CHAPTER 34 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
CHAPTER 34 – Elbow Synovitis, Loose Bodies, and Posteromedial Impingement
Kyle Anderson, MD
Athletic activities can lead to elbow inflammation and synovitis, joint degeneration, and formation of spurs and loose bodies. In fact, loose body removal represents the most common indication for elbow arthroscopy in this population.[23] Because of the high demand an athlete places on the elbow and other joints, even relatively small but newly acquired deficits in range of motion for a competitive athlete can be extremely disabling. Chronic motion loss, however, may be more easily accommodated. The necessary range of motion varies with the type of sport, the position played, and the individual mechanics necessary to remain competitive. Certainly, loose bodies and osteophytes adherent to the joint capsule can create mechanical blocks to motion, resulting in pain as well as decreased performance. Posteromedial impingement is often the result of the tremendous strain an athlete places on the elbow. The repetitive valgus forces generated during the acceleration and follow-through phases of pitching as the elbow goes into extension can result in osteochondral changes of the olecranon and distal humerus. [10] [24] A significant osteophyte forms on the posteromedial aspect of the olecranon process and impinges on the medial articular wall of the olecranon fossa. Over time, the osteophytes can fragment and form loose bodies.
Synovial disorders can also be the source of pain and mechanical symptoms equally disabling to an athlete. Diseases such as synovial chondromatosis, pigmented villonodular synovitis, and inflamed synovial plica can produce mechanical symptoms that can alter the normal mechanics of elbow motion. [8] [14] [19] The symptoms experienced may or may not be related to the activity. These conditions can sometimes be easily overlooked by assuming that the elbow symptoms are a result of the sports activity. The clinician should maintain a broad differential diagnosis. In this population, elbow arthroscopy can be an effective tool for the removal of inflamed synovial tissue, osteophytes, and loose bodies, returning an athlete to the previous level of competition.
A carefully performed history often provides the most important information. Symptoms are usually activity related. Patients often describe mechanical symptoms, such as catching, locking, and popping. The specific timing of pain can be important in determining the type of pathologic changes present.
| • | Insidious and progressive posterior elbow pain and limited elbow extension result from impinging posterior osteophytes; popping, locking, or catching suggests loose bodies. | |
| • | Symptoms are usually most prominent during the involved activity; the patient is often asymptomatic at rest. | |
| • | Specific timing of pain exacerbation during the activity can be telling. Pain in late innings during pitching can indicate ligamentous disease often unmasked after forearm muscles fatigue, whereas arthrosis presents more as pain and stiffness early in the morning or early in the activity. | |
| • | Specific timing of pain during the throwing motion itself can help differentiate between ligamentous injury (often most symptomatic during early acceleration) and impingement (which typically produces pain at ball release or follow-through). [15] [23] | |
| • | The patient may complain of intermittent swelling after activity. | |
| • | Paresthesias may result from ulnar nerve irritation either by impinging spurs or traction during throwing. |
| • | A brief examination of the cervical spine, shoulder, and wrist is always performed before the physical examination focuses on the elbow. Several conditions of the cervical spine and shoulder may present as elbow pain. | |
