Stress Fractures
fractures since the likely initial description by Breithaupt in 1855 of
a syndrome of painful swollen feet among marching Prussian soldiers.27 It took until 1956 for the first report of the condition in athletes.58
Originally the domain of military recruits and military physicians,
recreational and competitive athletes with stress fractures now
commonly present to civilian practitioners. Athletic populations
involved in team and individual sports increasingly develop overuse
injuries, and stress fractures have been reported in most bones in the
body.
in athletic populations because of a variability in training programs
and a lack of standardized reporting.166
Track and field teams have shown incidences ranging from 10% to 31%,
with lesser but substantial numbers noted for participants in
gymnastics, ballet, figure skating, basketball, crew, soccer, and
lacrosse.18,93 U.S. military recruits develop lower extremity stress fractures at a gender-dependent rate of up to 4% in men and 7% in women.4,80,95,103
when that bone is subjected to abnormal or unaccustomed stresses. This
condition is distinct from insufficiency fractures, wherein normal
stresses applied to abnormal bone produce fracture.
activities. Ground and joint reaction forces as well as muscle forces
stress the bone by application of force across unit areas of bone.
These stresses yield local deformation or change in length, termed strain. Therefore, stress, a measure of the load applied, produces strain or bone deformation in a given direction.42
This remodeling response to cyclic loading entails initial osteoclastic
bone resorption followed by osteoblastic new bone formation within
cortical bone as well as on the trabeculae of cancellous bone.33,39
The resorption process peaks at 3 weeks, but it takes 3 months to
adequately create the new bone to complete the remodeling cycle.70,96,158,176
When optimally loaded and with sufficient time for remodeling, bone
mass remains static, no stress fracture or injury ensues, and the bone
becomes stronger.70,71,110,158,186
However, repetitive loading, which outstrips the bone’s ability to
create new bone in the resorption tunnels and pits, engenders a
resorption-dominated accelerated remodeling process that actually
weakens the bone.41,71,96,110,120
Then, with continued repetitive loading, a positive feedback mechanism
develops in which increased mechanical usage stimulates bone turnover,
resulting in focally increased remodeling porosity and decreased bone
mass. This weakened site is thus more susceptible to further
microdamage, which will incite additional resorption. Ultimately,
stress fracture can result from continued loading superimposed onto the
focally decreased bone mass generated by progressively larger
resorption sites.162
the likely diagnosis of stress fracture. Most athletes can accurately
characterize
their
symptom progression and relate the gradual onset of vague pain over a
period of weeks during training. Symptoms are initially described as
mild and present only during the stress or activity.110
The symptoms very often occur during the first few weeks after an
increase in training volume or intensity, a change in technique or
surface, or an alteration of footwear. Any change in a previously
regimented training program may be the inciting historical event.42,83,120
For nonathletes, a recent unusual uptick in activity, like a vacation
with a great deal more walking than usual or a new aerobic exercise
program, may be described.62 If left
unchecked, the process may progress to persistent pain after training,
pain at rest, and even night pain. Pertinent historical questions
relate to potential risk factors. History of previous stress fractures
or other painful sites and the presence of eating disorders, leg length
discrepancy, or muscle imbalance should be evaluated. In the female
patient, age of menarche and presence of menstrual irregularities must
be considered. For athletes, training regimen alterations are usually
the root cause of the pain. For runners, the most common training
change is a significant increase in the distance run during a brief
period of training.150 Furthermore,
the potential impact to the patient must be assessed. For example, a
scholarship athlete may wish to make different treatment choices than a
weekend runner.
palpation and stressing, but findings vary depending on the location of
the stress fracture and the time from injury onset to presentation.
When the site is accessible, local swelling may be noted. Percussion of
the bone typically produces pain, but passive and active ranges of
motion of adjacent joints do not. The anatomic location of the pain can
help in the diagnosis. For example, femoral diaphyseal stress fractures
occur typically in the medial cortex, so lateral thigh pain is not
likely to be correlated with a stress fracture.62
Inaccessible sites require indirect physical tests for diagnosis. For
example, back pain produced by hip extension while standing on the
opposite leg may implicate stress fractures of the pars
interarticularis.29
development of a stress fracture is an increase in training frequency
and intensity. However, work based on the concepts of Grimston and
Frost allows analysis of the factors that may lead to bone’s failure to
successfully adapt to the mechanical loads to which it is exposed.13,69,85
Mechanical competence of bone depends on properties like bone density
and geometry, all related to cellular activity. The theoretical
mechanosensory system of bone, classically considered to be Wolff law,
can be understood as a mechanostat that senses strain, compares it to a
given threshold, and initiates an adaptive cellular response.
Physiologic, mechanical, and pharmacologic factors generate mechanostat
responses by providing functional stimuli to the bone. Systemic
constraints on bone health such as genetics or eating disorders may
impede the bone’s ability to respond despite messages from the
mechanostat.
bone density measurements predictive of fragility fracture risks, the
majority of young active individuals have normal bone density.15
Little work points to any significant connection between bone density
and risk of stress fracture in men. Studies of male soldiers and
runners typically find no difference in tibial bone density between
those with and those without stress fractures.17,52,77 While not clearly causally related, low bone density may be a risk factor for women.12
A multivariate analysis showed a strong association between low femoral
neck bone density and risk of stress fracture in female military
recruits.111 An 8% lower bone
density at the tibia was identified in a subgroup of female track
athletes who developed tibial stress fractures.17
However, the bone density measures for these women were still higher
than those for similar less active nonathletes, perhaps suggesting that
the bone density required by athletes may be greater than that needed
by the general population. In summary, bone density measurement does
not appear to be a useful screening tool for stress fractures.12
In a prospective evaluation of more than 600 military recruits, an up
to 10% smaller tibial width and cross-sectional area was found among
those who developed stress fractures.10 Similar results for male runners are reported.52
Although bone geometry likely affects stress fracture development, no
practical imaging system yet allows this variable to be used as a
screening tool.
lead to stress fracture development. Multiple factors influence the
clinical responses to bone loading.13
Most studies support the notion that poor baseline physical fitness
predisposes to stress fracture development when a significant increase
in activity occurs.49,165,192
However, well-conditioned athletes also develop stress fractures, so
other factors must be considered. Load magnitude and rate appear to
present the most significant stimulation of bone cellular dynamics, so
the training regimen of soldiers and athletes often merits scrutiny.13 Training modifications including rest periods,164,193 banning concrete as a training surface,83,151 use of running shoes,83,149 and restricting high-impact activities143,164,179
can reduce the incidence of stress fractures in military recruits.
