Spinal Injuries
Although not the usual focus of a sports medicine practitioner, its
importance should not be overlooked. Spinal conditions can have
substantial effects on an athlete’s performance, as well as important
implications of the propensity for neurological injuries. It is the
goal of this chapter to review the essentials of spinal examination,
specific injuries of the cervical and lumbar spine, and the current
recommendations for return to sport after athletic head injuries.
-
Among the most crucial tasks of the
on-field physician is to decide when a potential spine injury is benign
or requires immediate stabilization and further workup. -
The following features are indications
for immediate stabilization and immobilization and transfer to an
emergency department for evaluation:-
The athlete is down on the field.
-
No voluntary or spontaneous movement is noted.
-
Loss of consciousness has occurred.
-
There are objective neurological or cognitive deficits.
-
A palpable step-off is appreciated.
-
Localized tenderness and pain with a high index of suspicion.
-
-
In such cases, imaging studies—such as x-rays, computerized tomography (CT), or magnetic resonance imaging (MRI)—are indicated.
-
The athlete needs to be immobilized carefully and securely for transfer.
-
The on-field examination of an injured athlete starts with evaluation of the “ABCs” (Airway, Breathing, Circulation).
-
The Glasgow Coma Scale is a useful method of assessing quickly the neurocognitive status (see Table 7-3 in Chapter 7).
-
The pupils should be examined for reactivity and the gaze noted for signs of ocular deviation.
-
-
A detailed neurological examination should be performed.
-
The athlete should not be moved from a supine position.
-
Motor strength of individual muscles or
motions can be tested and graded (in the fully contracted or shortened
position) in the upper and lower extremities to assess function of
individual nerve root levels (Table 8-1 and Table 8-2).
-
-
Sensation to light touch should be graded as normal, diminished, or absent in each dermatome.
-
Importantly, rectal tone should be
assessed, particularly in the unconscious patient, as it may be the
only possible site of motor strength assessment. In the awake patient,
perianal sensation is a reflection of the most distal sacral nerve root
function (S2-5). -
Deep tendon reflexes should also be
tested. These include the biceps (C5), brachioradialis (C6), triceps
(C7), patella tendon (L4), and Achilles tendon (S1) reflexes.-
The bulbocavernosus reflex (assessed by
squeezing the glans of the penis or clitoris or gently tugging a Foley
catheter) results in involuntary contraction of the anal sphincter. -
Hyperreflexia (3 +) is an indication of upper motor neuron dysfunction, such as spinal cord compression.
-
Hyporeflexia (0 or 1 +) is an indication
of lower motor neuron dysfunction (such as compression of the cauda
equina or peripheral nerves). -
Clonus is elicited by jerking the ankle into dorsiflexion. More than four beats are considered pathologic.
-
An upgoing Babinski response is also an indication of upper motor neuron disease.
-
-
The spinous processes and paraspinal muscles should be palpated.
-
This can be performed by carefully logrolling the patient from side to side, although a supine examination can often suffice.
-
Importantly, a helmet should be left in place. Removing a helmet can cause harmful motion of an injured cervical spine.
-
The facemask and chin strap can, and should, be removed to allow assessment of the airway and eyes.
-
-
-
If a spinal injury is suspected, the athlete is then immobilized.
-
A transfer board is usually used.
-
The athlete is logrolled from side to side to place him/her on the board.
-
Taping or strapping the head and body to
the board is the most effective method of immobilizing the spine. A
cervical collar can also be used. -
Once again, the helmet should stay in place.
-
|
TABLE 8-1 GRADING OF MUSCLE STRENGTHa
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||
|
TABLE 8-2 MUSCLE NERVE ROOT LEVELS
|
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
-
Although many components are the same,
the in-office spinal assessment includes more detailed history and
neurological and palpatory examinations. -
A history of movements (e.g., extension versus flexion) that aggravate pain should be sought.
-
Tenderness of the spinous processes, facet joints, sacroiliac joints, ribs, and paraspinal muscles can be differentiated.
-
Though it should never be performed in the acute traumatic setting, neck and back range of motion should be quantified.
