Fracture, Calcaneus
Fracture, Calcaneus
Greg Nakamoto
Description
-
Calcaneus fractures can occur secondary to either acute trauma or recurrent stress (ie, calcaneal stress fracture). The focus here is on the management of acute traumatic fractures of the calcaneus.
-
Of primary concern when evaluating the acute calcaneus fracture is determining whether the fracture is extra- or intraarticular.
-
Most extraarticular fractures can be managed conservatively.
-
Current practice is for most intraarticular fractures to be treated surgically. Such fractures consequently should be referred for orthopedic evaluation.
-
Having said that, no universally accepted guidelines exist as to the optimal treatment of calcaneal fractures.
-
It should be noted that most calcaneal fractures (other than stress fractures) involve the articular surface.
-
-
Secondarily, one should be aware that many patients with acute calcaneus fractures have other coexisting lower extremity or vertebral injuries.
-
Synonym(s): Os calcis fracture; Heel bone fracture
Epidemiology
Prevalence
-
Most commonly seen in young men, representing ∼2% of all fractures seen in adults (1,2,3)
-
Calcaneal fractures are relatively rare in children, who account for only 5% of all calcaneal fractures (4).
-
The calcaneus is the most frequently fractured tarsal bone, accounting for 60% of all tarsal fractures (1).
-
∼25–30% of calcaneal fractures are extraarticular; 70–75% are intraarticular (1,2,3).
-
∼2% are open fractures (1).
Risk Factors
-
Fall from a height directly onto the heel
-
Other force of impact directly onto the heel (eg, motor vehicle accident)
-
Osteoporosis can predispose to calcaneal fractures despite a seemingly trivial mechanism of injury.
-
Extraarticular fractures of the calcaneal body and plantar tuberosity also can be caused by blunt-force trauma or a twisting injury (1).
-
Avulsion fractures of the calcaneal tuberosity can occur with abrupt contraction of the Achilles tendon (1).
-
Stress fractures of the calcaneus can occur as an overuse injury in athletes (1).
Commonly Associated Conditions
-
High-energy mechanism of injury usually is required for these fractures, resulting in a high incidence of coexisting lower extremity or spinal injury.
-
Calcaneal fractures occur bilaterally in 5–9% of patients (1,4).
-
10% of patients will have sustained a spinal compression fracture as well (1,4).
-
Often associated with significant local soft tissue injury
Alert
Acute compartment syndrome of the foot occurs in up to 10% of patients and is a surgical emergency (4).
 Diagnosis
DiagnosisHistory
Mechanism of injury:
-
Extraarticular fractures are more commonly due to an indirect mechanism such as a twisting injury or muscular avulsion.
-
Intraarticular fractures are due to high-energy accidents.
-
History of a fall from a height is particularly concerning for additional lower extremity and lumbar spine injury.
Physical Exam
-
Signs and symptoms include:
-
Heel pain
-
Swelling
-
Ecchymosis
-
-
Physical examination includes the following:
-
Look for associated soft tissue injury. Blisters may occur when swelling is substantial. Excessive soft tissue injury will influence duration of splinting before placing into a cast for those being treated conservatively or may delay definitive surgical treatment in those being treated operatively (1,5)[C].
-
Assess function of the nerves of the foot. With significant swelling, pulses may be difficult to assess; check capillary refill of the toes.
-
Ecchymosis that tracks distally to the sole of the foot, known as the Mondor sign, is pathognomonic for calcaneal fracture (1).
-
Check for evidence of lower extremity compartment syndrome. Significant swelling in the plantar arch may suggest plantar compartment syndrome. This requires emergent surgical referral even if the fracture itself is nonoperative (1)[A].
-
Look for associated lower extremity and vertebral fracture because of high incidence of coexisting injury.
-
P.173
Diagnostic Tests & Interpretation
Imaging
-
Goal of imaging is to confirm diagnosis of calcaneus fracture and to determine whether the fracture is intra- or extraarticular (5,6)[B].
-
Standard initial x-rays: Anteroposterior, lateral, and axial calcaneus (Harris) views; consider obtaining views of the contralateral heel for comparison purposes.
-
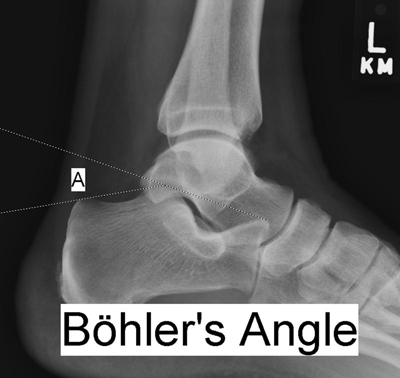
Böhler tuber joint angle (Figure 1):
-
A line is drawn between the posterosuperior aspect of the calcaneus and the highest point of the posterior subtalar articular surface; a second line, which intersects the first, is drawn from the highest point of the anterior process to the posterior margin of the subtalar surface (4).
-
Measures between 25 and 40 degrees, with a similar angle found in the two calcanei in any one person.
