Elbow/Forearm
Editors: Berquist, Thomas H.
Title: Musculoskeletal Imaging Companion, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Chapter 8 – Elbow/Forearm
Chapter 8
Elbow/Forearm
Thomas H. Berquist
Laura W. Bancroft
Protocols
Key Facts
-
Routine radiography
-
Minimal series: anteroposterior (AP) and lateral views
-
Trauma series: AP, lateral, and both oblique views. (The optimal lateral view for hemarthrosis is a cross-table lateral.)
-
-
Computed tomography (CT)
-
3-mm axial sections (for conventional imaging)
-
Bone and soft tissue settings
-
1-mm sections at 0.5-mm intervals for coronal and sagittal reformatting or three-dimensional images
-
-
Magnetic resonance imaging (MRI) (Table 8-1)
-
Patient positioning arm at side
Coils 5-inch circular (allows more
flexible positioning) Circumferential: elbow extended (more uniform
signal intensity) Flat-phased array coil: if arm or forearm need to be
included in field of view -
P.513
Fractures/Dislocations: Distal Humeral Fractures
Key Facts
-
Eighty percent of distal humeral fractures occur in children.
-
Fifteen percent of physeal fractures in children involve the distal humerus.
-
The mechanism of injury is a fall on the outstretched hand.
-
Fractures may be flexion or extension injuries. Extension injuries are 10 times more common than flexion injuries.
-
Extension fracture: oblique fracture with posterior displacement of the distal fragment
-
Flexion fracture: older age group; transverse fracture line; distal fragment anterior
-
-
Fractures usually are obvious on AP and
lateral radiographs. CT with coronal and sagittal reformatting if
helpful for evaluating subtle injuries. MRI is useful for physeal
fractures in young children. -
Treatment: closed reduction
-
Complications: neurovascular injury, premature physeal closure, arthrosis, malunion, nonunion
 |
|
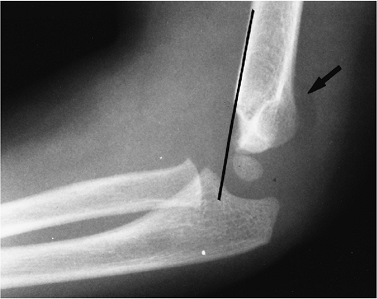
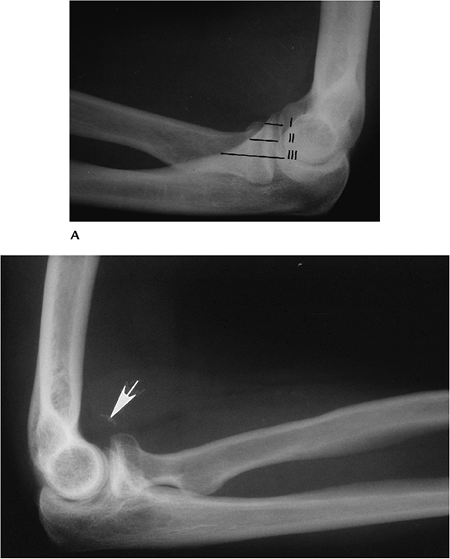
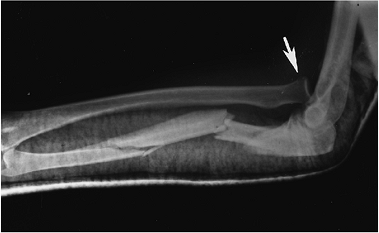
FIGURE 8-1 Distal humeral fracture. Lateral (A) and AP (B) radiographs of an extension supracondylar fracture. The distal fragment is displaced posteriorly (arrow).
|
P.514
 |
|
FIGURE 8-2 Supracondylar fracture line is not clearly seen, but the capitulum lies posterior to the anterior humeral line (black line),
indicating a fracture. The anterior humeral line should intersect the midcapitellum. There is also a positive posterior fat pad sign (arrow). |
Suggested Reading
Anderson SE, Otsuka NY, Steinbach LS. MR imaging of pediatric elbow trauma. Semin Musculoskel Radiol 1998;2:185–198.
Kinik H, Atalar H, Mergen E. Management of distal humeral fractures in adults. Arch Orthop Trauma Surg 1999;119:467–469.
Murphy BJ. MR imaging of the elbow. Radiology 1992;184:525–529.
P.515
Fractures/Dislocations: Epicondylar Fractures
Key Facts
-
Avulsion fractures of the epicondyle are common in children.
-
The injury is common in throwing athletes, specifically pitchers.
-
The medial epicondyle is particularly vulnerable between ages 9 and 14 years.
-
Mechanism of injury is varus and valgus forces. Medial epicondylar fractures are common; lateral epicondylar fractures are rare.
-
Displaced medial epicondylar fragments may be trapped in the joint.
-
Routine radiographs usually are adequate
for diagnosis. MRI is useful for subtle undisplaced fractures and
associated soft tissue injuries. -
Treatment: closed reduction for undisplaced fractures; pinning of displaced (>3 mm) fractures.
-
Complications: fragment entrapped in joint, instability.
 |
|
FIGURE 8-3 AP radiograph of the elbow in a young pitcher with an avulsed medial epicondyle (arrow).
|
P.516
Suggested Reading
Larson RL. Epiphyseal fractures in the adolescent athlete. Orthop Clin North Am 1973;4:839–851.
P.517
Fractures/Dislocations: Adult Distal Humeral Fractures
Key Facts
-
The distal humerus consists of medial and lateral columns with the trochlea between the two columns.
-
The mechanism of injury is trochlear
impaction into the humeral articular surface with flexor and extensor
muscles causing displacement of the epicondyles. -
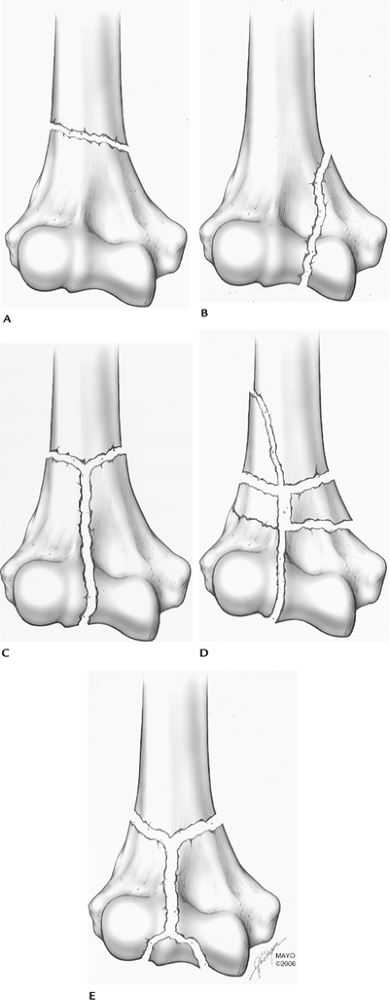
Fractures may be nonarticular, involve one condyle or have a “T” or “Y” configuration with varying degrees of comminution.
