Intra-Articular Injuries of the Knee
chondroepiphyseal avulsion of the anterior cruciate ligament (ACL)
insertion on the anteromedial tibial eminence.232,311 Tibial eminence fractures were once thought to be the pediatric equivalent of midsubstance ACL tears in adults.30,36,61,120,148,176,188,200,201,236,240,307,308
reported that it occurred in 3 per 100,000 children each year. The most
common causes of these fractures are bicycle accidents and athletic
activities.217
treatment of all fractures to operative treatment of certain fractures.
Garcia and Neer107 reported 42
fractures of the tibial spine in patients ranging in age from 7 to 60
years, 6 of whom had positive anterior drawer signs indicating
associated collateral ligament injuries. They reported successful
closed management in half their patients. Meyers and McKeever,216
however, recommended arthrotomy and open reduction for all displaced
fractures, followed by cast immobilization with the knee in 20 degrees
of flexion rather than hyperextension, believing that hyperextension
aggravated the injury in one of their patients. Gronkvist et al.120
reported late instability in 16 of 32 children with tibial spine
fractures, and recommended surgery for all displaced tibial spine
fractures, especially in children older than 10 years because “the
older the patient, the more the demand on the anterior cruciate
ligament-tibial spine complex.”120 Baxter and Wiley30 noted mild to moderate knee laxity at follow-up in 45 patients, even after anatomic reduction of the tibial spine. McLennan212
reported 10 patients with type III intercondylar eminence fractures
treated with closed reduction and with arthroscopic reduction with or
without internal fixation.
At
second-look arthroscopy 6 years after the initial injury, those treated
with closed reduction had more knee laxity than those treated
arthroscopically.
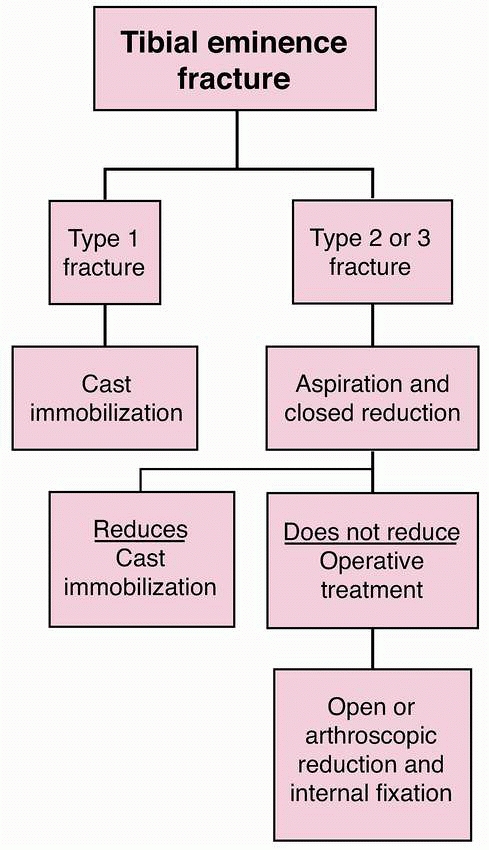
fractures and hinged or displaced fractures which are able to be
reduced can be treated closed. Hinged and displaced fractures which do
not reduce require open or arthroscopic reduction with internal
fixation. A variety of treatment options have been reported including
cast immobilization,188,223 closed reduction with immobilization,236,308 open reduction with immobilization,223 open reduction with internal fixation,225,236 arthroscopic reduction with immobilization,212 arthroscopic reduction with suture fixation,49,137,155,188,200,201 and arthroscopic reduction with wire,27 screw fixation,36,188,212 anchor fixation,298 and bioabsorbable fixation.264
reduced tibial spine fractures and for operative treatment of displaced
fractures is good. Most series report healing with an excellent
functional outcome despite some residual knee laxity.27,30,36,155,170,188,195,200,201,211,212,223,225,276,307,308 Potential complications include nonunion, malunion, arthrofibrosis, residual knee laxity, and growth disturbance.27,30,36,155,170,188,200,201,211,212,223,225,276,296,308
However, with increased participation in youth sports at earlier ages
and at higher competitive levels, tibial spine fractures resulting from
sporting activities are being seen with increased frequency. The most
common mechanism of tibial eminence fracture is forced valgus and
external rotation of the tibia, although tibial spine avulsion
fractures can also occur from hyperflexion, hyperextension, or tibial
internal rotation. As with ACL injury, tibial eminence fractures in
sport may result from both contact and noncontact injuries.
avulsion of the ACL insertion on the anteromedial tibial eminence. In a
cadaver study by Roberts and Lovell,250,251
fracture of the anterior intercondylar eminence was simulated by
oblique osteotomy beneath the eminence and traction on the ACL. In each
specimen, the displaced fragment could be reduced into its bed by
extension of the knee. In adults, the same stress might cause an
isolated tear of the ACL, but in children the incompletely ossified
tibial spine is generally weaker to tensile stress than the ligament,
so failure occurs through the cancellous bone beneath the subchondral
bone of the tibial spine. In addition, loading conditions may result in
differential injury patterns. In experimental models, midsubstance ACL
injuries tend to occur under rapid loading rates, whereas tibial
eminence avulsion fractures tend to occur under slower loading rates in
cadaveric and animal models.232,311
patterns. In a retrospective case-control study of 25 skeletally
immature patients with tibial spine fractures compared to 25 age- and
sex-matched skeletally immature patients with midsubstance ACL
injuries, Kocher et al.175 found narrower intercondylar notches in those patients sustaining midsubstance ACL injuries.
after an acute traumatic event. They are unable to bear weight on their
affected extremity.
hemarthrosis because of the intra-articular fracture and limited motion
due to effusion. Sagittal plane laxity is often present, but the
contralateral knee should be assessed for physiologic laxity. Gentle
stress testing should be performed to detect any tear of the medial
collateral ligament (MCL) or lateral collateral ligament (LCL) or
physeal fracture of the distal femur or proximal tibia.
fracture may lack full extension because of a mechanical bony block.
Patients with late nonunion of a displaced tibial spine fracture may
have increased knee laxity, with a positive Lachman examination and
pivot-shift examination.
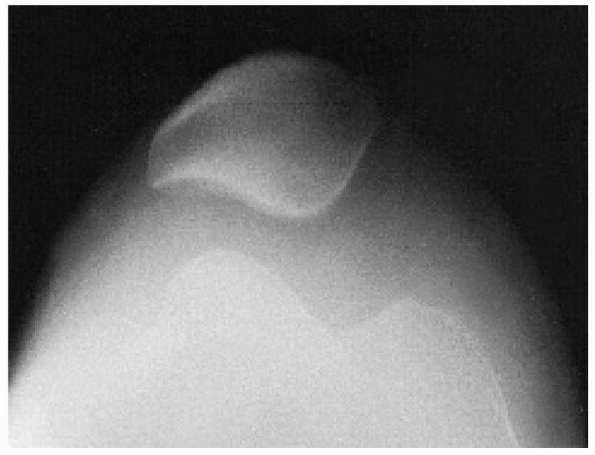
best on the lateral and tunnel views. The lateral radiograph is most
useful in fracture classification. Radiographs should be carefully
scrutinized as the avulsed fragment may be mostly nonossified cartilage
with only a small, thin ossified portion visible on the lateral view.
ascertain from the radiographs includes the classification type, amount
of displacement, size of the fracture fragment, comminution of the
fracture fragment, and status of the physes.
the diagnosis and management of tibial eminence fractures in children.
MRI may be helpful to confirm the diagnosis in cases with a very thin
ossified portion of the avulsed fragment or define adequacy of closed
redcution. MRI may also be useful to evaluate for associated collateral
ligament or distal femoral physeal injury; however, these are uncommon.
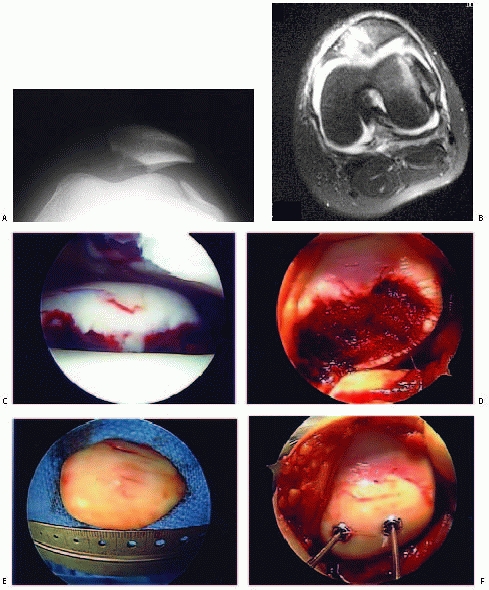
series of 80 skeletally immature patients who underwent surgical
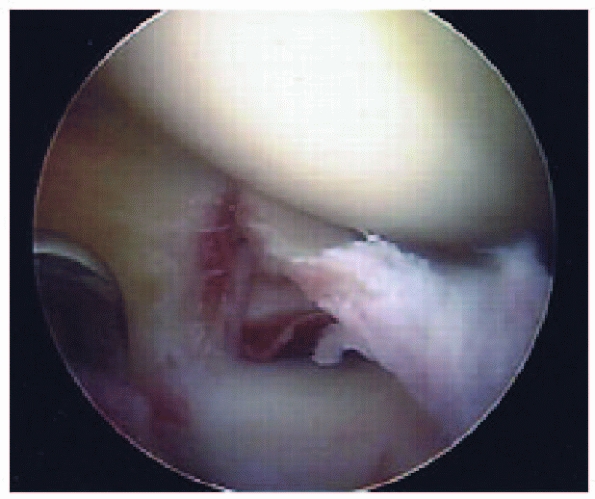
fixation of tibial eminence fractures, Kocher et al.177 found no associated chondral injuries and associated meniscal tear in only 3.8% (3/80) of patients (Fig. 24-1). Associated collateral ligament injury
or proximal ACL avulsion are uncommon, but have been reported.131,252
 |
|
FIGURE 24-1 Longitudinal meniscus tear associated with tibial eminence fracture.
|
 |
|
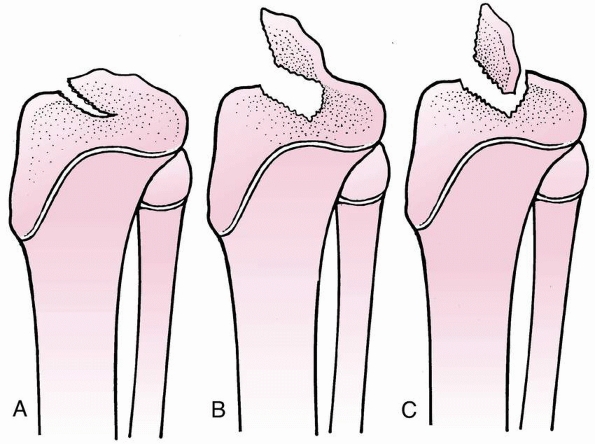
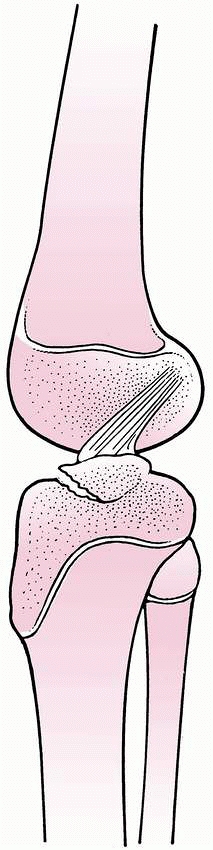
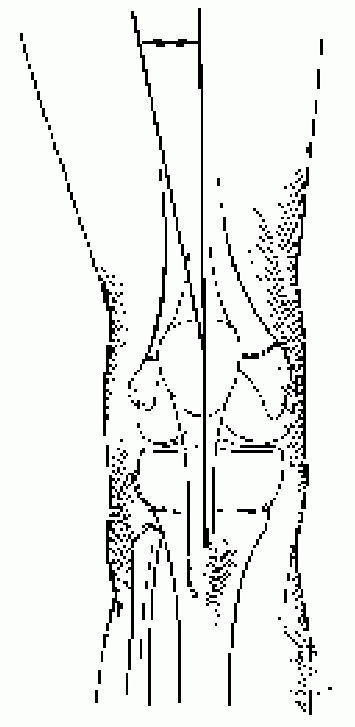
FIGURE 24-2 Classification of tibial spine fractures. A. Type I, minimal displacement. B. Type II, hinged posteriorly. C. Type III, complete separation.
|
-
Type 1—minimal displacement of the fragment from the rest of the proximal tibial epiphysis
-
Type 2—displacement of the anterior third
to half of the avulsed fragment, which is lifted upward but remains
hinged on its posterior border in contact with the proximal tibial
epiphysis -
Type 3—complete separation of the avulsed fragment from the proximal tibial epiphysis, with upward displacement and rotation
The interobserver reliability between type 1 and type 2/3 fractures is
good; however, differentiation between type 2 and 3 fractures may be
difficult.175
plateau lying between the anterior poles of the menisci forward to the
anterior tibial spine. It is triangular, with its base at the anterior
border of the proximal tibia. In the immature skeleton, the proximal
surface of the eminence is covered entirely with cartilage. The ACL
attaches distally to the anterior tibial spine with separate slips
anterior and lateral as well (Fig. 24-4). The
ligament originates off the posterior margin of the lateral aspect of
the intercondylar notch. The anterior horn of the lateral meniscus is
typically attached in the region of the intercondylar eminence at the
ACL insertion. In 12 patients with displaced tibial spine fractures
which did not reduce closed, Lowe et al.196
reported that the anterior horn of the lateral meniscus consistently
remained attached to the tibial eminence fracture fragment. The
posterior cruciate ligament (PCL) originates off the medial aspect of
the intercondylar notch and inserts on the posterior aspect of the
proximal tibia, distal to the joint line.
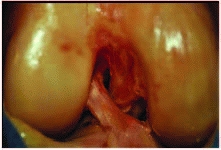
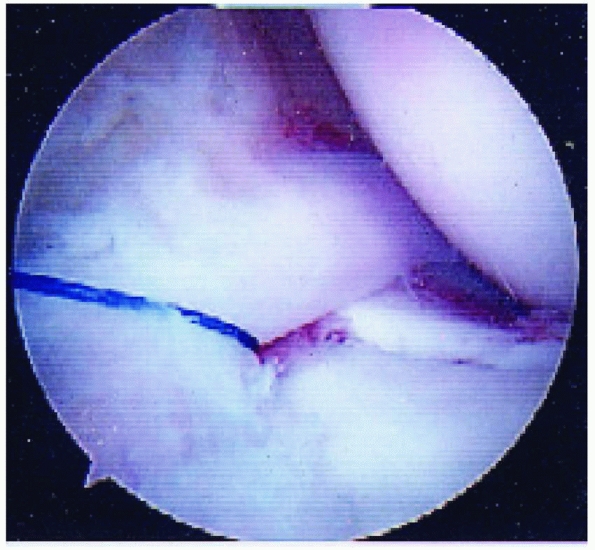
displaced tibial eminence fragment has been reported and may be a
rationale for considering arthroscopic or open reduction in displaced
tibial spine fractures (Fig. 24-5).54,59,94,177
Meniscal entrapment prevents anatomic reduction of the tibial spine
fragment, which may result in increased anterior laxity or a block to
extension.120,148,211,236,240 Furthermore, meniscal entrapment itself may cause knee pain after fracture healing.59 Falstie-Jensen and Sondergard Petersen,94 Burstein and colleagues,54 and Chandler and Miller59
have all reported cases of meniscal incarceration blocking reduction of
type 2 or 3 tibial spine fractures in children. The prevalence of
meniscal entrapment in tibial spine fractures may be common for
displaced fractures. As aforementioned, the anterior horn of the
lateral meniscus typically remains attached to the tibial eminence
fracture fragment. However, the anterior horn of the medial meniscus or
the intermeniscal ligament may become incarcerated. Mah and colleagues200
found medial meniscal entrapment preventing reduction in 8 of 10
children with type 3 fractures undergoing arthroscopic management. In a
consecutive series of 80 skeletally immature patients who underwent
surgical fixation of hinged or displaced tibial eminence fractures
which did not reduce in extension, Kocher et al.177
found entrapment of the anterior horn medial meniscus (n = 36),
intermeniscal ligament (n = 6), or anterior horn lateral meniscus (n =
1) in 26% (6/23) of hinged (type 2) fractures and 65% (37/57) of
displaced (type 3) fractures. The entrapped meniscus can typically be
extracted with an arthroscopic probe and retracted with a retaining
suture (Fig. 24-6).
Studies of the biomechanical strength of internal fixation suggest
similar fixation strength between bioabsorbable and metallic internal
fixation202 and increased fixation strength of suture fixation over internal fixation.87,202
fractures and for type 2 or 3 fractures that reduce closed. Closed
reduction is usually performed after aspiration of the hematoma with
placement of the knee in full extension or 20 to 30 degrees of flexion.
Radiographs are utilized to assess adequacy of reduction. If the
fracture fragment extends into the medial or lateral tibial plateaus,
extension may affect a reduction through pressure applied by medial or
lateral femoral condyle congruence (Fig. 24-7).
Fractures confined within the intercondylar notch, however, will not
reduce in this manner. Portions of the ACL are tight in all knee
flexion positions; therefore, there may not be any one position without
traction being applied by the ACL. Interposition of the anterior horn
medial meniscus or intermeniscal ligament may further block reduction.
to be close reduced (0/57). Bakalim and Wilpulla26 reported successful closed reduction in 10 patients. Smillie275 suggested that closed reduction by hyperextension can be accomplished only with a large fragment. Meyers and McKeever216
recommended cast immobilization with the knee in 20 degrees of flexion
for all type I and II fractures and open reduction or arthroscopic
treatment of all type III fractures.
 |
|
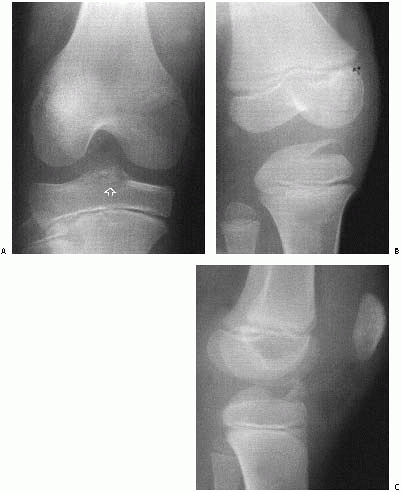
FIGURE 24-3 Stages of displacement of tibial spine fractures. A. Type I fracture, minimal displacement (open arrow). B. Type II fracture, posterior hinge intact. C. Type III fracture, complete displacement and proximal migration.
|
 |
|
FIGURE 24-4 ACL insertion on the tibial eminence.
|
 |
|
FIGURE 24-5 Meniscal entrapment under a tibial eminence fracture.
|
 |
|
FIGURE 24-6 Retraction of an entrapped anterior horn medial meniscus using a retaining suture.
|
type 2 and 3 tibial eminence fractures which do not reduce has been
advocated because of the potential for meniscal entrapment under the
fractured tibial eminence preventing anatomic closed reduction,54,59,94,200 the potential for instability and loss of extension associated with closed reduction and immobilization,120,148,211,236
the ability to evaluate and treat associated intra-articular meniscal
or osteochondral injuries, and the opportunity for early mobilization.
For displaced fractures, Wiley and Baxter307 found a correlation between fracture displacement at healing with knee laxity and functional outcome.
 |
|
FIGURE 24-7 Reduction of type II tibial fracture with knee in 10 to 20 degrees of flexion.
|
 |
|
FIGURE 24-8 Algorithm for the management of tibial eminence fractures in children.
|
Aspiration of hematoma and injection of local anesthetic is performed
under sterile conditions if the patient is in severe pain. A long-leg
cast is applied in 0 to 20 degrees of flexion. The patient and family
are cautioned to elevate the leg to avoid swelling. Radiographs are
repeated in 1 to 2 weeks to ensure that the fragment has not displaced.
The cast is removed 6 weeks after injury. A hinged knee brace is then
used and physical therapy initiated to regain motion and strength.
Patients are typically allowed to return to sports at 3 months after
injury if they demonstrate fracture healing and adequate motion and
strength.
reduction. The hematoma is aspirated and local anesthetic is injected
into the knee under sterile conditions. Reduction is attempted at both
full extension and 20 degrees of flexion.
Radiographs
are taken to assess reduction. If anatomic reduction is obtained, a
long-leg cast is applied in the position of reduction. Follow-up
radiographs are performed at 1 and 2 weeks postreduction to ensure
maintenance of reduction. Length of casting and postcasting management
is similar to type 1 fractures. If the fracture does not reduce
anatomically or if the fracture later displaces, operative treatment is
performed.
reduction; however, this is usually unsuccessful. Operative treatment
is typically performed.
arthroscopic reduction and internal fixation. However, open reduction
through a medial parapatellar incision can also be performed per
surgeon preference/experience or if arthroscopic visualization is
difficult. The author’s preferred fixation is epiphyseal cannulated
screws if the fragment is large or suture fixation if the fragment is
small or comminuted.
positioned supine on the operating room table. A lateral breakaway post
is used. Alternatively, a circumferential post can be utilized. A
standard arthroscope is used in most patients. A small (2.7-mm)
arthroscope is used in younger children. An arthroscopic fluid pump is
used at 35 torr. A tourniquet is routinely used. Standard anteromedial
and anterolateral portals are used. Accessory superomedial and
superolateral portals are used for screw insertion. Prior to insertion
of the arthroscope through the arthroscopic cannula, the large hematoma
is evacuated.
joint, medial compartment, and lateral compartment are essential to
evaluate for concomitant injuries. Usually, some anterior fat pad must
be excised with an arthroscopic shaver for complete visualization of
the intercondylar eminence fragment. Entrapped medial meniscus or
intermeniscal ligament is extracted with an arthroscopic probe and
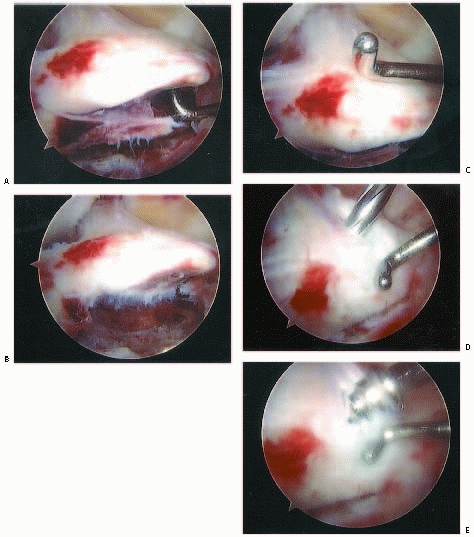
retracted with a retention suture (see Fig. 24-5). The base of the tibial eminence fragment is elevated (Fig. 24-9A) and the fracture bed débrided with an arthroscopic shaver and hand curette (Fig. 24-9B).
Anatomic reduction is obtained using an arthroscopic probe or
microfracture pick with the knee in 30 to 90 degrees of flexion (Fig. 24-9C).
