Ankle Fractures
-
Population-based studies suggest that the incidence of ankle fractures has increased dramatically since the early 1960s.
-
The highest incidence of ankle fractures occurs in elderly women.
-
Most ankle fractures are isolated
malleolar fractures, accounting for two-thirds of fractures, with
bimalleolar fractures occurring in one-fourth of patients and
trimalleolar fractures occurring in the remaining 5% to 10%. -
Open fractures are rare, accounting for just 2% of all ankle fractures.
-
Increased body mass index is considered a risk factor for sustaining an ankle fracture.
-
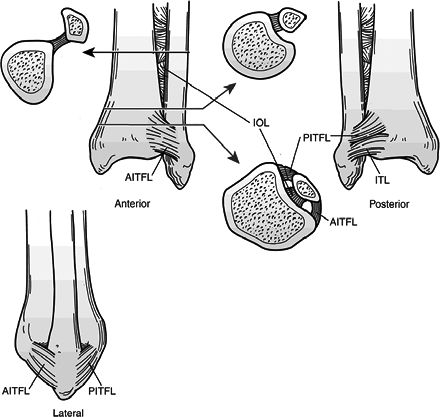
The ankle is a complex hinge joint
composed of articulations among the fibula, tibia, and talus in close
association with a complex ligamentous system (Fig. 38.1). -
The distal tibial articular surface is
referred to as the “plafond,” which, together with the medial and
lateral malleoli, forms the mortise, a constrained articulation with
the talar dome. -
The plafond is concave in the
anteroposterior (AP) plane but convex in the lateral plane. It is wider
anteriorly to allow for congruency with the wedge-shaped talus. This
provides for intrinsic stability, especially in weight bearing. -
The talar dome is trapezoidal, with the
anterior aspect 2.5 mm wider than the posterior talus. The body of the
talus is almost entirely covered by articular cartilage. -
The medial malleolus articulates with the
medial facet of the talus and divides into an anterior colliculus and a
posterior colliculus, which serve as attachments for the superficial
and deep deltoid ligaments, respectively. -
The lateral malleolus represents the
distal aspect of the fibula and provides lateral support to the ankle.
No articular surface exists between the distal tibia and fibula,
although there is some motion between the two. Some intrinsic stability
is provided between the distal tibia and fibula just proximal to the
ankle where the fibula sits between a broad anterior tubercle and a
smaller posterior tubercle of the tibia. The distal fibula has
articular cartilage on its medial aspect extending from the level of
the plafond distally to a point halfway down its remaining length. -
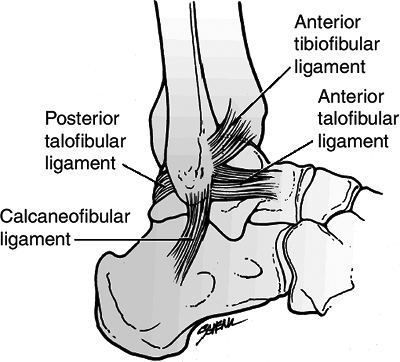
The syndesmotic ligament complex exists
between the distal tibia and fibula, resisting axial, rotational, and
translational forces to maintain the structural integrity of the
mortise. It is composed of four ligaments, including:-
Anterior inferior tibiofibular ligament.
-
Posterior inferior tibiofibular ligament. This is thicker and stronger than the anterior counterpart. Therefore, torsional
P.399
or translational forces that rupture the anterior tibiofibular ligament
may cause an avulsion fracture of the posterior tibial tubercle,
leaving the posterior tibiofibular ligament intact.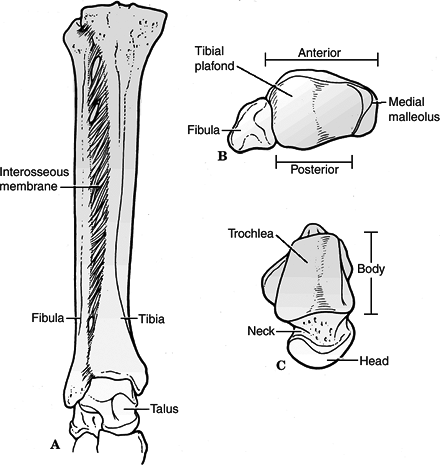 Figure
Figure
38.1. Bony anatomy of the ankle. Mortise view (A), inferior superior
view of the tibiofibular side of the joint (B), and superior inferior
view of the talus (C). The ankle joint is a three-bone joint with a
larger talar articular surface than matching tibiofibular articular
surface. The lateral circumference of the talar dome is larger than the
medial circumference. The dome is wider anteriorly than posteriorly.
The syndesmotic ligaments allow widening of the joint with dorsiflexion
of the ankle, into a stable, close-packed position.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Transverse tibiofibular ligament (inferior to posterior tibiofibular).
-
Interosseous ligament (distal continuation of the interosseous membrane) (Fig. 38.2).
-
-
The deltoid ligament provides ligamentous
support to the medial aspect of the ankle. It is separated into
superficial and deep components (Fig. 38.3):P.400-
Superficial portion: This is composed of
three ligaments that originate on the anterior colliculus but add
little to ankle stability.![]() Figure
Figure
38.2. Three views of the tibiofibular syndesmotic ligaments.
Anteriorly, the anterior inferior tibiofibular ligament (AITFL) spans
from the anterior tubercle and anterolateral surface of the tibia to
the anterior fibula. Posteriorly, the tibiofibular ligament has two
components: the superficial posterior inferior tibiofibular ligament
(PITFL), which is attached from the fibula across to the posterior
tibia, and the thick, strong inferior transverse ligament (ITL), which
constitutes the posterior labrum of the ankle. Between the anterior and
posterior inferior talofibular ligaments resides the stout interosseous
ligament (IOL).(Adapted from Browner B, Jupiter J, Levine A, eds. Skeletal Trauma: Fractures, Dislocations, and Ligamentous Injuries, 2nd ed. Philadelphia: WB Saunders, 1997.) -
Tibionavicular ligament: This suspends the spring ligament and prevents inward displacement of the talar head.
