Chronic Posterolateral Rotatory Instability of the Elbow
IV – Elbow Reconstruction > Part B – Evaluation and Treatment of
Elbow Disorders > 50 – Chronic Posterolateral Rotatory Instability
of the Elbow
(PLRI) to describe elbow instability caused by injury to the radial
ulnohumeral ligament (RUHL) or lateral ulnar collateral ligament
(LUCL). Since then the functional anatomy of the lateral collateral
ligament complex has been closely examined, and the diagnosis and
treatment of this condition have evolved with good results.
injuries that produce subluxation events may result in PLRI. A fall
onto a rotated forearm or a twisting event, such as a drill locking
into an object and sending a supination force into the forearm or
elbow, are typical mechanisms of injury. Unfortunately, surgical
approaches to the lateral side of the elbow may also result in damage
to the RUHL complex. Lateral epicondylitis surgery that involves the
posterior/distal aspect of the epicondyle and radial head approaches
for excision, replacement, or trauma may be associated with the
development of PLRI.
Cohen and Hastings to also result in PLRI. Repetitive use of the elbow
when associated with a long-standing inflammatory response and weakness
of the extensor musculature may result in stretching or disruption of
the RUHL complex.
patients who presented with symptoms of valgus instability after trauma
but did not show typical clinical findings of a deficient medial
collateral ligament complex. In this group, the radial head and lateral
ulna rotated and subluxated posteriorly when the elbow was forced into
valgus from a supinated and extended position. He attributed this
instability to the incompetence of posterolateral structures,
specifically the radial ulnohumeral ligament. Although these patients
had responded poorly to the standard treatment for valgus instability,
they did well after plication or reconstruction of this ligament.
O’Driscoll named this condition posterolateral rotatory instability and
developed the posterolateral rotatory instability test or pivot shift
test to assist in diagnosis.
really a new problem. In 1966 Osborne and Cotterill reported a group of
patients with posterior subluxations of the radial head. Three of the
30 patients had normal exams. These authors felt that laxity in the
posterolateral capsule caused this problem and successfully treated
their patients with plication or repair of the lateral ligament complex.
reported cases of recurrent elbow dislocations that were difficult to
treat. One of the Hassman et al. patients clinically had a stable
ulnohumeral joint despite a history of multiple dislocations. Other
case reports described posttraumatic subluxations of the elbow that
could be reproduced with maneuvers similar to the pivot shift test. The
patients complained of locking and snapping of the elbow. Stress
radiographs showed typical findings of PLRI: widening of the
ulnohumeral joint space and posterior subluxation of the radial head.
because of its bony articulations and soft tissue stabilizers. The
three bony articulations include the radiocapitellar joint, the
proximal radioulnar joint, and the ulnohumeral joint. With trochlea
cradled by the olecranon posterior and the coronoid anterior, the
ulnohumeral joint provides the primary static restraint to
varus/valgus, anterior/posterior, and rotatory motion at the elbow. The
radiocapitellar joint is an important secondary stabilizer, accepting
up to 60% axial loads when the elbow is extended.
static soft tissue stabilizers of the elbow. Three major components
make up the medial or ulnar ligament complex (MCL): the anterior medial
bundle, the posterior medial bundle, and the transverse oblique bundle.
Although the proximal fibers have been described as distinct
structures, distally they resemble more the ligaments of the shoulder
as capsular thickenings. The medial ligament complex protects the elbow
against valgus stress with the forearm in pronation. Biomechanical
studies have shown that only the anterior and posterior bundles play
important roles in elbow stability.
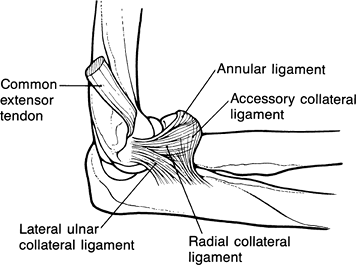
four components: the radial ulnohumeral ligament (RUHL) or lateral
ulnar collateral ligament (LUCL), the radial collateral ligament (RCL),
the annular ligament, and the accessory lateral collateral ligament (Fig. 50-1).