Cannulated guidewires are placed through portals just off the
superomedial and superolateral borders of the patella. A spinal needle
can be helpful for the localization of these portals. The guidewires
are placed into the intercondylar eminence at the base of the ACL.
Fluoroscopic assistance is utilized to confirm anatomic reduction, to
guide correct wire orientation, and to avoid guidewire protrusion
across the proximal tibial physis. A cannulated drill is used over the
guidewires and one or two screws are placed based on the size of the
tibial eminence fragment (Fig. 24-9D). Partially threaded 3.5-mm diameter screws (Fig. 24-9E)
are used in children and 4.5-mm diameter screws are used in
adolescents. The knee is brought through a range of motion to ensure
rigid fixation without fracture displacement and to evaluate for
impingement of the screw heads in extension.
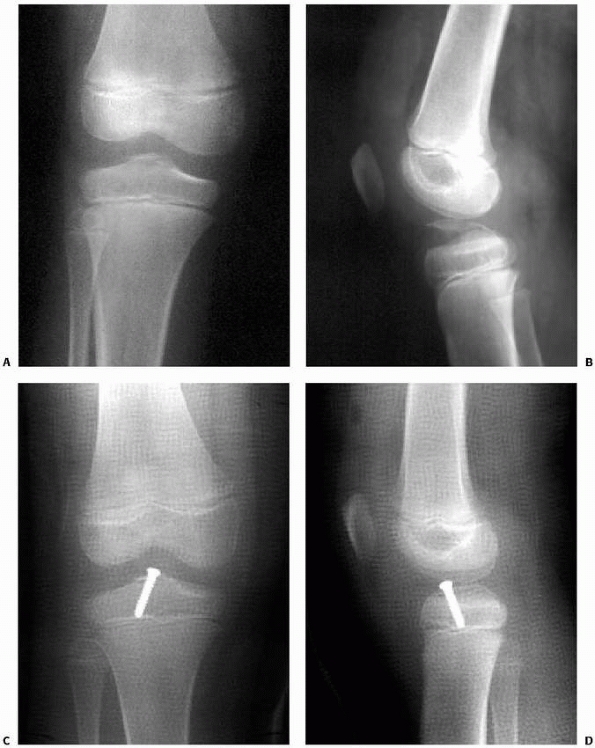
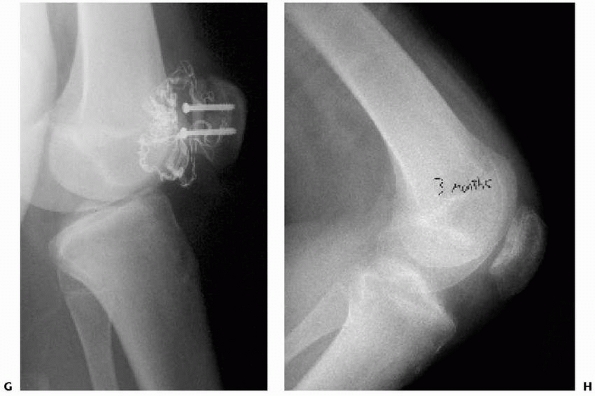
hinged knee brace and maintain touch-down weight bearing for 6 weeks
postoperatively. Motion is restricted to 0 to 30 degrees for the first
2 weeks, 0 to 90 degrees for the next 2 weeks, and then full range of
motion. The brace is kept locked in extension at night. Radiographs are
obtained to evaluate maintainance of reduction and fracture healing (Fig. 24-10).
Cast immobilization for 4 weeks postoperatively may be necessary in
younger children unable to comply with protected weight bearing and
brace immobilization. Physical therapy is routinely utilized to achieve
motion, strength, and sport-specific training. Patients are typically
allowed to return to sports at 12 to 16 weeks postoperatively depending
on knee function. Screws are not routinely removed. Functional ACL
bracing is utilized if there is residual knee laxity.
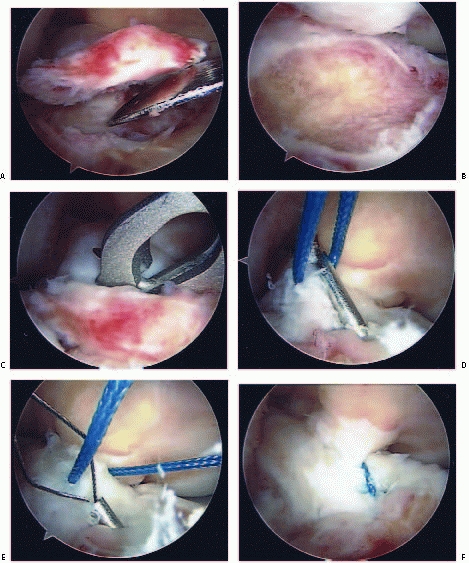
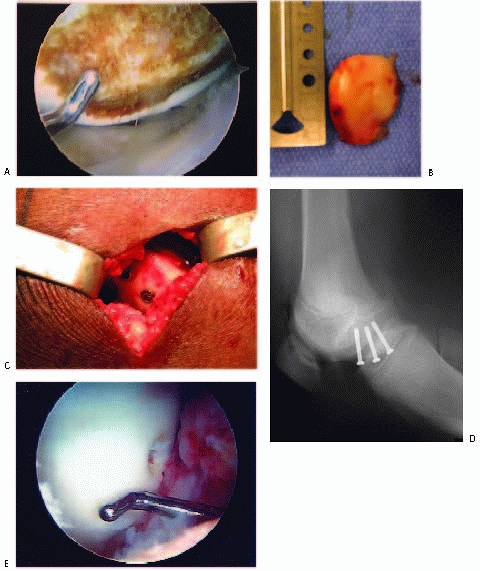
technique described for epiphyseal screw fixation. Accessory
superomedial and superolateral portals are not used. The fracture is
elevated (Fig. 24-11A) and the fracture base débrided (Fig. 24-11B). The fracture is reduced. A suture is passed through the base of the ACL using a suture punch (Fig. 24-11C)
or a suture passer. Two guidewires are placed using the tibial ACL
guide system from a small incision made just below the tibial tubercle.
The guidewires are placed through the base of the intercondylar
eminence fragment (Fig. 24-11D). Suture retrievers are placed through the guidewire tracts, the sutures are retrieved (Fig. 24-11E), and the sutures are tied down onto the tibia (Fig. 24-11F).
The procedure may be repeated for additional sutures. Heavy
nonabsorbable braided sutures or fiberwire is used. Although these
sutures traverse the proximal tibial physis, the risk of growth
disturbance is minimal given the small diameter of the guide wire holes.
-
In the closed management of tibial
eminence fractures, followup radiographs must be obtained at 1 and 2
weeks postinjury to verify maintenance of reduction. Late displacement
and malunion can occur, particularly for type 2 fractures. -
Aspiration of hemarthrosis and injection
of local anesthetic under sterile conditions can be helpful to minimize
pain and allow for full knee extension for attempted closed reduction. -
During arthroscopic reduction and
fixation of tibial spine fractures, arthroscopic visualization can be
difficult unless the large hematoma is evacuated prior to introduction
of the arthroscope. Adequate inflow and outflow is essential for proper
visualization. -
Careful attention to preparation of the fracture bed is important to provide optimal conditions for bony healing.
-
Attempted epiphyseal cannulated screw
fixation of small or comminuted tibial eminence fragments can fail as
the screw may further comminute the fragment. In these cases, suture
fixation is a better method. -
If epiphyseal cannulated screw fixation
is used, fluoroscopy is necessary to ensure that the screw does not
traverse the proximal tibial physis, which may result in a proximal
tibial physeal growth arrest. -
Early mobilization is helpful to avoid
arthrofibrosis which can occur with immobilization. However, in younger
children (less than 7 years old), compliance with protected weight
bearing and brace use can be problematic.
 |
|
FIGURE 24-9 Arthroscopic reduction and cannulated screw internal fixation of a displaced tibial spine fracture. A. Elevation of the tibial eminence fragment. B. Débridement of the fracture bed. C. Reduction of the tibial eminence. D. Drilling over the cannulated screw guidewire. E. Cannulated screw fixation.
|
reduced tibial spine fractures and for operative treatment of displaced
fractures is good. Most series report healing with an excellent
functional outcome despite some residual knee laxity.27,30,36,170,188,200,201,211,212,223,225,276,307,308 Potential complications include nonunion, malunion, arthrofibrosis, residual knee laxity, and growth disturbance.27,30,36,170,188,200,201,211,212,223,225,276,307,308
anatomic reduction and healing of tibial eminence fractures. Baxter and
Wiley30,307
found excellent functional results without symptomatic instability in
17 pediatric knees with displaced tibial spine fractures, despite a
positive Lachman examination in 51% of patients and increased mean
instrumented knee laxity of 3.5 mm. After open reduction and internal
fixation of type III fractures in 13 pediatric knees, Smith276
found instability symptoms in only 2 patients despite a positive
Lachman exam in 87% of patients. In a group of 50 children after closed
or
open treatment, Willis and coworkers308
found excellent clinical results despite a positive Lachman exam in 64%
of patients and instrumented knee laxity of 3.5 mm for type II
fractures and 4.5 mm for type III fractures. Similarly, Janarv et al.148 and Kocher et al.170 found excellent functional results despite persistent laxity even in anatomically healed fractures.
 |
|
FIGURE 24-10
Type III tibial spine fracture in an 11-year-old male child treated with arthroscopic reduction and 3.5-mm cannulated screw fixation. Preoperative anteroposterior (A) and lateral (B) radiographs. Postoperative anteroposterior (C) and lateral (D) radiographs. |
of tibial spine fractures in children is likely related to plastic
deformation of the ACL with tibial spine fracture. At the time of
tibial spine fixation, the ACL often appears hemorrhagic within its
sheath, but grossly intact and in continuity. In a primate animal
model, Noyes and coworkers232 found
frequent elongation and disruption of ligament architecture despite
gross ligament continuity in experimentally produced tibial spine
fractures at both slow and fasting loading rates. This persistent
anteroposterior laxity despite anatomic reduction may be avoided by
countersinking the tibial spine fragment within the epiphysis at the
time of reduction and fixation. However, ACL injury after previous
tibial spine fracture is rare.
with unrecognized injuries of the collateral ligaments or complications from associated physeal fracture.215,276,286
In addition, hardware across the proximal tibial physis may result in
growth disturbance with recurvatum deformity or shortening.226
 |
|
FIGURE 24-11 Arthroscopic reduction and suture fixation of a displaced tibial spine fracture. A. Elevation of the tibial eminence. B. Débridement of the fracture bed. C. Suture passing through the base of the ACL using a suture punch. D. Drilling of a tibial tunnel into the tibial eminence fragment using the ACL tibial guide. E. Retrieval of sutures using a suture passer. F. Appearance after suture fixation.
|
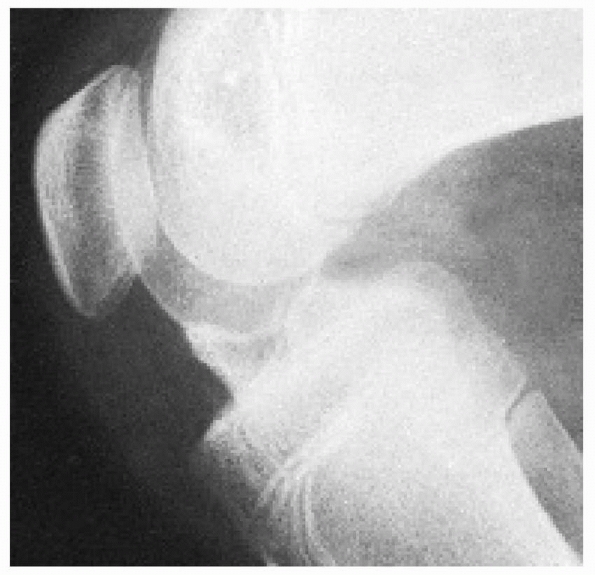
For symptomatic patients, this can be corrected by excision of the
manumitted fragment and anatomic reinsertion of the ACL. Alternatively,
excision of the fragment and ACL reconstruction can be considered in
adults and older adolescents.
 |
|
FIGURE 24-12 Lateral radiograph of a malunited displaced fracture of the intercondylar eminence of the tibia with an extension block.
|
closed can usually be managed by arthroscopic or open reduction with
internal fixation.161,194,296
Technically, débridement of the fracture bed and the fracture fragment
to fresh, bleeding bone is essential to optimize bony healing. Bone
graft may be required in cases of chronic nonunion. Again, excision of
the fragment and ACL reconstruction can be alternatively be considered
in adults and older adolescents.
problem after both nonoperative and operative management of tibial
eminence fractures. The milieu of a major traumatic intra-articular
injury, a large hemarthrosis, and immobilization can predispose to
arthrofibrosis. Avoidance of cast immobilization with early
mobilization utilizing physical therapy can minimize the risk of
arthrofibrosis. Dynamic splinting and aggressive physical therapy can
be employed during the first 3 months from fracture if stiffness is
present. If significant stiffness remains after 3 months from fracture,
patients should be managed with manipulation under anesthesia and
arthroscopy with lyses of adhesions. Overly vigorous manipulation
should be avoided in order to avert iatrogenic proximal tibial or
distal femoral physeal fracture.
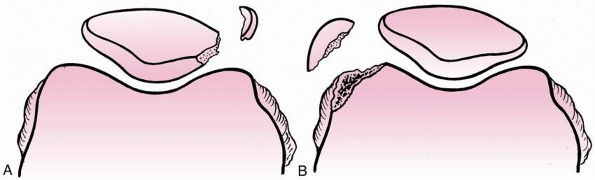
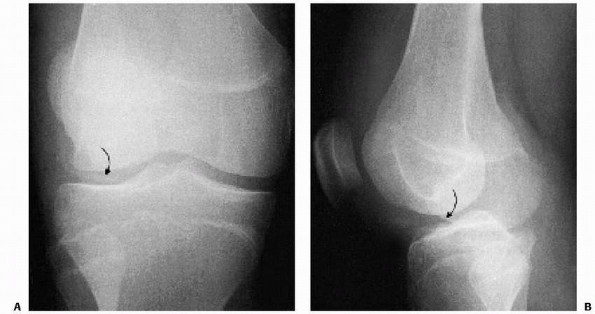
are more common than once thought. They are typically associated with
acute lateral patellar dislocations. The most common locations for
these fractures are the medial patellar facet or the lateral femoral
condyle (Fig. 24-13). The osteochondral
fracture fragments may range from small incidental loose bodies to
large portions of the entire articular surface. The prevalence of
osteochondral fractures associated with acute patella dislocation
ranges from 25% to 50%.13,43,95,206,229,282 Matelic et al.206 found 67% of children presenting with an acute hemarthrosis of the knee had an osteochondral fracture.
 |
|
FIGURE 24-13 Osteochondral fractures associated with dislocation of the right patella. A. Medial facet. B. Lateral femoral condyle.
|
osteochondral fragment may contain only a small ossified portion that
is visible on plain radiographs. MRI may be useful in identifying
associated osteochondral fractures in cases of traumatic patellar
dislocation. Acute osteochondral fractures must be differentiated from
acute chondral injuries, which do not involve subchondral bone, and
osteochondritis dissecans,100,178
which is a repetitive overuse lesion of the subchondral bone that may
result in a nonhealing stress fracture that can progress to fragment
dissection.
small loose bodies and fixation of larger osteochondral fragments. In
cases associated with patellar dislocation, lateral retinacular
release, medial retinacular repair, and medial patellofemoral ligament
repair may be performed adjunctively.
First, a direct blow to the knee with a shearing force applied to
either the medial or lateral femoral condyle can create an
osteochondral fracture. The second mechanism involves a
flexion-rotation injury of the knee in which an internal rotation force
is placed on a fixed foot, usually coupled with a strong quadriceps
contraction. The subsequent contact between the tibia and femur or
patella and lateral femoral condyle causes the fracture. This occurs
during an acute patellar dislocation. As the patella dislocates, the
medial retinaculum tears but the remaining quadriceps muscle-patellar
ligament complex still applies significant compressive forces as the
patella dislocates laterally and shears across the lateral femoral
condyle. The medial border of the patella then temporarily becomes
impacted on the prominent edge of the lateral femoral condyle before it
slides back tangentially over the surface of the lateral femoral
condyle due to pull of the quadriceps. Either the dislocation or the
relocation phase of this injury can cause an osteochondral fracture to
the lateral femoral condyle, the medial facet of the patella, or both (Fig. 24-14).
Interestingly, osteochondral fractures are uncommon with chronic,
recurrent subluxation or dislocation of the patella. In this situation,
the laxity of the medial knee tissues and decreased compressive forces
between the patella and the lateral femoral condyle prevents
development of excessive shear forces.
during sports-related activities. Most patients give a history of a
twisting injury consistent with acute patellar dislocation, but a few
report a direct blow to the lateral or medial femoral condyle,
accounting for a shear injury. The prevalence of osteochondral
fractures associated with acute patella dislocation ranges from 25% to
50% in the literature.13,43,95,206,229,282 Matelic et al.206 found 67% of children presenting with an acute hemarthrosis of the knee had an osteochondral fracture. Nietosvaara et al.229
reported that of 69 acute patellar dislocations in children and
adolescents, 62 (90%) occurred in falls; 39% also had osteochondral
fractures.
 |
|
FIGURE 24-14 Osteochondral fractures associated with dislocation of the patella. A. Medial facet of patella. B. Lateral femoral condyle.
|
On exam, tenderness to palpation over the medial femoral condyle,
lateral femoral condyle, or medial patella is exhibited. The patient
will usually resist attempts to flex or extend the knee and may hold
the knee in 15 to 20 degrees of flexion for comfort. The large
hemarthrosis is due to an intra-articular fracture of the highly
vascular subchondral bone. Joint aspiration may reveal a supernatant
layer of fat if allowed to stand for 15 minutes indicating an
intra-articular fracture. Late exam findings may be similar to those of
a loose body with intermittent locking or catching of the knee.
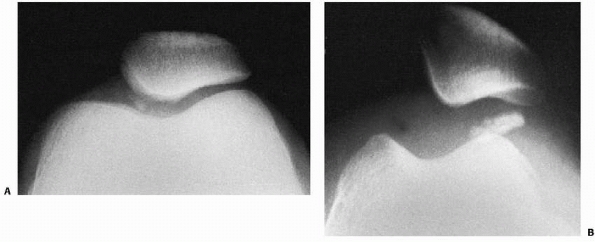
should begin with anteroposterior, lateral, and skyline plain
radiographs. However, a roentgenographic diagnosis can be difficult
because even a large osteochondral fragment may contain only a small
ossified portion that is visible on plain radiographs. A tunnel view
may help locate a fragment in the region of the intercondylar notch.
Because the osteochondral fragment may be difficult to see on plain
radiographs, radiographs must be carefully assessed for even the
smallest ossified fragment (Fig. 24-15).
reported that standard radiographs failed to identify the osteochondral
fracture in 36% of children who had an osteochondral fracture found
during arthroscopy. For this reason, supplemental studies such as MRI
or computed tomography (CT) arthrography may be necessary in cases
where there is high suspicion of osteochondral fracture despite
negative radiographs.48,169,305
Such cases would include an acute traumatic patellar dislocation in a
patient with a large hemarthrosis. Ligamentously lax patients with
chronic, recurrent, atraumatic patellar instability are less likely to
sustain osteochondral fractures. A high-riding patella may also have a
protective effect against associated intra-articular osteochondral
fractures. Patients with an Insall index greater than 1.3 have a
decreased chance of sustaining an osteochondral fracture compared with
patients that have an Insall index within normal limits.48
An arthrogram effect is usually present during MRI given the large
hemarthrosis. Arthroscopic examination can also be done as the
definitive diagnostic (and potentially therapeutic) test.
knee is based on the site, the type, and the mechanism of injury. The
classification outlined in Table 24-1 is based on the descriptions of osteochondral fractures by Kennedy160 and Smillie.275
the medial and lateral femoral condyles during flexion and extension of
the knee.113,142
With increasing knee flexion, the contact area on the articular surface
of the patella moves to the proximal patella. Between 90 and 135
degrees of flexion, the patella glides into the intercondylar notch
between the femoral condyles. The two primary areas of contact are the
medial patellar facet with the medial femoral condyle and the
superolateral quadrant of the lateral patellar facet with the lateral
femoral condyle. Soft tissue support for the patellofemoral joint
includes the quadriceps muscle, the medial patellofemoral ligament, the
patellar tendon, and the vastus medialis and lateralis muscles.
but the rest of the quadriceps muscle-patellar ligament complex
continues to apply significant compression forces as the patella
dislocates laterally. These forces are believed to cause fracture of
the medial patellar facet, the lateral femoral condyle articular rim,
or both (see Fig. 24-13).160,234,254
Osteochondral fractures are uncommon with chronic recurrent subluxation
or dislocation of the patella because of laxity of the medial
retinaculum and lesser compressive forces on the patella and the
lateral femoral condyle.
 |
|
FIGURE 24-15 Osteochondral fracture of lateral femoral condyle after patellar dislocation. A. Fragment seen in lateral joint space. B. Lateral view.
|
helped to explain the occurrence of osteochondral fractures in the
skeletally immature at a ultrastructural level. They noted that in the
joint of a juvenile, interdigitating fingers of uncalcified cartilage
penetrate deep into the subchondral bone providing a relatively strong
bond between the articular cartilage and the subchondral bone. In the
adult, the articular cartilage is bonded to the subchondral bone by the
well-defined calcified cartilage layer, the cement line. When shear
stress is applied to the juvenile joint, the forces are transmitted
into the subchondral bone by the interdigitating cartilage with the
resultant bending forces causing the open pore structure of the
trabecular bone to fail. In mature tissue, the plane of failure occurs
between the deep and calcified layers of the cartilage, the tidemark,
leaving the osteochondral junction undisturbed. Although the juvenile
and adult tissue patterns are different, they both provide adequate
fracture toughness to the osteochondral region. As the tissue
transitions, however, from the juvenile to the adult pattern during
adolescence, the fracture toughness is lost. The calcified cartilage
layer is only partially formed and the interdigitating cartilage
fingers are progressively replaced with calcified matrix. Consequently,
the interface between the articular cartilage and the subchondral bone
becomes a zone of potential weakness in the joint which may explain why
osteochondral fractures are seen frequently in adolescents and young
adults.
|
TABLE 24-1 Mechanism of Osteochondral Fractures
|
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
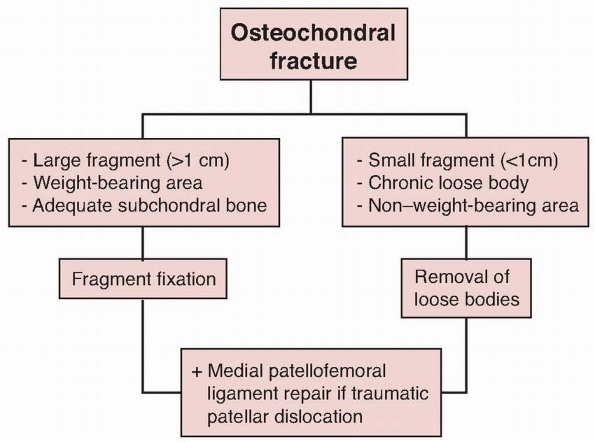
fractures of the knee is either surgical removal of the fragment or
fixation of the fragment.176
involves a weight-bearing area, and has adequate cortical bone attached
to the chondral surface, then fixation should be attempted.113,160,276,281,310,311
This can be done via arthroscopy or arthrotomy. Fixation options
include Kirschner wires, Steinmann pins, cannulated screws, and
variable pitch headless screws. Hardware removal is typically performed
after fracture healing. Lewis and Foster190
reported good results in eight osteochondral fractures after fixation
with Herbert bone screws without need for hardware removal. More
recently, bioabsorbable fixation devices are available which may
eliminate the need for hardware removal.
or from a non-weight-bearing region of the knee, then removal of loose
bodies is recommended.9,141,149,254,263
The fragment’s crater should be débrided to stable edges, and the
underlying subchondral bone should be perforated to encourage
fibrocartilage formation.
dislocation, concomitant repair of the medial retinaculum and medial
patellofemoral ligament at the time of fragment excision or fixation
may decrease the risk of recurrent patellar instability.64,253
 |
|
FIGURE 24-16 Algorithm for the management of osteochondral fracture in children.
|
dislocation with a large hemarthrosis, MRI is performed if initial
radiographs do not show any associated osteochondral fracture. If MRI
does not reveal any associated osteochondral fracture, these patients
are treated with a brief (1 to 2 weeks) period of immobilization,
followed by patellofemoral bracing and physical therapy emphasizing
patellar mobilization, straight-leg raises, progressive resistance
exercises, and vastus medialis strengthening. Routine diagnostic
arthroscopy and routine medial patellofemoral ligament repair are not
performed on initial patellofemoral dislocators. Patients are allowed
to return to sports 6 to 12 weeks after dislocation depending on their
patellar alignment and rehabilitation.
chronic loose bodies, and fractures involving nonweightbearing areas
are treated with arthroscopic removal of loose bodies. The fragment’s
crater is débrided to stable edges to prevent further loose bodies and
the underlying subchondral bone should be perforated to encourage
fibrocartilage formation. Lateral retinacular release with medial
retinacular/patellofemoral ligament repair is performed adjunctively in
cases of traumatic patellofemoral dislocation to decrease the risk of
recurrent patellofemoral instability.
involving weight-bearing areas with adequate subchondral bone are
treated with fragment fixation. At times, these osteochondral fracture
fragments can be very large, involving nearly the entire weight-bearing
surface of the medial patellar facet (Fig. 24-17) or lateral femoral condyle (Fig. 24-18).
