Hip Dislocations
-
Up to 50% of patients sustain concomitant fractures elsewhere at the time of hip dislocation.
-
Unrestrained motor vehicle accident
occupants are at a significantly higher risk for sustaining a hip
dislocation than passengers wearing a restraining device. -
Anterior dislocations constitute 10% to
15% of traumatic dislocations of the hip, with posterior dislocations
accounting for the remainder. -
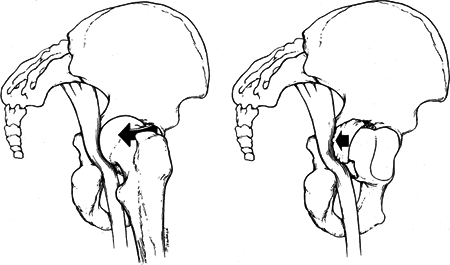
Sciatic nerve injury is present in 10% to 20% of posterior dislocations (Fig. 27.1).
-
The hip articulation has a
ball-and-socket configuration with stability conferred by bony and
ligamentous restraints, as well as the congruity of the femoral head
with the acetabulum. -
The acetabulum is formed from the confluence of the ischium, ilium, and pubis at the triradiate cartilage.
-
Forty percent of the femoral head is
covered by the bony acetabulum at any position of hip motion. The
effect of the labrum is to deepen the acetabulum and increase the
stability of the joint. -
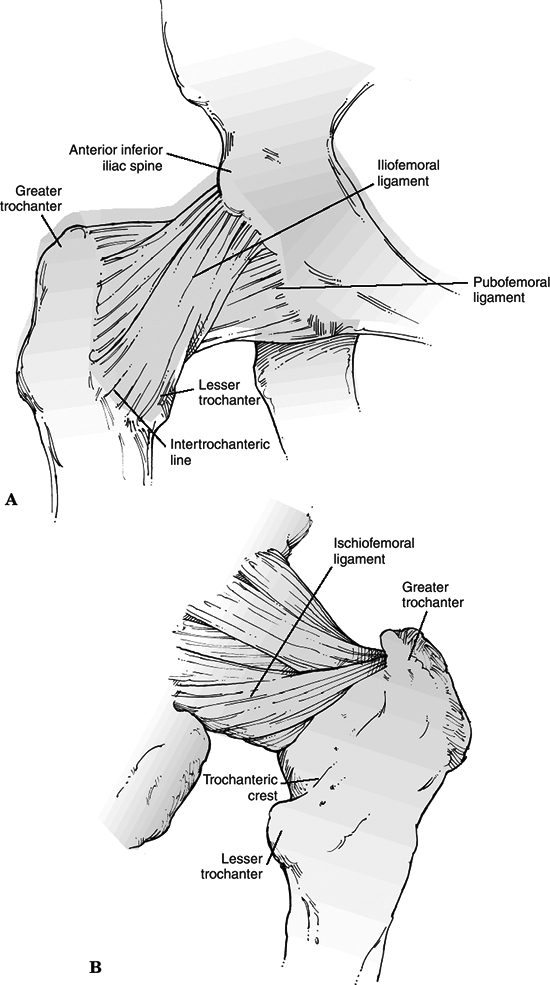
The hip joint capsule is formed by thick
longitudinal fibers supplemented by much stronger ligamentous
condensations (iliofemoral, pubofemoral, and ischiofemoral ligaments)
that run in a spiral fashion, preventing excessive hip extension (Fig. 27.2). -
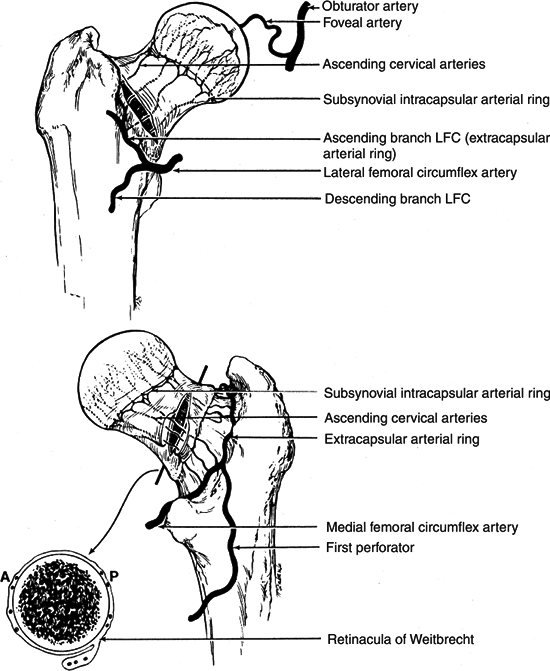
The main vascular supply to the femoral
head originates from the medial and lateral femoral circumflex
arteries, branches of the profunda femoral artery. An extracapsular
vascular ring is formed at the base of the femoral neck with ascending
cervical branches that pierce the hip joint at the level of the
capsular insertion. These branches ascend along the femoral neck and
enter the bone just inferior to the cartilage of the femoral head. The
artery of the ligamentum teres, a branch of the obturator artery, may
contribute blood supply to the epiphyseal region of the femoral head (Fig. 27.3). -
The sciatic nerve exits the pelvis at the
greater sciatic notch. A certain degree of variability exists in the
relationship of the nerve with the piriformis muscle and short external
rotators of the hip. Most frequently, the sciatic nerve exits the
pelvis deep to the muscle belly of the piriformis.