Shock-absorbing boot inserts may lead to fewer stress injuries in
recruits, but comfort and compliance issues prevent strong conclusions.155
Surveys of athletes relate changes in training in more than 80% of them
before the onset of a stress fracture. Increased training volume is
related to higher stress fracture risks in ballet dancers and runners.38,98
cannot be conclusively documented to contribute to stress fracture
development.13 Many investigators
have evaluated factors including joint mobility and laxity, and muscle
length. Only limited ankle dorsiflexion and increased hip external
rotation have been somewhat implicated in stress fracture development.77,78,91 Similarly, the contribution of foot structure to stress fracture risk is controversial.7,122,169
For example, some studies support an association in male military
recruits between high midfoot arch and greater risk of stress fracture.79,169 This correlation does not appear in all studies.130
The stress fracture-foot type relationship is likely variable depending
on which bone is involved. Leg length discrepancy actually appears to
increase the chance of stress fracture for military and athletic
individuals, but the risk is not specific to either the shorter or the
longer limb.17,38,68 The second metatarsal and second toe lengths do not correlate to risk of second metatarsal base stress fracture in dancers.55
stimuli transmitted to the bone. Conventionally, the training surface
is considered a factor in the development of stress fracture. Most
advise athletes to avoid training on hard, uneven surfaces, but no
clear scientific data support or refute this recommendation.13,109
Although ground reaction forces decrease with more compliant running
surfaces, these same surfaces may result in more or earlier muscle
fatigue.124,175
Even in military recruits, who display more variability in body size
than typical groups of similar athletes, no consistent associations
between stress fractures and body size and composition can be
demonstrated.49,77,179,192
endogenous hormones, sex hormones, primarily in women, appear to have
substantial impact on the stress fracture risks. No relationship
between lowered testosterone levels and stress fractures exists for
male athletes.170 Even when testosterone levels are decreased, they are typically within the range of normal for healthy adult men.88,117,171
Conversely, female athletes with menstrual irregularities uniformly are
found to have an increased risk for the development of stress
fractures. These women with menstrual disturbances present a two to
four times higher relative risk for stress fractures than eumenorrheic
athletes.12 Also, amenorrheic athletes are at a higher risk of developing multiple stress fractures.8 Yet use of oral contraceptives does not conclusively reduce the risk of stress fractures in these athletes.51,104
Lifetime menstrual history similarly yields information regarding the
risk of stress fracture, with the historically regular athletes
reporting a 20% less risk than those with very irregular menstrual
cycles.
risk with menstrual disturbance is unclear and most certainly
multifactorial. Nevertheless, the association is unassailable and
frequently found presenting together with eating disorders and
osteopenia. This combination, known as the female athlete triad, mandates attention be directed to all facets of the patient’s condition.12,64,141 Eating disorders occur more commonly in female athletes than males.94,144 Even active duty female soldiers admit to an 8% prevalence of eating disorders.112
Disordered eating patterns appear to increase the risk of stress
fractures in ballet dancers and young adult female track athletes.16,72 Indeed, extreme weight-control behavior in college athletes doubles the risk of stress fracture.132 Lower dietary calcium intake may well be an independent risk factor, particularly for female runners with irregular menses.51,104
incidence appears in late adolescence and early adulthood among
military recruits, competitive and recreational athletes, and dancers.14,19,81,92,95,122
Age is an important factor in determining the location of stress
fractures, but age does not appear to be an important factor in their
etiology.92
imaging studies, especially when a careful history and a classic
physical exam combine to make the diagnosis with certainty. However,
several radiographic modalities are at the disposal of the clinician
for definitive documentation and differential evaluations. Plain
radiographs, bone scintigraphs, computed tomography (CT) scans, and
magnetic resonance (MR) images are now the routine studies used to
evaluate and diagnose stress fractures.
process typically are not effective in demonstrating an abnormality.
Seldom do radiographic findings appear before 2 to 3 weeks from the
onset of symptoms. New periosteal bone formation, the classic
radiographic marker of a healing response, often does not appear until
3 months from symptom onset. Radiographic changes never appear for some
stress fractures in some patients.46
When changes are evident, several findings confirm the presence of a
stress fracture, rendering this modality poorly sensitive but highly
specific. Only 20% of bone scan foci positive for stress fractures
correlate with positive plain radiographic findings.127,196
The false-negative rate for radiographs approaches 100% for early Grade
I bone scan-positive lesions but drops to 24% for Grade III lesions,
demonstrating that stress fractures later in their course have more
ability to remodel and respond to the altered stresses, and the later
response often is apparent on plain radiographs.
formation, horizontal or oblique linear patterns of sclerosis,
endosteal callus, and a frank fracture line. The initial radiographic
sign of a progressing stress fracture is the so-called gray cortex,
which corresponds to a low-density cortical area affected by increased
osteoclastic bone resorption activity42 (Fig. 19-1).
As the process evolves in long bones, the stress fracture undergoes
marginal resorption and may yield an ovoid lucency within a thickened
area of cortical hyperostosis.29 A
late-stage stress fracture in cortical bone appears as a radiolucent
line with extension partially or completely across the cortex.
Similar-stage stress fractures in cancellous bone demonstrate a
fracture lucency oriented perpendicular to the trabeculae. Healing is
denoted by focal sclerosis in areas of cancellous bone, while
diaphyseal healing involves both periosteal and endosteal cortical
thickening.29 Plain films are most
likely to present positive findings in the fibula and metatarsals. The
x-ray beam should be centered over the painful, suspected bone. Plain
films typically are not helpful in discerning stress injuries to the
pars interarticularis. Some authors contend that plain films are
unlikely to yield positive results when investigating possible tibial
stress fractures, while others state the femur, pars interarticularis,
and tarsal bones are least likely to yield remarkable findings on
initial plain film investigation.29,46
studies are not required. If multiple sites of stress fracture are
possible based on history and physical exam, or if plain films do not
support the presumptive diagnosis of stress fracture, three-phase bone
scintigraphy has been the study of choice. Bone scan has long been
considered the most sensitive test for stress fracture, with
sensitivity approaching 100%.42,46 However, the sensitivity is not coupled with high specificity, so clinical features must be correlated.
different atomic weights, while a nuclide is the nucleus of a given
isotope. Nuclides or isotopes with differences in numbers of
protons
and neutrons are unstable and give off particles or electromagnetic
radiation in their transition to stability; this is known as radioactive decay.
These materials are synonymously termed radionuclides or radioisotopes.
When used for diagnostic purposes, the materials are termed
radiopharmaceuticals and radiotracers.163
 |
|
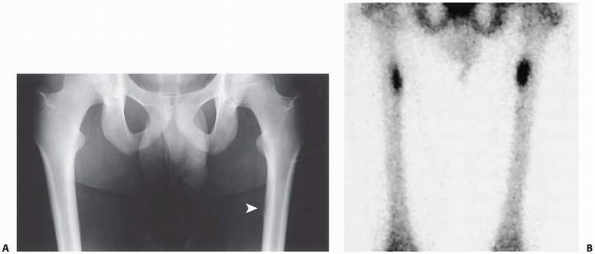
FIGURE 19-1 Imaging studies for a 20-year-old distance runner with bilateral proximal activity-related thigh pain. A. A plain radiograph demonstrates the gray cortex on the left femur (arrow) with minimal changes on the right. B.
Delayed spot image scintigraphic study shows Grade 3 increased activity at the left proximal femur, while the right side demonstrates a slightly less intense increased signal. |
MDP) is the radioisotope usually used for bone scans. Gamma radiation
is emitted, and the whole body dose for a bone scan is about 0.13 to
0.19 rad. The bladder dose, where the radioactivity is concentrated in
the urine, is 2.62 to 3.90 rads—hence, the need for frequent voiding
during and after the scanning period.
cost, has a 6-hour half-life, and emits gamma energy at an ideal
frequency for gamma cameras used in diagnostic imaging.163
intravenously. The mechanism of uptake in bone is not precisely
elucidated, but blood flow to the bone is a fundamental requirement. In
normal bone, uptake is in proportion to blood flow to the bone.
