Hand and Wrist
Editors: Berquist, Thomas H.
Title: Musculoskeletal Imaging Companion, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Chapter 9 – Hand and Wrist
Chapter 9
Hand and Wrist
Thomas H. Berquist
Protocols
-
Routine radiographs
-
Hand: posteroanterior (PA), lateral, oblique views
-
Wrist: PA, lateral, scaphoid views
-
Wrist motion (instability) series: PA
views with radial deviation, ulnar deviation, and clenched fist;
lateral views with dorsal and palmar flexion
-
-
Computed tomography (CT)
-
Two- to 3-mm axial and direct coronal or
sagittal images for conventional studies. Axial images at 1- and 0.5-mm
intervals for coronal and sagittal reformatting or three-dimensional
reconstruction.
-
-
Magnetic resonance imaging (MRI)
-
Field of view: 8 to 12 cm
-
Coil: wrist coil or flat 5-inch coil (motion studies)
-
Patient position: arm at side when possible; otherwise, arm above head (Table 9-1)
-
P.564
Suggested Reading
Berquist TH. MRI of the musculoskeletal system. Philadelphia: Lippincott Williams & Wilkins; 2006:719–801.
Schweitzer
ME, Natale P, Winalski CS, et al. Indirect wrist MR arthrography: The
effects of passive motion versus active exercise. Skel Radiol 2000;29:10–14.
ME, Natale P, Winalski CS, et al. Indirect wrist MR arthrography: The
effects of passive motion versus active exercise. Skel Radiol 2000;29:10–14.
Truong NP, Mann FP, Gilula LA, et al. Wrist instability series: Increased yield with clinical-radiological screening criteria. Radiology 1994;192:481–484.
P.565
Fractures/Dislocations: Distal Radius/Ulnar Fractures—Colles Fracture
Key Facts
-
Fractures of the distal radius are
common. In elderly patients, osteopenia results in fracture from minor
trauma. In children, incomplete or physeal fractures are common.
Fractures of the ulna or ulnar styloid commonly occur with distal
radial fractures. -
Distal radial fractures have multiple
eponyms such as Colles, Smith, Barton, and Chauffeur’s fractures. Today
most are categorized by the extent of articular involvement. Type A
fractures are extra-articular, Type B fractures are partial articular,
and Type C fractures involve both the radiocarpal joints and distal
radioulnar joint (DRUJ). -
Colles fracture is a term applied to
fractures to distal radial, with or without articular involvement, and
dorsal displacement of the distal fragment. -
Mechanism of injury: fall on the outstretched hand.
-
Anteroposterior (AP) and lateral
radiographs are diagnostic. However, CT is often performed to
completely evaluate articular involvement. -
Treatment: traction to reduce and reachieve radial length and palmar tilt. Closed reduction usually is successful.
-
Complications: occur in up to 33% of patients and include
-
Compressive neuropathy
-
Arthrosis
-
Malunion
-
Tendon rupture
-
Ligament injuries
-
Ischemic contractures
-
P.566
 |
|
FIGURE 9-1 Lateral radiograph of the wrist demonstrating incomplete fractures of the ulna (arrowhead) and a torus (buckle) fracture of the radius (curved arrow).
|
P.567
 |
|
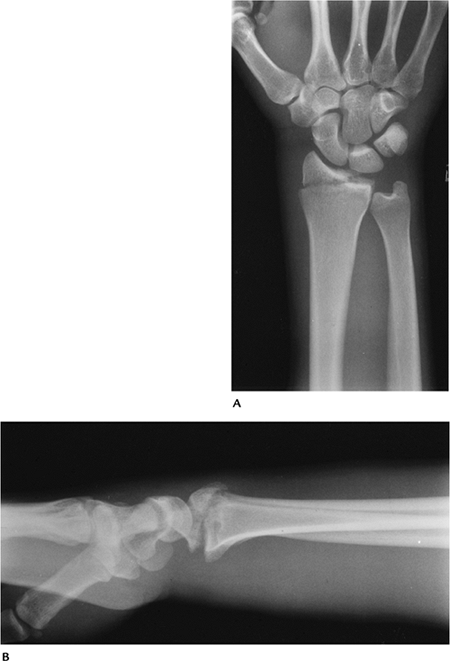
FIGURE 9-2
Lateral and PA radiographs of the wrist showing a typical Colles fracture with dorsal impaction of the radius and an ulnar styloid fracture. The fracture extends into the DRUJ (Type B). |
P.568
 |
|
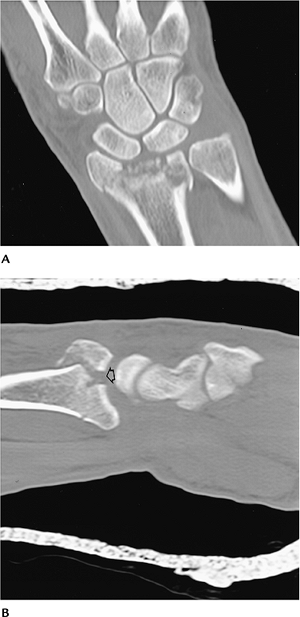
FIGURE 9-3 Coronal (A) and sagittal (B) CT images clearly demonstrate the fracture fragments and the extent of articular separation (open arrow in B).
|
P.569
 |
|
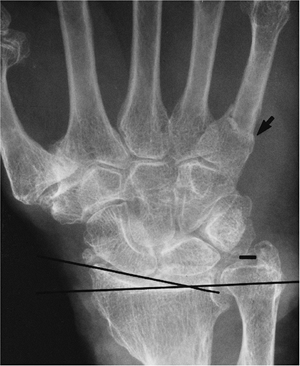
FIGURE 9-4 PA radiograph of an old Colles fracture with shortening of the radius and decreased radial inclination (lines). There is degenerative arthritis and an associated fifth metacarpal fracture (arrow).
|
Suggested Reading
Cooney WP, Dobyns JH, Linscheid RL. Complications of Colles’ fractures. J Bone Joint Surg 1980;62A:613–619.
Orthopedic Trauma Association Committee for Coding and Classification. Fracture and dislocation compendium. J Orthop Trauma 1996;10:26–30.
P.570
Fractures/Dislocations: Distal Radius/Ulnar Fractures—Smith Fracture
Key Facts
-
Smith fracture is a “reverse Colles fracture” with palmar displacement of the distal radial fragment.
-
Mechanism of injury: fall on a palmar flexed wrist.
-
Treatment: closed reduction; restore
radial length. Internal fixation may be required with significant
displacement or articular involvement. -
Complications: identical to Colles fracture complications.
 |
|
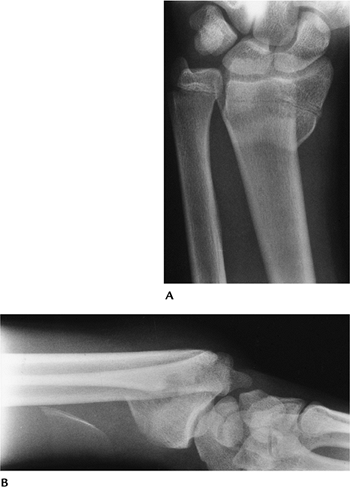
FIGURE 9-5 AP (A) and lateral (B) radiographs of a Smith fracture with palmar displacement of the distal radius.
|
Suggested Reading
Thomas FB. Reduction of Smith’s fracture. J Bone Joint Surg 1957;37B:463–470.
