CHAPTER 24 –
/* Styles NOT for IE6: */
body, fieldset {
overflow:visible;
}
/*—————————————————————————*/
/* Styles from style guide page views, as well as a few customizations. */
/*—————————————————————————*/
/* http://www.hsucd.com/mdc/styleguide/styleguide2.css */
/*—————————————————————————*/
/* The *html and *body hacks below should ONLY be in pages that have */
/* a floating TOC — they will break other pages */
/*—————————————————————————*/
/*
WAS_BOOKAPP_ENABLED is set
*/
#leftPane { position:fixed; }
/* SCCS PageBodyStyle.css %Z% %P% %I% %E% */
/* ???
PRE {font-family: courier new, lucida console; font-size: 9pt;}
CODE {font-family: courier new, lucida console; font-size: 9pt;}
*/
#bodycontent p,
.list,
.text {
}
.part-title,
.part-label {
background:none;
color:#003D6D;
font-size:18px;
font-weight:bold;
}
.part-small-caps,
.section-small-caps {
font-variant:small-caps;
}
#bodycontent h1,
.chapter-title,
.chapter-top-title,
.partsection-author,
.partsection-title {
color:#003D6D;
font-size:16px;
font-weight:bold;
}
.section-title,
.section-label,
.section-title-1,
.section-label-1 {
color:#003D6D;
font-size:16px;
font-weight:normal;
}
#bodycontent h2,
.title,
.section-title-2,
.section-label-2 {
color:#003D6D;
font-size:14px;
font-weight:bold;
}
#bodycontent h3,
.section-title-3,
.section-label-3 {
color:#000;
font-size:14px;
font-weight:normal;
}
#bodycontent h4,
.section-title-4,
.section-label-4,
.sub-section-title {
color:#003D6D;
font-size:13px;
font-weight:bold;
}
#bodycontent h5,
.section-title-5,
.section-label-5 {
color:#000;
font-size:13px;
font-weight:normal;
}
#bodycontent h6,
.section-title-6,
.section-label-6 {
color:#000;
font-size:12px;
font-weight:bold;
}
.section-title-7,
.section-label-7 {
color:#666;
font-size:12px;
font-weight:bold;
}
.section-title-8,
.section-label-8 {
color:#003D6D;
font-size:11px;
font-weight:bold;
}
.figure-text,
.figure-title,
.figure-caption,
.figure-source,
.footnote-figure {
font-size:11px;
}
.figure-source {
font-style:italic;
}
.figure-title,
.headercol,
.head {
font-weight:bold;
}
.sub-head {
color:#999;
font-size:11px;
}
.figure-source {
font-style:italic;
}
.box-sub-section-title {
font-weight:bold;
color:#666;
}
.footnote,
.small {
font-size:11px;
}
.quote {
font-style:italic;
}
.small-caps {
font-variant:small-caps;
}
.cross-out {
text-decoration:line-through;
}
.def-term {
}
.def-list {
font-weight:bold;
}
.def-desc {
font-style: italic;
}
.search-hit {
font-weight:bold;
color:#000;
background:#FCD09C;
}
.rowBGAlt {
background-color:#e4f0fc;
}
.rowBGWhite {
background-color:#FFF;
}
#bodycontent th {
background-color:#e4f0fc;
}
#bodycontent td {
padding:.2em;
}
#bodycontent sup {
/*font-size:11px;*/
padding:0 2px;
/*color:#390;*/
color:#06c;
vertical-align:baseline;
}
#bodycontent a {
text-decoration: none;
}
#bodycontent a.reference-link {
color: #0066CC;
text-decoration: underline;
}
#bodycontent a.reference-link:hover {
color: #FF9900;
text-decoration: none;
}
#bodycontent a.reference-link:active {
color: #FF6600;
text-decoration: underline;
}
/* SCCS style_book.css %Z% %P% %I% %E% */
#leftPaneContent {
background:none;
border:0 none;
}
#tocPane {
border:1px solid #BCBAB4;
}
.player .tabs ul {
margin-left:0;
}
.player .tabbtm {
border-right:1px solid #BCBAB4;
border-bottom:0 none;
border-left:1px solid #BCBAB4;
}
.contents_tree {
line-height:120%;
border-bottom:0 none;
}
.leftNav {
background-image: none;
}
var debugall = 0; // 1 to enable, 0 to disable. >1 for call tracing, >2 for verbose
var has_idx = 1;
var tocTree;
var tocTabs;
var tocFrame;
function initToc()
{
var debug = (debugall) ? debugall : 0; // 1 to enable, 0 to disable.