However, in abnormal situations like stress fractures that are
accompanied by high bone vascularity, factors other than bone blood
flow play a larger role in radiotracer uptake. New bone formation
proves to be the most important factor in the uptake, whereas bone
destruction without new bone formation yields no increase in uptake.29,163
and one delayed. The initial images acquired immediately after
radiotracer injection are representative of blood perfusion to bone and
soft tissue and correspond roughly to contrast angiography. The second
set of images, obtained approximately 2 to 5 minutes after injection
and termed the blood pool scans,
demonstrate radionuclide location in the soft tissues or extravascular
space. These images reflect the extent of hyperemia and capillary
permeability and generally correspond to the acuity and severity of the
injury. At 2 to 4 hours after injection, the delayed images document
radionuclide accumulation in the skeleton and, to a lesser extent, the
soft tissue. Over this time, 50% of the diphosphonate tracer is
postulated to be adsorbed on the hydroxyapatite matrix of bone, with
special affinity for new bone formation sites.46
scintigraphic diagnosis of stress fracture is made by focal increased
uptake on the third-phase images. Stress fractures are positive on all
three phases, but periostitis develops positive foci only on the
delayed images.5,29,157
Other soft tissue injuries are positive only in the first two phases,
allowing some differentiation between bony and soft tissue pathology.
However, the lack of specificity remains a disadvantage of this
modality.29,46
The typical list of conditions producing similar localized uptake
includes osteoid osteoma, other bony tumors, osteomyelitis, bony
infarct, and bony dysplasias. Due to its improved ability to
differentiate many of these conditions, MR imaging may be the
diagnostic method of choice in certain settings.
Acute stress fractures are positive on all three phases. As bony
healing proceeds, the initial phase perfusion scan normalizes first.
Within the ensuing few weeks, the blood pool second phase images return
to normal. Since bony remodeling continues for an extended period,
focal uptake on the delayed images resolves last. Uptake gradually
diminishes in intensity over a three to six month period, but some
increased uptake can last up to a year, even in uncomplicated stress
fractures with uneventful healing.5 Bone scans are not therefore particularly useful for monitoring healing and do not merit frequent repeating.
allows classification into milder or more severe stress fractures,
recognizing that these stress injuries occur along a continuum of bony
involvement196 (Table 19-1).
The minimally symptomatic Grade 1 or Grade 2 stress fractures typically
resolve more quickly and completely. The grading system can assist in
prescribing the requisite rest and rehabilitation intervals29 (Fig. 19-1).
rotates about the patient, generating three-dimensional images of
radioisotope uptake. This modality is particularly useful for
investigating suspected pars interarticularis and sacral stress
fractures.29,42
|
TABLE 19-1 Bone Scintigraphy and Magnetic Resonance Imaging Grading Scale
|
|||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||
specificity compared with bone scintigraphy for the evaluation of
stress fractures.100,152
The improved specificity derives from the comprehensive anatomic
visualization provided from this modality, allowing for precise
localization of the injury and differentiation from other possible
conditions. The bony tissue, with comparatively few mobile protons, is
not represented in significant detail. Instead, MR imaging accentuates
reactive edema in the soft tissues and marrow surrounding a stress
injury. This soft tissue response is seen best in edema-sensitive
sequences like fat-suppressed T2-weighted and short tau inversion
recovery (STIR) scans. Areas of edema appear as high signal intensity
sites on these sequences.29,57
grading system addresses the typical progression of stress injury
documented on MR images66 (Table 19-1).
Earliest injuries demonstrate increased signal intensity first in the
periosteum, then also in the marrow on STIR and T2-weighted images,
while the T1 scans are normal. In Grade 3 injuries, decreased marrow
signal occurs with the T1 sequence, while the STIR and T2 sequences
yield even higher intensity marrow changes. Grade 4 stress fractures
feature a low signal fracture line on both sequences continuous with
the cortex and medullary space57,66 (Fig. 19-2).
accurately diagnose stress fractures in most patients, MR images are
increasingly advocated as the study of choice.29,46,81 MR imaging
involves no exposure to ionizing radiation and requires much shorter
imaging times than bone scintigraphy. The specificity of MR images
significantly exceeds that of scintigraphs.168
Thus, straightforward cases can be investigated reliably without MR
imaging, but more difficult diagnostic dilemmas or problematic cases
warrant MR imaging, which is now regarded as the overall best technique
for assessment.67,75,172
 |
|
FIGURE 19-2
Coronal T1-weighted magnetic resonance image of a Grade 4 distal tibia stress fracture with visible fracture line and surrounding marrow edema. |
delineation of fracture line orientation is assisted with
three-dimensional CT information, which may improve treatment decisions
for certain bones such as the tarsal navicular.107,108
Longitudinal fracture lines in diaphyseal locations can also be
elucidated. Pars and sacral stress fractures are well characterized
with CT scans as well.42
modified rest to allow the bone remodeling process to equilibrate. The
inciting strain must be eliminated to break the cycle of accelerated
resorption, allowing new bone formation to catch up and adequately
repair the focus of stress fracture.42,150
Earlier initiation of rest, when the resorption-formation mismatch is
minimal, allows a brief period of activity restriction to suffice.126 For athletes, alternative training should continue provided regimens can be devised that unload the area of stress fracture.22 For nonathletes, a brief period of rest is usually well tolerated and adequate to reverse the process.
management approaches, but the overarching message of activity
modification and rest applies to every site.60,99
During this first phase of treatment, remediable risk factors should be
addressed. The training errors or changes that precipitated the stress
fracture should be identified and corrected.110
Braces or other forms of immobilization are seldom needed. No
controlled study strongly supports adjunctive measures like external
electrical stimulation or ultrasound.9,11,26,122,153
For high-level athletes, early pool running programs prove highly
successful at maintaining baseline fitness during the rest phase.28,76
The training program emphasizes progressive aerobic conditioning with
specified rest times to permit bone compensation for the slowly
increasing strains.28,164
Provided the progression does not reproduce the patient’s pain,
activity reintroduction proceeds steadily. Cross-training is advisable
to reduce the likelihood of recurrence.28
Surgery is seldom contemplated or required for the management of most
stress fractures. No study proves or disproves an adverse link between
healing of stress fractures and use of nonsteroidal anti-inflammatory
drugs.189 A trial of prophylactic
treatment with risedronate failed to demonstrate a reduction in stress
fracture risk among infantry recruits.125
prevents catastrophic consequences. Younger patients typically present
with inferior or medial neck lesions, commonly known as
compression-side stress fractures. Older patients are prone to
superior, tension-side fractures, and these are more likely to fail and
displace with continued activity.34,73,74
With either lesion, patients complain of activity-related diffuse groin
or anterior hip pain and have pain at the limits of hip rotation on
exam. MR images may be more accurate than scintigraphy in this region
and provide differential information for other causes of hip pain like
tendonitis, bone cysts, or avascular necrosis of the femoral head.168
treated with a modified rest protocol beginning with an initial period
of non-weight bearing until pain resolves. Stage 3 compression side
injuries, demonstrating a nondisplaced cortical crack, are still stable
and can be managed nonoperatively73,145 (Fig. 19-3).
Tension-sided stage 3 injuries, with a nondisplaced crack, can be
managed similarly with complete unloading and frequent clinical and
radiographic follow-up to document healing.50,73
However, because of the long-term functional consequences of a
displaced femoral neck fracture, some authors support stabilization
with cannulated screw fixation for this injury.61
Stage 4 injuries demonstrate widening of the cortical crack or even
frank displacement of the completed fracture. These injuries demand
operative stabilization. Nondisplaced complete fractures are stabilized
with multiple screws. Fluoroscopy-guided curettage of the tension side
fracture site has been advocated. In young people with displaced
fractures, emergent open reduction with internal fixation (ORIF) is
mandatory.73,188
A recent series of displaced femoral neck stress fractures in military
recruits identified an association between delayed surgery and varus
malreduction and an increased risk of both avascular necrosis and poor
function.114 In older patients, consideration can be given to hip arthroplasty depending on the individual situation.
