CHAPTER 9 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
CHAPTER 9 – Arthroscopic Treatment of Multidirectional Shoulder Instability
Jon K. Sekiya, MD
Neer and colleagues described the concept of multidirectional instability of the shoulder in detail in 1980. This established the difference between unidirectional instability and global laxity of the capsule inferiorly, posteriorly, and anteriorly. Initial treatments of this condition included open approaches aimed at decreasing capsular laxity by tensioning of the capsule, in particular inferiorly. As the pathoanatomy has become more defined and arthroscopic techniques for shoulder instability have improved, treatment has been more directed at arthroscopic stabilization procedures. Shoulder instability has been found to be a result of several pathologic processes, including capsular laxity, labral detachment, and rotator interval defects. Arthroscopic techniques have evolved from capsular shift by transglenoid sutures, Bankart repair and shift with biodegradable tacks or suture anchors, thermal capsulorrhaphy, rotator interval repair, and capsular plication. For treatment of patients with multidirectional shoulder instability for whom nonoperative attempts have failed, our current method is to perform an arthroscopic capsular shift by reducing capsular volume with capsular plication.
Typically, there is not a history of a traumatic shoulder dislocation, but it may be the inciting event. Most commonly, the instability is due to microtrauma resulting in global capsular laxity. There may be a history of recurrent dislocations or repetitive subluxation events.
| • | Apprehension test | |
| • | Relocation test | |
| • | O’Brien sign | |
| • | Jerk test | |
| • | Kim test | |
| • | Circumduction test | |
| • | Speed test |
Magnetic Resonance Arthrography
| • | Evaluate for capsular laxity, labral disease, biceps tendon disease, rotator cuff lesions |
| • | Evaluate for proximal humeral and glenoid bone defects |
Indications and Contraindications
In many patients with atraumatic multidirectional instability, the proper neuromuscular control of dynamic glenohumeral stability has been lost. The goal is to restore shoulder function through training and exercise. Patients with loose shoulders may not necessarily be unstable as evidenced by examination of the contralateral asymptomatic shoulder in patients with symptomatic multidirectional instability. The mainstay of treatment is nonoperative, with attempts to achieve stability by scapular and glenohumeral strengthening exercises. Those patients who have attempted a dedicated program of physical therapy, have functional problems, and remain unstable may then be candidates for surgical treatment.
Patients with a history of multidirectional instability who sustain fractures of the glenoid or humeral head with a dislocation generally require surgical treatment. In addition, significant defects in the humeral head associated with multiple dislocations consistent with Hill-Sachs lesions may require earlier surgical treatment. Glenoid erosion and lip fractures, if significant, can also necessitate surgical intervention if they are associated with recurrent instability.
Contraindications to surgical intervention may include patients with voluntary or habitual instability. In addition, patients who have not attempted a formal physiotherapy program should avoid initial surgical treatment. Furthermore, any patient unable or unwilling to comply with the postoperative rehabilitation regimen should not undergo surgical management.
Education of the patient is critical in planning surgical treatment for the individual with an unstable shoulder. The patients should have failed a trial of nonoperative treatment and have persistent instability with functional deficits. The goal of surgical treatment is to reduce capsular volume and to restore glenoid concavity with capsulolabral augmentation. By decreasing capsular volume, range of motion may be decreased as a result. It is important to discuss this possibility with the patient; some more active athletes, such as throwers, gymnasts, and volleyball players, may not tolerate losses of motion to maintain participation in their sport. Additional risks and benefits, including the risk of infection, recurrence of instability, pain, neurovascular injury, persistent functional limitations, and implant complication, should be discussed.
The surgical planning continues with the evaluation under anesthesia and diagnostic arthroscopy. This may alter the plan to include any combination of the following: capsular plication (anterior, posterior, or inferior), rotator interval closure, anterior-posterior labral repair, superior labral anterior-posterior (SLAP) repair, biceps tenodesis or tenotomy, and possible conversion to an open capsular shift.
The procedure can be performed under interscalene block or general endotracheal anesthesia with an interscalene block for postoperative pain control.
The patient is then placed in the lateral decubitus position with the affected shoulder positioned superior. An inflatable beanbag and kidney rests hold the patient in position. Pillows are placed to protect the peroneal nerve at the neck of the fibula on the down leg. An axillary roll is placed. The operating table is placed in a slight reverse-Trendelenburg position. The full upper extremity is prepared to the level of the sternum anteriorly and the medial border of the scapula posteriorly. The operative shoulder is placed in 10 pounds of traction and positioned in 45 degrees of abduction and 20 degrees of forward flexion.