-
Tibiocalcaneal ligament: This prevents valgus displacement.
-
Superficial tibiotalar ligament.
-
Deep portion: This intraarticular
ligament (deep tibiotalar) originates on the intercollicular grove and
the posterior colliculus of the distal tibia and inserts on the entire
nonarticular medial surface of the talus. Its fibers are transversely
oriented; it is the primary medial stabilizer against lateral
displacement of the talus.
-
-
The fibular collateral ligament is made up of three ligaments that, together with the distal fibula, provide lateral support
P.401
to the ankle. The lateral ligamentous complex is not as strong as the medial complex (Fig. 38.4).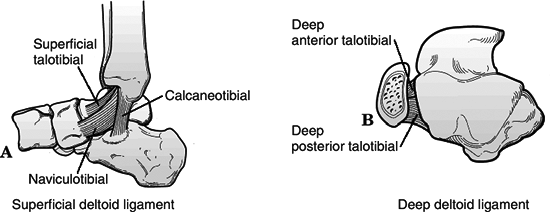 Figure
Figure
38.3. Medial collateral ligaments of the ankle. Sagittal plane (A) and
transverse plane (B) views. The deltoid ligament includes a superficial
component and a deep component. Superficial fibers mostly arise from
the anterior colliculus and attach broadly from the navicular across
the talus and into the medial border of the sustentaculum tali and the
posterior medial talar tubercle. The deep layer of the deltoid ligament
originates from the anterior and posterior colliculi and inserts on the
medial surface of the talus.(Adapted from Browner B, Jupiter J, Levine A, eds. Skeletal Trauma: Fractures, Dislocations, and Ligamentous Injuries, 2nd ed. Philadelphia: WB Saunders, 1997.)-
Anterior talofibular ligament: This is
the weakest of the lateral ligaments; it prevents anterior subluxation
of the talus primarily in plantar flexion. -
Posterior talofibular ligament: This is
the strongest of the lateral ligaments; it prevents posterior and
rotatory subluxation of the talus.![]() Figure 38.4. Lateral collateral ligaments of the ankle and the anterior syndesmotic ligament.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 38.4. Lateral collateral ligaments of the ankle and the anterior syndesmotic ligament.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Calcaneofibular ligament: This is lax in
neutral dorsiflexion owing to relative valgus orientation of calcaneus;
it stabilizes the subtalar joint and limits inversion; rupture of this
ligament will cause a positive talar tilt test.
P.402 -
-
Biomechanics
-
The normal range of motion (ROM) of the
ankle in dorsiflexion is 30 degrees, and in plantar flexion it is 45
degrees; motion analysis studies reveal that a minimum of 10 degrees of
dorsiflexion and 20 degrees of plantar flexion are required for normal
gait. -
The axis of flexion of the ankle runs
between the distal aspect of the two malleoli, which is externally
rotated 20 degrees compared with the knee axis. -
A lateral talar shift of 1 mm will decrease surface contact by 40%; a 3-mm shift results in >60% decrease.
-
Disruption of the syndesmotic ligaments
may result in decreased tibiofibular overlap. Syndesmotic disruption
associated with fibula fracture may be associated with a 2- to 3-mm
lateral talar shift even with an intact deep deltoid ligament. Further
lateral talar shift implies medial compromise.
-
including mechanism (axial versus rotational loading), chronicity
(recurrent ankle instability may result in chronic ligamentous laxity
and distorted ankle biomechanics), patient age, bone quality, position
of the foot at time of injury, and the magnitude, direction, and rate
of loading. Specific mechanisms and injuries are discussed in the
section on classification.
-
Patients may have a variable
presentation, ranging from a limp to nonambulatory in significant pain
and discomfort, with swelling, tenderness, and variable deformity. -
Neurovascular status should be carefully documented and compared with the contralateral side.
-
The extent of soft tissue injury should
be evaluated, with particular attention to possible open injuries and
blistering. The quality of surrounding tissues should also be noted. -
The entire length of the fibula should be
palpated for tenderness, because associated fibular fractures may be
found proximally as high as the proximal tibiofibular articulation. A
“squeeze test” may be performed approximately 5 cm proximal to the
intermalleolar axis to assess possible syndesmotic injury. -
A dislocated ankle should be reduced and
splinted immediately (before radiographs if clinically evident) to
prevent pressure or impaction injuries to the talar dome and to
preserve neurovascular integrity.
-
AP, lateral, and mortise views of the ankle should be obtained.
-
AP view
-
Tibiofibula overlap of <10 mm is abnormal and implies syndesmotic injury.
-
Tibiofibula clear space of >5 mm is abnormal and implies syndesmotic injury.
-
Talar tilt: A difference in width of the
medial and lateral aspects of the superior joint space of >2 mm is
abnormal and indicates medial or lateral disruption.
P.403 -
-
Lateral view
-
The dome of the talus should be centered under the tibia and congruous with the tibial plafond.
-
Posterior tibial tuberosity fractures can be identified, as well as direction of fibular injury.
-
Avulsion fractures of the talus by the anterior capsule may be identified.