Vague activity-related anterior thigh pain is the typical complaint,
and vigorous stressing on physical exam can reproduce the pain.34 Some longitudinal stress fractures, parallel to the cortex, appear best in MR images.182 Other sites including the distal femoral supracondylar region are also susceptible to stress fractures.159
Femoral shaft lesions occur in sites of compressive stress, are stable,
and heal with modified rest protocols. Only catastrophic complete
failures require reamed intramedullary stabilization.
 |
|
FIGURE 19-3
Coronal T1-weighted pelvis magnetic resonance image of a 50-year-old female runner demonstrates a Grade 3 left compression-side femoral neck stress fracture. The darker marrow signal represents edema. |
Other overuse injuries may simultaneously present or require
elimination from the differential diagnosis. Inflammation of the
aponeurotic tenoperiosteal origins of the tibialis posterior and soleus
muscles and of the fascial attachments to the posterior medial border
of the tibia produces pain previously termed shin splints and now
characterized as medial tibial stress syndrome.6,177
Pain from this inflammatory situation typically occurs along the medial
border of the tibia, improves after warm-up, and is worse in the
morning. Exertional compartment syndromes of the anterior or deep
posterior compartments present with muscle aching and subjective
tightness that increase shortly after exercise begins. No bony
tenderness usually accompanies this condition. Tibial stress fracture
pain is progressive, with a gradual onset exacerbated by exercise and
made worse with impact, ultimately occurring while simply walking, or
even at rest or at night. Tenderness is localized and bony.31
posteromedial compression injuries and occur usually in the proximal or
distal thirds.21,31 When a fracture has developed, a transverse orientation is typical (Fig. 19-2), but longitudinal stress fractures also are reported.102
These fractures respond well to cessation of the repetitive loading
activity, which almost always is distance running, along with complete
leg rest using crutches until the pain subsides.31
Some work suggests adjunctive treatment with a pneumatic brace may
facilitate earlier functional return to activity by accelerating the
initial time to pain-free walking, but other investigators have not
demonstrated a benefit.3,155,178,190 Pulsed ultrasound and capacitively coupled electrical stimulation treatments do not significantly reduce the healing time.9,156 Surgery is not required for this condition, but return to activity can take up to 3 months.150
stress fracture appears in the middle third of the anterior cortex.
This tension-side injury results from repetitive stress of jumping or
leaping, as seen in basketball players and ballet dancers. Bone pain is
easily demonstrated, and palpable periosteal thickening may be present
if the process is chronic. These fractures frequently progress to
nonunion, and complete fractures are also reported.21,84 In chronic cases, a transverse, wedge-shaped defect in the anterior cortex, dubbed the dreaded black line, is often seen in conjunction with cortical hypertrophy150 (Fig. 19-4). Tissue obtained from these sites demonstrates limited healing potential, consistent with a pseudarthrosis.138,154
However, even over 4 to 6 months, many of these fractures with chronic
changes and anterior fissures or cracks will remain symptomatic and
nonunited. Some authors have shown healing benefits from adjunctive
electrical stimulation or ultrasound in nonoperative protocols,11,26,153 while others demonstrate no benefits from these modalities.84 Transverse drilling of the nonunion sites reportedly stimulates healing and speeds time to return to activity.110,138,150
Reamed intramedullary nailing works well for recalcitrant cases and now
has some support as the initial treatment of choice for the anterior
cortical stress fracture nonunion.45,146,187 Following nail fixation, return to sport within 4 months is typical, although failure to unite and knee problems are reported.142,187
A small series touts anterior tension band plating for this lesion in
elite female athletes, with return to full activity at 10 weeks.23
 |
|
FIGURE 19-4
Lateral radiograph of the left tibia of a collegiate track athlete demonstrates anterior cortical hypertrophy and the dreaded black line of an anterior tension-side stress fracture. |
activities are at risk for the development of medial malleolus stress
fractures characterized by bony tenderness and ankle effusion. The
typically vertically oriented fracture line originates at the junction
between the malleolus and plafond directly above the medial border of
the talus, which is postulated to be the cyclic force transmitter.21,167
For grade 1 and 2 injuries, impact avoidance in a cast or pneumatic
brace achieves return to function in 6 to 8 weeks. For grade 3 and 4
stress fractures, similar conservative measures are appropriate, but
healing may take 4 to 5 months. More aggressive intervention is also
supported depending on the injury chronicity and the demands of the
patient. Drilling
may enhance healing.139
Screw fixation for displaced fractures, nonunion, and chronic cases and
in elite performers allows early motion and may promote earlier return
to activity.21,31
sprinters, hurdlers, middle-distance runners, football players,
basketball players, ballet dancers, and other athletes at risk for
tarsal navicular stress fracture.36,122 The insidious onset of vague medial arch pain usually accompanies dorsal navicular tenderness to palpation.30
The stress fracture occurs in the sagittal plane in the relatively
avascular central third of the bone, originating at the proximal dorsal
articular surface and extending in a plantar distal direction.21,184 Plain radiography often fails to demonstrate the navicular stress fracture.106
Although bone scintigraphy is sensitive, CT or MR imaging provides
specific information regarding fracture completeness and orientation21 (Fig. 19-5).
Conversely, less than 25% of patients treated with weight-bearing
immobilization heal, and the risk of delayed union and recurrence is
also much higher.40,59,65,107,115,137,184
Following the initial period of strict non-weight bearing, graduated
return to activity is pursued provided the physical exam reveals no
navicular tenderness.30 In cases of displaced fractures, delayed unions, and nonunions, surgical stabilization is undertaken.21
Regardless of chronicity, some authors recommend ORIF when imaging
confirms extension of the stress fracture into the body of the
navicular.161 Compression screw
fixation alone usually provides adequate stability. Often the dorsal
cortex is not visibly disrupted, so placing supplemental bone graft may
require more extensive dissection except in cases of complete,
displaced stress fractures or nonunions.65,115
Non-weight bearing after fixation is advised. Surgical and conservative
management leads to good results, but most patients note slight
long-term pain and functional loss even after return to activity.148
 |
|
FIGURE 19-5
T1-weighted magnetic resonance image of the right ankle of a collegiate basketball player shows a navicular stress fracture (arrow) originating at the talonavicular joint surface. |
The second metatarsal neck is the most likely site for stress fracture,
but all metatarsals are susceptible. Gradually worsening forefoot pain
exacerbated by running or dancing herald the diagnosis, especially when
accompanied by focal bony tenderness. For short-lived complaints,
initiation of modified rest without imaging studies usually leads to
symptom resolution. For uncertain diagnoses or chronic complaints,
imaging modalities provide clarification. A second metatarsal plantar
base stress fracture previously recognized only in female ballet
dancers appears to be secondary to the en pointe position and responds to rest and activity modification.82,136
This stress fracture site has now been reported in nondancer athletes,
and 50% of the patients in those small series required surgery for
nonunion.47,160
metatarsal, common in basketball players, often are slow to heal, and
can demonstrate high recurrence rates.97,183
The problematic site is in the proximal 1.5 cm of the diaphysis, where
cortical hypertrophy commonly occurs in running and jumping athletes,
rendering the zone relatively avascular with a narrow medullary canal.54 Treatment choices are predicated on the stage of the lesion as described by Torg and colleagues.183,185
Patients with acute fractures often acknowledge a 2- to 3-week
prodromal history of activity-related lateral foot pain. These acute
injuries show clear fracture lines with no medullary sclerosis and
little or no cortical hypertrophy. Healing in most acute fractures
ensues with a 6- to 8-week course of non-weight-bearing cast
immobilization.1,48,185,195 Closed treatment with full weight bearing appears to predispose to nonunion and refracture.97
Surgical management of acute stress fractures, especially in athletes,
is recommended by some to avoid prolonged healing. Sliding bone graft
procedures53,86,194 and intramedullary compression screw fixation56,101 techniques usually result in satisfactory healing within 3 months.128
symptoms will have radiographic evidence of delayed union or nonunion.