Alternatively, the beach chair position can be used. The head of the bed is raised to approximately 70 degrees with the affected shoulder off the side of the bed with support medial to the scapula. The head should be well supported and all bone prominences padded. The entire arm, shoulder, and trapezial region are prepared into the surgical field. We prefer the lateral decubitus position, which we believe provides an excellent view of the inferior and posterior capsular regions.
The bone landmarks, including the acromion, distal clavicle, acromioclavicular joint, and coracoid process, are demarcated with a marking pen. After preparation and draping, the glenohumeral joint is injected with 50 mL of sterile saline through an 18-gauge spinal needle to inflate the joint. A posterior portal is established 1 cm distal and 1 cm lateral to the standard posterior portal to allow access to the rim of the posterior glenoid for anchor placement in case a posterior labral or capsular repair is necessary. An anterior portal is then established at the level just superior to the subscapularis tendon lateral to the coracoid to place the most inferior and anterior anchor (5-o’clock portal). An additional anterior superior portal is not typically needed with the technique that we will describe.
Examination Under Anesthesia and Diagnostic Arthroscopy
The examination under anesthesia is performed on a firm surface with the scapula relatively fixed and the humeral head free to rotate. A load-and-shift maneuver, as described by Murrell and Warren, is performed with the patient supine. The arm is held in 90 degrees of abduction and neutral rotation while an anterior or posterior force is applied in an attempt to translate the humeral head over the anterior or posterior glenoid. A sulcus sign test is performed with the arm adducted and in neutral rotation to assess whether the instability has an inferior component. A 3+ sulcus sign that remains 2+ or greater in external rotation is considered pathognomonic for multidirectional instability. Testing is completed on both the affected and unaffected shoulders, and differences between the two are documented.
A diagnostic arthroscopy of the glenohumeral joint is then undertaken. The labrum, capsule, biceps tendon, subscapularis, rotator interval, rotator cuff, and articular surfaces are visualized in systematic fashion. This ensures that no associated lesions will be overlooked by poorly directed tunnel vision. Lesions typically seen in multidirectional instability include a patulous inferior capsule, labral fraying and