-
Decrease of 10 degrees versus the uninjured side is considered a significant difference.
![images]()
-
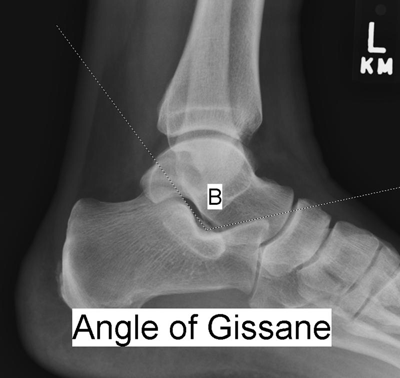
“Crucial angle” of Gissane (Figure 2): On the lateral x-ray, the angle formed by the wedge in which the lateral process of the talus sits; this angle is disrupted when axial compressive forces drive the talus as a wedge into this space. Radiograph of the uninjured side is useful for comparison; may not be as helpful as the Böhler angle in determining the presence of a calcaneus fracture (6).
-
-
Oblique (Broden) views can be helpful in assessing involvement of the articular surfaces.
-
Additional x-rays to consider based on history and physical examination include views of the contralateral foot (because of the significant incidence of bilateral injury and to compare Böhler and Gissane angles with the injured foot), ipsilateral ankle, and lumbar spine and pelvis (because of high frequency of associated fractures).
![images]()
-
CT scan (4,5,6)[A]:
-
In patients in whom x-rays are inconclusive, CT scan is considered the gold standard for confirming the diagnosis of calcaneal fracture.
-
Additionally, if plain films show articular involvement or if suspicion of articular involvement remains high despite equivocal plain films, then a CT scan is essential for a more specific analysis of the subtalar and calcaneocuboid joints because displacement of either likely will require surgical management.
-
Should include axial and coronal cuts
-
-
MRI: While not generally used for the evaluation of traumatic calcaneus injuries, MRI may be the preferred imaging modality in patients with suspected stress fractures, particularly in patients with severe osteoporosis, in whom a bone scan may appear falsely negative (4,6)[C].
-
Follow-up and special considerations: For extraarticular fractures being treated nonoperatively, postreduction imaging involves repeating the standard radiographs to assess adequacy of reduction after closed manipulation. Comparison with the opposite foot often is useful.
-
Differential Diagnosis
-
Talar fracture
-
Cuboid fracture
-
Malleolar fracture
-
Ankle dislocation
-
Ankle sprain
 Treatment
Treatment-
Ice and oral analgesics are useful in the prehospital setting, and oral analgesics may be required for some time after casting.
-
Reduction techniques:
-
Extraarticular calcaneal body fractures with minimal displacement: Mediolateral compression of the heel with the palms of the hands can be applied to reduce displaced extraarticular body fractures being treated nonoperatively.
-
Other extraarticular fractures or any intraarticular fractures: Surgical consultation for possible open reduction and internal fixation (ORIF). For details, see “Ongoing Care.”
P.174 -
-
Postreduction evaluation: Repeat x-rays in 1 wk in any patient being treated nonoperatively.
-
Immobilization:
-
Usually begins with splinting or bulky Jones dressing to accommodate changes in soft tissue swelling.
-
In patients who require casting (see “Ongoing Care”), the splint can be changed to a short-leg cast after the initial soft tissue injury has stabilized after ∼3–5 days.
-
In patients who require operative treatment, splinting is appropriate until the patient can see an orthopedic surgeon.
-
Surgery/Other Procedures
-
Intraarticular fractures and certain extraarticular fractures as listed below (see “Ongoing Care”) should undergo orthopedic evaluation for possible surgical treatment.
-
In patients requiring operative treatment, referral should be made promptly so that fixation can occur within 5–7 days.
-
In patients with significant associated soft tissue injury, prompt orthopedic referral allows for early interventions to reduce edema, which can take 7–14 days to accomplish. In such cases, operative treatment within the 1st 3 wks, before early consolidation of the fracture fragments, is preferred (5)[C].
-
All cases of compartment syndrome require emergent referral (1)[A].
 Ongoing Care
Ongoing Care-
Optimal management of calcaneal fractures, particularly of intraarticular fractures, remains controversial (2,5,6,7)[B]. New techniques, such as arthroscopically assisted percutaneous pinning, are being developed that may lead to more consistently improved outcomes.
-
Some general guidelines include:
-
Nondisplaced or minimally displaced extraarticular fractures of the body of the calcaneus can be treated with short-leg casting and no weight bearing for 2 wks, followed by range-of-motion exercises. Progressive weight bearing may start at 8 wks, with full weight bearing by 12 wks (1)[C].
-
Exceptions (extraarticular fractures that might best be treated surgically) (1,8)[C]:
-
Extraarticular fractures with a decrease of Böhler angle by 10 degrees versus the contralateral side
-
Fractures of the sustentaculum tali with >2 mm of displacement
-
Displaced avulsions of the Achilles tendon insertion from the calcaneal tuberosity
-
Significant fractures of the calcaneal body
-
-
Intraarticular fractures or extraarticular fractures as listed should be referred for orthopedic consultation (2)[B].