Medial patellar facet osteochondral fractures can be fixed through an
open lateral retinacular release by manually tilting the patella (see Fig. 24-17). Lateral femoral condyle osteochondral fractures typically require an oblique lateral arthrotomy for fragment fixation (see Fig. 24-18).
Z-knee retractors are helpful for exposure, and the knee is flexed or
extended to optimize visualization of the fracture bed. The
osteochondral fracture fragment and the fracture bed are débrided of
fibrous tissue to healthy bone. The fragment is replaced anatomically.
Countersunk cannulated screws (3.5-or 4.5-mm) or Herbert screws are
preferred for fixation because of the strength of fixation that allows
for fragment compression and early mobilization. Lateral retinacular
release with medial retinacular/patellofemoral ligament repair is
performed adjunctively in cases of traumatic patellofemoral dislocation
to decrease the risk of recurrent patellofemoral instability.
fragment can begin range-of-motion exercises immediately. Crutches may
be necessary in the immediate postoperative period but patients can
progress to weight bearing as tolerated. After osteochondral fracture
fixation, patients are treated with touch-down weight bearing in a
postoperative brace until fracture healing. Range of motion is allowed
from 0 to 30 degrees for the first 2 weeks, followed by 0 to 90 degrees
until fracture healing. The fracture is typically healed by 6 to 8
weeks postoperatively, and arthroscopy is then performed to confirm
fragment healing, remove hardware, and assess the integrity of the
articular surface. Return to athletic activities is permitted when full
range of motion is recovered and strength is symmetric.
-
An important pitfall to avoid is the
failure to diagnose osteochondral fractures associated with acute,
traumatic patellar dislocations. Radiographs should be scrutinized for
small osseous fragments, and MRI should be obtained in cases with
negative radiographs despite a high clinical suspicion for
osteochondral fracture. -
In cases of arthroscopic removal of loose
bodies associated with acute, traumatic patellar dislocation, strong
consideration should be given to repair of the medial structures
(medial retinaculum and medial patellofemoral ligament) in order to
decrease the risk of recurrent patellar instability. -
In cases of osteochondral fracture fixation, adequate internal fixation must be obtained to allow for early motion.
-
Screw heads should be countersunk or
headless, variable pitch screws should be used in order to avoid
scuffing of articular surfaces. -
In children or adolescents with growth
remaining, care must be taken to prevent crossing the distal femoral
physis with hardware.
involving the weight-bearing portion of the joint usually have a good
prognosis after removal of loose bodies.
involving the weight-bearing surfaces is more variable. Excision of
large fragments involving the weight-bearing articular surfaces
predictably leads to the development of degenerative changes.16
Fracture fixation resulting in fragment healing with a congruous
articular surface offers the best long-term prognosis; however, even
these cases may develop crepitus, stiffness, and degenerative changes.8
 |
|
FIGURE 24-17 Fixation of a medial patellar facet osteochondral fracture in an adolescent male athlete. A. Skyline radiograph demonstrating a fracture of the medial patellar facet with the fragment in the lateral recess. B. Axial MRI demonstrating medial facet fracture and loose fragment. C. Arthroscopic view of osteochondral fragment in the lateral recess. D. Open view of patella. E. Open view of osteochondral fragment. F. Open view of reduction and cannulated screw fixation of medial patellar facet.
|
with further osteochondral injury after both excision of loose bodies
and fracture fixation. Concomitant medial patellofemoral ligament
repair appears to decrease the risk of recurrent instability.29,253
Stiffness may occur, particularly after fracture fixation. Adequate
internal fixation is necessary to allow for early motion, which
decreases the risk of loss of motion. Stiffness may be treated with
aggressive therapy and dynamic splinting during the first 3 to 4 months
after injury. Beyond this time frame, manipulation under anesthesia
with arthroscopic lysis of adhesions is typically required. Nonunion
after fragment fixation may also occur, necessitating further attempts
at fracture fixation or fracture excision. Excision of larger
osteochondral fractures involving the weight-bearing articular surfaces
requires associated chondral resurfacing, such as marrow stimulation
procedures (microfracture), osteochondral grafting (mosaicplasty),
or autologous chondrocyte implantation.34,38,242,283
Complications related to hardware for fracture fixation may also occur.
Proud screw heads may scuff articular surfaces. Bioabsorbable implants
may result in synovitis with sterile effusions.
 |
|
FIGURE 24-17 (continued) G. Intraoperative lateral radiograph after fracture fixation. H. Lateral radiograph 3 months after fracture fixation and 6 weeks after screw removal demonstrating healing.
|
all subluxations and dislocations from varying causes are considered.
Patellar instability involves cases ranging from acute, traumatic
patellar dislocation to chronic, recurrent patellar subluxation in a
patient with ligamentous laxity.
in adolescents. Acute patellar dislocations in younger children usually
occur in the context underlying patellofemoral dysplasia.213
Chronic, atraumatic, recurrent patellofemoral instability occurs most
often in adolescent females, with underlying laxity and alignment risk
factors.
associated osteochondral fracture are treated with a short period of
immobilization followed by patellofemoral bracing and rehabilitation.
Acute, traumatic patellar dislocations with osteochondral fractures are
treated as discussed in the previous section with removal of loose
bodies or fracture fixation. Chronic, recurrent, atraumatic
patellofemoral instability is typically treated with patellofemoral
bracing, rehabilitation, and orthotics if needed. Recurrent
patellofemoral instability which has been recalcitrant to nonoperative
treatment can be managed with a variety of proximal and distal
realignment procedures.
flexion-rotation injury of the knee in which an internal rotation force
is placed on a fixed foot, usually coupled with a strong quadriceps
contraction. As the patella dislocates, the medial retinaculum and
medial patellofemoral ligament tear but the remaining quadriceps
muscle-patellar ligament complex still applies significant compressive
forces as the patella dislocates laterally and shears across the
lateral femoral condyle. This may result in associated osteochondral
fracture.
extended. Patellar dislocations are likely to be caused by falls,
gymnastics, dancing, cheerleading, and a wide variety of other
activities. Acute patellar dislocation also should be considered in the
evaluation of all athletic knee injuries in adolescents and young
adults.
often give a history of a twisting injury. Patients may remember
feeling or seeing the patella in a laterally displaced position. Most
acute patellar dislocations spontaneously reduce or reduce with
incidental knee extension. It is more unusual to see a patient with a
patellar dislocation which is unreduced (Fig. 24-19). Patients may report a “pop” associated with dislocation and a second “pop” associated with spontaneous reduction.
with any attempt passively to displace the patella. Patients may have a
positive apprehension test with lateral translation of the patella. A
defect may be palpable in the medial attachment of the vastus medialis
obliqus to the patella if the medial retinaculum is completely avulsed.
Tenderness on the lateral aspect of the knee usually is not as severe
as on the medial side. Hemorrhage into the joint may cause
hemarthrosis, and severe hemarthrosis should suggest the possibility of
an osteochondral fracture.253 Nietosvaara et al.229
reported that of 72 patients with acute patellar dislocations, 28 (39%)
had associated osteochondral fractures. These fractures included 15
capsular avulsions of the medial patellar margin and 15 loose
intra-articular fragments detached from the patella, the lateral
femoral condyle, or both. All knee ligaments should be carefully
evaluated because the mechanism of patellar dislocation may cause
associated ligamentous injuries.
 |
|
FIGURE 24-18 Fixation of a lateral femoral condyle osteochondral fracture in an adolescent female athlete. A. Arthroscopic view of the lateral femoral condyle. B. Open view of the fracture fragment. C. Open view of fracture fixation using cannulated screws through a limited lateral arthrotomy. D. Six weeks postoperative lateral radiograph demonstrating fracture healing. E. Arthroscopic appearance at the time of screw removal 6 weeks postoperatively.
|
primarily to detect any associated osteochondral fracture.
Occasionally, an osteochondral fragment from the medial aspect of the
patella or the lateral femoral condyle is visible on the
anteroposterior or lateral view. The classic “sunrise” view is
difficult to obtain in a child after acute dislocation because the
required positioning of the knee causes pain. Rarely, stress
radiographs may be obtained for evaluation of suspected physeal
fracture or ligamentous injury. CT or MRI may be valuable to check for
an osteochondral fracture.
 |
|
FIGURE 24-19 Acute dislocation of the left patella in a 6-year-old boy.
|
dislocations in children, acute dislocation should be distinguished
clinically from chronic patellar subluxation or dislocation.51,81,103,112 Approximately 15% of children with acute patellar dislocations experience recurrent dislocations. Cash and Hughston58
reported a 60% incidence of redislocation in patients 11 to 14 years of
age, 30% in patients 19 to 28 years of age, and in only one patient
older than 28 years of age.
mechanism. As the insertion site of all muscle components of the
quadriceps complex, it serves biomechanically to provide an extension
moment during range of motion of the knee joint. The trochlear shape of
the distal femur stabilizes the patella as it tracks through a range of
motion. The hyaline cartilage of the patella is the thickest in the
body.
patella contacts a relatively small area of the femoral groove. With
further flexion, the contact area moves superiorly and increases in
size. The medial facet of the patella comes in contact with the femoral
groove only when flexion reaches 90 to 130 degrees.
mm and lateral femoral condyle height is 3.4 mm. The patellar articular
cartilage is 6 to 7 mm deep, the thickest articular cartilage in the
body and a reflection of the joint’s inherent incongruity. The usual
normal lateral alignment of the patella is checked by the medial
quadriceps expansion and focal thickening of the capsule in the areas
of the medial patellofemoral and medial meniscopatellar ligaments.78
Dynamic stability depends on muscle forces, primarily the quadriceps
and hamstrings acting through an elegant lower extremity articulated
lever system that creates and modulates forces during gait. The
quadriceps blends with the joint capsule to provide a combination of
dynamic and static balance. Tightness or laxity of any of the factors
involved with maintenance of the balance leads to varying levels of
instability. Acute patellar dislocation almost always is in a lateral
direction unless it is due to a medially oriented direct blow or
follows over vigorous lateral retinacular release. Sallay et al.259
demonstrated avulsions of the medial patellofemoral ligament from the
femur in 94% (15 of 16) of patients during surgical exploration after
acute patellar dislocation. Desio et al.,78
using a cadaveric serial cutting model, found that the medial
patellofemoral ligament provided 60% of the resistance to lateral
patellar translation at 20 degrees of knee flexion. The medial
patellomeniscal ligament accounted for an additional 13% of the medial
quadrant restraining force. If the deficit produced by attenuation of
the medial vectors after acute dislocation is not eliminated,
patellofemoral balance is lost, resulting in feelings of giving way and
recurrent dislocation.
compressive load during activity. It has been estimated that at 60
degrees of knee flexion, the forces across the patellofemoral
articulation are three times the body weight and increase to over seven
times the body weight during full knee flexion with weight-bearing.
position in relation to the patellar tendon. This alignment can be
approximated by a line drawn from the anterosuperior iliac spine to the
center of the patella. The force of the patellar tendon is indicated by
a line drawn from the center of the patella to the tibial tubercle. The
angle formed by these two lines is called the quadriceps angle or Q angle (Fig. 24-20).
As this angle increases, the pull of the extensor mechanism tends to
sublux the patella laterally. Recurrent patellar dislocation is most
likely associated with some congenital or developmental deficiency of
the extensor mechanism, such as patellofemoral dysplasia, deficiency of
the vastus medialis obliquus, or an increased Q angle with valgus
malalignment of the quadriceps-patellar tendon complex.
appropriate sedation, reduction is done by flexing the hip to relax the
quadratus femoris, gradually extending the knee, and gently pushing the
patella medially back into its normal position. Gentle reduction should
be emphasized to avoid the risk of osteochondral fracture associated
with patellar relocation.
 |
|
FIGURE 24-20
The Q angle. Normal valgus alignment of the quadriceps mechanism: line drawn from the anterosuperior iliac spine to center of the patella, line drawn from center of the patella to tibial spine. |
Most patellar dislocations are treated nonoperatively with
immobilization, followed by patellofemoral bracing and rehabilitation.
Surgical repair may be indicated if the vastus medialis obliquus and/or
medial patellofemoral ligament is completely torn from the medial
aspect of the patella, leaving a large, palpable soft tissue gap. If
osteochondral fracture has occurred, arthroscopy/arthrotomy may be
indicated for removal or repair of an osteochondral loose body as
discussed in the previous section.
recalcitrant to nonoperative treatment is typically managed through
various proximal/distal patellofemoral realignment procedures. Surgical
options include isolated or combination procedures including lateral
retinacular release, medial retinacular plication, extensor mechanism
realignment, Galeazzi semitendinosis tenodesis, patellar tendon
hemitransfer, and tibial tunbercle osteotomy. Tibial tubercle osteotomy
is contraindicated in patients with an open tibial tubercle apophysis
due to the risk of a growth arrest resulting in recurvatum deformity.
Recently, increased attention has been paid to medial patellofemoral
ligament reconstruction.31,53,74
 |
|
FIGURE 24-21 Chronic lateral patellar subluxation in a 13-year-old girl.
|
osteochondral fracture are treated by closed methods with satisfactory
results. A cylinder cast or knee immobilizer is used for 2 weeks.
Patients are allowed full weight bearing as tolerated. After
immobilization, the patient is placed in a patellofemoral brace with a
lateral bolster. Physical therapy is begun, emphasizing straight-leg
raises, progressive resistance exercises, patellar mobilization, and
vastus medialis strengthening. Structural risk factors such as lateral
patellar tightness and pes planus with pronation are addressed.
Patients are allowed to return to sports 6 to 12 weeks after injury,
depending on their patellofemoral mechanics and rehabilitation.
for an associated osteochondral fracture, as described in the previous
section. Removal of loose bodies or fracture fixation is performed.
Adjunctive medial retinacular repair and medial patellofemoral ligament
repair is usually also performed to reduce the risk of recurrent
patellar instability.
adolescents, especially girls. Several risk factors have been
identified in children likely to have chronic subluxation or
dislocation, including age younger than 16 years, radiographic evidence
of dysplasia of the patella or lateral femoral condyle, significant
atrophy of the vastus medialis obliquus, hypermobility of the patella,
and multiple previous dislocations (Fig. 24-21).
Initial treatment of chronic patellar subluxation or dislocation in
adolescents is immobilization followed by aggressive physical therapy
for rehabilitation of the vastus medialis obliquus and quadriceps
muscles. Surgical intervention is warranted in children with several
risk factors who do not respond to this treatment regimen and continue
to have subluxation or dislocation.40,132,186,199 Micheli and Stanitski219
reviewed 33 skeletally immature patients with lateral retinacular
releases and found that the procedure did not interfere with permanent
alignment of the extensor mechanism. They recommended the technique for
children who do not respond to an aggressive physical therapy program.
The author usually performs medial retinaculum/medial patellofemoral
ligament repair with lateral retinacular release for cases of patellar
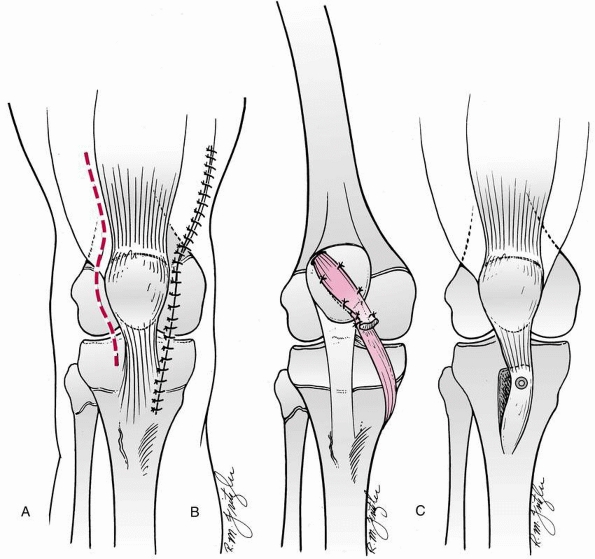
instability (Fig. 24-22A).
lateral release and medial repair, further correction of the medial
deficiency is indicated. Galeazzi transfer of the semitendinosis
through the inferior pole of the patella also has been reported in
skeletally immature patients (Fig. 22-22B).125
This may be indicated in adolescents with continued instability after
lateral release and medial realignment, or in children with associated
connective tissue disorders. In lieu of Galeazzi transfer, medial
patellofemoral ligament reconstruction may be considered.31,53,74
In skeletally mature patients with a significantly abnormal Q angle,
tibial tubercle osteotomy usually achieves good results. This technique
displaces the anterior tibial tubercle medially to decrease the Q angle
and anteriorly to reduce the patellofemoral contact forces (Fig. 24-22C).
Tibial tubercle osteotomy is contraindicated in patients with open
physes because of the possibility of growth disturbance of the anterior
tibial tubercle, with resulting genu recurvatum.
-
Unrecognized associated osteochondral fractures may present later as loose bodies.
-
Unrecognized associated ligamentous injury can present later as knee instability.
-
Aggressive nonoperative treatment should
be pursued for cases of patellofemoral instability before considering
surgical management. -
Patients with recurrent patellar
instability, particularly children, should be evaluated for underlying
patellofemoral dysplasia. -
Overzealous and injudicious use of lateral retinacular release may result in iatrogenic medial patellar instability.
 |
|
FIGURE 24-22 Surgical technique for treatment of chronic patellar subluxation or dislocation. A. Lateral retinacular release and medial imbrication. B. Semitendinosis tenodesis. C. Elmslie-Trillat procedure.
|
generally good. Approximately 1 in 6 children with acute patellar
dislocations experiences recurrent dislocations. Patients with a
younger age at first dislocation are at higher risk for recurrent
instability. Cash and Hughston58 noted 75% satisfactory results after nonoperative treatment in carefully selected patients.
instability. Lateral release alone without medial retinaculum/medial
patellofemoral ligament repair may not adequately prevent recurrent
dislocation. Stiffness, with lack of knee flexion, may occur after
Galeazzi tenodesis, if the graft is overly tensioned. After tibial
tubercle osteotomy, nonunion, hardware failure, neurovascular injury,
and compartment syndrome have been reported.
Meniscal disorders include meniscal tears, discoid meniscus, and
meniscal cysts. The exact incidence of meniscal injuries in children
and adolescents is unknown. King164
reported 52 patients younger than 15 years of age who had undergone
arthrotomy because of suspected meniscal injuries, and Fowler102
reported 117 meniscectomies in patients 12 to 16 years of age. Meniscal
injuries under the age of 10 are rare, unless associated with a discoid
meniscus.‡ The incidence of meniscal, as well as other intra-articular disorders, increases with age.73
With adolescence, increased size and speed, and increased athletic
demands, come higher-energy injuries and an increase of intra-articular
lesions.
adults. It is estimated that longitudinal tears comprise 50% to 90% of
meniscal tears in children and adolescents.176 Bucket-handle displaced tears are not uncommon (see Fig. 24-1). Also in these age groups, meniscal injuries are commonly associated with ACL injuries.57,88,177,203 Cannon57
estimated that repairable meniscal tears occur in 30% of all knees with
acute ACL rupture and in 30% of patients under 20 years old.
Approximately two thirds of repairable meniscal tears are associated
with ACL rupture, with the majority of these tears limited to the
posterior horn.
lateral meniscal tears in the pediatric and especially the adolescent
age group.281 There appears to be a relatively increased incidence
of lateral tears in the preadolescent age group, which may be due to the existence of lateral discoid menisci.176
traumatic in nature in children and adolescents. Multiple studies have
shown that between 80% to 90% of meniscal injuries in children and
adolescents are sustained during sporting activities.5,117,118,203,282
These numbers may be lower in the preadolescent age group. Meniscal
tears most commonly occur with twisting motions, associated frequently
with football, soccer, and basketball.
the flexed knee moves toward extension. This rotational force with the
knee partially flexed changes the relation of the femoral condyles to
the menisci, and forces the menisci toward the center of the joint,
where they are likely to be injured. These twisting mechanisms occur
primarily in sports and may cause associated ligamentous injuries.
Meniscal injuries also may be associated with degenerative changes,
cyst formation, or congenital anomalies.102
Other complaints include mechanical symptoms such as snapping,
catching, and locking. A bucket-handle tear that is displaced into the
intercondylar notch may present with a locked knee or a knee unable to
fully extend.
pediatric patient includes conditions resulting in a traumatic effusion
such as as ligamentous injury, osteochondral fracture, chondral injury,
and patellofemoral dislocation. In addition, conditions causing joint
line pain must be distinguished from meniscal tears, such as plica
syndrome, iliotibial friction band syndrome, osteochondritis dissecans,
and bone bruises.176
adolescents can be difficult to make. Due to the diversity of pathology
and the difficulty of examination of children, diagnostic accuracy of
clinical exam for meniscus tear has been shown to be as low as 29% to
59%.169,176
An accurate history may be difficult to obtain in a very young child.