splitting, widening of the rotator interval, and undersurface partial-thickness rotator cuff tears. After the glenohumeral joint is viewed from the posterior portal, the arthroscope is switched to the anterior portal to allow improved visualization of the posterior capsule and labrum. A switching stick can then be used in replacing the posterior cannula with an 8.25-mm distally threaded clear cannula (Arthrex, Inc., Naples, Fla), thus allowing passage of an arthroscopic probe and other instruments through the clear cannula to explore the posterior labrum for evidence of tears.
Specific Steps (
Box 9-1
)
| • | The arthroscope then remains in the posterior portal, and the anterior portal serves as the working portal for the anterior repair (and vice versa for the posterior repair). | |
| • | An arthroscopic rasp or chisel is used to mobilize any torn labrum from the glenoid rim. | |
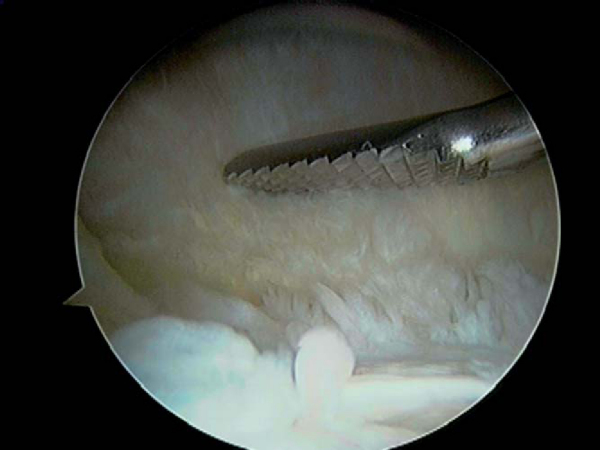
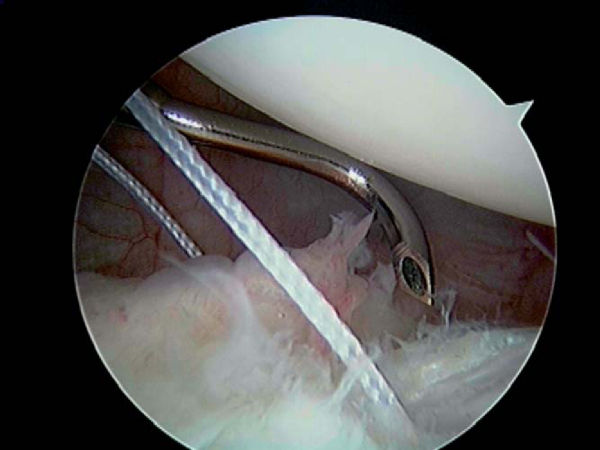
| • | A motorized synovial shaver or meniscal rasp is used to abrade the capsule adjacent to a labral tear and to débride and decorticate the glenoid rim to achieve a bleeding surface for capsular plication ( Fig. 9-1 ). |
2. Multi-Pleated Plication [15] [16]
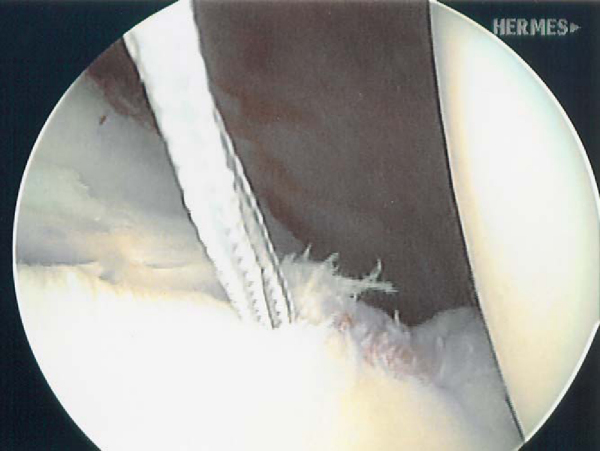
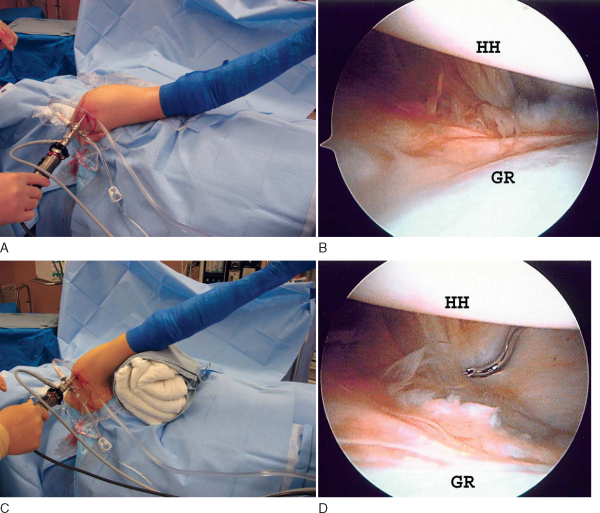
| • | A 3.0-mm Bio-Suture Tak anchor loaded with No. 2 FiberWire (Arthrex, Inc., Naples, Fla) is placed in the 5-o’clock position (right shoulder) for the anterior repair and in the 7-o’clock position for the posterior repair, and the sutures are brought out through the working portal ( Fig. 9-2 ). |
|
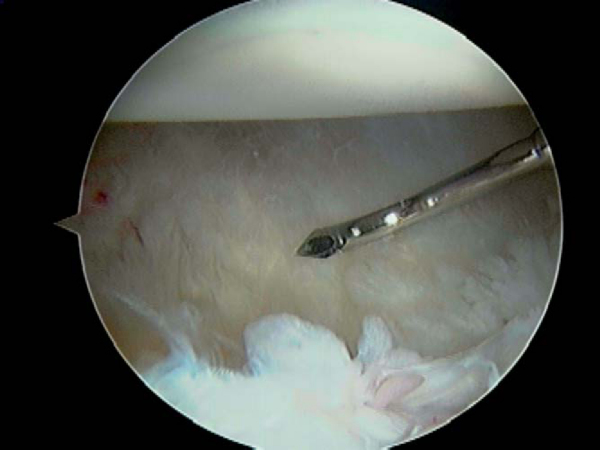
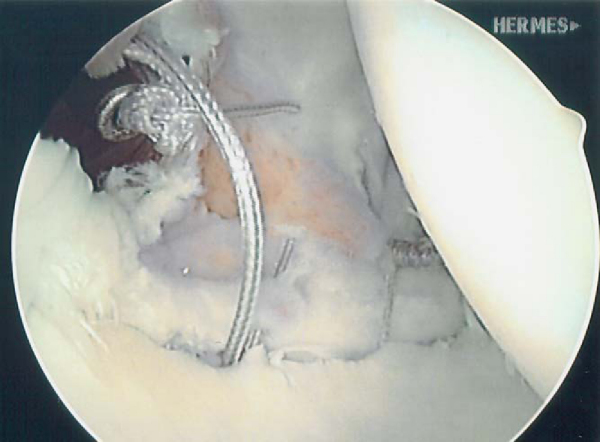
| • | A soft tissue penetrator (Spectrum suture hook, Linvatec, Largo, Fla) or crescent suture passer is passed through the labrum directly adjacent to the anchor, and the inferior FiberWire on the anchor is pulled through the labrum ( Fig. 9-3 ). |
|
| • | The penetrator is then used to pierce the inferior capsule in the most anterior inferior (5-o’clock anchor) and lateral point or posterior inferior (7-o’clock anchor) and lateral point. | |
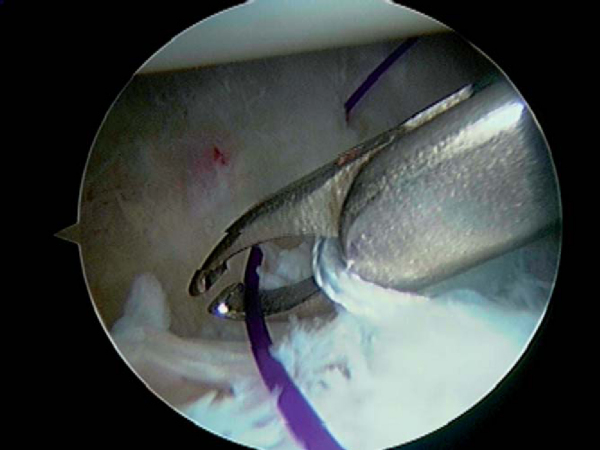
| • | Once the capsule is pierced through, a No. 1 polydioxanone (PDS) suture (Ethicon, Inc., Somerville, NJ) is shuttled into the joint and the penetrator is removed ( Fig. 9-4 ). |
|
| • | A suture grasper is then used to grab both the passed PDS suture and the labral suture to pull them out of the working portal. | |
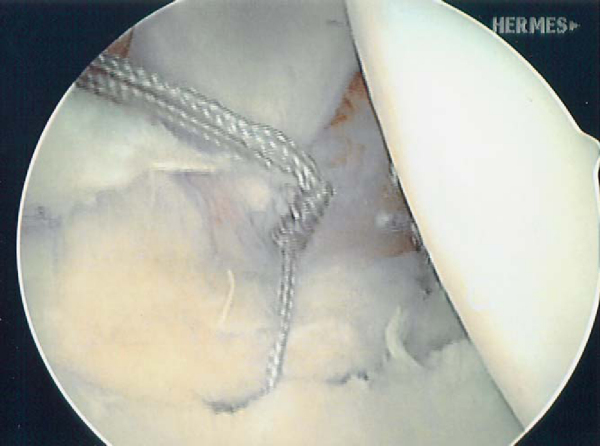