-
Hip dislocations almost always result
from high-energy trauma, such as motor vehicle accident, fall from a
height, or industrial accident. Force transmission to the hip joint
occurs with application to one of three common sources:-
The anterior surface of the flexed knee striking an object
-
The sole of the foot, with the ipsilateral knee extended
 Figure
Figure
27.1. Left: Sciatic nerve impingement by the posteriorly dislocated
femoral head. Right: Sciatic nerve impingement by a posterior
acetabular fracture fragment in a posterior fracturedislocation of the
hip.(From Rockwood CA Jr, Green DP, Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 4th ed, vol. 1. Philadelphia: Lippincott-Raven, 1996:1756 with permission.) -
The greater trochanter
P.303 -
-
Less frequently, the dislocating force
may be applied to the posterior pelvis with the ipsilateral foot or
knee acting as the counterforce. -
Direction of dislocation—anterior versus
posterior—is determined by the direction of the pathologic force and
the position of the lower extremity at the time of injury.
-
These comprise 10% to 15% of traumatic hip dislocations.
-
They result from external rotation and abduction of the hip.
-
The degree of hip flexion determines whether a superior or inferior type of anterior hip dislocation results:
-
Inferior (obturator) dislocation is the result of simultaneous abduction, external rotation, and hip flexion.
-
Superior (iliac or pubic) dislocation is the result of simultaneous abduction, external rotation, and hip extension.
-
-
They are much more frequent than anterior hip dislocations.
-
They result from trauma to the flexed knee (e.g., dashboard injury) with the hip in varying degrees of flexion:
-
If the hip is in the neutral or slightly
adducted position at the time of impact, a dislocation without
acetabular fracture will likely occur. -
If the hip is in slight abduction, an associated fracture of the posterior-superior rim of the acetabulum usually occurs.
-
 |
|
Figure 27.2. The hip capsule and its thickenings (ligaments) as visualized from anteriorly (A) and posteriorly (B).
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
 |
|
Figure
27.3. Vascular anatomy of the femoral head and neck. Top: Anterior aspect. Bottom: Posterior aspect. LFC, lateral femoral circumflex artery. (From Rockwood CA Jr, Green DP, Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 4th ed, vol. 2. Philadelphia: Lippincott-Raven, 1996:1662.)
|
-
Full trauma survey is essential because
of the high-energy nature of these injuries. Many patients are obtunded
or unconscious when they arrive in the emergency room as a result of
associated injuries. Concomitant intraabdominal, chest, and other
musculoskeletal injuries, such as acetabular, pelvic, or spine
fractures, are common. -
Patients presenting with dislocations of the hip typically are unable to move the lower extremity and are in severe discomfort.
-
The classic appearance of an individual
with a posterior hip dislocation is a patient in severe pain with the
hip in a position of flexion, internal rotation, and adduction.