-
In addition to the motor, sensory, and
reflex examination, the ambulatory neurologic examination should
include assessment for pathologic reflexes, such as Hoffmann’s and
inverted radial reflexes and root tension signs such as the
straight-leg raise and femoral stretch test. -
Imaging studies are indicated for patients with:
-
Worsening symptoms
-
A progressive neurological deficit
-
Symptoms that continue beyond 4 to 6 weeks
-
-
Following a general imaging protocol may be helpful.
-
Low back pain usually affects athletes at
some point in their career. It can be from an “overuse syndrome” or
acute trauma. Complaints may range from mild pain to severe pain after
a game or practice. -
Some injuries are characteristic of
certain sports: lumbar herniated disks in weight lifters, sacral stress
fractures in runners, and spondylolysis in football players and
gymnasts. -
Predominantly, axial low back pain suggests internal disc disruption from degenerative disc disease.
-
Predominantly, leg symptoms suggest radiculopathy from a herniated disc.
-
Infections, tumors, or inflammatory
arthritis are more typically suggested by nonmechanical back pain.
Other red flags are night pain, pain at rest, fever, or weight loss. -
The differential diagnosis of lumbar
spine injuries in athletes can be divided into two categories: serious
acute injuries and benign and chronic injuries (Box 8-1).
-
Acute fracture or dislocation
-
Large herniated disc/cauda equina syndrome
-
Epidural hematoma
-
Spinal cord injury
-
Lumbar strain/sprain
-
Degenerative disc disease
-
Spondylolysis/spondylolisthesis
-
Facet syndrome
-
Lumbar fractures are not uncommon with sports injuries.
-
The most benign of these are compression
fractures, noted by mild anterior wedging of the anterior vertebral
body. By definition, they do not involve the posterior vertebral body
and are stable fractures. -
Importantly, flexion-distraction
(seatbelt type) injury should be ruled out, because this is inherently
unstable and most often surgically stabilized. -
Simple compression fractures
are typically treated nonoperatively with a brace for 6 to 12 weeks. An
athlete can return to play after negative flexion-extension films,
resolution of pain, and full restoration of range of motion. -
Burst fractures are higher-energy injuries that can present with or without a neurological deficit and may be stable or unstable.
-
The fracture involves the posterior vertebral body and typically has canal compromise from retropulsed bone fragments.
-
Nonoperative treatment can include a
custom-molded thoracolumbar orthosis or extension cast for 12 weeks.
Our criteria for nonoperative treatment include:-
No neurological deficit.
-
Intact posterior ligaments (suggested by
<25 degrees kyphosis, no interspinous process widening, no facet
joint gapping, and confirmed by MRI inspection of the ligaments).
-
-
Patients with evidence of posterior
ligament injury but no neurological deficit can usually be treated by
posterior fixation alone (e.g., pedicle screw stabilization).-
We prefer to perform an anterior
decompression and reconstruction for those patients with a neural
deficit associated with retropulsed bone. Supplemental posterior
stabilization may also be considered.
-
-
Returning to play after treatment for a
burst fracture is controversial. There are little to no data of any
established criteria.-
In our practice, return to play criteria after nonoperative treatment is similar to those described for compression fractures.
-
After surgical treatment of a burst fracture, most physicians would probably not recommend return to contact sports.
-
-
-
Cauda equina syndrome (CES) is most commonly associated with a large lumbar disc herniation.
-
The clinical signs and symptoms of CES are:
-
Saddle anesthesia (inner thighs and perineum)
-
Bowel/bladder incontinence
-
Variable lower extremity sensory and/or motor deficit
-
-
The treatment of CES is surgical discectomy and is best performed within 48 hours from the onset of symptoms.
-
The most common cause for low back pain in athletes is a lumbar strain (muscular) or sprain (ligamentous).
-
They are caused by a subcatastrophic
stretch of the muscle or ligament fibers and usually result in
self-limited pain. In some cases, pain can become chronic. -
A strain is associated with paraspinal
muscle tenderness and sometimes a “trigger point” spasm, whereas a
sprain demonstrates tenderness localized to the interspinous process
region. -
Treatment of both sprains and strains
includes a short (1 to 2 days) period of rest, ice, and then a
stretching program directed by a trainer or physical therapist. -
Return to play after a strain or sprain
is allowed once the pain has subsided and range of motion and endurance
have been restored.
