Continuous Brachial Plexus Blocks
Editors: Chelly, Jacques E.
Title: Peripheral Nerve Blocks: A Color Atlas, 3rd Edition
Copyright ©2009 Lippincott Williams & Wilkins
> Table of Contents > Section
VI – Continuous Nerve Blocks in Infants and Children > 57 –
Continuous Brachial Plexus Blocks
VI – Continuous Nerve Blocks in Infants and Children > 57 –
Continuous Brachial Plexus Blocks
57
Continuous Brachial Plexus Blocks
Maria Matuszczak
Didier Sciard
A. Interscalene Approach
Supine, with the head slightly turned away from the side where the
block is performed, and the arm extended along the side of the body.
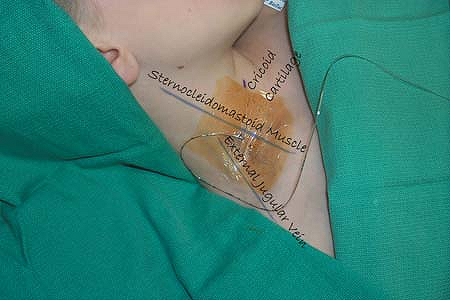
The lateral border of the sternocleidomastoid muscle is identified and
marked. Posteriorly, the groove between the anterior and the middle
scalene muscle is identified. Next, a line is drawn at the level of the
cricoid cartilage. At the intersection of these two lines, the brachial
plexus will be found in the interscalene groove.
The insertion point should be high in the interscalene groove. In an
appropriately anesthetized/sedated child, the insulated introducer
Tuohy needle, connected to a nerve stimulator (1.5 mA, 2 Hz, 0.1 ms),
is positioned parallel to the neck, close to the external jugular vein
and directed anteriorly to the interscalene groove. After appropriate
positioning of the needle to maintain the muscle response with a
current of 0.5 mA, the local anesthetic solution is slowly injected
after negative aspiration for blood. Maintaining the insulated
introducer needle in the same position, the catheter is threaded 2 cm
beyond the needle tip. The Tuohy needle is removed, and the catheter is
P.376
secured in place with Steri-Strip (3M, St. Paul, MN) and covered with a transparent dressing (Fig. 57-2).
 |
|
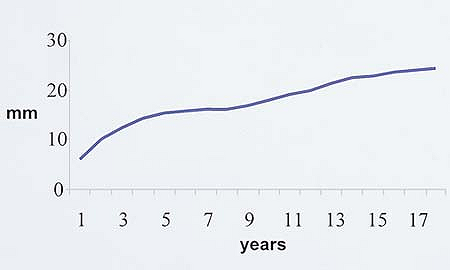
Figure 57-1. Skin–nerve distance.
|
-
The site of introduction of the needle is often lateral and posterior to the jugular vein.
-
A stimulation of the musculocutaneous
nerve or the median nerve is preferred to a stimulation of the axillary
nerve (deltoid contraction). -
The roots C8 and T1 (ulnar and median nerves) are partially blocked or not blocked with this approach.
-
If a trapezius contraction is elicited,
indicating a stimulation of the dorsal scapular root, the needle is too
posterior and should be redirected more anteriorly. -
If a diaphragm contraction is elicited,
indicating a stimulation of the phrenic nerve, the needle is too
anterior and should be redirected more posteriorly. -
A needle position parallel to the plexus sheath allows a better introduction of the catheter.
-
This approach should be used carefully in
children with reduced pulmonary function since a phrenic nerve block is
observed in 100% of the cases. -
Horner syndrome is a side effect related to cervical plexus diffusion encountered when using larger volumes.
-
Tunneling the catheter reduces catheter displacement in patients with good neck mobility.
|
Table 57-1. Bolus Volume Depending on Weight. Ropivacaine 0.2% for Continuous Infusion 0.4–0.5 mg/kg/h
|
||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||
P.377
 |
|
Figure 57-2. The Tuohy needle is removed and the catheter is secured in place and covered with a transparent dressing.
|
Suggested Readings
Dalens B. Regional anesthesia in infants, children, and adolescents. Baltimore: Williams & Wilkins, 1995:285–298.
Ivani G. Pediatric regional anaesthesia. A practical approach. Firenze, Italy: S.E.E. Firenze, 2001:103–112.
