stimulus too medially and moving the stimulus too quickly, so that the
response does not have time to develop. The only movements of real
significance are those of the great toe. Fanning of the lateral toes
without an abnormal movement of the great toe is seldom of any clinical
significance, and an absence of fanning does not negate the
significance of great toe extension.
potential discomfort. The knee must be extended; an upgoing toe may be
abolished by flexion of the knee. The best position is supine, with
hips and knees in extension and heels resting on the bed. If the
patient is seated, the knee should be extended, with the foot held
either in the examiner’s hand or on her knee. The response may
sometimes be reinforced by rotating the patient’s head to the opposite
side.
quick, flicking motion sometimes mistaken for withdrawal by the
inexperienced. The response may be a slow, tonic, sometimes clonic,
dorsiflexion of the great toe and the small toes with fanning, or
separation, of the toes. The slow great toe movement has been described
as a “majestic rise.” The nature of the stimulus may be related to the
speed of the toe movement; primarily proprioceptive stimuli (e.g.,
Gonda, Stransky, Szapiro) are more apt to be followed by a slow, tonic
response; exteroceptive stimuli by a brief, rapid extension. There may
occasionally be initial extension, followed by flexion; less often
brief flexion precedes extension. There may be extension of only the
great toe, or extension of the great toe with flexion of the small toes.
reflex. The central nervous system is organized according to movement
patterns, and one of the most basic patterns is avoidance or withdrawal
from a noxious stimulus. In higher vertebrates, the flexion response
includes flexion of the hip and knee, and dorsiflexion of the ankle and
toes, all serving to remove the threatened part from danger. Descending
motor systems normally suppress the primitive flexion response. When
there is disease involving the corticospinal tract, the primitive
flexion response may reappear, and the first clinical evidence of this
is the Babinski sign. With more severe and extensive disease the entire
flexion response emerges, so that stimulation of the sole causes
dorsiflexion not only of the toe, but also the ankle, as well as
flexion of the hip and knee (the “triple flexion” response). In
addition, there is
often contraction of the tensor fascia lata causing slight internal rotation at the hip and more rarely abduction of the hip.
the lower extremities characterized by dorsiflexion of the toes. With
severe corticospinal tract disease, the threshold for eliciting an
upgoing toe is lower, the reflexogenic zone wider, and more and more of
the other components of the primitive flexion reflex appear as part of
the response. This has led to a profusion of variations on the Babinski
method of eliciting the extensor plantar response. The most useful
variation is the Chaddock sign, and the Oppenheim is also often done.
aspect of the foot, not the sole, beginning about under the lateral
malleolus near the junction of the dorsal and plantar skin, drawing the
stimulus from the heel forward to the small toe. The Chaddock is the
only alternative toe sign that is truly useful. It may be more
sensitive than the Babinski but is less specific. It produces less
withdrawal than plantar stimulation. The two reflexes are
complementary; each can occur without the other, but both are usually
present. The Oppenheim sign is usually elicited by dragging the
knuckles heavily down the anteromedial surface of the tibia from the
infrapatellar region to the ankle. The response is slow and often
occurs toward the end of stimulation. A common ploy is to combine the
Oppenheim and the Babinski to make a suspicious toe declare itself, but
this is more painful and less useful than the Chaddock.
zone wide, the toe may go up with such minor stimuli as pulling back
the bed sheets or rapid removal of the sock or shoe. Occasionally there
is a “spontaneous Babinski,” occurring with no apparent manipulation of
the foot. There may even be contralateral or bilateral responses.
Sometimes the toes are held in a tonic position of dorsiflexion and
fanning. A tonic extensor plantar response must be distinguished from a
“striatal toe.”
reliable, dependable, and consistent signs in clinical neurology. But
it is not perfect, and the response to plantar stimulation may at times
be difficult to evaluate. The most common problem is distinguishing an
upgoing toe from voluntary withdrawal. The Babinski sign is part of a
withdrawal reflex, so flexion of the hip and knee are by no means
reliable indicators that the withdrawal movement is voluntary.
