Hip Arthroplasty for Intertrochanteric Hip Fractures
treated with internal fixation heal. However, certain unfavorable
fractures patterns, fractures in patients with severely osteopenic
bone, or patients with poor hardware placement, can lead to internal
fixation failure (nonunion). Randomized prospective studies of
displaced femoral-neck fractures in elderly osteoporotic patients have
shown a high complication rate associated with internal fixation of
these injuries. For this reason, most surgeons favor arthroplasty,
which has a documented excellent success rate and offers the advantage
of early weight bearing. This has led some surgeons to consider the use
of a prosthesis in the management of selected, osteoporotic,
intertrochanteric, hip fractures. In theory, this may allow earlier
mobilization and minimize the chance of internal fixation failure and
need for re-operation. The use of arthroplasty in this setting,
however, poses its own unique challenges including the need for
so-called “calcar replacing” prostheses and it raises questions
regarding the need for acetabular resurfacing and the management of the
often-fractured greater trochanteric fragment. The purpose of this
chapter is to review the indications, surgical techniques, and specific
technical details needed to achieve a successful outcome. Also
addressed are the potential complications of hip arthroplasty for
fractures of the intertrochanteric region of the femur.
whether stable or unstable, will heal uneventfully with accurately
placed internal-fixation devices. When the procedure is done correctly,
the fixation failure rate should be minimal. European studies have
found that hip arthroplasty can lead to successful outcomes; however,
there is a higher perioperative mortality rate among these patients
compared to those who undergo internal fixation. Therefore, the
indications for hip arthroplasty for peritrochanteric fractures include
patients with neglected intertrochanteric fractures when attempts at
open reduction and internal fixation (ORIF) are unlikely to succeed;
pathologic fractures due to neoplasm; internal
fixation
failures or established nonunions where the patient’s age and remaining
proximal-bone stock precludes a revision internal-fixation attempt;
(very rarely) in patients with severe preexisting, symptomatic
osteoarthritis of the hip; and an unstable fracture pattern. Recent
studies have documented that hip arthroplasty for salvage of failed
internal fixation provides predictable pain relief and functional
improvement.
with multiple medical co-morbidities, a thorough medical evaluation is
recommended. Preoperative correction of dehydration, electrolyte
imbalances, and anemia is important. In general, surgery is performed
within 48 hours of injury to avoid prolonged recumbency.
the hip, femur, and pelvis are important for preoperative planning. If
the surgeon has any concern of a pathologic fracture, computed
tomography (CT) or magnetic resonance imaging (MRI) scanning can
occasionally be helpful. If a pathologic fracture due to metastasis is
diagnosed, full-length femur radiographs are even more critical in
evaluating any distal lesions that would need to be addressed.
Appropriate imaging of the proximal fragment is important to allow
templating of the femoral component for length or offset and to
determine whether any proximal calcar augmentation will be necessary to
restore the normal neck-shaft relationship. Careful scrutiny of the hip
joint is necessary to detect evidence of acetabular degenerative change
that would make total hip arthroplasty more attractive than
hemi-arthroplasty. A final decision is often made intraoperatively
after visual inspection of the quality of the remaining acetabular
cartilage. If previous hardware from internal fixation is present,
specific screwdrivers and a broken screw removal set, with or without
the use of fluoroscopy, may assist the surgeon in hardware removal. It
is wise to have implant-specific extraction tools available. Obtaining
the original operative note can assist the surgeon in determining the
implant manufacturer if it is not recognized from the radiographs.
whether hemi-arthroplasty or total hip arthroplasty is appropriate, and
whether cemented or uncemented femoral component fixation is indicated.
I prefer to have both acetabular resurfacing and femoral-component
fixation options available intraoperatively. Although having such a
large inventory of implants available for a single case is laborious,
it is wise to be prepared for the unexpected situations that can be
found during these challenging reconstructions.
internal fixation, I recommend that a complete blood count with
differential, a sedimentation rate, and a C-reactive protein be
obtained preoperatively. I have not found aspiration to be predictable
in the setting of fixation failure and rely on preoperative serologies
and intraoperative frozen-section histology for decision making.
on whether the reason for performing the arthroplasty is an acute
fracture, a neglected fracture, a pathologic fracture, or a nonunion
with failed hardware. However, many surgical principles are commonplace
regardless of the preoperative diagnosis.
on the operating room table, and an intravenous antibiotic, typically a
first-generation cephalosporin, is given. Careful padding of the down
axilla, peroneal nerve area, and ankle can minimize the chance of a
neurological or skin pressure problem due to positioning. A stable
horizontal position can guide the surgeon to appropriate pelvic
positioning, which will facilitate proper acetabular-component
implantation. Several commercially available hip positioners are
available to simplify accurate and stable pelvic positioning.
