CHAPTER 38 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
CHAPTER 38 – Surgical Treatment of Posterolateral Instability of the Elbow
Marc Safran, MD
Although the term posterolateral rotatory instability was coined by and credited to O’Driscoll on the basis of his publication in 1991,[10] it was probably first described in 1966 by Osborne and Cotterill.[14] Elbow stability is maintained by bone anatomy as well as by the ligamentous attachments and balanced muscle forces. The integrity of the bone structures as well as of the medial and lateral ligamentous complexes is essential to elbow stability.
The ulnohumeral, radiohumeral, and radioulnar joints are the three articulations that compose the bone anatomy of the elbow joint. Each contributes to the stability of the elbow, which is one of the most stable, constrained joints in the body. The lateral and medial sides of the elbow have distinct ligamentous complexes. The medial or ulnar collateral ligament complex has three components: the anterior oblique ligament, also known as the anterior bundle; the posterior oblique ligament, also known as the posterior bundle; and the transverse ligament, also known as Cooper ligament. The anterior oblique ligament is functionally subdivided into anterior and posterior bands; it is widely considered to be the primary restraint to valgus stress. The lateral or radial side, known as the lateral collateral ligament complex, has four components: the lateral (or radial) ulnar collateral ligament, the radial collateral ligament, the annular ligament, and the accessory lateral collateral ligament. Deficiency of the lateral ulnar collateral ligament (LUCL) is widely believed to be the primary component in posterolateral rotatory instability as demonstrated by O’Driscoll.[11] Studies have questioned whether the LUCL is the essential lesion in posterolateral rotatory instability or if injuries to the radial collateral ligament and lateral capsule also contribute.[3] The lateral ligamentous injury that results in posterolateral rotatory instability usually occurs at the lateral epicondyle with at least some degree of tearing of the remainder of the lateral collateral ligament complex (namely, the radial collateral ligament). Furthermore, some cadaveric studies have been unable to produce posterolateral rotatory instability when the LUCL alone is cut.[18]
The LUCL attaches proximally to the lateral epicondyle of the humerus and distally to the tubercle of the supinator crest of the ulna. The humeral attachment is the isometric point on the lateral side of the elbow. The distal attachment is a broad fan-shaped thickening of the capsule that blends with and arches superficial and distal to the annular ligament to insert onto the ulna.[2] Besides acting as a stabilizer to varus stress of the elbow, it also serves as a posterior buttress to prevent posterior subluxation of the radial head. Posterolateral rotatory instability is defined as posterior radial head subluxation relative to the humerus while the normal proximal radioulnar relationship is maintained.