| • | The PDS suture is then tied with a simple knot to the FiberWire, and the PDS suture is then used to shuttle the working suture through the inferior tuck of capsule ( Fig. 9-5 ). |
|
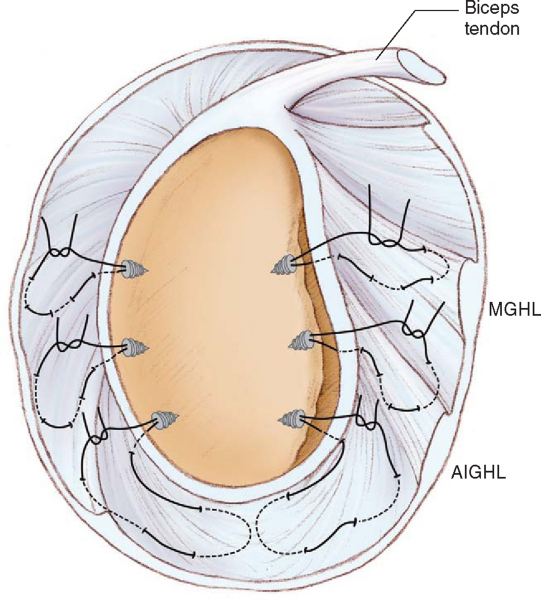
| • | This simple process is repeated while moving superiorly up the capsule until adequate capsular tension is restored ( Fig. 9-6 ). |
|
| • | The suture is checked to ensure that it will still slide, then a sliding-locking knot backed with three half-hitches is tied; the remaining suture is then cut (Figs. 9-7 and 9-8 [7] [8]). | |
| • | This is begun posteriorly and inferiorly (7-o’clock anchor), working posterior with additional anchors as necessary, and then anteriorly and inferiorly (5-o’clock anchor), working up anterior, again using additional anchors as necessary ( Fig. 9-9 ). |
|
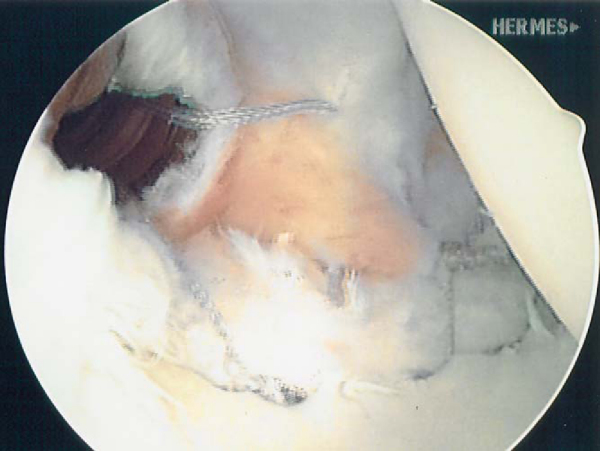
| • | The completed multi-pleated capsular plication reduces volume and improves stability ( Fig. 9-10 ). |
|
|
|
|
Figure 9-3 |
|
|
|
|
Figure 9-10 (From Sekiya JK. Arthroscopic labral repair and capsular shift of the glenohumeral joint: technical pearls for a multi-pleated plication through a single working portal. Arthroscopy 2005;21:766.) |
| • | We prefer the sliding-locking Weston knot, but there are a number of arthroscopic knot-tying techniques that work well. | |
| • | What is most important is that the surgeon be familiar with the knot used and be skilled in its use. | |
| • | The posterior braided suture exiting through the capsule is threaded through a knot pusher, and the end is secured with a hemostat. | |
| • | This suture serves as the post, which in effect will advance the capsule and labrum to the glenoid rim when the knot is tightened. | |
| • | The knot should be secured posteriorly on the capsule and not on the rim of the glenoid to prevent humeral head abrasion from the knot. | |
| • | Each half-hitch must be completely seated before the next half-hitch is thrown. | |
| • | Placing tension on the non-post suture and advancing the knot pusher “past point” will lock the Weston knot. | |
| • | A total of three alternating half-hitches are placed to secure the Weston knot. | |
| • | This knot has been found to be biomechanically similar to an open square knot.[4] |
| • | In this setting of multidirectional instability, the rotator interval may not require closure (defined by a 2+ or greater sulcus sign that does not improve in external rotation) if a multi-pleated repair is performed, plicating both the anterior and posterior bands of the inferior glenohumeral ligament and effectively bringing the entire inferior pouch superiorly. | |