Consideration should be given to the use of intraoperative blood
salvage (cell saver), as these surgeries can be long and bloody.
if possible, the previous incisions are used. If no previous incision
is present, then a simple curvilinear incision centered on the greater
trochanter will suffice. The fascia is incised in line with the skin
incision and the status of the greater trochanter is evaluated. If the
greater trochanter is not fractured, either an anterolateral or
posterolateral approach can be used effectively based on surgeon
preference. In the acute fracture situation it is always preferable, if
possible, to leave the abductor–greater trochanter–vastus lateralis
complex intact and immobilized in a long sleeve as much as possible
during the reconstruction.
be malunited and preclude access to the intramedullary canal. In this
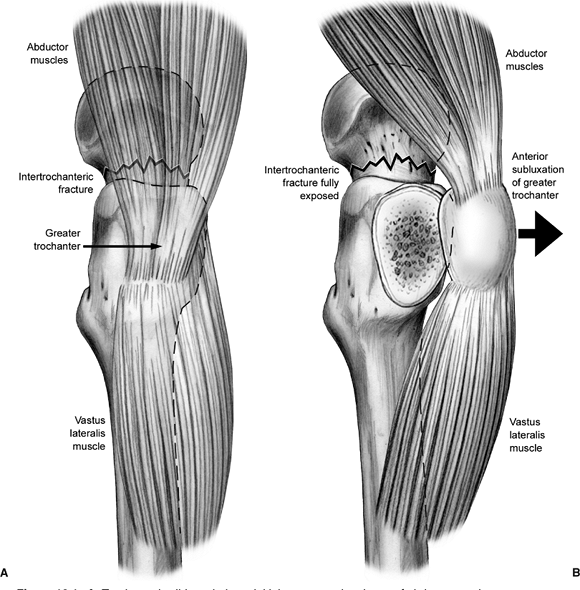
situation the so-called “trochanteric slide” technique may be useful (Fig. 18.1).
This technique of preserving the vastus-trochanter-abductor sleeve may
minimize the chance of so-called “trochanteric escape” and should be
used whenever possible.
 |
|
Figure 18.1. A. Trochanteric slide technique, initial exposure: the sleeve of abductors and vastus lateralis are in continuity. B.
Trochanteric slide technique, deep exposure. Note continuity of the musculotendinous sleeve with mobilization of the greater trochanter. |
to dislocate the hip prior to hardware removal. The torsional stresses
on the femur during surgical dislocation can be large, especially in
these typically stiff hips, and iatrogenic femur fracture can occur
with attempted hip dislocation. If previous surgery has been performed,
I prefer to obtain intraoperative cultures and frozen section
pathology. If there is evidence of acute inflammation or other gross
clinical evidence of infection, then I recommend removal of all
hardware, careful debridement of all tissues, and resection of the
proximal femoral-head fragment with placement of an antibiotic
impregnated polymethacrylate spacer. The reconstruction is then
performed in a delayed fashion after a period of organism-specific
intravenous antibiotics based on the sensitivities obtained from deep
intraoperative cultures.
posteriorly, depending upon surgeon preference and the status of the
abductor mechanism. The proximal fragment is excised, and the
acetabulum is circumferentially exposed. The quality of the remaining
acetabular cartilage is evaluated. If the cartilage is in reasonable
condition, then a hemi-arthroplasty can be used with good results.
Appropriate attention to head size with hemi-arthroplasty is important
as an undersized component can lead to medial loading, instability, and
pain, while an oversized component can lead to peripheral loading,
instability, and pain as well. If preexisting degenerative change or
the acetabular cartilage damaged is noted from prior hardware cutout, a
total hip replacement is preferable. Of course, even in the setting of
normal-appearing acetabular cartilage, an acetabular component may
provide more predictable pain relief, and this decision should be at
the surgeon’s discretion. The acetabulum is reamed carefully because
these hips do not have the thick, sclerotic subchondral bone commonly
found in patients with degenerative joint disease. The acetabulum is
reamed circumferentially until a bleeding bed is obtained. Either
cemented or uncemented acetabular component fixation can be used with
good results. I prefer uncemented acetabular fixation due to the
versatility it allows with multiple liner, bearing surface, and head
size options; I also typically augment initial cup fixation with screws.