if (debug>1) {alert(“initToc(ENTER)”);}
// Create the table of contents tree:
tocTree = new elsAjaxTree(‘tocTree’);
// The path to where your image icons are stored:
tocTree.imageFolder = ‘/about/layout/’;
// The URL to request children via AJAX
tocTree.ajaxRequestNodesBaseURL = ‘/das/book/body/1718/toc?fragment=true’;
// Params to include when parents/top nodes aren’t requested
tocTree.ajaxOmitParentsParam = ‘&TOC_ONLY_CHILDREN=true’;
// Params to include when parents/top nodes are requested
tocTree.ajaxRequestParentsParam = ”;
tocTree.activateTree();
tocTabs = dojo.byId(“tocTabs”);
tocFrame = dojo.byId(“tocFrame”);
if (debug) { alert(“initToc(): tree active, tocTabs=”+tocTabs+”, tocFrame=”+tocFrame); }
if (debug>1) {alert(“initToc(EXIT)”);}
}
dojo.addOnLoad(initToc);
var idxTree;
var idxTabs;
var idxFrame;
function initIdx()
{
var debug = (debugall) ? debugall : 0; // 1 to enable, 0 to disable.
if (debug>1) {alert(“initIdx(ENTER)”);}
// Create the index tree:
idxTree = new elsAjaxTree(‘idxTree’);
// The path to where your image icons are stored:
idxTree.imageFolder = ‘/about/layout/’;
// The URL to request children via AJAX
idxTree.ajaxRequestNodesBaseURL = ‘/das/book/body/1718/idx?fragment=true’;
// Params to include when parents/top nodes aren’t requested
idxTree.ajaxOmitParentsParam = ‘&TOC_ONLY_CHILDREN=true’;
// Params to include when parents/top nodes are requested
idxTree.ajaxRequestParentsParam = ”;
idxTree.activateTree();
idxTabs = dojo.byId(“idxTabs”);
idxFrame = dojo.byId(“idxFrame”);
if (debug) { alert(“initIdx(): tree active, idxTabs=”+idxTabs+”, idxFrame=”+idxFrame); }
if (debug>1) {alert(“initIdx(EXIT)”);}
}
dojo.addOnLoad(initIdx);
function showToc()
{
var debug = (debugall) ? debugall : 0; // 1 to enable, 0 to disable.
if (debug>1) {alert(“showToc(ENTER)”);}
idxTabs.style.display = “none”;
tocTabs.style.display = “block”;
idxFrame.style.display = “none”;
tocFrame.style.display = “block”;
if (debug) { alert(“showToc(): displaying toc”); }
if (debug>1) {alert(“showToc(EXIT)”);}
}
function showIdx()
{
var debug = (debugall) ? debugall : 0; // 1 to enable, 0 to disable.
if (debug>1) {alert(“showIdx(ENTER)”);}
tocTabs.style.display = “none”;
idxTabs.style.display = “block”;
tocFrame.style.display = “none”;
idxFrame.style.display = “block”;
if (debug) { alert(“showIdx(): displaying idx”); }
if (debug>1) {alert(“showIdx(EXIT)”);}
}
function showSelectedTab()
{
var debug = (debugall) ? debugall : 0; // 1 to enable, 0 to disable.
