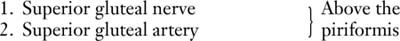
The Hip
surgical procedures performed in orthopaedics. Total joint replacement
for degenerative joint disease has revolutionized the lives of millions
of patients. Open approaches to the hip joint are also required for
hemiarthroplasties, tumor surgery, and for the treatment of infection
around the hip joint.
the most common approach for total hip replacement, has many variations
because of the different requirements of the several prosthetic designs
that can be inserted. The standard anterolateral approach is described;
readers are advised to consult the original papers of the designers of
the arthroplasty before performing a particular joint replacement. The posterior approach,
which is used extensively for hemiarthroplasty as well as for total hip
joint replacement, is probably the most common approach performed
around the hip joint. It is both safe and easy to perform with only one
assistant. The medial approach is rarely used, and then mainly for local procedures on the lesser trochanter and surrounding bone.
 |
|
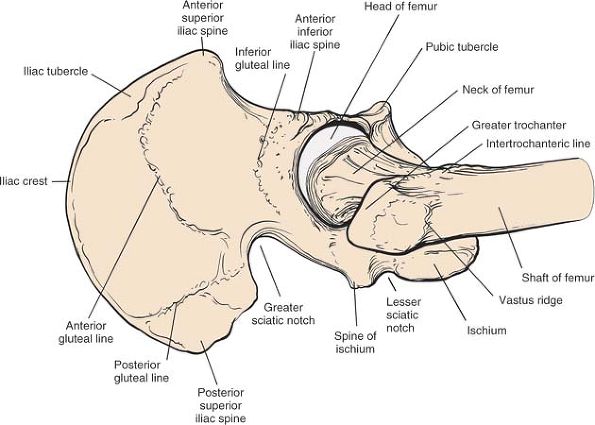
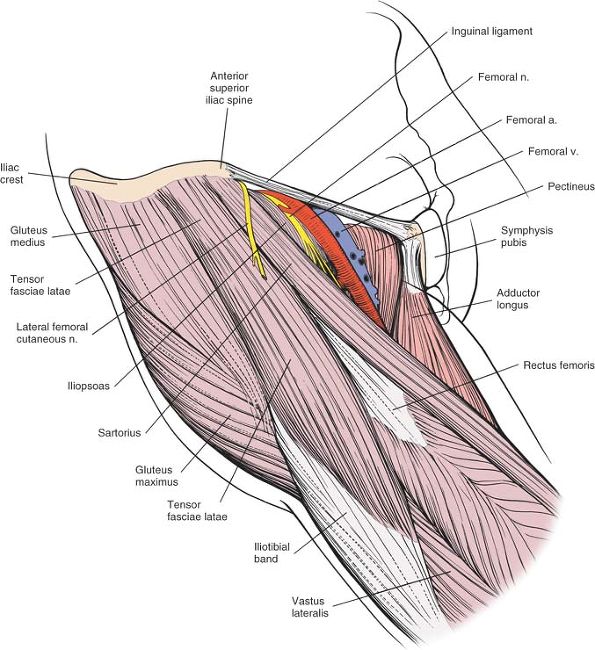
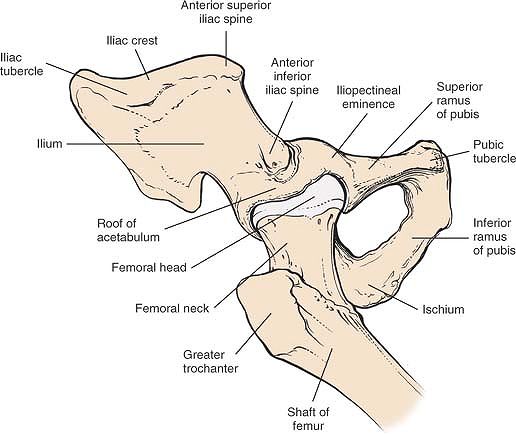
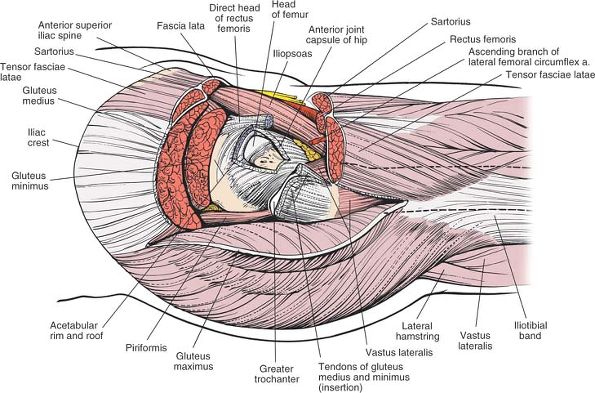
Figure 8-1 The intermuscular intervals used in the anterior, anterolateral, and posterior approaches to the hip.
|
increased in popularity. Most of these techniques utilize the classical
approaches described in this book. The length of the skin incision and
the underlying dissection is reduced. Minimal access surgery can create
less soft-tissue damage, but the visualization of the structures is
necessarily less. The techniques, therefore, are potentially more
hazardous, and an understanding of the underlying anatomy is important.
In addition, imaging may be indicated to ensure correct implant
position.
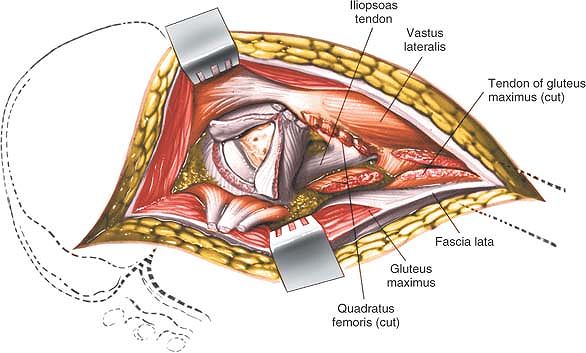
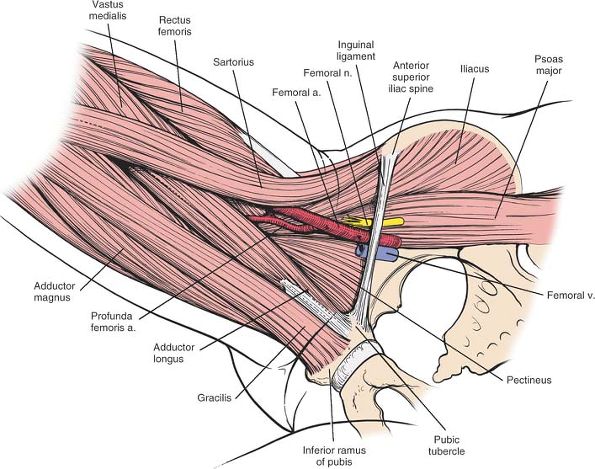
the muscular intervals that surround the joint. The anterior approach
uses the interval between the sartorius and the tensor fasciae latae;
the anterolateral approach uses the interval between the tensor fasciae
latae and the gluteus medius; the posterior approach gains access
either through the interval between the gluteus medius and the gluteus
maximus or by splitting the gluteus maximus; and the medial approach
exploits the interval between the adductor longus and the gracilis (Fig. 8-1).
approaches. Because the anterior and anterolateral approaches share so
much anatomy, they are grouped together. The anatomy for the posterior
and medial approaches follows the appropriate approach.
approach, gives safe access to the hip joint and ilium. It exploits the
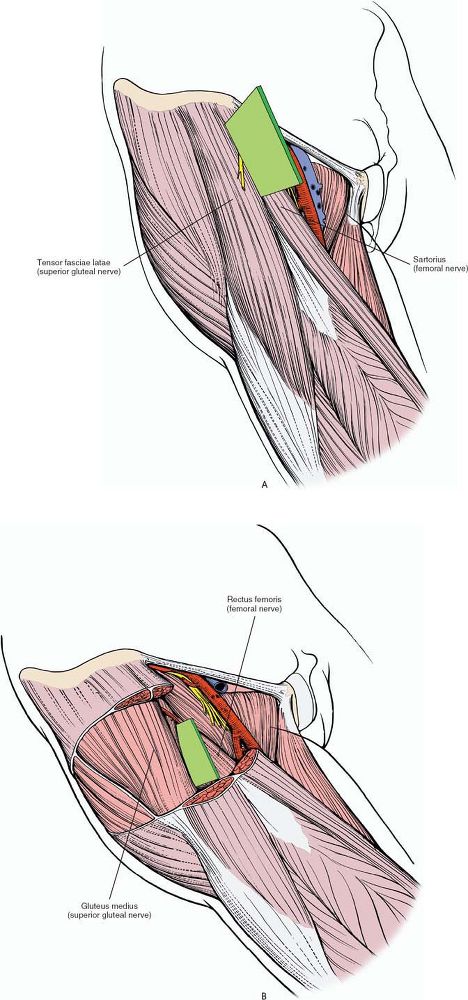
internervous plane between the sartorius (femoral nerve) and the tensor
fasciae latae (superior gluteal nerve) to penetrate the outer layer of
the joint musculature. Its uses include the following:
-
Open reduction of congenital dislocations of the hip when the dislocated femoral head lies anterosuperior to the true acetabulum7
-
Synovial biopsies
-
Intraarticular fusions
-
Total hip replacement
-
Hemiarthroplasty
-
Excision of tumors, especially of the pelvis
-
Pelvic osteotomies
completely as other incisions unless muscles are extensively stripped
off the pelvis.
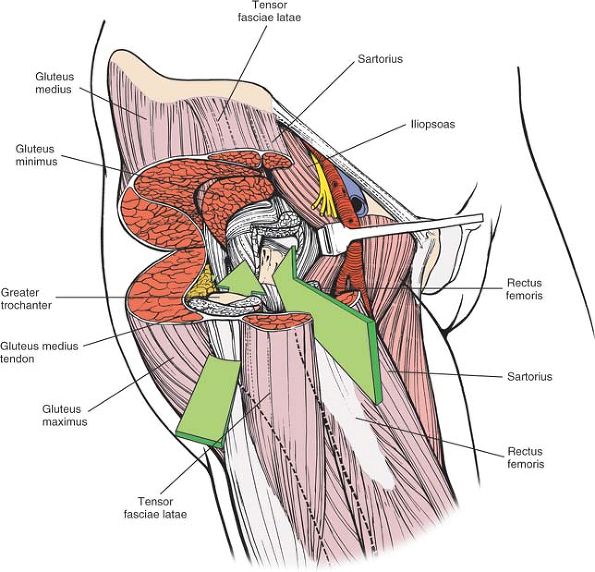
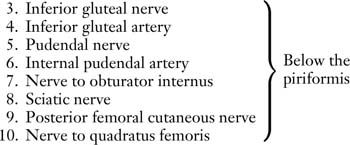
approach is to be used for pelvic osteotomy, place a small sandbag
under the affected buttock to push the affected hemipelvis forward (Fig. 8-2).
is subcutaneous and is easily palpable in thin patients. In obese
patients, it is covered by adipose tissue and is more difficult to
find. You can locate it most easily if you bring your thumbs up from
beneath the bony protuberance.
subcutaneous and serves as a point of origin and insertion for various
muscles. However, none of these muscles cross the bony crest; it
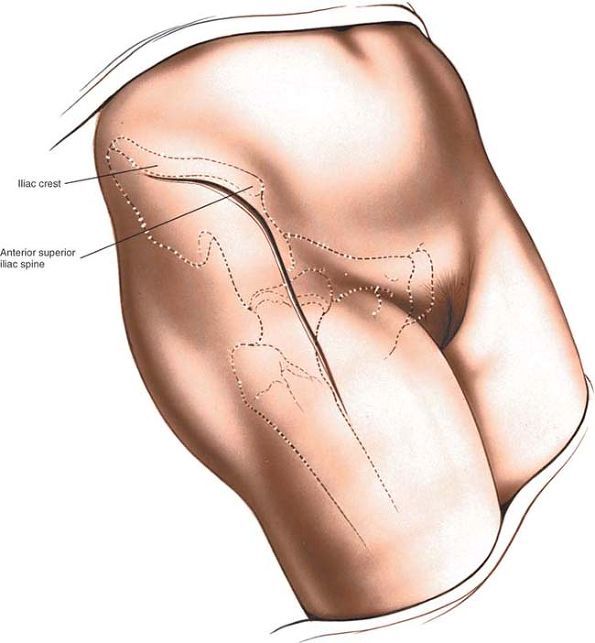
remains available for palpation (Fig. 8-3).
iliac crest to the anterior superior iliac spine. From there, curve the
incision down so that it runs vertically for some 8 to 10 cm, heading
toward the lateral side of the patella (see Fig. 8-3).
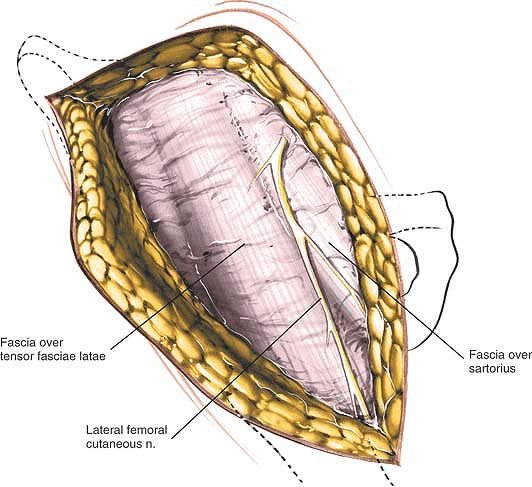
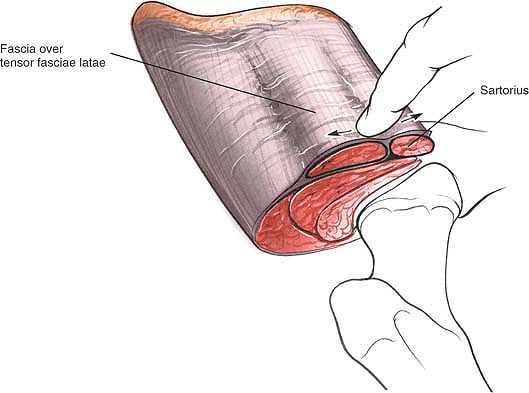
muscle, making it more prominent. Identify the gap between the tensor
fasciae latae and the sartorius by palpation (Fig. 8-6).
The best place to find it is some 2 to 3 inches below the anterior
superior iliac spine, since the fascia that covers both muscles just
below the spine makes the interval difficult to define at its highest
point. With scissors, carefully dissect down through the subcutaneous
fat along the intermuscular
interval.
