Ankle Fusion: Cannulated Screws
pain, decreased range of ankle motion, and limited ambulatory ability.
Ankle arthrodesis is the treatment of choice for patients suffering
from disabling pain from osteoarthritis, posttraumatic arthritis, or
rheumatoid arthritis. Numerous techniques have been reported in the
literature to obtain successful union. These include screws, plates and
screws, external fixation, and intramedullary devices. Each technique
has been met with success and failure.
Successful treatment of the underlying condition requires correction of
any deformity at the time of arthrodesis to allow for optimal union
rate and functional recovery.
nonunion, which ranges from 0% to 40%. Risk factors for the development
of a nonunion include diabetes, poor nutritional status, infection,
nicotine use, and peripheral neuropathy.
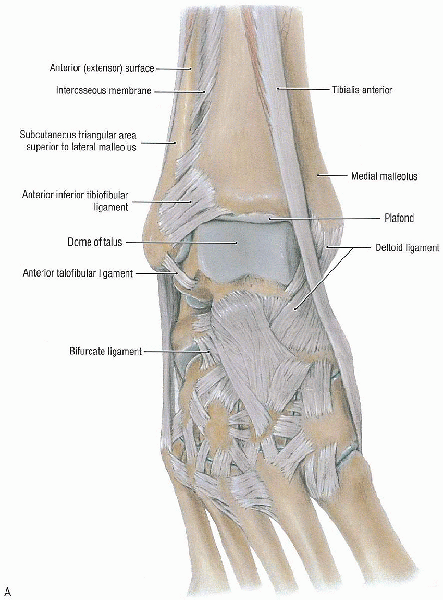
ankle joint (tibiotalar) includes the distal tibia and fibula and the
talar body (Fig. 32-1). As the tibial shaft
flares in the supramalleolar region, the dense cortical bone changes to
metaphyseal cancellous bone. The shape of the tibial articular surface
is concave with distal extension of the anterior and posterior lips.
This surface has been called the tibial plafond, which is a French word meaning ceiling.
The wedge-shaped talar dome sits within the mortise and is wider
anteriorly than posteriorly. When the ankle dorsiflexes, there is a
compensatory external rotation of the fibula. This leads to abduction
of the foot. The malleoli serve as pulleys for tendons reaching plantar
surface of the foot from the posterior and lateral compartments of the
leg.
posteriorly and is reinforced by collateral ligaments medially and
laterally. On the medial side, the heavy deltoid ligament is attached
above to the medial malleolus with its superficial fibers from the
anterior colliculus and stronger deep fibers originating from the
posterior colliculus. These fibers fan out to attach inferiorly to the
talus and calcaneus. The anterior talofibular, calcaneofibular, and
posterior talofibular ligaments are attached to the lateral malleolus.
The syndesmotic ligament complex includes the anteroinferior and
posteroinferior tibial-fibular ligaments, the interosseous ligament,
and the transverse tibial-fibular ligament and functions to stabilize
the distal fibula with the distal tibia.
unremitting pain that interferes with activities of daily living that
is not relieved by other treatment modalities such as nonsteroidal
antiinflammatory medication, modification of shoe wear, bracing, or
prior surgical débridement.
changes. These degenerative changes may follow trauma such a severe
ankle fracture or fracture-dislocation, pilon fracture, or unrecognized
chondral injury. Rheumatoid arthritis or other collagen disease is a
less common cause of ankle degeneration that may lead to complete loss
of ankle joint function. Chronic sepsis of an ankle is an indication
for fusion. Débridement performed first, followed by fusion, can be a
successful way to salvage an extremity. The Charcot ankle may lead to
progressive deformity and subsequent skin breakdown. Fusion about the
ankle in the Charcot foot usually encompasses more than just the
tibiotalar joint. Often, multiple hindfoot articulations must be fused
to give the patient a stable, plantigrade foot. Severe deformity is a
relative indication because equinus, varus, or valgus not amenable to
surgical release can lead to difficulty walking. Ankle fusion may be
the only option for a failed total ankle replacement if the limb is to
be salvaged in a functional manner.
arthrodesis includes a careful assessment. A thorough history is
essential specifically any preexisting medical conditions such as
peripheral vascular disease or diabetes should be elicited. A careful
physical examination, including assessment of any deformity, Achilles
tightness, palpation of pulses, and sensory status, is mandatory.