-
Treatment: internal fixation commonly required
-
Routine radiographs usually are diagnostic. CT with coronal and sagittal reformatting is important for operative planning.
-
Complications: poor reduction, exuberant
callus, reduced range of motion, arthrosis, nonunion (2%–10%), nerve
compression (15%), and postoperative infection.
 |
|
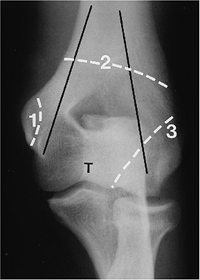
FIGURE 8-4 AP radiograph demonstrating the medial and lateral columns (black lines)
with the trochlea (T) between the columns. Fractures may be extra-articular (1), across both columns (2), or intra-articular (3) involving one or both columns. |
P.518
P.519
 |
|
FIGURE 8-5 Adult distal humeral fracture patterns. (A) Extra-articular. (B) One condyle. (C) Both condyles. (D,E) Both condyles with comminution.
|
P.520
 |
|
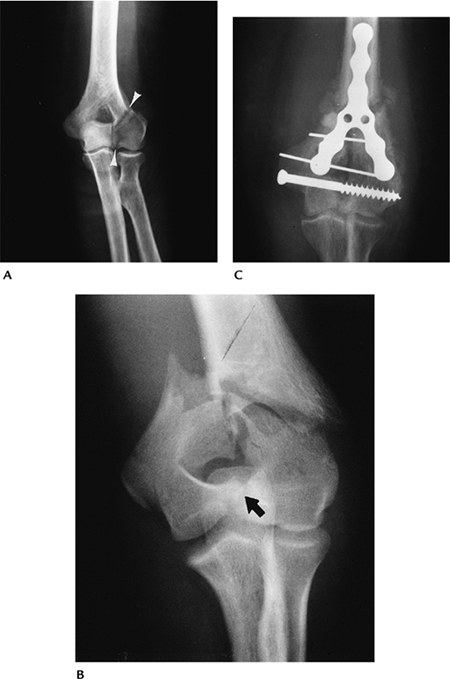
FIGURE 8-6 AP radiograph of a lateral column fracture entering the margin of the trochlea (arrowheads). (B) AP radiograph of an intra-articular “T” fracture. (C) AP radiograph after internal fixation of a “Y”-type fracture.
|
P.521
 |
|
FIGURE 8-7 CT images of a lateral column fracture reformatted in the coronal (A) and (B) sagittal planes.
|
Suggested Reading
Helfet
DL, Kloen P, Anand N, et al. Open reduction and internal fixation of
delayed unions and nonunions of fractures of the distal part of the
humerus. J Bone Joint Surg 2003;85A:33–44.
DL, Kloen P, Anand N, et al. Open reduction and internal fixation of
delayed unions and nonunions of fractures of the distal part of the
humerus. J Bone Joint Surg 2003;85A:33–44.
Ring D, Jupiter JB. Complex fractures of the distal humerus and their complications. J Shoulder Elbow Surg 1999;8:85–97.
P.522
Fractures/Dislocations: Capitellar Fractures
Key Facts
-
Capitellar fractures account for 1% of elbow injuries.
-
Fractures may involve the entire capitellum or the articular surface, or be comminuted and involve the radial head.
-
Mechanism of injury: direct blow or fall on the outstretched hand with force transmitted from the radius to the capitellum.
-
Subtle fractures may present with a positive fat pad sign and may require CT or MRI for detection.
-
Treatment: Loose fragments may require removal. K-wire fixation of large fragments may be necessary in certain cases.
 |
|
FIGURE 8-8 Lateral view of the elbow demonstrating a capitellar fracture (arrow) and displaced fat pad (open arrow).
|
Suggested Reading
Fowles JV, Dassab MT. Fractures of the capitellum humeria. J Bone Joint Surg 1975;56A:794–798.
P.523
Fractures/Dislocations: Fractures of the Proximal Radius
Key Facts
-
Fractures of the radial head and neck are
common, accounting for one third of elbow fractures. Fractures are
categorized as three types based on displacement or comminution of the
radial head or neck. Type I, undisplaced (<2 mm) head or neck
fracture; Type II, displaced head or neck fracture; Type III,
comminuted head or neck fracture. -
Mechanism of injury: Fall on the outstretched hand with the elbow partially flexed and pronated.
-
Associated elbow, forearm, and wrist injuries may be present.
-
Routine radiographs may be normal, except
for a positive fat pad sign. Follow-up in 10 to 14 days may demonstrate
the fracture. MRI or CT may be required for detection of subtle
fractures and for operative planning with complex fractures. -
Treatment: Undisplaced fractures are
treated with closed reduction. Displaced or comminuted fractures may
require internal fixation, resection, or arthroplasty. -
Complications include associated ulnar fracture, heterotopic ossification, instability, and arthrosis.
P.524
 |
|
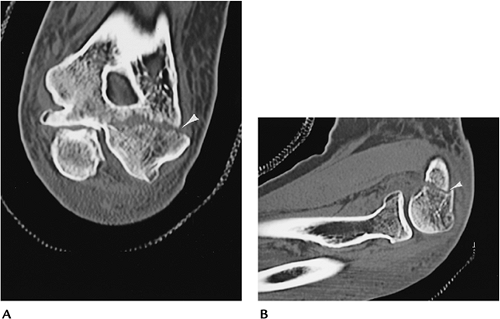
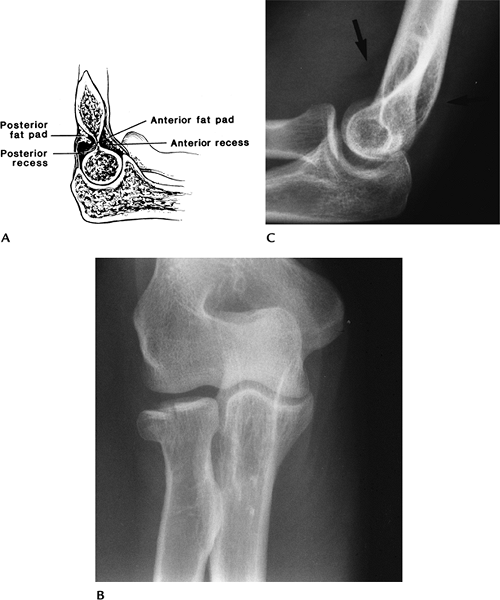
FIGURE 8-9 Fat pad sign. (A) Normal position of the fat pads. AP (B) and lateral (C) radiographs of a radial head fracture with displaced fat pads on the lateral view (arrows).