Patients present with symptoms of pain, locking, snapping, clicking, or recurrent instability usually preceded by trauma to the elbow (50% to 75%) or, less commonly, a history of previous elbow surgery.[4] A history of elbow dislocation is common, although some present with recurrent elbow sprains. Ligamentous laxity and childhood elbow fracture with a resultant cubitus varus deformity have also been reported to be predisposing factors.[12]
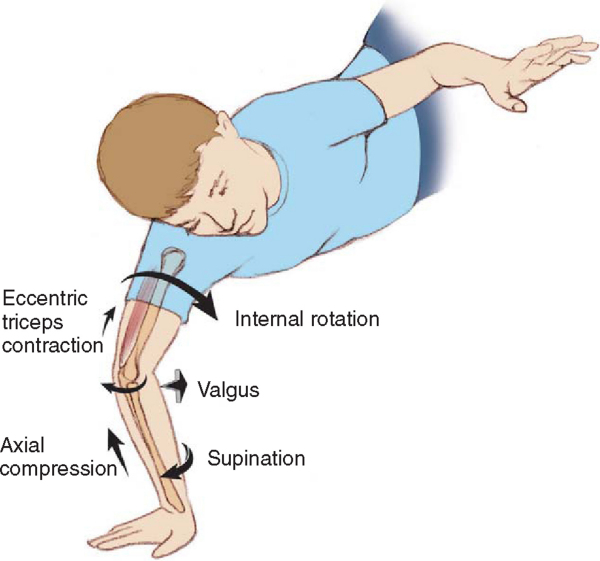
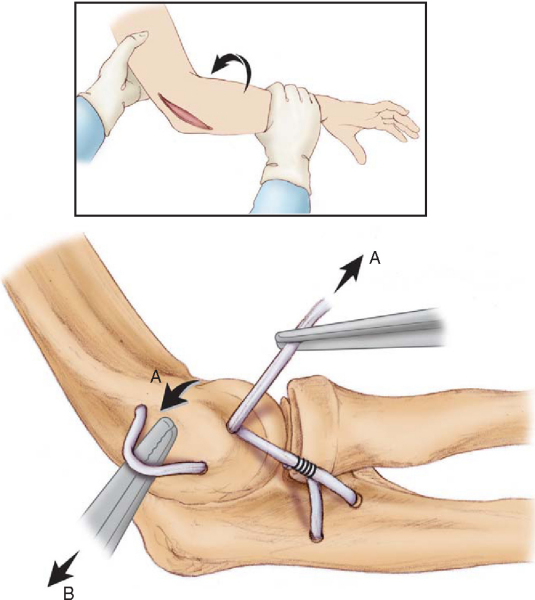
Disruption of the lateral ligaments with resultant posterolateral rotatory instability can occur iatrogenically from lateral elbow surgical approaches and arthroscopic elbow procedures. In the case of traumatic injury, the mechanism usually involves axial compression, hyperextension, and external rotation (supination) of the elbow (
Fig. 38-1
). Direct varus stress injuries are a less common cause. In general, injury to the lateral ligamentous structures is considered the initial stage in a continuum of instability[12] (
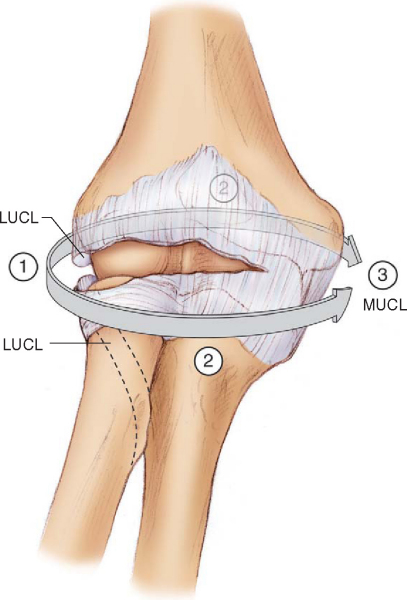
Fig. 38-2
). This begins with injury to the LUCL followed by injury to the entire lateral collateral ligament complex, the anterior and posterior capsule, and finally the posterior and anterior bands of the ulnar collateral ligament complex, leading to frank dislocation. O’Driscoll has also shown, however, that frank dislocation can occur before rupture of the ulnar collateral ligament.
|
|
|
|
Figure 38-1 |
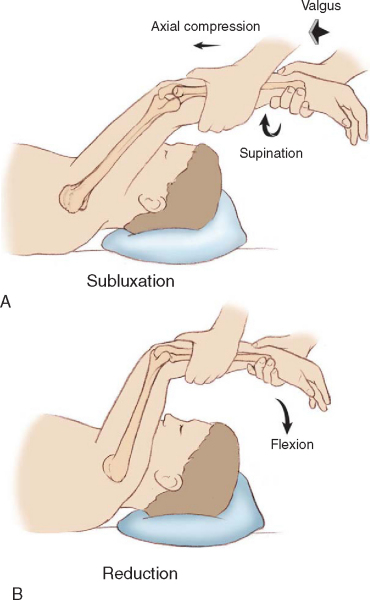
Clinical examination is usually unremarkable except for the posterolateral rotatory instability test (lateral pivot shift test), which is easiest to perform with the patient in a supine position (
Fig. 38-3
). With the shoulder forward elevated, the forearm is placed in full supination and extension. The elbow is then gently flexed while the examiner applies a slight valgus force and axial load. The radial head is subluxated in this starting position. A rotatory subluxation of the ulnohumeral joint with posterior subluxation of the radial head can be palpated as a posterior prominence and dimple in the skin just proximal to the radial head. With further flexion beyond 40 degrees, the radial head spontaneously reduces with a “clunk” as the triceps becomes taut, reproducing the patient’s symptoms and apprehension. With more significant injury and laxity, the clunk of reduction occurs in greater degrees of elbow flexion. This may be difficult to do in an awake patient, and thus guarding and apprehension alone are suggestive of a positive test result. Because of guarding, demonstration of the pivot shift may require local (intraarticular) or general anesthesia or fluoroscopy.