The older the patient, the more likely a history of specific injury.
The patient usually relates feeling or hearing a “pop” at the time of
injury, with frequent popping and giving way after injury. Pain is
reported by approximately 85% of patients, with tenderness over the
affected joint line. More than half report giving way and effusion of
the knee joint. McMurray’s and Apley’s tests may be helpful in the
diagnosis of a chronic lesion, but with acute injury the knee usually
is too painful to allow these maneuvers.69
series of patients with documented meniscal tears, almost one third of
the patients had no significant findings on physical examination. The
classic McMurray test may be of little value in this age group whose
tears are peripheral and not degenerative posterior horn lesions.176
The most accurate physical findings are joint line tenderness
(especially middle to posterior) and exacerbation of the pain with
varus (medial), valgus (lateral), and rotation stress (internal,
medial; external, lateral) at 30 to 40 degrees of knee flexion. Two
recent studies, by examiners with pediatric sports medicine experience,
have shown the diagnostic accuracy of clinical exam to be 86.3% and
93.5% overall.169,280
When medial meniscus tears were looked at alone, the sensitivity and
specificity of clinical exam were 62.1% and 80.7%, respectively.169 The sensitivity and specificity for lateral meniscal tears were 50% and 89.2%, respectively.169
meniscal injuries in children. MRI accuracy rates reportedly range from
45% to 90% in the diagnosis of meniscal tears.47,146,243,269 Sensitivity and specificity of 83% and 95%, respectively, has been shown in skeletally immature patients.169,279 Kocher et al.169
showed that for medial meniscal tears, the sensitivity and specificity
for MRI diagnosis was 79% and 92%, respectively. For lateral meniscal
tears, these numbers were 67% and 83%, respectively.169
In recent studies that compared the diagnostic accuracy of physical
exam versus MRI, clinical exam rates were equivalent or superior to MRI.152,169 These authors recommended judicious use of MRI in evaluating intra-articular knee disorders.
These signal changes do not extend to the superior or inferior
articular surfaces of the meniscus and likely represent vascular
developmental changes.176 Takeda et al.288
reviewed the MRI signal intensity and pattern in the menisci of 108
knees in 80 normal children 8 to 15 (average 12.2) years of age using
the classification of Zobal et al.,318
which allows for equivocation for type III signals. Using tibial
tubercle maturity as a definition of skeletal maturity, Takeda et al.288
found signal intensity to be proportional to age, with high signal
(grades III and III) evident in 80% of patients 10 years of age or
younger, 65% by 13 years of age, and 33% at 15 years of age, similar to
the false-positive rate of 29% reported in asymptomatic adults.111,184
Overall, two thirds of the patients had positive findings (grades II or
III), often grade III-A, which is equivocal extension through the
surface of the meniscus. Takeda et al.288
suggested that the decrease in signal intensity was proportional to
diminution of peripheral vascularity, especially in the posterior horn
of the meniscus. These investigators cautioned against
misinterpretation of pediatric knee MRI and emphasized the necessity
for correlation of the clinical findings with any imaging study
results. When interpreting an MRI of the developing knee, care must be
taken to identify a meniscal tear only when linear signal changes
extend to the articular surface. As with any test, clinical correlation
is mandatory before treatment decisions are made.
versus lateral), the location of the tear (posterior horn, body,
anterior
horn),
the chronicity of the tear (acute (<3 weeks), chronic (>3 weeks),
and the tear pattern (peripheral, bucket-handle, horizontal cleavage,
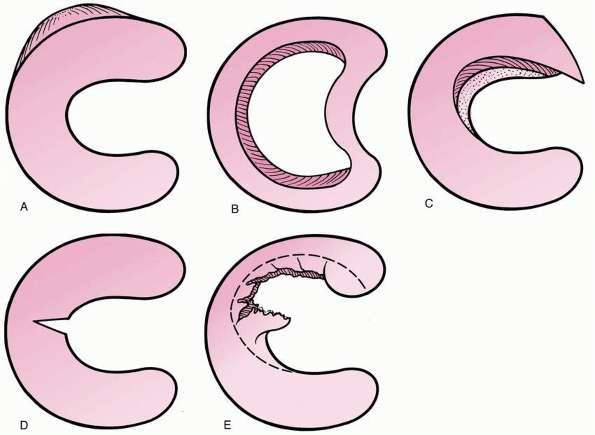
transverse, or complex) (Fig. 24-23).
Other important factors include site of the tear (outer third, middle
third, inner third), stability, and associated ligamentous and chondral
injuries.
 |
|
FIGURE 24-23 Meniscal tears in adolescents. A. Peripheral. B. Bucket-handle. C. Horizontal cleavage. D. Transverse. E. Complex.
|
By week 14, they assume the normal mature anatomic relationships. At no
point during their embryology are the menisci discoid in morphology.157
Thus, the discoid meniscus represents an anatomic variant, not a
vestigial remnant. The developmental vasculature of the menisci has
been studied extensively by Clark.62
The blood supply arises from the periphery and supplies the entire
meniscus. This vascular pattern persists through birth. During
postpartum development, the vasculature begins to recede and, by the
ninth month, the central third is avascular. This decrease in
vasculature continues until approximately age 10, when the menisci
attain their adult vascular patter. Injection dye studies by Arnoczky
and Warren22 have shown that only
the peripheral 10% to 30% of the medial and 10% to 25% of the lateral
meniscus receive vascular nourishment.
larger in anterior-posterior width than the anterior horn. The medial
meniscus covers approximately 50% of the medial tibial plateau. The
medial meniscus is attached firmly to the medial joint capsule through
the meniscotibial or coronary ligaments. There is a discrete capsular
thickening at its midportion which constitutes the deep MCL. The
inferior surface is flat and the superior surface concave so that the
meniscus conforms to its respective tibial and femoral articulations.
To maintain this conforming relationship, the medial meniscus
translates 2.5 mm posteriorly on the tibia as the femoral condyle rolls
backward during knee flexion.117,118
covers a larger portion, approximately 70%, of the lateral tibial
plateau. The lateral meniscus is more loosely connected to the lateral
joint capsule. There are no attachments in the area of the popliteal
hiatus and the fibular collateral ligament does not attach to the
lateral meniscus. Accessory meniscofemoral ligaments exist in up to one
third of cases. These arise from the posterior meniscus. If this
ligament inserts anterior to the PCL, it is known as the ligament of
Humphrey; if it inserts posterior to the PCL, it is known as the
ligament of Wrisberg. Due to the lack of restraining forces, the
lateral meniscus is able to translate 9 to 11 mm on the tibia with knee
flexion. This may account for the lower incidence of lateral meniscal
tears. Both menisci are attached anteriorly via the anterior transverse
meniscal ligament.117,118
medial and lateral geniculate arteries. These vessels form a
perimeniscal synovial plexus. There may be some contribution from the
middle geniculate artery. King,165
in the 1930s, published classic research indicating that the peripheral
meniscus did communicate with the vascular supply and thus was capable
of healing. It is believed that the inner two thirds of the meniscus
receives its nutrition through diffusion and mechanical pumping.
VI collagen are also present. The collagen fibers are oriented
primarily in a circumferential pattern, parallel with the long access
of the meniscus.117,118
There are also radial, oblique, and vertically oriented fibers.
Proteoglycans and glycoproteins are present in smaller concentrations
than in articular cartilage. The menisci also contain neural elements
including mechanoreceptors and type I and II sensory fibers. In a
sensory mapping study, Dye82
demonstrated that the probing of the peripheral meniscus led to pain
where as stimulation of the central meniscus elicited little or no
discomfort.
characterized the menisci as “functionless remnants of intra-articular
leg muscles.” The sentiment was held onto through the 1970s, when
menisci were routinely excised. Fairbanks,93
in 1948, published the first long-term follow-up of patients after
total menisectomy. His article warned that degenerative changes
followed menisectomy in a substantial proportion of patients. Now,
several reports have established the deleterious consequences of total
and even partial meniscectomy.5,71,88,176,203,214,246,248,295,303,313
Nowhere are these facts more important than in children and
adolescents, in whom the long-term effects of menisectomy will be
magnified by the activity level and longevity.
The menisci serve to increase contact area and congruency of the
femoral tibial articulation. This allows the menisci to participate in
load sharing and reduces the contact stresses across the knee joint. It
is estimated that the menisci transmit up to 50% to 70% of the load in
extension and 85% of the load in 90 degrees of flexion.6 Baratz and Fu28
showed that after total meniscectomy, contact area may decrease by 75%
and contact stresses increase by 235%. They also documented the
deleterious effects of partial menisectomy, demonstrating that the
contact stresses increased in proportion to the amount of meniscus
removed. Excision of small bucket-handle tears of the medial meniscus
increased contact stress by 65%, and resecting 75% of the posterior
horn increased contact stresses equivalent to that after total
meniscectomy.28 Repair of meniscal
tears, by either arthroscopic or open techniques, reduced the contact
stresses to normal. Multiple other studies have corroborated the
mechanical importance of the meniscus.117,118
cartilage, allowing it to participate in shock absorption. Shock
absorption capacity in the normal knee is 20% higher than in the
menisectomized knee.189,300
The menisci also have a role in joint stability. In the ACL deficient
knee, the posterior horn of the medial meniscus plays a very important
passive stabilizing role. In the ACL deficient knee, medial menisectomy
leads to a 58% increase in anterior translation at 90 degrees of
flexion.189,267
Given the presence of neural elements with in their substance, it is
also theorized that the menisci may have a role in proprioception.
vascular region of the meniscus may heal nonoperatively or may become
asymptomatic.117,118,176
Nonoperative treatment usually consists of rehabilitation of the
injured knee with the avoidance of pivoting and sports for 12 weeks.
Arthroscopic management is standard, with either partial menisectomy
using motorized shavers and baskets or meniscal repairs using
outside-in, all-inside, or inside-out techniques.155,225,308
indicating the poor long-term results of menisectomy in children have
made this less common. Up to 60% to 75% of patients have degenerative
changes after menisectomy. Manzione et al.203 reported 60% poor results in 20 children and adolescents after menisectomy. In cadaver studies, Baratz et al.28
showed that the contact stresses on the tibiofemoral articulation
increase in proportion to the amount of the meniscus removed and the
degree of disruption of the meniscal structure. Clearly, as much of the
meniscus should be preserved as possible.
be determined arthroscopically to help formulate treatment plans. Zaman
and Leonard316 recommended
observation of small peripheral tears, repair of larger peripheral
tears, and, when necessary, partial menisectomy, leaving as much of the
meniscus as possible; they concluded that total menisectomy is
contraindicated in young patients. In general, peripheral tears, which
are most common in children, and longitudinal tears are good candidates
for repair, with success rates of up to 90% reported.70,127,134,224
suggested over six decades ago that, based on experimental evidence in
dogs, longitudinal meniscal tears could heal if communication with
peripheral blood supply existed, it was not until the work of Arnoczky
and Warren23 in the 1980s that
meniscal repairs were begun based on documentation of the meniscal
blood supply. They believed that tears within 3 mm of the
meniscosynovial junction were vascularized, and ones more than 5 mm
away were avascular unless bleeding was seen at surgery. Tears in the
3- to 5-mm range had inconsistent vascularity. Children and adolescents
may have greater healing potential for meniscal repair. In adults,
meniscal repair is indicated for tears involving the outer third. In
children and adolescents, repair of tears in the middle third zone
typically heal as well.70,127,134,224
lateral meniscus, particularly in younger children. The discoid lateral
meniscus represents an anatomic variant of meniscal morphology. The
incidence is thought to be 3% to 5% in the general population80,151,152,176 and slightly higher in Asian populations.99,151,152,176 Discoid morphology almost exclusively occurs within the lateral meniscus, but medial discoid menisci have also been reported.99,151,152,176 The incidence of bilateral abnormality has been reported to be as high as 20%.10,33,241,274
complete morphology (type I), incomplete morphology (type II), and any
morphology that lack peripheral attachments (type III). Although often
synonymous with so-called “snapping knee syndrome,” discoid lateral
menisci may manifest in a variety of ways. Symptoms are often related
to the type of discoid present, peripheral stability of the meniscus,
and the presence or absence of an associated meniscal tear.12,80,99,151,228,255,312 Stable discoid menisci without associated tears will often remain asymptomatic, identified only as incidental findings
during MRI or arthroscopy.163
Unstable discoid menisci more commonly present in younger children and
often produce the snapping knee syndrome. In such instances, a painless
and palpable, audible or visible snap is produced with knee range of
motion, especially near terminal extension. Discoid menisci with
posterior instability and a redundant anterior segment may limit knee
extension.314 In children with
stable discoid lateral menisci, symptoms often present when an
associated tear is present. Unlike acute meniscal tears, such symptoms
may present insidiously without previous trauma. Signs and symptoms of
a meniscal tear may exist including pain, swelling, catching, locking,
and limited motion. On physical examination, there may be joint line
tenderness, popping, limited motion, effusion, terminal motion pain,
and positive provocative tests (McMurray maneuvers, Apley test).
Degenerative horizontal cleavage tears are the most common type of tear
seen, reported in the largest series to occur in 58% to 98% of
symptomatic discoid menisci.6,33,241
discoid lateral meniscus is confirmed. For asymptomatic discoid lateral
menisci, even if found incidentally on arthroscopy, conservative
treatment is indicated. For stable, complete or incomplete discoid
menisci, partial menisectomy, “saucerization,” is the treatment of
choice (Fig. 24-24). If meniscal instability
with detachment also exists, meniscal repair can also be performed.
Traditionally, complete menisectomy via open or arthroscopic means was
suggested for such lesions. However, the long-term results of complete
menisectomy and near-total menisectomy in children are poor with early
degenerative changes.5,7,88,124,176,187,203,214,235,246,248,294,295,303,313
Although there may be a rare instance where salvage of a discoid
meniscus may seem unobtainable, better arthroscopic technology and
techniques have made meniscal preservation the ideal treatment through
saucerization and repair.4 Osteochondritis dissecans has been described associated with discoid lateral meniscus or after saucerization.41,75,129
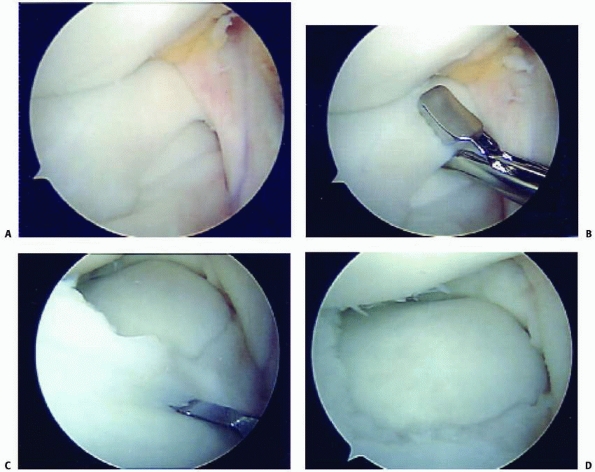 |
|
FIGURE 24-24 Discoid lateral meniscus saucerization. A. Complete type discoid lateral meniscus extending into the intercondylar notch. B. Excision of the central portion of the discoid meniscus. C. Excision of the anterior portion of the discoid meniscus. D. Appearance after saucerization.
|
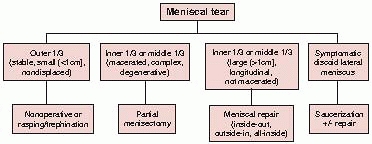 |
|
FIGURE 24-25 Algorithm for the management of meniscal tears in children and adolescents.
|
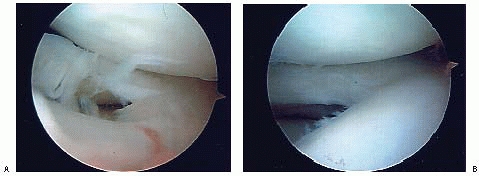 |
|
FIGURE 24-26 Complex inner third tear of the meniscus (A) treated with partial menisectomy (B).
|
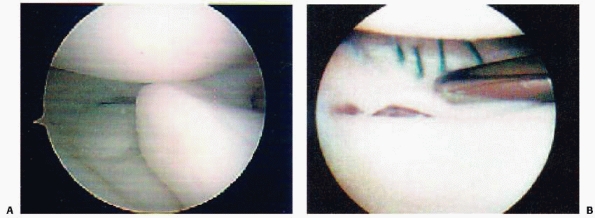 |
|
FIGURE 24-27 Longitudinal middle third tear of the meniscus (A) treated with inside-out meniscal repair (B).
|
documented outer third peripheral tear that is less than 1 cm long and
cannot be displaced more than 3 mm, the tear is allowed to heal. For a
similar tear in a chronic setting, we
arthroscopically
rasp or trephinate the interface between the meniscal edges and allow
the tear to heal. Protected weight bearing and limitation of flexion
beyond 90 degrees is prescribed for 4 weeks. Healing can be assessed
based on physical examination. Return to sports and activities are
based on the absence of physical examination findings and adequate
rehabilitation, usually at 2 to 3 months postoperatively.
third, which are longitudinal with a noncomminuted inner segment that
can be reduced anatomically, meniscal repair is performed. In the
chronic setting, rasping of the fragment edge, trephination, and use of
a fibrin clot may enhance healing. Patients are protected
postoperatively to allow for meniscal healing. Our postoperative
protocol for isolated meniscal repair involves touchdown weight bearing
for 6 weeks postoperatively. Range of motion is restricted to 0 to 30
degrees for the first 2 weeks followed by 0 to 90 degrees for the next
6 weeks. Progressive mobilization, strengthening, and sports-specific
therapy is performed under the direction of a physical therapy
protocol. Return to sports is allowed at 3 months postoperatively if
there is full range of motion, adequate strength, no symptoms (pain,
swelling, locking), and resolution of physical examination findings
(joint line tenderness, McMurray maneuvers, terminal range joint line
pain). Follow-up MRI is performed only in patients with persistent
symptoms or physical examination findings. Return to sports is
typically 3 to 4 months after meniscal repair.
inner third or middle third tears that are macerated, horizontal,
degenerative, or complex. Care should be taken to preserve as much
tissue as possible (Fig. 24-26). With
horizontal tears, the smaller of the two leaves is resected.
Rehabilitation after partial menisectomy includes weight bearing as
tolerated, range of motion, and strengthening. Return to sports and
activities is based on the absence of physical examination findings and
adequate rehabilitation, usually at 2 to 3 months postoperatively.
Patients who have undergone complete or near-total meniscectomy should
be followed longer-term to assess the development of degenerative
changes. In symptomatic patients or those developing degenerative
changes, replacement with an allograft meniscus or synthetic scaffold
may be considered.
meniscal repair over menisectomy whenever possible because of greater
healing potential in this age group, the long life span of these
patients, the poor results of total and near-total menisectomy, and the
lack of longer-term results of partial menisectomy. Meniscal repair
techniques include inside-out techniques, outside-in techniques, and
all-inside techniques. Outside-in techniques can be useful for anterior
horn medial or lateral meniscal tears. For body and posterior horn
tears, the traditional technique of meniscal repair has been inside-out
repair with vertical or horizontal sutures (Fig. 24-27).
Zone-specific cannulae are helpful to direct the flexible suture
needles to the appropriate position to avoid neurovascular structures.
In addition, we routinely make an incision posteromedially or
posterolaterally to retrieve the suture needles and tie the sutures
onto the joint capsule,
thus
protecting the saphenous nerve and vein medially and the peroneal nerve
laterally. Newer all-inside devices have eased the technique of
meniscal repair (Fig. 24-28). However, reports of articular cartilage damage from the heads of bioabsorbable arrows and darts exist.117,118
In addition, many of the available devices extend too far through the
capsule in the small pediatric knee, with potential for neurovascular
injury. The author prefers more recent all-inside suture devices with a
low profile in the joint. The author tends to use these for posterior
horn tears in adolescent knees. For smaller tears without substantial
displacement, the author uses these alone. For larger tears with
displacement such as displaced bucket-handle tears, the author uses
these in a hybrid manner with inside-out sutures.
treated urgently to allow for reduction and meniscal repair and to
avoid further injury to the meniscus. Meniscal tears in association
with ACL injuries are usually treated concurrently with ACL
reconstruction. ACL reconstruction is essential to provide a stable
environment for meniscal healing and prevention of further meniscal
tears. Healing rates are high with concurrent ACL reconstruction,
perhaps due to the healing environment of the associated postoperative
hemarthrosis. For meniscal repair in association with ACL
reconstruction, return to sports is dictated by the ACL reconstruction,
usually at 6 months postoperatively. For large, unstable meniscus tears
requiring a more involved meniscus repair, staging of the ACL
reconstruction approximately 3 months after meniscal repair can be
considered. This may result in a lower risk of arthrofibrosis,
rehabilitation focused on meniscal repair, and arthroscopic assessment
of meniscal healing at the time of ACL reconstruction.
-
Making the diagnosis of a meniscal tear
can be difficult in the child or adolescent. The differential diagnosis
is varied and includes other injuries and disorders that cause pain and
swelling or that cause joint line pain. Physical examination findings
are variable. MRI scans must be carefully scrutinized by the
orthopaedist because of the relatively high prevalence of normal signal
changes in the posterior horns. Extension of the meniscal signal to the
superior or inferior edge of the meniscus must be confirmed before
considering the MRI diagnostic of a meniscal tear. -
Total or near-total menisectomy should be
avoided in children and adolescents if at all possible to avoid the
development of degenerative changes. Patients who have had near total
or total menisectomy should be counseled regarding the risk of
arthritis and the potential for meniscus replacement with allograft or
synthetic scaffolds. -
Several technical pitfalls exist during
meniscal repair. During inside-out meniscal repair, a posterolateral
incision should be made for lateral meniscus repair to avoid iatrogenic
injury to the peroneal nerve and a posteromedial incision should be
made for medial meniscus repair to avoid iatrogenic injury to the
saphenous vein or nerve. During all-inside repair with meniscal repair
devices, consideration must be given to the size of the implant
relative to the pediatric knee. Implants that protrude too far may
injure neurovascular structures or cause local irritation or cysts.