|
P.525
 |
|
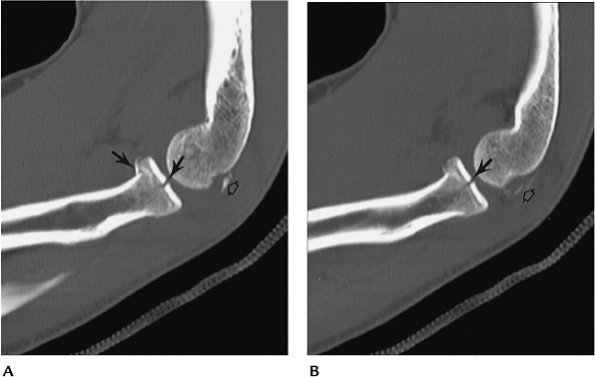
FIGURE 8-10 CT images in the sagittal plane (A,B) demonstrate a minimally displaced comminuted radial head fracture (arrows) with associated capitellar fragments (open arrow).
|
Suggested Reading
Corbett RH. Displaced fat pads in elbow trauma. Injury 1978;9:297–298.
Geel CW, Palmer AK. Radial head fractures and their effect on the radioulnar joint: A rationale for treatment. Clin Orthop 1992;275:79–84.
P.526
Fractures/Dislocations: Ulnar Fractures
Key Facts
-
The ulnar is susceptible to trauma because of its superficial location.
-
Mechanism of injury: direct blow after fall on the flexed elbow.
-
Most fractures are intra-articular.
-
Triceps fascia disruption leads to significant displacement and articular deformity.
-
Routine radiographs usually are diagnostic. The lateral view is most useful.
-
Treatment: Joint congruity must be restored, which usually requires internal fixation for displaced fractures.
-
Complications: instability, decreased
range of motion (3%–50%), articular deformity and arthrosis, ulnar
neuropathy (10%), and nonunion (5%).
 |
|
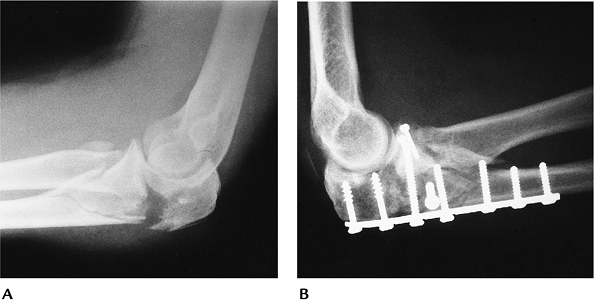
FIGURE 8-11 (A) Lateral view of the elbow showing a displaced olecranon and radial head fractures. (B) Fractures were internally fixed using plate and screw fixation.
|
Suggested Reading
Rettig AC, Waugh TR, Evanski PM. Fracture of the olecranon. A problem of management. J Trauma 1979;19:23–28.
P.527
Fractures/Dislocations: Coronoid Fractures
Key Facts
-
Isolated coronoid fractures are uncommon.
There are three categories of fracture. Type I: small avulsion of the
coronoid tip. Type II: fracture involves 50% of the coronoid, but does
not extend to the base. Type III: fracture of the coronoid base. -
Coronoid fractures are seen most commonly with posterior dislocations.
-
Recurrent dislocation is common after coronoid fracture/dislocation.
-
Displaced fractures can be detected on
radiographs. The lateral view is most useful. CT may be required for
detection of undisplaced fractures. -
Treatment: Closed reduction is adequate in most cases.
-
Complications: instability, arthrosis, recurrent dislocation.
P.528
 |
|
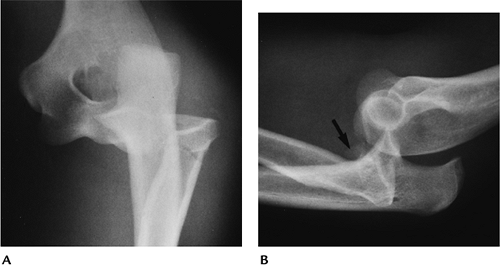
FIGURE 8-12 (A)
Lateral radiograph demonstrating the locations of Types I to III coronoid fractures. Lateral radiograph of the elbow after reduction of a posterior dislocation shows a small fragment from the coronoid tip (arrow) (Type I). |
Suggested Reading
Regan W, Morrey BF. Fractures of the coronoid process of the ulna. J Bone Joint Surg 1989;71A:1348–1354.
P.529
Fracture/Dislocations: Elbow Dislocations
Key Facts
-
Dislocation classifications refer to the position of the dislocation.
-
Most elbow dislocations are posterior and involve both the radius and ulna.
-
The mechanism of injury is a fall with the elbow extended.
-
Anterior, medial, and lateral dislocations are uncommon.
-
Associated injuries include coronoid, radial head, epicondylar fractures, and neurovascular injuries.
-
Postreduction CT imaging is important to fully assess the joint space and associated fractures.
-
Complications include arthrosis,
instability, decreased range of motion, neurovascular injury, and
extensive heterotopic ossification.
 |
|
FIGURE 8-13 AP (A) and lateral (B) radiographs of a posterolateral dislocation with associated fracture of the radial head (arrow) and neck.
|
Suggested Reading
Koyle SG. Posterior dislocations of the elbow. Clin Orthop 1991;269:201.
O’Driscoll SW, Morrey BF, Korinek S, et al. Elbow subluxations and dislocations: A spectrum of instability. Clin Orthop 1992;280:186–197.
Pugh
DMW, Wild LM, Schemitsch EH, et al. Standard surgical protocols for
treatment of elbow dislocations with radial head and coronoid
fractures. J Bone Joint Surg 2004;86A:1122–1130.
DMW, Wild LM, Schemitsch EH, et al. Standard surgical protocols for
treatment of elbow dislocations with radial head and coronoid
fractures. J Bone Joint Surg 2004;86A:1122–1130.
P.530
Fractures/Dislocations: Monteggia Fractures
Key Facts
-
Monteggia fracture or lesion is a dislocation of the radial head with an associated proximal ulnar fracture.
-
This injury accounts for only 7% of ulnar fractures and 0.7% of elbow injuries.
-
Four injury patterns are commonly described:
Type I Fracture of the ulna with anterior dislocation of the radial head (50%–75% of cases) Type II Fracture of the ulna with posterior or posterolateral radial head dislocation (10%–15% of cases) Type III Fracture of the ulna with lateral or anterolateral radial head dislocation (6%–20%; more common in children) Type IV Anterior dislocation with radial and ulnar fractures (5% of cases) -
Mechanism of injury: direct blow to posterior ulna, fall on the outstretched hand with elbow flexed, or hyperextension.