Voluntary withdrawal rarely causes dorsiflexion of the ankle, and there
is usually plantar flexion of the toes. Voluntary withdrawal is more
likely when the stimulus is too intense and uncomfortable. It helps if
the patient understands the importance of holding still and receives
some explanation of the relevance of this seemingly inane and cruel
test. Some patients have ticklish feet and will pull away from even a
light stimulus. If the patient is ticklish, it may help to simply hold
the ankle firmly. Internal rotation of the leg during the “withdrawal”
signals recruitment of the tensor fascia lata into the movement and
makes it more likely the response is reflex and not voluntary.
of the great toe. With repeated stimulation of the sole, the extensor
movement may decrease and then disappear. So the crucial observation is
the first toe movement on the first stimulation. Occasionally,
withdrawal makes it impossible to be certain whether the toe was truly
extensor or not; these are equivocal plantar responses. Some patients
have no elicitable plantar response, in which case the plantars are
said to be mute or silent. Asymmetry of the plantar responses may be
significant; a toe that does not go down as crisply as its fellow may
be suspect, even if it does not frankly go up. A toe is more likely to
go up late in the day or when the patient is tired.
structural disease; it may occur as a transient manifestation of
physiologic dysfunction of the corticospinal pathways. A Babinski sign
may sometimes be found in deep anesthesia and narcosis; drug and
alcohol intoxication; metabolic coma such as hypoglycemia; deep sleep;
post-ictally; and in other conditions of altered consciousness. The
plantar response returns to normal with recovery of consciousness.
 |
|
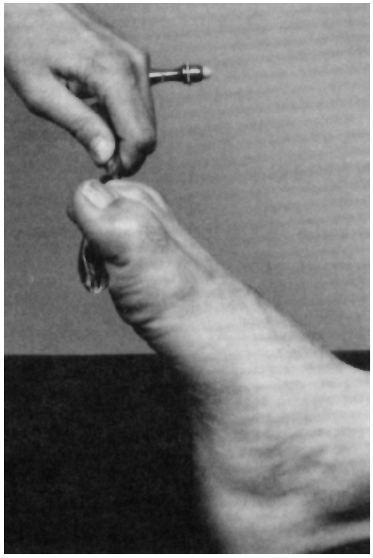
FIGURE 30.2
• Plantar grasp reflex. Brisk bending of toes to grasp reflex hammer handle. (Reprinted from Massey EW, Pleet AB, Scherokman BJ. Diagnostic Tests in Neurology: A Photographic Guide to Bedside Techniques. Chicago: Year Book Medical Publishers, Inc., 1985.) |
foot as well as the hand, with flexion and adduction of the toes in
response to a light pressure on the plantar surface of the foot,
especially its distal and medial portions. The plantar grasp normally
disappears by the end of the first year. A grasp reflex of the foot may
reappear in adults, along with a grasp reflex of the hand, in disease
of the opposite frontal lobe. The plantar grasp may be elicited by
drawing the handle of a reflex hammer from the midsole toward the toes,
causing the toes to flex and grip the hammer (Figure 30.2).
a plantar muscle reflex consisting of contraction of the toe flexors
following sudden stretching. This response is barely, if at all,
perceptible normally, but becomes more obvious with reflex
hyperactivity and, therefore, with corticospinal tract lesions. The
best known of this group of reflexes is the Rossolimo sign (Figure 30.3). Tapping the ball of the foot or plantar surfaces of the toes causes a quick plantar flexion of the toes.
 |
|
FIGURE 30.3 • Method of eliciting the Rossolimo sign.
|
less constant, more difficult to elicit, and usually less significant
diagnostically than those found in the lower extremities. A great deal
of confusion exists concerning the nomenclature of these reflexes, with
many variations and modifications of the same response. The
upper-extremity pathologic reflexes primarily fall into two categories:
frontal release signs (FRS) and exaggerations of or variations on the
finger flexor reflex. The grasp and palmomental reflexes are usually
classified as FRS. The finger flexor related responses are usually a
manifestation of the spasticity and hyperreflexia that occur in lesions
involving the corticospinal tract, so the Hoffman and Trömner signs are
usually classified as corticospinal tract signs. These responses occur
only with lesions above the C5 or C6 segment of the cervical spinal
cord.
grasping is an involuntary flexor response of the fingers and hand
following stimulation of the skin of the palmar surface of the fingers
or hand. The palmar grasp is normally present at birth and may be
strong enough to suspend the infant by her own grasp. The response
begins to diminish at the age of 2 to 4 months. It reappears primarily
in association with extensive neoplastic or vascular lesions of the
frontal lobes or with cerebral degenerative processes, usually
contralaterally but occasionally ipsilaterally. Although the grasp
reflex is usually classified as an FRS or primitive reflex, it may also
occur as evidence of corticospinal tract dysfunction in spastic
hemiplegia. The grasping responses are exaggerations of normal
reactions and occur as release phenomena; the groping response is a
more complicated reaction that is modified by visual and tactile
integration at the cortical level.
