CHAPTER 18 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
CHAPTER 18 – Arthroscopic Subscapularis Repair
Anthony A. Romeo, MD
An all-arthroscopic repair of the subscapularis tendon has seen significant interest in the past 10 years. As we refine our knowledge and arthroscopic techniques in repairing other rotator cuff tears, we are now more capable of addressing subscapularis tears in an all-arthroscopic fashion as well. The main advantages of an all-arthroscopic repair of the subscapularis tendon are smaller incisions, less postoperative pain, and the ability to better visualize and address coexisting pathologic processes, including labral tears and posterior superior rotator cuff tears. This chapter addresses the preoperative considerations and the techniques involved in performing an arthroscopic subscapularis repair.
In most cases, isolated high-grade subscapularis tears are a result of trauma. Most patients describe an event with excessive external rotation of the shoulder or with resistance to forceful external rotation. Some patients hear a “pop” and others feel the shoulder “slipping out of place.” In older individuals, tears may be associated with shoulder dislocations. Presenting complaints include anterior shoulder pain and difficulty reaching behind the back or tucking in a shirttail. These complaints can be relatively nonspecific, and it is important to consider the multiple causes of anterior shoulder pain, including acromioclavicular joint arthrosis or dislocation, biceps tendon tears or inflammation, anterior capsulolabral damage, and fractures of the lesser tuberosity.
As with all shoulder conditions, physical examination begins with a thorough examination of the shoulder including observation, range of motion, and strength testing. The two most common physical examination findings associated with subscapularis tears are increased external rotation compared with the opposite side and weakness of internal rotation. External rotation is evaluated with the arm at the side and compared with the opposite extremity.
Because other muscles, such as the pectoralis major, are strong internal rotators of the shoulder, special tests can isolate the subscapularis for assessment of internal rotation strength. The belly press test is performed by asking the patient to press the ipsilateral hand on the abdomen, maintaining the elbow anterior to the body. If the patient is not able to keep the elbow anterior to the trunk or if the wrist is flexed in attempting to press into the abdomen, the belly press test result is considered positive and the subscapularis is not functioning. The liftoff test requires the patient to be able to place the ipsilateral hand behind the back. The patient is asked to lift the hand off the back; if the patient is unable to do so, the test result is considered positive. A modification to this test, also known as the subscapularis lag test, involves placing the patient’s ipsilateral hand in maximum internal rotation off the back. The examiner asks the patient to keep the hand off the back as the hand is released. If the patient is not able to maintain the hand away from the body and the hand falls onto the back, the lag test result is considered positive.
A standard shoulder imaging series including an axillary view is obtained to assess for alternative pathologic changes, such as fractures and glenohumeral arthritis. Magnetic resonance imaging is the “gold standard” imaging modality for diagnosing subscapularis tendon tears. Magnetic resonance arthrography improves the sensitivity of diagnosis of questionable tears. The magnetic resonance image provides information about the quality of the muscle belly, the amount of fatty infiltration, and any displacement of the long head of the biceps tendon (
Fig. 18-1
). The tendon should be assessed on both axial and sagittal images with verification of its insertion on the lesser tuberosity.
Indications and Contraindications
The most common indication for subscapularis repair is pain nonresponsive to conservative management. In younger individuals, consideration for repair in the absence of pain should be given to restore normal shoulder mechanics. Important secondary indications are restoration of shoulder function and, in selected cases, treatment of recurrent shoulder instability.
Relative contraindications to surgery include lack of pain, severe atrophy, retraction or significant fatty degen eration on magnetic resonance imaging, and rotator cuff tear arthropathy. Absolute contraindications are severe medical illness precluding anesthesia and ongoing active infection. The decision to perform an open or arthroscopic procedure should be based on the surgeon’s individual comfort level with the chosen technique. Open repair and arthroscopic repair are simply different techniques, and the ultimate surgical goals are the same regardless of which technique is chosen.
Most patients are placed under general anesthesia. We prefer to supplement every case with an interscalene block. This reduces the amount of anesthetic required during the case and improves pain control in the postoperative period. If the patient’s medical condition does not allow general anesthesia, regional anesthesia can be performed alone with sedation. Maintenance of a mean arterial pressure of 70 to 90 mm Hg or a systolic pressure near 100 mm Hg allows maximal visualization and minimizes bleeding. We have also used epinephrine in the arthroscopic solution to help control bleeding and to maximize visualization.
We prefer the beach chair position for arthroscopic repairs of the subscapularis (
Fig. 18-2
). It is a familiar position and allows the surgeon to attend to other pathologic lesions at the same time. The upper extremity can be easily moved and rotated to better visualize the subscapularis and its insertion. Furthermore, the beach chair position allows the surgeon to convert to an open procedure if necessary.