Delayed unions demonstrate a wider fracture completely through the
medial and lateral cortices with some medullary sclerosis (Fig. 19-6).
A very wide gap with periosteal new bone formation and complete
medullary sclerosis characterizes the appearance of established
nonunions.183,185 Delayed unions may heal with prolonged non-weight-bearing cast immobilization, but functional recovery often requires 6 months.185,195
Most active patients with delayed union and virtually all with an
established nonunion recover faster with surgical management. Torg185 advises sclerotic bone débridement and inlay bone
grafting. Others propose a sliding bone graft53 or compression screw fixation56,113,147 (Fig. 19-6). For those averse to surgery, electrical stimulation has been shown to be effective.90
 |
|
FIGURE 19-6 Middle-aged recreational runner with several-month history of worsening activity-related lateral foot pain. A.
Intermediate delayed union fifth metatarsal stress fracture with a complete fracture, some widening of the cortical gap, and moderate medullary sclerosis. B. Radiographic appearance 3 months following medullary drilling, bone grafting, compression screw stabilization, and initial period of non-weight bearing. |
bones in the lower extremity. Rare patellar stress fractures, usually
transverse but occasionally longitudinal, respond to extension
immobilization for 4 weeks followed by progressive rehabilitation.31,121,181
Runners and jumpers are susceptible to this injury. Failure to improve
and acute displacement are indications for open management with tension
band stabilization.140 Fibular
stress fractures occur typically in runners 1 to 2 inches above the
ankle joint line, are much less common than tibial injuries, and
usually respond to modified rest protocols.110,129 Talar neck and body stress fractures are rare, but talar head stress lesions appear in military recruits.173
Nonoperative management produces healing with only mild residual
symptoms. Stress fractures of the lateral process of the talus are
encountered on occasion, and a 6-week period of non-weight-bearing
produces control of symptoms.30,110 Surgical stabilization or excision may be considered for recalcitrant or displaced cases.20,24
Calcaneal stress fractures typically occur transversely through the
tuberosity in soldiers, runners, ballet dancers, and jumpers.30,174Conservative
treatment measures are always sufficient. Similarly, a few reports of
cuboid and cuneiform stress fractures describe successful modified rest
treatment protocols.105,119
Some calcaneal stress fractures occur in isolation, but most calcaneal
and other tarsal stress fractures are associated with at least one
other foot stress injury best diagnosed by MR imaging.133,174
repetitive strains associated with recurrent loading activities like
rowing, swimming, and throwing. The possibility of stress fracture
should be considered in athletes primarily involved in upper extremity
sports who complain of the gradual onset bony pain associated with the
activity. Physical examination typically reveals bony tenderness to
palpation and stressing. Imaging modalities are useful for clarifying
the diagnosis. Modified rest and training technique corrections or
alterations almost always result in early healing and return to
activity.37
competitive rowers, typically anterolaterally between the fourth and
ninth ribs.59 Most humerus stress
fractures occur in baseball pitchers, although other reports detail
occurrence in athletes ranging from tennis players to weight lifters.37
All of these athletes can be managed with modified rest and gradual
resumption of activity. One report describes progression of humerus
stress fractures to spontaneous shaft fractures in men in a baseball
league.25 The risk factors for
complete fracture include age over 30 years, a prolonged layoff from
pitching before resumption of participation, no regular exercise
program, and prodromal arm pain.
throwing sports or gymnastics, the presentation of gradually increasing
elbow pain with activity mandates consideration of an olecranon stress
fracture.37 Some patients who
complain less of prodromal symptoms and more of acute elbow pain
related to a particularly strong throwing effort may have tip avulsion
fractures involving up to the proximal third of the olecranon. Surgical
excision of the fractured tip allows early return to sport.135
Patients with classical stress fractures complain of longer duration
pain that recurs when throwing resumes. These fractures are usually
transverse and in the middle third of the olecranon. Among baseball
players, the olecranon is the most common site for stress fracture.
Adolescent gymnasts can also develop this stress fracture.118 For nondisplaced fractures, immobilization and progressive return to activity are recommended. When displaced
or delayed in healing, tension band fixation is effective.118,135,191
softball pitchers, tennis players, weight-lifters, and volleyball
players. Repetitive strains from underhanded softball pitching and
twohanded tennis backhand strokes are representative of the typical
inciting stresses. The athletes complain of bony pain with activity and
even after the activity. Depending on the stage of injury, radiographs
may demonstrate periosteal bone formation or a small cortical fracture.
All reports document healing with modified rest for 4 to 6 weeks and
progressive resumption of activity.35,37
but radial shaft stress fractures in young adults are less common.
Bilateral radial shaft stress fractures have been seen in a gymnast who
doubled her weekly training time.2
Athletes in any sport who begin a high-stress weight program are at
risk for developing a radial stress reaction. The typical modified rest
protocol should be instituted for the radius. If weight training is the
inciting stress but the athlete’s primary sport does not repetitively
load the radius, continued participation in the sport usually presents
no additional risk.
Patients describe a change in training volume and technique. Tennis
players may be susceptible at the second metacarpal because the racquet
provides a fulcrum.131 Rest from the
activity will yield healing and return to sport within 4 weeks,
provided technique errors and training overload are altered.
in female distance runners, most of whom have associated risk factors,
as well as female military recruits.89
When present, groin pain prevents further training, and single leg
stance reproduces the pain. Deep palpation of the bone in these
characteristically thin individuals typically elicits significant pain.
Plain films and bone scintigraphs are usually diagnostic. An 8- to
12-week modified training regimen allows graduated return to activity.134
distance runners but are also reported in their male counterparts.
Female military conscripts show dramatically increased risks for this
site.123 Most have prodromal low
back and buttock pain. Physical exam demonstrates localized tenderness
to palpation and stress of the sacroiliac region. SPECT scanning has
been the investigation of choice, but MR imaging now provides more
specificity. Implementation of initial protected weight bearing
followed by a progressive activity regimen reliably leads to uneventful
healing.32,63
majority of stress fractures, and this initial conservative approach
should be considered for all stress fractures and implemented for most.
However, patients with certain high-risk or problematic stress
fractures may benefit from early surgical intervention. Grade 3 or
grade 4 tension-side femoral neck stress fractures should be stabilized
with multiple screw fixation to promote healing and prevent
displacement. Because the patients who develop this injury are usually
runners, care must be taken to place the screws in good position and
avoid lateral entry points below the midportion of the level of the
lesser trochanter to minimize the risk of iatrogenic subtrochanteric
fracture from stress risers. Acutely displaced femoral neck stress
fractures require urgent ORIF in the typical younger, active population.
transverse cortical lucency have limited healing potential even with
activity modification. For patients who fail the rest and
rehabilitation protocol, or for those unwilling or unable to modify
their activities for perhaps as long as 1 year, reamed intramedullary
nailing predictably leads to healing of the stress fracture in a
shorter time course. Inadequate data make prediction of long-term
functional outcomes following nailing uncertain with regard to return
to unrestricted sport or military activity.
6-week period of non-weight-bearing cast immobilization is the
treatment of choice. For patients with delayed diagnosis or delayed
union, compression screw stabilization provides high union rates.