-
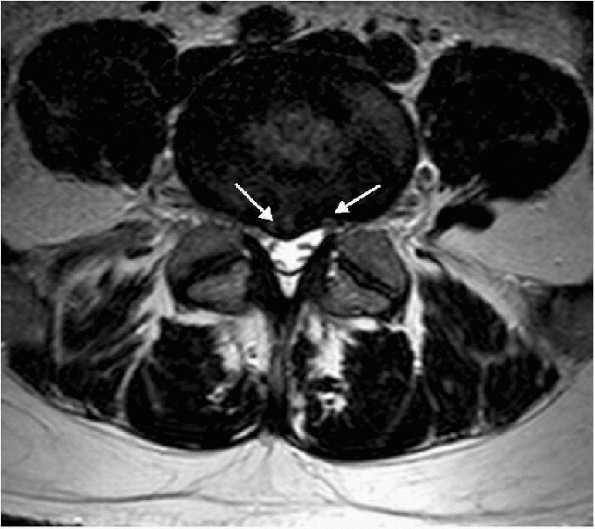
The link between degenerative disc
disease (DDD) and low back pain is still unclear, although it is
commonly believed that inflammatory factors within the nucleus leak out
through annular tears (Fig. 8-1) to stimulate
nociceptive nerve endings within the annulus and dorsal root ganglion.
This is because radiographic studies have detected high rates of DDD
and other degenerative abnormalities in asymptomatic patients. -
Compared with nonathletes, competitive athletes have a higher rate of degenerative changes in their lumbar spines.
-
Gymnasts, weight lifters, and football players are among the most at-risk athletes.
-
While competing, athletes appear to have
a higher rate of low back pain than nonathletes; however, once retired,
past participation in sports does not seem to be a substantial risk
factor.
-
-
DDD is irreversible. Treatment is
directed toward decreasing the intensity and frequency of symptoms,
thus improving lumbar mechanics and muscle physiology.-
In most cases, a carefully planned and executed physical therapy program is effective.
-
-
After treatment, the authors’ return-to-play criteria are:
-
Full painless range of motion
-
Ability to maintain a neutral posture during sports-specific exercises
-
Full muscle strength, endurance, and control
-
-
In the rare cases that nonoperative treatment fails, an interbody fusion with or without stabilization can be performed.
-
Return to play after lumbar fusion is
controversial because clear criteria have not been established. We have
a minimum requirement of solid radiographic fusion, in addition to
those criteria outlined previously for nonoperative treatment.
-
 |
|
Figure 8-1 Axial T2-weighted MRI image of an athlete with severe low back pain and no radicular symptoms. Note the annular fissuring (white arrows),
which are thought to allow inflammatory factors from the degenerated nucleus pulposus to “leak out” and stimulate nociceptive nerve endings in the posterior annulus. |
-
Stress fractures are common in athletes.
The most common region of the spine to be affected is the pars
interarticularis of the L5 (and less commonly L4) vertebra. -
This is termed spondylolysis and can be a frank, nonhealed fracture or a stress “reaction” that can only be noted on an MRI or bone scan.
-
Importantly, an adolescent athlete with
substantial back pain longer than 3 weeks should be evaluated with
plain lumbar radiographs and a bone scan, or a single-photon emission
computed tomography scan.-
A retrospective study comparing 100
adolescent athletes and 100 adults with acute low back pain showed that
47% of the adolescent athletes had spondylolysis, compared with only 5%
in the adult subjects. -
The presence and grade of spondylolysis/spondylolisthesis can influence the decision to allow return to play.
-
-
The prevalence of spondylolysis varies
from sport to sport and is highest in sports that require frequent or
sustained lumbar hyperextension maneuvers, such as diving (43%),
wrestling (30%), weight lifting (23%), throwing sports (27%), and
gymnastics (17%). -
Symptoms are localized to the low back, although referred pain to the buttocks or upper thighs is not uncommon.
-
Pain is exacerbated by hyperextension and relieved by flexing or squatting down.
-
A single-leg hyperextension test can be useful in determining whether one or both sides have symptoms.
-
Eighty-five percent of defects are detectable on a lateral lumbar film.
-
CT is the most sensitive modality for
detecting an established defect. Single-photon emission computed
tomography scan is the most sensitive method of detecting an occult
stress reaction.