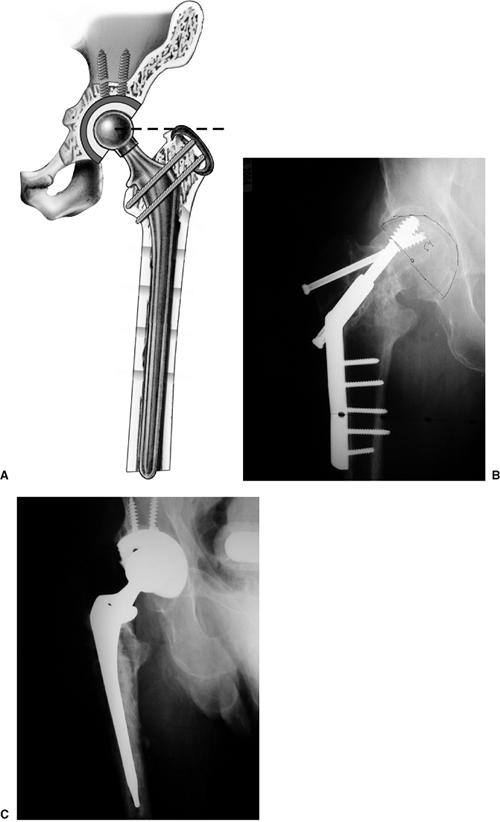
emphasized that the femoral side of the reconstruction is typically
more challenging in this setting. The general principles of femoral
reconstruction are summarized diagrammatically in Figure 18.2.
It is important to carefully evaluate the level of bony deficiency
medially. Typically, bone loss from the fracture or a nonunion results
in a bony deficiency well below the standard resection level for a
primary total-hip arthroplasty. Therefore, a calcar prosthesis is
usually necessary to restore leg length and hip stability. Femoral
components with modular calcar augmentations are available and allow
intraoperative flexibility in restoring the hip center. A large
posteromedial fragment may be reduced and stabilized with cerclage
wires or cables, which will help the surgeon judge appropriate femoral
component seating height. In the acute fracture situation, reduction by
wire or cable can potentially result in bony healing, thereby restoring
medial bone stock.
and so forth can alter the morphology of the proximal femur. These
alterations can deflect reamers and broaches leading to intraoperative
fracture or femoral perforation. I have found it useful to use a large
diameter burr to provisionally shape the funnel of the proximal femur.
Once these sclerotic areas have been opened, standard reamers and
broaches can be used to prepare the canal more safely.
recommended that a stem length is chosen that bypasses the most distal
stress riser (i.e., screw hole) in the shaft by at least two cortical
(diaphyseal) diameters. Because most adult femoral shafts are
approximately 30 mm in diameter, templating for 6 cm of bypass is a
good general guideline for stem length. Either cemented or uncemented
femoral-component fixation can be effective in this type of
reconstruction and is, of course, based on surgeon preference and
assessment of the intraoperative bone quality. If an uncemented femoral
component is chosen, it is wise to select an extensively coated design
that can achieve distal diaphyseal fixation. This strategy will allow
the surgeon to bypass stress risers effectively and not rely on
proximal boney support for implant stability. Cemented fixation may be
advantageous for elderly patients with capacious, osteopenic femoral
canals. Regardless of whether cemented or uncemented
fixation
is used intraoperatively, radiographs are recommended to assure
appropriate alignment and bypass of previous stress risers and to rule
out iatrogenic fracture or extravasation of cement. Extravasated cement
can be a cause of late periprosthetic fracture, and it is recommended
that careful removal of extravasated cement be performed. Small,
medial, screw-hole extravasations can typically be ignored as long as
they are bypassed sufficiently by the femoral component.
 |
|
Figure 18.2. A.