P.571
Fractures/Dislocations: Distal Radius/Ulnar Fractures—Barton Fracture
Key Facts
-
A Barton fracture is an intra-articular fracture of the radius involving the dorsal or volar lip of the radial styloid.
-
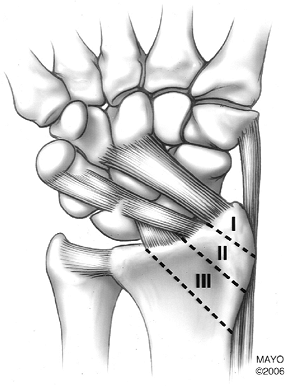
Radial styloid fractures are divided into
three zones. Zone I fractures may be stable without associated ligament
injuries. Zone II fractures commonly have associated ligament injury.
Zone III fractures are likely to have ligament injury and joint
incongruency (Fig. 9-6). -
Mechanism of injury: Palmar fractures
occur similar to Smith fractures. Dorsal fractures result from a fall
on the outstretched hand with the forearm pronated. -
Treatment: closed reduction unless the
articular surface cannot be restored. In the latter setting, internal
fixation may be required. -
Complications: similar to Colles fracture, except subluxation and arthrosis are more common.
 |
|
FIGURE 9-6
Zones of radial styloid (Barton fracture). Zone I: styloid tip, may be stable with no ligament injury. Zone II: possible ligament injury, may have articular deformity. Zone III: likely to have ligament injury and joint deformity. |
P.572
 |
|
FIGURE 9-7 Dorsal Barton fracture. AP (A) and lateral (B) radiographs of an intra-articular fracture of the lateral aspect of the radius.
|
P.573
Suggested Reading
DeOliveira JC. Barton’s fracture. J Bone Joint Surg 1973;55A:586–594.
Putnam MD. Radial styloid fractures. In: Blair WF, ed. Techniques in hand surgery. Baltimore: Williams and Wilkins; 1996:322–329.
P.574
Fractures/Dislocations: Distal Radius/Ulnar Fractures—Chauffeur’s Fracture
Key Facts
-
A Chauffeur’s fracture is an intra-articular fracture of the distal radius that predominately involves the radial styloid.
-
The fracture line typically enters the joint at the junction of the scaphoid and lunate fossae.
-
Mechanism of injury: axial compression
transmitted through the scaphoid. Decades ago, the injury was
associated with backfires resulting in the automobile starting crank
striking the wrist. -
AP and lateral radiographs are adequate for diagnosis.
-
Treatment: cast immobilization if minimally displaced. Percutaneous K-wires may be required to maintain reduction.
 |
|
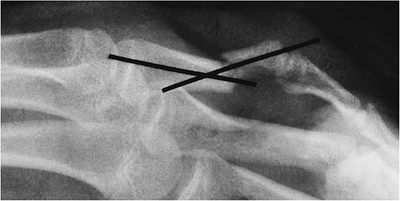
FIGURE 9-8 PA radiograph of a Chauffeur’s fracture during reduction with an external fixation.
|
P.575
Suggested Reading
Wood MB, Berquist TH. The hand and wrist. In: Berquist TH, ed. Imaging of orthopedic trauma, 2nd ed. New York: Raven Press; 1992:749–870.
P.576
Fractures/Dislocations: Galeazzi Fractures
Key Facts
-
The Galeazzi fracture is a fracture of
the distal radius, usually diaphysis, with associated subluxation or
dislocation of the DRUJ. -
Mechanism of injury: fall on the outstretched hand with hyperpronation of the forearm.
-
Treatment: reduction and internal fixation.
-
Routine radiographs are diagnostic.
-
Complications: malunion of the fracture and residual subluxation of the DRUJ.
 |
|
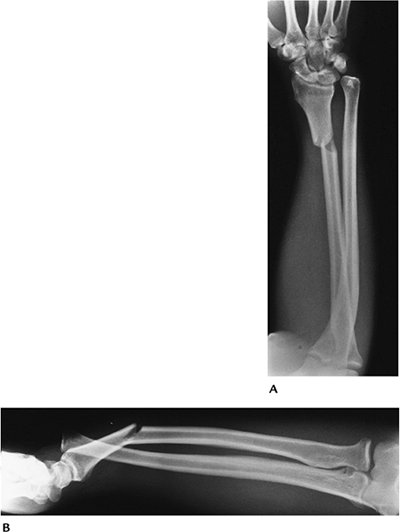
FIGURE 9-9 PA (A) and lateral (B) radiographs showing a distal radial fracture with dislocation of the DRUJ.
|
P.577
 |
|
FIGURE 9-10 PA radiograph after plate and screw fixation of the radial fracture and K-wire fixation of the joint.
|
Suggested Reading
Wood MB, Berquist TH. The hand and wrist. In: Berquist TH, ed. Imaging of orthopedic trauma, 2nd ed. New York: Raven Press; 1992:749–870.
P.578
Fractures/Dislocations: Distal Radioulnar Joint Subluxation/Dislocations
Key Facts
-
Subluxation or dislocation of the DRUJ may be dorsal (most common) or volar.
-
Mechanism of injury:
-
Dorsal—hyperpronation injury
-
Volar—hypersupination injury to the forearm
-
-
Routine radiographic findings may be
subtle. Axial CT or MRI with the wrist in pronation, neutral, and
supinated positions is most useful to confirm the diagnosis. -
Treatment: Closed reduction and cast
immobilization may be successful. Open repair may be best for long-term
results and optimal stability.
 |
|
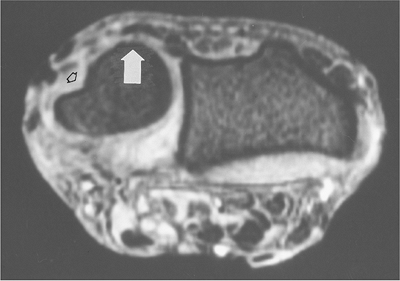
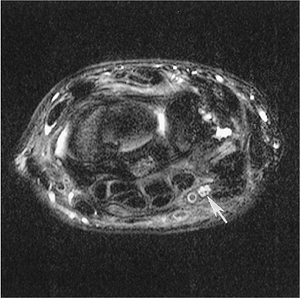
FIGURE 9-11 Axial fat-suppressed T2-weighted magnetic resonance (MR) image showing dorsal subluxation of the ulna (arrow) and absence of the extensor carpi ulnaris tendon (open arrow) as the result of a complete tear.
|
Suggested Reading
Hamlin C. Traumatic disruption of the distal radioulnar joint. Am J Sports Med 1977;5:93–96.