var selectedNode = null;
if (debug>1) {alert(“showSelectedTab(ENTER)”);}
if (tocTree)
{
selectedNode = tocTree.getCookie(‘elsTreeSelectedNode’);
}
else if (idxTree)
{
selectedNode = idxTree.getCookie(‘elsTreeSelectedNode’);
}
if (selectedNode)
{
var treename = selectedNode.substring(0,7);
// shows TOC by defaukt when loaded
if (treename && treename == “idxTree”)
{
// switch to Index
showIdx();
if (debug) { alert(“showSelectedTab(): switching to Index”); }
}
}
if (debug>1) {alert(“showSelectedTab(EXIT)”);}
}
//dojo.addOnLoad(showSelectedTab);
/*– SCCS layout/elsAjaxTree.css %Z% %P% %I% %E% –*/
/*—————————————————————————*/
/* Styles for operating the AJAX Tree Widget with the new MDC site design. */
/*—————————————————————————*/
#tocTree img {
float:left;
padding:1px 0;
}
#tocTree a {
display:block;
margin-left:18px;
text-decoration:none;
}
#tocTree a:hover {
text-decoration:underline;
}
#tocTree .vol {
display:block;
margin-left:18px;
}
#idxTree img {
float:left;
padding:1px 0;
}
#idxTree a {
display:block;
margin-left:18px;
text-decoration:none;
}
#idxTree a:hover {
text-decoration:underline;
}
#idxTree .idxtext {
display:block;
margin-left:18px;
}
.selectedTreeNode {
background-color:#eee;
}
.hoverable:hover {
cursor:pointer;
}
.ajaxLoading {
background: url(‘/about/layout/indicator.gif’) center left no-repeat;
margin-left:20px; /* Left spacing */
padding-left:20px;
}
/*#play_art #toc .contents_tree {
background-color:#fff;
list-style:none;
margin:0;
padding:.9em .9em 1.5em;
}*/
#play_book #tocTree .contents_tree {
background-color:#fff;
list-style:none;
margin:0;
padding:.9em .9em 1.5em;
}
#play_journal #tocTree .contents_tree {
background-color:#fff;
list-style:none;
margin:0;
padding:.9em .9em 1.5em;
}
#play_journal #tocTree li {
clear:both;
font-weight:normal;
margin:0;
}
#play_journal #current {
background-color:#fff;
border-top:1px solid #BCBAB4;
border-bottom:1px solid #BCBAB4;
font-weight:bold;
margin:0;
padding:.9em;
}
#play_journal #tocTree .date {
display:block;
font-weight:normal;
margin:0 0 0 18px;
}
#play_journal #tocTree .vol {
color:#000;
display:block;
font-weight:bold;
float:left;
margin:0 0 0 4px;
}
.treeroot {
margin:0px; /* Left spacing */
padding-left:0px;
display:block; /* Initially show sub nodes */
}
.treeroot ul {
margin:1px 0 0;
padding-left:0px;
display:block;
}
/*.treeroot li {
background-position:0;
list-style:none;
margin:0;
padding:0;
}*/
/*.contents_tree {
font-family:Arial,Helvetica,sans-serif;
font-size:12px;
font-size-adjust:none;
font-style:normal;
font-variant:normal;
font-weight:normal;
line-height:120%;
border-bottom:1px solid #BCBAB4;
overflow:auto
}*/
/*.contents_tree ul {
margin-left:10px;
padding-left:0px;
display:block;
}*/
/*.contents_tree li {
background-position:0 .3em;
list-style:none;
margin:0;
padding:.3em 0 .15em 16px;
}*/
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
CHAPTER 24 – Arthroscopic Management of Glenohumeral Arthritis
Shoulder arthroscopy has allowed clinicians to better diagnose and treat abnormalities of the glenohumeral joint. Arthroscopic stabilization and rotator cuff repairs are commonly performed shoulder procedures. [1] [6] [13] The use of arthroscopy has expanded to the treatment of osteoarthritis of various causes. [2] [10] [11] Most patients can tolerate advanced arthritis of the shoulder because it is not a weight-bearing joint. Arthroscopic débridement of the shoulder can be beneficial for removal of loose cartilage fragments, osteophytes, and loose bodies and for synovectomy. Despite the mixed results of arthroscopic débridement of knee arthritis, reports of arthroscopic débridement for shoulder arthritis have been favorable. [3] [7] [12] [14] Whereas shoulder arthroplasty is considered the “gold standard” for the treatment of shoulder osteoarthritis, arthroscopic débridement can be an alternative, especially for young and active patients, to delay the need for prosthetic replacement.
Most patients with shoulder osteoarthritis present with typical shoulder pain that is worse at night. Pain is related to activity. Shoulder osteoarthritis rarely presents with rest pain, with the exception of night pain. The patients also complain of restricted movement of the involved shoulder. A common complaint is difficulty reaching to the back and above the head. Severe forms of osteoarthritis of the shoulder will also have painful crepitation. Patients may also complain of a locking and clicking sensation if loose bodies are present.