Avoid cutting the lateral femoral cutaneous nerve (lateral cutaneous
nerve of the thigh), which pierces the deep fascia of the thigh close
to the intermuscular interval (Fig. 8-5).
 |
|
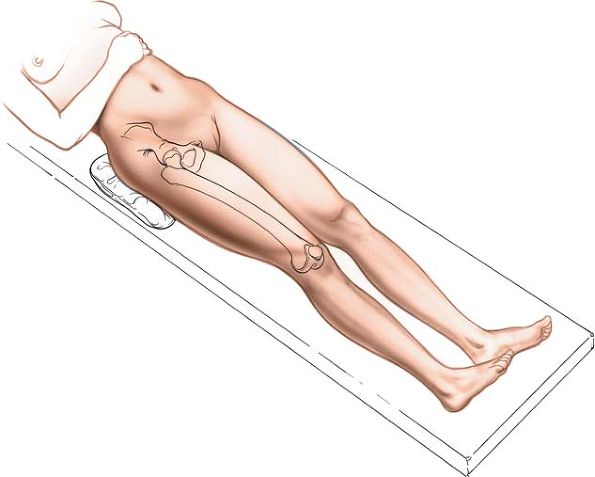
Figure 8-2 Position of the patient on the operating table for the anterior approach to the hip.
|
 |
|
Figure 8-3
Make a longitudinal incision along the anterior half of the iliac crest to the anterior superior iliac spine. From there, curve the incision down so that it runs vertically for some 8 to 10 cm. |
 |
|
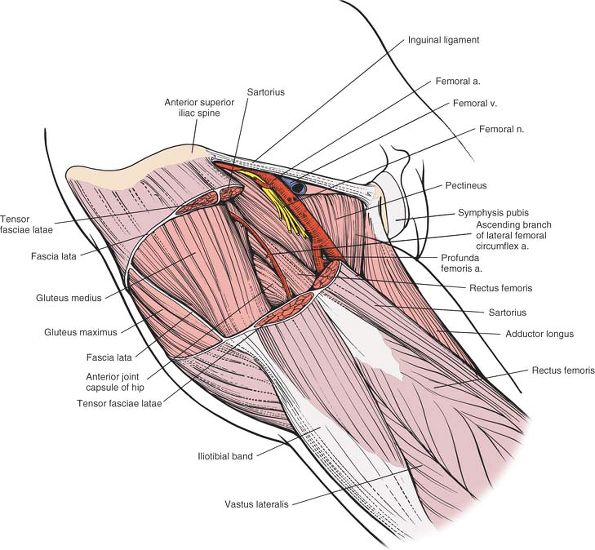
Figure 8-4 (A) The internervous plane lies between the sartorius (femoral nerve) and the tensor fasciae latae (superior gluteal nerve). (B) The deeper internervous plane lies between the rectus femoris (femoral nerve) and the gluteus medius (superior gluteal nerve).
|
fascia latae. Staying within the fascial sheath of this muscle will
protect you from damaging the lateral femoral cutaneous nerve because
the nerve runs over the fascia of the sartorius. Retract the sartorius
upward and medially and the tensor fascia latae downward and laterally (Fig. 8-7).
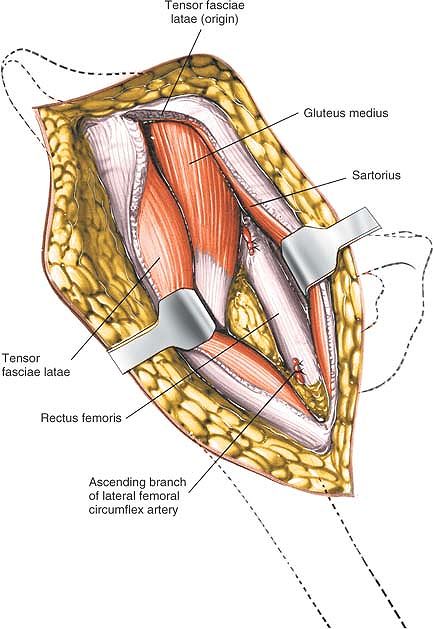
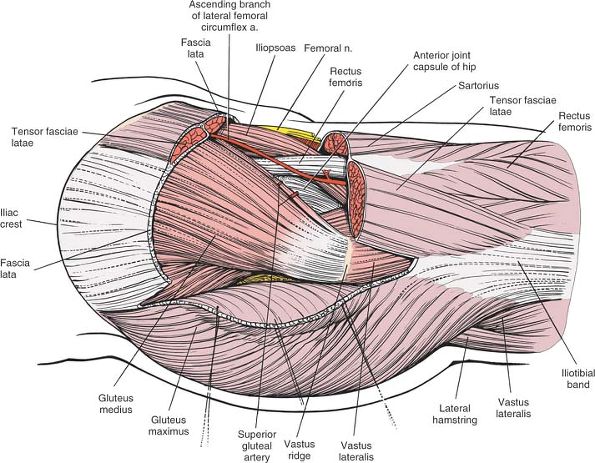
develop the internervous plane. The large ascending branch of the
lateral femoral circumflex artery crosses the gap between the two
muscles below the anterior superior iliac spine. It must be ligated or
coagulated.
brings you on to two muscles of the deep layer of the hip musculature,
the rectus femoris (femoral nerve)
and the gluteus medius (superior gluteal nerve) (Fig. 8-8).
 |
|
Figure 8-5
The lateral femoral cutaneous nerve (lateral cutaneous nerve of the thigh) pierces the deep fascia close to the intermuscular interval between the tensor fasciae latae and the sartorius. |
 |
|
Figure 8-6 Identify the gap between the tensor fasciae latae and the sartorius by palpation.
|
 |
|
Figure 8-7
Incise the deep fascia on the medial side of the tensor fasciae latae. Retract the sartorius upward and medially and the tensor fascia downward and laterally. |
head, from the anterior inferior iliac spine, and the reflected head,
from the superior lip of the acetabulum. The reflected head also takes
origin from the anterior capsule of the hip joint. It is intimate with
the capsule, making dissection between the two structures difficult.
rectus femoris and the gluteus medius, palpate the femoral artery. The
femoral pulse is well medial to the intermuscular interval; if you
dissect near it, you are out of plane. Detach the rectus femoris from
both its origins and retract it medially. Retract the gluteus medius
laterally (Fig. 8-9).
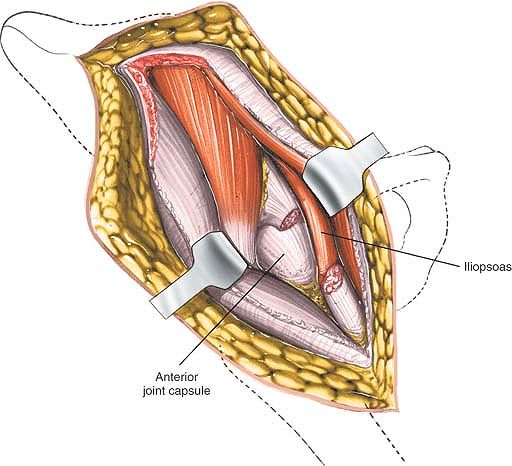
Inferomedially, you can see the iliopsoas as it approaches the lesser
trochanter: Retract it medially (Figs. 8-10 and 8-11).
The iliopsoas is often partly attached to the inferior aspect of the
hip joint capsule and must be released from it. Inferolaterally, the
shaft of the femur lies under cover of the vastus lateralis.
capsule on stretch; define the capsule with blunt dissection. Incise
the hip joint capsule as the surgery requires, with either a
longitudinal or a T-shaped capsular incision (Fig. 8-12). Dislocate the hip by external rotation after the capsulotomy.
reaches the thigh by passing over, behind, or through—usually over—the
sartorius muscle, about 2½ cm below the anterior superior iliac spine.
The nerve must be preserved when you incise the fascia between the
sartorius and the tensor fasciae latae; cutting it may lead to the
formation of a painful neuroma and may produce an area of diminished
sensation on the lateral aspect of the thigh (Fig. 8-14; see Fig. 8-5).
the nerve is well medial to the rectus femoris, it is not really in
danger unless you stray far out of plane to the wrong side of the
sartorius and the rectus femoris. If you lose the correct plane during
deep dissection, locate the femoral pulse by palpation. Within the
femoral triangle, the artery lies medial to the nerve (Figs. 8-15 and 8-16).
 |
|
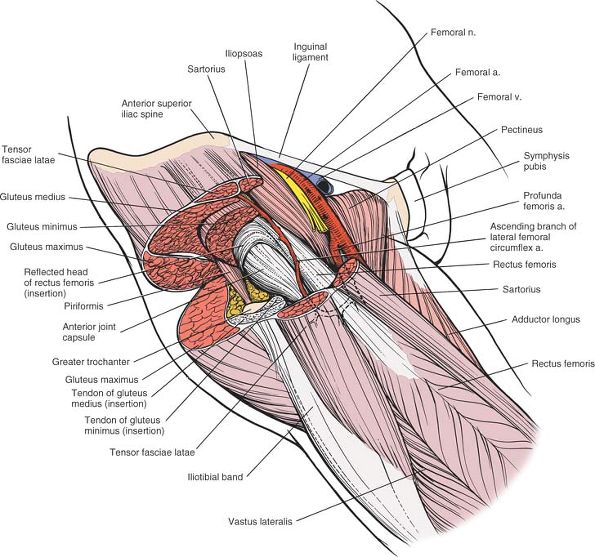
Figure 8-8
The deep layer of musculature, consisting of the rectus femoris and the gluteus medius, is now visible. The ascending branch of the lateral femoral circumflex artery must be ligated. |
 |
|
Figure 8-9 Detach the rectus femoris from both its origins, the anterior inferior iliac spine and the superior lip of the acetabulum.
|
 |
|
Figure 8-10 The hip joint capsule is now partly exposed. Retract the iliopsoas tendon medially.
|
 |
|
Figure 8-11 The hip joint capsule is fully exposed. Detach the muscles of the ilium if further exposure is needed.
|
 |
|
Figure 8-12 Incise the hip joint capsule.
|
 |
|
Figure 8-13
Proximal extension of the wound exposes the ilium. Distal extension of the incision exposes the anterior aspect of the femur in the interval between the vastus lateralis and the rectus femoris. It may be necessary to split muscle fibers to actually expose the lateral aspect of the femur. |
 |
|
Figure 8-14 Superficial view of the muscles of the anterior region of the hip, including the femoral triangle and its contents.
Sartorius. Origin. Anterior superior iliac spine and upper half of iliac notch. Insertion. Upper end of subcutaneous surface of tibia. Action. Flexor of thigh and knee and external rotator of hip. Nerve supply. Femoral nerve (L2-L4).
Tensor Fasciae Latae. Origin. From outer aspect of iliac crest between the anterior superior iliac spine and the tubercle of the iliac crest. Insertion. By iliotibial tract into Gerdy’s tubercle of the tibia. Action. Maintains stability of extended knee and extended hip. Nerve supply. Superior gluteal nerve.
|
 |
|
Figure 8-15
The tensor fasciae latae, the sartorius, and the fascia lata have been resected on the anterior aspect of the hip to reveal the gluteus medius, the rectus femoris, and the ascending branch of the lateral femoral circumflex artery. The hip joint capsule is visible between these two muscles. Medially, note the relationship between the iliopsoas and the rectus femoris. |
Ligate or coagulate it when you separate the two muscles (see Figs. 8-8, 8-15, 8-16, 8-17, and 8-18).
 |
|
Figure 8-16
The gluteus minimus, medius, and maximus have been resected to reveal the hip joint capsule and the reflected head of the rectus femoris. |
Detach the origins of the gluteus medius and minimus from the outer
wing of the ilium by blunt dissection. (This procedure is always
necessary during pelvic osteotomies.) Bleeding from the raw exposed
surface of the ilium can be controlled if you pack the wound with gauze
sponges. Individual bleeding points can be controlled by the
application of bone wax. There is no other way to stop bleeding.
iliac crest to expose that bone. In theory, the extension allows the
taking of bone graft, but it is rarely used.
incision downward along the anterolateral aspect of the thigh. Incise
the fascia lata in line with the skin incision; underneath it lies the
interval between the vastus lateralis and the rectus femoris. Try to
stay in the interval; you will have to split muscle fibers to expose
the anterior aspect of the femur. This extension gives excellent
exposure of the entire shaft of the femur (see Fig. 8-13).
the level of the hip joint to allow pelvis osteotomy. To obtain
visualization of the outer part of the ilium, gently strip the muscular
coverings from the bone at the level of the origin of the reflected
head of rectus. Using blunt instruments stay in contact with bone. This
dissection will lead you into the sciatic notch. Take great care that
any instrument inserted into the notch remains firmly on the bone,
since the sciatic nerve is also emerging through the notch. Detach the
straight head of the rectus femoris from the anterior inferior iliac
spine, and carefully lift off the iliacus muscle from the inside of the
pelvis, again sticking very carefully to the bone. A blunt instrument
will gradually lead you into the greater sciatic notch. At this stage,
both instruments should be in contact with each other and with the bone
of the sciatic notch. Retraction on both instruments will allow
visualization of the entire thickness of the pelvis at the level of the
top of the acetabulum, permitting an accurate osteotomy to be carried
out.
 |
|
Figure 8-17
The iliopsoas tendon has been retracted medially; the rectus femoris has been resected and the joint capsule opened to reveal the joint. |
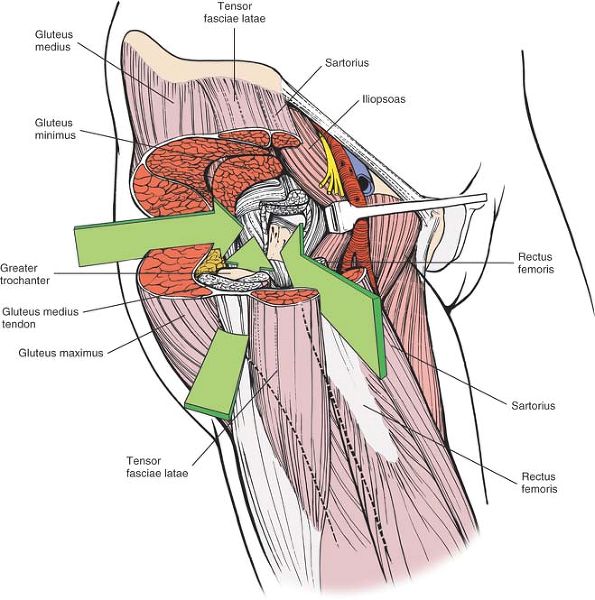
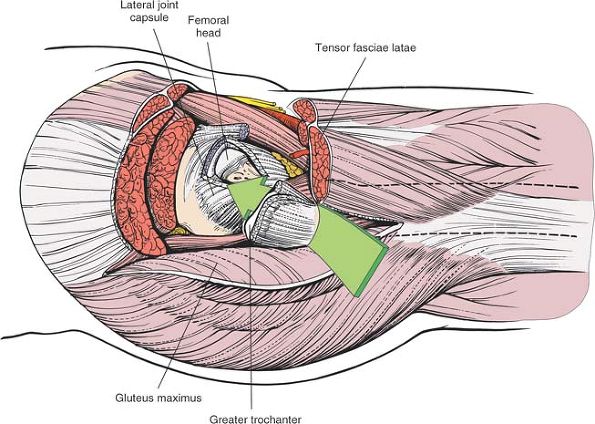
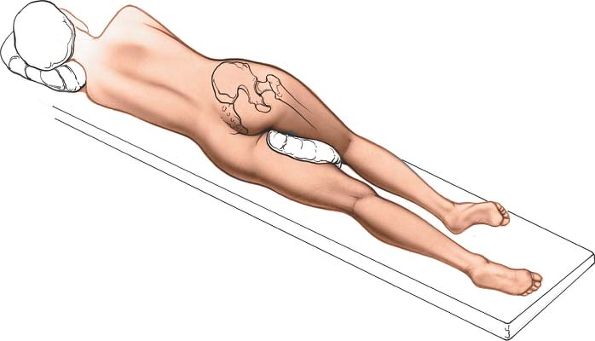
used for total joint replacements. It combines an excellent exposure of
the acetabulum with safety during reaming of the femoral shaft.
Popularized by Watson-Jones (D. Hirsh, personal communication, 1981)
and modified by Charnley,8 Harris,9 and Müller,10
it exploits the intermuscular plane between the tensor fasciae latae
and the gluteus medius. It also involves partial or complete detachment
of some or all of the abductor mechanism so that the hip can be
adducted during reaming of the femoral shaft and so that the acetabulum
can be more fully exposed (Fig. 8-19).