-
-
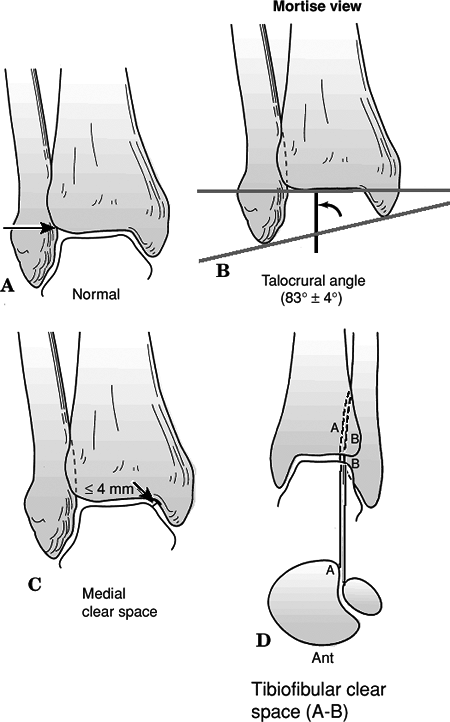
Mortise view (Fig. 38.5)
-
This is taken with the foot in 15 to 20 degrees of internal rotation to offset the intermalleolar axis.
-
A medial clear space >4 to 5 mm is abnormal and indicates lateral talar shift.
-
Talocrural angle: The angle subtended
between the intermalleolar line and a line parallel to the distal
tibial articular surface should be between 8 and 15 degrees. The angle
should be within 2 to 3 degrees of the uninjured ankle. -
Tibiofibular overlap <1 cm indicates syndesmotic disruption.
-
Talar shift >1 mm is abnormal.
-
-
A physician-assisted stress view with the
ankle dorsiflexed and the foot stressed in external rotation can be
used to identify medial injury with an isolated fibula fracture. -
Computed tomography (CT) scans help to delineate bony anatomy, especially in patients with plafond injuries.
-
Magnetic resonance imaging (MRI) may be used for assessing occult cartilaginous, ligamentous, or tendinous injuries.
-
Bone scan is useful in chronic ankle
injuries, such as osteochondral injuries, stress fractures, infection,
or reflex dystrophies.
-
Four patterns are recognized, based on “pure” injury sequences, each subdivided into stages of increasing severity.
-
This system is based on cadaveric studies.
-
Patterns may not always reflect clinical reality.
-
The system takes into account (1) the position of the foot at the time of injury and (2) the direction of the deforming force.
-
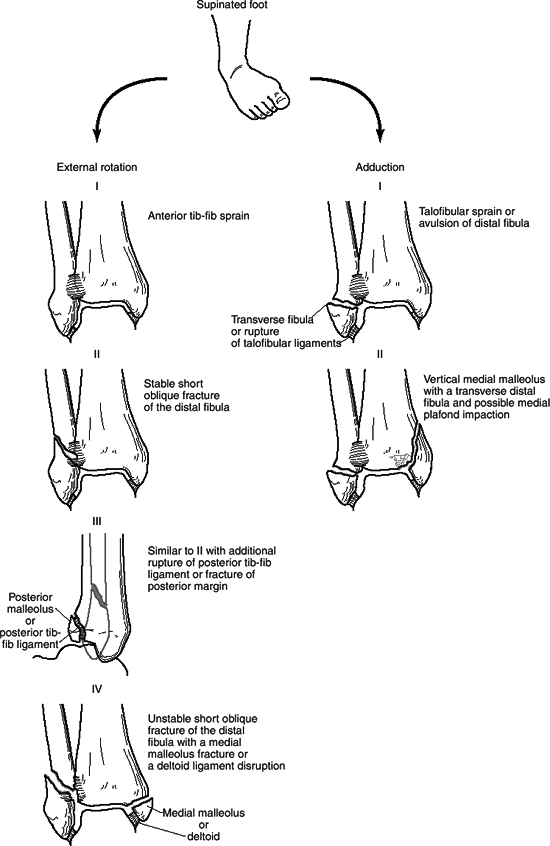
This accounts for 10% to 20% of malleolar fractures.
-
This is the only type associated with medial displacement of the talus.
| Stage I: | Produces either a transverse avulsion-type fracture of the fibula distal to the level of the joint or a rupture of the lateral collateral ligaments |
| Stage II: | Results in a vertical medial malleolus fracture |
-
This accounts for 40% to 75% of malleolar fractures.