It is extremely important to determine what the perceived limitations are for the patient. If the patient’s main complaint is stiffness, arthroscopic débridement alone may not suffice, and arthroscopic cheilectomy or capsulotomy may be needed to improve postoperative motion. If the patient also shows symptoms of subacromial bursitis, subacromial decompression should be performed to address disease in the subacromial space.
Physical examination usually demonstrates limited range of motion. Most patients who have a large inferior humeral spur will have limited forward flexion. Patients with a flattened humeral head will have limited external and internal rotation. Strength of the rotator cuff tendons is usually preserved; however, strength testing can be limited secondary to pain. Patients can also exhibit bursitis-type symptoms. As with all shoulder complaints, a full cervical examination should be performed to rule out referred pain from degenerative disease of the cervical spine.
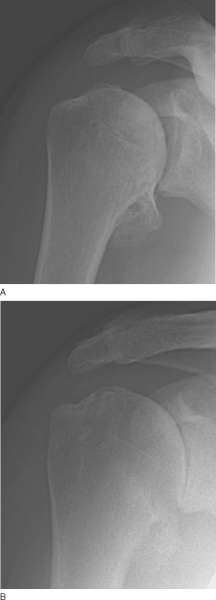
Plain radiographs demonstrate narrowing of the glenohumeral joint space. Orthogonal views can demonstrate the location of the humeral osteophytes. Standard radiographs include anteroposterior (
Fig. 24-1A
), axillary lateral (
Fig. 24-1C
), and scapula Y views of the glenohumeral joint and an anteroposterior view of the acromioclavicular joint. For patients presenting with predominantly arthritic symptoms, weight-bearing views of the glenohumeral joint should be performed to better diagnose the amount of joint space narrowing (
Fig. 24-1B
). For the weight-bearing view, an anteroposterior glenohumeral joint radiograph is taken with the patient holding a 1-pound weight in the hand with the shoulder abducted at around 30 to 45 degrees. This is analogous to the weight-bearing view of the lower extremities to demonstrate true joint space under load. This is extremely helpful for patients with inflammatory arthritis, where there can be absence of large osteophytes.
|
|
|
|
Figure 24-1 |
Magnetic resonance imaging can be obtained but is usually not required; it is, however, useful to investigate early arthritis to demonstrate the presence of cartilage wear. It can also show labral and rotator cuff disease. These lesions can be addressed concomitantly during surgery. Magnetic resonance imaging can also demonstrate the significance of posterior wear of the glenoid. The axial images from this three-dimensional analysis can help quantify the amount of glenoid deficiency.
Preoperative radiographic studies can be extremely helpful to define the size and position of osteophytes; a three-dimensional study like magnetic resonance imaging or computed tomography is best to achieve this. Another important evaluation is the shape of the glenoid. A bilobed glenoid, representing significant posterior wear, may require glenoidplasty or indicate less favorable outcome (
Fig. 24-2
).
|
|
|
|
Figure 24-2 |
Preoperative injections can be helpful to predict the patient’s response to surgery. Selective injection to the glenohumeral and subacromial space can be performed to determine the relative contribution of each compartment to the patient’s symptoms.
Indications and Contraindications
Understanding the etiology of shoulder osteoarthritis is extremely important. Patients with concentric glenoid wear may benefit from débridement and synovectomy, whereas patients with large osteophytes may benefit from cheilectomy and capsulotomy. The patient’s complaints are the most important guide as to which structural abnormalities need to be addressed surgically. Especially severe posterior wear of the shoulder with a bilobed glenoid may not benefit from surgical débridement and glenoidplasty. Patients who have anterior superior migration with acetabulization of the glenoid may also not benefit significantly from arthroscopic surgeries. In my practice, I have found that selective injection to the glenohumeral and subacromial space can help predict the response of the patients to arthroscopic treatment.
Most of the patients receive an interscalene block with general anesthesia. The interscalene block minimizes the use of narcotics intraoperatively and will decrease the incidence of postoperative nausea and complications. The block is also helpful for postoperative pain control so that the patients can transition smoothly to oral pain medication.