| • | If rotator interval closure is required, it is viewed with the arthroscope in the posterior portal. | |
| • | A crescent suture passer is advanced from the anterior portal through the anterior capsule–middle glenohumeral ligament just above the superior border of the subscapularis tendon 1 cm lateral to the glenoid. | |
| • | It is then passed through the middle glenohumeral ligament at the inferior border of the rotator interval. This makes up the inferior aspect of the rotator interval closure. | |
| • | A No. 0 PDS suture is then fed into the joint and retrieved with a penetrator through the superior glenohumeral ligament. | |
| • | The PDS suture is then withdrawn out the anterior cannula and switched for a FiberWire suture; the knot is tied blindly in the cannula as the closure is visualized through the posterior portal. |
| • | A crescent suture passer is advanced from the posterior portal through the posterior capsule just above the superior border of the capsular opening of the posterior portal. | |
| • | A No. 0 PDS suture is then fed into the joint and retrieved with a penetrator through the inferior border of the capsular opening in the posterior portal. | |
| • | The PDS suture is then withdrawn out the posterior cannula and switched for a FiberWire suture; the knot is tied blindly in the cannula as the closure is visualized through the anterior portal ( Fig. 9-11 ). |
| • | The patient is discharged to home on the day of surgery. | |
| • | The sutures are removed 6 to 8 days later. |
| • | The arm is immobilized in an UltraSling (DonJoy, Carlsbad, Calif) for 6 weeks. | |
| • | The arm is maintained in 30 degrees of abduction in neutral rotation. | |
| • | The sling is removed for bathing and for gentle pendulum and elbow, wrist, and hand range-of-motion exercises. | |
| • | Isometric exercises are started at week 3. | |
| • | Passive and active-assisted range of motion is started at week 3. | |
| • | Discontinue the sling at week 6. | |
| • | Active range of motion is begun at week 6. | |
| • | Sport-specific exercises are begun at 4 months. | |
| • | Begin overhead sports at 6 months. | |
| • | Return to contact sports at 6 to 8 months. |
| • | Loss of motion | |
| • | Recurrence of instability | |
| • | Neurovascular injury | |
| • | Failure to address missed causes of instability: Large Hill-Sachs lesions that cause instability and that are not addressed at surgery may lead to recurrence. |
The details of clinical studies of multidirectional shoulder instability repair are presented in
