CHAPTER 11 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
CHAPTER 11 – Open Repair of Anterior Shoulder Instability
The shoulder is notable in that it has the greatest range of motion of all the joints in the human body. Bone restraints to motion are minimal. The surrounding soft tissue envelope is the primary stabilizer that maintains the humeral head on the glenoid.
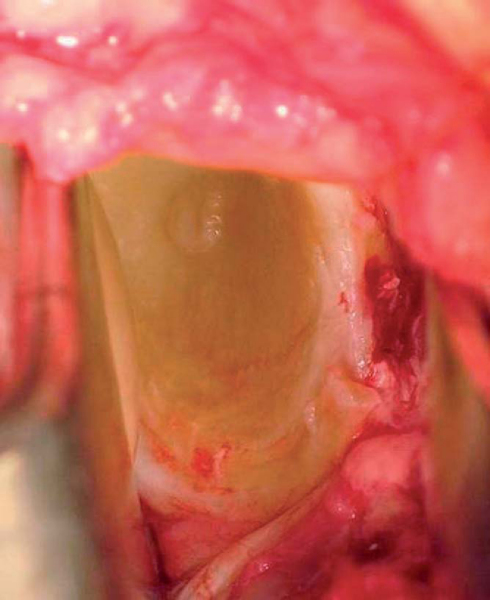
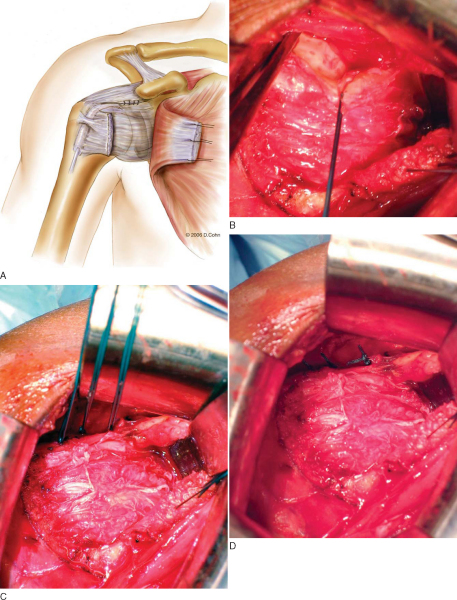
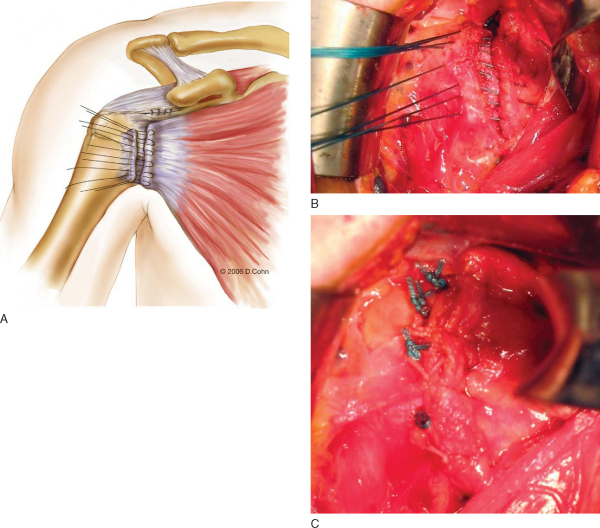
The shoulder capsule is large, loose, and redundant to allow the large range of shoulder motion. There are three main ligaments in the anterior capsule that help prevent subluxation or dislocation. These ligaments are known as the superior glenohumeral ligament, the middle glenohumeral ligament, and the inferior glenohumeral ligament complex (IGHLC). Damage to the IGHLC, which supports the inferior part of the shoulder capsule like a hammock, is related to most cases of anterior instability. The Bankart lesion,[1] involving detachment of the IGHLC insertion on the glenoid, is the most common pathologic lesion associated with traumatic anterior instability (
Fig. 11-1
). Defects or injuries to the superior and middle glenohumeral ligaments may also contribute to instability.[9]
The primary goals of the surgical treatment of shoulder instability are to restore stability and to provide the patient with nearly full pain-free motion. Older techniques of shoulder stabilization tended to limit shoulder range of motion in exchange for providing stability. We now understand that it is probably more important to preserve motion than it is to stabilize the shoulder. Techniques that limit shoulder motion often lead to osteoarthritis, whereas it is unusual for recurrent dislocation itself to lead directly to osteoarthritis. As a result, any method of open stabilization should be designed to provide full functional use of the shoulder as well as normal stability.
|
|
|
|
Figure 11-1 |
Preoperative Considerations[8]
The diagnosis of an anterior dislocation is usually readily apparent. The patient typically gives a history of a specific injury in which the shoulder “popped out.” In some cases, dislocation occurs with no history of significant trauma; these patients are frequently noted to have generalized ligamentous laxity and are less likely to demonstrate a Bankart lesion.