Illustration summarizing the general principles of femoral reconstruction for intertrochanteric fracture or salvage of failed internal fixation. Note the restoration of appropriate femoral-component height using a calcar-replacing stem. Referencing the tip of the greater trochanter as a guide to restoring the center of rotation. Secure fixation of the greater trochanter has been obtained as is typical: with a cable through and a cable below the lesser trochanter. Note the stem length chosen to bypass all cortical stress risers by a minimum of two diaphyseal diameters. B. Preoperative nonunion and hardware cutout after ORIF of an intertrochanteric fracture. Note the acetabular erosion superiorly from the lag screw. C. Postoperative reconstruction with a total hip arthroplasty with particulate bone grafting of the superior acetabular cavitary defect. |
reconstruction is the relationship between the center of the femoral
head and the tip of the greater trochanter: It should be essentially
coplanar. Although this may be difficult to assess in the presence of a
trochanteric fracture, usually, the greater trochanteric fragments are
still somewhat attached and can be used as a gross guide for evaluating
the appropriate level of calcar buildup. Trial reduction is performed,
and leg lengths and hip stability are assessed. Again, intraoperative
radiographs should be obtained. The author typically obtains an
intraoperative radiograph after the real acetabular component and the
trial femoral component are in place, and then once again after all of
the real components are implanted and greater trochanteric fragment
fixation, if necessary, is complete.
wise to use autogenous bone graft obtained from the resected
femoral-head fragment to fill any lateral cortical defects from prior
hardware as well as the interface with the greater trochanter and the
femoral shaft, if necessary. Countless methods of greater trochanteric
fixation have been described elsewhere in the literature, with mixed
results. In general, the use of multiple wires or a cable claw
technique is preferred. Regardless of the method chosen, the greater
trochanteric fixation should be stable through a full range of motion
of the hip. The fascia, subcutaneum, and the skin are closed per
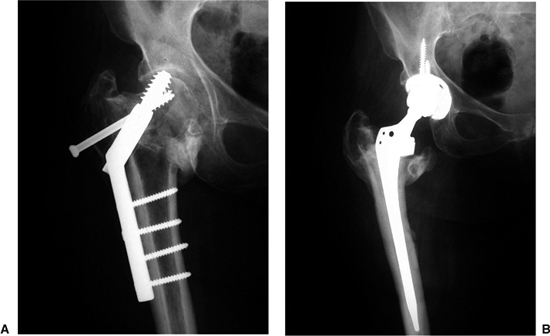
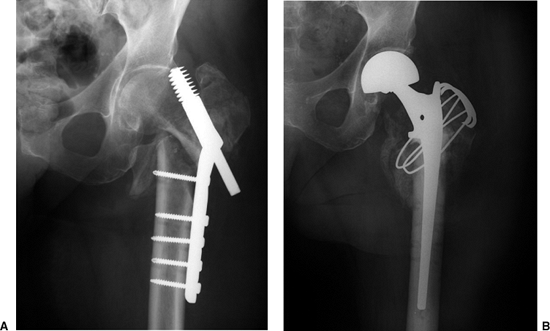
surgeon preference. Representative cases emphasizing these principles
are shown in Figures 18.2, 18.3, 18.4, and 18.5.
 |
|
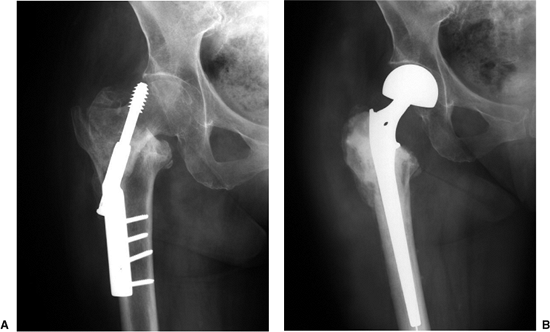
Figure 18.3. A. Preoperative failed ORIF with proximal fragment translation and screw cutout. B.
Postoperative reconstruction with a total hip arthroplasty with calcar augmentation to restore appropriate femoral-component height, thereby restoring leg length and hip stability. |
 |
|
Figure 18.4. A.
Preoperative failed ORIF of a reverse obliquity fracture. Note the difficulty in managing the greater trochanter in this situation. B. Postoperative reconstruction with calcar-replacing bipolar hemi-arthroplasty through a trochanteric slide technique. |
 |
|
Figure 18.5. A. Preoperative failed ORIF with screw cutout. The acetabular joint space is well preserved. B. Postoperative radiograph demonstrating a cemented calcar-replacing bipolar hemi-arthroplasty.