The patient is aligned on the edge of the table so that the affected shoulder and scapula are exposed. We place two folded towels on the medial edge of the scapula to retract it farther laterally. The back of the table is elevated completely to position the acromion parallel to the floor. The head is secured to the operating table with tape, or an optional head rest may be used if the table allows it. Care should be taken to prevent excessive flexion or extension in the neck.
Surgical Landmarks, Incisions, and Portals
We begin every case by outlining the bony landmarks on the skin. The posterior and anterior corners of the acromion as well as the soft spot between the posterior clavicle and anterior scapular spine are marked first. A line is drawn between the two corners of the acromion. The anterior and posterior edges of the clavicle are marked next along with the scapular spine. The acromioclavicular joint is palpated and marked. Finally, a circle is drawn over the prominence of the coracoid.
The posterior portal is the first portal to be established. With use of a three-finger shuck, the index finger of the same hand as the shoulder being operated on is placed in the soft spot between the clavicle and scapular spine. The middle finger is placed on the coracoid, and the thumb feels the interval between the infraspinatus and teres minor. This helps the surgeon find the best location for the posterior portal.
The anterior portal is generally placed just lateral to the coracoid and below the coracoacromial ligament. Although this portal can easily be established in outside-in technique by use of a spinal needle, we prefer to establish it through an inside-out technique. This involves driving the arthroscope anteriorly beneath the biceps tendon and gently pushing against the anterior capsule. The arthroscope is removed, and a Wissinger rod is pushed through the scope cannula to make a puncture hole in the rotator interval. The skin is tented anteriorly, and a No. 11 knife blade is used to make the skin incision. The rod is pushed through the skin incision, and a 6-mm clear cannula equipped with an outflow attachment is placed over the rod into the joint. The Wissinger rod is withdrawn, and the arthroscope is reintroduced.
An accessory anterolateral portal is made in all subscapularis repairs. This portal is located in the rotator interval anterior and medial to the anterolateral corner of the acromion. This places it about 1 to 2 cm superior and 2 cm lateral to the standard anterior portal. A spinal needle is used to localize this portal, with an intraarticular entrance site just posterior to the native biceps tendon (
Fig. 18-3
). After the portal is made, it is enlarged to allow the placement of a threaded 6-mm clear cannula. It is important not to place the two anterior portals too close to each other. This portal is established after sufficient anterior débridement is performed and the lesser tuberos ity is exposed. In most cases, the biceps tendon is released for later tenodesis as discussed later.
|
|
|
|
Figure 18-3 (Redrawn from Fox JA, Noerdlinger MA, Sasso LM, Romeo AA. Arthroscopic subscapularis repair. In Miller MD, Cole BJ, eds. Textbook of Arthroscopy. Philadelphia, Elsevier, 2004.) |
Examination Under Anesthesia and Diagnostic Arthroscopy
A thorough examination of both shoulders under anesthesia is performed on every patient after induction of anesthesia but before positioning. Range of motion, signs of instability, and arthritis are documented. Any previous surgical scars are marked and reused if possible.
We always start our procedures by performing a diagnostic glenohumeral arthroscopy. Any intraarticular pathologic process is addressed. If a coexisting superior cuff tear is present, we prefer to complete our subacromial work and superior cuff repair first before proceeding with subscapularis repair. This helps limit swelling of the shoulder and provides an easier working environment in the subacromial space.
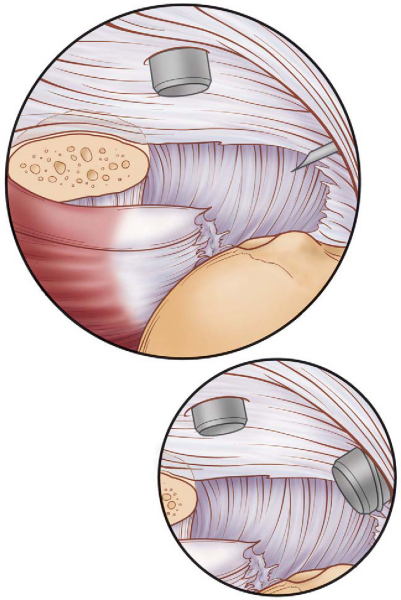
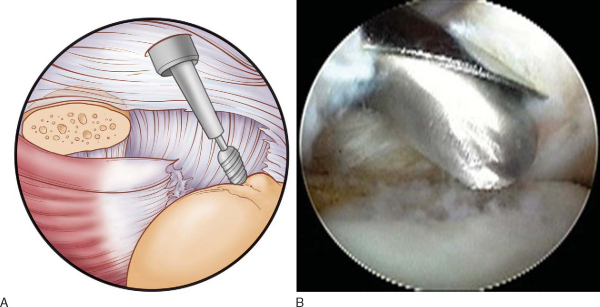
A dynamic examination of the subscapularis insertion is performed by advancing the arthroscope to the anterior aspect of the glenohumeral joint. The lens is pointed to look laterally and the shoulder is internally rotated. If significant retraction has occurred, it is possible to see the conjoined tendons and note the medial displacement of the long head of the biceps. A probe or a grasper can be used to examine the extent of the tear (
Fig. 18-4
).