The two methods seem to offer different approaches, but they are
actually variations on a theme. The differences should not obscure the
fundamental fact that all anterolateral approaches exploit the same
intermuscular plane, between the tensor fasciae latae and the gluteus
medius.
 |
|
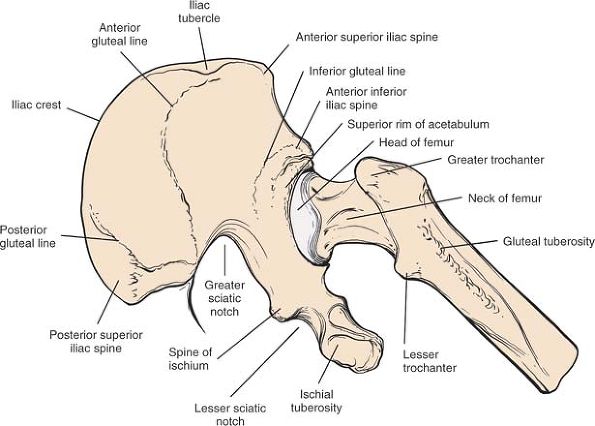
Figure 8-18 Osteology of the hip.
|
-
Total hip replacement10,11
-
Hemiarthroplasty
-
Open reduction and internal fixation of femoral neck fractures
-
Synovial biopsy of the hip
-
Biopsy of the femoral neck
Tilt the table away from you as the patient lies flat. Both maneuvers
allow the buttock skin and fat to fall posteriorly, away from the
operative plane, and lift the skin incision clear of the table, making
it easier to drape the patient. You must take this into account when
you insert the acetabular portion of a total joint replacement because
the guides used to position the acetabular prosthesis usually take the
ground as their reference plane.
 |
|
Figure 8-19 The route of the anterolateral approach to the hip joint.
|
 |
|
Figure 8-20
Position of the patient on the operating table for the anterolateral approach to the hip. Bring the greater trochanter to the edge of the table, and allow the buttocks, skin, and fat to fall posteriorly, away from the operative plane. |
 |
|
Figure 8-21 Incision for the anterolateral approach to the hip.
|
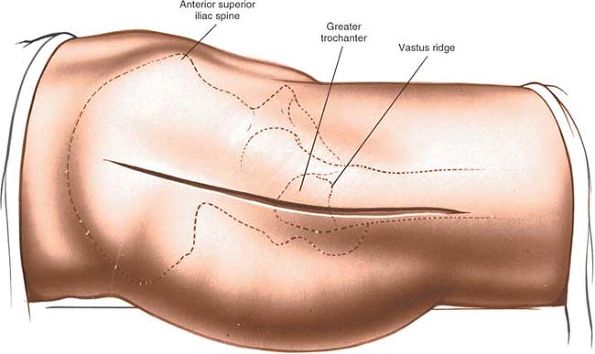
is subcutaneous. It is easy to palpate in all but the most obese
patients, who have a thick layer of adipose tissue covering it. To
palpate it, bring your thumbs up from beneath the bony protuberance.
a rough line that marks the fusion site of the greater trochanter to
the lateral surface of the shaft of the femur, is easiest to palpate
from distal to proximal. It is not palpable in obese patients.
lying across the opposite knee both to bring the trochanter into
greater relief and to move the tensor fasciae latae anteriorly. Make an
8- to 15-cm straight longitudinal incision centered on the tip of the
greater trochanter. The length of the incision relates to the size and
obesity of the patient as well as the surgeon’s experience. The
incision crosses the posterior third of the trochanter before running
down the shaft of the femur (see Fig. 8-21).
since the gluteus medius and the tensor fasciae latae have a common
nerve supply, the superior gluteal nerve. However, the superior gluteal
nerve enters the tensor fasciae latae very close to its origin at the
iliac crest; therefore, the nerve remains intact as long as the plane
between the gluteus medius and the tensor fasciae latae is not
developed up to the origins of both muscles from the ilium (see Fig. 8-19).
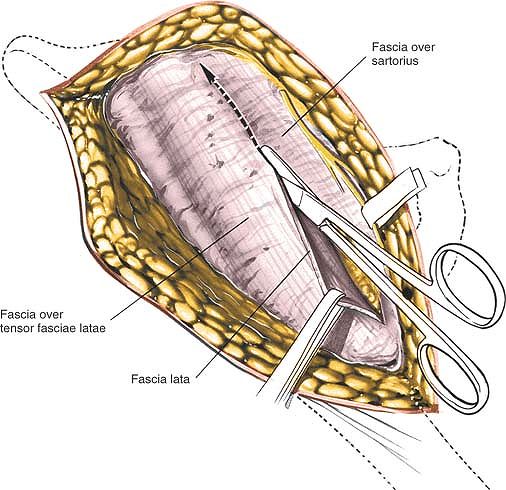
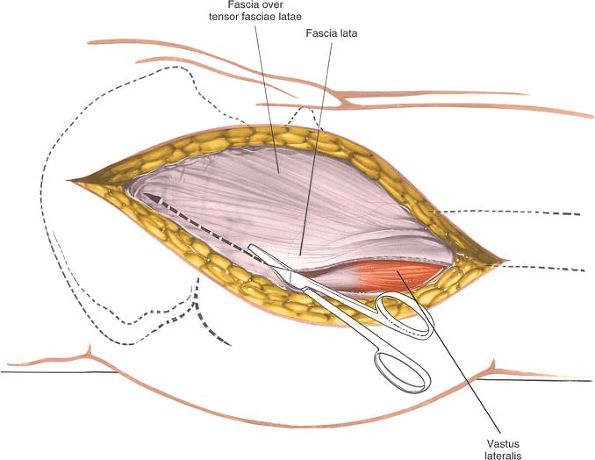
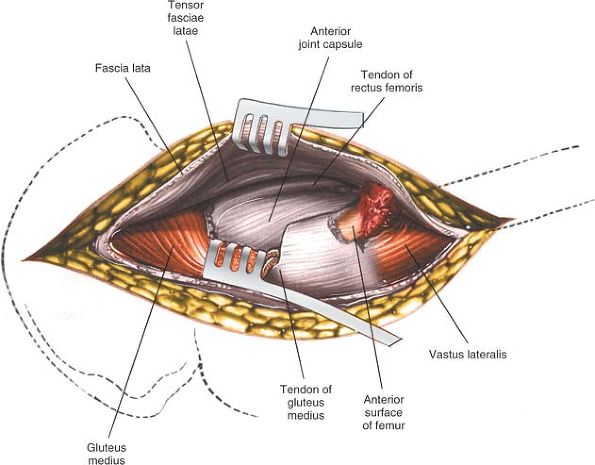
the deep fascia of the thigh. Using a sponge, gently push back
subcutaneous fat off the fascia lata until you can reach the fascia at
the posterior margin of the greater trochanter. Incise the fascia lata
at this point, entering the bursa that underlies it (Fig. 8-22). Now, divide the fascia lata in the line of its fibers superiorly, heading
proximally and anteriorly in the direction of the anterior superior
iliac spine. Finally, complete the fascial incision by extending the
cut distally and slightly anteriorly to expose the underlying vastus
lateralis muscle. Elevate this flap anteriorly by getting your
assistant to retract it forward, using a tissue-holding forcep. Now,
detach the few fibers of gluteus medius that arise from the deep
surface of this fascial flap and locate the interval between the tensor
fasciae latae (which is being lifted anteriorly by the assistant) and
the gluteus medius. This is best done by blunt dissection using your
fingers. A series of vessels cross the interval between the tensor
fasciae latae and the gluteus medius. These act as a guide to the
interval, but require ligation (Fig. 8-23).
 |
|
Figure 8-22 Incise the fascia lata posterior to the tensor fasciae latae.
|
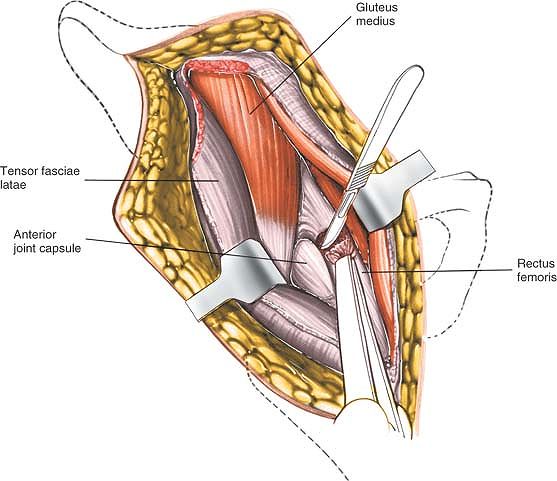
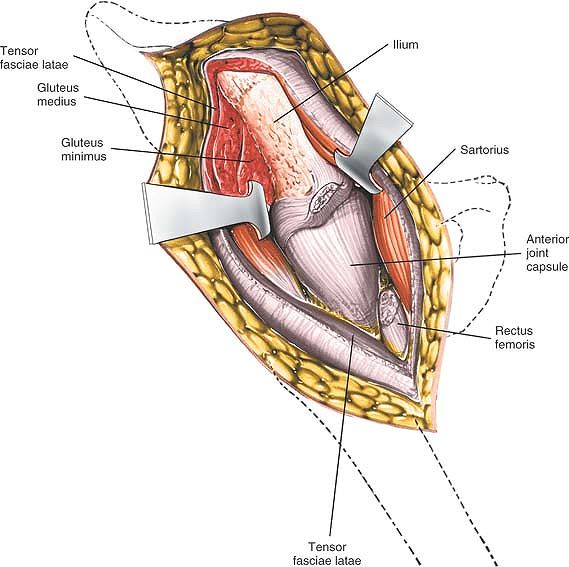
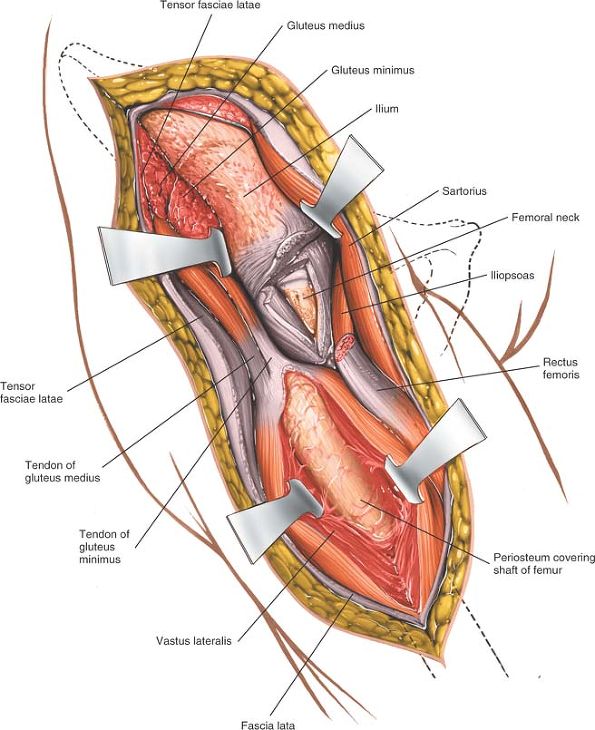
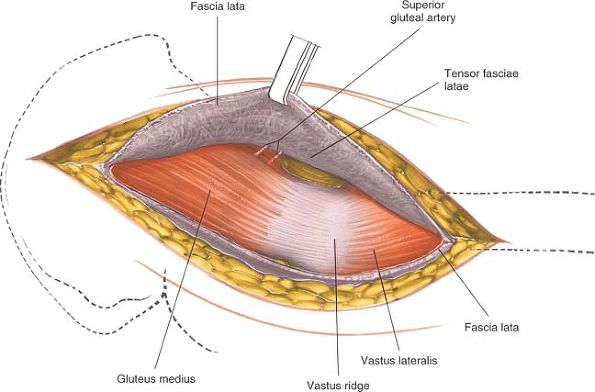
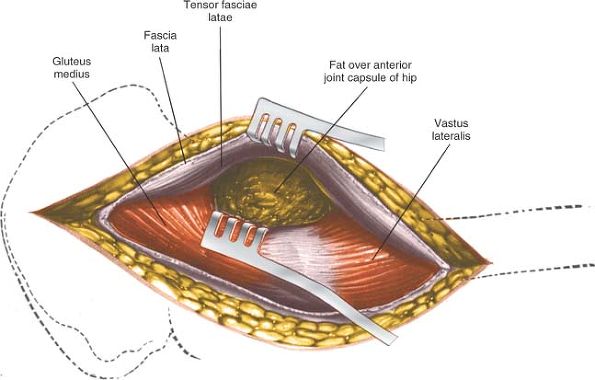
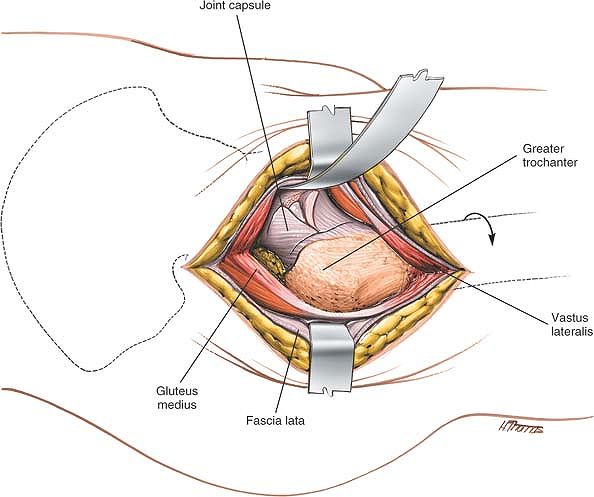
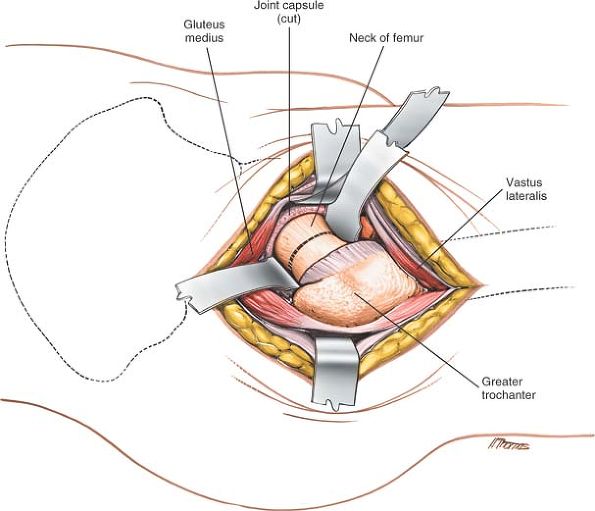
medius and minimus, and retract these muscles proximally and laterally
away from the superior margin of the joint capsule that covers the
femoral neck (Fig. 8-24).
stretch. Identify the origin of the vastus lateralis at the vastus
lateralis ridge. Incise the origin using a cautery knife, and reflect
the muscle inferiorly for about 1 cm. Under it is the anterior aspect
of the joint capsule, at the junction of the femoral neck and shaft.