-
Routine radiographs are diagnostic. Keep in mind, the dislocation may reduce during radiographic positioning (20% of cases).
-
Treatment: Closed reduction in children; open reduction usually required in adults.
-
Complications: recurrent dislocation, arthrosis, nonunion, and neurovascular injury.
P.531
 |
|
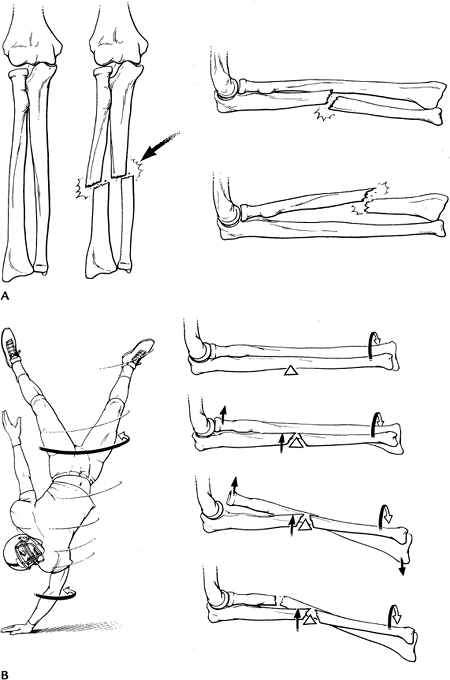
FIGURE 8-14 Monteggia fracture. (A) Oblique radiograph showing an anterior dislocation of the radial head with a proximal ulnar fracture. Postreduction AP (B) and lateral (C) radiographs with internal fixation of the ulnar fracture.
|
Suggested Reading
Bado J. The Monteggia lesion. Clin Orthop 1967;50:71–86.
P.532
Fractures/Dislocations: Forearm Fractures
Key Facts
-
Forearm fractures typically involve both
the radius and ulna (75%) or one osseous structure with dislocation at
the wrist or elbow. -
Mechanism of injury: direct blow or fall on the outstretched arm.
-
Fractures may be undisplaced, but muscle forces tend to cause angulation and rotation of fragments.
-
AP and lateral radiographs are
diagnostic. The elbow and wrist should be included to avoid overlooking
associated subluxation or dislocation. -
Treatment: Internal fixation commonly is required to prevent displacement.
-
Complications: reduced pronation and supination, nonunion, cross union, and neurovascular injuries.
P.533
 |
|
FIGURE 8-15 Forearm fracture. Mechanism of injury: direct blow in (A) and fall on the outstretched arm (B) with forces that tend to displace the fracture.
|
P.534
 |
|
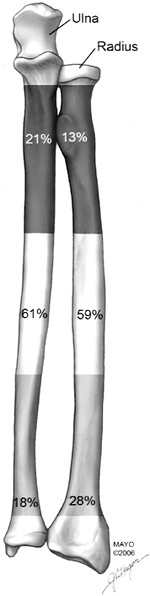
FIGURE 8-16 Incidence of proximal, mid-, and distal forearm fractures.
|
P.535
 |
|
FIGURE 8-17 Postreduction radiograph of a comminuted ulnar fracture with associated dislocation of the radial head.
|
Suggested Reading
Chapman
MW, Gordon JE, Zissimos AG. Compression plate fixation of acute forearm
fractures of the diaphysis of the radius and ulna. J Bone Joint Surg 1989;71A:159–169.
MW, Gordon JE, Zissimos AG. Compression plate fixation of acute forearm
fractures of the diaphysis of the radius and ulna. J Bone Joint Surg 1989;71A:159–169.
P.536
Osteochondritis Dissecans
Key Facts
-
Osteochondritis dissecans is common in adolescents, especially throwing athletes; 10% to 20% are bilateral.
-
Patients present with dull, aching pain in the involved elbow. Swelling and reduced motion are common.
-
The capitellum is most often involved.
-
Staging is important for treatment planning:
Stage I Intact cartilage with no displacement Stage II Fissure in articular cartilage with slight displacement Stage III Displaced -
Routine radiographs may not detect the
lesion and staging is difficult. MRI or magnetic resonance (MR)
arthrography is preferred for detection and staging. -
Treatment: conservative treatment for Type I; arthroscopic repair for Types II and III.
-
Complications: early arthrosis.
P.537
 |
|
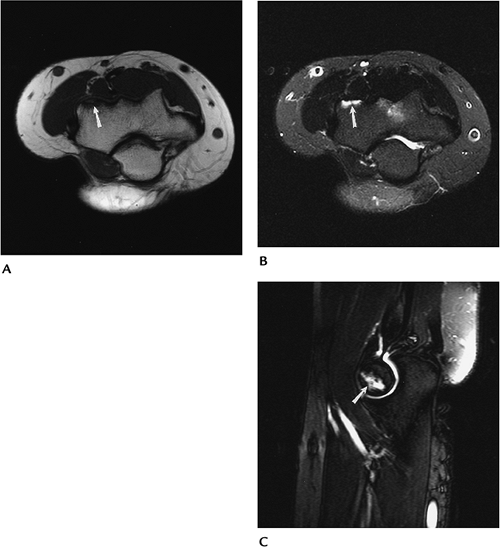
FIGURE 8-18 Axial T1- (A) and fast spin-echo T2-weighted (B) with fat suppression and sagittal fast spin-echo T2-weighted (C) fat-suppressed images demonstrate an undisplaced osteochondritis dissecans of the capitellum (arrow).
|
Suggested Reading
Herzog RJ. Magnetic resonance imaging of the elbow. Magn Reson Q 1993;9:188–210.
Kijowski R, De Smet AA. Radiography of the elbow of patients with osteochondritis dissecans of the capitellum. Skel Radiol 2005;34:266–271.
P.538
Soft Tissue Trauma: Biceps Tendon
Key Facts
-
The biceps tendon is the most commonly injured tendon of the elbow. Injuries are more common in men aged more than 40 years.
-
Injuries are most common at the radial tuberosity after catching a heavy weight with the elbow flexed and supinated.
-
Patients present with acute pain, fullness, and ecchymosis in the antecubital fossa.
-
Chronic microtrauma may result in
degeneration, partial tears, bursitis, or ganglion formation.
Bicipitoradial bursitis (55%) and micro bone avulsion (50%) are common
with partial tears. -
Imaging of biceps tendon pathology may be accomplished with routine radiographs, ultrasound, or MRI.
-
Radiographs: Irregularity of the radial tuberosity.
-
Ultrasound: Abnormal echo texture or cyst in case of ganglion.