Displaced fractures and established sclerotic nonunions require ORIF
and supplemental bone graft.
strict non-weight-bearing cast immobilization seldom require further
intervention. Many high-demand athletes may prefer cannulated screw
fixation for these acute fractures to speed return to activity. The
intermediate delayed union injury is preferentially managed with
intramedullary compression screw placement after the medullary canal at
the fracture site has been adequately drilled to remove fibrous tissue
and sclerotic bone (Fig. 19-6). The established
nonunion requires open débridement of the fracture gap with placement
of graft, combined with intramedullary screw placement, although a
recent report encourages use of a cannulated 4.5-mm screw without
exposure of the nonunion site and with an accelerated rehabilitation
program of progressive early loading and use of a semirigid full-length
shoe insert.147
and Weyton Tam, MD, for providing the figures in this chapter, and
Sheila M. Algan, MD; W. Bentley Edmonds, MD; Don McGinnis, MD; and
Brock Schnebel, MD, for providing cases and sports medicine expertise.
JH, Drez D Jr. Nonoperative treatment of stress fractures of the
proximal shaft of the fifth metatarsal (Jones fracture). Foot Ankle
1986;7:152-155.
R, Datz FL, Morton KA, et al. Bilateral fatigue fractures of the radial
shaft in a gymnast. Clin Nucl Med 1994;19:665-667.
CS, Flynn TW, Kardouni JR, et al. The use of a pneumatic leg brace in
soldiers with tibial stress fractures: a randomized clinical trial.
Milit Med 2004;169:880-884.
SA, Williams KM, Shaffer RA, et al. Epidemiological patterns of
musculoskeletal injuries and physical training. Med Sci Sports Exerc
1999;31:1176-1182.
Y, Yasuda K, Tohyama H, et al. Magnetic resonance imaging in stress
fractures and shin splints. Clin Orthop Relat Res 2004;421:260-267.
A, Wheat J, Milner C. Association between foot type and tibial stress
injuries: a systematic review. Br J Sports Med 2008;42:93-98.
GW, Saha S. Menstrual irregularity and stress fractures in collegiate
female distance runners. Am J Sports Med 1988;16:209-216.
BR, Matheson GO, Bergman G, et al. Do capacitively coupled electric
fields accelerate tibial stress fracture healing? A randomized
controlled trial. Am J Sports Med 2008; 36:545-553.
TJ, Ruff CB, Mourtada FA, et al. Dual-energy x-ray absorptiometry
derived structural geometry for stress fracture prediction in male U.S.
Marine Corps recruits. J Bone Miner Res 1996;11:645-653.
F, Mosconi M, Beccarisi G, et al. Use of capacitive coupled electric
fields in stress fracture in athletes. Clin Orthop 1995;310:145-149.
K, Grimston S. Factors associated with the development of stress
fractures in women. In: Burr DB, Milgrom C, eds. Musculoskeletal
Fatigue and Stress Fractures. Boca Raton: CRC Press, 2001:35-54.
K, Grimston S. Risk factors for developing stress fractures. In: Burr
DB, Milgrom C, eds. Musculoskeletal Fatigue and Stress Fractures. Boca
Raton: CRC Press, 2001: 15-33.
KL, Malcolm SA, Khan KM, et al. Bone mass and bone turnover in power
athletes, endurance athletes, and controls: a 12-month longitudinal
study. Bone 1997; 20:477-484.
KL, Malcolm SA, Thomas SA, et al. Risk factors for stress fractures in
female track-and-field athletes: a retrospective analysis. Clin J
Sports Med 1995;5:229-235.
KL, Malcolm SA, Thomas SA, et al. Risk factors for stress fractures in
track and field athletes: a 12-month prospective study. Am J Sports Med
1996;24:810-818.
KL, Malcolm SA, Thomas SA, et al. The incidence and distribution of
stress fractures in competitive track and field athletes. A 12-month
prospective study. Am J Sports Med 1996;24:211-217.
D, Kemper A, Brolinson PG. Current concepts in the evaluation and
management of stress fractures. Curr Sports Med Rep 2005;4:295-300.
O, Sen MK, Huang PC, et al. Anterior tension band plating for anterior
tibial stress fractures in high-performance female athletes: a report
of four cases. J Orthop Trauma 2006;20:425-430.
C, Khan K, Brukner P. Stress fracture of the body of the talus in
athletes demonstrated with computer tomography. Clin J Sports Med
1996;6:48-51.
T, Partin C, Chamberland P, et al. Spontaneous fractures of the humerus
during pitching: a series of 12 cases. Am J Sports Med 1992;20:468-470.
JC Jr, Brindle T, Nyland J, et al. Does pulsed low intensity ultrasound
allow early return to normal activities when treating stress fractures?
A review of one tarsal navicular and eight tibial stress fractures.
Iowa Orthop J 1999;19:26-30.
P, Bennell K, Matheson G. Diagnosis of stress fractures II. In: Stress
Fractures. Victoria: Blackwell Science, 1999:97-105.
P, Bennell K, Matheson G. Diagnosis of stress fractures I. In: Stress
Fractures. Victoria: Blackwell Science, 1999:83-96.
P, Bennell K, Matheson G. Stress fractures of the foot and ankle. In:
Stress Fractures. Victoria: Blackwell Science, 1999:163-186.
P, Bennell K, Matheson G. Stress fractures of the lower leg. In: Stress
Fractures. Victoria: Blackwell Science, 1999:147-161.
P, Bennell K, Matheson G. Stress fractures of the trunk. In: Stress
Fractures. Victoria: Blackwell Science, 1999:119-138.
P, Bennell K, Matheson G. The pathophysiology of stress fractures. In:
Stress Fractures. Victoria: Blackwell Science, 1999:1-13.
P, Bennell K. Matheson G. Stress fractures of the pelvis and thigh. In:
Stress Fractures. Victoria: Blackwell Science, 1999:139-146.
P, Bennell K. Matheson G. Stress fractures of the upper limb. In:
Stress Fractures. Victoria: Blackwell Science, 1999:107-117.
ME, Cook SD, Brinker MR, et al. A survey of running injuries in 1505
competitive and recreational runners. J Sports Med Phys Fitness
1990;30:307-315.
SG, Mahoney CM, Forster BB, et al. Tarsal navicular stress injury:
long-term outcome and clinicoradiological correlation using both CT and
MRI. Am J Sports Med 2005;33:1875-1881.
RD, Matheson GO, Carter DR. Stress fractures and stress injuries in
bone. In: Garrick JG, ed. Orthopaedic Knowledge Update: Sports
Medicine. 3rd ed. Rosemont, IL: American Academy of Orthopaedic
Surgeons, 2004:273-283.
PS, Harris RM. Intramedullary nailing for chronic tibial stress
fractures: a review of five cases. Am J Sports Med 1996;24:688-692.
R. The role of various imaging modalities in diagnosing stress
fractures. In: Burr DB, Milgrom C, eds. Musculoskeletal Fatigue and
Stress Fractures. Boca Raton: CRC Press, 2001:279-293.
B, Cook C, Nunley JA. Stress fractures of the second metatarsal base
occur in nondancers. Clin Orthop Relat Res 2007;461:197-202.
MF, O’Brien TJ, Lyons PM. Fractures of the fifth metatarsal: analysis
of a fracture registry. Clin Orthop Relat Res 1995;315:238-241.
AD, Jansen GR, Melby CL. Stress fractures in female army recruits:
implications of bone density, calcium intake, and exercise. J Am Coll
Nutr 1998;17:128-135.
KL, Bachrach LK, Sowers M, et al. The effect of oral contraceptives on
bone mass and stress fractures in female runners. Med Sci Sports Exerc
2007;39:1464-1473.
K, Bennell KL, Wrigley T, et al. Ground reaction forces, bone
characteristics, and tibial stress fracture in male runners. Med Sci
Sports Exerc 1999;31:1088-1093.