Nakamura R, Horie E, Imaeda T, et al. Criteria for diagnosing distal radioulnar joint subluxation by computed tomography. Skel Radiol 1996;25:649–653.
P.579
Fractures/Dislocations: Scaphoid Fractures
Key Facts
-
The scaphoid is the most commonly
fractured carpal bone in adults, accounting for 70% of all carpal
injuries. Scaphoid fractures in children account for only 2.9% of hand
and wrist fractures. -
Mechanism of injury: fall on the outstretched hand.
-
Scaphoid fractures may be difficult to detect and treat. Nonunion and avascular necrosis (AVN) are common complications.
-
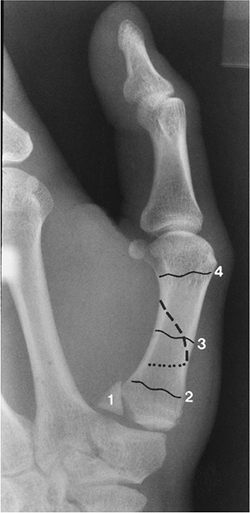
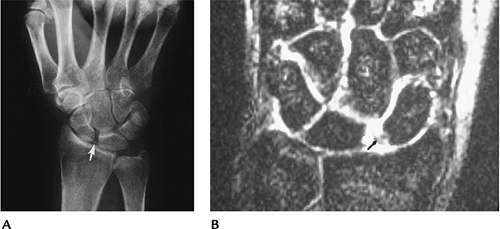
Scaphoid fractures are classified by
fracture location and orientation of the fracture line. Fractures may
involve the (1) tubercle, (2) distal articular surface, (3) fracture of
the distal third, (4) waist fracture, or (5) proximal pole fracture (Fig. 9-12). -
Imaging of scaphoid fractures requires
AP, lateral, and scaphoid views. Displacement or obliteration of the
navicular fat stripe is a useful sign for subtle fractures.
Radionuclide scans, MRI, or CT may be useful for detecting subtle
fractures and evaluating complications. -
Treatment: cast immobilization for
undisplaced fractures. Displaced fractures (>1 mm step-off or
angulation) are treated with internal fixation. -
Complications: delayed union (failure to
unite in 3 months), nonunion, malunion, AVN (most common with proximal
pole fractures), radioscaphoid impingement, and arthrosis.
P.580
 |
|
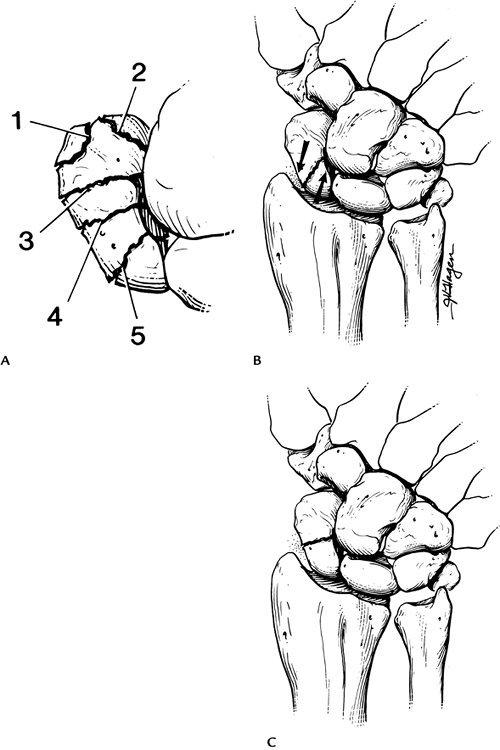
FIGURE 9-12 (A) Locations of scaphoid fractures: 1, tubercle; 2, distal articular surface; 3, distal third; 4, waist; 5, proximal pole. (B) Oblique fracture. Shearing forces (arrows) lead to instability and displacement. (C) Transverse waist fracture is more stable.
|
P.581
 |
|
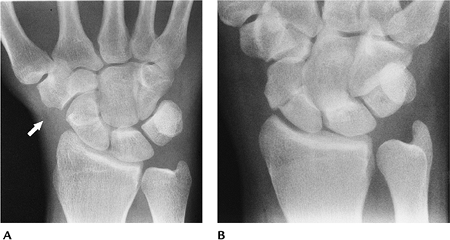
FIGURE 9-13 (A) Subtle scaphoid fracture with absent navicular fat stripe (arrow). (B) Displaced scaphoid waist fracture.
|
P.582
 |
|
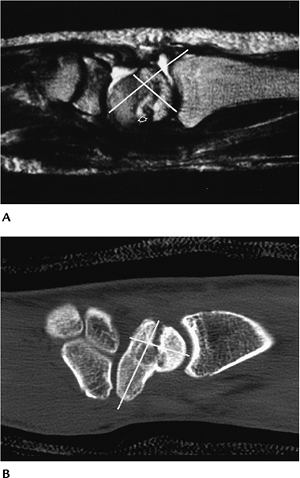
FIGURE 9-14 Humpback deformity. (A) Sagittal proton density-weighted MR image demonstrates fluid (open arrow) in the fracture line and deformity (white lines) caused by dorsal separation of the fracture’s fragments. (B) Sagittal reformatted CT image demonstrates a similar humpback deformity (lines) with sclerosis of the proximal fragment caused by AVN.
|
P.583
 |
|
FIGURE 9-15 Coronal T2-weighted MR image showing fluid (arrow) between the fragments caused by nonunion.
|
P.584
 |
|
FIGURE 9-16 PA view of a displaced scaphoid fracture with Herbert screw fixation. The proximal pole is sclerotic because of AVN.
|
Suggested Reading
Cooney WP III. Isolated carpal fractures. In: Cooney WP III, Linscheid RL, Dobyns JH, eds. The wrist: Diagnosis and operative treatment. St. Louis: Mosby; 1998:474–487.
Fisk GR. An overview of injuries of the wrist. Clin Orthop 1980;149:137–144.
P.585
Fractures/Dislocations: Other Carpal Fractures
Key Facts
-
Other carpal fractures occur less frequently than scaphoid fractures.
-
The triquetrum is the second most common carpal bone fractured followed by the capitate and lunate.
-
Mechanism of injury: fall on the outstretched hand; compressive or shearing forces.
-
Treatment: closed reduction and cast immobilization.
-
Imaging usually can be accomplished with
radiographs. The lateral view is most useful for triquetral fractures.