Table 9-1
.
| Author | Procedure Performed | Followup | Outcome |
|---|---|---|---|
| Duncan and Savoie[3] (1993) | Scope inferior capsular shift | 1-3 years | 100% satisfactory |
| Pagnani et al[14] (1996) | Scope stabilization by transglenoid sutures | Average: 4.6 years (range: 4-10 years) | 74% good–excellent |
| McIntyre et al[11] (1997) | Scope capsular shift | Average: 34 months | 95% good–excellent |
| Treacy et al[18] (1999) | Scope capsular shift | Average: 5 years | 88% satisfactory |
| Gartsman et al[8] (2000) | Scope labral repair and laser capsulorrhaphy | Average: 33 months (range: 26-63 months) | 92% good–excellent |
| Tauro[17] (2000) | Scope inferior capsular split and advancement | 2-5 years | 88% satisfactory |
| Fitzgerald et al[6] (2002) | Scope thermal capsulorrhaphy | Average: 3 years (range: 24-40 months) | 76% satisfactory |
| Favorito et al[5] (2002) | Scope laser-assisted capsular shift | Average: 28 months | 81.5% successful |
| Frostick et al[7] (2003) | Scope laser capsular shrinkage | Average: 26 months (range: 24-33 months) | 83% satisfactory |
| D’Allesandro et al[2] (2004) | Scope thermal capsulorrhaphy | Average: 38 months (range: 2-5 years) | 63% satisfactory |
| PEARLS AND PITFALLS | ||||||||||||||||||||||||||||||||||
Return to sports at 6 months
|
In Vitro Capsular Volume Studies
During the last several years, multiple studies have investigated the effect of surgical intervention on capsular volume. Comparisons have been made between open capsular shifts with numerous techniques, arthroscopic thermal plication, and arthroscopic suture capsular plications by testing of capsular volume in cadaveric specimens before and after procedures.
Table 9-2
summarizes the results and types of shifts performed in these studies.
| Author | Type of Capsular Shift | Amount of Volume Reduction |
|---|---|---|
| Miller et al[12] (2003) | 3 open (medial, lateral, vertical) | Medial: 37% |
| Lateral: 50% | ||
| Vertical: 40% | ||
| Karas et al[9] (2004) | 3 arthroscopic (thermal, suture plication, combined) | Scope thermal: 33% |
| Scope plication: 19% | ||
| Scope combined: 41% | ||
| Victoroff et al[19] (2004) | Arthroscopic thermal | Scope thermal: 37% |
| Luke et al[10] (2004) | Open inferior vs. arthroscopic thermal | Open inferior: 50% |
| Scope thermal: 30% | ||
| Cohen et al[1] (2005) | Open lateral vs. arthroscopic plication | Open lateral: 50% |
| Scope plication: 23% | ||
| Sekiya et al[15] (2006) | Open inferior vs. arthroscopic multi-pleated plication | Open inferior: 45% |
| Scope multi-pleated: 58% |
1.