The diagnosis of anterior subluxation is often more subtle. The chief complaint may be a sense of movement, pain, or clicking with certain activities. Pain, rather than instability, may be the predominant complaint. In throwers and other overhead athletes, “dead arm” episodes may occur during which the patient experiences a sharp pain followed by loss of control of the extremity.[10]
Apprehension tests are designed to induce anxiety and protective muscle contraction as the shoulder is brought into a position of instability. The anterior apprehension test is performed with the arm abducted and externally rotated. As the examiner progressively increases the degree of external rotation, the patient develops apprehension that the shoulder will slip out. This test result is uniformly positive in patients with anterior instability.
During the relocation test, the examiner’s hand is placed over the anterior shoulder of the supine patient. A posteriorly directed force is applied with the hand to prevent anterior translation of the humeral head. The shoulder is then abducted and externally rotated as it is in the apprehension test. A positive result is obtained when this anterior pressure allows increased external rotation and diminishes associated pain and apprehension. The relocation test seems to be more reliable in overhead athletes, and the result may not be positive in all cases of anterior instability.
The belly press and liftoff tests should also be performed to confirm the integrity of the subscapularis tendon.
Routine radiographic examination of the unstable shoulder includes an anteroposterior view (deviated 30 to 45 degrees from the sagittal plane to parallel the glenohumeral joint), a transscapular (Y) view, and an axillary view. In the assessment of more chronic instability, West Point and Stryker notch views are helpful in demonstrating bone lesions of the humeral head and glenoid.
Magnetic resonance imaging is not routinely performed in patients with instability because the findings are usually predictable; however, it may be helpful in preoperative planning. The accuracy of magnetic resonance imaging in determining labral disease is increased with arthrography. Because of the possibility of concomitant rotator cuff injury, magnetic resonance imaging should always be considered in older patients with instability—especially if strength and motion are slow to recover after an episode of dislocation.
Indications and Contraindications
The indications for surgical treatment of recurrent anterior shoulder instability are highly subjective. They include a desire of the patient to avoid recurrent problems with instability (including the necessity of reporting to the emergency department on a frequent basis to have the shoulder reduced), problems with recurrent pain, an inability to perform certain activities because of a fear of further shoulder instability, and the desire to improve athletic performance with improved shoulder stability. Failure of a thorough trial of nonoperative treatment is also an indication for surgical treatment.
There are several relative contraindications to performing a stabilization procedure by an arthroscopic method in patients in whom an operation is deemed advisable. Although there is controversy in this area, reported indications for open stabilization over arthroscopic stabilization include participation in a contact or collision sport, bone defects of the humeral head or glenoid, humeral avulsion of the glenohumeral ligaments, rupture of the subscapularis in association with a traumatic dislocation, failed open or arthroscopic repair, and atraumatic instability.
Contraindications to the open technique include voluntary instability and concomitant psychological issues. Large defects of the humeral head (Hill-Sachs lesions) or glenoid may require supplemental bone grafting to fill the defects.[2] I prefer to use arthroscopic methods of stabilization in throwing athletes. If an open method is used in this group, I recommend the technique of anterior capsulolabral reconstruction described by Jobe,[6] in which the subscapularis tendon is split rather than detached.
Surgical Technique[7]
The basic procedure for the open surgical treatment of recurrent anterior instability is a modification of the Bankart procedure[1] and involves repair of the anterior capsule and labrum to the glenoid. In most cases, the capsular ligaments are stretched as well as detached, and the procedure is also designed to remove any abnormal laxity.
The procedure is performed after placement of an interscalene block. In some cases, the block is supplemented with general anesthesia. The patient is positioned supine with the head of the operating table raised 15 to 30 degrees and the involved upper extremity abducted 45 degrees on an arm board. Folded sheets are placed beneath the elbow and taped to the arm board. The sheets maintain the arm in the coronal plane of the thorax and minimize extension of the shoulder.