| • | Range of motion, loss of extension: posterior olecranon spur, posterior compartment loose bodies, bridging osteophyte across olecranon fossa, anterior capsule contracture, collateral ligament contracture with or without ossification | |
| • | Range of motion, loss of flexion: coronoid spur, anterior compartment loose bodies, coronoid fossa spur, posterior capsule contracture or triceps adhesions, collateral ligament contracture | |
| • | Palpation: with or without joint effusion, warmth, or crepitation; posteromedial tenderness with valgus hyperextension and posteromedial impingement[24] or posterolateral tenderness in cases of lateral synovial plicae [8] [14] | |
| • | Ligamentous stability: medial collateral ligament insufficiency can lead to posteromedial fragmentation with formation of loose bodies or loss of extension; valgus testing is performed with the elbow in pronation at 30 and 90 degrees of elbow flexion. [7] [10] [24] | |
| • | Valgus extension overload test: combined valgus and gentle terminal extension[24] | |
| • | Neurovascular: palpate ulnar nerve during flexion and extension to assess for subluxation and assess for Tinel sign. | |
| • | Intraarticular injections can sometimes be helpful in assessing intraarticular versus extra-articular pathologic processes. |
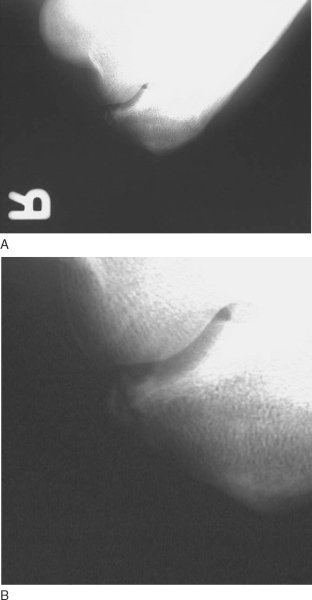
| • | Standard anteroposterior and lateral views are obtained ( Fig. 34-1 ). |
|
| • | The hyperflexion and external rotation view can increase visualization of the posteromedial olecranon out of its fossa ( Fig. 34-2 ). |
|
| • | When radiocapitellar disease is suspected, the external rotation view is obtained with the anterior elbow surface oriented at 40 degrees oblique relative to the cassette. |
|
|
|
|
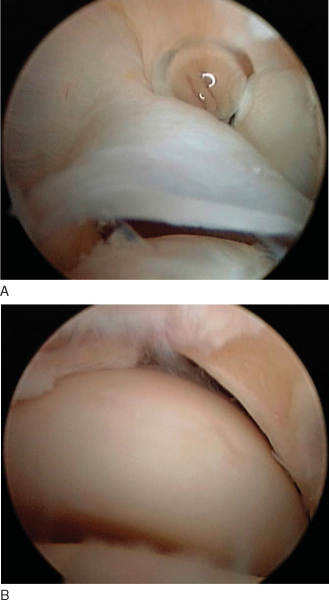
Figure 34-2 demonstrating posteromedial spur. B, Close-up view of the posteromedial fragment. |
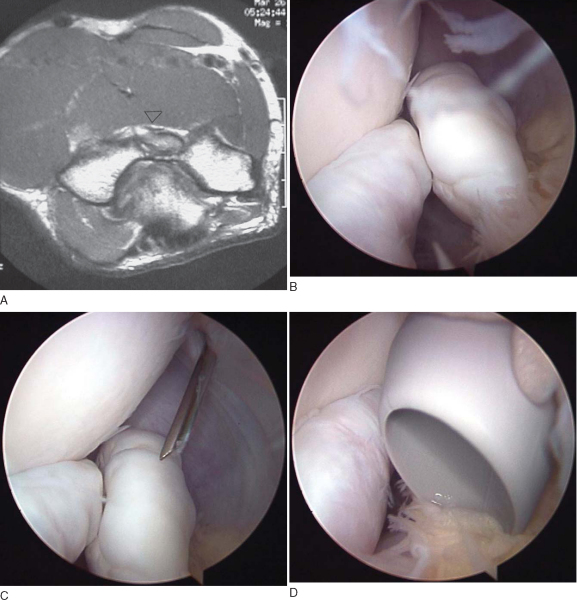
| • | Computed tomographic scanning and magnetic resonance imaging without contrast enhancement can provide additional information and details about synovial disease, particularly loose bodies, osteophytes filling the olecranon and coronoid fossa, capsular thickening, and chondral thinning, as well as useful information about the integrity of the collateral ligaments ( Fig. 34-3 ). |
|
| • | Ultrasonography can also be an inexpensive modality that can provide additional information, especially in assessing collateral ligaments both statically and dynamically. | |
| • | The authors prefer magnetic resonance imaging to assess the structural integrity of the ulnar collateral ligament and to evaluate for intraarticular disease; dynamic ultrasonography is performed for functional assessment. The performance of dynamic ultrasonography requires education and skill of the radiologist in applying a valgus stress to the elbow. |
|
|
|
|
Figure 34-3 |
Indications and Contraindications
In general, there are few absolute indications for surgery in dealing with an athlete. The primary indication is failure to return to competition after nonsurgical management. The most common indications for elbow arthroscopy in this population are removal of a loose body that is closely correlated with mechanical symptoms and loss of motion. The simple appearance of a loose body on radiographs may not necessarily produce symptoms. Most patients complain of locking, catching, or pain toward the extremes of motion.
In addition to osteophyte and loose body removal, arthroscopy is indicated for the treatment of synovial diseases, such as pigmented villonodular synovitis, synovial chondromatosis, and synovial plicae, which often produce debilitating pain, mechanical symptoms, and effusion.