Subtle injuries may require CT or MRI. -
Complications: nonunion, arthrosis, carpal tunnel syndrome.
 |
|
FIGURE 9-17 PA and lateral views showing a triquetral fracture (arrow) seen only on the lateral radiograph.
|
 |
|
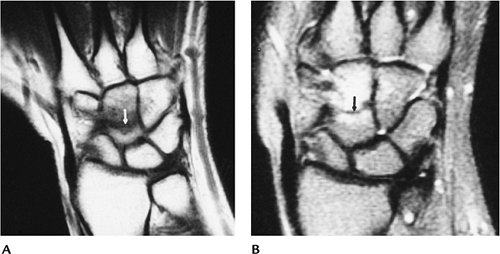
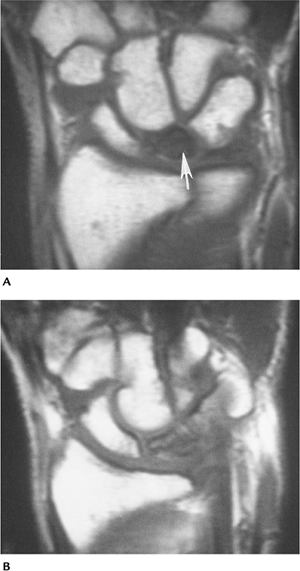
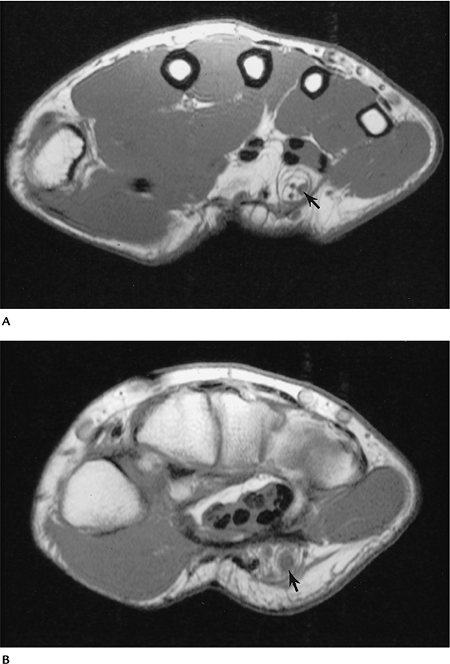
FIGURE 9-18 Coronal T1-weighted (A) and T2-weighted (B) images of a capitate fracture (arrow) with surrounding edema. Radiographs were normal.
|
 |
|
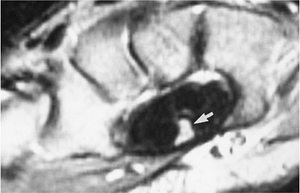
FIGURE 9-19 Sagittal T2-weighted fast spin-echo image with fat suppression demonstrating an undisplaced lunate fracture (arrow).
|
P.586
Suggested Reading
Berquist TH. Imaging of orthopedic trauma, 2nd ed. New York: Raven Press; 1992:749–870.
P.587
Fractures/Dislocations: Carpal and Carpometacarpal Dislocations
Key Facts
-
Dislocations of the carpus are most often associated with perilunate injury.
-
The transscaphoid perilunate dislocation
is most common. The proximal scaphoid maintains its lunate
relationship, and the distal scaphoid and remainder of the carpal bones
displace dorsally. -
Carpometacarpal dislocations are most often associated with distal carpal or metacarpal base fractures.
-
Mechanism of injury: fall on the outstretched hand.
-
Imaging may be accomplished with PA and
lateral radiographs. CT is best for subtle cases, evaluation of
osteochondral fractures, treatment planning, and postreduction
evaluation. -
Treatment: closed reduction if alignment can be restored; otherwise internal fixation.
-
Complications: arthrosis, AVN, instability.
P.588
 |
|
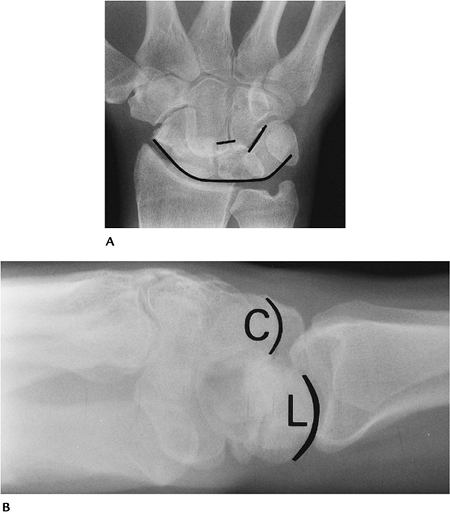
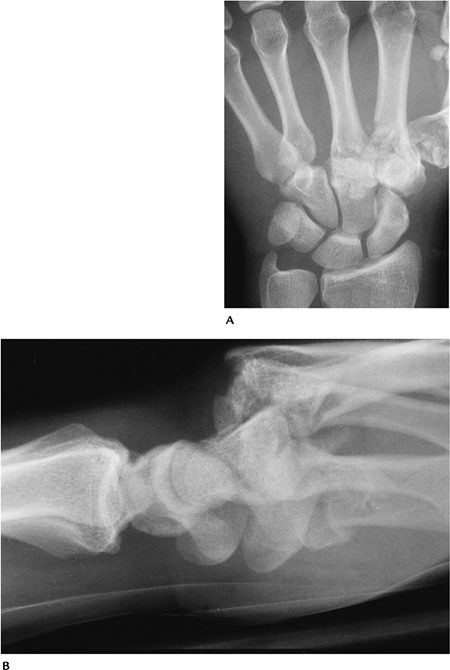
FIGURE 9-20 Transscaphoid perilunate dislocation seen on PA (A) and lateral (B) radiographs. The lunate and proximal scaphoid are in nearly normal position on the PA view (A). The second carpal row is irregularly aligned (lines). The displacement of the capitate (C) compared with the lunate (L) is obvious on the lateral view.
|
P.589
 |
|
FIGURE 9-21 PA (A) and lateral (B) radiographs of a carpometacarpal fracture/dislocation.
|
Suggested Reading
Gregor DP, O’Brien ET. Classification and management of carpal dislocations. Clin Orthop 1980;149:55–72.
P.590
Fractures/Dislocations: Metacarpal Fractures
Key Facts
-
Metacarpal fractures are common. The fourth and fifth metacarpals are most often injured.
-
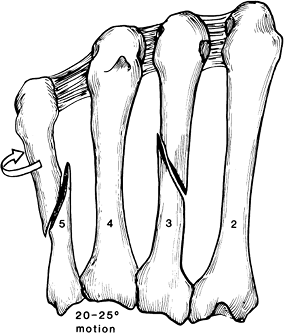
Fractures generally are categorized as thumb, mobile rays (fourth and fifth), and stable rays (second and third).
-
Thumb fractures are described by location. In order of decreasing frequency, fractures occur as follows:
-
Intra-articular basilar fractures
-
Proximal metaphyseal fractures
-
Transverse or spiral diaphyseal fractures
-
First metacarpal neck fractures
-
-
Second and third (stable rays) metacarpal fractures
-
Considered stable because of lack of motion at the carpometacarpal joints.
-
Neck fractures are most common.
-
Spiral fractures are less common.
-
-
Fourth and fifth (mobile rays) metacarpal fractures
-
Considered mobile because of motion at carpometacarpal joints.
-
Fractures of the neck and metacarpal bases occur more frequently.
-
Fracture of the fifth metacarpal neck (boxer’s fracture) is most common.
-
-
Mechanism of injury: direct trauma, axial loading.