Unlike the medial structures, these individual ligaments are often
difficult to differentiate proximally where they originate as a broad
band from the lateral epicondyle deep to the extensor wad. Distally,
the fibers either remain as a single broad band or split into two
bands, with the RCL constituting the more anterior band and the RUHL
the posterior band. The annular ligament sweeps over the radial head
and is thought to be a stabilizer of the proximal radioulnar joint. The
RCL primarily restrains varus stress.
 |
|
Figure 50-1 Anatomy of the lateral ligamentous complex of the elbow. Lateral ulnar collateral ligament = radial ulnohumeral ligament.
|
PLRI. This ligament originates from the posterior inferior aspect of
the lateral epicondyle and inserts on the supinator crest of the ulna.
The RUHL is often difficult to distinguish proximally and is more
easily identified at its distal insertion. Positioning the arm in varus
and supination may help differentiate this structure from the RCL.
capsule and musculature act as important dynamic stabilizers of the
elbow. The capsule augments the strength of both the medial and lateral
ligaments. With the elbow extended, the anterior capsule acts as a
powerful restraint against varus and valgus stresses. Surgical
techniques to restore stability incorporate the capsule with ligament
plication. The anconeus and extensor wad are important dynamic
restraints laterally whereas the flexor-pronator mass strengthens
stability medially.
that deficiencies of the RUHL and laxity of the lateral capsule allow
the proximal radioulnar joint to rotate and the radial head to sublux
posteriorly when stressed, leading to PLRI. In patients with this
instability, the radial head subluxates, and on rare occasions, can
dislocate posteriorly depending on the position of the elbow. With the
forearm supinated and slightly flexed, valgus stress applied to the
elbow causes rotation of the ulnohumeral joint, compression of the
radiocapitellar joint, and posterior subluxation of the radial head.
Extreme supination of the forearm stresses the posterolateral
structures whereas flexing the elbow releases the olecranon tip from
the olecranon fossa, allowing rotation of the ulnohumeral joint.
PLRI to occur. During posterolateral rotation, the proximal forearm
rotates as a unit so that the coronoid passes under the trochlea as the
radial head moves posterior. This explains why hyperflexion or extensor
results in reduction of the instability. In O’Driscoll’s anatomic
studies, the annular ligament was intact in all specimens. The
integrity of this joint distinguishes PLRI from other instabilities
such as recurrent dislocations of the radial head and elbow where
disruption of this joint was thought necessary for dislocation to occur.
the functional anatomy of the entire lateral collateral ligament
complex and its relation to PLRI. Cohen has shown that injury to the
RUHL alone was not sufficient to cause instability. The entire lateral
ligament complex as well as the lateral musculature played significant
roles. Similarly, Dunning et al. demonstrated that the RUHL and the RCL
needed to be cut before PLRI occurred. On the other hand, Seki et al.
and Olsen et al. found that transection of either the RUHL or the RCL
created this instability.
roles of the lateral ligament complex, most consider PLRI to be the
first phase of elbow instability that can develop into frank
dislocation. As proposed by Morrey and O’Driscoll
individually,
the mechanism leading to an unstable elbow is a progressive disruption
of the ring of soft tissue stabilizers beginning laterally and sweeping
medially. The first injured structure is the RUHL, resulting in PLRI
that can reduce spontaneously. Further injury tears anterior and
posterior capsules, resulting in ulnohumeral subluxations. Complete
dislocation occurs when the medial structures are disrupted, although
the anterior band of the medial collateral ligament may be only
minimally injured.
complaining of lateral elbow pain. The differential diagnosis of PLRI
includes lateral epicondylitis, radial tunnel syndrome, valgus
instability, and pure proximal radial head dislocation. Standard
valgus/varus instability tests are often normal. Valgus instability
should be tested with the forearm supinated and pronated. With valgus
loads, pronation of the forearm tests the medial collateral ligamentous
complex, whereas supination stresses posterolateral structures, in
particular the RUHL.