Other tests are the posterolateral drawer test, the prone pushup test, and the armchair pushup test.[16] The posterolateral drawer test is analogous to the rotatory version of the drawer or Lachman test of the knee. The prone pushup test is performed by asking the patient to attempt to push up from a prone position, first with the forearms maximally pronated and the thumbs pointed toward each other and then with the thumbs pointed outward and the forearms maximally supinated. The test result is positive if symptoms occur when the forearms are supinated but not when they are pronated. The chair pushup is performed by asking the patient to stand from a sitting position by pushing off of a chair with the hands grasping the armrests with palms facing inward (forearm supination). Pain on this maneuver is a positive test result. Reproducible symptoms of pain during the prone and chair pushup tests are positive results for posterolateral rotatory instability.
When a patient with chronic posterolateral rotatory instability is examined, evaluation for the presence of a palmaris longus tendon in either forearm or both forearms is important to determine whether the patient has this potential graft source.
Although posterolateral rotatory instability is primarily a clinical diagnosis, radiologic evaluation can be helpful. Studies include the posterolateral rotatory instability pivot shift test with fluoroscopic control or with stress radiographs to demonstrate radial head subluxation and ulnohumeral joint widening. Plain films can show bone avulsions or subtle signs of subluxation. Magnetic resonance imaging has been shown to be useful in identifying components of the lateral collateral complex with the appropriate thin-cut pulse sequences and an experienced radiology staff.[15] Arthroscopy is a useful adjunct to help identify radial head subluxation or lateral joint widening with stress testing and to assess any intraarticular disease.
Indications and Contraindications
Acute injuries after an initial subluxation or dislocation event are best treated nonsurgically with a splint or brace, keeping the forearm in pronation to allow the lateral ligaments to heal. However, if a bone avulsion exists, primary surgical repair may provide good results and prevent chronic disability. Chronic injuries do not respond well to conservative therapy and usually require surgery. Surgery is indicated for patients with the symptoms stated before, including recurrent instability of the elbow and evidence of posterolateral rotatory instability. Braces for chronic injuries are usually cumbersome and not well tolerated by the patients. Prolonged bracing can result in stiffness.
Relative contraindications to surgery are open physes, elbow arthritis, generalized ligamentous laxity, and voluntary dislocators. No absolute contraindications exist.
General anesthesia with the patient in the supine position is preferred.
Examination under anesthesia is carried out to include medial and lateral stability testing and posterolateral rotatory stability testing. The upper extremity is prepared and draped in the usual fashion, and a sterile tourniquet is applied to the upper arm. The graft of choice is the palmaris longus, with ipsilateral being the first choice and contralateral the second. If no palmaris longus is present, a lower extremity is prepared and draped for semitendinosus harvesting. Also, an allograft can be used.