-
Imaging with routine radiographs generally is diagnostic. CT may be required to more completely evaluate articular fractures.
-
Treatment: closed reduction of
nonangulated or nonarticular fractures. Angulated or articular
fractures require internal fixation. -
Complications: shortening, rotation (especially spiral fractures), decreased function, malunion, arthrosis.
P.591
 |
|
FIGURE 9-22
Radiograph of the thumb demonstrating an intra-articular fracture (1), Bennett fracture with lines demonstrating metaphyseal (2), diaphyseal (3), and distal neck fractures (4). |
P.592
 |
|
FIGURE 9-23
The second to fifth metacarpals. There is laxity in the transverse metacarpal ligament between the fourth and fifth metacarpals that leads to shortening and rotation with oblique or spiral factures. There is more motion allowed at the fourth and fifth metacarpal bases. |
 |
|
FIGURE 9-24 PA view of a fifth metacarpal neck fracture (boxer’s fracture) (arrow).
|
P.593
 |
|
FIGURE 9-25
PA radiograph showing intra-articular fractures of the second and third metacarpals and an undisplaced fracture of the fifth metacarpal base (arrow). |
Suggested Reading
Berquist TH. Imaging of orthopedic trauma, 2nd ed. New York: Raven Press; 1992:749–870.
P.594
Fractures/Dislocations: Phalangeal Fractures/Dislocations
Key Facts
-
Phalangeal fractures are the most common fractures in the hand. Fractures of the proximal phalanx are most common.
-
Dislocations of the phalangeal and metacarpophalangeal (MCP) joints usually are dorsal.
-
Mechanism of injury: direct blows, falls, athletic injuries.
-
Imaging with PA and lateral radiographs usually is adequate. CT may be required after reduction for osteochondral evaluation.
-
Treatment: closed reduction unless there is shortening, angulation, or significant articular involvement.
-
Complications: shortening, rotation, arthrosis, decreased joint function.
 |
|
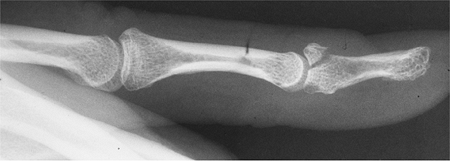
FIGURE 9-26 Lateral radiograph of an angulated proximal phalangeal fracture.
|
 |
|
FIGURE 9-27 Lateral view of a dorsal phalangeal dislocation (arrow).
|
P.595
 |
|
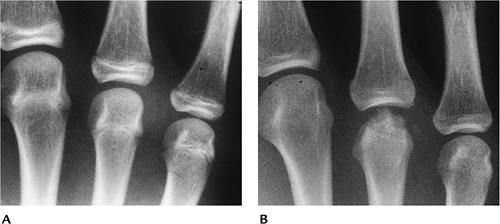
FIGURE 9-28 PA (A), oblique (B), and lateral (C) radiographs of a subtle volar plate middle phalanx (arrow) hyperextension injury.
|
 |
|
FIGURE 9-29 Lateral view of a hyperflexion Mallet fracture of the distal phalanx.
|
P.596
Suggested Reading
Ruby LK. Common hand injuries in athletes. Orthop Clin North Am 1980;11:819–839.
P.597
Carpal Instability
Key Facts
-
Carpal instability can be seen after fractures and ligament injuries, or in association with inflammatory arthropathies.
-
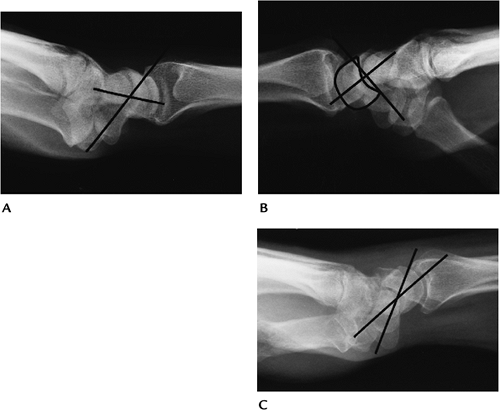
Dorsal intercalated segment instability
(DISI) is most common. The scapholunate angle is increased on the
lateral radiograph (<45 degrees), and the lunate faces dorsally. -
Volar intercalated segment instability is
seen less frequently. The scapholunate angle is decreased (<45
degrees), and the lunate is palmar flexed with palmar shift of the
capitate. -
Scapholunate advanced collapse (wrist)
results from chronic scapholunate dissociation or after scaphoid
fracture nonunion. Radiocarpal and scaphotrapezium trapezoid
arthropathy are a part of the collapse. -
Diagnosis can be accomplished on PA and lateral radiographs. Motion studies and CT or MRI are rarely indicated for diagnosis.
-
Treatment options include proximal row carpectomy, wrist fusion, or limited carpal (four corner) fusion.
 |
|
FIGURE 9-30 Lateral radiographs of the wrist demonstrating the normal scapholunate angle (lines, ~45 degrees) (A), DISI with increased scapholunate angle and the lunate angled dorsally (B), and volar intercalated segment instability with a decreased scapholunate angle and the lunate angled volarly (C).
|
P.598
 |
|
FIGURE 9-31 Scapholunate advanced collapse wrist. PA (A) and lateral (B) radiographs of the wrist demonstrate marked widening of the scapholunate space (open arrow) with proximal displacement of the capitate (arrow) and DISI deformity on the lateral radiograph (lines in B).
|
Suggested Reading
Cohen MS. Degenerative arthritis of the wrist: Proximal row carpectomy versus scaphoid excision and four corner arthrodesis. J Hand Surg 2001;26A:94–104.
Linscheid RL, Dobyns JH, Beabout JW, et al. Traumatic instability of the wrist: Diagnosis, classification, and pathomechanics. J Bone Joint Surg 1972;54A:1612–1632.
P.599
Soft Tissue Trauma/Miscellaneous Conditions: Ligament Injuries
Key Facts
-
Ligament injuries of the hand and wrist may occur as isolated injuries or in association with fractures.
-
Ligament anatomy of the wrist is complex, including dorsal and volar capsular ligaments and interosseous ligaments.
-
Ligamentous support of the MCP and
phalangeal joints is similar with collateral ligaments, accessory
collateral ligaments, and the volar plate. -
Common ligament injuries of the hand and wrist are as follows:
-
Scapholunate ligament tear
-
Lunotriquetral ligament tear
-
Triangular fibrocartilage complex tears
-
“Gamekeeper’s thumb”—tear of the ulnar collateral ligament of the first MCP joint
-
-
Imaging of ligament injuries may be accomplished with several approaches.
-
Stress views—varus and valgus of the involved joint (MCP, interphalangeal).
-
Motion series of the wrist—PA radial and ulnar deviation, flexion and extension lateral, clenched-fist PA.
-
Arthrography—involved wrist of the hand
or wrist is injected with iodinated contrast. Extravasation is seen
with capsule and ligament tears. Anesthetic can be injected to confirm
source of pain. -
MRI or MR arthrography—fluid (T2-weighted
image) or gadolinium passes through ligament and capsular defects. MR
arthrography is most accurate.