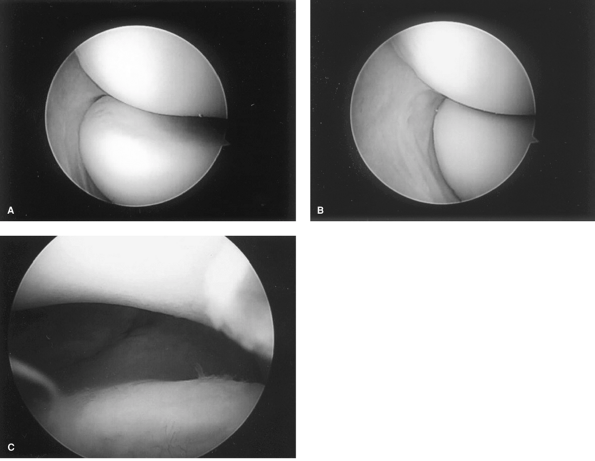
rotatory instability test or pivot shift test developed by O’Driscoll,
can help make the diagnosis. The pivot shift test for the elbow
resembles the pivot shift test for the anterior cruciate ligament
(ACL)–deficient knee. With the patient supine, the arm is raised
overhead, stabilizing the humerus to prevent external rotation. With
the forearm fully supinated and the elbow extended, a valgus-supination
force is applied to the elbow while slowing flexing it from an extended
position. As a result, the ulnohumeral joint rotates and the
radiohumeral joint subluxes posteriorly, sometimes even dislocating (Fig. 50-2A).
Dimpling of the skin may be seen proximal to the subluxing radial head.
As the elbow is flexed >40 degrees, the clinician may hear or feel
the radiohumeral joint suddenly reduce.
Feelings of pain or apprehension are considered a positive result in
such patients in the absence of instability. We prefer to perform the
pivot shift test with the patient positioned prone. Resting the arm
over the edge of the table stabilizes the humerus, allowing the
examiner to more easily palpate the radiohumeral joint during the
examination (Fig. 50-2B, C).
simulate the pivot shift test. The first requires the patient to push
up from a prone or wall position with the forearms maximally pronated
so that the thumbs are turned toward each other. The test is repeated
with forearms maximally supinated. The patient with PLRI will not want
to allow the elbow to fully flex, describing a felling of pain and/or
instability. Another test requires a patient to push up out of a chair
using the armrests. With palms facing inward, essentially placing them
in supination, pushing up will produce similar symptoms of pain.
Although elbow dislocation is the inciting event in 75% of patients
younger than 20 years of age, varus extension stress without true
dislocation is more likely the initiating event in older patients. PLRI
can also occur secondary to repetitive stresses on the elbow. Some
patients who present with lateral epicondylitis may also have PLRI.
Repetitive motion may produce laxity in the lateral ligamentous
complex, leading to secondary lateral epicondylitis. Previous surgery
to the lateral side of the elbow can cause iatrogenic instability. PLRI
has also been reported following radial head excision.
occasionally giving way of the elbow. As the instability may overstress
the lateral musculature, lateral epicondylitis symptoms are common. The
subluxation events may produce swelling in the posterolateral capsule
and enlarged plica with resulting secondary plica syndrome. True
dislocations tend to be rare. Rather, patients describe the elbow
slipping in and out of the joint in certain positions but especially
when the arm is supinated and slightly flexed.
the elbow should be obtained but are often normal. Bony avulsions
following ligament injury can be identified. On lateral views, typical
PLRI radiographic findings include widening of the ulnohumeral joint
space with posterior subluxation of the radial head. These are best
illustrated with radiographic or fluoroscopic stress views while
performing the pivot shift test with the patient under anesthesia (Fig. 50-3A, B). Associated changes include degenerative changes on the capitellum and spur formation on the lateral aspect of the olecranon.
and any such injuries can be identified on MRI using special
sequencing, this study requires experience in elbow MRI by both the
radiologist and MRI technician. MR arthrograms may prove more useful,
especially in posttraumatic cases.
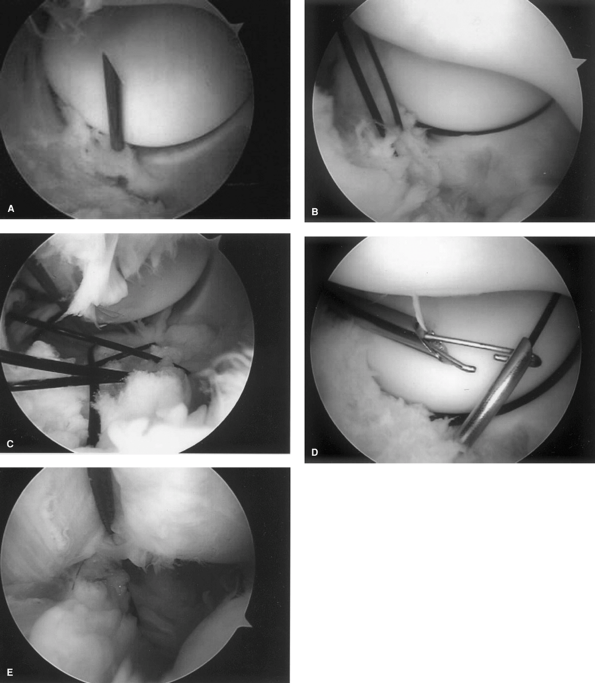
fluoroscopy may be valuable in making the diagnosis. Diagnostic
arthroscopy can also demonstrate PLRI in a patient in whom instability
is suspected. The pivot shift test should be performed while viewing
from the anteromedial portal. The radial head will rotate and translate
posterior if PLRI is present; with a competent ligament, the radial
head will rotate but not translate (Fig. 50-4A, B).