Patients with an anterior dislocation hold the hip in marked external
rotation with
P.306
mild
flexion and abduction. The appearance and alignment of the extremity,
however, can be dramatically altered by ipsilateral extremity injuries. -
A careful neurovascular examination is
essential, because injury to the sciatic nerve or femoral neurovascular
structures may occur at time of dislocation. Sciatic nerve injury may
occur with stretching of the nerve over the posteriorly dislocated
femoral head. Posterior wall fragments from the acetabulum may also
pierce or partially lacerate the nerve. Usually, the peroneal portion
of the nerve is affected, with little if any dysfunction of the tibial
nerve. Rarely, injury to the femoral artery, vein, or nerve may occur
as a result of an anterior dislocation. Ipsilateral knee, patella, and
femur fractures are common. Pelvic fractures and spine injuries may
also be seen.
-
An anteroposterior (AP) radiograph of the pelvis is essential, as well as a cross-table lateral view of the affected hip.
-
On the AP view of the pelvis:
-
The femoral heads should appear similar
in size, and the joint spaces should be symmetric throughout. In
posterior dislocations, the affected femoral head will appear smaller
than the normal femoral head. In anterior dislocation, the femoral head
will appear slightly larger than the normal hip because of
magnification of the femoral head to the x-ray cassette. -
The Shenton line should be smooth and continuous.
-
The relative appearance of the greater
and lesser trochanters may indicate pathologic internal or external
rotation of the hip. The adducted or abducted position of the femoral
shaft should also be noted. -
One must evaluate the femoral neck to rule out the presence of a femoral neck fracture before any manipulative reduction.
-
-
A cross-table lateral view of the affected hip may help distinguish a posterior from an anterior dislocation.
-
Use of 45-degree oblique (Judet) views of
the hip may be helpful to ascertain the presence of osteochondral
fragments, the integrity of the acetabulum, and the congruence of the
joint spaces. Femoral head depressions and fractures may also be seen. -
Computed tomography (CT) scans are
usually obtained following closed reduction of a dislocated hip. If
closed reduction is not possible and an open reduction is planned, a
computed tomography scan should be obtained to detect the presence of
intra-articular fragments and to rule out associated femoral head and
acetabular fractures. -
The role of magnetic resonance imaging in
the evaluation of hip dislocations has not been established; it may
prove useful in the evaluation of the integrity of the labrum and the
vascularity of the femoral head.
relationship of the femoral head to the acetabulum and (2) whether or
not associated fractures are present.
 |
|
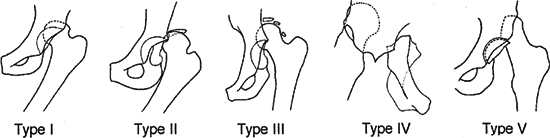
Figure 27.4. Thompson and Epstein classification of posterior hip dislocations.
|
| Type I: | Simple dislocation with or without an insignificant posterior wall fragment |
| Type II: | Dislocation associated with a single large posterior wall fragment |
| Type III: | Dislocation with a comminuted posterior wall fragment |
| Type IV: | Dislocation with fracture of the acetabular floor |
| Type V: | Dislocation with fracture of the femoral head |
| Type I: | Superior dislocations, including pubic and subspinous |
| IA: | No associated fractures |
| IB: | Associated fracture or impaction of the femoral head |
| IC: | Associated fracture of the acetabulum |
| Type II: | Inferior dislocations, including obturator, and perineal |
| IIA: | No associated fractures |
| IIB: | Associated fracture or impaction of the femoral head |
| IIC: | Associated fracture of the acetabulum |
-
One should reduce the hip on an emergency
basis to decrease the risk of osteonecrosis of the femoral head; it
remains controversial whether this should be accomplished by closed or
P.308
open
methods. Most authors recommend an immediate attempt at a closed
reduction, although some believe that all fracture-dislocations should
have immediate open surgery to remove fragments from the joint and to
reconstruct fractures.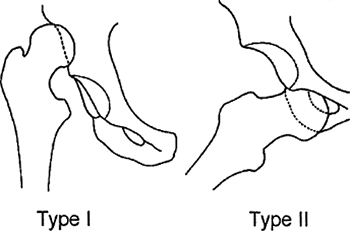 Figure 27.5. Epstein classification of anterior hip dislocations.(From Rockwood CA Jr, Green DP, eds. Rockwood and Green’s Fractures in Adults, 3rd ed. Philadelphia: Lippincott-Raven, 1996:1576–1579.)