The surgeon initially stands in the axilla. Two assistants are used. The first assistant’s primary responsibilities are to control arm position and to keep the humeral head reduced during the capsular repair. The first assistant alternates position with the surgeon. When the surgeon is in the axilla, the first assistant stands lateral to the arm. When the surgeon moves to the lateral aspect of the arm, the first assistant shifts to the axilla. The first assistant also holds the humeral head retractor when it is in position. The second assistant stands on the opposite side of the table and holds the medial (glenoid) retractors. The use of a mechanized arm holder can free up the assistants’ hands and may facilitate exposure.
Examination Under Anesthesia and Arthroscopic Evaluation
I routinely examine the shoulder under anesthesia to confirm the presence of abnormal anterior translation. Drawer tests are best performed in 90 degrees of abduction and neutral rotation where translation is greatest. Translation is graded 1+ if there is increased translation compared with the opposite shoulder but neither subluxation nor dislocation occurs. If the head can be subluxated over the glenoid rim but then spontaneously reduces, translation is graded 2+. Frank dislocation without spontaneous reduction constitutes 3+ translation.
I also routinely perform an arthroscopic examination of the shoulder in the beach chair position before open stabilization. The arthroscopic examination allows identification and treatment of concomitant injuries to the shoulder, including superior labral and rotator cuff disease that can be difficult to identify through an open approach. In addition, the examination is helpful in planning the specific method of capsular repair.
Specific Steps (
Box 11-1
)
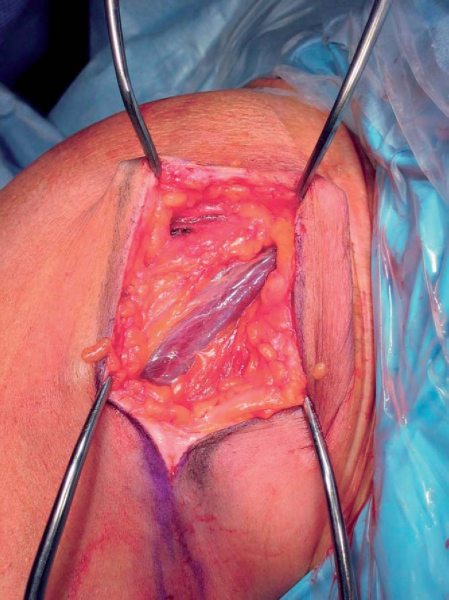
The skin is incised along the anterior axillary crease (
Fig. 11-2
) in a longitudinal fashion along Langer’s lines. The incision is placed lateral to the coracoid process. The deltopectoral interval is identified (
Fig. 11-3
), the cephalic vein is retracted laterally, and the interval is developed. The clavipectoral fascia is then incised at the lateral border of the conjoined tendon at its coracoid attachment, and the coracoacromial ligament is divided to facilitate exposure of the superior aspect of the capsule and, particularly, the rotator interval area.
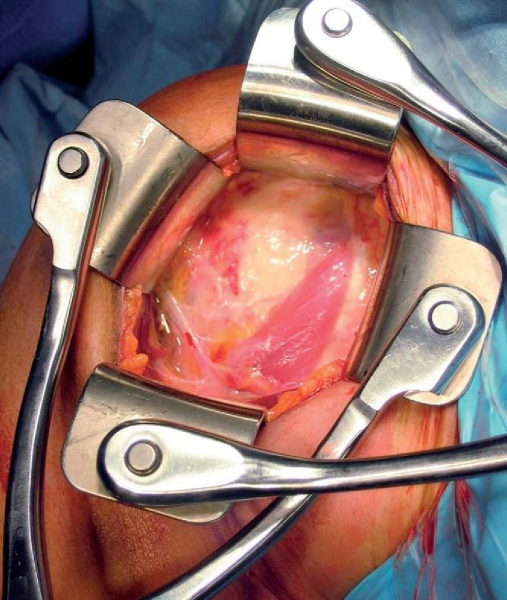
Two self-retaining retractors are then placed in the wound (
Fig. 11-4
). Placement of these retractors frees the assistants to aid in arm position and shoulder reduction. At this point, the surgeon shifts position from the axilla and stands lateral to the arm. If a mechanized arm holder is used, it is attached to the forearm when the surgeon moves from the axilla.
