Popliteal Cyst in the Child
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Popliteal Cyst in the Child
Popliteal Cyst in the Child
Paul D. Sponseller MD
Description
Popliteal cyst is a painless soft-tissue mass in the medial popliteal fossa behind the knee.
Epidemiology
-
Most common soft-tissue lesion about the knee in children
-
Affects children 2–14 years old
Incidence
Incidence decreases after 9 years of age (1,2).
Prevalence
Twice as common in males (2)
Risk Factors
-
Most are isolated cases.
-
Juvenile rheumatoid arthritis
-
Other chronic inflammation of the knee
Genetics
No Mendelian pattern is known.
Etiology
-
Likely resulting from weakness in the
posterior knee joint capsule between the semimembranosus muscle and the
medial head of the gastrocnemius -
Rarely related to intra-articular lesions
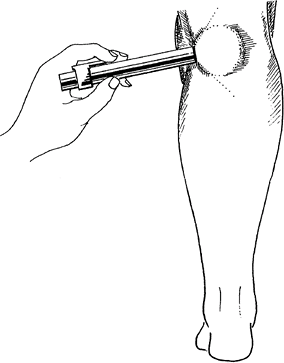 Fig. 1. A diagnosis of popliteal cyst in a child may be confirmed by transillumination.
Fig. 1. A diagnosis of popliteal cyst in a child may be confirmed by transillumination.
Signs and Symptoms
-
Protrusion between the medial gastrocnemius and semitendinosus muscles
-
Swelling of the medial side of the popliteal space just lateral to the semitendinosus muscle
-
Usually asymptomatic, but can cause discomfort and restrict ROM of knee if excessively enlarged
-
Usually waxes and wanes in size, depending on the child’s activity level
-
Typically present for some time before the child is brought to the physician
Physical Exam
-
Examine the affected lower limb for
swelling of the medial side of the popliteal space just medial to the
semimembranosus muscle. -
Compress the cyst to check for pain.
-
Usually painless
-
The remainder of the knee examination usually is normal.
-
-
Examine the gait.
-
No limp should be evident.
-
-
Transilluminate the cyst in a darkened room with a point light source (e.g., strong penlight) (Figs. 1 and 2).
-
With the patient prone, place the light source on the skin next to the area of swelling.
-
If the mass illuminates more strongly and
evenly than the surrounding fatty tissue, the fluid-filled nature of
cyst is confirmed, and a diagnosis of solid tumor is excluded.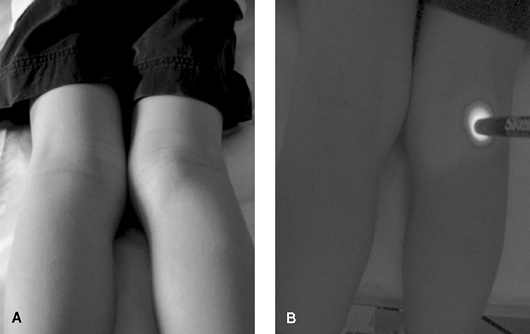 Fig. 2. Prone 7-year-old with popliteal cyst. A: External appearance of cyst. B: After transillumination. Note that the cyst picks up light remote from the source in comparison with surrounding tissues.
Fig. 2. Prone 7-year-old with popliteal cyst. A: External appearance of cyst. B: After transillumination. Note that the cyst picks up light remote from the source in comparison with surrounding tissues.
-
Tests
Lab
-
Aspiration is not commonly performed.
-
However, if the cyst is aspirated, the cyst fluid is clear and gelatinous.
-
If the cyst fluid is not clear and
gelatinous, send the aspirate for the following tests to rule out
septic arthritis or soft-tissue abscess:-
Cell count
-
Gram stain
-
Culture
-
-
Imaging
-
Plain-film radiography is optional to rule out bony disorder.
-
Duplex ultrasound and MRI (rarely indicated) characterize a questionable cyst further and rule out malignancy (3).
Pathological Findings
-
Synovial fluid–filled sac in the semimembranosus-gastrocnemius interval
-
Rarely related to intra-articular lesions
Differential Diagnosis
-
Malignant disease
-
Vascular anomaly
-
Soft-tissue abscess
P.337
General Measures
-
The patient’s activity may be restricted when the cyst is large.
-
Surgical excision may be necessary if the cyst is symptomatic (rare).
-
The recurrence rate after surgical excision is 20–40% (2).
-
-
No treatment is required if no intra-articular lesion is present.
-
Left untreated, 70% of cysts disappear spontaneously after months to years (they may wax and wane in size) (3,4).
-
-
If it is desired to confirm the diagnosis
and increase the chance of resolution, the cysts may be aspirated with
a large-bore needle, followed by immobilization for immediate
decompression.-
However, the recurrence rate is high.
-
Surgery
-
Excision of the cyst through a transverse incision in the posterior popliteal region:
-
May be done as an outpatient procedure
-
-
Immobilization for several weeks postoperatively
Complications
The rate of recurrence of the cyst after surgical treatment is ~20–40% (2).
Patient Monitoring
-
No routine follow-up is needed.
-
Instruct the parent to return if the lesion changes in symptoms or in character.
References
1. De Greef I, Molenaers G, Fabry G. Popliteal cysts in children: a retrospective study of 62 cases. Acta Orthop Belg 1998;64:180–183.
2. Willis
RB. Sports medicine in the growing child. Overuse injuries. In:
Morrissy RT, Weinstein SL, eds. Lovell and Winter’s Pediatric
Orthopaedics, 6th ed. Philadelphia: Lippincott Williams & Wilkins,
2006:1414–1421.
RB. Sports medicine in the growing child. Overuse injuries. In:
Morrissy RT, Weinstein SL, eds. Lovell and Winter’s Pediatric
Orthopaedics, 6th ed. Philadelphia: Lippincott Williams & Wilkins,
2006:1414–1421.
3. De
Maeseneer M, Debaere C, Desprechins B, et al. Popliteal cysts in
children: prevalence, appearance and associated findings at MR imaging.
Pediatr Radiol 1999;29:605–609.
Maeseneer M, Debaere C, Desprechins B, et al. Popliteal cysts in
children: prevalence, appearance and associated findings at MR imaging.
Pediatr Radiol 1999;29:605–609.
4. Seil R, Rupp S, Jochum P, et al. Prevalence of popliteal cysts in children. A sonographic study and review of the literature. Arch Orthop Trauma Surg 1999;119:73–75.
Codes
ICD9-CM
727.51 Popliteal cyst
Patient Teaching
-
Inform parents about the benign nature of the condition.
-
Explain the similarity of the pathologic process to that of the Baker cyst in adults.
-
Mention the lack of underlying knee disease and the absence of increased synovial fluid production.
FAQ
Q: Is MRI indicated for a popliteal cyst in a child?
A: Not unless the cyst is atypical and does not transilluminate, or separate symptoms are referable to the knee.
Q: Is follow-up needed?
A: If it is a typical cyst, no follow-up is needed unless symptoms develop.