-
MRI: T2-weighted images show increased signal in tendon or disruption. Ganglion cysts are well-defined, high-intensity masses.
-
Treatment: Operative intervention is
often required for complete tears, partial tears with 30% to 40%
function loss and ganglion cysts.
 |
|
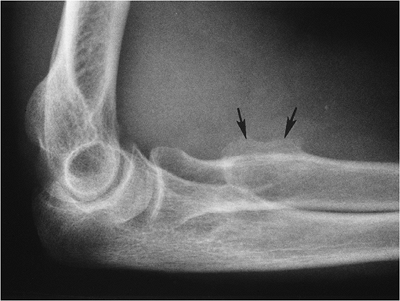
FIGURE 8-19 Lateral radiograph showing irregularity of the radial tuberosity (arrows) caused by chronic microtrauma.
|
P.539
 |
|
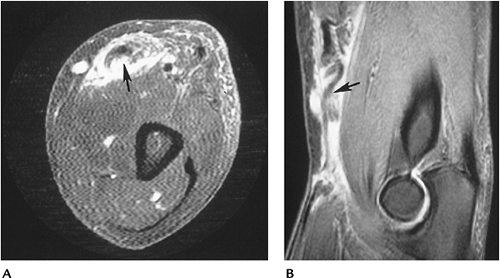
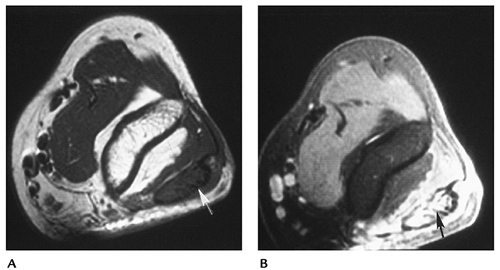
FIGURE 8-20 Biceps tendon tear. Axial (A) and sagittal (B) T2-weighted images of a biceps tendon tear (arrow) with retraction and surrounding hemorrhage and edema.
|
Suggested Reading
Chew ML, Giuffre BM. Disorders of the distal biceps brachii tendon. Radiographics 2005;25:1227–1237.
Fitzgerald SW, Curry DR, Erickson SJ, et al. Distal biceps tendon injury. MR imaging diagnosis. Radiology 1994;191:203–206.
P.540
Soft Tissue Trauma: Triceps Tendon Injuries
Key Facts
-
Inflammation of the triceps tendon is common, but tendon ruptures are rare.
-
Triceps ruptures occur with deceleration forces while the triceps is contracted.
-
Triceps tears are more common in patients with systemic diseases or patients on steroid therapy.
-
Imaging of triceps injuries can be accomplished using radiographs, ultrasound, or MRI.
-
Radiographs: Up to 80% of triceps injuries have an avulsed olecranon fragment visible on the lateral view.
-
Ultrasound: Abnormal echo texture or loss of tendon substance with complete disruption.
-
MRI: T2-weighted or short TI inversion
recovery (STIR) sequences show increased signal intensity in tendon
(varies with extent of tear). Axial and sagittal image planes are most
useful. -
Treatment of inflammatory and partial tears may be conservative. Complete tears are corrected surgically.
 |
|
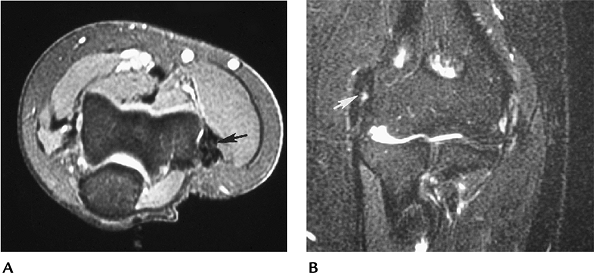
FIGURE 8-21 Axial T1- (A) and T2- (B) weighted images showing abnormal signal intensity and thickening of the triceps (arrow) caused by a high-grade tear.
|
Suggested Reading
Tiger E, Mayer DP, Glazer R. Complete avulsion of the triceps tendon. MRI diagnosis. Comput Med Imaging Graphics 1993;17:51–54.
P.541
Soft Tissue Trauma: Flexor/Extensor Tendon Injuries
Key Facts
-
Tendinopathy or tears of the flexor or extensor tendons are common.
-
Injury to the common extensor tendon
(lateral epicondylitis, tennis elbow) is common with repetitive
microtrauma. Injury most commonly involves extensor carpi radialis
brevis origin. Lateral epicondylitis affects 50% of throwing athletes,
and 50% of tennis players aged more than 30 years will develop symptoms. -
Injury to the common medial flexor tendon
occurs less frequently. The injury usually involves the flexors and
pronator teres. The syndrome occurs in 1% to 3% of adults, especially
golfers and throwing athletes. -
Four stages of epicondylitis have been described by Kraushaar and Nirschl.
-
Stage 1: inflammatory, resolves
-
Stage 2: tendinosis and angiofibroblastic degeneration
-
Stage 3: tendinosis with rupture
-
Stage 4: a combination of 2 and 3 plus scarring and calcification
-
-
Ultrasound or MRI is most useful when
imaging studies are performed. Axial and coronal T2-weighted or STIR
images are most useful. -
Treatment of most tendinopathies is conservative. Partial or complete tears in athletes may require surgical repair.
 |
|
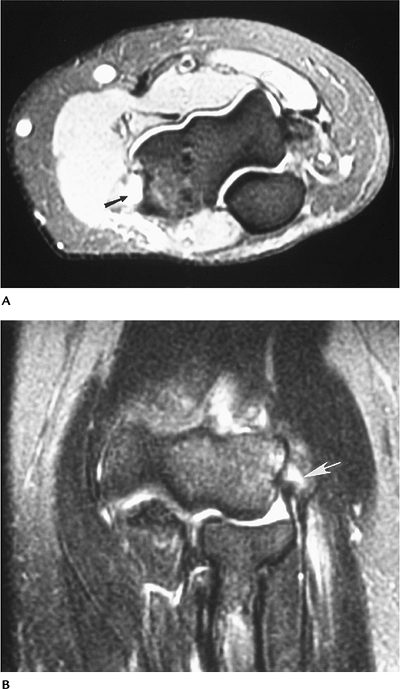
FIGURE 8-22 Extensor tendinopathy. Axial (A) and coronal (B) T2-weighted images showing tendon thickening and abnormal signal intensity (arrow) in the extensor tendon.
|
P.542
 |
|
FIGURE 8-23 Partial tear of the common extensor origin. Axial (A) and coronal (B) T2-weighted images showing increased signal intensity (arrow) resulting from a partial tear.
|
P.543
Suggested Reading
Kijowski R, DeSmet AA. Magnetic resonance imaging findings in patients with medial epicondylitis. Skel Radiol 2005;34:196–202.