Figure 27.5. Epstein classification of anterior hip dislocations.(From Rockwood CA Jr, Green DP, eds. Rockwood and Green’s Fractures in Adults, 3rd ed. Philadelphia: Lippincott-Raven, 1996:1576–1579.) -
The long-term prognosis worsens if
reduction (closed or open) is delayed more than 12 hours. Associated
acetabular or femoral head fractures can be treated in the subacute
phase.
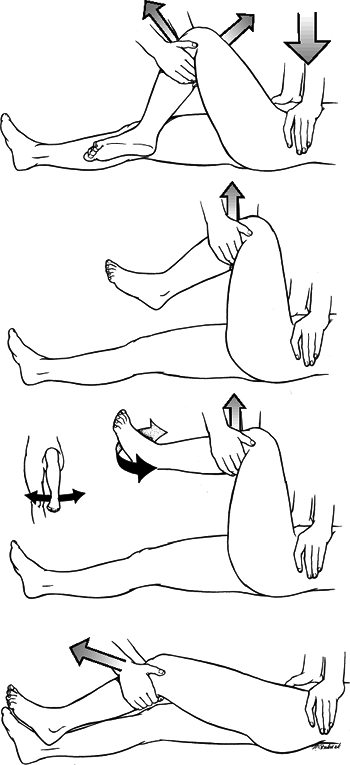
reduction can be attempted with in-line traction with the patient lying
supine. The preferred method is to perform a closed reduction using
general anesthesia, but if this is not feasible, reduction under
intravenous sedation is possible. There are three popular methods of
achieving closed reduction of the hip:
deformity. The patient is placed supine with the surgeon standing above
the patient on the stretcher. Initially, the surgeon applies in-line
traction while the assistant applies countertraction by stabilizing the
patient’s pelvis. While increasing the traction force, the surgeon
should slowly increase the degree of flexion to approximately 70
degrees. Gentle rotational motions of the hip as well as slight
adduction will often help the femoral head to clear the lip of the
acetabulum. A lateral force to the proximal thigh may assist in
reduction. An audible “clunk” is a sign of a successful closed
reduction (Fig. 27.6).
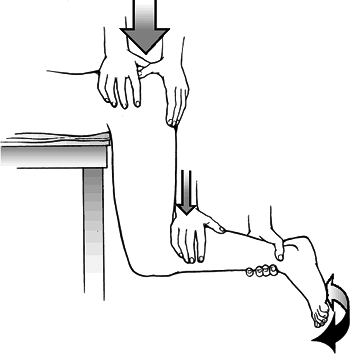
affected leg hanging off the side of the stretcher. This brings the
extremity into a position of hip flexion and knee flexion of 90 degrees
each. In this position, the assistant immobilizes the pelvis, and the
surgeon applies an anteriorly directed force on the proximal calf.
Gentle rotation of the limb may assist in reduction (Fig. 27.7).
fractures and are not as frequently used as reduction techniques. In
the Bigelow maneuver, the patient is supine, and the surgeon applies
longitudinal traction on the limb. The adducted and internally rotated
thigh is then flexed at least 90 degrees. The femoral head is then
levered into the acetabulum by abduction, external rotation, and
extension of the hip. In the reverse Bigelow maneuver, used for
anterior dislocations, traction is again applied in the line of the
deformity. The hip is then adducted, sharply internally rotated, and
extended.
-
Following closed reduction, radiographs
should be obtained to confirm the adequacy of reduction. The hip should
be examined for stability while the patient is still sedated or under
anesthesia. If there is an obvious large displaced acetabular fracture,
the stability examination need not be performed.-
Stability is checked by flexing the hip
to 90 degrees in neutral position. A posteriorly directed force is then
applied. If any sensation of subluxation is detected, the patient will
require additional diagnostic studies and possibly surgical exploration
or traction.![]() Figure 27.6. The Allis reduction technique for posterior hip dislocations.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 27.6. The Allis reduction technique for posterior hip dislocations.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Following successful closed reduction and completion of the stability examination, the patient should undergo CT evaluation.
P.309P.310 -
 |
|
Figure 27.7. The Stimson gravity method of reduction
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
Indications for open reduction of a dislocated hip include:
-
Dislocation irreducible by closed means.
-
Nonconcentric reduction.