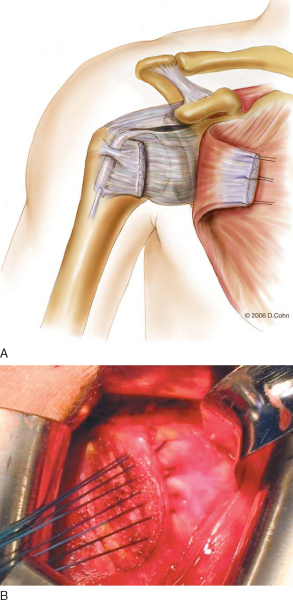
The bicipital groove and the lesser tuberosity are identified. A vertical tenotomy of the subscapularis tendon is performed with electrocautery approximately 1 cm medial to its insertion on the lesser tuberosity (
Fig. 11-5
). The medial portion of the tendon is tagged with heavy No. 1 nonabsorbable braided polyester (Ethibond) sutures. The interval between the anterior aspect of the capsule and the subscapularis tendon is then carefully developed with a combination of blunt and sharp dissection.
The laxity and quality of the capsule are then assessed. If there is a lesion in the rotator interval, it is generally closed at this point with No. 1 nonabsorbable braided polyester (Ethibond) sutures (
Fig. 11-6
). A transverse capsulotomy is then performed (
Fig. 11-7
), and a ring (Fukuda) retractor is placed intra-articularly. The anterior glenoid neck is explored for evidence of a Bankart lesion. The joint is then irrigated to remove any residual loose bodies.
|
|
|
|
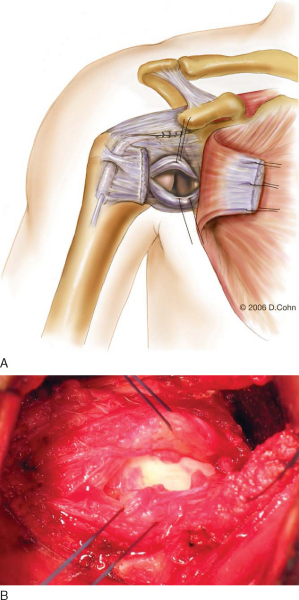
Figure 11-6 |
If a Bankart lesion is noted, the capsulolabral separation at the anteroinferior glenoid neck is extended medially with use of an elevator or knife to allow placement of a retractor along the glenoid neck (
Fig. 11-8
). The glenoid neck is then roughened with an osteotome or motorized bur to provide a bleeding surface (
Fig. 11-9
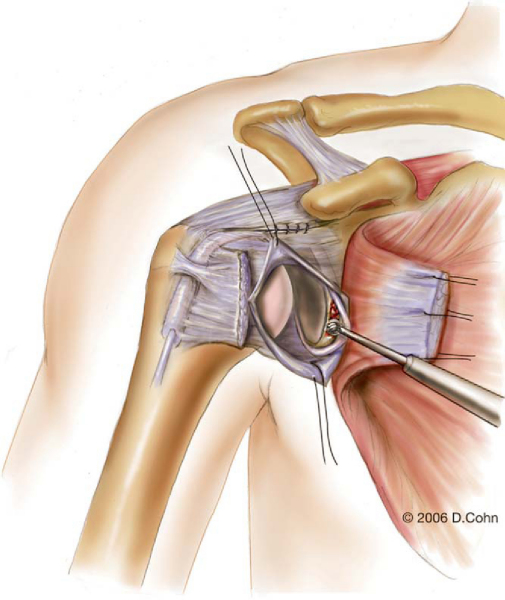
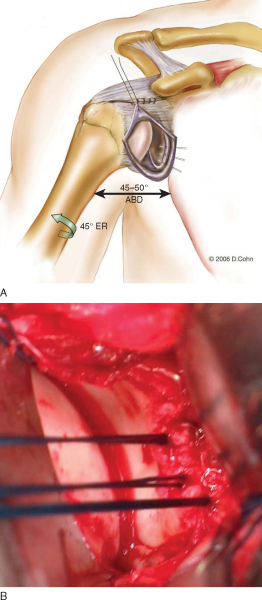
). Two or three suture anchors are placed in the anteroinferior glenoid neck near but not on the articular margin of the glenoid (
Fig. 11-10
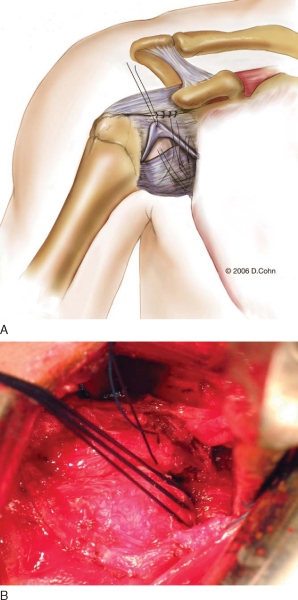
). The arm is placed in 45 degrees of abduction and 45 degrees of external rotation. The inferior capsular flap is then mobilized slightly medially and superiorly. The inferior flap is reattached to the anterior aspect of the glenoid to repair the Bankart lesion with use of the suture anchors (
Fig. 11-11
). The goal is not to reduce external rotation but to obliterate excess capsular volume and to restore the competency of the IGHLC at its glenoid insertion.