Peripheral neuropathy is a known cause of nonunion and its presence,
although not an absolute contraindication, may lead to the use of
adjunctive methods such as internal or external bone stimulation. Other
areas of the hindfoot should be evaluated for presence of arthrosis.
This can be done radiographically with use of computed tomography to
assess the subtalar
joint
or selective lidocaine injection to rule out other areas of the “ankle”
that may be the cause of persistent postoperative pain. If a subtalar
arthrodesis will be required, it can be performed with only a slight
extension of the surgical incision. Bone stock also must be assessed.
If the indication is posttraumatic, there may be a need for bone
grafting; if the fusion follows a failed total ankle replacement; major
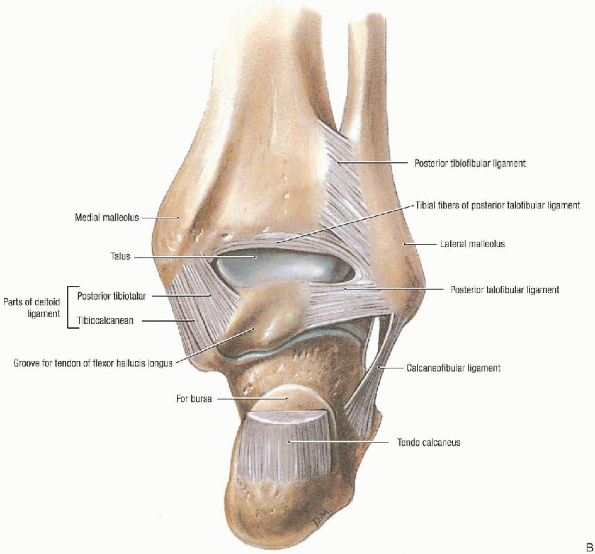
bone grafting usually is necessary. A standard radiographic ankle
trauma series, including anteroposterior, lateral, and mortise views,
is required to assess the joint (Fig. 32-2). Standing views may offer a better picture of the clinical situation.
 |
|
FIGURE 32-1. Ankle joint: anterior view (A) and posterior view (B). (From Agur AMR, Lee MJ. Grant’s atlas of anatomy, 10th ed. Philadelphia: Lippincott Williams & Wilkins, 1999, with permission.)
|
disposal for performing this operation, I prefer a fusion of bony
surfaces with compression provided by three cannulated, partially
threaded screws. If bone stock does not suffice or if intraoperative
complication leads to overresection of bony surfaces, an external
fixator can be used to provide compression.
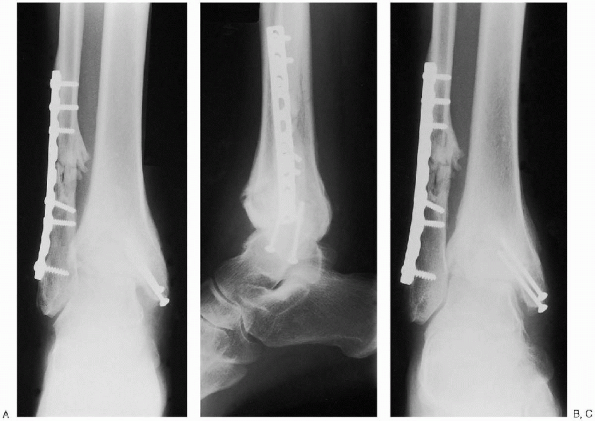
extremity and includes a radiolucent table that can accommodate image
intensification, a sterile bolster, osteotomes, curettes, a sagittal
saw, and cannulated screws. Intraoperative fluoroscopy is mandatory to
confirm foot position, bony cuts, and screw placement. A secondary plan
of action should be available if the bone stock is not adequate to
accept stable fixation. In this case, an external fixator is usually
the implant of choice and should be available (Fig. 32-3).
 |
|
FIGURE 32-1. Continued.