Bluntly dissect up the anterior part of the joint capsule, lifting off
the fat pad that covers it. The fat pad can reduce postoperative
scarring and adhesions and should be preserved even though it intrudes
into the operative field (Fig. 8-25).
all of the abductor mechanism and then dissecting up the femoral neck
superficial to the capsule of the joint until a suitable retractor can
be placed over the anterior lip of the acetabulum.
neutralizing the abductor mechanism, allowing the femur to fall
posteriorly. They also permit adduction of the leg for safe femoral
reaming and accurate positioning of prosthetic stems within the femoral
shaft. The technique chosen depends on the prosthesis to be used.
 |
|
Figure 8-23
Retract the fascia lata and the tensor fasciae latae muscle, which it envelopes, anteriorly, revealing the gluteus medius and a series of vessels that cross the interval between the tensor fasciae latae and the gluteus medius. |
 |
|
Figure 8-24
Retract the gluteus medius posteriorly and the tensor fasciae latae anteriorly, uncovering the fatty layer directly over the joint capsule. |
 |
|
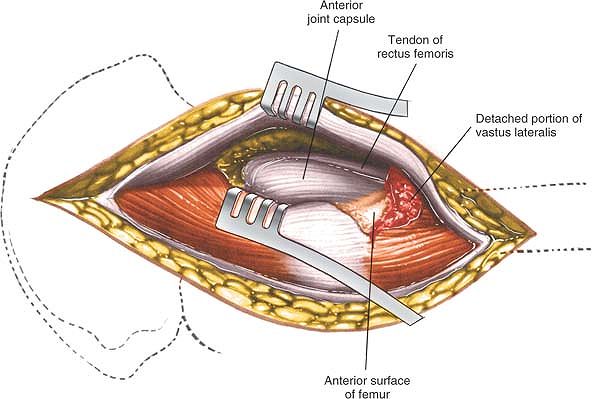
Figure 8-25 Bluntly dissect the fat pad off the anterior portion of the joint capsule to expose it and the rectus femoris tendon.
|
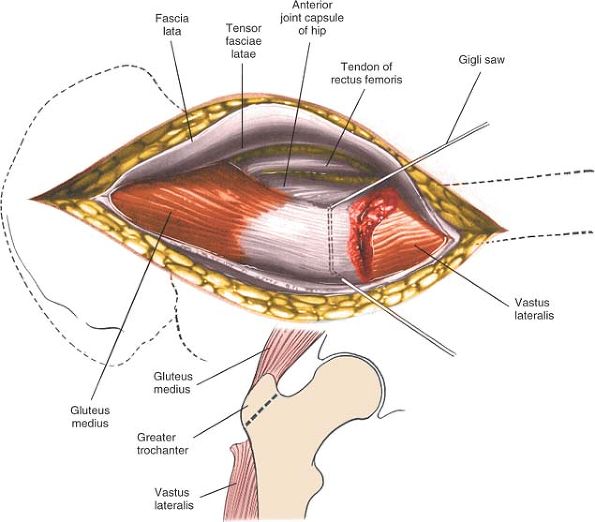
-
Trochanteric osteotomy.
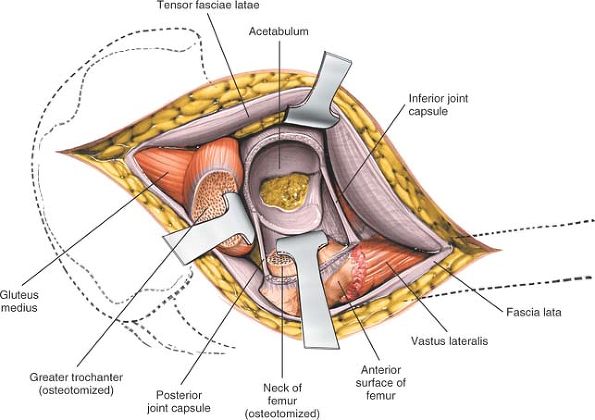
Performing a trochanteric osteotomy allows complete mobilization of the
gluteus medius and minimus muscles, which in turn allows excellent
exposure of the shaft of the femur during femoral reaming. Palpate the
vastus lateralis ridge on the lateral border of the femur, from distal
to proximal. Osteotomize the trochanter, using either an oscillating
saw or a Gigli saw, and reflect it upward with the attached gluteus
medius and minimus muscles. The base of the osteotomy should be at the
base of the vastus lateralis ridge. The upper end of the osteotomy may
be either intracapsular or extracapsular; the thickness of the
osteotomized portion of bone varies considerably, depending on the
prosthesis you intend to use. Alternatively, detach the trochanter
using two cuts at right angles to one another. This will leave the
trochanter looking like the roof of a Swiss chalet. This technique
maximizes the bone-to-bone contact surface area and, because of its
shape, also is inherently more stable after fixation than a straight
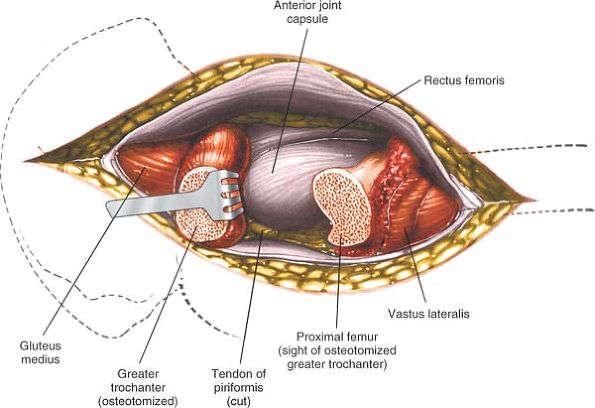
osteotomy.Reflect the osteotomized trochanter upward. To free it
completely, release some soft tissues (including the tendon of the
piriformis muscle) from its posterior aspect (Figs. 8-26 and 8-27). -
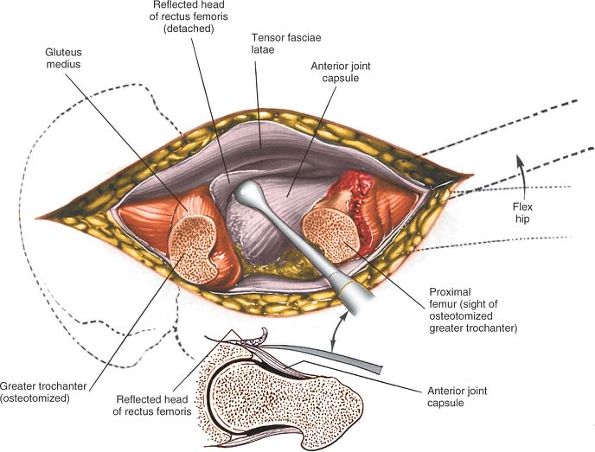
Partial detachment of the abductor mechanism.
Place a stay suture in the anterior portion of the gluteus medius just
above its insertion into the greater trochanter. Cut the insertion of
this anterior portion off the trochanter. Identify the thick white
tendon of the gluteus minimus as it inserts onto the anterior aspect of
the trochanter and incise it. The exact amount of the gluteus medius
that must be detached varies considerably from case to case (Fig. 8-28). In thin, nonmuscular people, you may even be able to preserve the whole of the gluteus medius attachment.
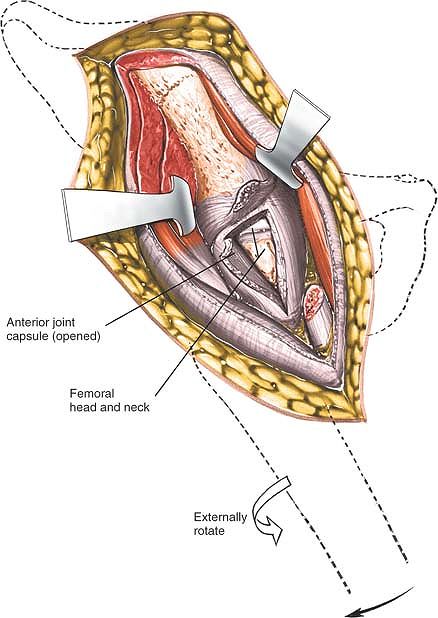
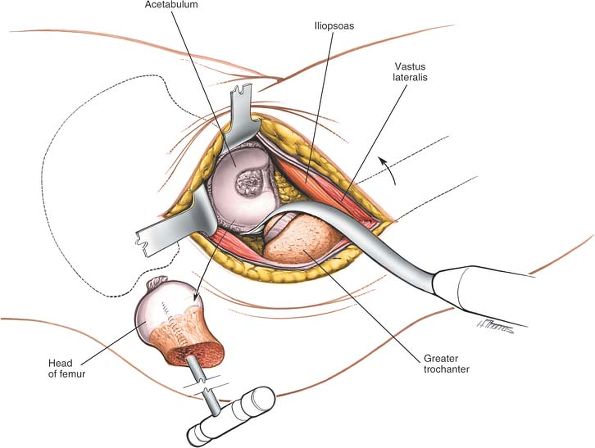
capsule in line with the femoral neck and head. Detach the reflected
head of the rectus femoris from the joint capsule to expose the
anterior rim of the acetabulum (Fig. 8-29, and inset).
(This plane is easier to open up if the leg is partly flexed, since the
rectus femoris remains relaxed. Flexing the leg also keeps the femoral
nerves and vessels off the stretch and farther from the operative
field.) Elevate part of the psoas tendon from the capsule. Because both
the rectus femoris and the psoas may insert into the capsule, the plane
between muscle and capsule is often difficult to establish.
acetabulum. Make certain that the dissection and the insertion of
retractors remain beneath the rectus femoris and iliopsoas, because the
neurovascular bundle lies anterior to the psoas. If you cannot develop
a plane between the psoas and the capsule, incise the capsule and
insert a retractor around the femoral head so that you can see the
joint better.
 |
|
Figure 8-26 Osteotomize the greater trochanter.
|
 |
|
Figure 8-27 Reflect the osteotomized portion of the trochanter superiorly (with the attached gluteus medius) to reveal the joint capsule.
|
 |
|
Figure 8-28
The joint capsule may also be exposed by partial resection of the gluteus medius tendon from the anterior portion of the trochanter. |
 |
|
Figure 8-29 Reflect the head of the rectus femoris from the anterior portion of the joint capsule.
|
 |
|
Figure 8-30
Incise the anterior joint capsule to reveal the femoral head and neck and the acetabular rim. If further proximal exposure is needed, incise the fascia lata proximally toward the iliac crest and along the iliac crest anteriorly. To facilitate dislocation of the hip, incise the tight fascia lata and the fibers of the gluteus maximus (inset). |
longitudinal incision. Develop this into a T-shaped incision by cutting
the attachment of the capsule to the acetabulum as far around as you
can reach. Now incise the capsule transversely at the base of the neck
to convert the T-shaped incision into an H-shaped one (Fig. 8-30, and inset). Dislocate the hip by externally rotating it after you have performed an adequate capsulotomy (Fig. 8-31).
most laterally placed structure in the neurovascular bundle in the
femoral triangle, thus the structure closest to the operative field and
most at risk. The most common problem is compression neurapraxia,
caused by overexuberant medial retraction of the anterior covering
structures of the hip joint. Less frequently, the nerve is directly
injured by retractors placed in the substance of the iliopsoas (see Figs. 8-41 and 8-42).
may be damaged by incorrectly placed acetabular retractors that
penetrate the iliopsoas, piercing the vessels as they lie on the
surface of the muscle. You can avoid this complication by making sure
that the tip of the retractor is placed firmly on bone, with no
intervening tissue. The anterior retractor should be placed in the
1-o’clock position for the right hip and in the 11-o’clock position for
the left hip. Finding the correct plane between the rectus femoris and
the anterior part of the hip joint capsule is easier if the limb is in
about 30° of flexion.
 |
|
Figure 8-31
To expose the acetabulum, dislocate and resect the femoral head. Placing three or four Homan-type retractors around the lip of the acetabulum provides excellent exposure. |
are being dislocated. For that reason, it is critical that you do an
adequate capsular release before attempting dislocation. To dislocate
the joint, lever the femoral head out of the acetabulum with a skid
(such as a Watson-Jones) while your assistant gently externally rotates
the limb. Your assistant has a considerable lever arm during this
procedure—if rotating the leg too forcibly, a spiral fracture of the
femur can result.
osteotomize the rim of the acetabulum, which often has an osteophyte,
to achieve dislocation.
extreme force, it is safer to perform a double osteotomy of the femoral
neck, excising a 1-cm portion of it: then remove the femoral head
(which is lying free) with a corkscrew.
limb is placed in full adduction and external rotation for reaming of
this femoral shaft. In order for the operator to gain a good enough
view of the cut surface of the femur, the femoral shaft must be
adducted. If the incision in the fascia lata has been placed too far
anteriorly, then the fascia lata will resist adduction and enthusiastic
assistants may cause femoral shaft fracture. This is the reason why the
fascia lata should be incised initially at the posterior border of the
greater trochanter. If the fascia lata gets in your way when attempting
to adduct the leg, it is safest to incise it along the lines of fibers
of gluteus maximus (see Fig. 8-30).
your superficial dissection, may prevent the adduction of the leg and
complete dislocation of the hip needed for femoral reaming because it
impinges on the trochanter. If it does, make an incision into the
posterior flap of the tensor fasciae latae, heading obliquely upward
and backward in line with the fibers of the gluteus maximus, which also
inserts into the iliotibial tract (see Fig. 8-30).
This maneuver may also be necessary to achieve reduction of the
prosthetic hip when the leg has been lengthened by the operative
procedure.
fascia on the muscle’s anterior aspect close to its origin from the ilium (see Fig. 8-30).
Alternatively, continue the fascial incision farther down the lateral
aspect of the femoral shaft. These maneuvers are seldom necessary.
 |
|
Figure 8-32
Extend the incision down the lateral aspect of the thigh, incising the deep fascia and splitting the vastus lateralis in line with its musculature to reach the lateral aspect of the femur. |
correctly placing the retractors. Different approaches use different
retractors, but three or four Homan-type retractors placed around the
lip of the acetabulum, directly on bone, give as good an exposure as
any (see Fig. 8-31).
thigh, and incise the deep fascia in line with the skin incision. Split
the vastus lateralis to gain access to the lateral aspect of the femur.
In this way, you can usefully extend the approach to include the entire
length of the femur. Distal extension is often needed when the approach
is used for open reduction and internal fixation of fractures of the
femoral neck (Fig. 8-32).
allows excellent exposure of the hip joint for joint replacement. It
avoids the need for trochanteric osteotomy. Because the bulk of the
gluteus medius muscle is preserved intact, it permits early
mobilization of the patient following surgery. However, the approach
does not give as wide an exposure as the anterolateral approach with
trochanteric osteotomy. It is, therefore, difficult to perform revision
surgery using this approach.
 |
|
Figure 8-33 Make a longitudinal incision centered over the tip of the greater trochanter in the line of the femoral shaft.
|
greater trochanter at the edge of the table. This allows the buttock
muscles and gluteal fat to fall posteriorly away from the operative
plane (see Fig. 8-20).
below. Palpate the lateral aspect of the greater trochanter and, below
that, the line of the femur that feels like a resistance against the
examining hand.
trochanter. Make a longitudinal incision that passes over the center of
the tip of the greater trochanter and extends down the line of the
shaft of the femur for approximately 8 cm (Fig. 8-33).
gluteus medius muscle are split in their own line distal to the point
where the superior gluteal nerve supplies the muscle. The vastus
lateralis muscle is also split in its own line lateral to the point
where it is supplied by the femoral nerve.
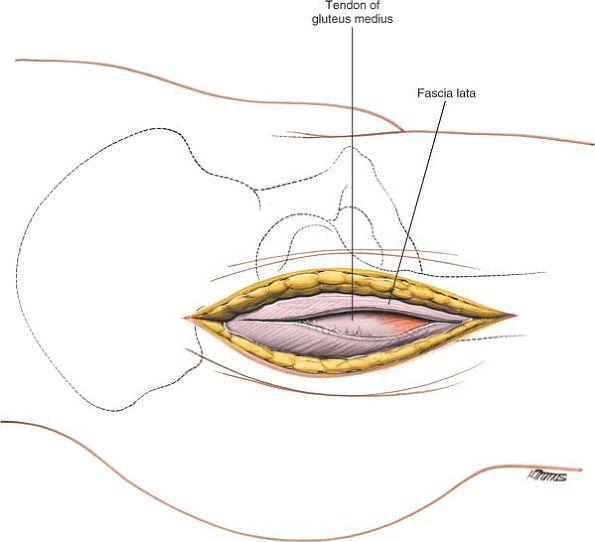
the skin incision. Retract the cut edges of the fascia to pull the
tensor fasciae latae anteriorly and the gluteus maximus posteriorly.