TB Jr. Fractures and anatomical variations of the proximal portion of
the fifth metatarsal. J Bone Joint Surg Am 1975;57A:788-792.
TB Jr. Fractures of the proximal fifth metatarsal: selecting the best
treatment option. J Am Acad Orthop Surg 1995;3:110-114.
G, Pizzari T, Mayes S. The influence of second toe and metatarsal
length on stress fractures at the base of the second metatarsal in
classical dancers. Foot Ankle Int 2007;28:1082-1086.
AL, Coel MN, Mink JH. Imaging of stress injuries to bone: radiography,
scintigraphy, and MR imaging. Clin Sports Med 1997;16:275-290.
S, Giombini A, Di Cesare A, et al. Stress fractures of the ribs in
elite competitive rowers: a report of nine cases. Skeletal Radiol
2007;36:951-954.
KA, Frankel VH. Problematic stress fractures. In: Burr DB, Milgrom C,
eds. Musculoskeletal Fatigue and Stress Fractures. Boca Raton: CRC
Press, 2001:305-319.
I. Physical diagnosis of stress fractures. In: Burr DB, Milgrom C, eds.
Musculoskeletal Fatigue and Stress Fractures. Boca Raton: CRC Press,
2001:271-278.
KD, Blackwell JB, Gilmour WN. Operation for nonunion of stress fracture
of the tarsal navicular. J Bone Joint Surg Br 1989;71B:105-110.
M, Bergman AG, Hoffman KL, et al. Tibial stress reaction in runners:
correlation of clinical symptoms and scintigraphy with a new magnetic
resonance imaging grading system. Am J Sports Med 1995;23:472-481.
HM. Wolff law and bone’s structural adaptation to mechanical usage: an
overview for clinicians. Angle Orthod 1994;64:175-188.
NT, Dhuper S, Warren MP, et al. Nutrition and the incidence of stress
fractures in ballet dancers. Am J Clin Nutr 1990;51:779-783.
M, Minutoli F, Scribano E, et al. CT and MR imaging findings in
athletes with early tibial stress injuries: comparison with bone
scintigraphy findings and emphasis on cortical abnormalities. Radiology
2005;235:553-61.
MM, Keller BA, Brehm BA. Water running with and without a flotation
vest in competitive and recreational runners. Med Sci Sports Exerc
1997;29:1374-1378.
M, Milgrom C, Stein M, et al. External rotation of the hip. A predictor
of risk for stress fractures. Clin Orthop Relat Res 1987;216:131-134.
M, Milgrom C, Stein M, et al. The low arch, a protective factor in
stress fractures. A prospective study of 295 military recruits. Orthop
Rev 1985;14:709-712.
RB, Gerber FH, Laughlin RL, et al. Distribution and natural history of
stress fractures in US Marine recruits. Radiology 1983;146:339-346.
SK. An application of mechanostat theory to research design: a
theoretical model. Med Sci Sports Exerc 1993;25:1293-1297.
ML, Haarbo J, Christiansen C. Low bone mass and high bone turnover in
male long-distance runners. J Clin Endocrinol Metab 1993;77:770-775.
N, Ashkenazi I, Levi Y, et al. Characteristics of skeletal stress
fractures in female military recruits of the Israel defense forces on
bone scintigraphy. Clin Nucl Med 2006; 31:742-749.
GB Jr. Treatment of delayed unions and nonunions of the proximal fifth
metatarsal with pulsed electromagnetic fields. Foot Ankle
1994;15:552-556.
LY. Biomechanical analysis of the foot and ankle for predisposition to
developing stress fractures. J Orthop Sports Phys Ther 1985;7:96-101.
A, Orava S. The role of age in the development of stress and fatigue
fractures. In: Burr DB, Milgrom C, eds. Musculoskeletal Fatigue and
Stress Fractures. Boca Raton: CRC Press, 2001:55-71.
AW, Weiss CB Jr, Wheeler, DL. Stress fractures of the femoral shaft in
athletes: more common than expected. A new clinical test. Am J Sports
Med 1994;22:248-256.
C, Powers PS, Dick R. Athletes and eating disorders: the National
Collegiate Athletic Association study. Int J Eating Disorders
1999;26:179-188.
BH, Cowan DN, Tomlinson JP, et al. Epidemiology of injuries associated
with physical training among young men in the army. Med Sci Sports
Exerc 1993;25: 197-203.
BH, Harris J, Vinh TN, et al. Exercise-induced stress fractures and
reactions of bone. Epidemiology, etiology, and classification. Exerc
Sports Sci Rev 1989;17: 379-422.
PO, Karlsson M, Redlund-Johnell I, et al. Closed treatment of Jones
fracture: good results in 40 cases after 11-26 years. Acta Orthop Scand
1994;65:545-547.
EW, Jonson SR, Cohen ME, et al. Stress fractures of the pelvis in
female navy recruits: an analysis of possible mechanisms of injury.
Milit Med 2000;165:142-146.
JL, Bachrach LK, Procter-Gray E, et al. Risk factors for stress
fracture among young female cross-country runners. Med Sci Sports Exerc
2007;39:1457-1463.
KM, Fuller PJ, Brukner PD, et al. Outcome of conservative and surgical
management of navicular stress fracture in athletes. Am J Sports Med
1992;20:657-666.
ZA, Khan KM, Fuller PJ. Stress fractures of the tarsal navicular bone:
CT findings in 55 cases. AJR Am J Roentgenol 1993;160:111-115.
J, Tulikoura I, Konttinen Y, et al: Bone stress injuries of the lower
extremity: a review. Acta Orthop Scan 2002;73:359-368.
TD, Dixit S, Pezzin LE, et al. The relation between stress fractures
and bone mineral density: evidence from active-duty army women. Arch
Phys Med Rehab 2000; 81:73-79.
CH, Huang GS, Chao KH, et al. Surgical treatment of displaced stress
fractures of the femoral neck in military recruits: a report of 42
cases. Arch Orthop Trauma Surg 2003;123:527-533.
T, Triantafyllou SJ, Baker ER, et al. Women athletes with menstrual
irregularity have increased musculoskeletal injuries. Med Sci Sports
Exerc 1986;18:374-379.
JD, Webber CE, Martin J, et al. Relationship among running mileage,
bone density, and serum testosterone in male runners. J Appl Physiol
1992;73:1165-1170.
VM, Niva M, Kiuru M, Pihlajamaki H. Risk factors for bone stress
injuries: a follow-up study of 102,515 person-years. Med Sci Sports
Exerc 2007;39:1061-1066.
C, Finestone A, Novack V, et al. The effect of prophylactic treatment
with risedronate on stress fracture incidence among infantry recruits.
Bone 2004;35: 418-424.
C, Friedman E. Early diagnosis and clinical treatment of stress
fractures. In: Burr DB, Milgrom C, eds. Musculoskeletal Fatigue and
Stress Fractures. Boca Raton: CRC Press, 2001:295-303.
N, Shelbourne D, van Meter CD, et al. Outpatient percutaneous screw
fixation of the acute Jones fracture. Am J Sports Med 1993;21:720-723.
LC, Nelson FR, Norton JP, et al. Orthopedic history and examination in
the etiology of overuse injuries. Med Sci Sports Exerc 1989;21:237-243.
A, Puffer JC, Green GA. Lifestyles and health risks of collegiate
athletes: a multicenter study. Clin J Sports Med 1997;7:262-272.
MH, Sormaala MJ, Kiuru MJ, et al. Bone stress injuries of the ankle and
foot: an 86-month MRI-based study of physically active young adults. Am
J Sports Med 2007; 35:643-649.