|
|
|
|
Figure 18-4 (A redrawn from Fox JA, Noerdlinger MA, Sasso LM, Romeo AA. Arthroscopic subscapularis repair. In Miller MD, Cole BJ, eds. Textbook of Arthroscopy. Philadelphia, Elsevier, 2004.) |
Specific Steps (
Box 18-1
)
In many cases of significant subscapularis tear, the biceps tendon anchor within the bicipital groove has been disrupted, and the tendon itself is subluxed medially. We have not attempted to resuspend the biceps within the intertubercular groove. Rather, in almost all cases, our preference is to release the biceps tendon intra-articularly at the superior labrum and to perform an open subpectoral biceps tenodesis once the subscapularis repair has been completed. This approach is helpful for two reasons. First, it allows increased visualization and working area within the anterior shoulder as the biceps is now absent. Second, it eliminates any possibility of recurrent biceps subluxation or persistent pain from stenosis of the tendon or from a biceps tendon abnormality within the groove.
This step is somewhat analogous to performing a subacromial decompression. By removal of bone from the postero lateral tip of the coracoid, two goals are met. First, there is extra space for the technical aspect of the subscapularis repair to be performed. Second, it provides the repaired subscapularis more space, with no mechanical impingement from the coracoid.
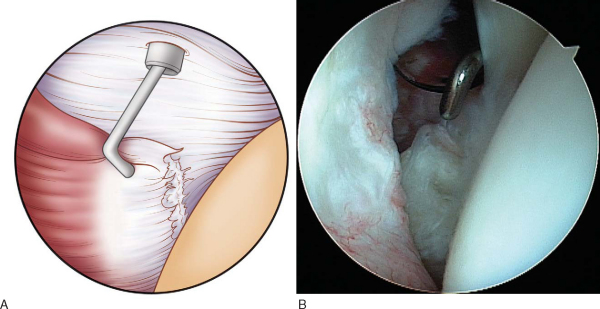
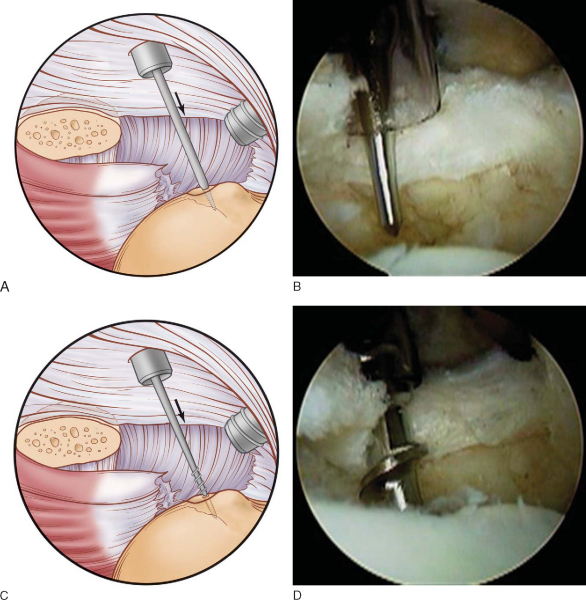
We start with débridement of the capsular tissue of the rotator interval at the superior edge of the subscapularis to expose the coracoid (
Fig. 18-5
), by use of a combination of a mechanical shaver and a radiofrequency device, working through the anterior portal. This area can be quite vascular, and prompt attention to any bleeding is required to maintain visualization. By keeping the shaver on the lateral edge of the coracoid, no neurovascular structures will be violated. Once the coracoid is reached, an electrothermal device is used to further remove the soft tissue attachment on the tip of the coracoid and expose the undersurface. A 4.0-mm bur is then used to remove about 5 mm of the posterolateral tip of the coracoid, again working through the anterior portal (
Fig. 18-6
).