The procedure can be performed under general anesthesia, regional anesthesia, or a combination thereof, depending on the preferences of the surgeon, anesthesiologist, and patient. Most surgeons prefer a general anesthetic because it provides total muscle relaxation as well as allowing immediate postoperative neurologic assessment. The patient is positioned supine if arthroscopy is planned in combination with a reconstructive procedure. The supine position (
Fig. 34-4
) permits a smoother transition to an open procedure, such as collateral ligament reconstruction. Alternatively, arthroscopy can be performed in the prone position or the lateral decubitus position if a padded arm holder is available. Both of these positions can provide excellent arthroscopic exposure, but conversion to an open procedure can be more difficult.
|
|
|
|
Figure 34-4 |
After the patient is properly positioned and landmarks are identified, the elbow is flexed to 90 degrees and the joint is distended with 20 to 40 mL of normal saline through the lateral soft spot (
Fig. 34-5
). This has been shown in cadaveric studies to help protect neurovascular structures by increasing the distance between neurovascular structures and the portals by up to 1 cm.[17]
|
|
|
|
Figure 34-5 |
Surgical Landmarks, Incisions, and Portals
The number and placement of portals may differ, depending on the condition being treated. Most surgeons use two anterior portals and two or three posterior portals. Several studies have suggested different initial portal sites, and there continues to be considerable controversy about the safest initial portal. [1] [2] [4] [5] [11] [17] [21] The most commonly used portals are described in
Table 34-1
.
| Portal | Description | Nearest Neurovascular Structure |
|---|---|---|
| Midlateral | “Soft spot”—center of triangle between olecranon, radial head, capitellum | 7 mm (posterior antebrachial cutaneous nerve) |
| Proximal lateral[1] | 2 cm proximal, 1 cm anterior to lateral epicondyle | 7.9 mm extended, 13.7 mm flexed (radial nerve) |
| Anterolateral[2] | 3 cm distal, 1 cm anterior to lateral epicondyle | 1.4 mm extended, 4.9 mm flexed (radial nerve) |
| Proximal medial[21] | 2 cm proximal, just anterior to medial epicondyle | 12-23 mm (median nerve) |
| Anteromedial[2] | 2 cm distal, 2 cm anterior to medial epicondyle | 2 mm extended, 7 mm flexed (median nerve); 4 mm (median nerve) |
| Posterolateral[5] | Proximal to olecranon, lateral edge of triceps | >15-20 mm |
| Posterocentral[2] (trans-triceps) | Proximal to olecranon, through triceps tendon | >15-20 mm |
Examination Under Anesthesia and Diagnostic Arthroscopy
Before the patient is positioned for arthroscopy, an examination under anesthesia is performed to evaluate range of motion as well as ligamentous stability. After the patient is positioned properly, the diagnostic arthroscopy is performed. The capsule and synovium may be thickened and inflamed, making introduction of the initial cannula difficult. In addition to a thorough inspection of both the anterior and posterior compartments, ligament integrity can be assessed with provocative testing under direct intraarticular visualization. [10] [12] A negative valgus stress does not, however, exclude significant partial tears of the ligament.[16]
Specific Steps (
Box 34-1
)
Whether a lateral or medial portal is established first is a matter of the surgeon’s preference. It is more important that the surgeon develop a routine that is thorough and can be performed consistently. A secondary portal can be established under direct visualization with spinal needle localization if loose bodies are present. Surgeons who advocate establishing a medial portal first and then a lateral portal under direct visualization argue that this is safer because the average distance between the medial portals and the median nerve is greater than the distance between the lateral portals and the radial or posterior interosseous nerve.[4] We prefer to establish a proximal lateral portal as described by Field and Altchek,[10] which is on average 13.7 mm from the radial nerve in a flexed elbow (
Fig. 34-6
). This portal allows broad visualization of the anterior compartment.
| Surgical Steps | ||||||||||||
|
|
|
|
|
Figure 34-6 |
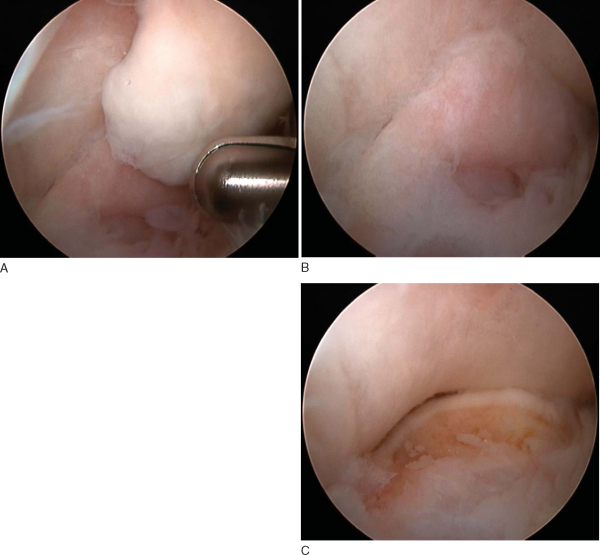
2. Anterior Compartment Assessment and Débridement
When the procedure is started from the lateral portal, examination of the medial gutter is performed first, followed by a search for loose bodies across the entire ante rior compartment from medial to lateral. All fragments should be removed as they are encountered because visualization can change and loose bodies can move to a less accessible area during the procedure. An arthroscopic grasper or shaver is used for smaller fragments or fragments adherent to the capsule. A spinal needle can also be used to stabilize the fragment and prevent it from migrating into a recess. Fluid flow should be well controlled, especially once a loose body has been localized. Allowing outflow at the cannula can help bring the loose body toward the arthroscopic grasper. Very large loose bodies may need to be broken into smaller pieces to be removed through the cannula. This can also be accomplished by removal of the fragment and the cannula in one maneuver after the portal skin incision is extended and the portal carefully dilated with a spreading clamp (
Fig. 34-7
). The camera can also assist in pushing the fragment out through the portal while pulling with the grasper. Sometimes, the plica may be more easily resected by getting a rough edge started with either a bovie or a retractable hook blade. It may be necessary to switch portals and view from the medial side to resect all pathologic tissue completely from the lateral compartment.