|
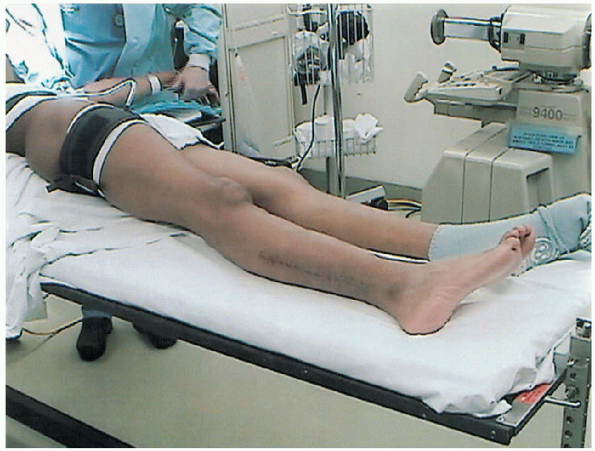
The ipsilateral iliac crest should be prepared and draped if a need for
autogenous bone graft is contemplated. A well-padded tourniquet should
be placed on the ipsilateral proximal thigh. The patient’s position
should take into account the need for intraoperative image
intensification, with the ability to obtain anteroposterior, lateral,
and mortise views. The draping of the extremity should allow for 90
degrees of knee flexion.
incisions; however, if there was no previous surgery and no internal
fixation is present, a lateral incision alone may be used. Laterally,
the incision parallels the fibula and begins 8 cm proximal to the tip
of the lateral malleolus (Fig. 32-5). This
incision extends distally and curves toward the fourth metatarsal
across the sinus tarsi. A second anteromedial incision is made over the
medial malleolus (Fig. 32-6).
The lengths of these incisions are altered, depending on the presence
of preexisting hardware. If hardware from a previous internal fixation
or attempted fusion is present, it should be removed after the exposure
has been performed and before any osteotomies are performed.
 |
|
FIGURE 32-2. Anteroposterior (A), lateral (B), and mortise (C) preoperative radiographs.
|
 |
|
FIGURE 32-3. Equipment for ankle fusion. Bottom row, third from left: cannulated screws and curettes (3), osteotomes (4), and sagittal saw. Top row and bottom left:
external fixator trays (3) and rings from a fixator set. The fixator is used when a patient’s bone stock is not adequate for stable fixation. |
 |
|
FIGURE 32-4. Position of the patient.
|
 |
|
FIGURE 32-5. The lateral incision begins 8 cm from the tip of the malleolus.
|
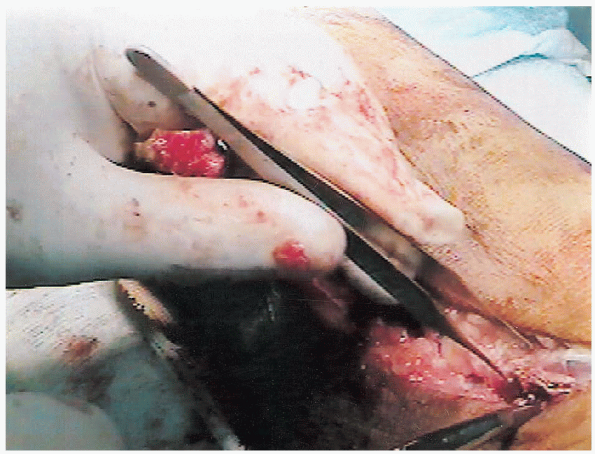
on the lateral side, soft tissues, including the peroneals and flexor
hallucis longus are sharply elevated from the fibula. An oblique
osteotomy is performed 6 to 8 cm proximal to the tip of the fibula.

The fibula is freed of all soft tissue by subperiosteal elevation. A
towel clip is used to pull traction on the fibula, and the bone is
released from its ligamentous attachments at the distal end.

Exposure to the lateral talotibial joint is now afforded. Deep
dissection distally occurs between the extensor hallucis brevis muscle
belly and the peroneal tendons (Fig. 32-7).