Cohen SB, Wiley W, Goradia VK, et al: Anterior capsulorrhaphy: an in vitro comparison of volume reduction–arthroscopic plication versus open capsular shift.
Arthroscopy 2005; 21:659-664.
2.
D’Alessandro DF, Bradley JP, Fleischli JE, Connor PM: Prospective evaluation of thermal capsulorrhaphy for shoulder instability: indications and results, two to five-year followup.
Am J Sports Med 2004; 32:21-33.
3.
Duncan R, Savoie 3rd FH: Arthroscopic inferior capsular shift for multidirectional instability of the shoulder: a preliminary report.
Arthroscopy 1993; 9:24-27.
4.
Elkousy HA, Sekiya JK, Stabile KJ, McMahon PJ: A biomechanical comparison of arthroscopic sliding and sliding-locking knots.
Arthroscopy 2005; 21:204-210.
5.
Favorito PJ, Langenderfer MA, Colosimo AJ, et al: Arthroscopic laser-assisted capsular shift in the treatment of patients with multidirectional shoulder instability.
Am J Sports Med 2002; 30:322-328.
6.
Fitzgerald BT, Watson BT, Lapoint JM: The use of thermal capsulorrhaphy in the treatment of multidirectional instability.
J Shoulder Elbow Surg 2002; 11:108-113.
7.
Frostick SP, Sinopidis C, Al Maskari S, et al: Arthroscopic capsular shrinkage of the shoulder for the treatment of patients with multidirectional instability: minimum 2-year followup.
Arthroscopy 2003; 19:227-233.
8.
Gartsman GM, Roddey TS, Hammerman SM: Arthroscopic treatment of anterior-inferior glenohumeral instability: two to five-year followup.
J Bone Joint Surg Am 2000; 82:991-1003.
9.
Karas SG, Creighton RA, DeMorat GJ: Glenohumeral volume reduction in arthroscopic shoulder reconstruction: a cadaveric analysis of suture plication and thermal capsulorrhaphy.
Arthroscopy 2004; 20:179-184.
10.
Luke TA, Rovner AD, Karas SG, et al: Volumetric change in the shoulder capsule after open inferior capsular shift versus arthroscopic thermal capsular shrinkage: a cadaveric model.
J Shoulder Elbow Surg 2004; 13:146-149.
11.
McIntyre LF, Caspari RB, Savoie 3rd FH: The arthroscopic treatment of multidirectional shoulder instability: two-year results of a multiple suture technique.
Arthroscopy 1997; 13:418-425.
12.
Miller MD, Larsen KM, Luke T, et al: Anterior capsular shift volume reduction: an in vitro comparison of 3 techniques.
J Shoulder Elbow Surg 2003; 12:350-354.
13.
Murrell GA, Warren RF: The surgical treatment of posterior shoulder instability.
Clin Sports Med 1995; 14:903.
14.
Pagnani MJ, Warren RF, Altchek DW, et al: Arthroscopic shoulder stabilization using transglenoid sutures. A four-year minimum followup.
Am J Sports Med 1996; 24:459-467.
15.
Sekiya JK, Willobee JA, Miller MD, et al. Arthroscopic multi-pleated capsular plication compared with open inferior capsular shift for multidirectional instability. Arthroscopy, in press.
16.
Sekiya JK: Arthroscopic labral repair and capsular shift of the glenohumeral joint: technical pearls for a multiple pleated plication through a single working portal.
Arthroscopy 2005; 21:766.
17.
Tauro JC: Arthroscopic inferior capsular split and advancement for anterior and inferior shoulder instability: technique and results at 2 to 5-year followup.
Arthroscopy 2000; 16:451-456.
18.
Treacy SH, Savoie 3rd FH, Field LD: Arthroscopic treatment of multidirectional instability.
J Shoulder Elbow Surg 1999; 8:345-350.
19.
Victoroff BN, Deutsch A, Protomastro P, et al: The effect of radiofrequency thermal capsulorrhaphy on glenohumeral translation, rotation, and volume.
J Shoulder Elbow Surg 2004; 13:138-145.