contraction of the mentalis and orbicularis oris muscles causing
wrinkling of the skin of the chin with slight retraction and sometimes
elevation of the angle of the mouth in response to scratching or
stroking the palm of the ipsilateral hand. The reflex is best elicited
by stroking a blunt point over the thenar eminence, either from wrist
toward thumb or vice versa, or by tapping this area. The PMR is so
frequently present in normal persons that significance can only be
attached to a marked exaggeration of the response or a conspicuous
asymmetry between the two sides. If the response is marked, the
reflexogenic zone may be wide, including the hypothenar area. The
localizing value and clinical significance of these reflexes are
limited. A unilateral PMR may occur with bilateral, contralateral, or
ipsilateral lesions.
the patient’s fingers and distal phalanx of the thumb in response to a
stretch stimulus delivered with a reflex hammer (Figure 28.6).
The Hoffmann and Trömner signs are alternative methods of delivering
the stretch stimulus. They are prominent when the other upper-extremity
DTRs are hyperactive, as in corticospinal tract lesions. These signs
are not necessarily pathologic and are often present to some degree in
normal individuals. As with the PMR, they are only of clinical
significance when markedly active or very asymmetric. A very active,
complete Hoffmann or Trömner sign, especially if unilateral or
associated with other reflex abnormalities or a consistent history, is
certainly suggestive if not diagnostic of corticospinal tract
involvement.
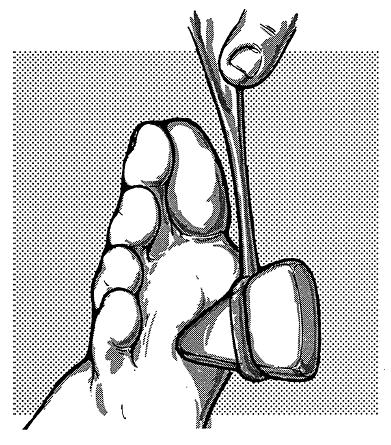
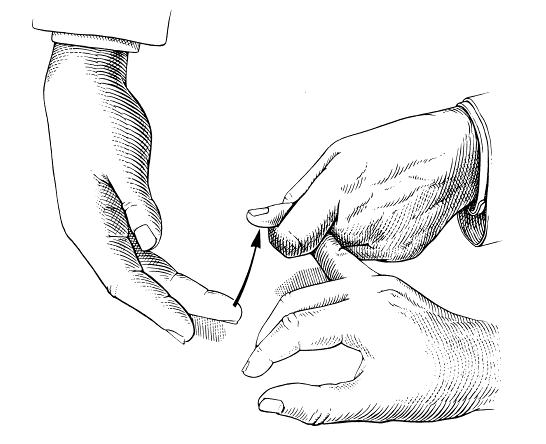
is held with the wrist dorsiflexed and fingers partially flexed. With
one hand, the examiner holds the partially extended middle finger
between her index finger and thumb or between her index and middle
fingers. With a sharp, forcible flick of the other thumb, the examiner
nips or snaps the nail of the patient’s middle finger, forcing the
distal finger into sharp, sudden flexion followed by sudden release (Figure 30.4).
The rebound of the distal phalanx stretches the finger flexors. If the
Hoffmann sign is present, this is followed by flexion and adduction of
the thumb and flexion of the index finger, and sometimes
flexion
of the other fingers as well. If only the thumb or only the index
finger responds the sign is “incomplete.” In the Trömner sign, the
examiner holds the patient’s partially extended middle finger, letting
the hand dangle, then, with the other hand, thumps or flicks the finger
pad (Figure 30.5).
The response is the same as that in the Hoffmann test. The two methods
are equivalent and either manner of testing may be used; both are
sometimes referred to as the Hoffmann test.
 |
|
FIGURE 30.4 • Method of eliciting the Hoffmann sign.
|
protrusion of the lips, primarily the lower, often with depression of
the lateral angles of the mouth, in response to pressing firmly
backward on the philtrum of the upper lip, a minimal tap to the lips,
or sweeping a tongue blade briskly across the lips. When exaggerated,
the response may include not only puckering and protrusion of the lips,
but also sucking and even tasting, chewing, and swallowing movements.
The sucking reflex is normal in infants; stimulation of the perioral
region is followed by sucking movements of the lips, tongue, and jaw. A
rooting (searching) reflex is when the lips, mouth, and even head
deviate toward a tactile stimulus delivered beside the mouth or on the
cheek. The sucking reflex disappears after infancy, when sucking
becomes a voluntary rather than reflex phenomenon. Like the other FRS,
it may reappear in some patients with diffuse cerebral disease.
contractions induced by the sudden passive stretching of a muscle or
tendon. It often accompanies the spasticity and hyperactive DTRs seen
in corticospinal tract disease. Clonus occurs most frequently at the
ankle, knee, and wrist, occasionally
elsewhere.