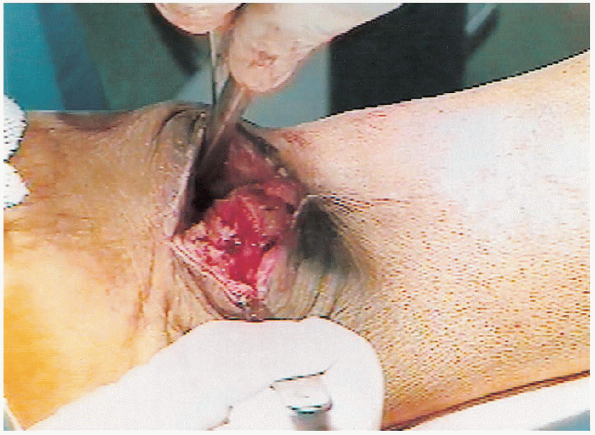
Attention is then tuned to the medial side. Care is taken to preserve
the saphenous vein and its branches. The posterior tibial tendon and
posteromedial neurovascular structures are freed and protected. The
medial malleolus is then osteotomized at a 45-degree angle toward the
corner of the joint.

Care is taken to avoid overresection of the medial tibial flare,
because it serves to anchor hardware. The anterior ankle capsule is
then elevated to view the articular surface from both sides (Fig. 32-8).
 |
|
FIGURE 32-6. Anteromedial incision over the medial malleolus.
|
 |
|
FIGURE 32-7. Identifying the external hallucis brevis muscle belly.
|
this point, the articular surfaces of the tibial plafond and talar dome
are denuded of remaining cartilage down to bleeding subchondral bone.

If severe deformity exists, the appropriate osteotomy is performed to
get the surfaces of the tibia and talus opposed. This is accomplished
with the aid of an oscillating saw or osteotomes.
 In
Ineither case, it is critical to avoid overresection of bone, especially
on the talar side, so as not to compromise bone stock. No more than 3
to 4 mm of the bone should be resected.
 |
|
FIGURE 32-8. Elevation of the ankle joint capsule.
|
 |
|
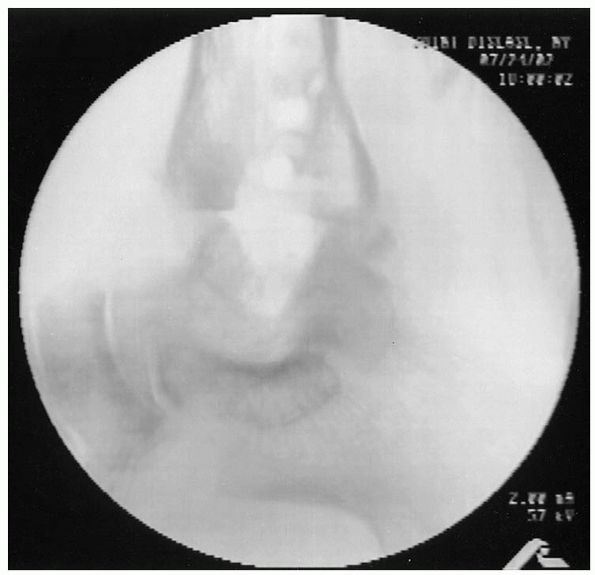
FIGURE 32-9. Angle of Gissane should line up with the mid-axis of the tibia.
|
critical point is positioning of the foot before internal fixation. The
hindfoot should be placed in a plantigrade position with the ankle at
90 degrees. The hindfoot should be placed in 5 degrees of valgus and
slight external rotation. The talus is translated slightly posteriorly
to place the foot in line with the weight-bearing axis. This can be
confirmed radiographically by aligning the angle of Gissane with the
midshaft of the tibia on the lateral radiograph (Fig. 32-9).

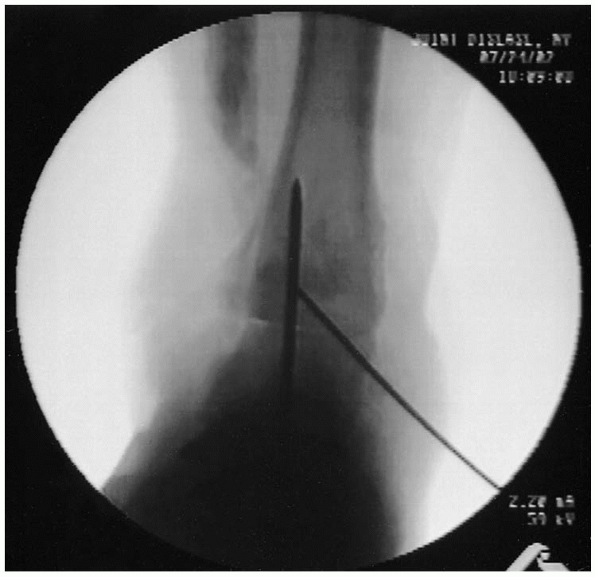
 A second, smaller Kirschner wire is placed across the tibiotalar articulation for rotational control (Fig. 32-11).