-
Fracture of the acetabulum or femoral head requiring excision or open reduction and internal fixation.
-
Ipsilateral femoral neck fracture.
-
-
A standard posterior approach
(Kocher-Langenbeck) will allow exploration of the sciatic nerve,
removal of posteriorly incarcerated fragments, treatment of major
posterior labral disruptions or instability, and repair of posterior
acetabular fractures. -
An anterior (Smith-Peterson) approach is
recommended for isolated femoral head fractures. A concern when using
an anterior approach for a posterior dislocation is the possibility of
complete vascular disruption. By avoiding removal of the capsule from
the femoral neck and trochanters (i.e., taking down the capsule from
the acetabular side), injury to the lateral circumflex artery or its
branches should not occur. -
An anterolateral (Watson-Jones) approach
is useful for most anterior dislocations and combined fracture of both
femoral head and neck. -
A direct lateral (Hardinge) approach will allow exposure anteriorly and posteriorly through the same incision.
-
In the case of an ipsilateral displaced or nondisplaced femoral neck fracture, closed reduction of the hip should not be
P.311
attempted. The hip fracture should be provisionally stabilized through
a lateral approach. A gentle reduction is then performed, followed by
definitive fixation of the femoral neck. -
Management after closed or open reduction
ranges from short periods of bed rest to various durations of skeletal
traction. No correlation exists between early weight bearing and
osteonecrosis. Therefore, partial weight bearing is advised.-
If reduction is concentric and stable: A short period of bed rest is followed by protected weight bearing for 4 to 6 weeks.
-
If reduction is concentric but unstable: Skeletal traction for 4 to 6 weeks is followed by protective weight bearing.
-
-
The outcome following hip dislocation ranges from an essentially normal hip to a severely painful and degenerated joint.
-
Most authors report a 70% to 80% good or
excellent outcome in simple posterior dislocations. When posterior
dislocations are associated with a femoral head or acetabular fracture,
however, the associated fractures generally dictate the outcome. -
Anterior dislocations of the hip are
noted to have a higher incidence of associated femoral head injuries
(transchondral or indentation types). The only patients with excellent
results in most authors’ series are those without an associated femoral
head injury.
-
Osteonecrosis: This is observed in 5% to
40% of injuries, with increased risk associated with increased duration
of dislocation (>6 to 24 hours); however, some authors suggest that
osteonecrosis may result from the initial injury and not from prolonged
dislocation. Osteonecrosis may become clinically apparent up to 5 years
after injury. Repeated reduction attempts may also increase its
incidence. -
Posttraumatic osteoarthritis: This is the
most frequent long-term complication of hip dislocations; the incidence
is dramatically higher when dislocations are associated with acetabular
fractures or transchondral fractures of the femoral head. -
Recurrent dislocation: This is rare
(<2%), although patients with decreased femoral anteversion may
sustain a recurrent posterior dislocation, whereas those with increased
femoral anteversion may be prone to recurrent anterior dislocations. -
Neurovascular injury: Sciatic nerve
injury occurs in 10% to 20% of hip dislocations. It is usually caused
by a stretching of the nerve from a posteriorly dislocated head or from
a displaced fracture fragment. Prognosis is unpredictable, but most
authors report 40% to 50% full recovery. Electromyographic studies are
indicated at 3 to 4 weeks for baseline information and prognostic
guidance. If no clinical or electrical improvement is seen by 1 year,
surgical intervention may be considered. If a sciatic nerve injury
occurs after closed reduction is performed, then entrapment of the
nerve is likely and surgical exploration is indicated. Injury to the
femoral nerve and femoral vascular structures has been reported with
anterior dislocations. -
Femoral head fractures: These occur in
10% of posterior dislocations (shear fractures) and in 25% to 75% of
anterior dislocations (indentation fractures). -
Heterotopic ossification: This occurs in
2% of patients and is related to the initial muscular damage and
hematoma formation. Surgery increases its incidence. Prophylaxis
choices include indomethacin for 6 weeks or use of radiation. -
Thromboembolism: This may occur after hip
dislocation owing to traction-induced intimal injury to the
vasculature. Patients should be given adequate prophylaxis consisting
of compression stockings, sequential compression devices, and
chemoprophylaxis, particularly if they are placed in traction.