-
P.600
 |
|
FIGURE 9-32 Arthrogram of the first MCP joint showing extravasation (arrow) resulting from gamekeeper’s thumb with an ulnar collateral ligament tear.
|
P.601
 |
|
FIGURE 9-33
Conventional wrist arthrogram in a patient with ulnar pain showing injection of the DRUJ. Contrast passes through a triangular fibrocartilage tear (1) into the radiocarpal joint and then through a lunotriquetral ligament tear (2) into the intercarpal joint. |
 |
|
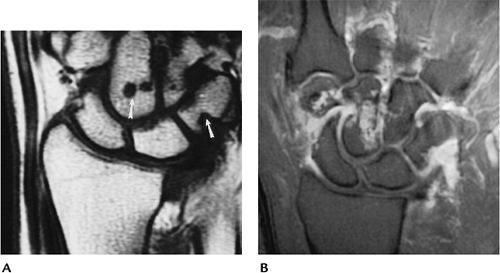
FIGURE 9-34 Scapholunate tear. (A) Clenched-fist view showing widening of the scapholunate joint (arrow). (B) Coronal T2-weighted image showing the ligament tear (arrow).
|
P.602
 |
|
FIGURE 9-35 Triangular fibrocartilage tear. MR arthrogram showing contrast in the radiocarpal joint with a tear (arrow) in the triangular fibrocartilage.
|
Suggested Reading
Girgis W, Epstein RE. Magnetic resonance imaging of the hand and wrist. Semin Roentgenol 200;35:286–296.
Schweitzer
ME, Brahine SK, Holder J, et al. Chronic wrist pain: Spin-echo and
short TI inversion recovery MR imaging and conventional and MR
arthrography. Radiology 1992;182:205–211.
ME, Brahine SK, Holder J, et al. Chronic wrist pain: Spin-echo and
short TI inversion recovery MR imaging and conventional and MR
arthrography. Radiology 1992;182:205–211.
P.603
Soft Tissue Trauma/Miscellaneous Conditions: Tendon Injuries
Key Facts
-
Tendon injuries include partial and complete tears, subluxation or dislocation, and tendinitis. The last is most common.
-
Tendinitis may be the result of infection, previous fracture, or overuse.
-
Imaging of tendon injuries can be
performed with tenography, ultrasound, or MRI. The latter is
noninvasive and preferred in most cases. T2-weighted sequences in the
axial and coronal or sagittal planes can detect inflammation and tears.
With tears, both ends of the tendon must be demonstrated for operative
planning. -
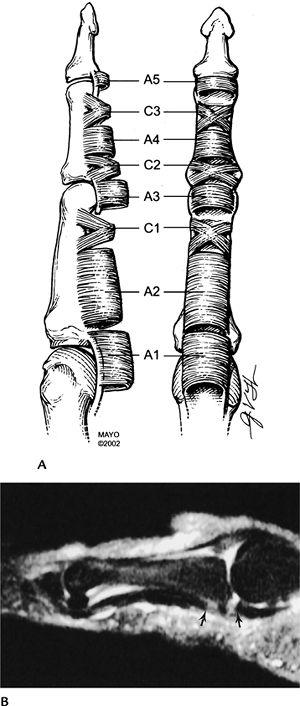
Tears in the pulley systems of the flexor
tendons may also occur. Patients should be studied in the sagittal
plane with the finger in flexion and extension.
 |
|
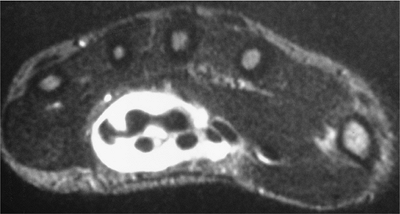
FIGURE 9-36
The normal tendon is low intensity on MRI and has minimal high signal intensity fluid in the tendon sheath. This T2-weighted image shows fluid-distended tendon sheaths caused by flexor tenosynovitis. |
P.604
 |
|
FIGURE 9-37 Flexor tendon and pulley injuries. (A) The pulley system that maintains position of the flexor tendons. (B) Sagittal fat-suppressed fast spin-echo T2-weighted image demonstrates a tear with slight separation of the flexor tendon (arrows).
The relationship to the phalanges is maintained indicating the pulley system is intact. Images in flexion would confirm the intact pulley system. |
P.605
Suggested Reading
Clavero JA, Alomar X, Moukill JM, et al. MR imaging of ligament and tendon injuries of the fingers. Radiographics 2002;22:237–257.
Paradella JA, Balkisoon ARA, Hayes CW, et al. Bowstring injury of the flexor tendon pulley system: MR imaging. AJR Am J Roentgenol 1996;167:347–349.
P.606
Soft Tissue/Miscellaneous Conditions: de Quervain Tenosynovitis and Intersection Syndrome
Key Facts
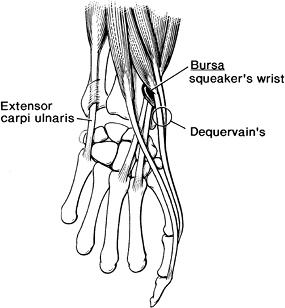
-
De Quervain tenosynovitis involves the first dorsal extensor compartment.
-
Patients present with pain and restriction of the extensor pollicis brevis and abductor pollicis longus.
-
The condition is most common in women 30
to 50 years of age involved in overuse of motions such as grasp and
radial and ulnar deviation of the wrist. -
Clinical symptoms may mimic a scaphoid fracture, flexor carpi radialis tendinitis, or intersection syndrome (squeaker’s wrist).
-
Intersection syndrome occurs slightly proximal to de Quervain tenosynovitis (Fig. 9-38).
A bursa may form between the extensor carpi radialis longus and brevis
and the abductor pollicis longus and extensor pollicis brevis. -
Patients with intersection syndrome are
frequently involved in racket sports and present with pain, weak grip,
and crepitation (squeaker’s wrist). -
MRI or ultrasound may be used to confirm
the diagnosis. The region of the radial styloid may have abnormal
signal intensity as the result of chronic tendon thickening. A
fluid-filled bursa is typical in intersection syndrome.
 |
|
FIGURE 9-38 De Quervain and intersection syndrome (squeaker’s wrist).
|
P.607
 |
|
FIGURE 9-39
De Quervain tenosynovitis. Coronal fast spin-echo fat-suppressed T2-weighted image demonstrates marrow edema in the radial styloid and thickening (arrow) of the adjacent tendons. |
 |
|
FIGURE 9-40 Intersection syndrome. Axial fat-suppressed T2-weighted image demonstrating a fluid-filled bursa (arrow).
|
Suggested Reading
Costa CR, Morrison WB, Carrino JA. MRI features of intersection syndrome of the forearm. AJR Am J Roentgenol 2003;181:1245–1249.
Glajchen N, Schweitzer ME. MRI features in de Quervain’s tenosynovitis of the wrist. Skel Radiol 1996;25:63–65.