Detach any fibers of the gluteus medius that attach to the deep surface
of this fascia by sharp dissection. The vastus lateralis and the
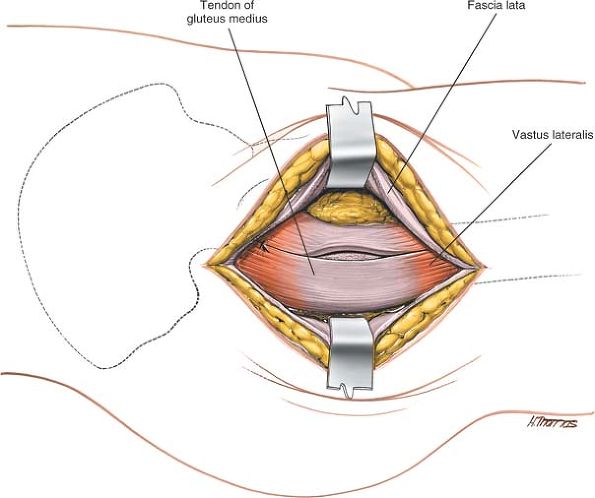
gluteus medius are now exposed (Fig. 8-34).
the trochanter. Do not go more than 3 cm above the upper border of the
trochanter because more proximal dissection may damage branches of the
superior gluteal nerve. Split the fibers of the vastus lateralis muscle
overlying the lateral aspect of the base of the greater trochanter.
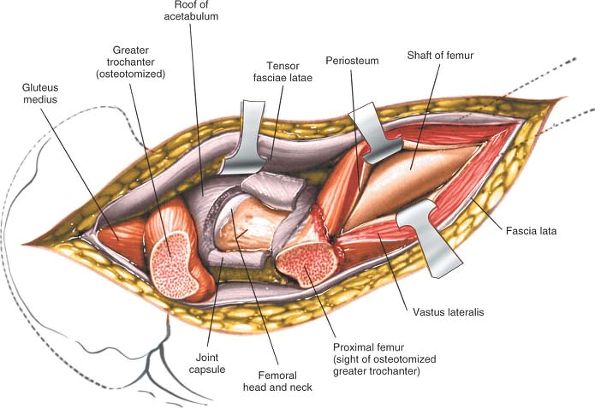
Next, develop an anterior flap that consists of the anterior part of
the gluteus medius muscle with its underlying gluteus minimus and the
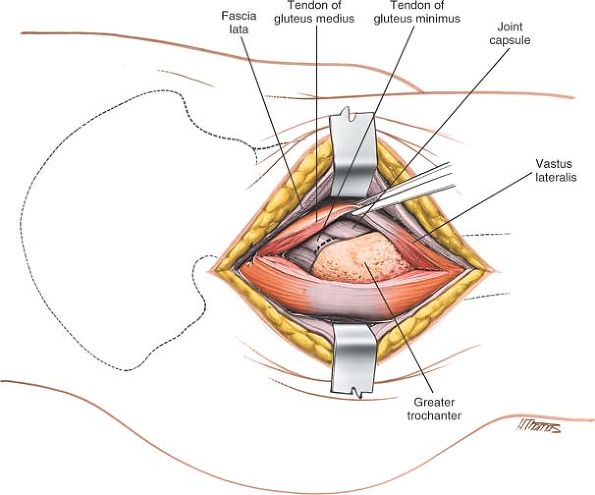
anterior part of the vastus lateralis muscle (Fig. 8-35).
You will need to detach the muscles from the greater trochanter either
by sharp dissection or by lifting off a small flake of bone. Continue
developing this anterior flap, following the contour of the bone onto
the femoral neck, until the anterior hip joint capsule is fully
exposed. You will need to detach the insertion of the gluteus minimus
tendon to the anterior part of the greater trochanter (Fig. 8-36).
Develop the plane between the hip joint capsule and the overlying
muscles, using a swab pushed into the potential space using a blunt
instrument.
 |
|
Figure 8-34 Divide the deep fascia in the line of the skin incision, retracting the fascial edges to pull the tensofasciolate anteriorly.
|
 |
|
Figure 8-35
Split the fibers of gluteus medius above the tip of the greater trochanter and extend this incision distally on the lateral aspect of the trochanter until 2 cm of the vastus lateralis is also split. |
Extract the femoral head using a cork screw. Complete the exposure of
the acetabulum by inserting appropriate retractors around the
acetabulum (Fig. 8-39).
runs between the gluteus medius and minimus muscles approximately 3 to
5 cm above the upper border of the greater trochanter. More proximal
dissection may cut this nerve or may produce a traction injury. For
this reason, insert a stay
suture
at the apex of the gluteus medius split. This will ensure that the
split does not inadvertently extend itself during the operation (see Fig. 8-37).
 |
|
Figure 8-36
Develop this anterior flap and divide the tendon of the gluteus minimus muscle to reveal the anterior aspect of the hip joint capsule. |
 |
|
Figure 8-37 Enter the capsule using a longitudinal T-shaped incision.
|
 |
|
Figure 8-38 Osteotomize the femoral neck using an oscillating saw.
|
lateral structure in the anterior neurovascular bundle of the thigh, is
vulnerable to inappropriately placed retractors. Anterior retractors
should be placed strictly on the bone of the anterior aspect of the
acetabulum and should not infringe on the substance of the psoas muscle.
the shaft of the femur, split the vastus lateralis muscle in the
direction of its fibers (see Lateral Approach in Chapter 9). The incision cannot be extended proximally.
 |
|
Figure 8-39 Extract the femoral head. Insert appropriate retractors to reveal the acetabulum.
|
 |
|
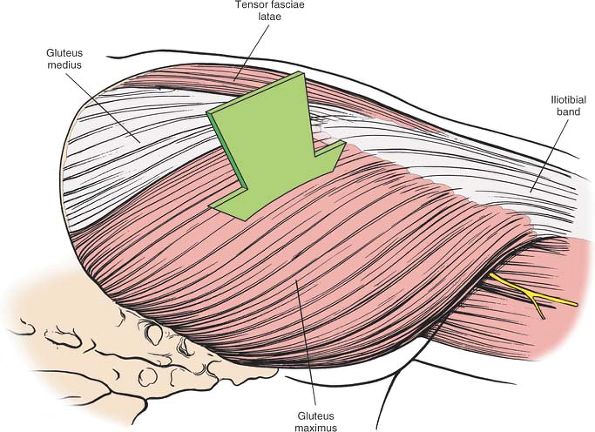
Figure 8-40 Superficial musculature of the lateral aspect of the hip.
|
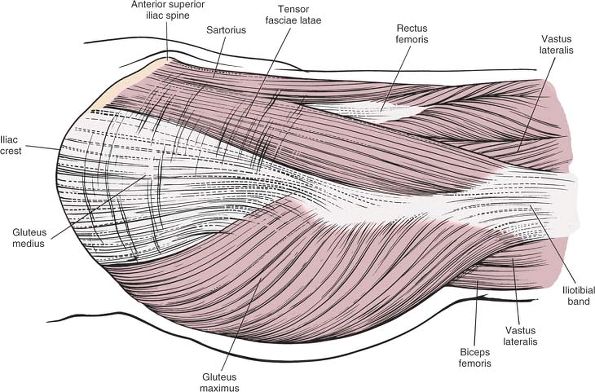
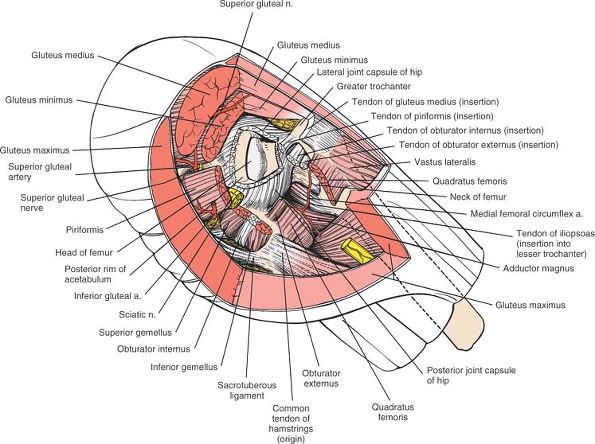
muscles around the hip joint. In hip surgery, its importance lies in
its relationship to three muscles: the sartorius, the tensor fasciae
latae, and the gluteus maximus. The fascia lata covers the sartorius;
it also splits into a deep and superficial layer to enclose the tensor
fasciae latae and gluteus maximus (Fig. 8-40).
If the iliac crest is viewed from the lateral side, the outer layer of
the covering seems to consist of the fascia lata of the thigh and the
muscles that it encloses. The sartorius lies farther anteriorly. The
gluteus medius, which arises from the outer wing of the ilium, is
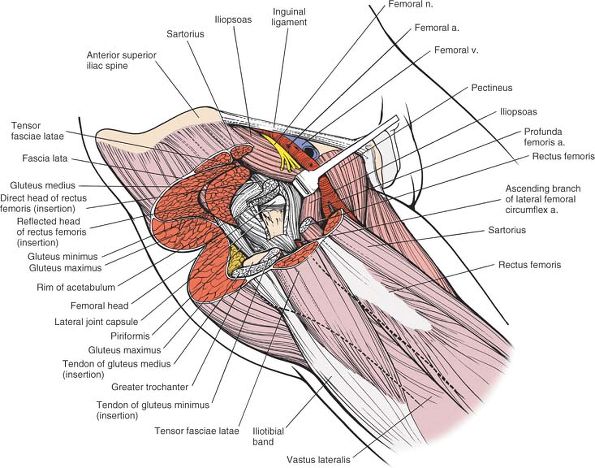
covered by the fascia lata, not enclosed by it (Fig. 8-41).
to the hip lies in the relationship between the tensor fasciae latae
and the gluteus medius. The tensor fasciae latae, a superficial
structure, arises from the anterior portion of the outer lip of the
iliac crest. The gluteus medius arises from the outer wall of the
ilium, between the anterior and posterior gluteal lines. The origins of
the two muscles are, therefore, almost continuous, but the tensor
fasciae latae is slightly more superficial (lateral) and anterior than
the gluteus medius (Fig. 8-42).
tract, the thickening of the deep fascia of the thigh, while the
gluteus medius inserts into the anterior and lateral part of the
greater trochanter. Thus, as the muscles run from origins to
insertions, the tensor fasciae latae rises to an even more superficial
position in relation to the gluteus medius (see Figs. 8-41 and 8-42).
lata posterior to the posterior margin of the tensor fasciae latae and
retract the cut fascial edge anteriorly. Because the fascia lata
actually encloses the tensor fasciae latae, the muscle is retracted
with the fascia (see Fig. 8-41).
 |
|
Figure 8-41
Resecting the sartorius, tensor fasciae latae, and fascia lata and reflecting the anterior portion of the gluteus maximus posteriorly reveal the gluteus medius and more anterior structures of the hip region. The fascia lata splits to envelop the tensor fasciae latae, but it only covers the gluteus medius muscle. Gluteus Medius. Origin. Outer aspect of ilium between anterior and posterior gluteal lines and its overlying fascia. Insertion. Lateral surface of greater trochanter. Action. Abductor and medial rotator of hip. Nerve supply. Superior gluteal nerve.
|
plane to reach the femoral neck; then they follow the joint capsule
medially to expose the anterior rim of the acetabulum. The techniques
used in this approach differ mainly in how they detach the abductor
mechanism to allow adduction of the femur for femoral reaming and
retraction of the femoral neck posteriorly for adequate exposure of the
acetabulum.
The interval between them forms a true internervous plane. Two
structures, the lateral femoral cutaneous nerve and the ascending
branch of the lateral femoral circumflex artery, lie between them; they
must be identified and avoided during the dissection (see Figs. 8-14 and 8-15).
consists of the rectus femoris (femoral nerve) and the gluteus medius
(superior gluteal nerve). The interval between them is also an
internervous plane; exploiting it is difficult, mainly because the
short head of the rectus femoris originates partly from the anterior
capsule of the hip joint, where the iliopsoas partly inserts (see Figs. 8-15 and 8-16).
 |
|
Figure 8-42
The gluteus medius, gluteus minimus, and rectus femoris have been resected to reveal the muscular layers down to the hip joint capsule. Resection of the joint capsule exposes the acetabulum and the femoral head and neck. |
vastus lateralis and gluteus medius to provide direct access to the hip
joint capsule. The approach is limited superiorly by the superior
gluteal nerve, which traverses the substance of gluteus medius.
is the site of attachment of two important structures. The sartorius
takes its origin from it, and the inguinal ligament uses it as a
lateral attachment. The anterior superior iliac spine is rarely used as
a bone graft because the lateral cutaneous nerve of the thigh lies so
close to it.
-
The external oblique
forms the outer layer of the muscles of the anterior abdominal wall. It
originates from the outer strip of the anterior half of the iliac crest. -
The internal oblique
forms the middle layer of the muscles of the anterior abdominal wall.
It originates from the center strip of the anterior half of the iliac
crest. -
The tensor fasciae latae arises from the outer lip of the anterior half of the iliac crest.
are not detached during the anterior approach; the tensor fasciae latae
is.
results partly from the pull of the aponeurosis of the vastus lateralis
during growth and partly from the fusion of the trochanter apophyses of
the shaft of the femur (Fig. 8-43; see Fig. 8-41).
side from an almost continuous line of origin along the anterior end of
the iliac crest. The two muscles diverge a short distance below the
anterior superior iliac spine so that the rectus femoris can emerge
from between them (see Fig. 8-14).
itself is triangular. In cross section, it is unusually slim at its
origin and thick just before it inserts into the iliotibial tract. Its
action is difficult to interpret, because another large muscle, the
gluteus maximus, also inserts into the iliotibial tract. In cases of
poliomyelitis, dividing the iliotibial tract relieves flexion and
abduction contractures of the hip joint.
important in standing in a one-legged stance, waiting in a bus line,
for instance, where the muscle may maintain the stability of the
extended knee and hip.12
considerably finer than those of the gluteus medius, but the difference
in the quality of fibers rarely makes it easier to identify the plane
between the two muscles.
muscle in the body, crossing both the hip and the knee. The individual
fibers within the muscle are also the longest in the body; they leave
the sartorius weak but capable of extraordinary contraction.
fasciae latae and the sartorius. Both complicate the superficial
surgical dissection of the anterior approach.
-
The ascending branch of the lateral femoral circumflex artery
is a comparatively large artery that often requires ligation. It is one
of a series of vessels that run circumferentially around the thigh (see
Anterior Approach to the Hip above). This is one of the rare instances in which a vessel crosses an internervous plane (see Figs. 8-15 and 8-16). -
The lateral femoral cutaneous nerve (lateral cutaneous nerve of the thigh)
arises from the lumbar plexus or, occasionally, from the femoral nerve
itself. From there, it descends through the pelvis on the surface of
the iliacus muscle. It enters the thigh under the inguinal ligament
anywhere between the anterior superior iliac spine and the mid-inguinal
point. The nerve pierces the fascia lata just below and medial to
P.441
the
anterior superior iliac spine. The path it takes may vary considerably,
as it can pass either around or through the sartorius muscle (see Fig. 8-14).
 |
|
Figure 8-44 The anterior and anterolateral approaches to the hip joint, showing their muscular boundaries.
|
lateral femoral cutaneous nerve have been reported, particularly from
the section that runs behind the inguinal ligament and from the point
where the nerve pierces the fascia lata. These syndromes consist of
painful paresthesias on the lateral side of the thigh, conditions that
may be relieved by decompressing the nerve. Occasionally, decompression
may have to extend into the pelvis, since the nerve may be compressed
on the surface of the iliacus.
runs through both the superficial and the deep surgical dissection,
mainly because its origin is relatively superficial while its insertion
is deep (see Figs. 8-40, 8-41 and 8-42).
From an anterior approach, the gluteus medius appears to be one of the
muscles of the inner layer over the hip joint. From an anterolateral
approach, it occupies a more superficial position.
this muscle, knowledge of which prevents confusion during the
anterolateral approach to the hip. First, fibers of the gluteus medius
commonly arise from the deep surface of the fascia latae. This means
that when you elevate the fascial flap to gain access to the anterior
border of gluteus medius, you often have to detach muscular fibers from
the inner surface of the fascia. Although the fascia lata encloses the
tensor fasciae latae muscle and covers the gluteus medius, in many
cases the fascia lata actually serves as part of the origin of the
gluteus medius muscle.