Kraushaar BS, Nirschl RL. Tendinosis of the elbow (tennis elbow). J Bone Joint Surg 1999;81A:259–278.
Struijs
PAA, Spruyt M, Assendelft WJJ, et al. The predictive value of
diagnostic sonography for effectiveness of conservative treatment of
tennis elbow. AJR Am J Roentgenol 2005;185:1113–1118.
PAA, Spruyt M, Assendelft WJJ, et al. The predictive value of
diagnostic sonography for effectiveness of conservative treatment of
tennis elbow. AJR Am J Roentgenol 2005;185:1113–1118.
P.544
Soft Tissue Trauma: Muscle Injuries
Key Facts
-
Muscle injuries to the upper extremity are infrequent compared with injuries to the lower extremity.
-
Muscle strains usually are stretch injuries resulting from eccentric overload.
-
MRI is most useful for detection and
staging (partial, complete) of muscle injuries. Axial and coronal or
sagittal T2-weighted or STIR sequences show increased signal intensity
in the involved muscle. -
Treatment is conservative for partial tears. Surgery may be required for complete tears.
 |
|
FIGURE 8-24 Anconeus strain. Axial T2-weighted image of the elbow showing increased signal intensity (arrow) resulting from repetitive microtrauma.
|
Suggested Reading
Herzog RJ. Magnetic resonance imaging of the elbow. Magn Reson Q 1993;9:188–210.
P.545
Soft Tissue Trauma: Ligament Injuries
Key Facts
-
The radial and ulnar collateral ligaments provide important support for elbow stability.
-
The ulnar collateral ligament complex is
most important for stability. Injuries usually occur when valgus force
is applied to the elbow. Such injuries are commonly seen in athletes
involved in throwing sports or javelin throwing. Causes of medial elbow
pain in throwing athletes include:-
Medial tendon overuse
-
Flexor/pronator muscle tears
-
Ulnar collateral ligament tears
-
Avulsion of the coronoid tubercle
-
Posteromedial impingement
-
Ulnar neuropathy
-
Ulnar nerve subluxation
-
Medial antebrachial cutaneous nerve injury
-
-
Radial collateral ligament injuries occur less frequently. Injuries are the result of varus stress.
-
Imaging can be accomplished with
conventional arthrography, ultrasound, MRI, or MR arthrography. The
anterior band of the ulnar collateral ligament is optimally imaged in
the coronal plane. The transverse band is less clinically significant
and sometimes absent. This may be difficult to identify on MR images. -
Treatment: Partial tears may be treated conservatively. Complete tears may require surgical intervention.
P.546
 |
|
FIGURE 8-25 Radial collateral ligament tear. AP radiograph of an elbow arthrogram showing contrast extravasation (arrow) resulting from ligament disruption.
|
P.547
 |
|
FIGURE 8-26
Partial tear of the anterior band of the ulnar collateral ligament. Coronal T2-weighted image showing increased signal intensity about and in the ligament (arrow) resulting from a partial tear. |
Suggested Reading
Carrino
JA, Morrison WB, Zon KH, et al. MR imaging and MR arthrography of the
ulnar collateral ligament of the elbow: Prospective evaluation of
2-dimensional pulse sequences for detection of complete tears. Skel Radiol 2001;30:625–632.
JA, Morrison WB, Zon KH, et al. MR imaging and MR arthrography of the
ulnar collateral ligament of the elbow: Prospective evaluation of
2-dimensional pulse sequences for detection of complete tears. Skel Radiol 2001;30:625–632.
Cotton
A, Jacobson J, Brossmann J, et al. Collateral ligaments of the elbow.
Conventional MR imaging and MR arthrography with oblique coronal plane
and elbow flexion. Radiology 1997;204:806–812.
A, Jacobson J, Brossmann J, et al. Collateral ligaments of the elbow.
Conventional MR imaging and MR arthrography with oblique coronal plane
and elbow flexion. Radiology 1997;204:806–812.
Ward
SI, Teefey SA, Paletta GA, et al. Sonography of the medial collateral
ligament of the elbow: A study of cadavers and healthy male volunteers.
AJR Am J Roentgenol 2002;180:389–394.
SI, Teefey SA, Paletta GA, et al. Sonography of the medial collateral
ligament of the elbow: A study of cadavers and healthy male volunteers.
AJR Am J Roentgenol 2002;180:389–394.
P.548
Neoplasms: Bone Tumors
Key Facts
-
Osseous neoplasms of the elbow are rare.
-
Characterization of lesions is accomplished most easily with routine radiographs.
-
CT or MRI is most useful for staging of lesions.
-
Table 8-2 summarizes malignant and benign osseous neoplasms in the elbow and forearm.
 |
|
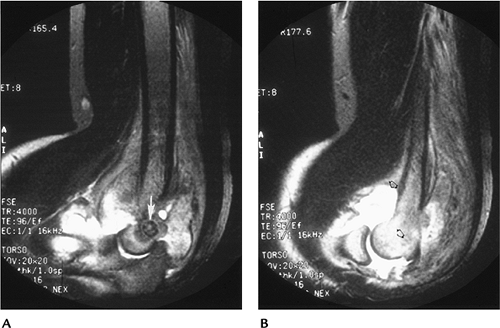
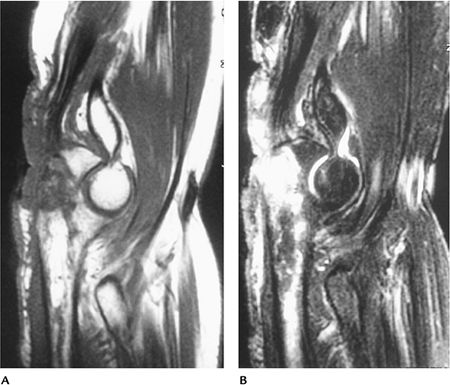
FIGURE 8-27 Osteoid osteoma. Sagittal fast spin-echo fat-suppressed T2-weighted images (A,B) showing an osteoid osteoma (arrow in A). There is edema and a large reactive joint effusion (open arrows), typical of osteoid osteoma.
|
P.549
|
TABLE 8-2 SKELETAL NEOPLASMS OF THE ELBOW AND FOREARM
|
||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Suggested Reading
Unni KK. Dahlin’s bone tumors: General aspects and data on 11,087 cases. 5th ed. Philadelphia: Lippincott-Raven; 1996.
P.550
Neoplasms: Soft Tissue Tumors
Key Facts
-
Soft tissue tumors are most effectively identified and categorized with MRI.
-
As a general rule, benign lesions are well defined, with homogeneous signal intensity.