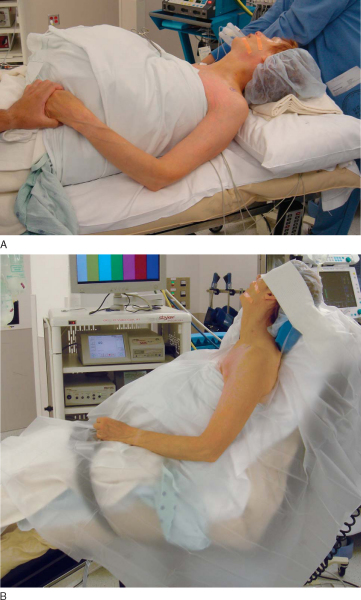
Arthroscopic débridement of the shoulder can be performed in either the beach chair or lateral position. In this chapter, the setup for a beach chair position is outlined.
For the beach chair position, I use a regular operating room table with a full-length beanbag (
Fig. 24-3
). I prefer this setup as it can accommodate patients with various body habitus and weights. A beach chair position add-on device to the operating table can make setup easy and quick; however, patients who are large or small may not fit as well as with a beanbag.
|
|
|
|
Figure 24-3 |
The patient is first positioned with the bed in a reflex position with the foot of the table flexed. The back of the table is then raised up to the beach chair position. The reflex position will prevent the patient’s slipping toward the end of the bed. The beanbag is then folded in to expose the operative shoulder. The operative shoulder is exposed up to the medial border of the scapula. The beanbag is then wrapped around the head and the lower torso while it is being inflated. This setup allows excellent control of the body and the head during the operation. After the beanbag is inflated, the patient and the beanbag are then shifted over to the edge of the table to expose the operative shoulder. Because the full-length beanbag is cradling the patient, this is a stable setup and will expose the operative shoulder nicely (see
Fig. 24-3
). An arm-holding device facilitates positioning and traction of the shoulder.
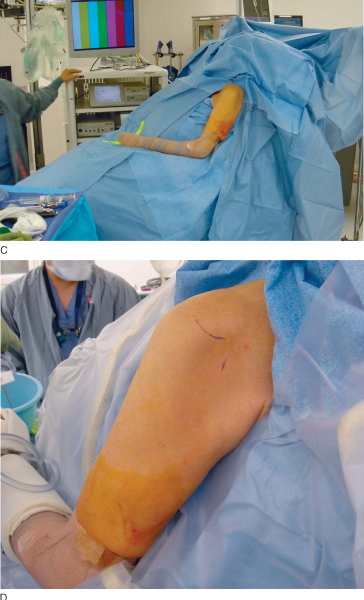
Surgical Landmarks, Incisions, and Portals
For arthroscopic débridement of the shoulder, standard shoulder arthroscopy portals can be used. A posterior arthroscopy portal is used for diagnostic arthroscopy. The landmark for the portal is the posterior soft spot of the shoulder. An anterior portal is used as the working portal. The landmark of the anterior portal is just lateral to the tip of the coracoid process. An accessory posterior portal can be used for access to the inferior part of the shoulder for removal of loose bodies and inferior osteophytes. The landmark for the accessory posterior portal is 2 cm below and in line with the standard posterior portal. [4] [5] The accessory portal should be established by spinal needle localization under direct visualization (
Fig. 24-4
).
|
|
|
|
Figure 24-4 |
Diagnostic arthroscopy is performed to reveal any labral or rotator cuff tears, which can be addressed concomitantly. A torn labrum or frayed rotator cuff can be débrided with a mechanical shaver or repaired if appropriate.