| Stage I: | Produces disruption of the anterior tibiofibular ligament with or without an associated avulsion fracture at its tibial or fibular attachment |
| Stage II: | Results in the typical spiral fracture of the distal fibula, which runs from anteroinferior to posterosuperior |
| Stage III: | Produces either a disruption of the posterior tibiofibular ligament or a fracture of the posterior malleolus |
| Stage IV: | Produces either a transverse avulsion-type fracture of the medial malleolus or a rupture of the deltoid ligament |
 |
|
Figure
38.5. X-ray appearance of the normal ankle on mortise view. (A) The condensed subchondral bone should form a continuous line around the talus. (B) The talocrural angle should be approximately 83 degrees. When the opposite side can be used as a control, the talocrural angle of the injured side should be within a few degrees of the noninjured side. (C) The medial clear space should be equal to the superior clear space between the talus and the distal tibia and less than or equal to 4 mm on standard x-rays. (D) The distance between the medial wall of the fibula and the incisural surface of the tibia, the tibiofibular clear space, should be less than 6 mm. (A–C, Adapted from Browner B, Jupiter J, Levine A, eds. Skeletal Trauma: Fractures, Dislocations, and Ligamentous Injuries, 2nd ed. Philadelphia: WB Saunders, 1997; D, from Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
 |
|
Figure
38.6. Schematic diagram and case examples of Lauge-Hansen supination-external rotation and supination-adduction ankle fractures. A supinated foot sustains either an external rotation or adduction force and creates the successive stages of injury shown in the diagram. The supination-external rotation mechanism has four stages of injury, and the supination-adduction mechanism has two stages. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
 |
|
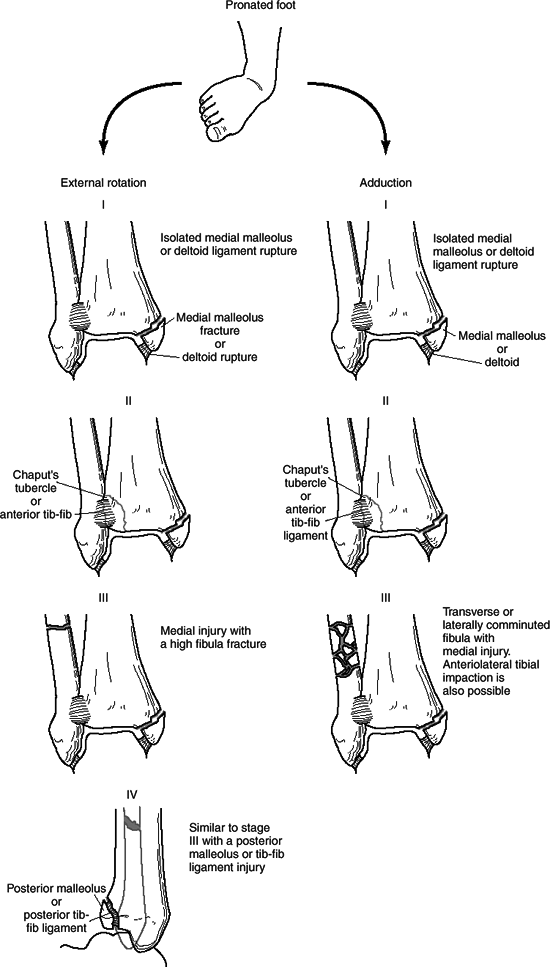
Figure
38.7. Schematic diagram and case examples of Lauge-Hansen pronation-external rotation and pronation-abduction ankle fractures. A pronated foot sustains either an external rotation or abduction force and creates the successive stages of injury shown in the diagram. The pronation-external rotation mechanism has four stages of injury, and the pronation-abduction mechanism has three stages. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
This accounts for 5% to 20% of malleolar fractures.
| Stage I: | Results in either a transverse fracture of the medial malleolus or a rupture of the deltoid ligament |
| Stage II: | Produces either a rupture of the syndesmotic ligaments or an avulsion fracture at their insertion sites |
| Stage III: | Produces a transverse or short oblique fracture of the distal fibula at or above the level of the syndesmosis; this results from a bending force that causes medial tension and lateral compression of the fibula, producing lateral comminution or a butterfly fragment |
-
This accounts for 5% to 20% of malleolus fractures.
| Stage I: | Produces either a transverse fracture of the medial malleolus or a rupture of the deltoid ligament |
| Stage II: | Results in disruption of the anterior tibiofibular ligament with or without avulsion fracture at its insertion sites |
| Stage III: | Results in a spiral fracture of the distal fibula at or above the level of the syndesmosis running from anterosuperior to posteroinferior |
| Stage IV: | Produces either a rupture of the posterior tibiofibular ligament or an avulsion fracture of the posterolateral tibia |
-
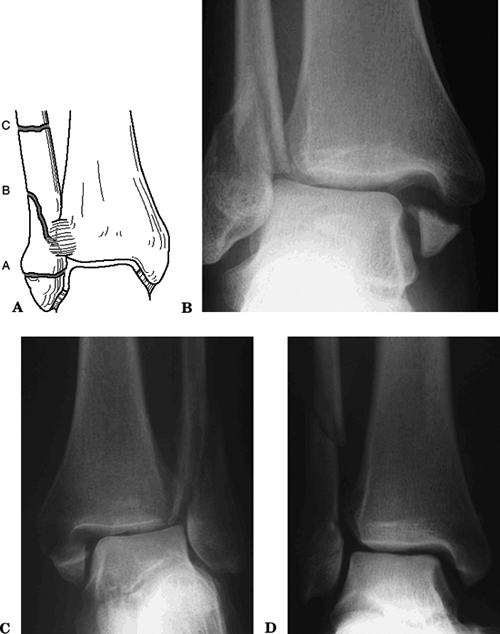
This is based on the level of the fibular
fracture: the more proximal, the greater the risk of syndesmotic
disruption and associated instability. Three types of fractures are
described:
| Type A: | This involves a fracture of the fibula below the level of the tibial plafond, an avulsion injury that results from supination of the foot and that may be associated with an oblique or vertical fracture of the medial malleolus. This is equivalent to the Lauge-Hansen supination-adduction injury. |
| Type B: | This oblique or spiral fracture of the fibula is caused by external rotation occurring at or near the level of the syndesmosis; 50% have an associated disruption of the anterior syndesmotic ligament, whereas the posterior syndesmotic ligament remains intact and attached to the distal fibular fragment. There may be an associated injury to the medial structures or the posterior malleolus. This is equivalent to the Lauge-Hansen supination-eversion injury. |
| Type C: | This involves a fracture of the fibula above the level of the syndesmosis causing disruption of the syndesmosis almost always with associated medial injury. This category includes Maisonneuve-type injuries and corresponds to Lauge-Hansen pronation-eversion or pronation-abduction Stage III injuries. |
 |
|
Figure 38.8. (A) Schematic diagram of the Danis-Weber classification of ankle fractures.