In addition, while viewing from the posterolateral portal, we have
found the arthroscope can be easily driven through the lateral gutter
and into the lateral aspect of the ulnohumeral joint if instability is
present. We have described this as the “elbow drive through” sign,
resembling the drive through sign in shoulder instability (Fig. 50-4C).
 |
|
Figure 50-2
The posterolateral rotatory instability (PLRI) test or pivot shift test. The test is performed by applying a valgus stress to the elbow with the humerus stabilized and the forearm maximally supinated. Symptoms occur as the arm is brought from full extension into slight flexion. A: Performing the test in the supine position maximally externally rotates the arm and allows the examiner to use both hands to manipulate the elbow. B: Performing the test with the patient prone stabilizes the humerus and frees one hand to more easily palpate the radiohumeral joint. C: Exam under anesthesia demonstrates the subluxation of severe PLRI. |
 |
|
Figure 50-3 Neutral (A) and stress (B) views of the elbow demonstrate widening of the ulnohumeral joint and posterior subluxation of the radial head.
|
 |
|
Figure 50-4 Arthroscopic findings of PLRI. A: The view from the anteromedial portal shows the normal position of the radial head with the forearm in pronation. B:
During the PLRI or pivot shift test, the radial head can be seen to sublux posteriorly. In a stable elbow, the radial head would rotate but not translate posteriorly. C: Drive through sign. |
posterolateral instability is often making the correct diagnosis. Once
that is made, appropriate treatment measures may be taken.
eliminating the secondary, pain-producing pathology; often a simple
elbow sleeve will provide sensory feedback and stabilize the elbow
enough to significantly reduce subluxation events. NSAIDs in pill and
cream form may help with the swelling and inflammation of the
extensors, muscles, and plica. Physiotherapy to include pain control
modalities, tissue massage, extensor muscle strengthening, and
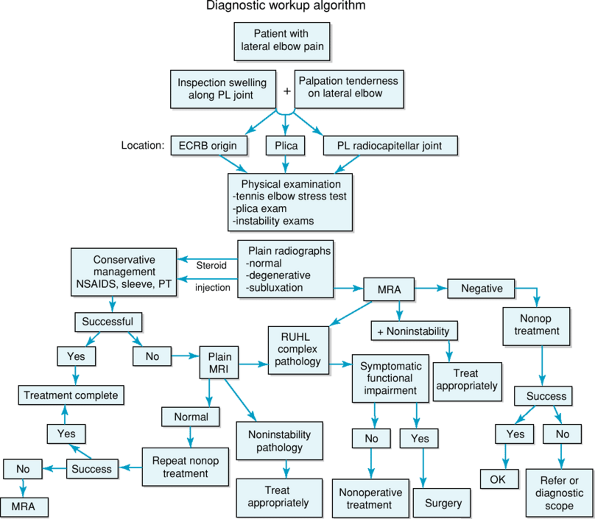
biofeedback exercises to control subluxation may be helpful as well (Fig. 50-5).
functional impairment in the affected elbow not relieved by
nonoperative management. Radiographic or MRI evidence alone is not a
sufficient indication. Contraindications may include an uncooperative
patient, psychiatric disorders, grade II or worse arthritis, or
surgical inexperience with the reconstructive techniques and anatomic
variations associated with this instability.
plication/repair, open graft reconstruction, or arthroscopic
plication/repair. The specific technique used depends more on the
surgeon’s preference, experience, and the number of previous surgeries
rather than any specific guidelines.