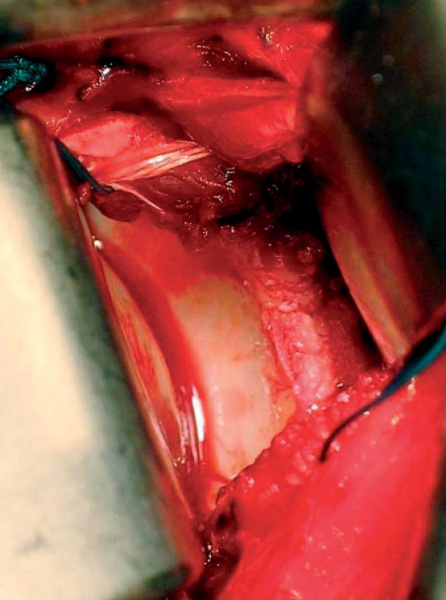
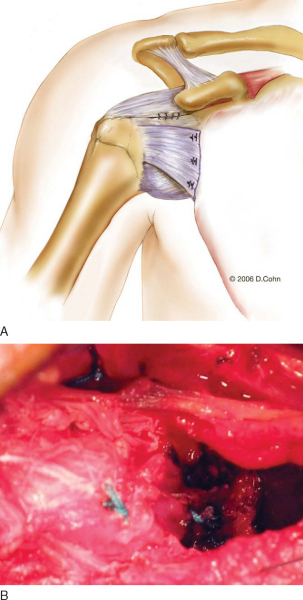
After repair of the Bankart lesion (or in the absence of a Bankart lesion), an anterior capsulorrhaphy is performed to eliminate excess capsular laxity. The arm is maintained in 45 degrees of abduction and 45 degrees of external rotation, and the superior and inferior capsular flaps are reapproximated with forceps. The shoulder is held in a reduced position. If the capsular flaps can be overlapped, the capsule is shifted to eliminate excess capsular volume: if there is 5 mm (or less) of overlap, the capsule is imbricated by shifting the superior flap over the inferior flap and passing the sutures a second time through the superior flap (
Fig. 11-12
); with more than 5 mm of capsular overlap, the capsulotomy is extended in a vertical direction near its lateral insertion on the humeral neck, and a T-plasty capsular shift is performed (
Fig. 11-13
). The inferior capsular flap is shifted superolaterally, and the superior flap is moved over the inferior flap in an inferolateral direction. The transverse portion of the capsulotomy is then closed.
|
|
|
|
Figure 11-12 |
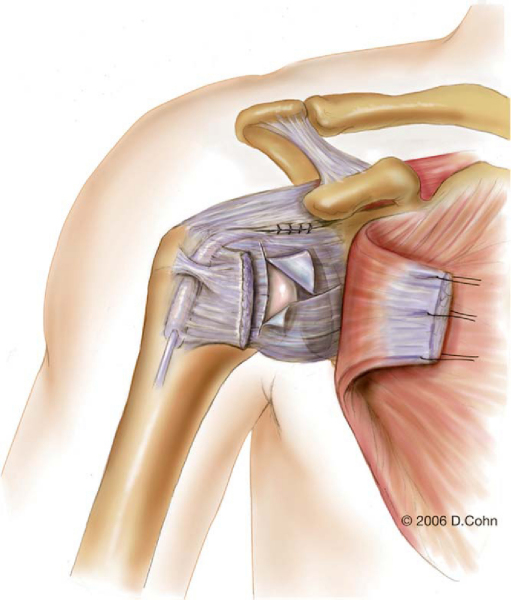
After the capsule has been addressed satisfactorily, the subscapularis is reapproximated, but not shortened, with nonabsorbable suture (
Fig. 11-14
). The deltopectoral interval is loosely closed with absorbable suture. Routine wound closure is then performed.
|
|
|
|
Figure 11-14 |
| PEARLS AND PITFALLS | |||||||||||||||||||||||||||
|
The standard rehabilitation protocol is described in
Box 11-2
. Special situations are noted at the end of
Box 11-2
.