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
Maisonneuve fracture
-
Originally described as an ankle injury
with a fracture of the proximal third of the fibula, this is an
external rotation-type injury; it is important to distinguish it from
direct trauma fractures.
-
-
Curbstone fracture
-
This avulsion fracture off the posterior tibia is produced by a tripping mechanism.
-
-
LeForte-Wagstaffe fracture
-
This anterior fibular tubercle avulsion
fracture by the anterior tibiofibular ligament is usually associated
with Lauge-Hansen SER-type fracture patterns.
-
-
Tillaux-Chaput fracture
-
This avulsion of anterior tibial margin
by the anterior tibiofibular ligament is the tibial counterpart of the
LeForte-Wagstaffe fracture.
-
-
Collicular fractures
-
Anterior colliculus fracture: The deep portion of the deltoid may remain intact.
-
Posterior colliculus fracture: The
fragment is usually nondisplaced because of stabilization by the
posterior tibial and the flexor digitorum longus tendons; classically,
one sees a “supramalleolar spike” very clearly on an external rotation
view.
-
-
Chip avulsion
-
Small avulsions of either colliculus can be noted.
-
-
Pronation-dorsiflexion fracture
-
This displaced fracture off the anterior
articular surface is considered a pilon variant when there is a
significant articular fragment.
-
-
Closed reduction should be performed for
displaced fractures. Fracture reduction helps to minimize postinjury
swelling, reduces pressure on the articular cartilage, lessens the risk
of skin breakdown, and minimizes pressure on the neurovascular
structures. -
Dislocated ankles should be reduced before radiographic evaluation.
-
Open wounds and abrasions should be
cleansed and dressed in a sterile fashion as dictated by the degree of
injury. Fracture blisters should be left intact and dressed with a
well-padded sterile dressing. -
Following fracture reduction, a
well-padded posterior splint with a U-shaped component should be placed
to provide fracture stability and patient comfort. -
Postreduction radiographs should be
obtained for fracture reassessment. The limb should be aggressively
elevated with or without the use of ice.
-
Indications for nonoperative treatment include:
-
Nondisplaced, stable fracture patterns with an intact syndesmosis.
-
Displaced fractures for which stable anatomic reduction is achieved.
-
An unstable or multiple trauma patient in
whom operative treatment is contraindicated because of the condition of
the patient or the limb.
-
-
Patients with stable fracture patterns
can be placed in a short leg cast or a removable boot or stirrup and
allowed to bear weight as tolerated. -
For displaced fractures, if anatomic
reduction is achieved with closed manipulation, a bulky dressing and a
posterior splint with a U-shaped component may be used for the first
few days while swelling subsides. The patient is then placed in a long
leg cast to maintain rotational control for 4 to 6 weeks with serial
radiographic evaluation to ensure maintenance of reduction and healing.
If adequate healing is demonstrated, the patient can be placed in a
short leg cast or fracture brace. Weight bearing is restricted until
fracture healing is demonstrated.
-
Open reduction and internal fixation (ORIF) is indicated for:
-
Failure to achieve or maintain closed reduction with amenable soft tissues.
-
Unstable fractures that may result in talar displacement or widening of the ankle mortise.
-
Fractures that require abnormal foot positioning to maintain reduction (e.g., extreme plantar flexion).
-
Open fractures.
-
-
ORIF should be performed once the
patient’s general medical condition, swelling about the ankle, and soft
tissue status allow. Swelling, blisters, and soft tissue issues usually
stabilize within 5 to 10 days after injury with elevation, ice, and
compressive dressings. Occasionally, a closed fracture with severe soft
tissue injury or massive swelling may require reduction and
stabilization with use of external fixation to allow soft tissue
management before definitive fixation. -
Lateral malleolar fractures distal to the
syndesmosis may be stabilized using a lag screw or Kirschner wires with
tension banding. With fractures at or above the syndesmosis,
restoration of fibular length and rotation is essential to obtain an
accurate reduction. This is most often accomplished using a combination
of lag screws and plate. -
Management of medial malleolar fractures
is controversial. In general, with a deltoid rupture the talus follows
the fibula. Indications for operative fixation of the medial malleolus
include concomitant syndesmotic injury, persistent widening of the
medial clear space following fibula reduction, inability to obtain
adequate fibular reduction, or persistent medial fracture displacement
after fibular fixation. Medial malleolar fractures can usually be
stabilized with cancellous screws or a figure-of-eight tension band. -
Indications for fixation of posterior
malleolus fractures include involvement of >25% of the articular
surface, >2 mm displacement, or persistent posterior subluxation of
the talus. Fixation may be achieved by indirect reduction and placement
of an anterior to posterior lag screw, or a posterior to anterior lag
screw through a separate incision. -
Fibula fractures above the plafond may
require syndesmotic stabilization. After fixation of the medial and
lateral malleoli is achieved, the syndesmosis should be stressed
intraoperatively by lateral pull on the fibula with a bone hook or by
stressing the ankle in external rotation. Syndesmotic instability can
then be recognized clinically and under image intensification. Distal
tibia-fibula joint reduction is held with a large-pointed reduction
clamp A syndesmotic screw is placed 1.5 to 2.0 cm above the plafond
from the fibula to the tibia. Controversy exists as to the number of
purchased cortices (three or four) and the size of the screw (3.5 or
4.5 mm). The need for ankle dorsiflexion during syndesmotic screw
placement is also controversial. -
Very proximal fibula fractures with
syndesmosis disruption can usually be treated with syndesmosis fixation
without direct fibula reduction and stabilization. One must however,
ascertain correct fibula length and rotation before placing syndesmotic
fixation. -
Following fracture fixation, the limb is
placed in a bulky dressing incorporating a plaster splint. Progression
to weight bearing is based on the fracture pattern, stability of
fixation, patient compliance, and philosophy of the surgeon.