-
-
Nonsurgical treatment of spondylolysis includes rest, brace immobilization, and pain control.
-
Medications include nonsteroidal anti-inflammatory drugs.
-
An antilordotic (Boston) brace (worn for up to 6 months) leads to resolution of symptoms in about 80% of cases.
-
Unilateral defects heal better than bilateral defects, though healing is not necessary for return to play.
-
Athletes can return to sports after nonoperative treatment of a pars defect if:
-
There is no pain with extension on examination.
-
The athlete remains pain-free after the brace is removed.
-
Functional restoration of endurance and range of motion has been achieved.
-
-
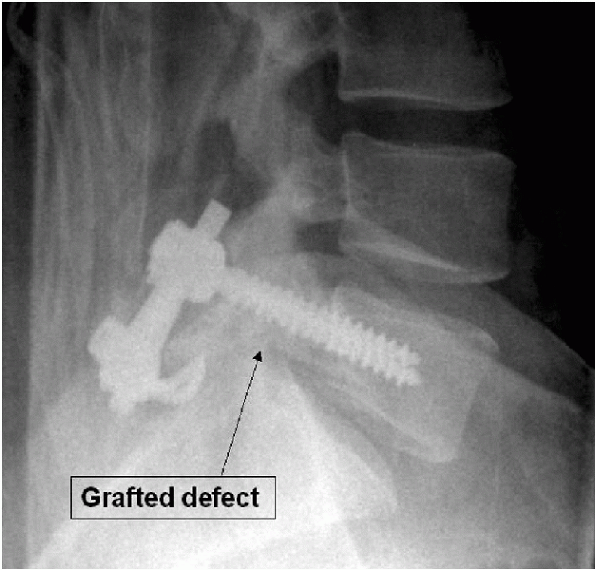
In recalcitrant cases, surgery might be
considered. Although a single-level fusion remains the current gold
standard, a pars defect repair may be considered in some cases (Fig. 8-2).
 |
|
Figure 8-2
Postoperative lateral radiograph of an athlete who underwent a pars repair instead of a lumbar fusion for recalcitrant pain from a spondylolytic defect of the L5 vertebra. |
-
Cervical spine injuries continue to make up a large percentage of spinal injuries in sports.
-
Injuries range from cervical sprains to catastrophic complete spinal cord injuries (SCIs).
-
An estimated 10% to 15% of football players experience an injury to the cervical spine.
-
The overall incidence of SCI in the high
school and college populations is around 1 in 100,000. Most are
incomplete with preservation of varying degrees of neurologic function. -
In an analysis of football players from
1977 to 1989, catastrophic SCIs were secondary to fracture dislocations
or anterior compression (burst) fractures in 33% and 22% of cases,
respectively.
-
-
Preexisting spinal stenosis predisposes
to SCI; in such cases, athletes can sustain cord injury without bony or
ligamentous disruption. -
The mechanism of injury is often direct axial load.
-
Particularly in football players, the
cervical spine is flexed (which straightens it from its usual lordotic
posture) on impact. This decreases its ability to dissipate the load.
With increasing loads, the spine fails in flexion, thus resulting in
vertebral body comminution (subluxation) of facet joint dislocation. -
Experimentally, Maiman et al.
found the average axial load to failure to be less with a straightened
versus normolordotic posture. The greatest force applied to the spine
was found when the load was applied to the vertex of the skull. This
decreased as the load was moved forward on the skull. -
Torg et al.
described the “spear tackler’s spine.” It occurs in athletes who use
improper tackling technique, using the top of their football helmet to
hit an opposing player head-on.-
This is associated with an increased risk for permanent neurologic damage.
-
Affected athletes demonstrate narrowing
of the cervical spinal canal, persistent straightening or reversal of
the normal lordotic curve, and concomitant preexisting posttraumatic
roentgenographic abnormalities of the cervical spine. -
Although axial loads combined with
flexion cause the majority of fracture dislocations of the cervical
spine, other mechanisms can cause injuries as well.
-
-
Rotation, extension, and shear forces
alone or in combination have been implicated in various fracture
patterns observed in the cervical spine. -
Although the multiple fractures
experienced by athletes participating in contact sports such as
football are beyond the scope of this chapter, they have led to the
National Collegiate Athletic Association (NCAA) Football Rule Committee
outlawing the use of one’s helmet to tackle an opponent.