|
|
|
|
Figure 18-5 (A redrawn from Fox JA, Noerdlinger MA, Sasso LM, Romeo AA. Arthroscopic subscapularis repair. In Miller MD, Cole BJ, eds. Textbook of Arthroscopy. Philadelphia, Elsevier, 2004.) |
|
|
|
|
Figure 18-6 (A redrawn from Fox JA, Noerdlinger MA, Sasso LM, Romeo AA. Arthroscopic subscapularis repair. In Miller MD, Cole BJ, eds. Textbook of Arthroscopy. Philadelphia, Elsevier, 2004.) |
3. Mobilization of Subscapularis
By use of a grasper or a probe placed through the anterior portal, the mobility of the torn subscapularis is assessed. If the tendon can be reduced to the lesser tuberosity relatively tension free, one can proceed directly to the repair. If, on the other hand, the tendon is not mobile, soft tissue dissection must be performed, most commonly by use of a radiofrequency device. This involves first releasing the soft tissue fibrous attachments between the coracoid and subscapularis. A release of the coracohumeral ligament and the anterior capsule is also helpful. Finally, the middle glenohumeral ligament, which crosses at a 45-degree angle to the tendon, should be released by a shaver or an electrothermal device.
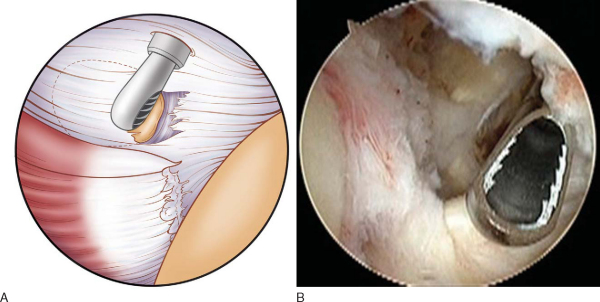
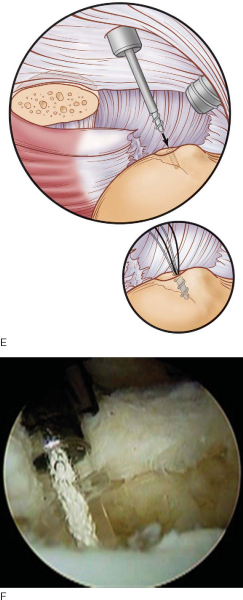
4. Preparation of the Tendon Edge and Lesser Tuberosity
A 5.0-mm shaver is inserted through the anterior portal and used to freshen up and remove the frayed edges of the torn subscapularis. Next, the shoulder is internally rotated and slightly abducted to visualize the lesser tuberosity. A 4.0-mm bur is placed through the anterolateral portal and used to prepare the bony bed for placement of suture anchors (
Fig. 18-7
). In most cases, the tendon insertion is slightly medialized, and a small amount of the articular surface is included in the resection.
|
|
|
|
Figure 18-7 (A redrawn from Fox JA, Noerdlinger MA, Sasso LM, Romeo AA. Arthroscopic subscapularis repair. In Miller MD, Cole BJ, eds. Textbook of Arthroscopy. Philadelphia, Elsevier, 2004.) |
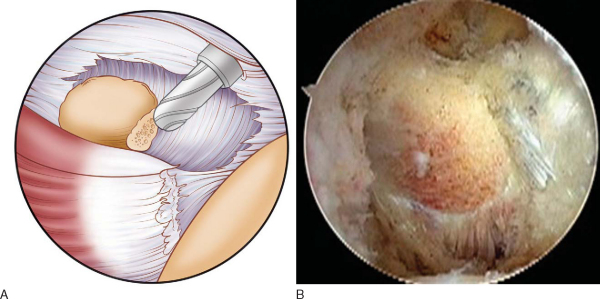
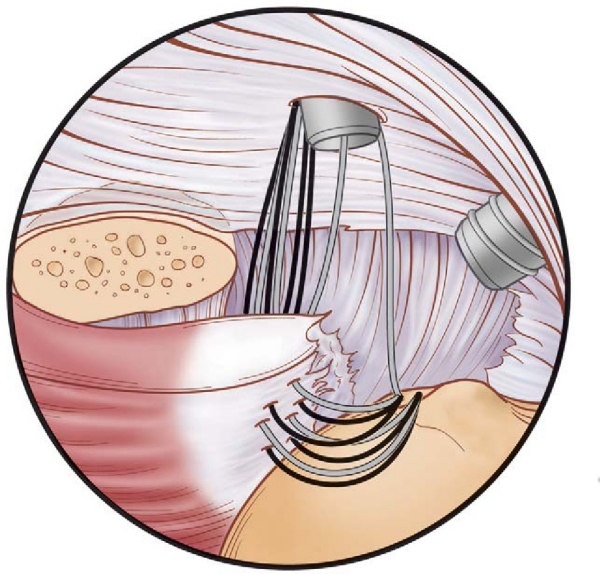
The suture anchors are placed through the anterior portal (
Fig. 18-8
). This portal allows optimal anchor placement at a 45-degree angle to the bone (dead man’s angle). We prefer to use double-loaded anchors because they provide better stability for the repair. We place the anchors initially at the inferior edge of the subscapularis footprint before proceeding superiorly, which allows us good visualization throughout the repair process. We separate the anchors by 5 to 8 mm. In general, partial repairs can be accomplished with one or two anchors; a maximum of three anchors is required for complete ruptures.