Implants that are high-profile or protrude may damage the articular
surface of the femoral condyle. Sterile effusions and synovitis may
occur with bioabsorbable implants.
reported on meniscal repair in 29 patients under the age of 18 (25 had
closed physes and 17 underwent concomitant ACL reconstruction). They
reported 100% clinical healing at an average follow up of 5 years.221 Noyes and Barber-Westin229 looked at meniscal tears extending into the avascular zone in patients younger than 20 years old.91
Skeletal maturity had been reached in 88%. Their success rate in this
group was 75%. This study showed a higher rate of healing with
concomitant ACL reconstruction. Eggli et al.88
found an overall healing rate for repair of isolated meniscal tears of
88% in patients younger than 30, compared to 67% in patients over age
30. Johnson et al.150 showed a 76% healing rate at an average follow-up of greater than 10 years in a population
that averaged 20 years old at the time of surgery. Factors that have
been shown to correlate with increased healing of meniscal repairs
include younger age, decreased rim width (peripheral tears), repairs of
the lateral meniscus, concomitant ACL reconstruction, time from injury
to surgery of less than 8 weeks, and tear length of less than 2.5 cm.3,56,57,88,117,118,150,291
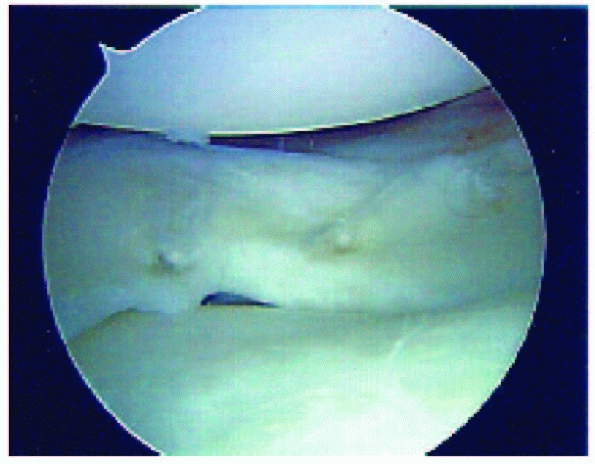 |
|
FIGURE 24-28 Longitudinal tear of the outer third of the posterior horn meniscus treated with all-inside fixation devices.
|
may include hemorrhage, infection, persistent effusion, stiffness, and
neuropathy. Both the popliteal artery and inferior geniculate branches
are close to the posterior capsule and are easily lacerated.
Postoperative infection should be suspected if swelling or pain
persists with an elevated temperature. Swelling is best treated with
external compression dressings, and stiffness is best prevented by
appropriate postoperative rehabilitation. Neuroma formation rarely
causes significant symptoms, but occasionally persistent localized
tenderness may warrant excision.
The increased frequency of diagnosis of knee ligament injuries in
children is likely related to increased participation in youth sports
at higher competitive levels, the advent of arthroscopy and MRI, and an
increased awareness of injuries in this age group.
knees with acute traumatic hemarthroses in series ranging from 35 to
138 patients.91,168,179,197,281,293 Stanitski et al.278
reported 70 children and adolescents with acute traumatic knee
hemarthroses; arthroscopic examination revealed ACL injuries in 47% of
those 7 to 12 years of age and in 65% of those 13 to 18 years of age.
They determined that boys 16 to 18 years of age engaged in organized
sports and girls 13 to 15 years of age engaged in unorganized sports
had the highest risk for complete ACL tears; 60% of these patients had
isolated ACL tears.
dependent on the loading conditions and the developmental anatomy.
Fractures of the epiphyses or physes about the knee are more common
than ligamentous injuries alone. Isolated knee ligament injury in
children younger than 14 years of age tends to be rare because of the
relative strength of the ligaments compared to the physes.83,153,208,302
The inherent ligamentous laxity in children also may offer some
protection against ligament injury, but this decreases as the
adolescent approaches skeletal maturity. Faster loading conditions
favor ligamentous injuries, whereas slower loading conditions favor
fracture. Narrowing of the intercondylar notch during skeletal
development may also predispose to ligamentous injury.175 Fractures and ligamentous injuries may occur concurrently. Bertin and Goble,39
after reviewing 29 fractures, concluded that physeal fractures about
the knee are associated with a higher incidence of ligamentous injury
than physeal fractures around other joints. In addition, tibial
eminence fractures, even after anatomic fixation and healing, tend to
demonstrate persistent ACL laxity.170
children were isolated case reports, and most recommendations were for
conservative treatment. More recent reports have indicated an increased
awareness of ligament injury in association with physeal fractures,65 as well as isolated ligament injuries, and a more aggressive approach, especially in adolescents approaching skeletal maturity.37,89,90,224,268,287
Management of some of these injuries, particularly ACL injuries in
skeletally immature patients, is controversial. Nonreconstructive
treatment of complete tears typically results in recurrent functional
instability with risk of injury to meniscal and articular cartilage. A
variety of reconstructive techniques have been utilized, including
physeal sparing, partial transphyseal, and transphyseal methods using
various grafts. Conventional adult ACL reconstruction techniques risk
potential iatrogenic growth disturbance due to physeal violation.
Growth disturbances after ACL reconstruction in skeletally immature
patients have been reported.
child’s age. In younger children, ligamentous injury typically is
associated with significant polytrauma. Clanton et al.61
reported that 5 of 9 children with acute knee ligament injuries were
struck by automobiles. In contrast, adolescents are more likely to
sustain ligamentous injury during contact sports or sports that require
“cutting” maneuvers while running.273
As exact a description as possible of the mechanism of injury should be
obtained, including the position of the knee at the time of injury, the
weight-supporting status of the injured knee, whether the force applied
was direct or indirect (generated by the patient’s own momentum), and
the position of the extremity after injury. Older adolescents may
describe the knee as buckling or “jumping out of place” and can usually
relate the location and severity of their pain as well as the time
between injury and onset of pain and swelling. Rapid intraarticular
effusion within 2 hours of injury suggests hemarthrosis, usually from
injury to the ACL.
four mechanisms capable of producing disruption of the ligamentous
structures about the knee: abduction, flexion, and internal rotation of
the femur on the tibia; adduction, flexion, and external rotation of
the femur on the tibia; hyperextension; and anterior-posterior
displacement. The most common mechanism in adolescents is abduction,
flexion, and internal rotation of the femur on the tibia occurring
during athletic competition when the weight-bearing extremity is struck
from the lateral side. The classic abduction, flexion, and internal
rotation injury in the adolescent may cause the “unhappy triad” of
O’Donoghue: tears of the MCL and ACL and injury to the medial meniscus.
direct blow to the medial aspect of the knee may tear the LCL, usually
with avulsion from the fibula or a physeal injury through the distal
femur.145 Isolated injuries of the ACL and PCL have been reported.140,208,260
Disruption of the ACL with minimal injury to other supporting
structures may be caused by hyperextension, marked internal rotation of
the tibia on the femur, and pure deceleration. In contrast, isolated
injury of the PCL most often is caused by a direct blow to the front of
the tibia with the knee in flexion.
Large areas of ecchymosis and extensive effusion are easily identified,
but smaller areas may require careful palpation. In general, acute
hemarthrosis suggests rupture of a cruciate ligament, an osteochondral
fracture, a peripheral tear in the vascular portion of a meniscus, or a
tear in the deep portion of the joint capsule.69,72
The absence of hemarthrosis is not, however, an indication of a less
severe ligament injury, because with complete disruption the blood in
the knee joint may escape into the soft tissues rather than distend the
joint. The range of motion of the injured knee, especially extension,
is compared with that of the uninjured knee. If significant effusion
prevents full extension, sterile aspiration can be performed. If
complete knee extension is impossible after aspiration, the diagnosis
of an entrapped meniscus should be considered.
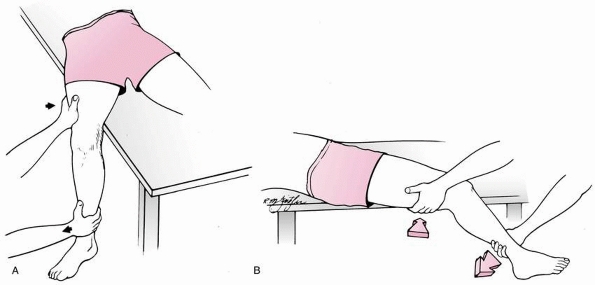 |
|
FIGURE 24-29 Valgus stress test of MCL. Extremity is abducted off table, knee is flexed to 20 degrees, and valgus stress is applied. A. Frontal view. B. Lateral view.
|
origins and insertions should locate tenderness at the site of the
ligament injury. A defect in the collateral ligaments often can be felt
if the MCL is avulsed from its insertion on the tibia or if the LCL is
avulsed from the fibular head. If the neurovascular status is normal,
stability should be evaluated by stress testing.
with or without concomitant fracture, is very subjective, and its
usefulness depends on the knowledge and experience of the examiner.
Stress testing may be done immediately after injury in cooperative
adolescents who do not have other significant injuries, but sedation or
general anesthesia may be required for accurate diagnosis. In
nonemergent situations, beginning the examination by testing the
uninjured knee often calms patients and makes them more cooperative; it
also establishes a baseline for assessing the ligamentous stability of
the injured knee as knee laxity varies during childhood.135
In the standard stress tests of specific collateral and cruciate
ligaments of the knee described in the following sections, the
uninjured knee should be examined first.
The valgus or abduction stress test is done with the child supine on
the examining table and the knee to be examined on the side of the
table closest to the examiner. The extremity is abducted off the side
of the table and the knee is flexed approximately 20 degrees (Fig. 24-29).
With one hand about the lateral aspect of the knee and the other
supporting the ankle, the examiner applies gentle abduction or valgus
stress to the knee while the hand at the ankle gently externally
rotates the leg. Stability of the knee is noted at 20 degrees of
flexion and again at neutral.
Ligament. The varus or adduction stress test is done in a manner
similar to the valgus stress test. It should be done with the
knee
in full extension and in 20 degrees of flexion. The LCL may be palpable
as a taut structure on the lateral aspect of the knee.
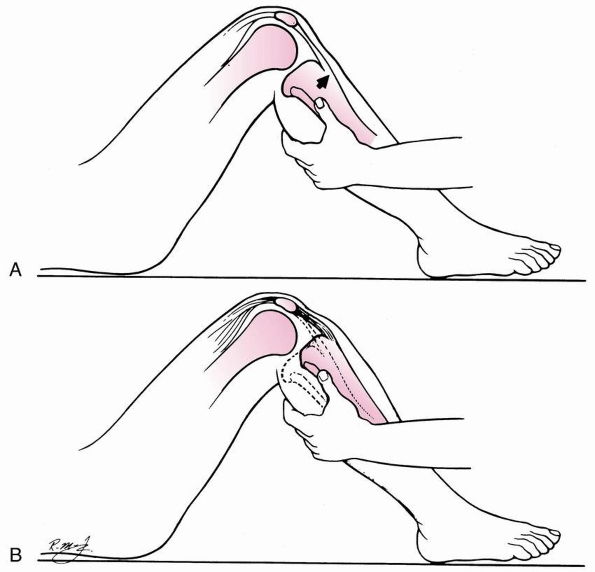 |
|
FIGURE 24-30
Anterior drawer test of ACL. Foot is positioned in internal, external, and neutral rotation during examination. With anterior cruciate insufficiency, an anterior force (A) displaces the tibia forward (B). |
different when tested in extension and in flexion. If a collateral
ligament is torn but the cruciate ligaments and posterior capsule are
intact, little instability can be detected with the knee extended.
Flexion of the knee relaxes the capsule and more instability is evident
with the same degree of ligamentous injury. Significant instability
with varus or valgus stress testing with the knee in full extension
usually indicates a cruciate as well as a collateral ligament
disruption.
anterior drawer test, as described by Slocum, is the classic maneuver
for testing the stability of the ACL (Fig. 24-30).
The Lachman and pivot-shift tests, however, are considered more
sensitive for evaluating ACL injury when the examination can be done in
a relaxed, cooperative adolescent (Fig. 24-31).
To perform the Lachman test, the examiner firmly stabilizes the femur
with one hand while using the other hand to grip the proximal tibia,
with the thumb placed on the anteromedial joint margin. An anteriorly
directed lifting force applied by the palm and fingers causes anterior
translation of the tibia in relation to the femur that can be palpated
by the thumb; a soft or mushy end point indicates a positive test. When
the ACL is disrupted, the normal patellar ligament slope is obliterated.
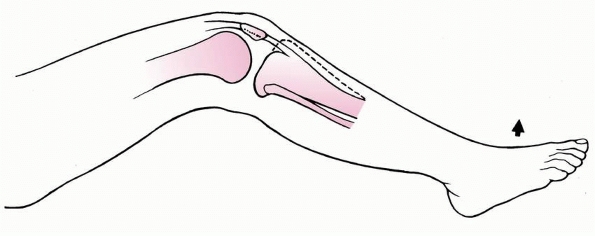 |
|
FIGURE 24-31 Lateral pivot-shift test of ACL.
|
posterior drawer test for evaluation of the PCL is done with the
patient supine. With the patient’s foot secured to the table and the
hip flexed, a posterior force is applied to the proximal tibia.
Posterior movement of the tibia on the femur greater than in the
uninjured extremity indicates posterior instability (Fig. 24-32).
when any ligament injury of the knee is suspected in children. The
radiographs are carefully inspected for evidence of occult epiphyseal
or physeal fractures or bony avulsions. The intercondylar notch,
especially, is inspected to detect a tibial spine fracture, which is
confirmed by anterior or posterior instability on physical examination.
Occasionally, a small fragment of bone avulsed from the medial femur or
proximal tibia indicates injury to the MCL. Similarly, avulsion of a
small fragment of bone from the proximal fibular epiphysis or the
lateral aspect of the distal femur may indicate LCL injury.
helpful to evaluate medial and lateral instability associated with
physeal fractures. Gentle stress views may be obtained with sedation,
but general anesthesia may be required if the diagnosis is unclear.
Stress must be performed carefully to avoid further physeal injury,
which may lead to physeal arrest. There are no accepted guidelines
correlating joint space widening medially or laterally with knee joint
instability in children, and stress views of the opposite knee may be
required for comparison. If plain radiographs show a fracture of the
distal femoral or proximal tibial physis, stress views may be obtained
only to evaluate suspected ligamentous instability. Conversely, if the
initial radiographs appear normal but there is significant effusion
about the knee, stress views or MRI may be obtained to rule out a
fracture of the physis of the distal femur or proximal tibia.
anterior or posterior tibial spine indicative of injury to the ACL or
PCL, widening of the joint space, and posterior subluxation of the
tibia on the femur. Clanton et al.61 considered a joint space of 8 mm or wider to be a definitive indication of ligament injury. Sanders et al.260
reported 1.8 cm of posterior subluxation of the tibia on the
anteroposterior stress view in a 6-year-old child with complete PCL
disruption.
injuries in the knee. MRI should be used to confirm an uncertain
diagnosis or to gain further information that may affect treatment.
Conventional MRI can give information regarding MCL injury, LCL injury,
ACL injury, PCL injury, posterolateral corner injury, bone bruising,
chondral injury, and meniscal injury.
severity of the injury, the specific anatomic location of the injury,
and the direction of the subsequent instability caused by an isolated
ligament injury or combination of ligament injuries.
number of fibers of the ligament with localized tenderness but no
instability.
A
second-degree sprain is disruption of more ligamentous fibers, causing
loss of function and more joint reaction but no significant
instability. A third-degree sprain is complete disruption of the
ligament, resulting in instability. Although difficult to assess
clinically, the degree of sprain also is determined during stress
testing by the amount of separation of the joint surfaces: first-degree
sprain, 5 mm or less; second-degree sprain, 5 to 10 mm; and
third-degree sprain, more than 10 mm.
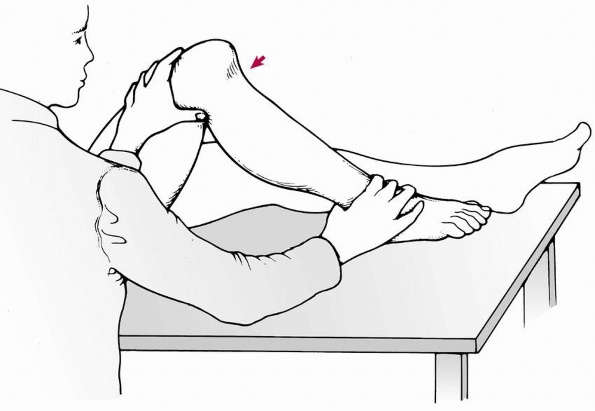 |
|
FIGURE 24-32 PCL injury. Note posterior sagging of the tibia with posterior cruciate injury.
|
-
MCL insufficiency (Fig. 24-33)
-
Femoral origin
-
Middle portion
-
Tibial insertion
-
-
ACL insufficiency
-
Femoral origin
-
Interstitial
-
Tibial insertion
-
Without avulsion of the intercondylar eminence
-
With avulsion of the intercondylar eminence
-
-
-
LCL insufficiency (Fig. 24-34)
-
Femoral origin
-
Middle portion
-
Fibular insertion
-
-
PCL insufficiency
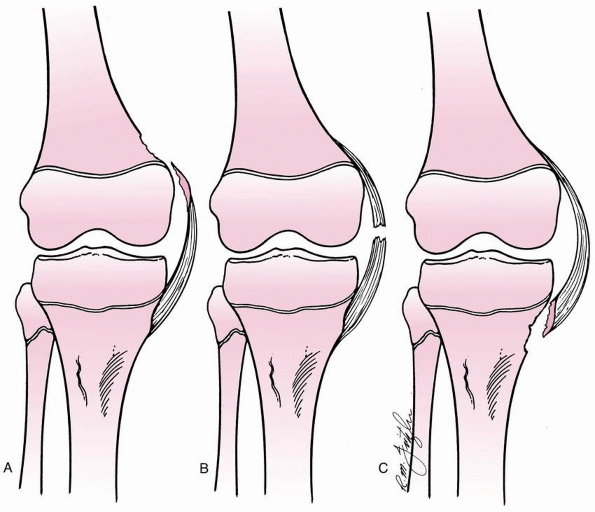 |
|
FIGURE 24-33 MCL injury. A. Femoral origin. B. Middle portion. C. Tibial insertion.
|
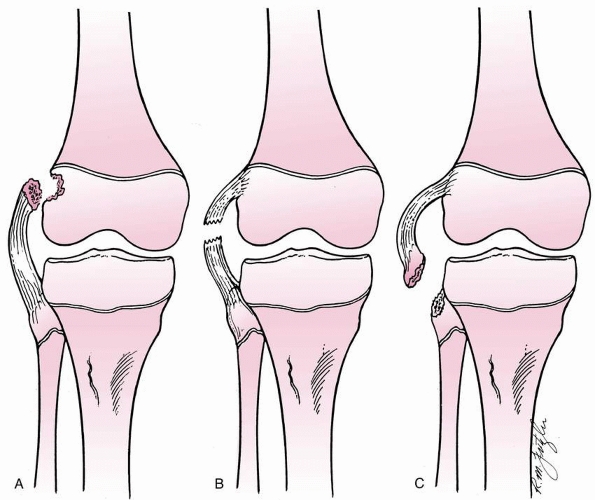 |
|
FIGURE 24-34 LCL injury. A. Femoral origin. B. Middle portion. C. Fibular insertion.
|
-
One-plane instability (simple or straight)
-
One-plane medial
-
One-plane lateral
-
One-plane posterior
-
One-plane anterior
-
-
Rotary instability
-
Anteromedial
-
Anterolateral
-
In flexion
-
Approaching extension
-
-
Posterolateral
-
Posteromedial
-
-
Combined instability
-
Anterolateral-posterolateral
-
Anterolateral-anteromedial
-
Anteromedial-posteromedial
-
for example, means that the tibia moves abnormally away from the femur
on the medial side. In anteromedial rotary instability, the tibia
rotates anteriorly and externally and moves away from the femur on the
medial side. The classification becomes more complex as more
significant ligamentous injuries involving more anatomic locations are
included, but determining the type of instability resulting from the
injury is helpful in planning treatment.
femoral epiphysis and insert into the proximal tibial and fibular
epiphyses, except for the superficial portion of the MCL, which inserts
into the proximal tibial metaphysis distal to the physis (Fig. 24-35).
In children, these ligaments are stronger than the physes, and
significant tensile stresses usually produce epiphyseal or physeal
fractures rather than ligamentous injury. The ACL originates from the
posterolateral intercondylar notch and
inserts
into the tibia slightly anterior to the intercondylar eminence. The PCL
originates from the posteromedial aspect of the intercondylar notch and
attaches on the posterior aspect of the proximal tibial epiphysis. The
ACL in children has collagen fibers continuous with the perichondrium
of the tibial epiphyseal cartilage; in adults, the ligament inserts
directly into the proximal tibia by way of Sharpey’s fibers. This
anatomic difference probably accounts for the fact that fracture of the
anterior tibial spine occurs more frequently in children than does ACL
injury.
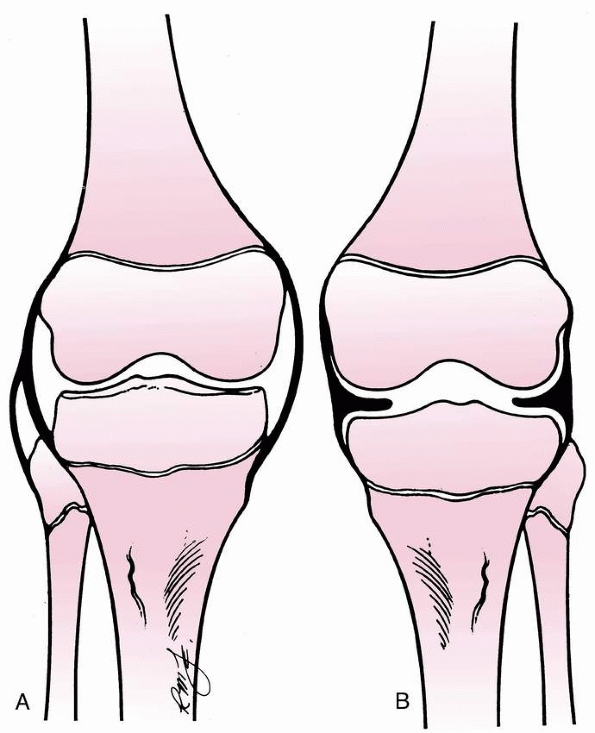 |
|
FIGURE 24-35 Anatomy of medial and collateral ligaments of the knee in the adolescent. A. Superficial origins and insertions. B. Capsular and meniscal attachments.
|
injuries in patients with open physes. Nonoperative management of
partial tears may be successful in some patients.179
However, nonoperative management of complete tears in skeletally
immature patients generally has a poor prognosis with recurrent
instability leading to further meniscal and chondral injury, which has
implications in terms of development of degenerative joint disease.11,115,147,209,220,222,244 Graf et al.,115 Mizuta et al.,222 and Janarv et al.147
have reported instability symptoms, subsequent meniscal tears,
decreased activity level, and need for ACL reconstruction in the
majority of skeletally immature patients treated nonoperatively in
series of 8, 18, and 23 patients, respectively. Similarly, when
comparing the results of operative versus nonoperative management of
complete ACL injuries in adolescents, McCarroll et al.209 and Pressman et al.244
found that those managed by ACL reconstruction had less instability,
higher activity and return to sport levels, and lower rates of
subsequent reinjury and meniscal tears.
potential iatrogenic growth disturbance due to physeal violation. Cases
of growth disturbance have been reported in animal models86,121,136 and clinical series.180,182,192
Animal models have demonstrated mixed results regarding growth
disturbances from soft tissue grafts across the physes. In a canine
model with iliotibial band grafts through 5/32 inch tunnels,
Stadelmeier et al.277 found no
evidence of growth arrest in the four animals with soft tissue graft
across the physis, whereas the four animals with drill holes and no
graft demonstrated physeal arrest. In a sheep model of transphyseal
reconstruction, Seil et al.262 did
not find clinically relevant growth disturbances despite consistent
physeal damage. In a rabbit model using a semitendinosis graft through
2-mm tunnels, Guzzanti et al.121 did
have cases of growth disturbance; however, these were not common: 5%
shortening (1/21) and 10% distal femoral valgus deformity (2/21).