Specific Steps (
Box 38-1
)
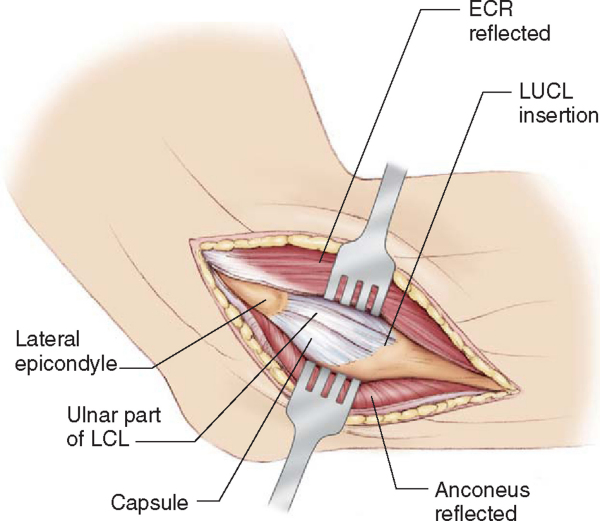
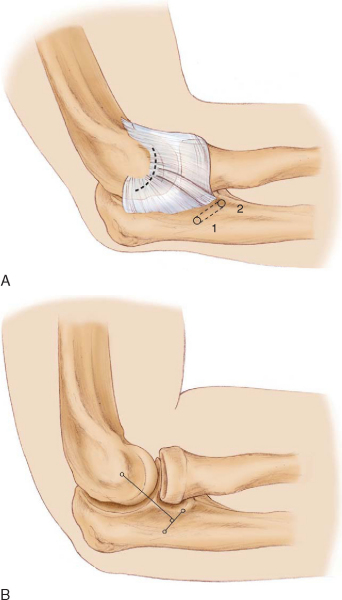
An 8- to 10-cm lateral (Kocher) incision is made beginning approximately 3 cm proximal to the lateral epicondyle and extending over the lateral epicondyle and along the anterior border of the anconeus distally (
Fig. 38-4
). The interval between the anconeus and the extensor carpi ulnaris is developed. The proximal anconeus and distal triceps can be reflected from the lateral supracondylar ridge and the lateral epicondyle to improve exposure. The extensor carpi ulnaris is elevated off the annular ligament and the common extensor tendon–extensor carpi radialis brevis is elevated off the anterior aspect of the lateral epicondyle to expose the lateral ligamentous complex. Care must be taken to preserve the anterior capsule and LUCL remnant. This is best accomplished by beginning the dissection distally in the interval. Use of a periosteal or Freer elevator rather than a knife may facilitate dissection while reducing the risk of injury to the underlying lateral collateral ligament complex. The posterolateral rotatory instability pivot test can be performed again at this time to identify ligament and capsular deficiencies. The LUCL is examined and assessed for primary repair. If adequate tissue is not available, a ligamentous graft reconstruction is indicated.
Primary repair is performed by reattachment of the intact ligament to the inferior posterior portion of the lateral epicondyle with suture anchors or transosseous sutures with or without anterior and posterior capsular plication. Two drill holes are placed in the midportion of the lateral epicondyle at the anatomic origin of the LUCL. A nonabsorbable suture is placed through a drill hole, and a running locked stitch is placed down the ligament remnant and back up the contralateral side. The suture is then tied over the bone bridge. Alternatively, a suture anchor is placed at the origin of the LUCL, and a locked running suture is placed in the LUCL remnant for the primary repair. The forearm is pronated and splinted at 60 to 90 degrees of flexion.
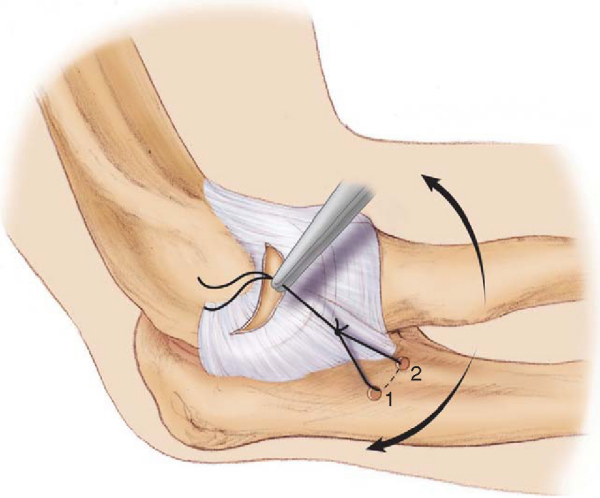
Reconstruction of the deficient LUCL is performed with a free ligamentous autograft, such as the palmaris longus tendon or semitendinosus. Required graft length is approximately 20 cm. The palmaris longus can be harvested through a 1-cm incision at the distal volar wrist crease with a standard tendon stripper. A capsular incision is made anterior to the lateral ligamentous complex for joint inspection and later imbrication. Two 3.5-mm drill holes are placed in the ulna, one into the supinator tubercle just distal to the lateral attachment of the capsule and the other approximately 1 to 1.5 cm posterior in a perpendicular line to the axis of the LUCL. The underlying bone is channeled with a curved awl connecting the two holes (
Fig. 38-5
).