GW, Diment MT. Olecranon stress fractures in throwers: a report of two
cases and a review of the literature. Clin Orthop 1992;278:58-61.
MJ, Hamilton WG, Munyak J, et al. Stress fractures at the base of the
second metatarsal in ballet dancers. Foot Ankle Int 1996;17:89-94.
S, Karpakka J, Hulkko A, et al. Diagnosis and treatment of stress
fractures located at the midtibial shaft in athletes. Int J Sports Med
1991;12:419-422.
S, Taimela S, Kvist M, et al. Diagnosis and treatment of stress
fracture of the patella in athletes. Knee Surg Sports Trauma Arthrosc
1996;4:206-211.
NK, Webner D, Sennett B, et al. Recurrent fracture after operative
treatment for a tibial stress fracture. Clin Orthop Relat Res
2006;456:254-258.
CL. The level of competition as a factor for the development of eating
disorders in female collegiate athletes. J Youth Adolesc
1999;28:583-595.
HK, Ruohola JP, Weckstrom M, et al. Long-term outcome of undisplaced
fatigue fractures of the femoral neck in young male adults. J Bone
Joint Surg Br 2006; 88B:1574-1579.
VF, Johansson CG, Micheli LJ. Anterior tibial stress fracture treated
with intramedullary nailing: a case report. Clin J Sports Med
1995;5:58-62.
DA, Duncan M, Meyer SJ. Fifth metatarsal Jones fracture fixation with a
4.5-mm cannulated stainless steel screw in the competitive and
recreational athlete: a clinical and radiographic evaluation. Am J
Sports Med 2005;33:726-733.
NJ, Brukner PD, Makdissi M, et al. Navicular stress fractures: outcomes
of surgical and conservative management. Br J Sports Med
2006;40:692-695.
D, Goergen TG. Physical injury: concepts and terminology. In: Resnick
D, Kransdorf MJ, eds. Bone and Joint Imaging, 3rd ed. Philadelphia:
Elsevier Saunders, 2005:789-830.
AC, Shelbourne KD, McCarroll JR, et al. The natural history and
treatment of delayed union stress fractures of the anterior cortex of
the tibia. Am J Sports Med 1988;16:250-255.
C, Ekenman I, Tornqvist H, et al. The anterior stress fracture of the
tibia: an atrophic pseudoarthrosis. Scand J Med Sci Sports
1997;7:249-252.
K, Handoll HH, Ashford R. Interventions for preventing and treating
stress fractures and stress reactions of bone of the lower limbs in
young adults. Cochrane Database Syst Rev 2005;CD000450.
JP, Armstrong DW 3rd, Frassica FJ, et al. The effect of pulsed
ultrasound in the treatment of tibial stress fractures. Orthopedics
2004;27:1192-1195.
ST, Bostman OM, Kiuru MJ, et al. Bilateral femoral fatigue fracture. An
unusual fracture in a military recruit. Clin Orthop Relat Res
2006;456:259-263.
J, Orava S, Alanen J. Operative treatment of stress fractures of the
proximal second metatarsal. Scand J Med Sci Sports 2007;17:383-386.
MB. Bone fatigue and remodeling in the development of stress fractures.
In: Burr DB, Milgrom C, eds. Musculoskeletal Fatigue and Stress
Fractures. Boca Raton: CRC Press, 2001:161-182.
R. Radionuclide techniques. In: Resnick D, Kransdorf MJ, eds. Bone and
Joint Imaging, 3rd ed. Philadelphia: Elsevier Saunders, 2005:86-117.
RA, Brodine SK, Almeida SA, et al. Use of simple measures of physical
activity to predict stress fractures in young men undergoing a rigorous
physical training program. Am J Epidemiol 1999;149:236-242.
RA. Incidence and prevalence of stress fractures in military and
athletic populations. In: Burr DB, Milgrom C, eds. Musculoskeletal
Fatigue and Stress Fractures. Boca Raton: CRC Press, 2001:1-14.
AY, Morin WD, Gorman JD, et al. The superiority of magnetic resonance
imaging in differentiating the cause of hip pain in endurance athletes.
Am J Sports Med 1996; 24:168-176.
A, Leichter I, Giladi M, et al. Combined effect of foot arch structure
and an orthotic device on stress fractures. Foot Ankle 1989;10:25-29.
ST, Burge MR. Prospective evaluation of risk factors for
exercise-induced hypogonadism in male runners. West J Med 1998;169:9-13.
R, Rutherford OM. Spine and total body bone mineral density and serum
testosterone levels in male athletes. Eur J Appl Physiol
1993;67:330-334.
MJ, Niva MH, Kiuru MJ, et al. Stress injuries of the calcaneus detected
with magnetic resonance imaging in military recruits. J Bone Joint Surg
Am 2006;88A: 2237-2242.
JR, Milburn PD. Effect of different synthetic sport surfaces on ground
reaction forces at landing in netball. Int J Sport Biomech
1988;4:130-145.
JC, Edelstein DW, Calvo RD, et al. Stress fractures in the athlete:
diagnosis and management. Sports Med 1992;14:336-346.
EJ, DeHaven KE, Sebastienelli WJ, et al. The effect of a pneumatic leg
brace on return to play in athletes with tibial stress fractures. Am J
Sports Med 1997;25: 322-328.
S, Kujala UM, Osterman K. Stress injury proneness: a prospective study
during a physical training program. Int J Sports Med 1990;11:162-165.
SJ, Theodorou DJ, Resnick D. Imaging findings in symptomatic patients
with femoral diaphyseal stress injuries. Acta Radiol 2006;47:377-384.
JS, Balduini FC, Zelko RR, et al. Fractures of the base of the fifth
metatarsal distal to the tuberosity: classification and guidelines for
nonsurgical and surgical management. J Bone Joint Surg Am
1984;66A:209-214.
JS, Pavlov H, Cooley LH, et al. Stress fractures of the tarsal
navicular: a retrospective review of 21 cases. J Bone Joint Surg Am
1982;64A:700-712.
HK, Jaworski ZG. Periosteal stress-induced reactions resembling stress
fractures: a radiologic and histologic study in dogs. Clin Orthop Relat
Res 1985;199: 284-291.
KE, Younas SA, Lintner DM, et al. Chronic anterior midtibial stress
fractures in athletes treated with reamed intramedullary nailing. Am J
Sports Med 2005;33: 1071-1076.
T, Vara A, Meurman KO. Displaced stress fractures of the femoral neck
in young male adults: a report of 12 operative cases. J Trauma
1988;28:1562-1569.
P, Batt ME. Do nonsteroidal anti-inflammatory drugs adversely affect
stress fracture healing? A short review. Br J Sports Med 2005;39:65-69.
GP, Wetzler MJ, Levy AS, et al. A pneumatic leg brace for the treatment
of tibial stress fractures. Clin Orthop Relat Res 1991;270:302-305.
RD, Johns JC. Nonunion of an olecranon stress fracture in an adolescent
gymnast: a case report. Am J Sports Med 1990;18:432-434.
AC, Moore J, Bracker M, et al. Risk factors associated with stress
reactions in female marines. Milit Med 1997;162:698-702.
BM, Yanklowitz BA. The pathophysiology and treatment of stress
fractures in military personnel. J Am Podiatr Med Assoc 1978;68:317-325.
RR, Torg JS, Rachun A. Proximal diaphyseal fractures of the fifth
metatarsal: treatment of the fractures and their complications in
athletes. Am J Sports Med 1979; 7:95-101.
TS, Elkanovitch R, Frank G. Interpretation and classification of bone
scintigraphic findings in stress fractures. J Nucl Med 1987;28:452-457.