Specific Steps (
Box 24-1
)
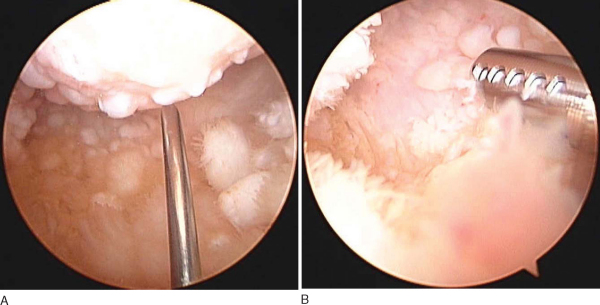
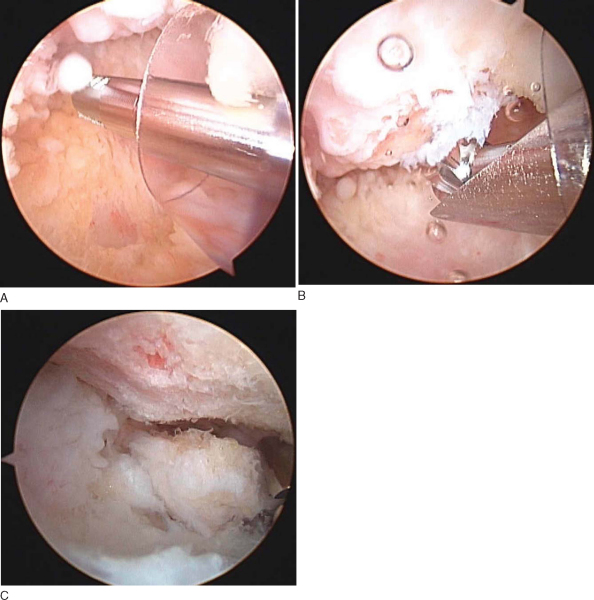
1. Débridement, Synovectomy, and Removal of Osteophytes
A thermal coagulation device is used to remove any inflamed synovium. Biceps tendon tears affecting more than 50% of the tendon width should be treated with a biceps tenotomy or tenodesis, depending on the activity level of the patient. This portion of the operation should be discussed with the patient preoperatively regarding the incidence of biceps deformity after tenotomy. After débridement of the soft tissues, excessive osteophytes can be removed with a narrow osteotome or mechanical bur. The accessory posterior portal can be helpful for access to the inferior portion of the shoulder (
Fig. 24-5
). Previous cadaveric studies have shown that the accessory portal provides safe access to the inferior capsule; the average distance between the portal and the axillary nerve is approximately 3 cm. When cheilectomy of the inferior osteophyte is performed, a mechanical bur can be used. The lateral attachment of the inferior capsule represents the inferior part of the anatomic neck of the humerus. An inferior osteophyte will be medial but inferior to the reflection of the capsule (
Fig. 24-5B
). I usually use the attachment of the inferior capsule to define where the normal anatomic neck is; cheilectomy can be performed safely medial to it. Frequent intraoperative radiographic or fluoroscopic evaluation is extremely helpful to determine the extent of the excision (
Fig. 24-6
). Large loose bodies can also be removed through the accessory posterior portal (
Fig. 24-7
).
| Surgical Steps | |||||||||
|
|
|
|
|
Figure 24-5 |
|
|
|
|
Figure 24-6 |
|
|
|
|
Figure 24-7 |
Microfracture can be performed on contained lesions on the humerus and glenoid; however, the outcome of this procedure in the shoulder has not been well documented. Glenoidplasty can also be performed to reshape the concavity of the shoulder. This is a more extensive procedure, and in my experience, I have not found significant benefit.
For stiff shoulders, capsulotomy can also be performed arthroscopically to increase range of motion. Following standard procedure for capsular release as outlined elsewhere in greater detail, this is usually performed with a thermal coagulation device at a low temperature setting. The anterior capsule is cut close to the glenoid from the rotator interval superiorly to the 5-o’clock position inferiorly. [8] [15] The axillary nerve is closest to the capsule in this location, and it is usually safer first to elevate the capsule off the inferior musculature and then carefully to cut it under direct visualization. This can also be performed with the thermal coagulation device under the capsule, cutting toward the joint to protect the axillary nerve that is inferior to the capsule. The arthroscope is then switched to the anterior portal to complete the posterior capsulotomy through the posterior portal.
After intraarticular examination and dissection, I proceed to the subacromial space. If a significant amount of bursitis is present, a subacromial bursectomy is performed. Acromioplasty is not needed unless the patient has a large acromial spur and had signs of impingement symptoms preoperatively.
The patients are allowed full range of motion after débridement. They are encouraged to work on end range of motion early, especially after capsulotomy and removal of osteophytes. Strengthening of the rotator cuff tendons usually begins 3 to 4 weeks after surgery.