|
|
|
|
Figure 18-8 (A, C, and E redrawn from Fox JA, Noerdlinger MA, Sasso LM, Romeo AA. Arthroscopic subscapularis repair. In Miller MD, Cole BJ, eds. Textbook of Arthroscopy. Philadelphia, Elsevier, 2004.) |
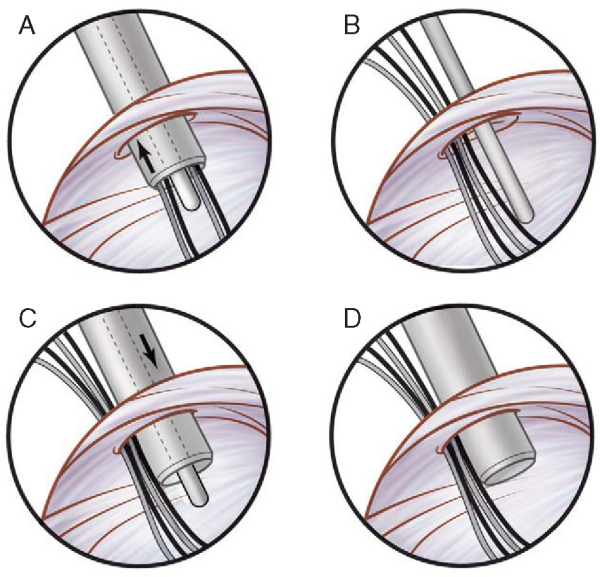
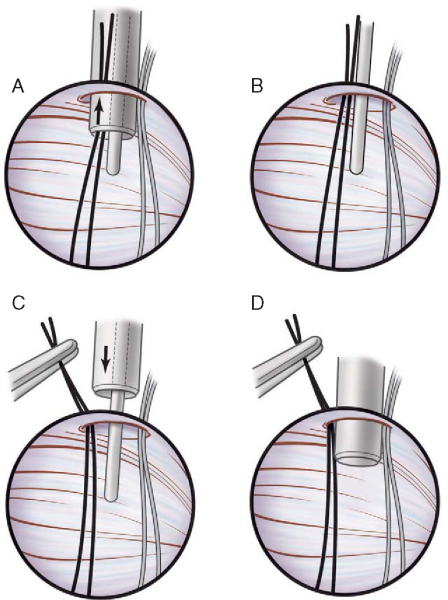
6. Suture Management and Passage
To aid in suture management, a switching stick is placed through the anterior cannula, and the cannula is removed. The sutures are then pulled out of the cannula, and a hemostat is placed on them. The cannula is placed back over the switching stick into the joint (
Fig. 18-9
). This leaves the anterior cannula empty to facilitate the use of shuttling devices. To perform the repair, we use a 30-degree suture lasso (Arthrex, Naples, FL), a curved Spectrum device (Linvatec, Utica, NY), or a penetrator (Arthrex, Naples, Fla).
|
|
|
|
Figure 18-9 (Redrawn from Fox JA, Noerdlinger MA, Sasso LM, Romeo AA. Arthroscopic subscapularis repair. In Miller MD, Cole BJ, eds. Textbook of Arthroscopy. Philadelphia, Elsevier, 2004.) |
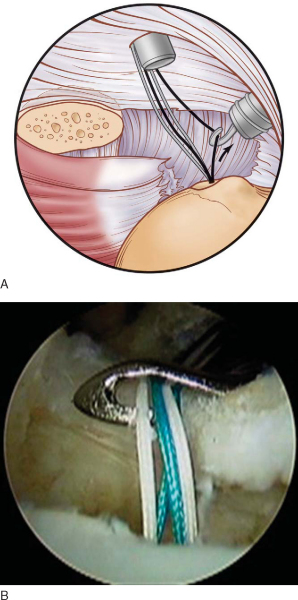
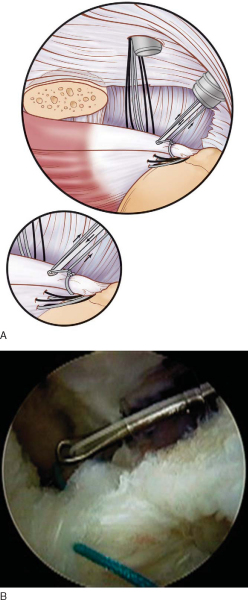
The suture limb that will be placed in the subscapularis is pulled from the anterior portal out through the anterolateral portal by a crochet hook (
Fig. 18-10
). The suture lasso or the Spectrum device is placed through the anterior portal and used to penetrate the tendon. The suture should be passed at an angle from lateral to medial through the entire thickness of the tendon.