|
|
|
|
Figure 38-5 |
A suture is passed through the drill holes, and a hemostat is attached to help identify the isometric attachment of the lateral collateral ligament complex on the lateral epicondyle. The hemostat is placed on the lateral epicondyle, and the elbow is flexed and extended to identify the isometric point at which both limbs of the suture remain taut (
Fig. 38-6
). This point should correspond to the middle of the capitellum on a lateral radiograph.
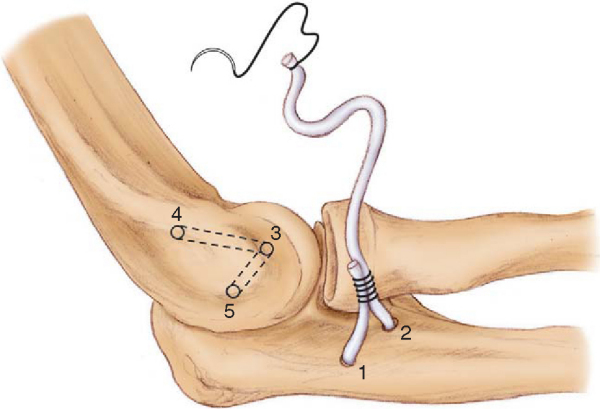
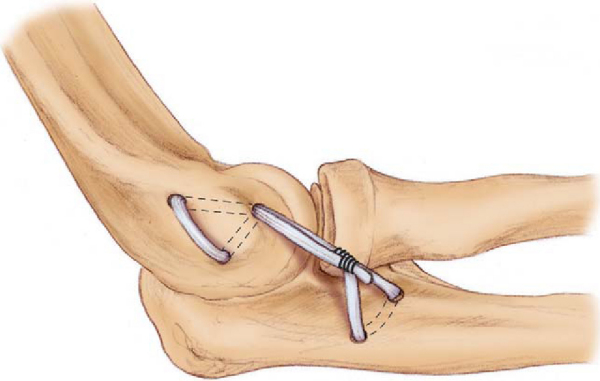
A 4.5-mm drill hole is placed at the isometric point angled medially and proximally toward the supracondylar ridge and burred to a size of 5 or 6 mm. This hole should tend anterior and proximal to the established isometric point, especially during enlargement, to ensure that the graft is tight in extension. A second hole is made just posterior to the supracondylar ridge, about 1.5 cm proximally, and a tunnel is developed between the two. A second tunnel is made from the same isometric entry point by drilling a third hole 1 to 1.5 cm distal to the second hole so that a bridge of bone remains between it and the first tunnel (
Fig. 38-7
).
The graft is passed through the ulnar tunnel from anterior to posterior. One end of the graft is passed into the isometric hole in the humerus, out the proximal tunnel, along the posterior humeral cortex, and back in the distal tunnel, emerging through the isometric hole (
Fig. 38-8
).