Second,
there is often a thin fascial layer covering the gluteus medius muscle
on its outer aspect just above the greater trochanter. In order to pick
up the anterior border of the muscle for dissection, you frequently
need to incise this fascial layer. If you do not do this, it is
difficult to pick up the anterior border of the muscle since this
fascial layer is continuous with the fascia covering the outer aspect
of the greater trochanter.
Paralysis leads to a Trendelenburg gait, in which the patient cannot
prevent his hip from adducting when he puts weight on the affected leg
during walking.
muscle and the anterior part of the greater trochanter. It may become
inflamed, producing pain.
crosses the intermuscular plane between the gluteus medius and the
tensor fasciae latae and must be cut if the dissection extends up to
the pelvis. Whether denervation of the tensor fasciae latae muscle is
clinically significant is a moot point.
and vastus lateralis. The anterior flap of the dissection is lifted off
the underlying greater trochanter until the tendon of gluteus minimus
and the anterior hip joint capsule are revealed. The exposure is made
possible because it utilizes the bursa beneath gluteus medius that
separates the muscle from the bone superiorally (see above).
finding the plane between the joint capsule and the surrounding
structures, because every muscle that crosses the hip joint directly
sends some of its fibers to insert into the capsule.
and the gluteus medius. The rectus femoris has two heads of origin,
both of which must be detached. The straight head arises from the
anterior inferior iliac spine; the reflected head arises from just
above the acetabulum and from the joint capsule itself. The gluteus
medius arises from the outer aspect of the ilium, between the middle
and posterior gluteal lines. While the intermuscular plane between the
two muscles is easy to define and develop, the rectus is difficult to
mobilize from the anterior joint capsule because part of it actually
originates from the capsule itself (see Figs. 8-15, 8-16 and 8-17).
intrudes into the inferomedial portion of the operative field, must be
retracted medially to expose the anterior part of the joint. The
iliopsoas crosses the hip joint directly; it sends some of its fibers
to insert into the joint capsule (see Fig. 8-17).
muscles, the psoas major and the iliacus. The iliopectineal bursa
separates part of the tendon from the hip joint. The bursa, which may
communicate with the joint itself, is usually obliterated in
degenerative disease of the hip, leaving the tendon anchored to the
anterior and medial portions of the joint capsule.
the thigh beneath the inguinal ligament. They lie on the psoas major
muscle, halfway between the anterior superior iliac spine and the pubic
tubercle, the midinguinal point. The femoral artery is thus directly
anterior to the hip joint, with the psoas muscle interposed. The
femoral nerve lies lateral, and the femoral vein medial, to the artery.
(This arrangement can be remembered through the mnemonic “VAN”—vein, artery, nerve.)
of the acetabulum do not damage any of these structures, although a
neurapraxia of the femoral nerve (the most lateral of the triad) may
occur if retraction is prolonged and forceful.
bones are probably biting into the substance of the psoas; they can
damage any of the neurovascular structures that lie in the femoral
triangle. Avoiding these complications depends on keeping to the bone
of the acetabular margin and staying beneath the reflected head of the
rectus femoris and the iliopsoas.
division of gluteus minimus tendon. This does not appear to cause a
postoperative Trendelenburg gait, however.
capsule and the overlying muscles. This plane is occupied by a small
amount of fatty tissue that allows the plane to be opened up by using a
swab and blunt dissection. This useful plane is always present in
primary surgery, but in revision surgery, it is obliterated by scar
tissue. Therefore, there is inherently more risk of damaging the
femoral vessels that lie anterior to the hip joint capsule in revision
surgery than in primary surgery.
access to the joint and can be performed with only one assistant.
Because they do not interfere with the abductor mechanism of the hip,
they avoid the loss of abductor power in the immediate postoperative
period. Posterior approaches allow excellent visualization of the
femoral shaft, thus are popular for revision joint replacement surgery
in cases in which the femoral component needs to be replaced.
posterior capsule, if dislocation of any prosthesis occurs, it will
result from flexion and internal rotation of the hip. Thus, there may
be a higher dislocation rate than that from anterior approaches if the
posterior approach is used in fractured neck of femur surgery in
elderly bedridden patients who often lie in bed with their hips in a
flexed and adducted position.
-
Hemiarthroplasty14,15,16
-
Total hip replacement, including revision surgery
-
Open reduction and internal fixation of posterior acetabular fractures
-
Dependent drainage of hip sepsis
-
Removal of loose bodies from the hip joint
-
Pedicle bone grafting17
-
Open reduction of posterior hip dislocations
 |
|
Figure 8-45 Position of the patient on the operating table for the posterior approach to the hip joint.
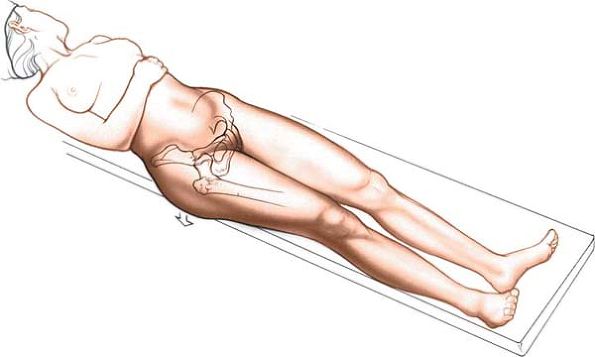
|
affected limb uppermost. Because most patients requiring surgery are
elderly and have delicate skin, it is important to protect the bony
prominences of the legs and pelvis with pads placed under the lateral
malleolus and knee of the bottom leg and a pillow between the knees.
Drape the limb free to leave room for movement during the procedure (Fig. 8-45).
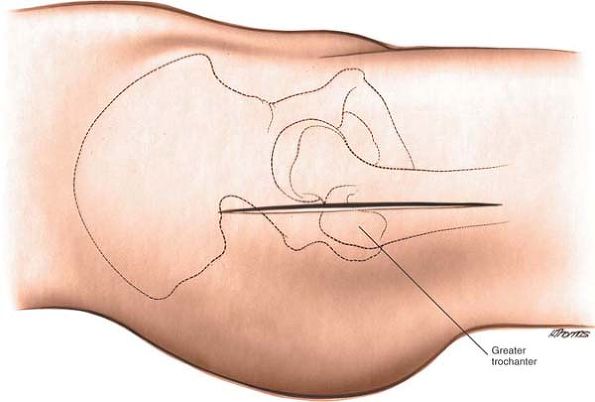
on the outer aspect of the thigh. The posterior edge of the trochanter
is more superficial than the anterior and lateral portions, and, as
such, it is easier to palpate (see Fig. 8-21).
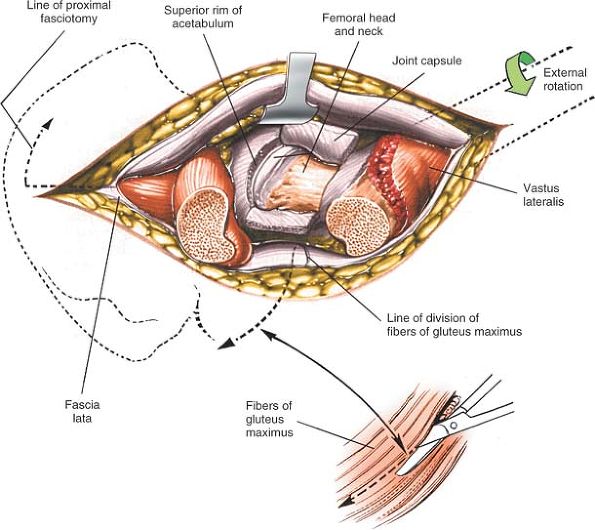
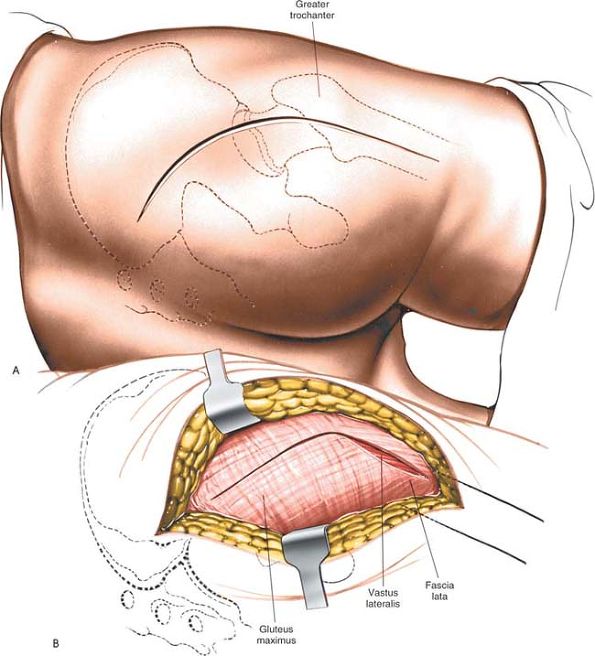
posterior aspect of the greater trochanter. Begin your incision some 6
cm to 8 cm above and posterior to the posterior aspect of the greater
trochanter. The part of the incision that runs from this point to the
posterior aspect of the trochanter is in line with the fibers of the
gluteus maximus. Curve the incision across the buttock, cutting over
the posterior aspect of the trochanter, and continue down along the
shaft of the femur (Fig. 8-47A).
If you flex the hip 90° and make a straight longitudinal incision over
the posterior aspect of the trochanter, it will curve into a
“Moore-style” incision when the limb is straight. The final incision is
curved and 10 to 15 cm long, centered on the posterior aspect of the
greater trochanter.
However, the gluteus maximus, which is split in the line of its fibers,
is not significantly denervated because it receives its nerve supply
well medial to the split (Fig. 8-46).
 |
|
Figure 8-46
There is no true internervous plane. Split the fibers of the gluteus maximus, a procedure that does not cause significant denervation of the muscle. |
femur to uncover the vastus lateralis. Lengthen the fascial incision
superiorly in line with the skin incision, and split the fibers of the
gluteus maximus by blunt dissection (Fig. 8-47B). (The fascial covering of the gluteus maximus varies considerably in its thickness. In the elderly, it is quite thin.)
superior and inferior gluteal arteries, which enter the deep surface of
the muscle and ramify outward like the spokes of a bicycle wheel;
hence, splitting the muscle inevitably crosses a vascular plane. In
addition to the arterial bleeding, venous bleeding must be anticipated.
If you split the muscle gently, you may be able to pick up, coagulate,
and cut the crossing vessels before they are stretched and avulsed by
the blunt dissection of the split. Obviously, vessels
that are torn when stretched retract into the muscle and are more difficult to control.
 |
|
Figure 8-47 (A) Skin incision for the posterior approach to the hip joint. (B) Incise the fascia lata.
|
 |
|
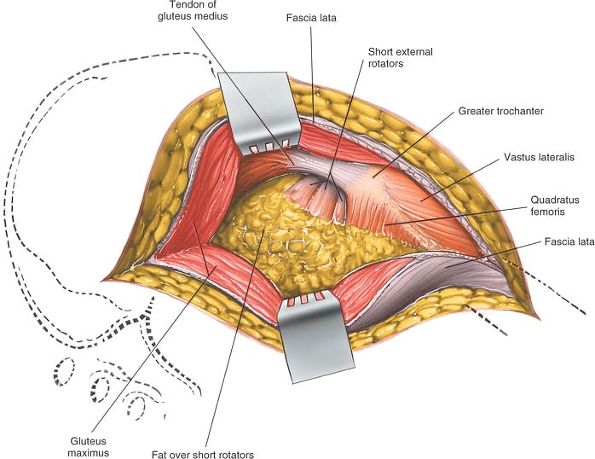
Figure 8-48 Retract the gluteus maximus to reveal the fatty layer over the short external rotators of the hip.
|
deep fascia of the thigh. Underneath is the posterolateral aspect of
the hip joint, still covered by the short external rotator muscles,
which attach to the upper part of the posterolateral aspect of the
femur (Fig. 8-48).
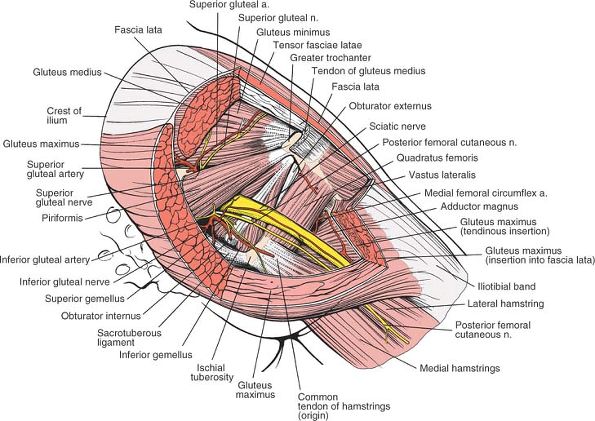
through the greater sciatic notch and runs down the back of the thigh
on the short external rotator muscle, encased in fatty tissue. The
nerve crosses the obturator internus, the two gemelli, and the
quadratus femoris before disappearing beneath the femoral attachment of
the gluteus maximus. You can find the nerve lying on the short external
rotators, and it can be easily palpated. Do not dissect to see the
nerve; you may cause unnecessary bleeding from the vessels lying in the
fat around it (Fig. 8-49).
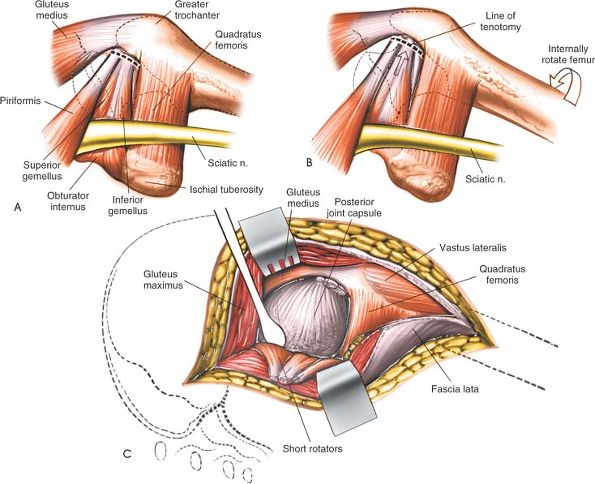
rotator muscles on a stretch (making them more prominent) and to pull
the operative field farther from the sciatic nerve (Fig. 8-50A,B).
internus tendons just before they insert into the greater trochanter.
Detach the muscles close to their femoral insertion and reflect them
backward, laying them over the sciatic nerve to protect it during the
rest of the procedure (Fig. 8-50C).
(The upper part of the quadratus femoris may also have to be divided to
fully expose the posterior aspect of the joint capsule, but the muscle
contains troublesome vessels that arise from the lateral circumflex
artery. Normally, it should be left alone.)