|
|
|
|
Figure 18-10 (A redrawn from Fox JA, Noerdlinger MA, Sasso LM, Romeo AA. Arthroscopic subscapularis repair. In Miller MD, Cole BJ, eds. Textbook of Arthroscopy. Philadelphia, Elsevier, 2004.) |
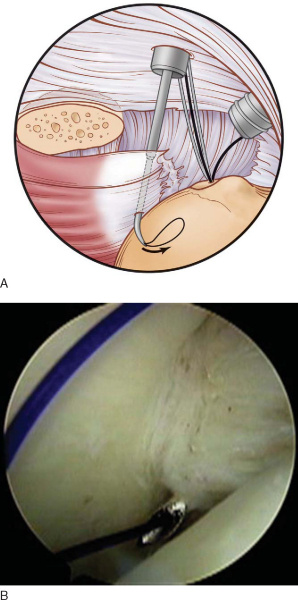
Once the passage device has penetrated through the tendon, its nitinol loop or polydioxanone (PDS) suture is advanced (
Fig. 18-11
) and retrieved with the crochet hook through the anterolateral portal.
|
|
|
|
Figure 18-11 (A redrawn from Fox JA, Noerdlinger MA, Sasso LM, Romeo AA. Arthroscopic subscapularis repair. In Miller MD, Cole BJ, eds. Textbook of Arthroscopy. Philadelphia, Elsevier, 2004.) |
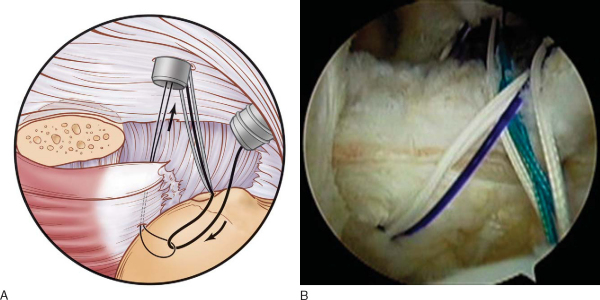
The anchor suture is then fixed to the passing wire or suture and shuttled through the tendon and back out the anterior portal (
Fig. 18-12
). Care must be taken not to unload the anchor.
|
|
|
|
Figure 18-12 (A redrawn from Fox JA, Noerdlinger MA, Sasso LM, Romeo AA. Arthroscopic subscapularis repair. In Miller MD, Cole BJ, eds. Textbook of Arthroscopy. Philadelphia, Elsevier, 2004.) |
The same process is repeated for the other suture limb, resulting in a mattress configuration in the subscapularis tendon (
Fig. 18-13
). Once both limbs have been retrieved, they are placed outside of the anterior cannula by the switching stick technique (
Fig. 18-14
). A hemostat is again placed to secure the two limbs, and the process is repeated for the next anchor. At the end of this process, two mattress sutures should be passed through the subscapularis tendon. It is important to place the sutures at least 5 mm apart to achieve optimal fixation.
|
|
|
|
Figure 18-13 (Redrawn from Fox JA, Noerdlinger MA, Sasso LM, Romeo AA. Arthroscopic subscapularis repair. In Miller MD, Cole BJ, eds. Textbook of Arthroscopy. Philadelphia, Elsevier, 2004.) |
|
|
|
|
Figure 18-14 (Redrawn from Fox JA, Noerdlinger MA, Sasso LM, Romeo AA. Arthroscopic subscapularis repair. In Miller MD, Cole BJ, eds. Textbook of Arthroscopy. Philadelphia, Elsevier, 2004.) |
7. Additional Anchor Placement
It is up to the surgeon’s preference to tie sutures immediately or after placement of all remaining anchors. We prefer to tie the sutures last because in our hands, this allows better visualization and thus improved placement of the remaining anchors and sutures.
