Continuous Lumbar Plexus Blocks
VI – Continuous Nerve Blocks in Infants and Children > 59 –
Continuous Lumbar Plexus Blocks
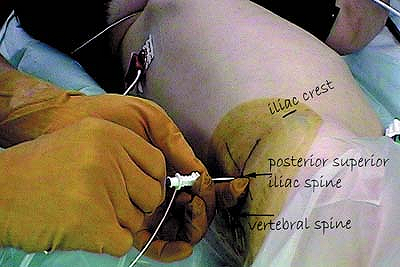
The highest point on the iliac crest is identified. A line is drawn
from this point to the spine processes (SP). The posterior superior
iliac spine (PSIS) is identified. A parasagital line to the vertebral
spine is drawn passing through the posterior superior iliac spine. The
intersection of these two lines is the point of insertion of the
introducer needle (Figs. 59-2, 59-3).
The needle is introduced perpendicular to the skin or lightly directed
posteriorly in an appropriately anesthetized/sedated child. After bone
contact with the transverse process of L4 or L5, the needle is
redirected to the cranial or caudal direction (angle between 30 and 45
degrees) and 1 cm deeper until a contraction of the quadriceps (femoral
n.) is elicited. With an appropriate muscle response still present at a
current of 0.5 mA and after negative aspiration for blood the
appropriate amount of local anesthetic solution is slowly injected.
Maintaining the introducer needle in the same
position,
the catheter is threaded 2 cm beyond the needle tip. The introducer
needle is removed and the catheter is secured in place with benzoin and
a transparent adhesive dressing. Blood pressure has to be monitored
because of a possible epidural or subarachnoid injection. The absence
of epidural spread is assessed by the presence of an adequate reaction
to pinprick of the opposite leg after emergence.
 |
|
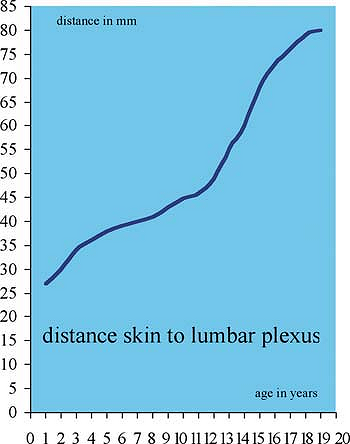
Figure 59-1. Distance skin to lumbar plexus.
|
-
This block should only be performed by an anesthesiologist trained in pediatric regional techniques.
-
The technique described above is Winnie’s
approach; we do not use Chayen’s approach because of a higher incidence
of epidural spread reported in the literature. -
The shortest needle that can easily reach
the plexus has to be used because of the potential risk of visceral
organ (kidney) puncture. -
Ultrasound guidance can help to determine the depth of the lumbar plexus.
-
Peritoneal or visceral infection, trauma
to the lumbar spine, lumbar vertebral deformities, and coagulopathy are
contraindications for this block. -
A slow injection (1 mL/10 seconds) of the local anesthetic is advised.
-
The absence of epidural spread is
assessed by the presence of an adequate reaction to a pinprick of the
opposite leg after emergence from anesthesia. -
A stimulating catheter can be used in older children.
|
Table 59-1. Maximum Initial Bolus Volume of Ropivacaine 0.2%—Psoas Compartment Approach
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
Figure 59-2. Lumbar plexus landmarks.
|
 |
|
Figure 59-3. Lumbar plexus catheter placement.
|
C, Pirat Ph, Raux O, et al. Perioperative continuous peripheral nerve
blocks with disposable infusion pumps in children: A prospective
descriptive study. Anesth Analg 2003;97:687–690.
C, Raux O, Gaudard P, et al. Continuous psoas compartment blocks after
major orthopedic surgery in children: a prospective computed
tomographic scan and clinical studies. Anesth Analg 2004;98(3):623–628.
D, Matuszczak M, Gebhard R, et al. Continuous posterior lumbar plexus
block for acute postoperative pain control in young children. Anesthesiology 2001;95:1521–1523.
Preoperative analgesia for fractured femur with leg in traction.
Anesthesia and postoperative analgesia for femur and knee surgery;
postoperative physiotherapy and complex regional pain syndrome.