The risk of arthroscopic débridement is similar to the risk of any shoulder arthroscopic surgery. With the excision of osteophytes and glenoidplasty, there is a higher risk of bleeding and potential injury to the axillary nerve in dissecting inferiorly. Regional anesthesia is helpful in this setting as the patient should not be paralyzed and the axillary nerve can react if any dissecting equipment is close.[15]
There has been a paucity of long-term results on arthroscopic débridement of the shoulder; most of the reports are case series without any comparison or control group. There are also a variety of recommendations regarding the need for glenoidplasty and subacromial decompressions. The results are summarized in
Table 24-1
.
| Author | No. of Patients | Followup | Treatment | Outcome |
|---|---|---|---|---|
| Ellman et al[7] (1992) | 18 | 6 months-3 years | Arthroscopic subacromial decompression | Subjective improvement |
| Weinstein et al[14] (2000) | 25 | 30 months | Lavage, débridement, bursectomy | 80% good–excellent |
| Kelly et al[9] (2000) | 14 | 34 months | Glenoidplasty | 80% good–excellent |
| Cameron et al[3] (2002) | 61 | 45 patients with minimum of 2 years | Débridement with and without capsular release | 87% would have surgery again |
| 88% improvement in pain | ||||
| Safran et al[12] (2002) | 17 | Prospective 4-year study, minimum of 1 year | Débridement plus bursectomy | 85% good to excellent at 6 months |
| 70% at 2-4 years |
1.
Bishop J, Klepps S, Lo IK, et al: Cuff integrity after arthroscopic versus open rotator cuff repair: a prospective study.
J Shoulder Elbow Surg 2006; 15:290-299.
2.
Bishop JY, Flatow EL: Management of glenohumeral arthritis: a role for arthroscopy?.
Orthop Clin North Am 2003; 34:559-566.
3.
Cameron BD, Galatz LM, Ramsey ML, et al: Non-prosthetic management of grade IV osteochondral lesions of the glenohumeral joint.
J Shoulder Elbow Surg 2002; 11:25-32.
4.
Davidson PA, Rivenburgh DW: The 7-o’clock posteroinferior portal for shoulder arthroscopy.
Am J Sports Med 2002; 30:693-696.
5.
Difelice GS, Williams 3rd RJ, Cohen MS, Warren RF: The accessory posterior portal for shoulder arthroscopy: description of technique and cadaveric study.
Arthroscopy 2001; 17:888-891.
6.
Edwards TB, Walch G, Nove-Josserand L, et al: Arthroscopic débridement in the treatment of patients with isolated tears of the subscapularis.
Arthroscopy 2006; 22:941-946.
7.
Ellman H, Harris E, Kay SP: Early degenerative joint disease simulating impingement syndrome: arthroscopic findings.
Arthroscopy 1992; 8:482-487.
8.
Esmail AN, Getz CL, Schwartz DM, et al: Axillary nerve monitoring during arthroscopic shoulder stabilization.
Arthroscopy 2005; 21:665-671.
9.
Kelly EW, Steinmann SP, O’Driscoll SW. Arthroscopic glenoidplasty for advanced glenohumeral osteoarthritis. Presented at the 67th annual meeting of the American Academy of Orthopaedic Surgeons; Orlando, Fla; 2000.
10.
McCarty 3rd LP, Cole BJ: Nonarthroplasty treatment of glenohumeral cartilage lesions.
Arthroscopy 2005; 21:1131-1142.
11.
Parsons 4th IM, Weldon 3rd EJ, Titelman RM, Smith KL: Glenohumeral arthritis and its management.
Phys Med Rehabil Clin N Am 2004; 15:447-474.
12.
Safran MR, Wolde-Tsadik G, Crawford D. Prospective outcome study of arthroscopic débridement of grade IV glenohumeral arthritis. Presented at the annual meeting of the American Academy of Orthopaedic Surgeons; Dallas, Texas; 2002.
13.
Verma NN, Dunn W, Adler RS, et al: All-arthroscopic versus mini-open rotator cuff repair: a retrospective review with minimum 2-year followup.
Arthroscopy 2006; 22:587-594.
14.
Weinstein DM, Bucchieri JS, Pollock RG, et al: Arthroscopic débridement of the shoulder for osteoarthritis.
Arthroscopy 2000; 16:471-476.
15.
Wong KL, Williams GR: Complications of thermal capsulorrhaphy of the shoulder.
J Bone Joint Surg Am 2001; 83(suppl 2 pt 2):151-155.