-
-
Contact sports such as football, rugby, and wrestling place patients at high risk for injury.
-
Most cervical spine injuries in football
players result from hyperflexion, but other mechanisms—including
hyperextension, rotation, and lateral bending—have been reported. -
Wrestlers commonly exhibit neck
hyperflexion but also may endure rotational and horizontal shearing
forces that place great stresses on the intervertebral disks, facet
joints, and spinal ligaments.
-
-
SCI has also been documented in noncontact sports, such as diving, surfing, and gymnastics.
-
These events usually result from the
individual striking his/her head at the bottom of the pool or body of
water, thus causing neck hyperflexion. -
Gymnasts may sustain injuries after “missed” maneuvers that result in an uncontrolled fall.
-
-
A player may be permitted to return to play after treatment of a cervical fracture in the following situations:
-
The fracture is fully healed, and there is normal alignment.
-
A single-level fusion has been performed below the level of C2.
-
There is no residual canal compromise.
-
There is no pain or neural deficit.
-
There is no instability or olisthesis on flexion-extension films.
-
-
A player may not be permitted to return to play in the following cases:
-
The fracture is healed in a kyphotic posture.
-
A multilevel (2 or more) fusion has been performed.
-
C1-C2 fusion has been performed.
-
Rotatory instability is present.
-
There is residual canal compromise.
-
A residual neural deficit exists.
-
Pain persists.
-
There is evidence of instability on flexion-extension films.
-
-
Neurapraxia of the cervical cord, otherwise known as transient quadriplegia, is fairly common in contact sports participants.
-
It is characterized by bilateral burning pain, tingling, and loss of sensation in the upper and/or lower extremities.
-
Burning dysesthesias and paresthesias usually occur in a glove-like distribution.
-
Motor deficits can vary from mild weakness to total paralysis, depending on the extent of insult to the spinal cord.
-
-
By definition, symptoms are transient, and complete recovery usually occurs within 10 to 15 minutes but may take up to 48 hours.
-
Axial load with hyperextension or flexion
of the cervical spine is often the inciting event. A pincer mechanism
that theoretically causes a brief compression of the cord is thought to
play a role in the transient nature of the symptoms. -
Standard radiographic evaluation of the
cervical spine is usually negative for fractures or dislocations but
incidental findings—such as congenital stenosis, spondylosis,
P.101Klippel-Feil syndrome, or evidence of intervertebral disk disease—may be present.
-
Preexisting cervical stenosis may be a predisposing factor.
-
-
Reversible MRI spinal cord signal abnormalities have been documented.
-
The decision to allow an athlete to return to play after an episode of transient quadriplegia is controversial.
-
Torg et al. have held that an athlete may play after one or two episodes, provided there is full neurologic recovery.
-
Others are more reluctant, recommending
no play after just one episode, particularly if there is any underlying
spinal canal stenosis. -
From this, the term functional stenosis
has arisen, which denotes loss of the cerebrospinal fluid space
anterior and posterior to the spinal cord on a midsagittal MRI (Fig. 8-3), has been used as a contraindication to return to play.
-
-
Burner syndrome is one of the most common
injuries in contact sports. The “burner” or “stinger” was named after
the pain, tingling, and burning experienced in the upper extremity of
the athlete after contact. -
These injuries usually occur after the athlete strikes his head against another player, a wall, or a mat.
-
The athlete experiences sudden pain,
burning, and sometimes tingling that begins in the neck, radiates into
the shoulder, and continues down the arm and into the hand. -
Symptoms do not follow a dermatomal
pattern. Weakness of the supraspinatus, infraspinatus, deltoid, and
biceps muscle are often noted, which usually presents hours to days
after the injury.
-
-
Burners are a type of brachial plexus
injury, usually resulting from traction to the brachial plexus or
compression of the cervical root at the intervertebral foramen. Direct
impact to the plexus within the supraclavicular region has also been
reported.-
Traction injuries can occur with
tackling. This causes sudden lateral deviation of the head away from
the affected side and simultaneous depression of the ipsilateral
shoulder.-
These injuries are more frequent in high school athletes, possibly because of less developed supportive neck musculature.