P.608
Neoplasms: Bone Tumors
Key Facts
-
Bone tumors are uncommon in the hand and wrist compared with the axial skeleton and lower extremity.
-
Benign tumors are more common than malignant tumors.
-
Table 9-2 lists common tumor and tumorlike conditions in the hand and wrist.
-
Routine radiographs remain the main
screening technique for patients with suspected bone neoplasms. CT or
MRI is useful for treatment planning.
 |
|
FIGURE 9-41
Enchondromas. PA radiograph of the hand demonstrating multiple lytic expanding lesions in the second metacarpal and second and third phalanges. |
P.609
|
TABLE 9-2 BONE TUMOR AND TUMORLIKE CONDITIONS IN THE HAND AND WRIST
|
||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Suggested Reading
Pozanski AK. The hand in radiologic diagnosis. Philadelphia: WB Saunders; 1984.
Unni KK. Dahlin’s bone tumors: General aspects and data on 11,087 cases, 5th ed. Philadelphia: Lippincott-Raven; 1996.
P.610
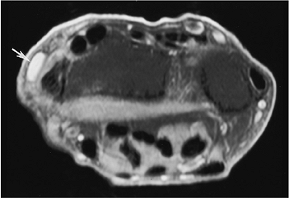
Neoplasms: Soft Tissue Masses
Key Facts
-
Most soft tissue masses of the hand and wrist are benign.
-
Imaging of soft tissue masses is
difficult with radiographs. Ultrasound is useful, but MRI is preferred
for detection and classification of these lesions. -
Common soft tissue masses of the hand and wrist include
-
Ganglion cysts (commonly associated with internal derangements of the wrist)
-
Epidermoid cysts (distal finger)
-
Glomus tumors (subungual or palmar aspect of finger)
-
Giant cell tumor of the tendon sheath
-
Mucoid cysts (distal joints of hand)
-
Lipomas
-
Hemangiomas
-
Neuromas
-
 |
|
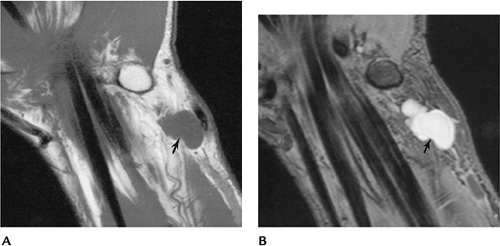
FIGURE 9-42 Coronal T1- (A) and fat-suppressed fast spin-echo T2-weighted (B) images of the wrist demonstrating a lobulated ganglion cyst (arrow).
|
P.611
 |
|
FIGURE 9-43 Lipoma. Axial (A) and sagittal (B) T1-weighted images of a lobulated fatty lesion (arrows) characteristic of a lipoma.
|
Suggested Reading
Butler ED, Hamell JP, Seipel RS, et al. Tumors of the hand. A 10-year survey and report of 437 cases. Am J Surg 1960;100:293–302.
P.612
Arthropathies
Key Facts
-
Numerous arthropathies affect the hand and wrist (Table 9-3).
-
Routine radiographs of the hands provide
the best screening tool for patients with arthritis. Dynamic
contrast-enhanced MRI can detect synovial changes early and monitor
disease activity. -
Image features and distribution of involvement are useful in determining the type of arthritis.
-
Swelling: uniform, periarticular, fusiform (sausage digit—psoriasis), lumpy (rheumatoid nodules, sarcoid)
-
Subluxation: common with rheumatoid arthritis and systemic lupus erythematosus
-
Mineralization: usually normal except infection or rheumatoid arthritis
-
Calcification: seen in gouty tophi, scleroderma, mixed connective tissue disease, tumoral calcinosis, and chondrocalcinosis
-
Distal joints: osteoarthritis, psoriasis
-
Proximal joints: rheumatoid arthritis
-
|
TABLE 9-3 ARTHROPATHIES OF THE HAND AND WRIST
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
P.613
 |
|
FIGURE 9-44
PA view of the hand and wrist with changes of osteoarthritis in the distal phalangeal joints and wrist. There are changes of erosive osteoarthritis in the second through fourth distal phalangeal joints. |
P.614
 |
|
FIGURE 9-45 Rheumatoid arthritis. (A) Early changes in the wrist with soft tissue swelling and erosions (arrowheads). (B) Advanced rheumatoid arthritis with carpal collapse and erosion of the distal radius and ulna.
|
 |
|
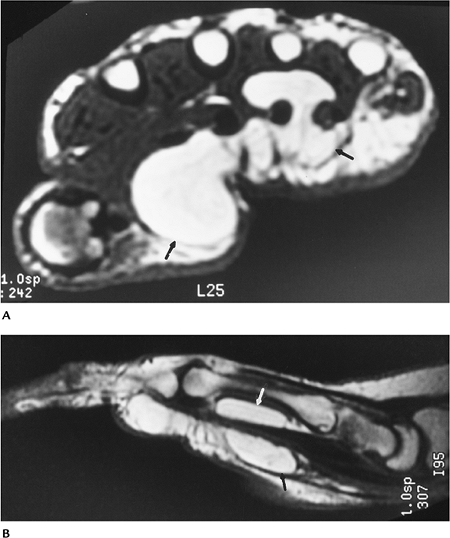
FIGURE 9-46 Rheumatoid arthritis. (A) Coronal T1-weighted image demonstrating erosions (arrows) not apparent on radiographs. (B) Contrast-enhanced image shows enhancing synovium and carpal erosions in the capitate and trapezium.
|
P.615
 |
|
FIGURE 9-47
Psoriatic arthritis. PA radiograph demonstrates fusiform swelling of the third and fourth fingers with increased bone density and aggressive erosive changes in the proximal interphalangeal and to a lesser degree the distal interphalangeal joints. The MCP and wrist are spared. |
Suggested Reading
Brower AC. Arthritis in black and white. Philadelphia: WB Saunders; 1997:33–67.
P.616
Avascular Necrosis
Key Facts
-
AVN can involve any osseous structure in
the hand and wrist. AVN commonly involves the lunate (Kienböck
disease), the proximal scaphoid after fracture (Preiser disease), and,
to a lesser extent, the capitate and metacarpal heads. -
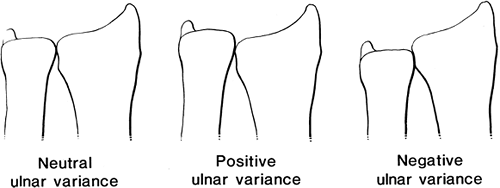
Kienböck disease is considered traumatic.
Patients present with vague wrist pain. AVN of the lunate is associated
with ulnar minus variance (ulna shorter than radius). -
Routine radiographs often are normal in
early stages of AVN. Later, bone sclerosis and fragmentation occur.