| Standardized Postoperative Rehabilitation Protocol | ||||||||||||||||||||||||||||||
From Pagnani MJ, Galinat BJ, Warren RF. Glenohumeral instability. In DeLee JC, Drez D, eds. Orthopaedic Sports Medicine. Philadelphia, WB Saunders, 1994:580-622. |
Recurrent instability is the greatest concern after any stabilization procedure. Subcutaneous hematoma formation is the most common complication in my experience (1.5% of cases). If a hematoma forms, it may be observed as long as the wound is not draining. When the hematoma causes persistent wound drainage, surgical evacuation is recommended.
Subscapularis rupture has been reported after open anterior stabilization. Although I have no experience with subscapularis rupture in this setting, I recommend meticulous reapproximation of the tendon and restriction of external rotation for 3 months postoperatively as prophylactic measures to prevent its occurrence.
The published recurrence rates after open stabilization for anterior instability have generally been low, ranging from 0% to 10% in most series (
Table 11-1
). However, one report from West Point described a failure rate of 22% in active cadets, indicating that results are not uniformly and predictably good.[11] The outcome of open stabilization in contact athletes appears to be superior to that reported in similar populations with arthroscopic techniques. [5] [7] The reported motion loss with current open techniques is also acceptable; in my experience, 84% of patients regained all or nearly all of their motion. No patient lost more than 15 degrees of external rotation compared with the contralateral side. Finally, when the incision is placed in the anterior axillary crease, the cosmetic result is usually satisfactory (
Fig. 11-15
).
| Author | N | Recurrence Rate |
|---|---|---|
| Cole et al[3] (2000) | 24 | 9% |
| Gill et al[4] (1997) | 60 | 5% |
| Hubbell et al[5] (2004) | 20 | 0% |
| Pagnani and Dome[7] (2002) | 58 | 3% |
| Uhorchak et al[11] (2000) | 66 | 22% |
| Wirth et al[12] (1996) | 142 | 3% |
1.
Bankart ASB: The pathology and treatment of recurrent dislocation of the shoulder-joint.
Br J Surg 1938; 26:23-29.
2.
Chen AL, Hunt SA, Hawkins RJ, Zuckerman JD: Management of bone loss associated with recurrent anterior glenohumeral instability.
Am J Sports Med 2005; 33:912-925.
3.
Cole BJ, L’Insalata J, Irrgang J, Warner JJP: Comparison of arthroscopic and open anterior shoulder stabilization: a two to six-year followup study.
J Bone Joint Surg Am 2000; 82:1108-1114.
4.
Gill TJ, Micheli LJ, Gebhard F, Binder C: Bankart repair for anterior instability of the shoulder. Long-term outcome.
J Bone Joint Surg Am 1997; 79:850-857.
5.
Hubbell JD, Ahmad S, Bezenoff LS, et al: Comparison of shoulder stabilization using arthroscopic transglenoid sutures versus open capsulolabral repairs: a 5-year minimum followup.
Am J Sports Med 2004; 32:650-654.
6.
Jobe FW, Giangarra CE, Kvitne RS, Glousman RE: Anterocapsulolabral reconstruction of the shoulder in athletes in overhead sports.
Am J Sports Med 1991; 19:428-434.
7.
Pagnani MJ, Dome DC: Surgical treatment of traumatic anterior shoulder instability in American football players: two- to-six year followup in fifty-eight athletes.
J Bone Joint Surg Am 2002; 84:711-715.
8.
Pagnani MJ, Galinat BJ, Warren RF: Glenohumeral Instability.
In: DeLee JC, Drez D, ed. Orthopaedic Sports Medicine,
Philadelphia: WB Saunders; 1994:580-622.
9.
Pagnani MJ, Warren RF: Stabilizers of the glenohumeral joint.
J Shoulder Elbow Surg 1994; 3:173-190.
10.
Rowe CR, Zarins B: Recurrent transient subluxation of the shoulder.
J Bone Joint Surg Am 1981; 63:863-872.
11.
Uhorchak JM, Arciero RA, Huggard D, Taylor DC: Recurrent shoulder instability after open reconstruction in athletes involved in collision and contact sports.
Am J Sports Med 2000; 28:794-799.
12.
Wirth MA, Blatter G, Rockwood Jr CA: The capsular imbrication procedure for recurrent anterior instability of the shoulder.
J Bone Joint Surg Am 1996; 78:246-260.