-
-
Cervical root compression occurs at the
level of the intervertebral foramen. The foramen is dynamically
narrowed during activities that cause cervical spinal extension,
compression, and rotation toward the symptomatic side.-
These injuries are more commonly seen in
collegiate or professional athletes and present with more neck pain and
diminished range of motion than the patients with traction injuries.
-
-
Direct trauma to the supraclavicular region at Erb’s point can produce Burner syndrome with upper trunk deficits predominating.
-
Spurling’s test (lateral flexion and
rotation of the head toward the symptomatic side) is used to evaluate
compression-type injuries, whereas the brachial plexus stretch test
(lateral flexion away from the symptomatic side) can be used to
evaluate tractiontype injuries.
-
-
Central cervical canal and foraminal
stenosis are reported as risk factors for recurrent burners. Logically,
this association has been described for compression and extension-type
injuries but not traction mechanisms.-
Athletes with a history of recurrent
burners, associated DDD, or congenital stenosis should abstain from
participation in contact sports.
-
-
The physician must determine whether
symptoms are from cervical cord or root pathology. This important
distinction is often made on the playing field.-
By definition, burners present with unilateral arm symptoms.
-
Athletes who present with bilateral upper or any lower extremity symptoms are more likely to have had a more serious SCI.
-
Focal neck tenderness or severe pain with
motion should raise suspicion of a fracture or ligamentous injury to
the cervical spine.-
In these cases, the spine should be
immobilized using a collar and backboard, and the patient transported
to a hospital for immediate imaging. -
Burners are self-limited syndromes that
usually do not cause permanent sequelae. Even with this favorable
natural history, certain restrictions should be placed on athletes
after sustaining these injuries to prevent more severe problems in the
future.
-
-
Athletes should also be started on
year-round trapezial strengthening programs. Theoretically,
strengthening the neck musculature may increase the shock-absorbing
capacity of the cervical spine. -
Athletes must fulfill particular criteria before they can return to play:
-
Complete resolution of paresthesias
-
Full range of motion of the neck
-
No pain
-
Negative Lhermitte’s test (axial compression of head results in electric-like sensation down to the lower back)
-
Normal strength
-
-
-
Athletes who are prone to burners can use special equipment to help prevent injuries.
-
Commonly used devices are thicker
shoulder pads, neck rolls, springs, and the “cowboy collar.” They must
fit correctly and be used with properly fitting shoulder pads to be
effective.
-
-
Educating participants about proper
athletic technique is also important. Proper tackling and blocking
techniques, with avoidance of spearing, should be taught to young
football players as they are first learning the sport.
 |
|
Figure 8-3 A sagittal T2-weighted
MRI of an athlete with functional stenosis, noted by complete effacement (or loss) of cerebrospinal fluid anterior and posterior to the spinal cord. This is thought to increase the risk for SCI with athletic trauma to the neck. |
-
Neck pain, or the so-called “jammed neck,” is one of the most common complaints among athletes, especially football players.
-
Patients can sustain an injury to the
musculotendinous unit (sprain) or paraspinal muscle itself (strain).
Therefore, one sprains a tendon but strains a muscle. -
Typically, the athlete will present with localized neck pain without radiation to the arms or back.
-
Athletes may have decreased cervical range of motion secondary to pain.
-
Sometimes the pain may be localized to one specific cervical level.
-
There are no neurologic deficits.
-
-
Treatment is based on severity and etiology.
-
Generally, the use of a cervical collar and analgesic medications is continued until pain and spasm subsides.
-
After the collar is removed, range-of-motion exercises can begin.
-
Return to athletic participation is delayed until painless full range of motion is achieved.
-
Instability may necessitate surgical stabilization to prevent future neurologic injury.
-
-
Acute disc herniations in contact sports are rare.
-
Head-on collisions or other events
leading to axial loading can result in increased intradiscal pressure.
If large enough, cord compression can manifest as either transient or
permanent quadriplegia or quadriparesis. Patients may present with
acute paralysis of all four extremities, as well as loss of pain and
temperature sensation.-
Patients may also present with anterior cord syndrome. However, acute radicular symptoms can occur alone.
-
-
MRI is the study of choice to detect a herniated disc.