-
These fractures require emergent irrigation and debridement in the operating room.
-
Stable fixation is important prophylaxis
against infection and helps soft tissue healing. It is permissible to
leave plates and screws exposed, but efforts should be made to cover
hardware, if possible. -
Tourniquet use should be avoided.
-
Antibiotic prophylaxis should be continued postoperatively.
-
Serial debridements may be required for removal of necrotic, infected, or compromised tissues.
-
Nonunion: Rare and usually involve the
medial malleolus when treated closed, associated with residual fracture
displacement, interposed soft tissue, or associated lateral instability
resulting in shear stresses across the deltoid ligament. If
symptomatic, it may be treated with ORIF or electrical stimulation.
Excision of the fragment may be necessary if it is not amenable to
internal fixation and the patient is symptomatic. -
Malunion: The lateral malleolus is
usually shortened and malrotated; a widened medial clear space and a
large posterior malleolar fragment are most predictive of poor outcome.
The medial malleolus may heal in an elongated position resulting in
residual instability. -
Infection: Occurs in <2% of closed
fractures; leave implants in situ if stable, even with deep infection.
One can remove the implant after the fracture unites. The patient may
require serial debridements with possible arthrodesis as a salvage
procedure. -
Posttraumatic arthritis: Secondary to
damage at the time of injury, from altered mechanics, or as a result of
inadequate reduction. It is rare in anatomically reduced fractures,
with increasing incidence with articular incongruity. -
Reflex sympathetic dystrophy: Rare and may be minimized by anatomic restoration of the ankle and early return to function.
-
Compartment syndrome of foot: Rare.
-
Tibiofibular synostosis: This is associated with the use of a syndesmotic screw and is usually asymptomatic.
-
Loss of reduction: Reported in 25% of unstable ankle injuries treated nonoperatively.
-
Loss of ankle ROM may occur.
-
Pilon fractures account for 7% to 10% of all tibia fractures.
-
Most pilon fractures are a result of high-energy mechanisms; thus, concomitant injuries are common and should be ruled out.
-
Most common in men 30 to 40 years old.
-
Axial compression: fall from a height
-
The force is axially directed through the
talus into the tibial plafond, causing impaction of the articular
surface; it may be associated with significant comminution. If the
fibula remains intact, the ankle is forced into varus with impaction of
the medial plafond. Plantar flexion or dorsiflexion of the ankle at the
time of injury results in primarily posterior or anterior plafond
injury, respectively.
-
-
Shear: skiing accident
-
Mechanism is primarily torsion combined
with a varus or valgus stress. It produces two or more large fragments
and minimal articular comminution. There is usually an associated
fibula fracture, which is usually transverse or short oblique.
-
-
Combined compression and shear
-
These fracture patterns demonstrate
components of both compression and shear. The vector of these two
forces determines the fracture pattern.
-
-
Because of their high-energy nature,
these fractures can be expected to have specific associated injuries:
Calcaneus, tibial plateau, pelvis, and vertebral fractures.
-
Most pilon fractures are associated with high-energy trauma; full trauma evaluation and survey may be necessary.
-
Patients typically present nonambulatory with variable gross deformity of the involved distal leg.
-
Evaluation includes assessment of neurovascular status and evaluation of any associated injuries.
-
The tibia is nearly subcutaneous in this
region; therefore, fracture displacement or excess skin pressure may
convert a closed injury into an open one. -
Swelling is often massive and rapid,
necessitating serial neurovascular examinations as well as assessment
of skin integrity, necrosis, and fracture blisters. -
Meticulous assessment of soft tissue
damage is of paramount importance. Significant damage occurs to the
thin soft tissue envelope surrounding the distal tibia as the forces of
impact are dissipated. This may result in inadequate healing of
surgical incisions with wound necrosis and skin slough if not treated
appropriately. Some advise waiting 7 to 10 days for soft tissue healing
to occur before planning surgery.
-
AP, lateral, and mortise radiographs should be obtained.
-
CT with coronal and sagittal reconstruction is helpful to evaluate the fracture pattern and articular surface.
-
Careful preoperative planning is
essential with a strategically planned sequence of reconstruction;
radiographs of the contralateral side may be useful as a template for
preoperative planning.
-
Based on the severity of comminution and the displacement of the articular surface.
-
It is the most commonly used classification.