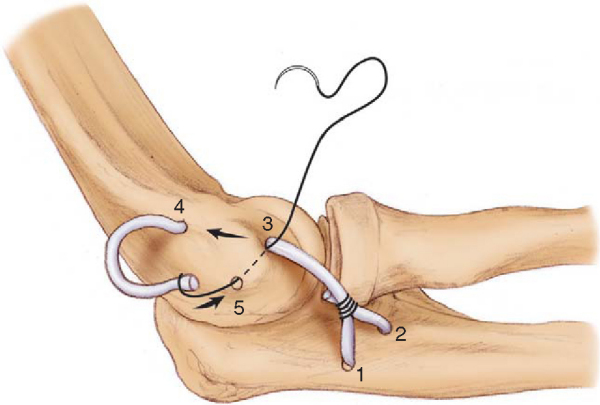
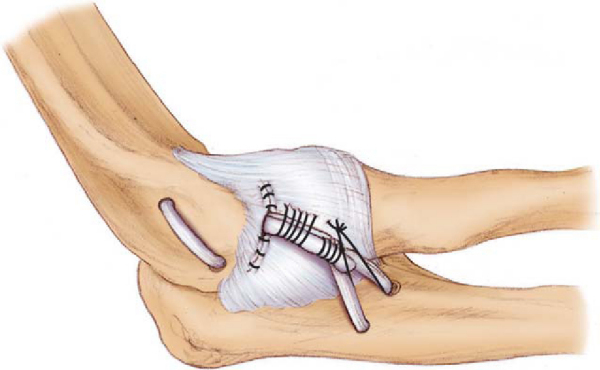
The graft is tensioned with the arm maximally pronated in 30 to 40 degrees of flexion and sutured to itself in a figure-of-eight configuration (Figs. 38-9 and 38-10 [9] [10]).
Alternatively, some surgeons make a single, blind-ended tunnel in the lateral epicondyle at the isometric point and fix the graft, after appropriate measurement, with an interference screw. This eliminates the need for three holes and two tunnels in the lateral epicondyle. The resultant graft is double-stranded instead of a three-ply reconstruction with the figure-of-eight graft originally described. Another variation uses a single blind-ended tunnel at the supinator crest with an interference screw. The interference screw technique can be used on either end or on both ends (humeral and ulnar) for fixation. The capsule is closed beneath the graft and plicated as necessary (
Fig. 38-11
).
The graft is tensioned further by pulling it anteriorly and suturing it to the capsule and by closing the distal loop of the figure-of-eight construct (
Fig. 38-12
). The overlying soft tissues are closed in layers in the standard fashion.
An above-elbow splint is placed postoperatively with the forearm in pronation and the elbow at 90 degrees of flexion. It is removed at 1 week, and a 30-degree extension block splint or hinged brace is applied for 6 weeks. Full range of motion in a hinged elbow brace is initiated at 6 weeks. Bracing is usually discontinued after 3 months, at which point the patient begins a strengthening program within pain-free limits. This can be variable on the basis of the patient’s compliance and the strength of the repair. Full recovery is expected after 6 to 9 months.
Potential complications include cutaneous nerve damage (from incision or tendon harvesting), persistent flexion contracture, and persistent instability. Care is required to prevent fracturing through bone bridges. Persistent instability can often be attributed to a posteriorly placed tunnel on the humerus that leaves the graft lax in extension, where posterolateral rotatory instability tends to occur. Persistent flexion contracture (<10 degrees) can be protective as posterolateral rotatory instability occurs most frequently in extension.
| PEARLS AND PITFALLS | ||||||||||||||||||||||||||||||||||||
|
Primary repair of the LUCL, when possible, has excellent results. Osborne and Cotterill[14] reported excellent results in eight patients with transosseous repair, and Nestor et al[9] reported excellent results in three patients. Ligamentous reconstruction results have been mixed (
Table 38-1
). O’Driscoll and Morrey reported a 90% success rate in restoring stability in the absence of arthritis or radial head fracture; 60% of patients experienced excellent results, whereas 40% continued to have pain or some loss of motion.
| Author | Followup (Mean) | Outcome |
|---|---|---|
| Sanchez-Sotelo et al (2005) | 6 years | 40 of 45 (89%) stable |
| 38 of 45 (86%) satisfied | ||
| Olsen and Sojbjerg[13] (2003) | 44 months | 14 of 18 (78%) stable |
| 17 of 18 (94%) satisfied | ||
| [*]Nestor et al[9] (1992) | 42 months | 10 of 11 (91%) stable |
| 7 of 11 (64%) excellent | ||
| [*]Lee and Teo[6] (2003) | 24 months | 10 of 10 (100%) stable |
| 10 of 10 (100%) satisfied |
1.