-
Patients with persistent clinical and
radiological evidence of spinal cord compression should be offered
surgery, which may include anterior cervical diskectomy and interbody
fusion. -
Radiographic evaluation of the cervical spine of football players can reveal asymptomatic cervical spondylosis.
-
In one study, 7% of freshman college football players demonstrated abnormally narrowed disk spaces.
-
Early degenerative changes have been attributed to years of repetitive loading from tackling.
-
Severe degenerative changes—including
foraminal stenosis, central canal stenosis resulting from posterior
osteophytes, and the loss of normal cervical lordosis—can result in the
classic “spear tacklers spine.”
-
-
Contraindications to returning to play after a cervical disc herniation are:
-
Presence of pain (axial neck or radicular)
-
Neural deficit
-
Limitation of range of motion
-
Any evidence of myelopathy (walking imbalance, hyperreflexia, pathological reflexes) (e.g., Hoffmann’s or inverted radial reflex)
-
-
Narrowing or stenosis of the cervical spinal canal can predispose athletes to SCI.
-
Two forms of cervical stenosis have been described in athletes: developmental and acquired.
-
Developmental stenosis,
otherwise known as congenital stenosis, is present at birth and is
characterized by shortened pedicles causing an abnormally narrow canal,
sometimes described as funnel-shaped. -
Acquired stenosis
is the result of reactive bony thickening and ligamentous hypertrophy
that can result from repeated collisions in sports over time. Other
pathoanatomic features include disc bulges, spondylolysis, and
osteophytes.
-
-
Methods for diagnosing and quantifying cervical stenosis have been suggested.
-
Sagittal canal diameter is measured on a
standard lateral cervical spine radiograph. The measurement is recorded
as the anteroposterior distance between the posterior aspect of the
vertebral body and the nearest point along on the spinolaminar junction.-
Wolfe et al. established normal parameters for this dimension.
-
The average diameters at C1, C2, and
C3-C7 were 22 mm, 20 mm, and 17 mm, respectively. Sagittal canal
diameters of more than 15 mm were established as normal, and diameters
of less than 13 mm were defined as stenotic.
-
-
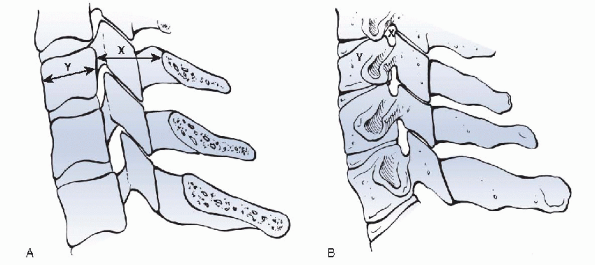
Taking different vertebral sizes into account, Torg et al.
derived a ratio of the anteroposterior canal diameter to the
anteroposterior vertebral body diameter. A value below 0.8 was defined
as spinal stenosis (Fig. 8-4).-
Herzog et al.
have questioned the reliability of the Torg ratio, finding it to have a
high sensitivity but a poor positive predictive value for detecting
clinically significant cervical narrowing. -
Studies that have evaluated the cervical
spines of clinically asymptomatic professional football players showed
abnormal Torg ratios in 33% to 49%. -
The high incidence of these abnormally
low ratios is the result of the large vertebral body size in this
population, with absolute dimensions of the spinal canal being
adequately capacious for the spinal cord. -
MRI evaluation of these players revealed adequate space available for the cord in these athletes and thus no true stenosis.
-
Currently, evaluation for functional spinal stenosis, with either MRI or CT myelogram, is becoming the new standard.
-
-
Functional spinal stenosis is defined as obliteration of the cerebrospinal fluid cushion surrounding the cervical spinal cord.
-
This method of evaluation is being used
by many team physicians for decision making regarding athletes’ return
to play, as well as treatment and activity modifications.
-
 |
|
Figure 8-4 The Torg ratio is calculated by dividing the sagittal diameter of the vertebral canal (X) by the diameter of the vertebral body (Y).
|
-
Congenital anomalies of the cervical
spine can predispose an athlete to spinal injuries by changing the
mechanics and load dissipating properties of the cervical spine. -
Congenital anomalies can occur by failure of formation or segmentation.