-
Prognosis correlates with increasing grade.
| Type 1: | Nondisplaced cleavage fracture of the ankle joint |
| Type 2: | Displaced fracture with minimal impaction or comminution |
| Type 3: | Displaced fracture with significant articular comminution and metaphyseal impaction |
-
Combination of the Lauge-Hansen classification of ankle fractures and the Ruedi-Allgöwer classification.
| Type A: | Malleolar fractures with significant posterior lip involvement (Lauge-Hansen SER IV injury) |
| Type B: | Spiral fractures of the distal tibia with extension into the articular surface |
| Type C: | “Central impaction injuries” as a result of talar impaction, either with or without fibula fracture; subtypes 1, 2, and 3 correspond to the Ruedi-Allgöwer classification |
functional status, severity of injury to bone, cartilage, and soft
tissue
envelope, degree of comminution and osteoporosis, and the capabilities of the surgeon.
 |
|
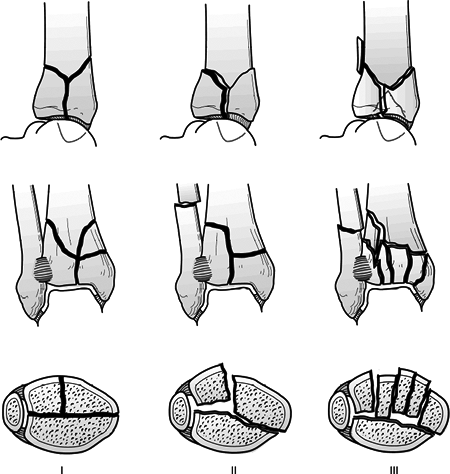
Figure
38.9. Ruedi and Allgöwer classified distal tibia fractures into three types based on the degree of articular comminution, as illustrated. The majority of the literature on fractures of the distal tibia has used this classification. (Adapted from Müller M, Allgöwer M, Schneider R, et al. Manual of Internal Fixation, 2nd ed. New York: Springer-Verlag, 1979.)
|
-
This is used primarily for nondisplaced fracture patterns or severely debilitated patients.
-
Manipulation of displaced fractures is unlikely to result in reduction of intraarticular fragments.
-
Loss of reduction is common.
-
Inability to monitor soft tissue status and swelling is a major disadvantage.
-
Displaced pilon fractures are usually treated surgically.
-
Surgery may be delayed for several days
(7 to 14 days on average) to allow for optimization of soft tissue
status, including a diminution of swelling about the ankle, resolution
of fracture blisters, and sloughing of compromised soft tissues. -
High-energy injuries can be treated with
spanning external fixation to provide skeletal stabilization,
restoration of length and partial fracture reduction while awaiting
definitive surgery. Associated fibula fractures may undergo ORIF at the
time of fixator application.
-
Maintenance of fibula length and stability.
-
Restoration tibial articular surface.
-
Bone grafting of metaphyseal defects.
-
Buttressing of the distal tibia.
-
Articular fracture reduction can be
achieved percutaneously or through small limited approaches assisted by
a variety of reduction forceps, with fluoroscopy to judge fracture
reduction. -
The metaphyseal fracture can be stabilized either with plates or with a nonspanning or spanning external fixator.
-
Bone grafting of metaphyseal defects is indicated.
-
Internal fixation: Open fracture
reduction and plate fixation may be the best way to achieve a precisely
reduced articular surface. To minimize the complications of plating,
the following techniques have been recommended:-
Surgical delay until definitive surgical treatment using initial spanning external fixation for high energy injuries.
-
Use of small, low-profile implants.
-
Avoidance of incisions over the anteromedial tibia.
-
Use of indirect reduction techniques to minimize soft tissue stripping.
-
Use of percutaneous techniques for plate insertion.
-
-
Joint spanning external fixation: This
may be used in patients with significant soft tissue compromise or open
fractures. Reduction is maintained via distraction and ligamentotaxis.
If adequate reduction is obtained, external fixation may be used as
definitive treatment.-
Articulating versus nonarticulating
spanning external fixation: Nonarticulating (rigid) external fixation
are most commonly used, theoretically allowing no ankle motion.
Articulating external fixation allows motion in the sagittal plane,
thus preventing ankle varus and shortening; application is limited, but
theoretically it results in improved chondral lubrication and nutrition
owing to ankle motion, and it may be used when soft tissue integrity is
the primary indication for external fixation.
-
-
Hybrid external fixation: This is a type
of nonspanning external fixator. Fracture reduction is enhanced using
thin wires with or without olives to restore the articular surface and
maintain bony stability. It is especially useful when internal fixation
of
P.416
any kind is contraindicated. There is a reported 3% incidence of deep wound infection.
best done after fracture comminution has consolidated and soft tissues
have recovered. It is generally performed as a salvage procedure after
other treatments have failed and posttraumatic arthritis has ensued.
-
Initial splint placement in neutral dorsiflexion with careful monitoring of soft tissues.
-
Early ankle and foot motion when wounds and fixation allow.
-
Non–weight bearing for 12 to 16 weeks, then progression to full weight bearing once there is radiographic evidence of healing.
-
Even when accurate reduction is obtained,
predictably excellent outcomes are not always achieved, and less than
anatomic reduction can lead to satisfactory outcomes. -
Soft tissue slough, necrosis, and
hematoma: These result from initial trauma combined with improper
handling of soft tissues. One must avoid excessive stripping and skin
closure under tension. Secondary closure, skin grafts, or muscle flaps
may be required for adequate closure. -
Nonunion: Results from significant
comminution and bone loss, as well as hypovascularity and infection. It
has a reported incidence of 5% regardless of treatment method. -
Malunion: Common with nonanatomic
reduction, inadequate buttressing followed by collapse, or premature
weight bearing. The reported incidence is up to 25% with use of
external fixation. -
Infection: Associated with open injuries
and soft tissue devitalization. It has a high incidence with early
surgery under unfavorable soft tissue conditions. Late infectious
complications may manifest as osteomyelitis, malunion, or nonunion. -
Posttraumatic arthritis: More frequent
with increasing severity of intraarticular comminution; it emphasizes
the need for anatomic restoration of the articular surface. -
Tibial shortening: Caused by fracture
comminution, metaphyseal impaction, or initial failure to restore
length by fibula fixation. -
Decreased ankle ROM: Patients usually average <10 degrees of dorsiflexion and <30 degrees of plantar flexion.