The same process is repeated to place the sutures through the upper edge of the tendon. Only one limb of the second suture on the last anchor is placed through the tendon (
Fig. 18-15
). This will be the first suture to be tied and will allow restoration of the height of the tendon.
|
|
|
|
Figure 18-15 (Redrawn from Fox JA, Noerdlinger MA, Sasso LM, Romeo AA. Arthroscopic subscapularis repair. In Miller MD, Cole BJ, eds. Textbook of Arthroscopy. Philadelphia, Elsevier, 2004.) |
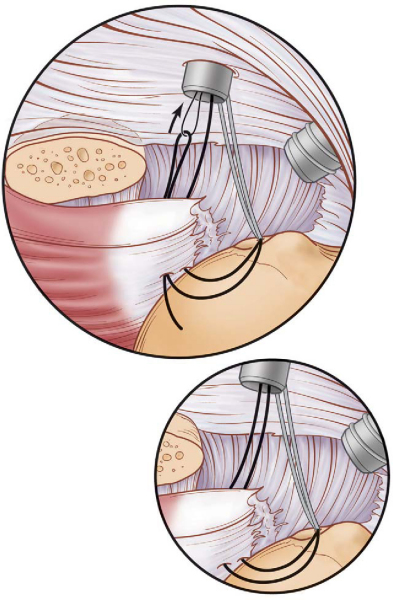
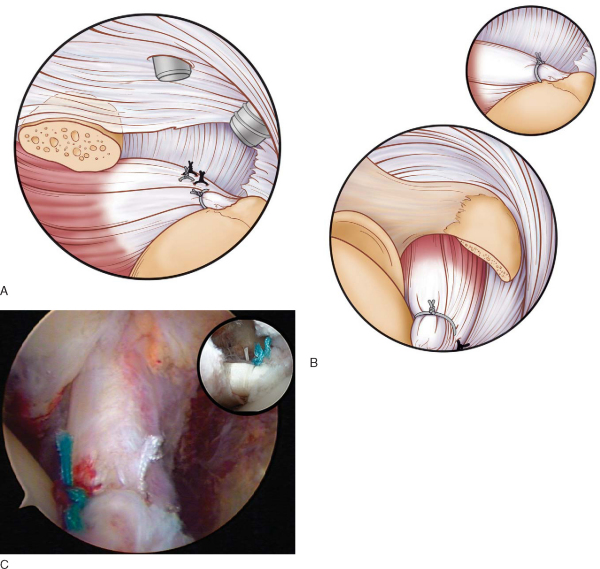
The anterolateral portal is used for arthroscopic knot tying as it allows the surgeon to pass-point the knots and provides a better angle of approach to the tendon. We start by tying the most superior suture to set the position of the remaining sutures.
A crochet hook is used to retrieve the two limbs of the most superior suture out of the anterolateral portal. The arm is internally rotated and forward flexed to better visualize the knots. Multiple alternating half-hitches with alternating posts are placed, and the suture ends are cut (
Fig. 18-16
). The process is repeated for the second suture on the proximal anchor, followed by the inferior anchor. Ideally, the sutures are tied to place the knot on the tendon side of the repair, not the tuberosity (
Fig. 18-17
).
|
|
|
|
Figure 18-16 (A redrawn from Fox JA, Noerdlinger MA, Sasso LM, Romeo AA. Arthroscopic subscapularis repair. In Miller MD, Cole BJ, eds. Textbook of Arthroscopy. Philadelphia, Elsevier, 2004.) |
|
|
|
|
Figure 18-17 (A and B redrawn from Fox JA, Noerdlinger MA, Sasso LM, Romeo AA. Arthroscopic subscapularis repair. In Miller MD, Cole BJ, eds. Textbook of Arthroscopy. Philadelphia, Elsevier, 2004.) |
The arm is gently rotated to inspect the security of the repair and the tied knots. If necessary, gentle débridement can be performed with a shaver. Motion is assessed to determine limits for the postoperative rehabilitation program. Wounds are closed in a standard fashion, and the arm is placed into an abduction pillow sling.
The postoperative rehabilitation program is individualized on the basis of the quality and security of the repair and the biologic quality of the torn tendon. However, our general rehabilitation protocol is described here.
Initially, for the first 2 weeks, we allow forward elevation to 90 degrees and internal rotation to the abdomen. We limit external rotation to 40 degrees to prevent stretching of the repair. From 2 to 6 weeks, we allow the patient to increase external rotation as tolerated; however, we do not permit stretching or manipulation by a physical therapist. Forward elevation is increased to 140 degrees.
At 6 weeks, the sling is discontinued, and we begin active range of motion with progression to full motion as tolerated. We do not start strengthening until 12 weeks after surgery.
Sports-related rehabilitation is initiated at 5 months postoperatively. We allow return to collision sports at 9 months. Patients should expect maximal improvement to occur by about 12 months postoperatively.
Complications are those seen with arthroscopic shoulder surgery and rotator cuff repair. These include infection, nerve damage, stiffness, repair failure, and complications from fluid extravasation.
| PEARLS AND PITFALLS | |||||||||||||||||||||||||||
|
Arthroscopic subscapularis repair is a relatively new procedure; therefore, very little information is available in the literature regarding its results. Open repair of the subscapularis has been reported with acceptable results.