Examining the effect of a tensioned soft tissue graft across the
physis, Edwards et al.86 found a
substantial rate of deformity. In a canine model with iliotibial band
graft tensioned to 80 N, these investigators found significant
increases, compared to the nonoperated control limb, in distal femoral
valgus deformity and proximal tibial varus deformity despite no
evidence of a bony bar.86 Similarly, Houle et al.136 reported growth disturbance after a tensioned tendon graft in a bone tunnel across the rabbit physis.
reported one case of 20 mm shortening in a series of 24 skeletally
immature patients reconstructed with transphyseal semitendinosis and
gracilis grafts. This was associated with staple graft fixation across
the physis. Koman and Sanders182
reported a case of distal femoral valgus deformity requiring osteotomy
and contralateral epiphyseodesis after transphyseal reconstruction with
a doubled semitendinosis graft. This case was also associated with
fixation across the distal femoral physis. Kocher et al.180
reported an additional 15 cases of growth disturbances gleaned from a
questionnaire of expert experience, including 8 cases of distal femoral
valgus deformity with an arrest of the lateral distal femoral physis, 3
cases of tibial recurvatum with an arrest of the tibial tubercle
apophysis, 2 cases of genu valgum without arrest due to a lateral
extra-articular tether, and 2 cases of leg-length discrepancy (one
shortening and one overgrowth). Associated factors included fixation
hardware across the lateral distal femoral physis in three cases, bone
plugs of a patellar tendon graft across the distal femoral physis in
three cases, large (12-mm) tunnels in two cases, lateral
extra-articular tenodesis in two cases, fixation hardware across the
tibial tubercle apophysis in two cases, over-the-top femoral position
in one case, and suturing near the tibial tubercle apophysis in one
case.180
skeletally immature patients include primary repair, extra-articular
tenodesis, transphyseal reconstruction, partial transphyseal
reconstruction, and physeal sparing reconstruction. Primary ligament
repair61,92 and extra-articular tenodesis alone115,209
have had poor results in children and adolescents, similar to adults.
Transphyseal reconstructions with tunnels that violate both the distal
femoral and proximal tibial physes have been performed with hamstrings
autograft, patellar tendon autograft, and allograft tissue.11,181,191,209
Partial transphyseal reconstructions violate only one physis with a
tunnel through the proximal tibial physis and over-the-top positioning
on the femur or a tunnel through the distal femoral physis with an
epiphyseal tunnel in the tibia.17,44,123
A variety of physeal-sparing reconstructions have been described to
avoid tunnels across either the distal femoral or proximal tibial
physis.14,52,77,122,138,162,171,172,218,293
have been described that utilize hamstrings tendons under the
intermeniscal ligament and over-the-top on the femur, through
allepiphyseal femoral and tibial tunnels, and with a femoral epiphyseal
staple.14,52,77,122,162,218,238,293
In adolescent patients with growth remaining, transphyseal
reconstructions have been performed with hamstrings autograft, patellar
tendon autograft, quadriceps tendon autograft, and allograft tissue.11,20,24,85,104,109,110,205,209,210,266,270,278,301
In addition, partial transphyseal reconstructions have been described
with a tunnel through the proximal tibial physis and over-the-top
positioning on the femur or a tunnel through the distal femoral physis
with an epiphyseal tunnel in the tibia.17,44,123,193
with crutches or a hinged knee brace for 1 to 3 weeks, depending on
resolution of symptoms. Return to athletic activities is allowed when a
full, painless range of motion is achieved and the patient can run and
cut without pain. Isolated complete (grade III) disruption of the MCL
can be treated with 6 weeks of immobilization in a hinged knee brace
followed by rehabilitation
of
the quadriceps muscles and knee motion provided this is an isolated
injury. The physician must ensure that there is no associated injury to
the ACL before using nonoperative treatment for a grade III MCL injury.
Grade III disruptions of the MCL in adolescents associated with injury
of the ACL are usually treated with ACL reconstruction without formal
MCL repair. The MCL is protected with a hinged knee brace and allowed
to heal.
despite the image projected by celebrity athletes and their urgent
care. A frank discussion must be held with the parents and the patient
concerning future vocation, sport demands, treatment options, outcomes,
and risks involved with return to current sport activity. The
orthopaedic surgeon must assume the role of a “knee counselor,”
particularly with patients with a history of chronic knee abuse. All
treatment algorithms are based on an accurate and complete diagnosis,
which is achieved by clinical, imaging, and, if necessary, arthroscopic
means. The treatment goal is a functional knee without progressive
intra-articular damage or predisposition to premature osteoarthrosis.
have a tremendous amount of growth remaining, while others are
essentially done growing. The consequences of growth disturbance in the
former group would be severe, requiring osteotomy and/or limb
lengthening. However, the consequences of growth disturbance in the
latter group would be minimal. When treating a skeletally immature
athlete with an ACL injury, it is important to know their chronologic
age, their skeletal age, and their physiologic age. Skeletal age can be
determined from an anteroposterior radiograph of the left hand and
wrist per the atlas of Greulich and Pyle.119 Alternatively, skeletal age can be estimated from knee radiographs per the atlas of Pyle and Hoerr.245 Physiologic age is established using the Tanner staging system (Table 24-2).289
In the office, the patient can be informally staged by questioning. In
the operating room, after the induction of anesthesia, Tanner staging
can be confirmed. The vast majority of ACL injuries in skeletally
immature patients occur in adolescents. The management of these
injuries in preadolescent children is particularly vexing, given the
poor prognosis with nonoperative management, the substantial growth
remaining, and the consequences of potential growth disturbance.
|
TABLE 24-2 Tanner Staging Classification of Secondary Sexual Characteristics
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
The goal of this program is defined from the outset: it is a
temporizing measure until the patient becomes mature enough for an
adult-type ACL reconstruction, or it is the definitive choice for a
patient willing to accept the functional limitations. The author uses a
three-phase approach. Phase one begins shortly after injury and lasts 7
to 10 days. Brief immobilization (3 to 5 days) with a knee immobilizer
for comfort is followed by daily out-of-brace exercises with active
knee flexion and passive knee extension. Ambulation is with
crutch-protected partial weight bearing. During this time, the author
reinforces patient education on the consequences of imprudent return to
high-level sports. Phase two focuses on rehabilitation of the lower
extremity and lasts
approximately
6 weeks. Emphasis is placed on restoration of full knee motion,
flexibility, strength, and endurance with particular attention to
regaining the normal quadriceps/hamstring strength ratio. As the ratio
is normalized, crutch use is decreased and then eliminated. The role of
functional bracing has not been defined in children and issues of fit,
size, and cost need to be considered. Phase three continues the
rehabilitation, incorporates the use of a functional brace for sports,
and allows return to low- and moderate-demand sports when quadriceps
and hamstring strength and endurance are equal to those of the
opposite, noninjured side as determined by isokinetic testing at
functional speeds (>260 degrees/second). In the final part of this
phase, sports readiness tasks are done at less than full speed. Monthly
followup evaluates program compliance and rules out any further knee
changes in function. Compliance with a nonoperative program designed to
be a temporizing measure often is quite difficult for an emerging
athlete who is surrounded by peer, coaching, and, often, parental
pressures to return to highdemand sports.
In prepubescent patients, the author performs a physeal-sparing,
combined intra-articular and extra-articular reconstruction utilizing
autogenous iliotibial band.171,172
In adolescent patients with significant growth remaining, the author
performs transphyseal ACL reconstruction with autogenous hamstrings
tendons with fixation away from the physes.181
In older adolescent patients approaching skeletal maturity, the author
performs conventional adult ACL reconstruction with interference screw
fixation using either autogenous central third patellar tendon or
autogenous hamstrings.
acute ACL reconstruction is not performed within the first 3 weeks
after injury to minimize the risk of arthrofibrosis. Prereconstructive
rehabilitation is performed to regain range of motion, decrease
swelling, and resolve the reflex inhibition of the quadriceps. ACL
reconstruction may be staged in some cases if there is a displaced,
bucket-handle tear of the meniscus that requires extensive repair in
order to protect the meniscal repair from the early mobilization
prescribed by ACL reconstruction. Skeletally immature patients must be
emotionally mature enough to actively participate in the extensive
rehabilitation required after ACL reconstruction.
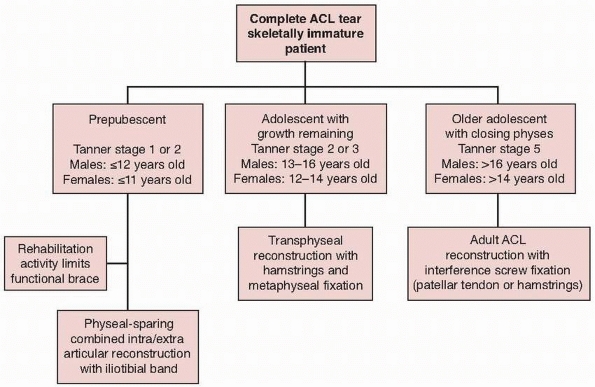 |
|
FIGURE 24-36 Algorithm for ACL reconstruction in skeletally immature patients.
|
without concurrent chondral or repairable meniscal injury, the author
first attempts nonreconstructive treatment with a program of
rehabilitation, functional bracing, and return to nonhigh-risk
activities. Although the results of nonreconstructive treatment are
generally poor with subsequent functional instability and risk of
injury to meniscal and articular cartilage, surgical reconstruction
poses the risk of growth disturbance. Furthermore, some patients are
able to cope with their ACL insufficiency or modify their activities,
allowing for further growth and aging such that an adolescent-type
reconstruction can be performed with transphyseal hamstrings tendons in
a more anatomic manner.
or repairable meniscal injury or those with functional instability
after nonreconstructive treatment, the author performs a
physeal-sparing, combined intra-articular and extraarticular
reconstruction utilizing autogenous iliotibial band (Fig. 24-37).171,172
This procedure is a modification of the combined intra-articular and
extra-articular reconstruction described by MacIntosh and Darby.198
The author’s rationale for utilization of this technique is to provide
knee stability and improve function in prepubescent skeletally immature
patients with complete intrasubstance ACL injuries while
avoiding
the risk of iatrogenic growth disturbance by violating the distal
femoral and/or proximal tibial physes. In the author’s opinion, the
consequences of potential iatrogenic growth disturbance caused by
transphyseal reconstruction in these young patients is prohibitive.
Recognizing that this reconstruction is nonanatomic, the author
counsels patients and families that they may require revision
reconstruction if they develop recurrent instability, but that this
procedure may temporize for further growth such that they may then
undergo a more conventional reconstruction with drill holes.
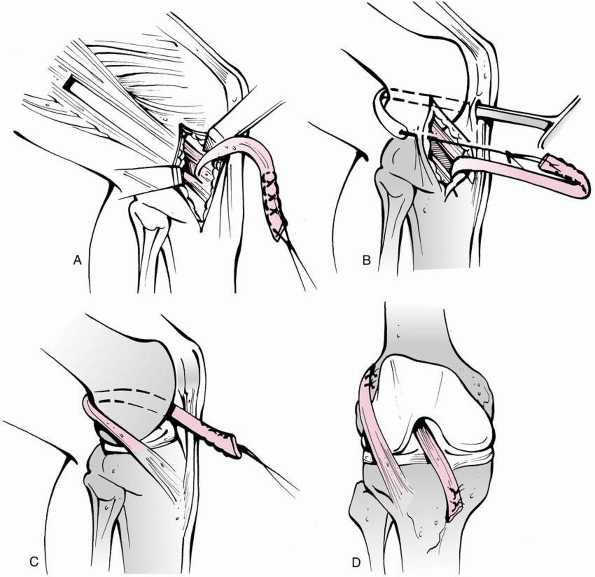 |
|
FIGURE 24-37
Physeal-sparing, combined intra-articular and extra-articular reconstruction utilizing autogenous iliotibial band for prepubescents. A. The iliotibial band graft is harvested free proximally and left attached to the Gerdy tubercle distally. B. The graft is brought through the knee in the over-the-top position posteriorly. C. The graft is brought through the knee and under the intermeniscal ligament anteriorly. D. Resulting intra-articular and extra-articular reconstruction. |
an overnight observation procedure. Local anesthesia with sedation may
not be reliable in prepubescent children with the potential for a
paradoxical effect of sedation. The child is positioned supine on the
operating table with a pneumatic tourniquet about the upper thigh which
is used routinely. Examination under anesthesia is performed to confirm
ACL insufficiency.
incision of approximately 6 cm is made obliquely from the lateral joint
line to the superior border of the iliotibial band (Fig. 24-38A).
Proximally, the iliotibial band is separated from subcutaneous tissue
using an periosteal elevator under the skin of the lateral thigh. The
anterior and posterior borders of the iliotibial band are incised and
the incisions carried proximally under the skin using curved
meniscotomes (see Fig. 24-38A). The iliotibial
band is detached proximally under the skin using a curved meniscotome
or an open tendon stripper. Alternatively, a counterincision can be
made at the upper thigh to release the tendon. The iliotibial band is
left attached distally at the Gerdy tubercle. Dissection is performed
distally to separate the iliotibial band from the joint capsule and
from the lateral patellar retinaculum (Fig. 24-38B). The free proximal end of the iliotibial band is then tubularized with a no. 5 ethibond whip stitch.
standard anterolateral viewing and anteromedial working portals.
Management of meniscal injury or chondral injury is performed if
present. The ACL remnant is excised. The over-the-top position on the
femur and the over-the-front position under the intermeniscal ligament
are identified. Minimal notchplasty is performed to avoid iatrogenic
injury to the perichondrial ring of the distal femoral physis which is
in very close proximity to the over-the-top position.32 The free end of the iliotibial band graft is brought through the over-the-top position using a full-length clamp (Fig. 24-38C) or a two-incision rear-entry guide (see Fig. 24-37) and out the anteromedial portal (Fig. 24-38D).
the proximal medial tibia in the region of the pes anserinus insertion.
Dissection is carried through the subcutaneous tissue to the
periosteum. A curved clamp is placed from this incision into the joint
under the intermeniscal ligament (Fig. 24-38E).
A small groove is made in the anteromedial proximal tibial epiphysis
under the intermeniscal ligament using a curved rat-tail rasp to bring
the tibial graft placement more posterior. The free end of the graft is
then brought through the joint (Fig. 24-38F), under the intermeniscal ligament in
the anteromedial epiphyseal groove, and out the medial tibial incision (Fig. 24-38G).
The graft is fixed on the femoral side through the lateral incision
with the knee at 90 degrees flexion and 15 degrees external rotation
using mattress sutures to the lateral femoral condyle at the insertion
of the lateral intermuscular septum to effect an extra-articular
reconstruction (Fig. 24-38H). The tibial side
is then fixed through the medial incision with the knee flexed 20
degrees and tension applied to the graft. A periosteal incision is made
distal to the proximal tibial physis as checked with fluoroscopic
imaging. A trough is made in the proximal tibial medial metaphyseal
cortex and the graft is sutured to the periosteum at the rough margins
with mattress sutures (see Fig. 24-37).
 |
|
FIGURE 24-38 Technique of physeal sparing combined intra-articular and extra-articular ACL reconstruction using iliotibial band. A. The iliotibial band is harvested through an oblique lateral knee incision. B.
The iliotibial band graft is detached proximally, left attached distally, and dissected free from the lateral patellar retinaculum. C. The iliotibial band graft is brought through the knee using a full-length clamp placed from the anteromedial portal through the over-the-top position into the lateral incision. D. The graft is then brought through the over-the-top position. E. A clamp is placed from a proximal medial leg incision under the intermeniscal ligament. A groove is made in the anteromedial tibial epiphysis using a rasp. F. The graft is brought through the knee in the over-the-top position and under the intermeniscal ligament. |
 |
|
FIGURE 24-38 (continued) G. The graft is brought out the proximal medial leg incision. H.
It is sutured to the intermuscular septum and periosteum of the lateral femoral condyle through the lateral knee incision, and it is sutured in a trough to the periosteum of the proximal medial tibial metaphysis. |
weight bearing for 6 weeks. Range of motion is limited from 0 to 90
degrees for the first 2 weeks, followed by progressive full range of
motion. A continuous passive motion from 0 to 90 degrees and
cryotherapy are used for 2 weeks postoperatively. A protective
postoperative brace is used for 6 weeks.
complete ACL tear, the author does not advocate initial
nonreconstructive treatment since the risk of functional instability
with injury to the meniscal and articular cartilage is high, the risk
and consequences of growth disturbance from ACL reconstruction are
less, and the author’s transphyseal technique is an anatomic
reconstruction. In these patients, the author performs transphyseal ACL
reconstruction with autogenous hamstrings tendons with fixation away
from the physes.181
an overnight observation procedure. Local anesthesia with sedation may
be performed in the emotionally mature adolescent child. The patient is
positioned supine on the operating table with a pneumatic tourniquet
about the upper thigh which is not used routinely. Examination under
anesthesia is performed to confirm ACL insufficiency.
diagnosis is in doubt, arthroscopy can be performed first to confirm
ACL tear. A 4-cm incision is made over the palpable pes anserinus
tendons on the medial side of the upper tibia (Fig. 24-39A).
Dissection is carried through skin to the sartorius fascia. Care is
taken to protect superficial sensory nerves. The sartorius tendon is
incised longitudinally and the gracilis and semitendinosis tendons are
identified. The tendons are dissected free distally and their free ends
whip-stitched with no. 2 or no. 5 ethibond suture. They are dissected
proximally using sharp and blunt dissection. Fibrous bands to the
medial head of gastrocnemius should be sought and released. A closed
tendon stripper is used to dissect the tendons free proximally.
Alternatively, the tendons can be left attached distally, and an open
tendon stripper used to release the tendons proximally. The tendons are
taken to the back table, where excess muscle is removed and the
remaining ends are whip-stitched with no. 2 or no. 5 ethibond sutures.
The tendons are folded over a closed loop endobutton. The graft
diameter is sized and the graft is placed under tension.
standard anterolateral viewing and anteromedial working portals.
Management of meniscal injury or chondral injury is performed if
present. The ACL remnant is excised. The over-the-top position on the
femur is identified. Minimal notchplasty is performed to avoid
iatrogenic injury to the perichondrial ring of the distal femoral
physis, which is in very close proximity to the over-the-top position.32
A guidewire is drilled through the hamstrings harvest incision into the
posterior aspect of the ACL tibial footprint. The guidewire entry point
on the tibia should be kept medial to avoid injury to the tibial
tubercle apophysis. The guidewire is reamed with the appropriate
diameter reamer. Excess soft tissue at the tibial tunnel is excised to
avoid arthrofibrosis. The transtibial over-the-top guide of the
appropriate offset to ensure a 1-mm or 2-mm back wall is used to pass
the femoral guide pin (Fig. 24-39C). The
femoral guide pin is overdrilled with the endobutton reamer. Both are
removed in order to use the depth gauge to measure the femoral tunnel
length. The guide pin is replaced and brought through the distal
lateral thigh. The
femur is reamed to the appropriate depth (femoral tunnel length – endobutton length + 8 mm to flip the endobutton).
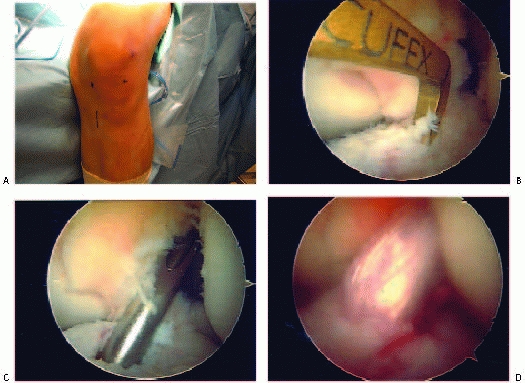 |
|
FIGURE 24-39 Transphyseal reconstruction with autogenous hamstrings for adolescents with growth remaining. A.The gracilis and semitendinosis tendons are harvested through an incision over the proximal medial tibia. B. The tibial guide is used to drill the tibial tunnel. C. The transtibial over-the-top offset guide is used to drill the femoral tunnel. D. Hamstrings graft after fixation.
|
in slot of the guidewire and pulled through the tibial tunnel, through
the femoral tunnel, and out the lateral thigh. These are then pulled to
bring the endobutton and graft through the tibial tunnel and into the
femoral tunnel. One set of sutures is used to “lead” the endobutton,
while the other set of sutures is used to “follow.” Once the graft is
fully seated in the femoral tunnel, the “follow” sutures are pulled to
flip the endobutton (Fig. 24-39D). The flip can
be palpated in the thigh and tension is applied to the graft to endure
no graft slippage. The knee is then extended to ensure no graft
impingement. The knee is then cycled approximately 10 times with
tension applied to the graft. The graft is fixed on the tibial side
with the knee in 20 to 30 degrees of flexion, tension applied to the
graft, and a posterior force placed on the tibia. On the tibial side,
the graft is either fixed with a soft tissue interference screw if
there is adequate tunnel distance (at least 30-mm) below the physis to
ensure metaphyseal placement of the screw or with a post and spiked
washer. Fluoroscopy can be used to ensure that the fixation is away
from the physes. Postoperative radiographs are shown in Figure 24-40.
weightbearing for 2 weeks. Range of motion is limited from 0 to 90
degrees for the first 2 weeks, followed by progressive full range of
motion. A continuous passive motion from 0 to 90 degrees and
cryotherapy are used for 2 weeks postoperatively. A protective
postoperative brace is used for 6 weeks.
Occasionally, the lateral capsular sign is seen on radiographs obtained
for evaluation of knee injury. Most often, the LCL is avulsed from the
proximal fibular epiphysis; proximal and midsubstance tears are
uncommon. This injury is treated in the same manner as injury to the
MCL. For isolated grade III injuries, a 6-week period of immobilization
in a hinged knee brace is recommended. If ACL injury is associated with
LCL injury, treatment is as described for combined injuries of the MCL
and ACL. In young children, the LCL is repaired and the ACL is left
untreated. If instability persists as the adolescent nears skeletal
maturity, intra-articular reconstruction can be done at that time. In
adolescents near skeletal maturity at the time of injury, the author
prefers to repair both the ACL and LCL.
