Continuous Terminal Nerve Blocks
Editors: Chelly, Jacques E.
Title: Peripheral Nerve Blocks: A Color Atlas, 3rd Edition
Copyright ©2009 Lippincott Williams & Wilkins
> Table of Contents > Section
VI – Continuous Nerve Blocks in Infants and Children > 58 –
Continuous Terminal Nerve Blocks
VI – Continuous Nerve Blocks in Infants and Children > 58 –
Continuous Terminal Nerve Blocks
58
Continuous Terminal Nerve Blocks
Maria Matuszczak
A. Continuous Axillary Blocks
The axillary artery in the axilla crease is identified. The insertion
point is directly next to the artery at the lateral border of the
axillary crease.
In an appropriately anesthetized/sedated child the needle is inserted
directly next to the artery, pointing almost parallel to the artery in
a proximal direction with a 30° to 45° angle to the skin. As
appropriate muscle twitches in the hand are still present at a current
of 0.5 mA, the local anesthetic solution is slowly injected after
negative aspiration for blood. Maintaining the introducer needle in the
same position, the catheter is threaded 2 cm beyond the needle tip (Fig. 58-2). The introducer needle is removed and the catheter is secured in place with benzoin and a transparent adhesive dressing.
P.382
 |
|
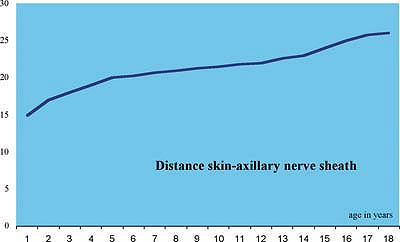
Figure 58-1. Skin–nerve distance, axillary approach.
|
-
At this level, there are no vital structures and it is a perfect approach for beginners in pediatric peripheral nerve blocks.
-
By introducing the needle more distally
from the axilla crease, the catheter can be placed close to a specific
nerve that needs to be anesthetized. -
Because of shoulder mobility the axillary catheter is easily dislocated.
-
To prevent easy dislocation, the catheter
can be tunneled by inserting a longer needle subcutaneously at the
midhumeral level toward the axillary crease. Only when the needle is
close to the axillary crease, look for nerve stimulation. -
In obese children, ultrasound guidance facilitates this approach.
-
This approach can be used to rescue an
incomplete continuous infraclavicular block. Ulnar distribution is
sometimes missed by the infraclavicular approach. -
Ultrasound can be used to localize the
axillary nerves, to position the needle, and to verify that the local
anesthetic is injected via the catheter around the nerves. -
A stimulating catheter can be used in older children.
 |
|
Figure 58-2. Axillary catheter placement.
|
P.383
|
Table 58-1. Maximal Initial Volume Bolus of Ropivacaine 0.2%
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Suggested Readings
Dadure C, Capdevila X. Continuous peripheral nerve blocks in children. Best Pract Res Clin Anaesthesiol 2005;19(2):309–321.
Dadure
C, Pirat Ph, Raux O, et al. Perioperative continuous peripheral nerve
blocks with disposable infusion pumps in children: A prospective
descriptive study. Anesth Analg 2003;97:687–690.
C, Pirat Ph, Raux O, et al. Perioperative continuous peripheral nerve
blocks with disposable infusion pumps in children: A prospective
descriptive study. Anesth Analg 2003;97:687–690.
Dalens B. Regional anesthesia in infants, children, and adolescents. Baltimore: Williams & Wilkins, 1995.
De la Linde CM, Polo A, Lopez-Andrade A. Continuous axillary plexus block in pediatrics. Rev Esp Anesthesiol Reanim 1997;44:87–88.
Diwan R, Vas L, Shah T. Continuous axillary block for upper limb surgery in a patient with epidermolysis bullosa simplex. Paediatr Anaesth 2001;11:603–606.
Ivani G, Mossetti V. Continuous peripheral nerve blocks. Paediatr Anaesth 2005;15:87–90.
Marhofer P, Frickey N. Ultrasonographic guidance in pediatric regional anesthesia. Part 1: theoretical background. Paediatr Anaesth 2006;16(10):1008–1018.
Mezzatesta
JP, Scott DA, Schweitzer SA, et al. Continuous axillary brachial plexus
block for postoperative pain relief: intermittent bolus versus
continuous infusion. Reg Anesth 1997;22:357–362.
JP, Scott DA, Schweitzer SA, et al. Continuous axillary brachial plexus
block for postoperative pain relief: intermittent bolus versus
continuous infusion. Reg Anesth 1997;22:357–362.
Roberts S. Ultrasonographic guidance in pediatric regional anesthesia. Part 2: techniques. Paediatr Anaesth 2006;16:1125–1132.