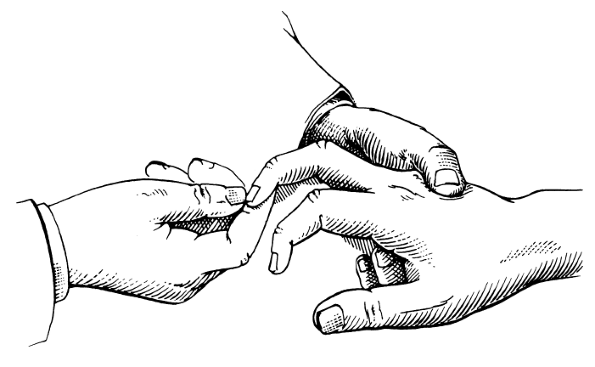
Ankle clonus consists of a series of rhythmic alternating flexions and
extensions of the ankle. It is easiest to obtain if the examiner
supports the leg, preferably with one hand under the knee or the calf,
grasps the foot from below with the other hand, and quickly dorsiflexes
the foot while maintaining slight pressure on the sole at the end of
the movement (Figure 30.6).
The leg and foot should be well relaxed, the knee and ankle in moderate
flexion, and the foot slightly everted. The response is a series of
alternating contractions. Unsustained clonus fades away after a few
beats; sustained clonus persists as long as the examiner continues to
hold slight dorsiflexion pressure on the foot. Unsustained (transient,
exhaustible, or abortive) symmetric ankle clonus may occur in normal
individuals with physiologically fast DTRs. Sustained clonus is never
normal. In severe spasticity clonus may occur spontaneously or with the
slightest stimulus. Slight plantar flexion pressure, as in stepping on
the accelerator of a car, may cause violent, uncontrollable, repetitive
jerking of the foot. A single tap on the tendon to elicit the ankle
jerk will occasionally provoke clonus.
 |
|
FIGURE 30.5 • Method of eliciting the Trömner sign.
|
 |
|
FIGURE 30.6 • Method of eliciting ankle clonus.
|
up-and-down movements of the patella. It may be elicited if the
examiner grasps the patella between index finger and thumb and executes
a sudden, sharp, downward thrust, holding downward pressure at the end
of the movement. The leg should be extended and relaxed. Patellar
clonus may appear when eliciting the patellar or suprapatellar reflex.
Clonus of the wrist or of the fingers may be produced by a sudden
passive extension of the wrist or fingers. Clonus of the jaw occurs
occasionally. Nonorganic clonus occurs rarely. False clonus
(pseudoclonus) in psychogenic disorders is poorly sustained and
irregular in rate, rhythm, and excursion. At the ankle, true clonus can
usually be stopped by sharp passive plantar flexion of the foot or the
great toe; false clonus is not altered by such a maneuver.
tone in the extensor, or antigravity, muscles of the limbs and the
spine. This phenomenon is known as decerebrate rigidity. In patients
with extreme decrebrate rigidity, there is opisthotonos, with all four
limbs stiffly extended, the head back, and the jaws clenched. The arms
are internally rotated at the shoulders, extended at the elbows, and
hyperpronated, with the fingers extended at the metacarpophalangeal
joints and flexed at the interphalangeal joints. The legs are extended
at the hips, knees, and ankles, and the toes are plantar flexed. The
position is an exaggeration or caricature of the normal standing
position. The deep tendon reflexes are exaggerated, the tonic neck and
labyrinthine reflexes are present, and the righting reflexes abolished.
brainstem at any level between the superior colliculi or the
decussation of the rubrospinal pathway and the rostral portion of the
vestibular nuclei. The vestibular nuclei enhance extensor tone, and
integrity of the vestibular nuclei is necessary for decrebrate rigidity
to occur. These nuclei are intact, but isolated from the midbrain,
specifically from the red nuclei and rubrospinal tracts. Activity in
the reticular formation is also important, particularly the pontine
reticular nuclei and the medial reticulospinal tract, which also
facilitates extensor muscle tone. Experimentally, decerebrate rigidity
is abolished by section of the vestibulospinal pathways. In patients,
when the process extends to involve the medulla the decerebration
disappears. The most common cause of decerebrate rigidity in humans is
trauma, and the presence of extensor posturing is a poor prognostic
indicator.
elbows and wrists with extension of the legs and feet. The causative
lesion is higher than that causing decerebrate rigidity, preserving the
function of the rubrospinal tract, which enhances flexor tone in the
upper extremities.