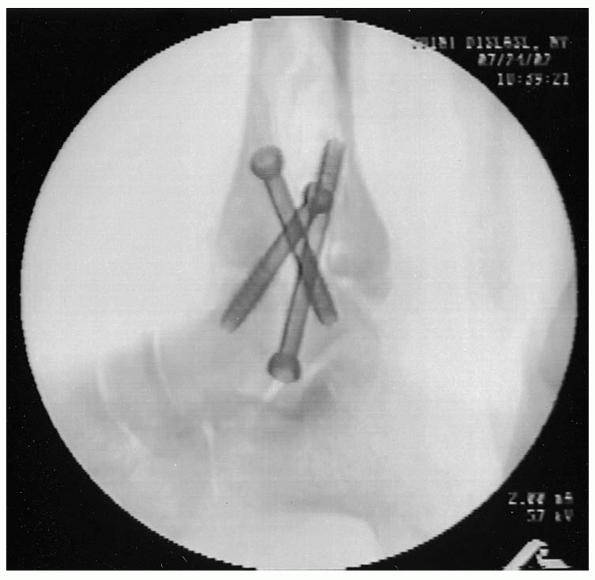
A second, smaller Kirschner wire is placed across the tibiotalar articulation for rotational control (Fig. 32-11).At this point, the position of the fusion is checked radiographically
on anteroposterior, lateral, and mortise views. With acceptable
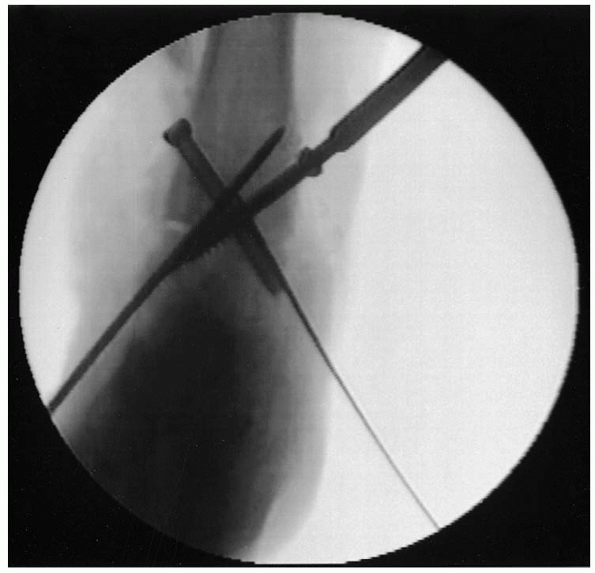
alignment achieved, the guide wires for the cannulated screws are
placed. These can be 6.5-, 7.3-, or 8.0-mm, cannulated, partially
threaded cancellous screws, depending on the size of the patient. Two
screws are placed from proximal to distal aspects. The proximal, medial
guide wire is placed approximately 2 cm above the articular surface,
about 5 mm posterior to the midaxis of the tibia and angling about 60
degrees toward the anterolateral talus.

The second wire is placed 2 cm proximal to the joint on the lateral
side and 5 mm anterior to the midaxis of the tibia and is angled
posteromedially into the talus.
 The third wire starts distally and enters the talus anterolaterally, and it is angled proximally into the posteromedial tibia.
The third wire starts distally and enters the talus anterolaterally, and it is angled proximally into the posteromedial tibia. 
After the guide wires are placed and confirmed radiographically, the
lengths are measured and the outer cortices overdrilled. The shorter
thread screws (16 mm) should be used to avoid threads across the fusion
site, allowing for maximal compression.