|
after surgery; however, the surgeon should individualize the
rehabilitation regimen based on patient compliance quality of
intraoperative component-fixation achieved, and most importantly, the
status of the greater trochanter. If trochanteric fixation was
required, the selective use of an abduction orthosis, partial weight
bearing for 6 weeks, and avoidance of abductor strengthening until
trochanteric union has occurred are recommended. Sutures are typically
removed at 2 weeks and periodic radiographs are obtained to evaluate
component fixation and trochanteric healing status. Clinical and
radiographic follow-up is typically performed at the discretion of the
treating surgeon; for younger patients, follow-up visits are preferred
at 6 weeks, 12 weeks, and 1, 2, and 5 years postoperatively, then every
2 years thereafter. For asymptomatic elderly patients with
transportation difficulties, of course, the follow up periods are
typically modified to 6 weeks, 3 months, one year, then every 5 years
thereafter.
intertrochanteric fracture in the literature. They generally document
the efficacy of arthroplasty as an alternative treatment for the acute
fracture; however, complications still remain concerning. Most reports
regard salvage of failed internal fixation. Haidukewych and Berry
reported on 60 patients undergoing hip arthroplasty for salvage of
failed ORIF. Overall, functional status improved in all patients, and
the 7 year survivorship free of revision was 100%. Pain relief was
predictable. Dislocation was not problematic; however, persistent
trochanteric complaints and problems obtaining bony trochanteric union
were common. Both bipolar and total hip arthroplasties performed well.
Calcar-replacing designs and long stem prostheses were necessary in the
majority of cases.
older patients undergoing these surgeries. Thromboembolic prophylaxis,
perioperative antibiotics, and early mobilization are recommended. If a
long-stem cemented implant is used, intraoperative embolization and
cardiopulmonary complications can occur. It is important to lavage and
dry the canal thoroughly prior to cementing in these frail patients,
and little, if any, pressurization should be used. Infection and
dislocation are surprisingly rare after such reconstructions in which
modern techniques and implants are used. Dislocations are managed with
closed reduction and bracing as long as the trochanteric fragment
fixation remains secure.
pain, and nonunion are the most common complications after these
reconstructions. Patients should be counseled preoperatively that such
chronic complaints are very common. Bony union will occur in most but
not all trochanteric fragments. Stable trochanteric fibrous unions in
good position will often be asymptomatic and not require treatment.
Displaced trochanteric escape, if symptomatic, is typically treated
with a repeat internal fixation attempt with some form of bone
grafting. The best treatment is prevention, with extremely secure
initial trochanteric fixation, the use of the trochanteric slide
technique if mobilization of the trochanter is required, liberal use of
autograft bone at the trochanter-femur interface, and careful
postoperative rehabilitation.
armamentarium of the surgeon treating intertrochanteric hip fractures.
In general, it is reserved for neglected fractures, pathologic
fractures due to neoplasm, salvage of internal fixation failure and
nonunion, and (rarely) for fracture in patients with severe,
symptomatic, preexisting degenerative change. Attention
to
specific technical details is important to avoid complications and
provide a durable reconstruction. Trochanteric complications are
common, but functional improvement and pain relief are predictable.
S, Moore T, Proano F. Bipolar prosthetic replacement for the management
of unstable intertrochanteric hip fractures in the elderly. Clin Orthop 1987;224:169–170.
P, Casteleyn PP, DeBoerk H, et al. Treatment of unstable
intertrochanteric and subtrochanteric fractures in elderly patients:
primary bipolar arthroplasty compared with ORIF. J Bone Joint Surg 1989;71(8):1214–1225.
P, Casteleyn PP, Opdecam P. Primary bipolar arthroplasty or total hip
arthroplasty for the treatment of unstable intertrochanteric or
subtrochanteric fractures in elderly patients. Acta Orthop Belg 1994:60:124–128.
P, Casteleyn PP, Opdecan P. Hip arthroplasty for failed internal
fixation of intertrochanteric and subtrochanteric fractures in the
elderly patient. Arch Orthop Trauma Surg 1994;113:222–227.
SF, Stern RE, Kulich RG. Primary Bateman-Leinbach bipolar prosthetic
replacement of the hip in the treatment of unstable intertrochanteric
fractures in the elderly. Orthopedics October 1990;13:1131–1136.
Y-H, Oh J-H, Koh Y-G. Salvage of neglected unstable intertrochanteric
fractures with cementless porous-coated hemiarthroplasty. Clin Orthop 1992;277:182–187.
EM, Rand JA. Nonunion of intertrochanteric fractures of the femur
following open reduction and internal fixation: results of second
attempts to gain union. Clin Orthop 1987;218:81–89.
D, Haentjens P, Reynders P, et al. Hip arthroplasty for failed internal
fixation of intertrochanteric and subtrochanteric fractures in the
elderly patient. Acta Orthop Belg 1994;60:135–139.