The senior author (A. A. R.) has reviewed the results of 14 patients with subscapularis tendon tears treated arthroscopically (
Table 18-1
). The average followup was 27 months. Three patients had an associated supraspinatus tear. One patient fell 2 weeks after surgery and required a revision arthroscopy. No neurovascular complications were noted. Forward elevation improved from 138 to 161 degrees, external rotation from 70 to 86 degrees. The American Shoulder and Elbow Surgeons (ASES) score improved from 46 to 82. The Simple Shoulder Test score improved from 7 to 10 on a 12-point scale. The unadjusted Constant score was 75 of 100 for the surgical side and 79 for the unaffected side, suggesting a functional result similar to that of the unaffected shoulder. On the Rowe function subscale, 79% of patients rated their results good to excellent.
| Author | Followup | Outcome |
|---|---|---|
| Romeo (2005) | 27 months | Forward elevation improved from 138 to 161 degrees |
| External rotation improved from 70 to 86 degrees | ||
| ASES score improved from 46 to 82 | ||
| Simple Shoulder Test score improved from 7 to 10/12 | ||
| 79% good to excellent results | ||
| Bennett[1] (2003) | Minimum of 2 years | Constant score improved from 43 to 74 |
| ASES score improved from 16 to 74 | ||
| VAS for pain dropped from 9 to 2/10 | ||
| Function improved from 25% to 82% | ||
| Burkhart and Tehrany[2] (2002) | 10.7 months | Forward elevation improved from 96 to 146 degrees |
| UCLA score improved from 10.7 to 30.5 | ||
| 92% good to excellent results |
Bennett[1] reviewed the results of eight patients with isolated subscapularis tears treated arthroscopically. The patients were observed for a minimum of 2 years. The Constant score improved from 43 to 74. The ASES score improved from 16 to 74. The visual analogue scale for pain dropped from 9/10 to 2/10. The percentage of function improved from 25% to 82%.
Burkhart and Tehrany[2] reported the results of 25 patients with subscapularis tears treated arthroscopically; 8 patients had isolated complete tears, 6 patients had other rotator cuff disease, and 11 patients had partial tears with other rotator cuff tears. The average followup was 10.7 months. Forward elevation improved from 96 to 146 degrees. The UCLA scores improved from 10.7 to 30.5; 92% of patients reported good to excellent results. UCLA scores were similar between isolated and combined tears and between complete and partial tears.
These studies suggest excellent early results and restoration of the force couples, leading to stable, painless glenohumeral joint motion. Although arthroscopic subscapularis repair is a technically demanding technique, we believe that a secure repair can be accomplished arthroscopically and that outcomes after all-arthroscopic repair are similar to those of traditional open techniques.
1.
Bennett WF: Arthroscopic repair of isolated subscapularis tears: a prospective cohort with 2- to 4- year followup.
Arthroscopy 2003; 19:131-143.
2.
Burkhart SS, Tehrany AM: Arthroscopic subscapularis tendon repair: technique and preliminary results.
Arthroscopy 2002; 18:454-463.
Edwards et al., 2005.
Edwards TB, Walch G, Sirveaux F, et al: Repair of tears of the subscapularis.
J Bone Joint Surg Am 2005; 87:725-730.
Fox et al., 2003.
Fox JA, Noerdlinger MA, Romeo AA: Arthroscopic subscapularis repair.
Tech Shoulder Elbow Surg 2003; 4:154-168.
Gerber and Krushell, 1991.
Gerber C, Krushell RJ: Isolated rupture of the tendon of the subscapularis muscle. Clinical features in 16 cases.
J Bone Joint Surg Br 1991; 73:389-394.
Gerber et al., 1996.
Gerber C, Hersche O, Farron A: Isolated rupture of the subscapularis tendon.
J Bone Joint Surg Am 1996; 78:1015-1023.
Lo and Burkhart, 2002.
Lo IK, Burkhart SS: Subscapularis tears: arthroscopic repair of the forgotten rotator cuff tendon.
Tech Shoulder Elbow Surg 2002; 3:282-291.
Lyons and Green, 2005.
Lyons RP, Green A: Subscapularis tendon tears.
J Am Acad Orthop Surg 2005; 13:353-363.
Nerot, 1993–94.
Nerot C: Rotator cuff ruptures with predominant involvement of the subscapularis tendon.
Chirurgie 1993–94; 291:103-106.
Richards et al., 2003.
Richards DP, Burkhart SS, Lo IK: Subscapularis tears: arthroscopic repair techniques.
Orthop Clin North Am 2003; 34:485-498.
Tennent et al., 2003.
Tennent TD, Beach WR, Meyers JF: A review of the special test associated with shoulder examination. Part I: the rotator cuff tests.
Am J Sports Med 2003; 31:154-160.