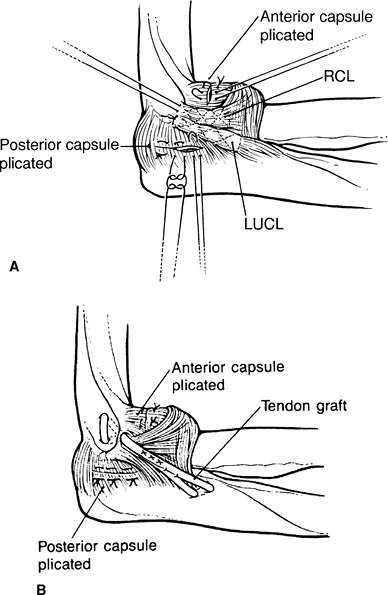
plicate, repair, and reconstruct the RUHL. With the patient supine, the
elbow is entered through a modified Kocher approach, exposing the
entire lateral ligament complex from the lateral epicondyle to the
supinator crest. The pivot shift test is performed to identify laxity
in the lateral capsule and insufficiencies of the RUHL. An attenuated
or detached ligament can be repaired by reattaching the ligament
through bone to the posterior inferior lateral epicondyle. The ligament
can be advanced or imbricated as needed. The loose capsule is
plicated with sutures tied following completion of the repair (Fig. 50-6A).
One simple technique for doing this is to place double-sutured anchors
at the origin of the RUHL on the condyle. One set of sutures can be
used to plicate the ligament and repair it to the epicondyle while the
second is used to repair any associated damage to the extensor muscle.
 |
|
Figure 50-5
Diagnostic workup algorithm. PL, posterolateral; ECRB, extensor carpi radialis brevis; NSAIDs, nonsteroidal anti-inflammatory drugs; PT, physiotherapy; MRA, magnetic resonance arthrogram; MRI, magnetic resonance imaging; RUHL, radial ulnohumeral ligament. |
necessary should the ligament tissue be of poor quality owing to
extensive trauma, multiple previous surgeries, or excessive injections.
In this technique an open posterolateral extensile approach is used.
The anconeus is retracted and any residual ligament or capsule split
longitudinally. The anatomic origin and insertion sites are identified
and then tested using a suture while ranging the elbow. We normally
drill our tunnel into the insertion site or the supinated crest of the
ulna first using a Beath pin. This pin is then overreamed with a 5.5-
or 6-mm reamer unicortically. The midportion of the graft is then
pulled into the tunnel until it contacts the ulnar cortex, and the
graft is fixed into the ulnar tunnel using an interference screw. The
isometric point on the humerus is then retested, and the proximal end
of the graft is passed into the tunnel and fixed using either a docking
technique, Endobutton, or interference screw. The elbow is positioned
in 40-degree flexion and the forearm fully pronated (Fig. 50-6B).
The semitendinosus is the most common allograft. Single or double limbs
of the graft can be passed through the isometric origin of the lateral
epicondyle. However, a recent study by King et al. has shown no
biomechanical differences between single- or double-strand grafts.
plicate or repair the RUHL. As mentioned earlier, PLRI can be diagnosed
by a posterior subluxing radial head during a pivot shift test or by
seeing a drive through sign. While
viewing
through the posterolateral portal, the surgeon passes an absorbable
suture into the joint through a spinal needle placed into the joint
directly adjacent to the lateral aspect of the proximal ulna at the
level of the supinator crest (Fig. 50-7A).
The first two sutures pierce the annular ligament. The suture is
retrieved adjacent to the posterior inferior aspect of the lateral
epicondyle, near the normal origin site of the RUHL. Four to seven
sutures can be passed, starting distal to proximal. The two ends of
each suture are brought out together through a lateral incision and are
tied separately in the same order. By pulling the sutures prior to
tying, one should see the lateral structures tighten and the lateral
gutter space collapse (Fig. 50-7B–D).
 |
|
Figure 50-6 Open lateral reconstruction for PLRI as described by O’Driscoll. A:
Repair of the radial ulnohumeral ligament by imbricating the ligament and reattaching it to its insertion point on the lateral epicondyle. The redundant posterolateral capsule is also plicated. B: Reconstruction of the ligament with a free tendon graft. It is essential to place the ligament in its correct anatomic position on the humeral epicondyle and supinator crest of the ulna. The posterolateral capsule is also plicated. RCL, radial collateral ligament; LUCL, lateral ulnar collateral ligament. |
augmented with a suture anchor. Through an additional portal, the
anchor is placed at the isometric point onto the posterior aspect of
the lateral epicondyle. One limb is passed into the joint, lassoing all
the plication sutures before being retrieved near the ulna. The
plication sutures are then tied, closing the lateral gutter and
plication the entire lateral ligament complex. The suture from the
anchor is then passed subcutaneously back over the tied sutures to the
anchor portal; tying this suture then pulls the entire plicated
ligament complex back toward the humerus, essentially reattaching the
entire ligament complex to the lateral epicondyle.