The insertion point is lateral to the femoral artery pulse and 1 to 3
cm below the inguinal ligament. The introducer needle is advanced
parallel to the femoral artery in an appropriately anesthetized/sedated
child. When a contraction of the vastus intermedius is elicited and
still present at 0.5 mA, the appropriate dose of local anesthetic is
slowly injected after negative aspiration for blood. Maintaining the
introducer needle in the same position, the catheter is threaded 2 cm
beyond the needle tip. The introducer needle is removed and the
catheter is secured in place with benzoin and a transparent adhesive
dressing (Figs. 59-5, 59-6).
-
A femoral nerve block can be performed
with the leg in many positions as long as it is possible to locate the
femoral artery and the inguinal ligament. -
The catheter should not be thread more than 3 cm.
-
Easy block to perform even outside the operative room.
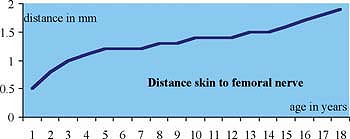 Figure 59-4. Distance skin to femoral nerve.P.388Table 59-2. Maximum Initial Bolus Volume of Ropivacaine 0.2%—Continuous Femoral Nerve Block
Figure 59-4. Distance skin to femoral nerve.P.388Table 59-2. Maximum Initial Bolus Volume of Ropivacaine 0.2%—Continuous Femoral Nerve Blockkg 2–10 kg 15 kg 20 kg 25 kg 30 kg 40 kg 50 kg 60 kg 70 kg mL 1 mL/kg 10 mL 12 mL 15 mL 15 mL 17.5 mL 20 mL 20 mL 25 mL -
This block is perfectly indicated for femur fracture with the leg in traction.
-
Ultrasound can be used to localize the
femoral nerve, to position the needle, and to verify that the local
anesthetic is injected via the catheter around the nerve. -
A stimulating catheter can be used in older children.
 |
|
Figure 59-5. Femoral nerve block landmarks.
|
 |
|
Figure 59-6. Femoral catheter placement.
|
Preoperative analgesia for fractured femur with leg in traction.
Anesthesia and postoperative analgesia for femur and knee surgery;
postoperative physiotherapy and complex regional pain syndrome.
The anterior iliac spine and the pubic tubercle are identified. A line
is drawn between these two landmarks, demarcating the inguinal
ligament. The junction of the lateral third and the medial two-thirds
of this line is marked. The insertion point of the needle is 0.5 cm to
1.0 cm caudally to the junction marked and lateral to the femoral
artery. The needle is introduced perpendicular to the skin. A first
loss of resistance is felt when the needle passes through the fascia
lata, and a second loss of resistance is felt when the needle passes
through the fascia iliaca. After negative aspiration for blood the
appropriate volume of local anesthetic is slowly injected. Maintaining
the introducer needle in the same position, the catheter is threaded 2
cm beyond the needle tip. The introducer needle is removed and the
catheter is secured in place with benzoin and a transparent adhesive
dressing (Fig. 59-8).
-
Easy block to perform by beginners.
-
The nerve stimulator is not needed, no painful movements of fractured extremity.
-
In children, according to the literature, the fascia iliaca block has a greater success rate compared to the femoral block.
 |
|
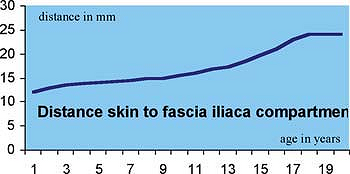
Figure 59-7. Distance skin to fascia iliaca compartment.
|
|
Table 59-3. Maximum Initial Bolus Volume of Ropivacaine 0.2%—Continuous Fascia Iliaca Compartment Block
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
Figure 59-8. Fascia iliaca landmarks.
|
C, Pirat Ph, Raux O, et al. Perioperative continuous peripheral nerve
blocks with disposable infusion pumps in children: a prospective
descriptive study. Anesth Analg 2003;97:687–690.
O, Sallabery M, Schreiber-Deturmeny E, et al. Continuous fascia iliaca
compartment block in children: a prospective evaluation of plasma
bupivacaine concentrations, pain scores, and side effects. Anesth Analg 2001;92:1159–1163.