-
Malignant tumors are inhomogeneous,
especially on T2-weighted sequences; have irregular margins; and may
encase neurovascular structures and bone. -
Intravenous gadolinium is useful to
define cysts (do not enhance) and areas of necrosis. We routinely use
contrast-enhanced fat-suppressed T1-weighted images in patients with
neoplasms.
 |
|
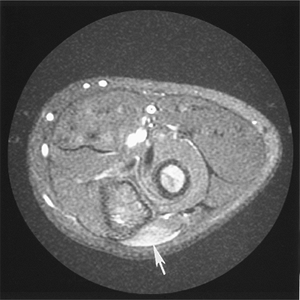
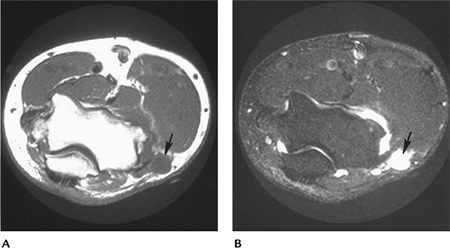
FIGURE 8-28 Ganglion cyst. Axial T1- (A) and T2- (B) weighted images showing a benign cyst (arrow) with uniform increased intensity on T2-weighted and low signal intensity on T1-weighted sequences.
|
P.551
 |
|
FIGURE 8-29 Malignant fibrous histiocytoma. Axial T1- (A) and T2-weighted (B) images of this malignant lesion. Signal inhomogeneity is most easily appreciated on the T2-weighted image (B).
|
Suggested Reading
Berquist TH. Magnetic resonance imaging of musculoskeletal neoplasms. Clin Orthop 1989;244:101–118.
P.552
Infection
Key Facts
-
Musculoskeletal infections may present as an acute or insidious process.
-
Skeletal infections typically present in medullary bone with hyperemia and edema.
-
Soft tissue infections may be diffuse or result in more localized abscess formation.
-
Joint space infections may present with soft tissue changes, joint effusion, or joint and bone involvement.
-
Routine radiographs usually are normal
early, except for soft tissue swelling. MRI is most useful for early
detection and evaluation of bone and soft tissue involvement.
 |
|
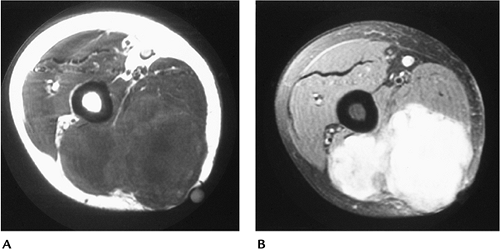
FIGURE 8-30 Soft tissue abscess. Sagittal T2-weighted (A) and post–gadolinium-enhanced fat-suppressed (B) images showing a large nonenhancing fluid collection.
|
P.553
 |
|
FIGURE 8-31 Sagittal T1- (A) and T2-weighted (B) images demonstrate diffuse soft tissue edema and abnormal signal intensity in the ulna due to osteomyelitis.
|
Suggested Reading
Berquist TH, Broderick DF. Musculoskeletal infection. In: Berquist TH, ed. MRI of the musculoskeletal system. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2006:916–947.
P.554
Arthropathies
Key Facts
-
Arthropathies involving the elbow include
degenerative arthritis secondary to trauma and systemic arthropathies,
such as rheumatoid arthritis, hemophiliac arthropathy, gout, and
arthropathy secondary to dialysis. -
Routine radiographs remain the primary screening technique for detection and characterization of arthropathies.
-
Radionuclide scans and MRI detect changes
earlier than radiographs. Intravenous gadolinium studies show changes
in articular cartilage and synovial pathology more readily.
 |
|
FIGURE 8-32 Rheumatoid arthritis. AP radiograph showing joint space narrowing and erosive changes.
|
P.555
P.556
 |
|
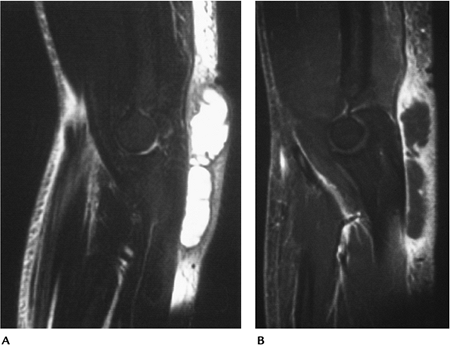
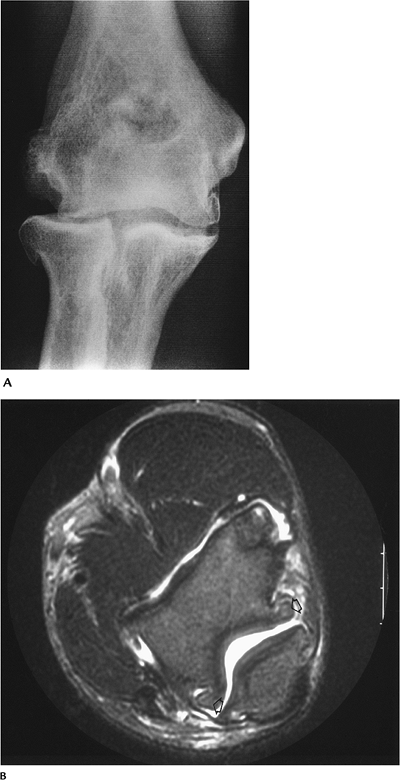
FIGURE 8-33 Osteoarthritis. (A) AP radiograph showing bone sclerosis and osteophytes typical of osteoarthritis. (B) Axial T2-weighted MR image showing a joint effusion with osteophytes (open arrows).
|
P.557
 |
|
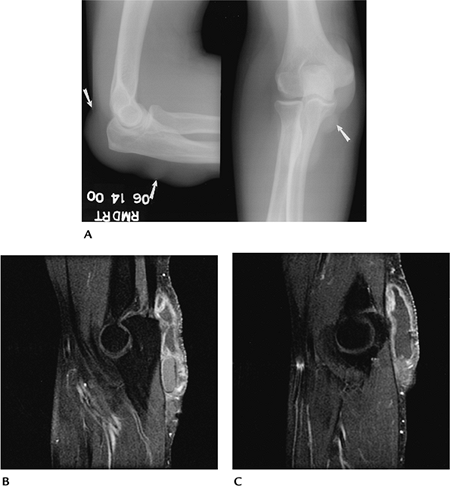
FIGURE 8-34 Gout. (A) AP and lateral radiographs demonstrate prominent nodular swelling (arrows). Sagittal (B,C)
post-contrast fat-suppressed T1-weighted images demonstrate enhancement of the distended bursal lining caused by gouty inflammation. |
Suggested Reading
Brower AC. Arthritis in black and white. 2nd Ed. Philadelphia: WB Saunders; 1997:325–342.