technique. Patients are immediately immobilized in a splint with the
elbow flexed to 70 to 90 degrees with the arm in full pronation. After
1 to 2 weeks, limited flexion of 45 to 90 degrees is initiated with the
elbow protected in a double-hinged elbow brace. Full range of motion in
the brace is allowed at 3 weeks. Full painless range of motion should
be achieved by 6 weeks, following which wrist and elbow strengthening
exercises in the brace are started. At 10 to 12 weeks, the brace can be
removed once the patient can perform all strengthening exercises in the
brace painfree.
described in the literature. In O’Driscoll’s first paper, four of five
patients were followed for 15 to 30 months. None had any recurrence of
instability, and all achieved full range of motion. In a follow-up
study by Nestor et al. on 11 patients, 3 patients underwent repair
whereas 7 underwent ligament reconstruction with palmaris graft.
Stability was achieved in ten patients with seven having an excellent
functional result.
found 90% satisfaction with no subluxations if the radial head is
intact and no degenerative articular changes are present. Patient
satisfaction decreases to 67% to 75% in the face of radial head
excision or arthritis. Mild flexion contracture (10 degrees) is
accepted as it protects against instability. Recurrent laxity or
redislocation has been reported but usually occurs after reinjury
involving significant stress.
average follow-up of 41 months (range 12 to 103 months) who underwent
operative management of PLRI at our institution. Diagnostic arthroscopy
confirmed PLRI in all patients. Thirty-seven patients were treated with
open techniques: 34 had ligament repair and 3 had reconstruction with
tendon graft. Seventeen patients were treated with arthroscopy: 11 had
ligament plication alone whereas 6 required an anchor to augment the
repair.
of lateral epicondyle release. Indications for open rather than
arthroscopic repair included having concurrent procedures such as
lateral epicondyle release, open extensor mass avulsion repairs, and
release of the posterior interosseous nerve.
from 88 to 95 (p = 0.008). Open repairs improved from 146 to 176 (p = 0.0001) and arthroscopic repairs from 144 to 182 (p < 0.001). Overall, open and arthroscopic techniques were shown to be equally effective (unpublished data).
 |
|
Figure 50-7
Arthroscopic reconstruction of posterolateral instability is accomplished by passing plication sutures through the ulnar side of the ligament with a spinal needle (A), retrieving them through the humeral side (B). These sutures are then retrieved out the soft spot portal and tied, closing the lateral ligament complex (C). This complex may be repaired to the humerus by passing a stitch around the plicated sutures (D) and tying the entire complex to the humerus. |
in a patient who complains of vague elbow pain and giving way with a
history of an elbow dislocation or previous lateral elbow surgery.
Although the topic is currently debated, the radial ulnohumeral
ligament does play an important role in this instability. Future
investigations will help determine the exact role of the lateral
collateral ligament complex in the unstable elbow. Indeed, PLRI is part
of a continuum of injury from instability to frank dislocation.
provocative tests are challenging to perform and radiographic studies
are not helpful. Early recognition following acute trauma and attention
to detail during open elbow procedures provide the best prevention of
PLRI. Diagnostic arthroscopy is an excellent tool to demonstrate this
instability. Although arthroscopic plication and repair have shown to
be as effective as open techniques, the clinician should be prepared
for open reconstruction if needed.
D, Verdegaal SHM, Obermann WR, et al. Posterolateral dislocation of the
elbow joint: relationship to medial instability. J Bone Joint Surg Am. 2000;82:555–560.
GJW, Dunning CE, Zarzour DS, et al. Single-strand reconstruction of the
lateral ulnar collateral ligament restores varus and posterolateral
instability of the elbow. J Shoulder Elbow Surg. 2002;11:60–64.
HG, Weiland AJ, Schatz JA, et al. Posterolateral rotatory instability
of the elbow: usefulness of MR imaging in diagnosis. Radiology. 1997;204:185–189.
A, Olsen BS, Jensen SL, et al. Functional anatomy of the lateral
collateral ligament complex of the elbow: configuration of Y and its
role. J Shoulder Elbow Surg. 2002;11:53–59.