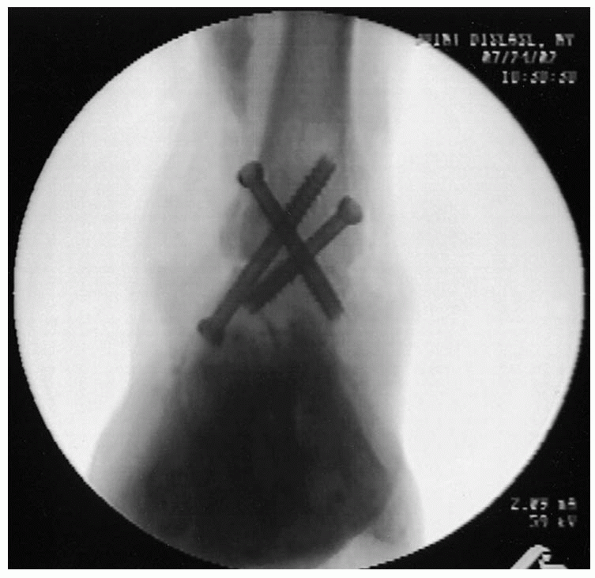
It is critical to check screw lengths radiographically and by direct
visualization if possible to avoid penetration of the subtalar joint,
which may lead to subtalar joint irritability. The medial screw may need to be countersunk to avoid prominent hardware in the subcutaneous medial tibia (Fig. 32-12). In the laboratory,
the cross-screw technique has been shown to be more biomechanically
sound than a plate-screw construct. The final construct is confirmed on
anteroposterior and lateral radiographs (Figs. 32-13 and 32-14).
 |
|
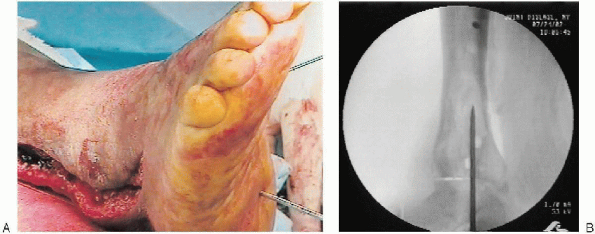
FIGURE 32-10. A and B: A Steinmann pin is placed across ankle to hold the position of the foot.
|
 |
|
FIGURE 32-11. A second provisional Kirschner wire is placed for rotational control.
|
 |
|
FIGURE 32-12. Medial screw placement with countersinking of the head.
|
harvested from the distal fibula, or autogenous iliac crest bone graft
can be obtained and packed around the fusion site laterally after
decortication. A suction drain is placed, and the wounds are closed in
layers with nylon sutures for the skin in a tension-free manner.
Sterile compressive dressings are applied, and a padded posterior
plaster slab with a U-shaped mold is applied to the ankle.
this time, the drain can be removed. The patient is mobilized without
bearing weight on the affected site, with an emphasis on leg elevation
while not ambulating. At 10 days to 2 weeks, the splint is removed, the
wound checked, and the sutures discontinued. The patient is again
placed in a short leg cast or a cast-brace orthosis, and weight bearing
is avaoided for 3 months. The patient is followed radiographically at
6-week intervals. By 3 months, it is expected there is at least 50%
bridging across the fusion site. At this point, the patient’s
weight-bearing status is advanced slowly to a flat foot stance,
followed by full weight bearing as tolerated. At this point,
physiotherapy may be initiated for lower extremity strengthening and
subtalar range of motion. The patient’s activity level progresses as
pain-free mobility returns. A patient who has undergone ankle fusion
will most likely require modifications in shoe wear. Most often, a
rocker sole needs to be added to allow for easier push during gait.
 |
|
FIGURE 32-13. Final anteroposterior view.
|
 |
|
FIGURE 32-14. Final lateral view.
|
well-executed ankle fusion. If recognized early, this can be treated
with local wound care and intravenous antibiotics. Nerve complications
may lead to suboptimal results. The superficial and deep peroneal
nerves and the sural nerve are at risk laterally, as well as the
posterior tibial nerve if a medial approach is used. Neuroma formation
can be quite painful, and careful identification of these peripheral
nerves and protection during surgery helps to avoid these complications
Excessive plantar flexion, internal rotation, or malpositioning in the
varus or valgus plane can compromise the final result. Malposition can
have detrimental effects on adjacent joints of the foot, with resultant
progressive degenerative changes.