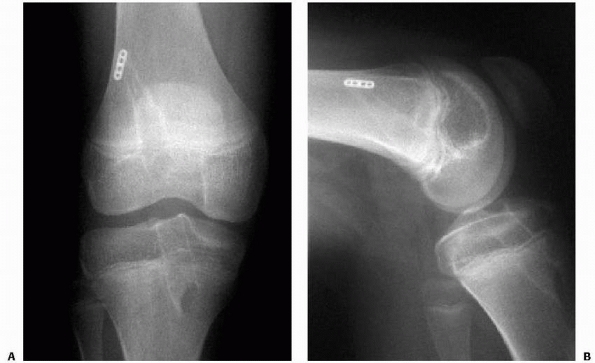 |
|
FIGURE 24-40 Transphyseal reconstruction with autogenous hamstrings for adolescents with growth remaining. Postoperative anteroposterior (A) and lateral (B) radiographs.
|
If nondisplaced, they should be treated with immobilization; if
displaced, they should be treated with open reduction and internal
fixation.
adolescents can be treated with 6 weeks of immobilization in a
cast-brace or hinged knee brace. If significant functional symptoms
persist in an adolescent, the PCL can be reconstructed at or near
skeletal maturity. In a young child with grade III MCL or LCL injury in
addition to PCL injury, the collateral ligament can be surgically
repaired to convert the multiplane instability to single-plane
instability. PCL injury may be associated with ACL injury, primarily in
knee dislocations, and surgical intervention usually is appropriate for
this combination of injuries, especially in patients nearing skeletal
maturity.60
because the forces required to produce dislocation are more likely to
fracture the distal femoral or proximal tibial epiphysis.108
Acute knee dislocation usually involves major injuries of associated
soft tissues and ligaments and often neurovascular injuries. Injuries
typically occur in older skeletally mature adolescents from high-energy
trauma, such as motor vehicle injuries, pedestrian versus motor vehicle
injury, bicycle versus motor vehicle injury, trampoline injuries, and
high-energy contact sports.
and most information has been obtained from reports of knee
dislocations in adults. Because of the potential for associated
vascular injury, acute knee dislocations in children may be emergent
situations. The dislocation causes obvious deformity about the knee.
With anterior dislocation, the tibia is prominent in an abnormal
anterior position (Fig. 24-41). With posterior dislocation, the femoral condyles are abnormally prominent anteriorly.
knee should be evaluated with gentle stress testing. For isolated
anterior or posterior dislocations, the integrity of the collateral
ligaments should be carefully evaluated. Some knees may spontaneously
reduce after dislocation or reduce with manipulation of the leg for
transport.
carefully evaluated both before and after reduction, especially the
dorsalis pedis and posterior tibial pulses and peroneal nerve function.
Any abnormal vascular findings, either before or after reduction,
require arteriography.67,76,108,116,159
Arteriography is unnecessary when pulses are normal before and after
reduction; however, the vascular status should be carefully monitored
for 48 to 72 hours after reduction. Vascular status may also be
assessed with ultrasonography or MR angiography. Abnormalities in the
sensory or motor function of the foot and distribution of the peroneal
nerve function should be noted. Peroneal nerve injury has been reported
in 16% to 40% of cases.67,76,108,116,159
MRI is usually performed to assess the integrity of the cruciate and
collateral ligaments, the posterolateral and posteromedial corners, the
menisci, and the articular surfaces.
cruciate ligaments. With direct anterior or posterior dislocation, the
collateral ligaments and the soft tissues may be retained because the
femoral condyles are stripped out of their capsular and collateral
ligament attachments and when reduced slip back inside them. Associated
medial displacement
is
often accompanied by LCL disruption. Associated lateral displacement is
often accompanied by MCL disruption. Knee dislocations in adolescents
have been associated with tibial spine fractures, osteochondral
fractures of the femur or tibia, meniscal injuries, and peroneal nerve
injuries.67
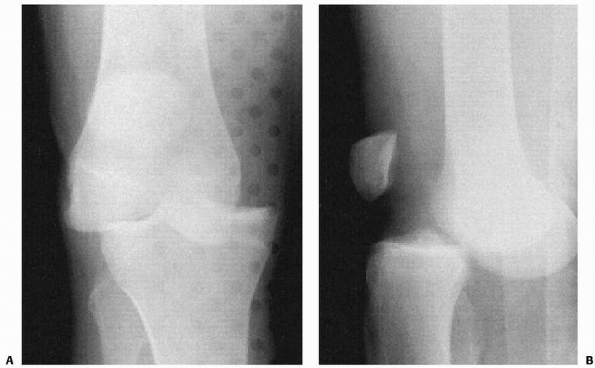 |
|
FIGURE 24-41 Dislocation of the knee. A,B. Anteromedial dislocation of the knee in a 14-year-old girl.
|
reconstructive management. Acutely, the knee is reduced under
anesthesia. The knee should then be examined to assess the ligamentous
injuries. The neurovascular status of the extremity is carefully
assessed pre- and postreduction. Vascular imaging is performed if
indicated. Arterial exploration and repair or bypass grafting is
performed by a vascular surgeon if indicated. If emergent vascular
repair is performed, fasciotomies are usually also performed however
ligamentous reconstruction is typically delayed. An MRI is obtained to
document the injured structures. The knee is braced with protected
weight bearing and limited motion.
after injury. Primary ligament repairs become more difficult after this
period of time because of scarring and lack of definition of tissues.
Reconstructions may be staged or at one setting. Surgery often combines
arthroscopic and open techniques. General principles include ligament
repair for collateral ligament injuries, ligament repair for cruciate
ligament avulsions, ligament reconstruction for midsubstance cruciate
ligament injuries, and meniscal repair. Allograft tissue is often used
because of the multiligamentous nature of the injury. PCL
reconstruction can be performed with tibial inlay techniques or
arthroscopic techniques with a tibial tunnel and one or two femoral
tunnels. Medially, the MCL can be primarily repaired or reattached if
avulsed. The medial meniscus may be torn if the MCL is torn in its
midsubstance. Laterally, the LCL, popliteofibular ligament, popliteus,
and posterolateral capsule may need to be repaired. The peroneal nerve
should be decompressed and protected during repair.
the substantial risk of stiffness after knee dislocation surgery.
Limited motion in a hinged knee brace and protected weight bearing are
utilized, followed by mobilization and strengthening.
-
With nonoperative treatment of complete
ACL tears in children and adolescents, sufficient counseling must be
performed so that the patient and the family understand the relative
risks and benefits of nonoperative treatment versus ACL reconstruction.
Compliance with bracing and activity restriction must be monitored.
Careful regular follow-up is necessary to evaluate for instability
episodes and further meniscal/chondral injury. Once further meniscal or
chondral injury occurs, ACL reconstruction should be advised because of
the risk of degenerative joint disease associated with injury episodes. -
Pitfalls to avoid with the
physeal-sparing iliotibial band reconstruction in prepubescents include
harvesting a short graft insufficient to reach the medial tibial
incision, difficulty passing the graft through the posterior joint
capsule, and difficulty passing the graft under the intermeniscal
ligament. -
Pitfalls to avoid with the transphyseal
hamstrings reconstruction in adolescents with growth remaining include
amputation of the hamstring grafts, poor tunnel placement, and graft
impingement. -
Based on the 15 cases of growth
disturbance after ACL reconstruction in skeletally immature patients
reported, the author recommends careful attention to technical details
during ACL reconstruction in skeletally immature patients, particularly
the avoidance of fixation hardware across the lateral distal femoral
epiphyseal plate.180 Care should also be taken to avoid injury to the vulnerable tibial tubercle apophysis.173,265
Given the cases of growth disturbances associated with transphyseal
placement of patellar tendon graft bone blocks, the author recommends
the use of soft tissue grafts. Large tunnels should likely be avoided
as likelihood of arrest is associated with greater violation of
epiphyseal plate
P.925cross-sectional
area. The two cases of genu valgum without arrest associated with
lateral extra-articular tenodesis raise additional concerns about the
effect of tension on physeal growth. Finally, care should be taken to
avoid dissection or notching around the posterolateral aspect of the
physis during over-the-top nonphyseal femoral placement to avoid
potential injury to the very close perichondrial ring and subsequent
deformity.173
tears in skeletally immature patients is generally poor with recurrent
instability leading to further meniscal and chondral injury which has
implications in terms of development of degenerative joint disease.11,115,121,147,209,220,222,244
surgical procedure. Several case series exist regarding ACL
reconstruction in skeletally immature patients. However, most series
are small and variably report the patients’ skeletal age and growth
remaining. Primary ligament repair61,92 and extra-articular tenodesis alone1158,209
have had poor results in children and adolescents, similar to adults.
Transphyseal reconstructions with tunnels that violate both the distal
femoral and proximal tibial physes have been performed with hamstrings
autograft, patellar tendon autograft, and allograft tissue.11,20,24,85,104,205,209,210,266,270,278,301
These anatomic ACL reconstruction procedures have high success rates as
in adult patients; however, there is risk injury to the physis,
particularly in prepubescent patients. In a follow-up outcome study of
61 knees in 59 skeletally immature Tanner stage 3 adolescents with
growth remaining (mean chronologic age: 14.7 years old, range: 11.6 to
16.9 years old) who underwent transphyseal reconstruction with
autogenous hamstrings graft and metaphyseal fixation, a revision rate
of 3% with excellent functional outcome, return to competitive sports,
and no cases of growth disturbance was found.181
Partial transphyseal reconstructions violate only one physis with a
tunnel through the proximal tibial physis and over-the-top positioning
on the femur or a tunnel through the distal femoral physis with an
epiphyseal tunnel in the tibia.17,44,123 These procedures are also near anatomic with good clinical results; however, the potential for growth disturbance exists.
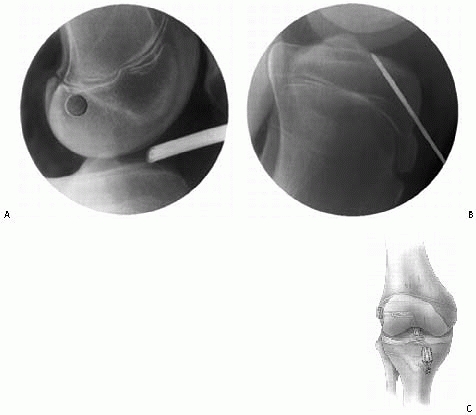 |
|
FIGURE 24-42 Physeal-sparing epiphyseal ACL reconstruction with autogenous hamstrings for prepubescents with growth remaining. A. Femoral tunnel placement within the epiphysis. B. Tibial tunnel placement within the epiphysis. C. Appearance after epiphyseal graft fixation.
|
described to avoid tunnels across either the distal femoral or proximal
tibial physis.14,52,77,122,162,218,238,293
In general, these procedures are nonanatomic and have some persistent
knee laxity; however, they avoid physeal violation. In a follow-up
outcome study of 44 skeletally immature prepubescent children who were
Tanner stage 1 or 2 (mean chronologic age: 10.3 years old; range:
3.6-14 years old) who underwent the physeal sparing combined
intra-articular and extra-articular ACL reconstruction technique using
autogenous iliotibial band that were described above, a revision ACL
reconstruction rate of 4.5% with excellent functional outcome, return
to competitive sports,
and no cases of growth disturbance was found.171,172 Anderson14,15
described a more anatomic physeal-sparing reconstruction in
prepubescent children by utilizing carefully placed epiphyseal femoral
and tibial tunnels with an autogenous hamstrings graft and epiphyseal
fixation (Fig. 24-42). In 12 skeletally
immature patients with mean age 13.3 years old (SD: 1.4), he found
excellent functional outcome without growth disturbance.14,15
similar to adults: arthrofibrosis, persistent instability, unrecognized
concomitant injury, infection, graft failure, neurovascular injury, and
donor site morbidity. In skeletally immature patients, growth
disturbance can occur from iatrogenic physeal injury as previously
discussed.
F, Cassard X, Sales de Gauzy J, et al. Meniscal tears in children and
adolescents: results of operative treatment. J Pediatr Orthop B
2007;16(1):56-60.
N, Ochi M, Uchio Y, et al. Torn discoid lateral meniscus treated using
partial central meniscectomy and suture of the peripheral tear.
Arthroscopy 2004;20(5): 536-542.
P, Bertini FA, Buzzi R, et al. Arthroscopic meniscectomy for discoid
lateral meniscus in children and adolescence: a 10-year follow-up. Am J
Knee Surg 1999;12: 83-87.
AM, Burke DL. In-vitro measurement of static pressure distribution in
synovial joints. Part I: tibial surface of the knee. J Biomech Eng
1983;105:216-225.
JH, Lee SH, Yoo JC, et al. Arthroscopic partial meniscectomy with
repair of the peripheral tear for symptomatic discoid lateral meniscus
in children: results of minimum 2 years of follow-up. Arthroscopy
2008;24(8):888-898.
JP. Osteochondral fracture in the knee joint associated with
hypermobility and dislocation of the patella: report of 18 cases. J
Bone Joint Surg Am 1965;47: 1491-1502.
PM. Osteochondral fractures and osteochondritis dissecans in
sportsmen’s knee injuries. J Bone Joint Surg Br 1977;59:108.
PM, Patel DV, Marx CI. Congenital discoid lateral meniscus in children:
a followup study and evaluation of management. J Bone Joint Surg Br
1991;73:932-939.
PM, Patel DV, Zorrilla P. The natural history and treatment of rupture
of the anterior cruciate ligament in children and adolescents. A
prospective review. J Bone Joint Surg Br 2002;84(1):618-619.
AF. Transepiphyseal replacement of the anterior cruciate ligament in
skeletally immature patients. A preliminary report. J Bone Joint Surg
Am 2003;85-A(7): 1255-1263.
AF. Transepiphyseal replacement of the anterior cruciate ligament using
quadruple hamstring grafts in skeletally immature patients. J Bone
Joint Surg Am 2004; 86-A(Suppl 1 Pt 2):201-209.
AF, Pagnani MJ. Osteochondritis dissecans of the femoral condyles:
long-term results of excision of the fragment. Am J Sports Med 1997;25:
830-834.
M, Noyes FR, Barber-Westin SD. Anterior cruciate ligament allograft
reconstruction in the skeletally immature athlete. Am J Sports Med
1994;22(1):48-54.
J. The diagnosis and management of meniscus injuries in skeletally
immature athlete. Oper Tech Sports Med 1998;6:186-196.
H. Late results after meniscectomy in the knee joint: a clinical and
roentgenologic follow-up investigation. Acta Orthop Scand Suppl
1970;133:1-111.
SP, Warren RF, Spivak JM. Meniscal repair using an exogenous fibrin
clot: an experimental study in dogs. J Bone Joint Surg Am
1988;70:1209-1217.
ER, Ganley TJ, Goode JR, et al. Anterior cruciate ligament
reconstruction in adolescents with open physes. Am J Sports Med
2000;28(2):168-175.
RS, Banks AJ. Arthroscopically guided Kirschner wire fixation for
fractures of the intercondylar eminence of the tibia. J R Coll Surg
Edinb1995;40:260-262.
ME, Fu FH, Mentago R. Meniscal tears: the effect of menisectomy and of
repair on intraarticular contact areas and stress in the human knee. Am
J Sports Med 1986; 14:270-274.
FH. III. Acute dislocation of the patella, osteochondral fractures, and
injuries to the extensor mechanism of the knee. Instr Course Lect
1976;25:40-49.
MP, Wiley JJ. Fractures of the tibial spine in children. An evaluation
of knee stability. J Bone Joint Surg Br 1988;70B:228-230.
LS, Vidal AF. Traumatic patellar dislocation in children and
adolescents: treatment update and literature review. Curr Opin Pediatr
2004;16(1):29-36.
CT, Potter HG, Paletta GA Jr. The relationship of the femoral origin of
the anterior cruciate ligament and the distal femoral physeal plate in
the skeletally immature knee. An anatomic study. Am J Sports Med
2001;29:781-787.
G, Biant LC, Carrington RW, et al. A prospective, randomized comparison
of autologous chondrocyte implantation versus mosaicplasty for
osteochondral defects in the knee. J Bone Joint Surg Br
2003;85(2):223-230.
GC, Mascia A, Miniaci A. Treatment of unstable osteochondritis
dissecans lesions of the knee using autogenous osteochondral grafts
mosaicplasty. Arthroscopy 1999; 15:312-316.
T, Gokce A, Bekler H. Osteochondritis dissecans of the medial femoral
condyle associated with malformation of the menisci. Orthopedics
2008;31(5):504.
S, Davis D, Dina T, et al. A prospective and blinded investigation of
magnetic resonance imaging of the knee: abnormal findings in
asymptomatic subjects. Clin Orthop Relat Res 1992;282:177-185.
K. Imaging of acute injuries of the articular surfaces (chondral,
osteochondral, and subchondral fractures). Skeletal Radiol
1999;28:545-560.
MR, Romero A, Kubiak E, et al. Suture versus screw fixation of
displaced tibial eminence fractures: a biomechanical comparison.
Arthroscopy 2005;21(10): 1172-1176
TA, Russell D. Interarticular horizontal dislocation of the patella: a
case report. J Bone Joint Surg Am 1965;47:1393-1396.
GD, Ahmad CS. Combined medial patellofemoral ligament and medial
patellotibial ligament reconstruction in skeletally immature patients.
J Knee Surg 2008;21(4): 328-332.
DB, Viola A, Fulkerson JP. Entrapment of the medial meniscus in a
fracture of the tibial eminence arthroscopy. Arthroscopy 1988;4:47-50.
MS, Noyes FR. Arthroscopic evaluation of meniscal repairs after
anterior cruciate ligament reconstruction and immediate motion. Am J
Sports Med 1991;19:489-494.
WD, Vittori JM. The incidence of healing in arthroscopic meniscal
repairs in the anterior cruciate ligament-reconstructed knee versus
stable knees. Am J Sports Med 1992;20:176-181.
WG, Shelbourne KD, Zoellner GB, et al. Treatment of knee joint
instability secondary to rupture of the posterior cruciate ligament:
report of a new procedure. J Bone Joint Surg Am 1983;65:310-322.
CR, Ogden JA. Development of the menisci of the human knee joint:
morphological changes and their potential role in childhood meniscal
injury. J Bone Joint Surg Am 1983;65:538-547.
CH Jr, Braitman HE. Popliteal artery injury following fracture or
dislocation at the knee: diagnosis and management. Arch Surg
1977;112:969-973.
KE, Arnoczky SP. Meniscus repair: basic science, indications for
repair, and open repair. Instr Course Lect 1994;43:65-74.
M, Ochi M, Sumen Y, et al. Reconstruction of the medial patellofemoral
ligament for the treatment of habitual or recurrent dislocation of the
patella in children. J Bone Joint Surg Br 2003;85(6):887-890.
M, Ochi M, Sumen Y, et al. Relationship between osteochondritis
dissecans of the lateral femoral condyle and lateral menisci types. J
Pediatr Orthop 2006;26(1): 79-82.
S, Burks R, Bachus K. Soft tissue restraints to lateral patellar
translation in the human knee. Am J Sports Med 1998;26:59-65.
SF, Vaupel GL, Dye CC. Conscious neurosensory mapping of the internal
structures of the human knee without intraarticular anesthesia. Am J
Sports Med 1998;26: 773-777.
JL, Cardenas CD, Sopa D. Avulsion of the femoral attachment of the
anterior cruciate ligament in a 7-year-old child. J Bone Joint Surg Am
1982;64:1376-1378.
PH, Grana WA. Anterior cruciate ligament reconstruction in the immature
athlete: long-term results of intra-articular reconstruction. Am J Knee
Surg 2001;14: 232-237.
TB, Greene CC, Baratta RV, et al. The effect of placing a tensioned
graft across open growth plates. A gross and histologic analysis. J
Bone Joint Surg Am 2001;83-A(5):725-734.
AK, Becker C, Weimann A, et al. Biomechanical evaluation of different
fixation methods for tibial eminence fractures. Am J Sports Med
2007;35(3):404-410.
S, Larsen ST, Schmidt MB. The significance of hemarthrosis of the knee
in children. Arch Orthop Trauma Surg 1988;107(2):96-98.
L, Svenningsen S, Benum P. Poor results of anterior cruciate ligament
repair in adolescents. Acta Orthop Scand 1988;59:684-686.
S, Sondergard Petersen PE. Incarceration of the meniscus in fractures
of the intercondylar eminence of the tibia in children. Injury
1974;15:236-238.
JF, Marshall JL. Injury to the anterior cruciate ligament producing the
pivot-shift sign. J Bone Joint Surg Am 1979;61:710-714.
JF, Marshall JL. The natural history and diagnosis of anterior cruciate
ligament insufficiency. Clin Orthop Relat Res 1980;147:29-38.
R, Broom ND, Hardy AE, et al. Why is the adolescent joint particularly
susceptible to osteochondral shear fracture? Clin Orthop Rel Res
2000;381:212-221.
PJ. Meniscal lesions in the adolescent: the role of arthroscopy in the
management of adolescent knee problems. In: Kennedy JC, ed. The Injured
Adolescent Knee. Baltimore: Williams & Wilkins, 1979:43-76.
R, Wheatley W, Uribe JW, et al. Intra-articular anterior cruciate
ligament reconstruction using patellar tendon allograft in the
skeletally immature patient. Arthroscopy 2002;18(8):824-828.
K, Iseki F, Mikura Y. Partial resection of the discoid meniscus in the
child’s knee. J Bone Joint Surg Br 1981;63:391-395.
IS, Jackson JP. Tibial intercondylar fractures in children: a review of
the classification and the treatment of malunion. Injury
1981;13:165-169.
HM, Haus J. Intraarticular stabilization after anterior cruciate
ligament tear in children and adolescents: results 6 years after
surgery. Knee Surg Sports Traumatol Arthrosc 2006;14(5):417-424.
F, Ellermann A, Hoffmann F, et al. Multicenter-study of operative
treatment of intraligamentous tears of the anterior cruciate ligament
in children and adolescents: comparison of four different techniques.
Knee Surg Sports Traumatol Arthrosc 2006; 14(9):797-803.
H, Glasgow S, Sapega A, et al. Magnetic resonance imaging of knee
disorders: clinical value and cost effectiveness in a sports medicine
practice. Am J Sports Med 1996;24:99-103.
J, Hungerford DS, Zindel M. Patellofemoral joint mechanics and
pathology: I. Functional anatomy of the patellofemoral joint. J Bone
Joint Surg Br 1976;58: 287-290.
A, Ballard A. Posterior cruciate ligament avulsion associated with
ipsilateral femur fracture in a 10-year-old child. J Trauma
1988;28:1393-1396.
BK, Lange RH, Fujisaki CK, et al. Anterior cruciate ligament tears in
skeletally immature patients: meniscal pathology at presentation and
after attempted conservative treatment. Arthroscopy 1992;8(2):229-233.
WW, Pysle SI, eds. Radiographic Atlas of Skeletal Development of the
Hand and Wrist. 2nd ed. Stanford: Stanford University Press, 1959.
V, Falciglia F, Gigante A, et al. The effect of intra-articular ACL
reconstruction on the growth plates of rabbits. J Bone Joint Surg Br
1994;76(6):960-963.
V, Falciglia F, Stanitski CL. Physeal-sparing intraarticular anterior
cruciate ligament reconstruction in preadolescents. Am J Sports Med
2003;31(6):949-953.
V, Falciglia F, Stanitski CL. Preoperative evaluation and anterior
cruciate ligament reconstruction technique for skeletally immature
patients in Tanner stages 2 and 3. Am J Sports Med 2003;31(6):941-948.