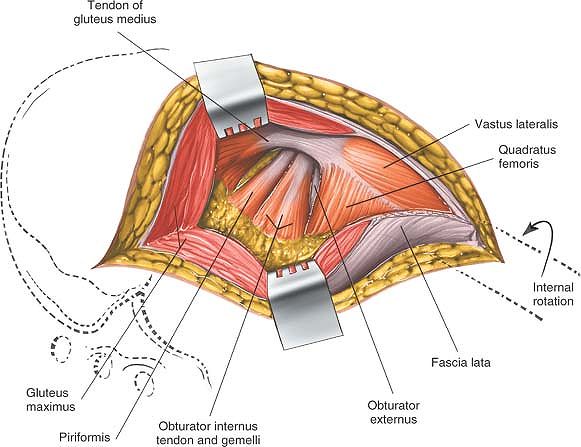
fully exposed. The hip joint capsule can be incised with a longitudinal
or T-shaped incision. Dislocation
of the hip is achieved by internal rotation after capsulotomy (Fig. 8-51). Posterior joint capsulotomy will have exposed the femoral head and neck.
 |
|
Figure 8-49
Push the fat posteromedially to expose the insertions of the short rotators. Note that the sciatic nerve is not visible; it lies within the substance of the fatty tissue. Place your retractors within the substance of the gluteus maximus superficial to the fatty tissue. |
exposed or transected during this approach. However, it is sometimes
involved in major complications. It can be damaged if it is compressed
by the posterior blade of a self-retaining retractor used to split the
gluteus maximus. Always keep the retractors on the cut surfaces of the
rotators; the muscles will protect the nerve.
common peroneal branches within the pelvis; on occasion, you may expose
these two “sciatic nerves” during this approach. If you have identified
the sciatic nerve but think that it looks too small, search for the
nerve’s other branch; it is in danger if it is overlooked.
leaves the pelvis beneath the piriformis. It spreads cephalad to supply
the deep surface of the gluteus maximus. Its branches are inevitably
cut when the gluteus maximus is split; you can identify and coagulate
them before they are avulsed if you are dissecting carefully.
from beneath the lower border of the piriformis when pelvic fractures
involve the greater sciatic notch. If it retracts into the pelvis and
bleeding is brisk, turn the patient over into the supine position, open
the abdomen, and tie off the artery’s feeding vessel, the internal
iliac artery.
-
Enlarge the skin incision. Obese patients
may have a considerable layer of subcutaneous tissue over the buttock
that restricts deep exposure; lengthening the skin incision and
dissecting subcutaneously can compensate for this problem. -
Extend the fascial incision superiorly and inferiorly.
-
Detach the upper half of the quadratus femoris. Because the muscle contains troublesome vessels,
P.448P.449
it should be divided about 1 cm from its insertion to make hemostasis
easier. Its excellent blood supply is useful both when the muscle is
transposed and in treatment of some cases of nonunion of femoral neck
fractures (Fig. 8-52).![]() Figure 8-50 (A, B)
Figure 8-50 (A, B)
Internally rotate the femur to bring the insertion of the short
rotators of the hip as far lateral to the sciatic nerve as possible. (C)
Detach the short rotator muscles close to their femoral insertion and
reflect them backward, laying them over the sciatic nerve to protect it.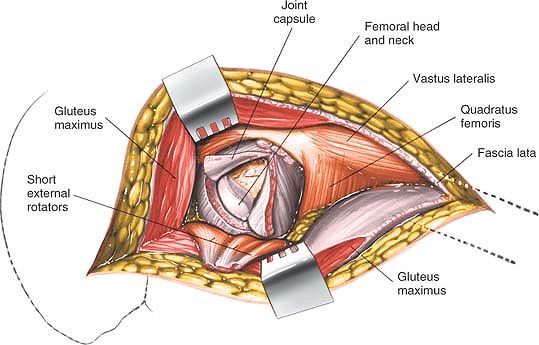 Figure 8-51 Incise the posterior joint capsule to expose the femoral head and neck.
Figure 8-51 Incise the posterior joint capsule to expose the femoral head and neck. -
Detach the insertion of the gluteus
maximus tendon from the femur to increase the exposure of the femoral
neck and shaft. This maneuver is particularly useful during total joint
replacement, especially revision joint replacement. If you detach the
tendon, position acetabular retractors on the rim of the acetabulum as
you would in the anterolateral approach. As long as the retractors are
firmly on bone and do not crush soft tissues against the acetabular
rim, no vital structures will be damaged (see Fig. 8-52).
 |
|
Figure 8-52 To gain additional exposure, cut the quadratus femoris and the tendinous insertion of the gluteus maximus.
|
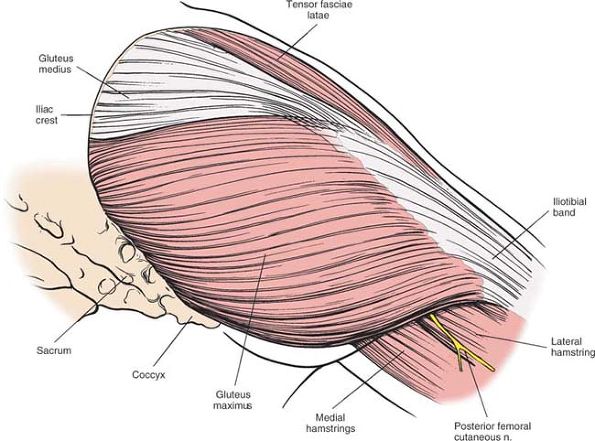
joint form two sheaths or layers. The outer layer consists of the
gluteus maximus. The inner layer consists of the short external
rotators of the hip, the piriformis, the superior gemellus, the
obturator internus, the inferior gemellus, and the quadratus femoris.
The sciatic nerve runs vertically between the two layers, down through
the operative field (Figs. 8-53 and 8-54).
buttock like the front cover of a book. It inserts partly into the
iliotibial band and partly into the gluteal tuberosity of the femur.
Also inserting into the band, but further anteriorly, is the tensor
fasciae latae. Together, the gluteus maximus, the fascia lata (which
covers the gluteus medius), and the tensor fasciae latae form a
continuous fibromuscular sheath, the outer layer of the hip musculature
(see Fig. 8-53). As Henry18 noted, the layer can be viewed as the “pelvic deltoid”: it covers the hip much as the deltoid muscle covers the shoulder.
 |
|
Figure 8-53 The superficial musculature of the posterior approach of the hip joint. The gluteus maximus predominates.
Gluteus Maximus. Origin.
From posterior gluteal line of ilium and that portion of the bone immediately above and behind it; from posterior surface of lower part of sacrum and from side of coccyx; and from fascia covering gluteus medius. Insertion. Into iliotibial band of fascia lata and into gluteal tuberosity. Action. Extends and laterally rotates thigh. Nerve supply. Inferior gluteal nerve. |
each of which changes the posterior approach. The most natural
separation, the Marcy-Fletcher approach,19 lies at the anterior border of the
gluteus maximus, between the gluteus maximus (inferior gluteal nerve)
and the gluteus medius. This approach uses a true internervous plane.
 |
|
Figure 8-54
The gluteus maximus and the gluteus medius have been resected to reveal the gluteus minimus, the piriformis, and the short rotator muscles. Note the relationship of the neurovascular structures to the piriformis. Gluteus Minimus. Origin. From outer surface of ilium between anterior and inferior gluteal lines. Insertion. Into impression on anterior border of greater trochanter via tendon that gives expansion to joint capsule. Action. Rotates thigh medially and abducts it. Nerve supply. Superior gluteal nerve.
Piriformis. Origin. From front of sacrum via fleshy digitations from second, third, and fourth portions of sacrum. Insertion. Into upper border of greater trochanter via round tendon. Action. Rotates thigh laterally and abducts it. Nerve supply. Branches from first and second sacral nerves.
Obturator Internus. Origin. From inner surface of anterolateral wall of pelvis and from surfaces of greater part of obturator foramen. Insertion. Onto medial surface of greater trochanter above trochanteric fossa. Action. Rotates thigh laterally. Nerve supply. Any nerve from sacral plexus.
Quadratus Femoris. Origin. From upper part of external border of tuberosity of ischium. Insertion. Into upper part of linea quadrata, the line that extends vertically downward from intertrochanteric crest. Action. Rotates thigh laterally. Nerve supply. Branch from sacral plexus.
|
 |
|
Figure 8-55 The gluteus minimus, piriformis, and short rotators have been resected to uncover the posterior aspect of the hip joint.
|
involve splitting the fibers of the gluteus maximus. They are more
popular than the Marcy-Fletcher approach even though they do not
operate in an internervous plane, mainly because they offer excellent
exposure of the hip joint.
which the skin incision is centered, is the easiest bony prominence to
palpate around the hip. Its posterior aspect is relatively free of
muscles; its anterior and lateral aspects are covered by the tensor
fasciae latae and the gluteus medius and minimus muscles and are much
less accessible.
neck and the shaft of the femur. From there, it projects both upward
and backward (Fig. 8-56). The following five muscles insert into it:
-
The gluteus medius
attaches by a broad insertion into its lateral aspect. Below this
insertion, the bone is covered by the beginnings of the iliotibial
tract. A bursa, occasionally a site of inflammation, lies between the
tract and the bone over the relatively bare portion of the trochanter.
The bursa can be the site of bacterial infection (historically, most
frequently tuberculosis). -
The gluteus minimus is attached to the anterior aspect of the trochanter, where its tendon is divided in the anterolateral approach (see Fig. 8-54).
-
The piriformis
inserts via a tendon into the middle of the upper border of the greater
trochanter. Its insertion forms a surgical landmark for the insertion
of certain types of intramedullary rods into the femur. The bone is
perforated just medial to it,
P.453
the easiest route into the medulla of the femoral shaft (see Fig. 8-54).![]() Figure 8-56 Osteology of the posterior aspect of the hip and pelvis.
Figure 8-56 Osteology of the posterior aspect of the hip and pelvis. -
Obturator externus tendon.
Immediately below the insertion of the piriformis lies the trochanteric
fossa, a deep pit that marks the attachment of the obturator externus
tendon (see Fig. 8-54). -
The obturator internus tendon inserts with the two gemelli into the upper border of the trochanter, posterior to the insertion of the piriformis (see Fig. 8-54).
cleavage of the skin at almost 90°, but the resulting scar is always
hidden by clothing. Most patients who undergo this approach are elderly
and tend not to form exuberant scar tissue, and they heal with a fine
line scar.
outer muscle layer by splitting the fibers of the gluteus maximus, the
single largest muscle in the body. The fibers of the gluteus maximus
are extremely coarse; they run obliquely downward and laterally across
the buttock. The muscle’s innervation, the inferior gluteal nerve,
emerges from the pelvis beneath the inferior border of the piriformis
and almost immediately enters the muscle’s deep surface close to its
medial border, its origin. From there, the nerve’s branches spread
throughout the muscle. Splitting the gluteus maximus close to its
lateral insertion does not denervate significant portions of the
muscle, because its main nerve supply passes well medial to the most
medial point of splitting (see Fig. 8-53).
standing still; it comes into play during stair climbing or standing up
from a sitting position. (During normal walking, hip extension is
primarily a function of the hamstrings rather than the gluteus maximus.)
inner muscular layer (the short external rotators of the hip) to expose
the posterior hip joint capsule (see Fig. 8-55).
Five muscles form the inner layer: the piriformis, the superior
gemellus, the tendon of the obturator internus, the inferior gemellus,
and the quadratus femoris.
passing structures is the key to understanding the neurovascular
anatomy of the area (see Fig. 8-54). All
neurovascular structures that enter the buttock from the pelvis pass
through the greater sciatic notch, either superior or inferior to the
piriformis, which itself passes from the pelvis to the buttock through
the notch.
 |
 |
emerges from the pelvis above the piriformis. It crosses behind the
posterior border of the gluteus medius and runs in the space between
the gluteus medius and the gluteus minimus, supplying both before
sending fibers to the tensor fasciae latae.
the largest branch of the internal iliac artery, enters the pelvis
above the upper border of the piriformis and runs with its nerve,
supplying the gluteus medius and gluteus minimus and sending a nutrient
vessel to the ilium on the gluteal line. The nutrient vessel may bleed
when a larger posterior iliac bone graft is taken. The superior gluteal
artery also sends branches to the overlying gluteus maximus, forming
part of the muscle’s dual arterial supply.
fractures, especially in those involving the greater sciatic notch. If
it retracts into the pelvis, its bleeding must be controlled by an
extraperitoneal approach to the pelvis so that its feeding vessel, the
internal iliac artery, can be ligated. In pelvic fractures, selective
angiography may aid in the diagnosis of a ruptured superior gluteal
artery. During the angiography, the artery may be embolized through the
diagnostic cannula, avoiding a pelvic exploration.21
If you are using the anterior or posterior approaches to the acetabulum
using a trochanteric osteotomy, the superior gluteal vessels must be
intact in order to avoid muscle necrosis of the gluteus medius and
minimus. This is because the origin and insertion of the muscles is
detached in these approaches. If the acetabular fracture involves a
displaced fracture of the greater sciatic notch, preoperative
angiography is advised to ensure that the neurovascular pedicle to
these structures is intact.
reaches the buttock beneath the lower border of the piriformis. It
enters the deep surface of the gluteus maximus almost immediately.
which follows the inferior gluteal nerve, supplies the gluteus maximus.
The branch it sends along the sciatic nerve was the original axial
artery of the limb. In rare cases, this artery can serve as one guide
to the sciatic nerve during surgery. The inferior gluteal artery may
also be torn in pelvic fractures, but not as frequently as the superior
gluteal artery.
encountered during the posterior approach to the hip because its course
in the buttock is very short. It turns around the sacrospinous ligament
before entering the perineum.
runs with the pudendal nerve. The artery is usually well clear of the
operative field during posterior approaches, but damage to it has been
reported. Local pressure against the ischial spine usually controls
bleeding; if not, or if the artery has retracted, an extraperitoneal
approach through the space of Retzius22 may be needed to ligate the parent trunk.
enters its muscle almost as soon as it emerges from behind the inferior
border of the piriformis. The nerve also supplies the superior gemellus.
which is formed by roots from the lumbosacral plexus (L4, L5, S1, S2,
S3), appears in the buttock from beneath the lower border of the
piriformis, just lateral to the inferior gluteal and pudendal nerves
and vessels. It is usually surrounded by fat and is often easier to
feel than to see. It passes vertically down the buttock together with
its artery, lying on the short external rotator muscles of the inner
muscular sleeve, the obturator internus, the two gemelli, and the
quadratus femoris. Farther distally, it passes deep (anterior) to the
biceps femoris and disappears from view, lying on the adductor magnus.
long as you are aware of its position. It can be injured if it is
trapped in the posterior blade of the self-retaining retractor that
holds the fascial edge. It also can be damaged if it is not protected
during reduction of the prosthetic head into the acetabulum.
hamstring muscles except the short head of the biceps femoris and the
extensor portion of the adductor magnus in the thigh. All its branches
arise from the medial side of the nerve. Dissections around the sciatic
nerve in the thigh therefore should remain on the lateral (safe) side,
since the only branch coming
off
that side runs to the short head of the biceps, a muscle that causes
few clinical problems if its nerve supply is damaged (see Fig. 8-54).
the terminal branches of the sciatic nerve, supply all the muscles
below the knee. In addition, they (and other sciatic branches) supply
skin over the sole of the foot, the dorsum of the foot (except for its
medial side), and the calf and lateral side of the lower leg. Damage to
the sciatic nerve at the level of the hip joint injures both tibial and
common peroneal elements, resulting in a balanced flaccid paralysis
below the knee, together with paralysis of the hamstring muscles.
Complete sciatic nerve lesions are relatively rare; more often, the
damage seems to affect either the tibial or the common peroneal
components. Hence, neurologic findings may vary regardless of the level
of the lesion.
approaches to the hip. The question then arises as to whether the nerve
was damaged at the operative site or whether it was compressed as it
turns around the fibular head, usually during postoperative care. The
differential diagnosis can be made by doing an electromyogram (EMG) of
the short head of the biceps, the only muscle of the thigh that is
supplied by the common peroneal division of the sciatic nerve. Lesions
in the pelvis or at the level of the hip joint denervate this muscle.
Lesions at the level of the fibular head leave it unaffected.
the hip joint is formed by nerve fibers. The remaining 80% is made up
of connective tissue. Nerve repairs in this area are often
unsuccessful, because bundle-to-bundle contact is difficult to achieve.
supplies a large area of skin on the back of the thigh. The nerve
actually lies on the sciatic nerve until the sciatic passes deep to the
biceps femoris. Then the posterior femoral cutaneous nerve continues
superficial to the hamstring muscles but deep to the fascia lata,
sending out several cutaneous branches.
emerges from the pelvis behind the sciatic nerve and runs with it on
its deep surface as it crosses the tendon of the obturator internus and
the two gemelli. The nerve then passes deep to the quadratus femoris
before entering its anterior surface. It also gives off muscular
branches to the inferior gemellus.
make a right-angled turn; it curves round the lesser sciatic notch of
the ischium. The muscle has a tricipital tendon that is reinforced at
its insertion by the superior and inferior gemelli.