P.378
B. Infraclavicular Approach
Two different approaches are possible for the
infraclavicular approach to continuous brachial plexus block: vertical
and coracoid.
infraclavicular approach to continuous brachial plexus block: vertical
and coracoid.
Anesthesia and postoperative analgesia for arm, elbow, forearm, or hand
surgery. This is a very good approach for a fractured humerus or elbow
because the block can be performed without moving the fractured arm.
The depth of the brachial plexus at this level has not yet been
investigated in children. For an adult, the skin–plexus distance is
about 4 cm. In children, the plexus is found at a depth of 1 to 4 cm.
Vertical Infraclavicular Approach
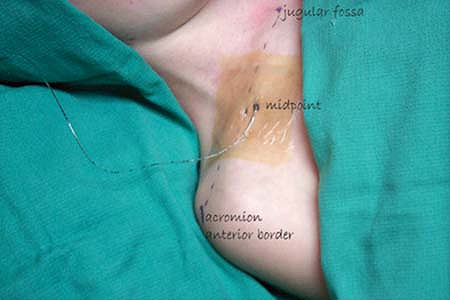
The ventral border of the acromial process of the scapula (lateral
landmark) is identified as well as the fossa jugularis (medial
landmark). A line is drawn between these two landmarks, and the
midpoint of this line, just below the clavicle, is the point of
insertion.
The Tuohy needle is introduced strictly vertical to the supine position
in an appropriately anesthetized/sedated child. It is essential to
obtain a movement of the hand (radial, median, or ulnar). Contraction
of the muscles of the arm is not sufficient. With an appropriate muscle
response still present at a current of 0.5 mA, the local anesthetic
solution is slowly injected after negative aspiration for blood.
Maintaining the insulated introducer needle in the same position, the
catheter is threaded 2 cm beyond the needle tip and directed to the
axilla (Fig. 57-3). The Tuohy needle is removed, and the catheter is secured in place with Steri-Strip and covered with a transparent dressing.
|
Table 57-2. Bolus Volume Depending on Weight. Ropivacaine 0.2% for Continuous Infusion 0.4–0.5 mg/kg/h
|
||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||
P.379
 |
|
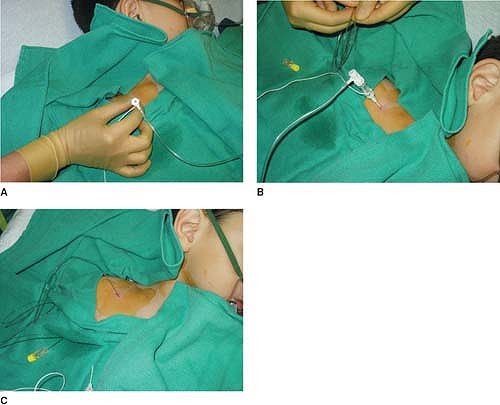
Figure 57-3. The catheter is threaded.
|
 |
|
Figure 57-4. Coracoid infraclavicular approach.
|
P.380
Coracoid Infraclavicular Approach
The Tuohy needle is introduced strictly vertical to the supine position
of the patient, at 1 to 2 cm medial and caudal (depending on the age)
to the coracoid process in an appropriately anesthetized/sedated child.
The plexus is found at a depth of 1 to 4 cm. It is essential to obtain
a movement of the hand (radial, median, or ulnar). Contraction of the
muscles of the arm is not sufficient. With an appropriate muscle
response still present at a current of 0.5 mA, the local anesthetic
solution is slowly injected after negative aspiration for blood (Fig. 57-4).
The catheter is introduced, directed to the axilla, and advanced no
more than 2 cm beyond the tip of the needle. The catheter is secured in
place with Steri-Strip and covered with a transparent dressing.
-
A pneumothorax can occur if the needle is directed too medially.
-
If the plexus is not found at an appropriate depth, the needle should be redirected more laterally.
-
The ulnar distribution is sometimes missed by the infraclavicular approach.
-
Because of the reduced mobility of this area, catheter displacement is very unlikely.
Suggested Readings
Dalens B. Regional anesthesia in infants, children, and adolescents. Baltimore: Williams & Wilkins, 1995:299–303.
Schuepfer GK, Joehr M. Infraclavicular vertical plexus blockade: a safe alternative to the axillary approach? Anesth Analg 1997;84:233.