-
An intraarticular fracture still might be treated nonoperatively if it is completely nondisplaced (5)[C].
-
Follow-Up Recommendations
-
Conservative treatment should be reserved for extraarticular fracture only. All intraarticular fractures or the specific extraarticular fractures listed earlier should be referred for consideration of surgical fixation.
-
In patients treated conservatively, removal from splinting/casting should be followed by referral to physical therapy to restore normal flexibility and strength before allowing return to play.
Patient Education
-
Patients should be informed early on that treatment can be difficult and that adverse outcomes can be potentially severe and disabling at times.
-
Chronic pain and posttraumatic arthritis are not uncommon.
Complications
-
In both operatively and nonoperatively treated patients, chronic disability owing to pain from an improperly functioning or arthritic subtalar or calcaneocuboid joint may occur (1,6).
-
Complications specifically seen in patients undergoing ORIF include (1):
-
Infection
-
Pain
-
Swelling
-
Delayed would healing
-
Nonunions of the fracture fragments
-
Lateral impingement of the peroneal tendon
-
Sural nerve injury
-
P.175
References
1. Nickelbur S, Dixon T, Probe R. Calcaneus fractures. eMedicine. Retrieved Aug 10, 2009, from http://emedicine.medscape.com/article/1232246-overview; 2008.
2. Bajammal S, Tornetta P, Sanders D, et al. Displaced intra-articular calcaneal fractures. J Orthop Trauma. 2005;19:360–364.
3. Ibrahim T, Rowsell M, Rennie W, et al. Displaced intra-articular calcaneal fractures: 15-year follow-up of a randomised controlled trial of conservative versus operative treatment. Injury. 2007.
4. Khan A, Rahim R, Irion K, et al. Calcaneus fractures. eMedicine. Retrieved Aug 10, 2009, from http://emedicine.medscape.com/article/388031-overview; 2008.
5. Sanders R. Displaced intra-articular fractures of the calcaneus. J Bone Joint Surg Am. 2000;82:225–250.
6. Simpson RB. Fractures of the calcaneus. Curr Opin Orthop. 2007;18:124–127.
7. Randle JA, Kreder HJ, Stephen D, et al. Should calcaneal fractures be treated surgically? A meta-analysis. Clin Orthop Relat Res. 2000;377:217–227.
8. Thermann H, Krettek C, Hüfner T, et al. Management of calcaneal fractures in adults. Conservative versus operative treatment. Clin Orthop Relat Res. 1998;353:107–124.
Additional Reading
Buckley R, Tough S, McCormack R, et al. Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures: a prospective, randomized, controlled multicenter trial. J Bone Joint Surg Am. 2002;84-A:1733–1744.
Lewis G. Biomechanics as a basis for management of intra-articular fractures of the calcaneus. J Am Podiatr Med Assoc. 1999;89:234–246.
Miric A, Patterson B. Pathoanatomy of intra-articular fractures of the calcaneus. J Bone Joint Surg. 1998;80A:207–212.
Rockwood C, Green D, Bucholz R, et al., eds. Rockwood and Green's fractures in adults, 4th ed. Philadelphia: Lippincott-Raven Publishers, 1996.
Swanson SA, Clare MP, Sanders RW. Management of intra-articular fractures of the calcaneus. Foot Ankle Clin. 2008;13:659–678.
 Codes
CodesICD9
-
733.95 Stress fracture of other bone
-
825.0 Fracture of calcaneus, closed
-
825.1 Fracture of calcaneus, open
Clinical Pearls
-
During the initial evaluation of a patient with a calcaneus fracture, be aware that many patients will have a coexisting lower extremity or vertebral fracture. 10% will have coexisting compartment syndrome of the foot, which is a surgical emergency.
-
Proper management of calcaneus fractures requires determining if the fracture is intraarticular or extraarticular. Intraarticular fractures generally are best treated surgically, whereas extraarticular fractures (with the exceptions noted under “Ongoing Care”) are often treated nonoperatively. If x-rays are equivocal, CT scan is used to determine if the fracture is intraarticular.
-
Optimal treatment of calcaneal fractures is still controversial, with posttraumatic arthritis being the cause of most cases of chronic disability.
-
In nonoperative cases, athletes may be ready to return to play in as little as 8–12 wks depending on the severity of the original injury. In operative cases, the duration of immobilization and recovery is more variable and depends on the particulars of the fracture.
-
Consensus suggests that long-term outcome is determined mainly by the degree of joint destruction at the time of injury (8).
-
It seems poorer outcomes are seen more commonly in patients who develop arthritis of the subtalar joint; consequently, there might be a link between preservation of the subtalar joint at the time of initial treatment conferring a better long-term prognosis (6).
-
There seems to be a subset of calcaneal fractures that has a poor outcome regardless of treatment (1).
-