-
Klippel-Feil syndrome is secondary to failure of segmentation that may involve one or more motion segments.
-
Torg and Glasgow classified Klippel-Feil syndrome into two types:
-
Type I involves a long congenital fusion (more than two segments).
-
Type II has one or two fused segments.
-
-
As the number of fused segments
increases, the ability of the cervical spine to dissipate loads
decreases. More force is concentrated on the unfused motion segments,
increasing the chance for injury in these regions with contact sports.
-
-
Failure of formation can present as odontoid agenesis, hypoplasia, or os odontoideum.
-
These can result in atlantoaxial instability, which places athletes participating in contact sports at great risk for SCI.
-
-
In some instances, an athlete can have failure of formation of the atlanto-occipital junction.
-
These individuals are prone to experience
compression of the posterior columns of the spinal cord at the
posterior margin of the foramen magnum and should be restricted from
contact sports.
-
-
Spina bifida occulta is another congenital anomaly. It is usually an incidental finding and is asymptomatic.
-
It should not usually hinder participation in athletics.
-
-
On-field examination of a suspected head
injury should include pupillary examination and an assessment of the
level of consciousness.-
The Glasgow Coma Scale is a useful measurement.
-
-
In cases of athletic head injuries,
treatment should include immediate immobilization (as described
previously for cervical spine injuries) and removal of the facemask,
leaving the helmet in place.-
Trendelenburg (head lower than body/heart) hypotonic intravenous fluids are contraindicated because they can cause further increases in intracerebral pressure.
-
-
Among all sports, teenage football is associated with the highest risk of head injury. Between 75% and 85% are concussions.
-
A concussion is caused by temporary diminished cerebral blood flow after an impact.
-
In 90% of cases, there is no loss of consciousness, thus making diagnosis difficult.
-
After having one concussion, an athlete is at four times the risk for another one.
-
Tables 7-2 and 7-4 in Chapter 7 cover grading and management of concussions.
-
-
The concept of the second impact syndrome is important to understand. This refers to a minor second injury after an incomplete recovery from a previous head injury.
-
This can lead to massive intracerebral hypertension.
-
Mortality has been reported in about 50% of cases because patients can die without any prodromal loss of consciousness.
-
Second impact syndrome is associated with
a 100% rate of permanent neurological sequelae. This highlights the
importance of understanding the criteria for return to play after
athletic concussions.
-
P, Zurakowski D, Kriemler S, et al. Spondylolysis: returning the
athlete to sports participation with brace treatment. Orthopedics
2002;25;653-657.
JA, Carras R, Hyman RA, et al. Cervical myelopathy caused by
developmental stenosis of the spinal canal. J Neurosurg 1979;
51:362-367.
RJ, Wiens JJ, Dillingham MF, et al. Normal cervical spine morphometry
and cervical spinal stenosis in asymptomatic professional football
players: plain film radiography, multiplanar computed tomography, and
magnetic resonance imaging. Spine 1991; 16(suppl):S178-S186.
DJ, Sances A Jr, Myklebust JB, et al. Compression injuries of the
cervical spine: a biomechanical analysis. Neurosurgery 1983; 13:254-260.
SA, Schulte KR, Callaghan JJ, et al. Cervical spinal stenosis and
stingers in collegiate footfall players. Am J Sports Med 1994;
22:158-166.
JS, Pavlov H, Genuario SE, et al. Neurapraxia of the cervical spinal
cord with transient quadriplegia. J Bone Joint Surg Am 1986;
68:1354-1370.
JS, Truex RC Jr, Marshall J, et al. Spinal injury at the level of the
third and fourth cervical vertebrae from football. J Bone Joint Surg Am
1977;59-A:1015-1019.
JS, Truex R Jr, Quedenfeld TC, et al. The National Football Head and
Neck Registry: report and conclusions 1978. JAMA 1979;241: 1477-1479.
JS, Vegso JJ, O’Neill MJ, et al. The epidemiologic, pathologic,
biomechanical, and cinematographic analysis of football induced
cervical spine trauma. Am J Sports Med 1990;18:50-57.
BS, Khilnani M, Malis L. The sagittal diameter of the bony cervical
spinal canal and its significance in cervical spondylosis. J Mt Sinai
Hosp 1956;23:283-292.