T, Uematsu K, Kasanami R, et al. Long-term clinical and radiographic
follow-up of total resection for discoid lateral meniscus. Arthroscopy
2006;22(12):1339-1343.
JE, Micheli LJ, McManana GB. Semitendinosus tenodesis for recurrent
subluxation or dislocation of the patella. Clin Orthop Relat Res
1979;144:31-35.
M, Shino K, Kawano K, et al. Usefulness of MRI for detecting
intrasubstance tear and/or degeneration of lateral discoid meniscus.
Arthroscopy 1994;10:645-653.
Y, Yoshida G, Tomihara T, et al. Bilateral osteochondritis dissecans of
the lateral femoral condyle following bilateral total removal of
lateral discoid meniscus: a case report. Arch Orthop Trauma Surg
2008;128(11):1265-1268.
LK, Yamaga H, Ida K, et al. Arthroscopic meniscectomy for discoid
lateral meniscus in children. J Bone Joint Surg Am 1988;70:1495-1500.
JM, Masear VR. Avulsion fracture of the tibial eminence associated with
severe medial ligamentous injury in an adolescent: a case report and
review of the literature. Am J Sports Med 1984;12:330-333.
NJ, Houghton GR. Osteochondral fractures of the knee in children. In:
Houghton GR, Thompson GH, eds. Problematic Musculoskeletal Injuries in
Children. London: Butterworths, 1983.
RY, Rivera VR, Pautz MJ, et al. Ligamentous laxity of the knee during
childhood and adolescence. J Pediatr Orthop 2008;28(2):184-187.
JB, Letts M, Yang J. Effects of a tensioned tendon graft in a bone
tunnel across the rabbit physis. Clin Orthop Relat Res 2001;391:275-281.
TW, Hsu KY, Cheng CY, et al. Arthroscopic suture fixation of tibial
eminence avulsion fractures. Arthroscopy 2008;24(11):1232-1238.
JC, Andrews JR, Cross MJ, et al. Classification of knee ligament
instabilities: part I. The medial compartment and cruciate ligaments. J
Bone Joint Surg Am 1976; 58:159-172.
JC, Hergenroeder PT, Courtenay BG. Osteochondritis dissecans of the
femoral condyles. J Bone Joint Surg Am 1984;66:1340-1348.
H. Arthroscopic treatment of lateral discoid meniscus: technique and
long-term results. Clin Orthop Relat Res 1982;167:19-28.
PA. Nonoperative treatment of complete tears of the medial collateral
ligaments of the knee. J Bone Joint Surg Am 1983;65:323-329.
PM, Nystrom A, Werner S, et al. Anterior cruciate ligament injuries in
skeletally immature patients. J Pediatr Orthop 1996;16(5):673-677.
PM, Westblad P, Johansson C, et al. Long-term follow-up of anterior
tibial spine fractures in children. J Pediatr Orthop 1995;15:63-68.
EW, McLeod TL. Osteochondral fragments of the distal end of the femur
fixed with bone pegs: report of two cases. J Bone Joint Surg Am
1977;59:677-679.
MJ, Lucas GL, Dusek JK, et al. Isolated arthroscopic meniscal repair: a
long-term outcome study (more than 10 years). Am J Sports Med
1999;27:44-49.
KN, Pogrund H. Traumatic rupture of the medial ligament of the knee in
a 4-year-old boy: a case report and review of the literature. J Bone
Joint Surg Am 1978; 60:402-403.
YB, Yum JK, Koo BH. A new method for arthroscopic treatment of tibial
eminence fractures with eyed Steinmann pins. Arthroscopy
1999;15:672-675.
P, Järvinen M. Knee ligament injuries in adolescents: 8-year follow-up
of conservative management. J Bone Joint Surg Br 1988;70:772-776.
EB. Discoid lateral meniscus of the knee joint. nature, mechanism, and
operative treatment. J Bone Joint Surg Am 1957;39:77-87.
SH, Ha KI, Ahn JH, et al. Anterior cruciate ligament reconstruction in
the young patient without violation of the epiphyseal plate.
Arthroscopy 1999;15(7):792-795.
YG, Ihn JC, Park SK, et al. An arthroscopic analysis of lateral
meniscal variants and a comparison with MRI findings. Knee Surg Sports
Traumatol Arthrosc 2006; 14(1):20-26.
AG. Meniscal lesions in children and adolescents: a review of the
pathology and clinical presentation. Injury 1983;15:105-108.
KE, Kocher MS, Hresko MT, et al. Discoid lateral meniscus: prevalence
of peripheral rim instability. J Pediatr Orthop 2004;24:79-82.
S, Koltai JL, Dittmer H. Significance of arthroscopy in children with
knee joint injuries. Eur J Pediatr Surg 1992;2(3):169-172.
MS, DiCanzio J, Zurakowski D, et al. Diagnostic performance of clinical
examination and selective magnetic resonance imaging in the evaluation
of intraarticular knee disorders in children and adolescents. Am J
Sports Med 2001;29:292-296.
MS, Foreman ES, Micheli LJ. Laxity and functional outcome after
arthroscopic reduction and internal fixation of displaced tibial spine
fractures in children. Arthroscopy 2003;19:1085-1090.
MS, Garg S, Micheli LJ. Physeal sparing reconstruction of the anterior
cruciate ligament in skeletally immature prepubescent children and
adolescents. J Bone Joint Surg Am 2005;87(11):2371-2379.
MS, Garg S, Micheli LJ. Physeal sparing reconstruction of the anterior
cruciate ligament in skeletally immature prepubescent children and
adolescents. Surgical technique. J Bone Joint Surg Am 2006;88(Suppl 1
Pt 2):283-293.
MS, Hovis WD, Curtin MJ, et al. Anterior cruciate ligament
reconstruction in skeletally immature knees: an anatomical study. Am J
Orthop 2005;34(6):285-290.
MS, Mandiga R, Klingele KE, et al. Anterior cruciate ligament injury
versus tibial spine fracture in the skeletally immature knee: a
comparison of skeletal maturation and notch width index. J Pediatr
Orthop 2004;24(2):185-188.
MS, Micheli LJ. The pediatric knee: evaluation and treatment. In Insall
JN, Scott WN, eds. Surgery of the Knee. 3rd ed. New York:
Churchill-Livingstone, 2001: 1356-1397.
MS, Micheli LJ, Gerbino PG, et al. Tibial eminence fractures in
children: prevalence of meniscal entrapment. Am J Sports Med
2003;31(3):404-407.
MS, Micheli LJ, Yaniv M, et al. Functional and radiographic outcome of
juvenile osteochondritis dissecans of the knee treated with
transarticular drilling. Am J Sports Med 2001;29(5):562-566.
MS, Micheli LJ, Zurakowski D, et al. Partial tears of the anterior
cruciate ligament in children and adolescents. Am J Sports Med
2002;30(5):697-703.
MS, Saxon HS, Hovis WD, et al. Management and complications of anterior
cruciate ligament injuries in skeletally immature patients: survey of
the Herodicus Society and the ACL Study Group. J Pediatr Orthop
2002;22(4):452-457.
MS, Smith JT, Zoric BJ, et al. Transphyseal anterior cruciate ligament
reconstruction in skeletally immature pubescent adolescents. J Bone
Joint Surg Am 2007; 89(12):2632-2639.
JD, Sanders JO. Valgus deformity after reconstruction of the anterior
cruciate ligament in a skeletally immature patient. A case report. J
Bone Joint Surg
R, Burnett Q, Veenstra M, et al. The prevalence of abnormal magnetic
resonance imaging findings in asymptomatic knees: with correlation of
magnetic resonance imaging arthroscopic findings in symptomatic knees.
Am J Sports Med 1994;22: 739-745.
DH, Kim TH, Kim JM, et al. Results of subtotal/total or partial
meniscectomy for discoid lateral meniscus in children. Arthroscopy
2009;25(5):496-503.
YH, Chin LS, Wang NH, et al. Anterior tibial spine fracture in
children: follow-up evaluation by biomechanical studies. Chung Hua I
Hsueh Tsa Chih 1996;58:183-189.
IM, Torzilli PA, Warren RF. The effect of medial menisectomy on
anterior-posterior motion of the knee. J Bone Joint Surg Am
1982;64:883-888.
AD, Imbuldeniya AM, Hunt DM. Transphyseal reconstruction of the
anterior cruciate ligament in prepubescent children. J Bone Joint Surg
Br 2008;90(10): 1317-1322.
IK, Kirkley A, Fowler PJ, et al. The outcome of operatively treated
anterior cruciate ligament disruptions in the skeletally immature
child. Arthroscopy 1997;13(5): 627-634.
SJ. Avulsion of a fibrous union of the intercondylar eminence of the
tibia: a case report. J Bone Joint Surg Am 1994;76:1565-1567.
ML, Guillaume JM, Launay F, et al. Surgical management of type II
tibial intercondylar eminence fractures in children. J Pediatr Orthop B
2008;17(5):231-235.
J, Chaimsky G, Freedman A, et al. The anatomy of tibial eminence
fractures: arthroscopic observations following failed closed reduction.
J Bone Joint Surg Am 2002; 84-A(11):1933-1938.
R, Wissinger AH, Donaldson WF. Preliminary experience with a method of
quadricepsplasty in recurrent subluxation of the patella. J Bone Joint
Surg Am 1975; 57:600-607.
JY, Adili A, Otsuka NY, et al. Follow-up study of arthroscopic
reduction and fixation of type III tibial eminence fractures. J Pediatr
Orthop 1998;18:475-477.
JY, Otsuka NY, McLean J. An arthroscopic technique for the reduction
and fixation of tibial-eminence fractures. J Pediatr Orthop
1996;16:119-121.
AT, Duncan D, Oka R, et al. Biomechanical comparison of four different
fixation techniques for pediatric tibial eminence avulsion fractures. J
Pediatr Orthop 2008; 28(2):159-162.
M, Pizzutillo PD, Peoples AB, et al. Menisectomy in children: a
long-term follow-up study. Am J Sports Med 1983;11:111-115.
MJ, Siegel MG. Arthroscopic reconstruction of the ACL with
semitendinosisgracilis autograft in skeletally immature adolescent
patients. Am J Knee Surg 1997; 10(2):60-69.
PJ, Micheli LJ. Avulsion of the femoral attachment of the posterior
cruciate ligament in an 11-year-old boy: a case report. J Bone Joint
Surg Am 1979;61:431-432.
JR, Rettig AC, Shelbourne KD. Anterior cruciate ligament injuries in
the young athlete with open physes. Am J Sports Med 1988;16(1):44-47.
JR, Shelbourne KD, Porter DA, et al. Patellar tendon graft
reconstruction for midsubstance anterior cruciate ligament rupture in
junior high school athletes: an algorithm for management. Am J Sports
Med 1994;22:478-484.
JG. Lessons learned after second-look arthroscopy in type III fractures
of the tibial spine. J Pediatr Orthop 1995;15:59-62.
JG. The role of arthroscopic surgery in the treatment of fractures of
the intercondylar eminence of the tibia. J Bone Joint Surg Br
1982;64B:477-480.
F, Rang M, Heslin DJ. Acute dislocation of the patella in children: the
natural history. Clin Orthop Relat Res 1979;139:88-91.
MH. Isolated avulsion of the tibial attachment of the posterior
cruciate ligament of the knee. J Bone Joint Surg Am 1975;57:669-672.
MH, McKeever FM. Follow-up notes. fracture of the intercondylar
eminence of the tibia. J Bone Joint Surg Am 1970;52:1677-1684.
LJ, Rask B, Gerberg L. Anterior cruciate ligament reconstruction in
patients who are prepubescent. Clin Orthop Relat Res 1999;364:40-47.
PJ, Willis AA, Warren RF. Associated injuries in pediatric and
adolescent anterior cruciate ligament tears: does a delay in treatment
increase the risk of meniscal tear? Arthroscopy 2002;18(9):955-999.
H, Kubota K, Shiraishi M, et al. The conservative treatment of complete
tears of the anterior cruciate ligament in skeletally immature
patients. J Bone Joint Surg Br 1995;77(6):890-894.
ML, Wallin G, Wikstad I. Fractures of the intercondylar eminence of the
tibia. A review of 35 patients. J Bone Joint Surg Br 1981;63B:89-91.
KJ, Dowdall J, Grannell M, et al. Tibial spine fractures. An analysis
of outcome in surgically treated type III injuries. Injury
1999;30:289-292.
J, Reynders R, Broos P. Transepiphyseal fixation of anterior cruciate
avulsion in a child: report of a complication and review of the
literature. Arch Orthop Trauma Surg 1993;112:101-103.
DC, Drez D, Finney TP. Lateral meniscal variant with absence of
posterior coronary ligament. J Bone Joint Surg Am 1992;74:1186-1190.
Y, Aalto K, Kallio PE. Acute patellar dislocation in children:
incidence and associated osteochondral fractures. J Pediatr Orthop
1994;14:513-515.
FR, Barber-Westin SD. Arthroscopic repair of meniscal tears extending
into the avascular zone in patients younger than 20 years of age. Am J
Sports Med 2002;30: 589-600.
FR, Bassett RW, Grood ES, et al. Arthroscopy in acute traumatic
hemarthrosis of the knee: incidence of anterior cruciate tears and
other injuries. J Bone Joint Surg Am 1980;62:687-695.
FR, Delucas JL, Torvik PJ. Biomechanics of ACL failure: an analysis of
strainrate sensitivity and mechanisms of failure in primates. J Bone
Joint Surg Am 1974; 56A: 236-253.
K, Miura H, Matsuda S, et al. Arthroscopic resection of the discoid
lateral meniscus: long-term follow-up for 16 years. Arthroscopy
2006;22(9):967-971.
HJ, Klasen HJ, Reddingius RE. Fractures of the intercondylar eminenece
in children and adolescents. Arch Orthop Trauma Surg 1988;107:242-247.
AW, Drez D, Cooper JL. Anterior cruciate ligament injuries in patients
with open physes. Am J Sports Med 1994;22(1):44-47.
D, Dimakopoulos P, Penoncourt P. Bucket handle tear of a discoid
meniscus: arthroscopic diagnosis and partial excision. Orthopaedics
1986;9:607-608.
F, Mignani G, Valdiserri L. Fractures of the intercondylar eminence of
the tibia in children. Ital J Orthop Traumatol 1986;12:441-446.
L, Minas T, Brittberg M, et al. Treatment of osteochondritis dissecans
of the knee with autologous chondrocyte transplantation: results at 2
to 10 years. J Bone Joint Surg Am 2003;85-A(Suppl 2):17-24.
DW, Callaghan JJ, Sikes RA, et al. The accuracy of selective MRI
compared to the findings of arthroscopy of the knee. J Bone Joint Surg
Am 1988;70:192-198.
AE, Letts RM, Jarvis JG. Anterior cruciate ligament tears in children:
an analysis of operative versus nonoperative treatment. J Pediatr
Orthop 1997;17(4): 505-511.
DA, Friederich NF, Buzzi R, et al. Discoid lateral meniscus in
children: long-term follow-up after total meniscectomy. J Bone Joint
Surg Am 1998;8:1579-1586.
JM. Fractures of the condyles of the tibia: an anatomical and clinical
end-result study of 100 cases. J Bone Joint Surg Am 1968;50:1505-1521.
SC, Driscoll SE. Simultaneous osteochondral avulsion of the femoral and
tibial insertion of the anterior cruciate ligament: report of a case in
a 13-year-old boy. J Bone Joint Surg Am 1981;63:1342-1343.
TD, Paulos LE, Parker RD, et al. Discoid lateral meniscus: case report
of arthroscopic attachment of a symptomatic Wrisberg-ligament type.
Arthroscopy 1987; 3:277-282.
AC, Chesterman PJ. Isolated avulsion of the tibial attachment of the
posterior cruciate ligament in childhood. J Bone Joint Surg Br
1986;68:747.
MH, Noyes FR, Barber-Westin SD. Arthroscopic repair of meniscal tears
that extend into the avascular zone. A review of 198 single and complex
tears. Am J Sports Med 1998;26:87-95.
ND, Hoffman BK. Tear of the attachment of a normal meniscus of the knee
in a 4-year-old child. J Bone Joint Surg Am 1970;52:809-811.
WE, Wilkins KE, Neidre A. Acute insufficiency of the posterior cruciate
ligament in children. J Bone Joint Surg Am 1980;62:129-130.
R, Pape D, Kohn D. The risk of growth changes during transphyseal
drilling in sheep with open physes. Arthroscopy 2008;24(7):824-833.
WH Jr, Bibliani LU, Andrews DL, et al. Osteochondritis dissecans of the
knee: a surgical approach. Orthop Rev 1985;14(2):56-63.
A, Lakshmanan P, Peehal J, et al. An analysis of different types of
surgical fixation for avulsion fractures of the anterior tibial spine.
Acta Orthop Belg 2008;74(1): 90-97.
KG, Apel PJ, Pfeiffer RP, et al. The anatomy of the proximal tibia in
pediatric and adolescent patients: implications for ACL reconstruction
and prevention of physeal arrest. Knee Surg Sports Traumatol Arthrosc
2007;15(4):320-327.
KD, Gray T, Wiley BV. Results of transphyseal anterior cruciate
ligament reconstruction using patellar tendon autograft in Tanner stage
3 or 4 adolescents with clearly open growth plates. Am J Sports Med
2004;32(5):1218-1222.
SC, Markolf KL. The role of the meniscus in the anterior-posterior
stability of the loaded cruciate deficient knee: effect of partial
versus total excision. J Bone Joint Surg Am 1988;68:71-79.
PT, Metcalf MH, Larson RV. Anterior cruciate ligament injuries in the
skeletally immature patient. Am J Orthop 1999;28(11):624-628.
DM, Arnoczky SP, Dodds J, et al. The effect of drilling and soft tissue
grafting across open growth plates. A histologic study. Am J Sports Med
1995;23(4): 431-435.
CL. Anterior cruciate ligament injury in the skeletally immature
patient: diagnosis and treatment. J Am Acad Orthop Surg
1995;3(3):146-158.
CL. Correlation of arthroscopic and clinical examinations with magnetic
resonance imaging findings of injured knees in children. Am J Sports
Med 1998;26:2-6.
CL, Harvell JC, Fu F. Observations on acute knee hemarthrosis in
children and adolescents. J Pediatr Orthop 1993;13(4):506-510.
CL, Paletta GA. Articular cartilage injury with acute patellar
dislocation in adolescents. Am J Sports Med 1998;26(1):52-55.
JR, Briggs KK, Rodrigo JJ, et al. Outcomes of microfracture for
traumatic chondral defects of the knee: average 11-year follow-up.
Arthroscopy 2003;19(5): 477-484.
S, DiGennaro GL, Marchiodi L, et al. Arthroscopic surgery of the
discoid meniscus during childhood. Chir Degli Org Mov 1997;82:335-339.
O, Miyatsu M, Yamashita I, et al. Problems with repeated arthroscopic
surgery in the discoid meniscus. Arthroscopy 1991;7:68-71.
DJ, Dines DM, Hershon SJ, et al. Natural history of a type III fracture
of the intercondylar eminence of the tibia in an adult: a case report.
Am J Sports Med 1989; 17:132-133.
Y, Ikata T, Yoshida S, et al. MRI high signal intensity in the menisci
of asymptomatic children. J Bone Joint Surg Br 1998;80:463-467.
JM, Whitehouse RH. Clinical longitudinal standards for height, weight,
height velocity, and stages of puberty. Arch Dis Child 1976;51:170-179.
JJ, Arciero RA. Arthroscopic evaluation of meniscal repairs: factors
that affect healing. Am J Sports Med 1994;22:797-802.
T. Isolated avulsion fracture of the tibial attachment of the posterior
cruciate ligament. J Bone Joint Surg Am 1977;59:68-72.
V, Kinnuen P, Serlo W. Arthroscopy of the acute traumatic knee in
children. Prospective study of 138 cases. Acta Orthop Scand
1993;64(5):580-582.
R, Cunningham F. Arthroscopic treatment of the discoid lateral
meniscus: Results of long term followup. Arthroscopy 1989;5:101-109.
B, Lutz N, Dutoit M, et al. Nonunion after fracture of the anterior
tibial spine: case report and review of the literature. J Pediatr
Orthop B 2009;18(2):90-92.
V, Williams A, Tennant SJ, et al. Meniscal movement: an in-vivo study
using dynamic MRI. J Bone Joint Surg Br 1999;81:37-41.
JR, Irribarra LA, Baar AK, et al. Arthroscopic fixation of displaced
tibial eminence fractures: a new growth plate-sparing method.
Arthroscopy 2008;24(11):1239-1243.
As, Wosk J. Shock absorption of the menisectomized and painful knees: a
comparative in vivo study. J Biomed Eng 1983;5:157-161.
P, Galli M, Bait C, et al. Surgical treatment of anterior cruciate
ligament injuries in adolescents using double-looped semitendinosis and
gracilis tendons: supraepiphysary femoral and tibial fixation.
Arthroscopy 2004;20(4):447-449.
JI, Broussard TS. Disruption of the anterior cruciate ligament in a
3-year-old child. J Bone Joint Surg Am 1984;66:1113-1114.
ER, Root L, Lierner U, et al. Discoid lateral meniscus in
children—long-term follow-up after excision. J Bone Joint Surg Am
1995;77(9):1357-1361.
LM, Scholz S, Rusch M, et al. Hemarthrosis after trauma to the
pediatric knee joint: what is the value of magnetic resonance imaging
in the diagnostic algorithm? J Pediatr Orthop 2001;21(3):338-342.
W, Canale ST, Dutkowsky JP, et al. Prediction of angular deformity and
leg-length discrepancy after anterior cruciate ligament reconstruction
in skeletally immature patients. J Pediatr Orthop 1994;14:516-521.
RB, Blokker C, Stoll TM, et al. Long-term follow-up of anterior tibial
eminence fractures. J Pediatr Orthop 1993;13:361-364.
JH, Nunley JA. Compressive fixation of osteochondritis dissecans
fragments with Herbert screws. J Orthop Trauma 1987;1:74-77.
SL-Y, Hollis JM, Adams DJ, et al. Tensile properties of the human
femur-anterior cruciate ligament-tibia complex: the effects of specimen
age and orientation. Am J Sports Med 1991;19:217-225.
RR, Henderson RC, Campion ER, et al. Menisectomy in children and
asolescents: a long term follow-up study. Clin Orthop Relat Res
1992;279:180-189.
WJ, Choi IH, Chung CY, et al. Discoid lateral meniscus in children:
limited knee extension and meniscal instability in the posterior
segment. J Pediatr Orthop 2008; 28(5):544-548.
RB. The external semilunar cartilage as a complete disc. In: Cleland J,
Mackey JY, Young RB, eds. Memoirs and Memoranda in Anatomy. London:
Williams and Norgate, 1889:179.
B. Avulsion fracture of the tibial eminence: treatment by open
reduction and pinning. J Bone Joint Surg Am 1977;59:1111-1114.
MS, Borrello JA, Siegel MJ et al. Pediatric knee MR imaging: pattern of
injury in the immature skeleton. Radiology 1994;190:397-401.