Early detection can be accomplished with radionuclide scans, but MRI is
the technique of choice for early detection and after the healing
process. -
MRI of AVN can be performed using T1- and
T2-weighted sequences. The coronal plane is most useful for the lunate,
proximal scaphoid, and other carpal bones. Intravenous gadolinium is
useful for evaluating flow and subtle changes.
 |
|
FIGURE 9-48
Normal (neutral), ulnar positive, and ulnar negative variance. Ulnar negative variance is associated with AVN of the lunate. Ulnar positive variance is associated with ulnar lunate abutment syndrome. |
P.617
 |
|
FIGURE 9-49 Baseball player with hand pain after trauma. (A) Initial radiograph is normal. (B) Eight weeks later, there is fragmentation of the fourth metacarpal head as the result of AVN.
|
P.618
 |
|
FIGURE 9-50 AVN of the lunate. (A) Initial T1-weighted MR image showing no signal (arrow) in the lunate because of AVN. (B)
Follow-up T1-weighted image after 3 months of cast immobilization showing return of signal to near normal after revascularization. |
P.619
Suggested Reading
Barnes NA, Howes AJ, Jeffers H, et al. Avascular necrosis of the third metacarpal head. Eur Radiol 2000;3:115–117.
Reinus WR, Conway WF, Totty WG, et al. Carpal avascular necrosis. MR imaging. Radiology 1986;160:689–693.
P.620
Nerve Compression Syndromes: Carpal Tunnel Syndrome
Key Facts
-
Patients with carpal tunnel syndrome
present with chronic discomfort and tingling in the distribution of the
median nerve. Nocturnal symptoms are common. Muscle atrophy may be
present on physical examination. -
Most patients are 30 to 60 years of age. Females outnumber males 5:1. The condition is bilateral in 50% of the cases.
-
Cause may be related to tenosynovitis, soft tissue masses, ganglion cysts, fracture deformity, anomalous muscles, or ischemia.
-
Diagnosis is based on physical
examination and nerve conduction studies. Imaging, when necessary, can
be accomplished with ultrasound or, more often, MRI. -
Treatment: decompression of carpal tunnel.
 |
|
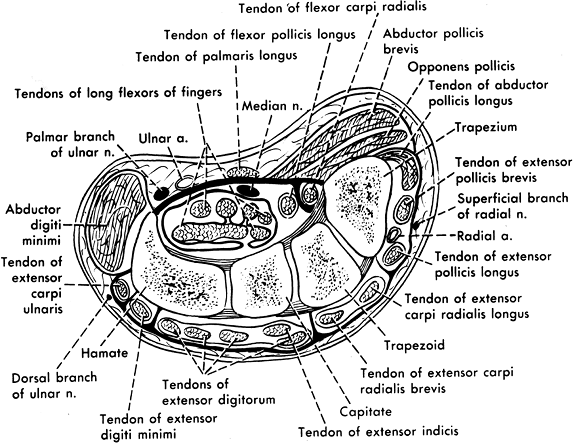
FIGURE 9-51 The relationships of the median and ulnar nerves in the wrist.
|
P.621
 |
|
FIGURE 9-52 Axial T2-weighted MR image showing deformity and increased signal intensity in the median nerve (arrow) causing carpal tunnel syndrome.
|
Suggested Reading
Ikeda K, Haughton VM, Hu KC, et al. Correlative MR anatomic study of the median nerve. AJR Am J Roentgenol 1996;167:1233–1236.
Mauer J, Bleochkowski A, Tempka A, et al. High-resolution MR imaging of the carpal tunnel and wrist. Acta Radiol 2000;41:78–83.
P.622
Nerve Compression Syndromes: Ulnar Nerve Compression
Key Facts
-
Ulnar nerve compression causes pain and tingling in the distribution of the nerve.
-
Compression most commonly occurs in Guyon canal (Fig. 9-53).
-
Cause is similar to carpal tunnel syndrome. Primary neural pathology or compression form and adjacent mass are most common.
-
Imaging of Guyon canal and the ulnar nerve is most easily accomplished with MRI.
-
T2-weighted axial and coronal or sagittal images are most useful.
 |
|
FIGURE 9-53 Axial T2-weighted image demonstrates increased signal intensity and enlargement of the ulnar nerve (arrow) resulting from trauma. Findings correlated with electromyography.
|
P.623
 |
|
FIGURE 9-54 Fibrolipoma of the ulnar nerve. Axial T1-weighted images (A,B) demonstrate an enlarged low signal intensity nerve with associated fatty tissue (arrow).
|
Suggested Reading
Berquist TH. MRI of the musculoskeletal system, 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2006:789–797.
P.624
Ulnar Lunate Abutment Syndrome
Key Facts
-
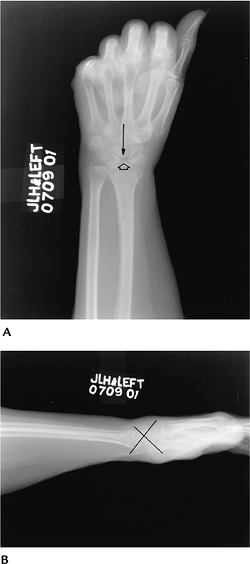
Ulnar lunate abutment syndrome is associated with ulnar positive variance (Fig. 9-55).
-
Patients present with ulnar wrist pain that often is exaggerated by ulnar deviation of the wrist.
-
Radiographs show ulnar positive variance
and sclerosis or cystic change in the lunate and triquetrum. Features
are more easily demonstrated with MRI for early bone, cartilage, and
triangular fibrocartilage abnormalities. -
Treatment: ulnar shortening when conservative treatment fails.
 |
|
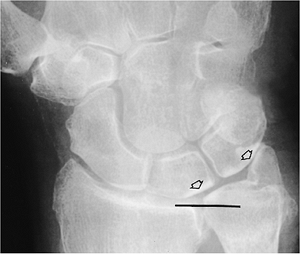
FIGURE 9-55 Ulnar lunate abutment syndrome. (A) PA radiograph demonstrates ulnar positive variance (line), prominent ulnar styloid, and sclerotic changes in the lunate and triquetrum caused by cartilage loss (open arrows).
|
P.625
 |
|
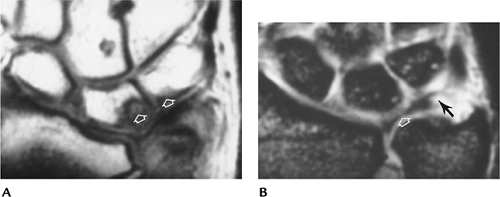
FIGURE 9-56 MR images in patients with ulnar lunate abutment syndrome. (A) T1-weighted image shows low signal intensity in the lunate and adjacent triquetrum. (B) Gradient echo coronal shows displacement of the radial aspect of the triangular fibrocartilage (open arrow) and a peripheral tear (black arrow).
|
Suggested Reading
Cerezal L, del Pinal F, Abascal F, et al. Imaging findings in the ulnar-sided wrist impaction syndromes. Radiographics 2002;22:105–121.
Palmer AK, Werner FW. Triangular fibrocartilage complex of the wrist—anatomy and function. J Hand Surg 1981;16:153–162.