Ball CM, Galatz LM, Yamaguchi K: Elbow instability: treatment strategies and emerging concepts.
Instr Course Lect 2002; 51:53-61.
2.
Cohen MS, Hastings II H: Rotatory instability of the elbow: the anatomy and role of the lateral elbow stabilizers.
J Bone Joint Surg Am 1997; 79:225-233.
3.
Dunning CE, Zarzour ZD, Patterson SD, et al: Ligamentous stabilizers against posterolateral rotatory instability of the elbow.
J Bone Joint Surg Am 2001; 83:1823-1828.
4.
Hall JA, McKee MD: Posterolateral rotatory instability of the elbow following radial head resection.
J Bone Joint Surg Am 2005; 87:1571-1579.
5.
King GJ, Dunning CE, Zarzour ZD, et al: Single-strand reconstruction of the lateral ulnar collateral ligament restores varus and posterolateral rotatory instability of the elbow.
J Shoulder Elbow Surg 2002; 11:60-64.
6.
Lee BP, Teo LH: Surgical reconstruction for posterolateral instability of the elbow.
J Shoulder Elbow Surg 2003; 12:476-479.
7.
Mehta JA, Bain GI: Posterolateral rotatory instability of the elbow.
J Am Acad Orthop Surg 2004; 12:405-415.
8.
Morrey BF, O’Driscoll SW: Surgical reconstruction of the lateral collateral ligament.
In: Morrey BF, ed. The Elbow, 2nd ed. Master Techniques in Orthopaedic Surgery,
Philadelphia: Lippincott Williams & Wilkins; 2002:249-265.
9.
Nestor BJ, O’Driscoll SW, Morrey BF: Ligamentous reconstruction for posterolateral rotatory instability of the elbow.
J Bone Joint Surg Am 1992; 74:1235-1241.
10.
O’Driscoll SW, Bell DF, Morrey BF: Posterolateral rotatory instability of the elbow.
J Bone Joint Surg Am 1991; 73:440-446.
11.
O’Driscoll SW, Morrey BF, Korinek S, An KN: Elbow subluxation and dislocation. A spectrum of instability.
Clin Orthop 1992; 280:186-197.
12.
O’Driscoll SW, Spinner RJ, McKee MD, et al: Tardy posterolateral rotatory instability of the elbow due to cubitus varus.
J Bone Joint Surg Am 2001; 83:1358-1369.
13.
Olsen BS, Sojbjerg JO: The treatment of recurrent posterolateral instability of the elbow.
J Bone Joint Surg Br 2003; 85:342-346.
14.
Osborne G, Cotterill P: Recurrent dislocation of the elbow.
J Bone Joint Surg Br 1966; 48:340-346.
15.
Potter HG, Weiland AJ, Schatz JA, et al: Posterolateral rotatory instability of the elbow: usefulness of MR imaging in diagnosis.
Radiology 1997; 204:185-189.
16.
Regan WD, Korinek SL, Morrey BF, An KN: Biomechanical study of ligaments around the elbow joint.
Clin Orthop 1991; 271:170-179.
17.
Sanchez-Sotelo J, Morrey BF, O’Driscoll SW: Ligamentous repair and reconstruction for posterolateral rotatory instability of the elbow.
J Bone Joint Surg Br 2005; 87:54-61.
18.
Seki A, Olsen BS, Jensen SL, et al: Functional anatomy of the lateral collateral ligament complex of the elbow: configuration of Y and its role.
J Shoulder Elbow Surg 2002; 11:53-59.
19.
Singleton SB, Conway JE: PLRI: posterolateral instability of the elbow.
Clin Sports Med 2004; 23:629-642.
20.
Smith 3rd JP, Savoie 3rd FH, Field LD: Posterolateral rotatory instability of the elbow.
Clin Sports Med 2001; 20:47-58.
21.
Yadao MA, Savoie 3rd FH, Field LD: Posterolateral rotatory instability of the elbow.
Instr Course Lect 2004; 23:629-642.