P.558
Nerve Entrapment Syndromes
Key Facts
-
Nerve compression or entrapment syndromes fall into four categories:
-
First degree (neurapraxic): Conduction defects with no structural abnormalities evident. Cause may be blunt trauma or ischemia.
-
Second degree (axonometric): Disruption of nerve fibers with connective tissue intact. Regeneration can occur.
-
Third/fourth degree: Complete motor and sensory loss.
-
-
Cause of nerve compression syndromes
about the elbow varies to some degree depending on the nerve involved
(ulnar, median, or radial).-
Ulnar Nerve:
-
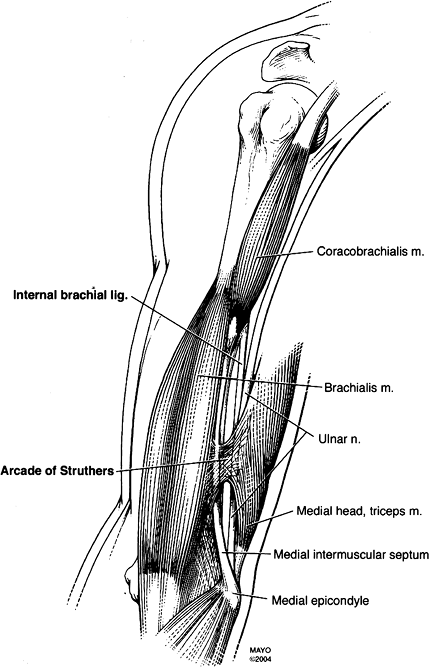
The nerve passes from anterior to posterior through the arcade of Struthers (Fig. 8-35). At the elbow the nerve lies posterior to the medial epicondyle before entering the cubital tunnel (Fig. 8-36). Causes of ulnar nerve compression include:
-
Fibrous adhesions
-
Muscle anomalies (anconeus epitrochlearis)
-
Absent cubical retinaculum (10%)
-
Thickened cubical retinaculum
-
Thickened ulnar collateral ligament
-
Vascular anomalies
-
Bursitis
-
Myotendinous inflammation
-
Ganglion cysts
-
Inflammatory arthropathies
-
Neoplasms
-
Prior fractures
-
Loose bodies
-
-
-
Median Nerve:
-
The median nerve lies beneath the
brachialis muscle accompanied by the brachial artery and vein and
biceps tendon. Median nerve compression occurs at the supracondylar
process and ligament of Struthers. Fractures of the humerus and elbow
commonly injure the median nerve. The median nerve may also be
compressed between the two heads of the pronator muscle (pronator
syndrome). Patients present with anterior elbow pain and tingling in
the median nerve distribution.
-
-
Radial Nerve:
-
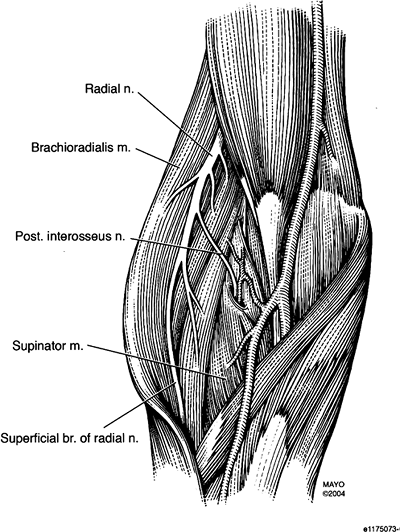
The radial nerve takes an anterior course 10 cm above the lateral epicondyle (Fig. 8-37)
dividing into superficial and posterior interosseous branches. The
radial nerve is vulnerable to compression from the lateral head of the
triceps to the distal forearm. More proximally, radial nerve injury is
associated with humeral fractures. Causes of radial nerve compression
include:
-
-
-
Imaging of soft tissue and neural structures is accomplished most easily with MRI.
 |
|
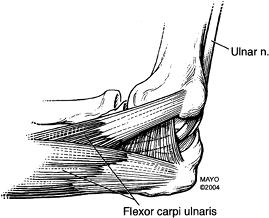
FIGURE 8-35 Ulnar nerve in the arm and the arcade of Struthers.
|
 |
|
FIGURE 8-36 Ulnar nerve in the cubital tunnel.
|
P.560
 |
|
FIGURE 8-37 Radial and posterior interosseous nerves.
|
P.561
 |
|
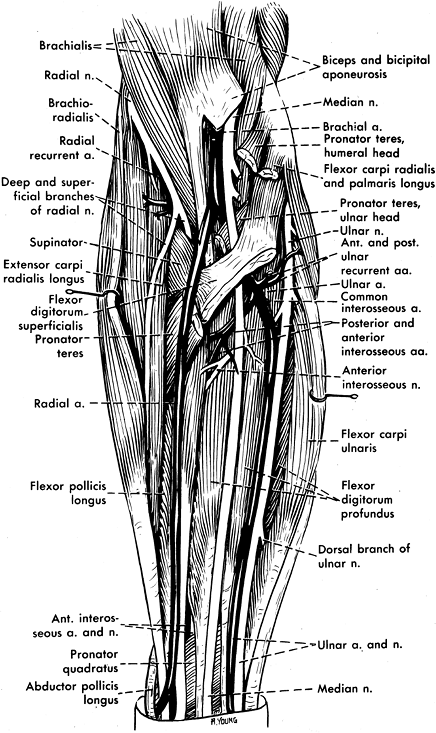
FIGURE 8-38 Neurovascular anatomy of the elbow and forearm.
|
P.562
 |
|
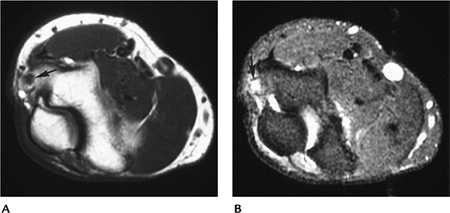
FIGURE 8-39 Ulnar neuritis. Axial T1- (A) and T2- (B) weighted images showing an enlarged ulnar nerve (arrow) with increased signal intensity on T2-weighted image (B).
|
Suggested Reading
Beltran J, Rosenberg ZS. Diagnosis of compression and entrapment neuropathies of the upper extremity. Value of MR imaging. AJR Am J Roentgenol 1994;163:525–531.
Major N. Magnetic resonance imaging of the elbow. Curr Probl Diagn Radiol 2000;1:27–40.
O’Driscoll SW, Horii E, Carmichael S, et al. The cubital tunnel and ulnar neuropathy. J Bone Joint Surg 1991;73A:613–617.