Its transversely running fibers form a clear surgical landmark. The
muscle has an excellent blood supply. At the lower border of its
insertion lies the cruciate anastomosis, consisting of the ascending
branch of the first perforating artery, the descending branch of the
inferior gluteal artery, and transverse branches of the medial and
lateral femoral circumflex arteries (see Fig. 8-54).
In this maneuver, the quadrate tubercle of the femur is detached,
leaving the muscular insertion of the quadratus femoris intact. The
resultant muscle-bone pedicle can be swung upward, and the bone can be
inserted across the fracture site.
was originally designed for surgery on flexed, abducted, and externally
rotated hips, the kinds of deformities caused by certain types of
congenital dislocation of the hip.
-
Open reduction of congenital dislocation
of the hip. The approach gives an excellent exposure of the psoas
tendon, which can block reduction of the hip.24 -
Biopsy and treatment of tumors of the inferior portion of the femoral neck and medial aspect of proximal shaft
-
Psoas release
-
Obturator neurectomy
obturator neurectomy. If a neurectomy is combined with an adductor
release, the approach can be performed through a short transverse
incision or a short longitudinal incision in the groin that permits
division
of the adductors close to their pelvic origin, an area where there is less bleeding.
 |
|
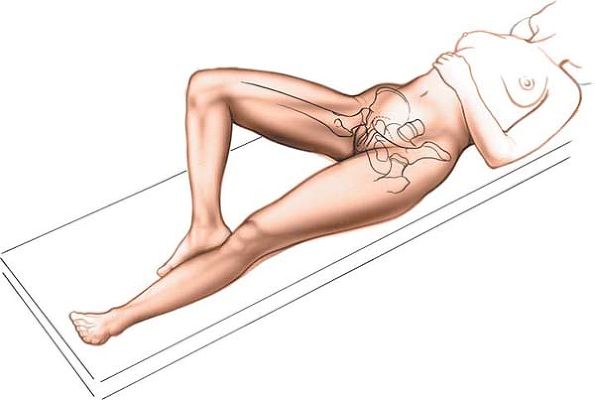
Figure 8-57 Position of the patient on the operating table for the medial approach to the hip.
|
affected hip flexed, abducted, and externally rotated. This may not be
possible in cases with fixed deformity, when the position is often
determined for you. The sole of the foot on the affected side should
lie along the medial side of the contralateral knee (Fig. 8-57).
from the medial side of the thigh and follow it up to its origin at the
pubis, in the angle between the pubic crest and the symphysis. The
adductor longus is the only muscle of the adductor group that is easy
to palpate.
move your thumb along the inguinal creases medially and obliquely
downward until you can feel the pubic tubercle. They are at the same level as the top of the greater trochanter.
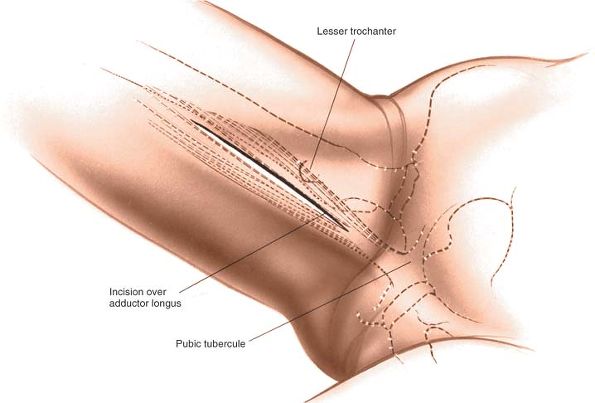
thigh, starting at a point 3 cm below the pubic tubercle. The incision
runs down over the adductor longus. Its length is determined by the
amount of femur that must be exposed (Fig. 8-58).
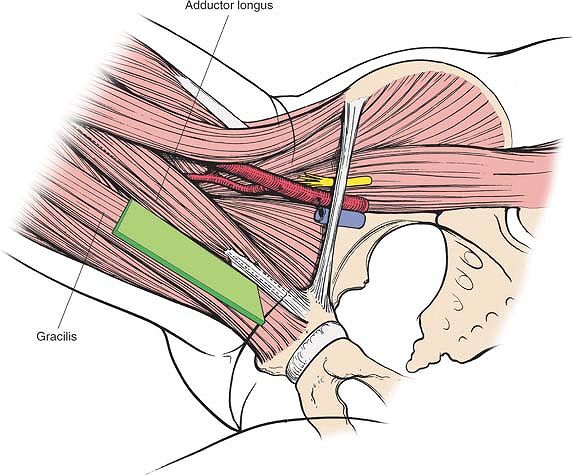
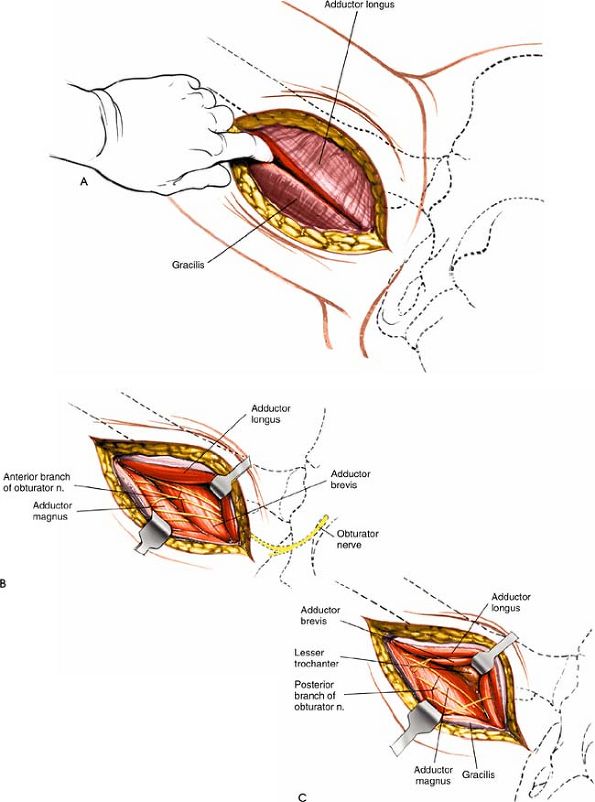
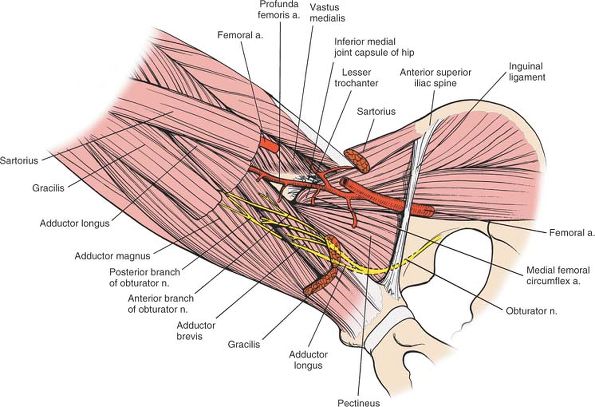
internervous plane, since both the adductor longus and the gracilis are
innervated by the anterior division of the obturator nerve. The plane
is nevertheless safe for dissection; both muscles receive their nerve
supplies proximal to the dissection (Fig. 8-59).
adductor brevis and the adductor magnus. The adductor brevis is
supplied by the anterior division of the obturator nerve. The adductor
magnus has two nerve supplies: Its adductor portion is supplied by the
posterior division of the obturator nerve, and its ischial
portion
is supplied by the tibial part of the sciatic nerve. The two muscles,
therefore, form the boundaries of an internervous plane (see Fig. 8-62).
 |
|
Figure 8-58 Incision for the medial approach to the hip.
|
 |
|
Figure 8-59
The intermuscular interval between the adductor longus and the gracilis is not an internervous plane because both muscles are innervated by the anterior division of the obturator nerve. The plane is safe, however, because the muscles receive their nerve supplies proximal to the dissection. |
 |
|
Figure 8-60 (A) Develop the plane between the gracilis and the adductor longus. (B)
Retract the adductor longus and the gracilis to reveal the adductor brevis with the overlying anterior division of the obturator nerve. (C) Retract the adductor brevis from the muscle belly of the adductor magnus to uncover the posterior division of the obturator nerve. Note the lesser trochanter in the depths of the wound. |
between the gracilis and the adductor longus. Like other intermuscular
planes in the adductor group, this plane can be developed with your
gloved finger (Fig. 8-60A).
adductor brevis and the adductor magnus until you feel the lesser
trochanter on the floor of the wound. Try to protect the posterior
division of the obturator nerve, the innervation to the muscle’s
adductor portion, to preserve the hip extensor function of the adductor
magnus (see Dangers below). Place a narrow retractor (such as a bone spike) above and below the lesser trochanter to isolate the psoas tendon.
 |
|
Figure 8-61
Anatomy of the medial approach to the hip. The thigh is abducted, slightly flexed, and externally rotated. The plane of the superficial dissection runs between the adductor longus and the gracilis. |
lies on top of the obturator externus and runs down the medial side of
the thigh between the adductor longus and the adductor brevis, to which
it is bound by a thin tissue. It supplies the adductor longus, the
adductor brevis, and the gracilis in the thigh (Fig. 8-60B).
lies in the substance of the obturator externus, which it supplies
before it leaves the pelvis. The nerve then runs down the thigh on the
adductor magnus and under the adductor brevis; it supplies the adductor
portion of the adductor magnus (Fig. 8-60C).
 |
|
Figure 8-62
The muscular layer of the medial approach to the hip. The dissection lies between the adductor brevis and the adductor magnus. The gracilis, adductor longus, and sartorius have been resected to reveal the deeper structures of the medial aspect of the thigh. Note the relationships of the anterior and posterior divisions of the obturator nerve to the adductor longus and adductor brevis. Note the proximity of the medial femoral circumflex artery to the insertion of the psoas tendon. Psoas Major. Origin. Anterior surface of transverse processes and bodies of the lumbar vertebrae and corresponding intervertebral disks. Insertion. Lesser trochanter of femur. Action. Flexor of hip and flexor of lumbar spine when leg is fixed. Nerve supply. Segmental nerves from second and third lumbar roots.
Iliacus. Origin.
Upper two thirds of iliac fossa, inner lip of iliac crest, anterior aspect of sacroiliac joint, and from the lumbosacral and iliolumbar ligaments. Insertion. Lesser trochanter of femur by common tendon with psoas. Action. Flexor of hip. Tilts pelvis forward when leg is fixed. Nerve supply. Femoral nerve (L2-L4). |
to cut these nerves to relieve muscular spasticity. If you are not
using it for that purpose, avoid transecting them.
passes around the medial side of the distal part of the psoas tendon.
It is in danger, especially in children, if you try to detach the psoas
without isolating the tendon and cutting it under direct vision (Fig. 8-62).
the psoas and iliacus, you can expose some 5 cm of femoral shaft distal
to the lesser trochanter by blunt dissection.
adductor compartment of the thigh. The adductors do not cover the hip
joint, since they all originate below the level of the joint itself.
layers of muscles, with the two divisions of the obturator nerve
running between each pair of layers. The superficial layer consists of
the adductor longus and the gracilis; the middle layer, the adductor
brevis; and the deep layer, the adductor magnus.
only muscle of the adductor group that is easily palpable at its
tendinous origin. Its structure is considered in detail in the
superficial surgical dissection.
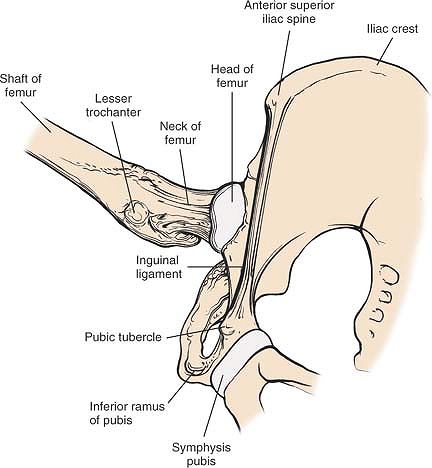 |
|
Figure 8-63 Osteology of the medial approach to the hip.
|
obliquely, since they run down and medially cross the front of the
thigh. A transverse insertion made in the groin, used for release of
the adductors, is parallel with the lines and should heal with minimal
scar formation. Meticulous closure of the deep fascia minimizes ugly
depressed scars.
gracilis. Both muscles are supplied by the anterior division of the
obturator nerve, but the nerves enter them close to their pubic
origins, leaving the intermuscular plane available for surgical use
(see Fig. 8-61).
long and thin, with long parallel-running fibers. Its aponeurotic
origin, a thin sheet of tendinous fibers arising from the pubis, lies
in an anteroposterior plane.
high incidence of avulsion fractures. The origin may ossify in those
who, like horseback riders, use their hip adductors excessively. This
ossification is known as rider’s bone. Calcification and ossification
are also seen in soccer players in whom the lesion may give rise to
chronic pain and loss of function.
divisions. The anterior division passes over the upper border of the
obturator externus and descends on the medial side of the thigh behind
the adductor longus, on the anterior surface of the adductor brevis. It
supplies sensory fibers to the hip joint.
contractures of the hip caused by spasticity of the adductor muscles.
To find it, define the interval between the adductor longus and the
adductor brevis, the point at which the nerve is available for section.
The nerve lies on the anterior surface of the adductor brevis, bound to
it by a thin areolar covering. There, it may divide into three or even
four bundles. Therefore, when performing an anterior obturator
neurectomy, dissect the nerve bundles proximally as far as possible to
avoid overlooking branches coming off higher up.
medial side of the knee, perhaps the reason hip pain is often referred
to the knee, especially in cases of slipped upper femoral epiphysis. (A
second pain commonly referred to the inside of the knee, originating in
the ovary, is thought to be due to direct irritation of the obturator
nerve by ovarian pathology, because the nerve runs adjacent to the
ovary in the pelvis.)
inserts into the tibia. In humans, the superficial medial ligament of
the knee is thought to have arisen as the degenerative tendon of the
adductor magnus and is sometimes referred to as the fourth hamstring
muscle.
R, Judet T, Letournel E: Fractures of the acetabulum classification and
surgical approaches: open reduction. J Bone Joint Surg 46A:1615, 1964
J, Liour Z, Yates M: Complex acetabular fractures: a transtrochanteric
lateral surgical approach. Clin Orthop Related Research 151:107, 1980
AT: The Moore self-locking vitallium prosthesis in fresh femoral neck
fractures: a new low posterior approach (the southern exposure). In:
American Academy of Orthopaedic Surgeons: instructional course
lectures, Vol. 16. St. Louis, CV Mosby, 1959
MH, Harvey JP, Moore TM: Treatment of displaced subcapital and
transcervical fractures of the femoral neck by muscle pedicle–bone
graft and internal fixation. J Bone Joint Surg (Am) 55:257, 1973
GH, Fletcher RS: Modification of the posterolateral approach to the hip
for insertion of femoral head prosthesis. J Bone Joint Surg (Am)
36:142, 1954
B, Meyer RP, Vrkkala K et al: The mechanisms of severe arterial injury
in surgery of the hip joint. Clin Orthop 141:122, 1979
AA: Ueber das ligamentjm pelvioprostaticum oper den apparat, durch
welchen die harnblane, die prostata uno der untern becken öffnung
befestgt sind. Arch Anat Physiol 188–189, 1841
AB jr: Primary open reduction of congenital dislocation of the hip
using a median adductor approach. J Bone Joint Surg (Am) 55:671, 1973