|
|
|
|
Figure 34-7 |
An arthroscopic valgus instability test can be performed during viewing from the proximal lateral or anterolateral portal. The medial aspect of the ulnohumeral joint is observed for any gap formation (
Fig. 34-8
). Any gap greater than 2 mm is considered abnormal.[10]
|
|
|
|
Figure 34-8 |
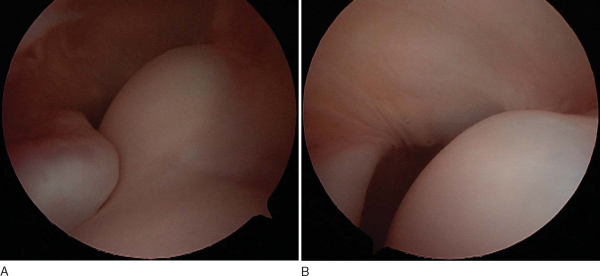
3. Posterior Compartment Assessment and Débridement
After completion of the anterior compartment, a cannula is left in place to maintain joint distention while the transition is made to the posterior compartment. Next, a posterolateral portal is established, which is located just radial to the triceps tendon at the level of the tip of the olecranon. This is the primary viewing portal for work to be done in the posterior compartment. Careful inspection will reveal loose bodies, spurs, chondromalacia, and fibrous debris. Débridement and loose body removal can be accomplished through a posterocentral (trans-triceps) portal (
Fig. 34-9
). The olecranon should be probed because fibrous tissue can often hide fragmentation that may be a source of persistent pain. Extreme caution must be used in operating the motorized shaver, especially while suction is used, because of the proximity of the ulnar nerve along the posteromedial olecranon. The scope can be advanced into the midlateral viewing area to assess the radial gutter and to remove any remaining pathologic tissue along the posterior aspect of the radial head and capitellum. This can also be accomplished by use of a midlateral portal or a 70-degree scope to improve visualization of this small compartment. Most plicae are posterolateral and are best removed by viewing from posterolateral and working from the midlateral portal (
Fig. 34-10
). The plicae can be resected with a motorized shaver.
|
|
|
|
Figure 34-9 |
|
|
|
|
Figure 34-10 |
Portal incisions are closed with 4-0 nylon sutures in a simple interrupted fashion. Sterile dressings are applied, and the arm is placed in a sling for comfort.
Elbow arthroscopy for the removal of loose bodies, débridement, and synovectomy is generally a safe procedure. Complications are uncommon and usually minor. The major concern is for the potential of neurovascular injury. The following complications have been reported [13] [18]:
| • | Direct nerve laceration | |
| • | Nerve compression due to suboptimal portal placement and levering of instruments | |
| • | Postoperative stiffness | |
| • | Potential for further loose body formation | |
| • | Portal drainage | |
| • | Infection |
Arthroscopy for the treatment of posteromedial impingement and elbow joint synovitis and for loose body removal in athletes can reduce pain and improve function. Most athletes are able to return to the same level of their sport after arthroscopic elbow surgery, particularly if no associated instability exists. [3] [6] [9] [14] [20] [22] [23] However, in certain athletes, depending on the type of sport and position played, reoperation rates are high, and return to the previous level of competition is less reliable.[3]
Table 34-2
summarizes clinical results after elbow arthroscopy for posteromedial impingement, loose body removal, and treatment of common synovial diseases.
| Author | Followup | Outcome |
|---|---|---|
| Wilson et al[24] (1983) | 12 months | 5/5 pitchers returned for at least one full season of maximum effectiveness |
| Andrews and Timmerman[3] (1995) | 42 months mean (minimum: 24 months) | 47/59 professional baseball players returned for at least one season (however, 33% reoperation rate, and 25% required ulnar collateral ligament reconstruction) |
| Bradley[6] (1995) | 24 months | 6/6 excellent and good objective and subjective results |
| Reddy et al[22] (2000) | 42.3 months mean (range: 7-115 months) | 47/55 baseball players returned to competition |
| Kim et al[14] (2006) | 33.8 months (range: 24-65.5 months) | 11/12 athletes reported excellent outcome and returned to competition |
1.
Adolfsson L: Arthroscopy of the elbow joint: a cadaveric study of portal placement.
J Shoulder Elbow Surg 1994; 3:53-61.
2.
Andrews JR, Carson WG: Arthroscopy of the elbow.
Arthroscopy 1985; 1:97-107.
3.
Andrews JR, Timmerman LA: Outcome of elbow surgery in professional baseball players.
Am J Sports Med 1995; 23:407-413.
4.
Baker CL, Jones GL: Arthroscopy of the elbow.
Am J Sports Med 1999; 27:251-264.
5.
Burman MS: Arthroscopy of the elbow joint: a cadaveric.
J Bone Joint Surg 1932; 14:349-350.
6.
Bradley JP: Arthroscopic treatment of posterior impingement of the elbow in NFL lineman [abstract].
J Shoulder Elbow Surg 1995; 2:S119.
7.
Callaway GH, Field LD, Deng XH, et al: Biomechanical evaluation of the medial collateral ligament of the elbow.
J Bone Joint Surg Am 1997; 79:1223-1230.
8.
Clarke RP: Symptomatic, lateral synovial fringe (plica) of the elbow joint.
Arthroscopy 1988; 4:112-116.
9.
Fideler BM, Kvitne RS, Jordan S, et al: Posterior impingement of the elbow in professional baseball players: results of arthroscopic treatment [abstract].
J Shoulder Elbow Surg 1997; 6:169-170.
10.
Field LD, Altchek DW: Evaluation of the arthroscopic valgus instability test of the elbow.
Am J Sports Med 1996; 24:177-183.
11.
Field LD, Altchek DW, Warren RF, et al: Arthroscopic anatomy of the lateral elbow: a comparison of three portals.
Arthroscopy 1994; 10:602-607.
12.
Field LD, Callaway GH, O’Brien SJ, et al: Arthroscopic assessment of the medial collateral ligament complex of the elbow.
Am J Sports Med 1995; 23:396-400.
13.
Kelly EW, Morrey BF, O’Driscoll SW: Complications of elbow arthroscopy.
J Bone Joint Surg Am 2001; 83:25-34.
14.
Kim DH, Gambardella RA, ElAttrache NS, et al: Arthroscopic treatment of posterolateral elbow impingement from lateral synovial plicae in throwing athletes and golfers.
Am J Sports Med 2006; 34:1-7.
15.
King JW, Brelsford HJ, Tullos HS: Analysis of the pitching arm of the professional baseball pitcher.
Clin Orthop 1969; 67:116-123.
16.
Kooima CL, Anderson K, Craig JV, et al: Evidence of subclinical medial collateral ligament injury and posteromedial impingement in professional baseball players.
Am J Sports Med 2004; 32:1602-1606.
17.
Lynch GH, Meyers JF, Whipple TL, et al: Neurovascular anatomy and elbow arthroscopy: inherent risks.
Arthroscopy 1986; 2:191-197.
18.
Marshall PD, Faircloth JA, Johnson SR, et al: Avoiding nerve damage during elbow arthroscopy.
J Bone Joint Surg Am 1993; 74:129-131.
19.
Ofluoglu O: Pigmented villonodular synovitis.
Orthop Clin North Am 2006; 37:23-33.
20.
Ogilvie-Harris DJ, Schemitsch E: Arthroscopy of the elbow for removal of loose bodies.
Arthroscopy 1993; 9:5-8.
21.
Poehling GG, Whipple TL, Sisco L, et al: Elbow arthroscopy. A new technique.
Arthroscopy 1989; 5:222-224.
22.
Reddy AS, Kvitne RS, Yocum LA, et al: Arthroscopy of the elbow: a long term clinical review.
Arthroscopy 2000; 16:588-594.
23.
Ward WG, Anderson TE: Elbow arthroscopy in a mostly athletic population.
J Hand Surg Am 1993; 18:220-224.
24.
Wilson FD, Andrews JR, Blackburn TA, et al: Valgus extension overload in the pitching elbow.
Am J Sports Med 1983; 11:83-88.