-
Sprains of the lateral ligaments of the ankle are the most common musculoskeletal injury in sports.
-
In the United States, it is estimated that one ankle inversion injury occurs each day per 10,000 people.
-
One year after injury, occasional intermittent pain is present in up to 40% of patients.
-
Most ankle sprains are caused by a
twisting or turning event to the ankle. This can result from either
internal or external rotation. -
Mechanism of injury and the exact ligaments injured depend on the position of the foot and the direction of the stress.
-
With ankle plantar flexion, inversion
injuries first strain the anterior talofibular ligament and then the
calcaneofibular ligament. -
With the ankle dorsiflexion and
inversion, the injury is usually isolated to the calcaneofibular
ligament. With ankle dorsiflexion and external rotation, the injury
more likely will involve the syndesmotic ligaments. The syndesmotic
ligaments, and in particular the posterior and inferior tibiofibular
ligament, can also be injured with the ankle dorsiflexed and the foot
internally rotated.
-
-
Mild ankle sprain: Patients have minimal
functional loss, no limp, minimal or no swelling, point tenderness, and
pain with reproduction of mechanism of injury. -
Moderate sprain: Patients have moderate
functional loss, inability to hop or toe-rise on the injured ankle, a
limp with walking, and localized swelling with point tenderness. -
Severe sprain: This is indicated by diffuse tenderness, swelling, and a preference for non–weight bearing.
-
This system does not delineate the specific ligaments involved.
-
Patients often describe a popping or tearing sensation in the ankle, and they remember the immediate onset of pain.
-
Some patients have an acute onset of
swelling around the lateral ankle ligaments and difficulty with weight
bearing secondary to pain. -
Significant physical examination findings
may include swelling, ecchymosis, tenderness, instability, crepitus,
sensory changes, vascular status, muscle dysfunction, and deformity. -
The location of the pain helps to
delineate the involved ligaments, and it can include the lateral aspect
of the ankle, the anterior aspect of the fibula, the medial aspect of
the ankle, and the syndesmotic region. -
The value of stress testing of the lateral collateral ankle ligaments in the acute setting is controversial.
-
At the time of injury, before swelling
and inflammation occur, the physician may be able to obtain valuable
information by performing an anterior drawer and varus stress
examination of the lateral collateral ankle ligaments. -
In patients who present several hours
after injury and who have powerful reflex inhibition, a stress test
without anesthesia is unlikely to give valuable clinical information.
-
-
Injury to the lateral collateral ankle
ligaments should be differentiated from other periarticular ligamentous
injuries on examination. Significant initial ecchymosis along the heel
P.418
indicates
possible subtalar ligamentous sprain. To evaluate potential syndesmotic
injury, the squeeze test and stress external rotation tests are
performed (see later).
-
Most patients should probably undergo
radiographic examination to rule out occult foot and ankle injuries
with an x-ray series of the foot and ankle.-
The injuries that need to be ruled out
include fracture of the base of the fifth metatarsal, navicular
fracture, fracture of the anterior process of the calcaneus, fracture
of the lateral process of the talus, os trigonal fracture, talar dome
fracture (osteochondritis dissecans), and posterior malleolar fracture.
-
-
In the acute setting, there probably is little role for performing radiographic stress testing.
-
Nonsurgical approaches are preferred for initial treatment for acute ankle sprains.
-
Initial treatment involves the use of rest, ice, compression (elastic wrap), elevation (RICE) and protected weight bearing.
-
For mild sprains, one can start early mobilization, ROM, and isometric exercises.
-
For moderate or severe sprains, one can
immobilize the ankle in neutral position, or slight dorsiflexion, for
the first 10 to 14 days, and then initiate mobilization, ROM, and
isometric exercises. Crutches are discontinued once the patient can
tolerate full weight on the ankle.
-
-
Once the initial inflammatory phase has
resolved, for the less severe ankle sprains (mild to moderate), one can
initiate a home rehabilitation program consisting of eversion muscle
group strengthening, proprioceptive retraining, and protective bracing
while the patient gradually returns to sports and functional
activities. Bracing or taping is usually discontinued 3 to 4 weeks
after resuming sports. For more severe sprains, taping or bracing
programs are continued during sports activities for 6 months, and a
supervised rehabilitation program used. -
Patients who continue to have pain in the
ankle that does not decrease with time should be reevaluated for an
occult osseous or chondral injury. -
Patients with a history of recurrent
ankle sprains who sustain an acute ankle sprain are treated in a manner
similar to that described earlier.
-
Syndesmotic sprains account for approximately 1% of all ankle sprains.
-
Syndesmotic sprains may occur without a fracture or frank diastasis.
-
Many of these injuries probably go undiagnosed and cause chronic ankle pain.
-
Type I diastasis involves lateral subluxation without fracture.
-
Type II involved lateral subluxation with plastic deformation of the fibula.
-
Type III involves posterior subluxation/dislocation of the fibula.
-
Type IV involves superior subluxation/dislocation of the talus within the mortise.
-
Immediately after a syndesmotic ankle
sprain, the patient will have well-localized tenderness in the area of
the sprain, but soon thereafter, with ensuing swelling and ecchymosis,
the precise location of the sprain often becomes obscured. -
Patients ordinarily present to physicians
several hours, if not days, after these injuries, with difficulty in
weight bearing, ecchymosis extending up the leg, and marked swelling.
The clue to chronic, subclinical syndesmotic sprains is the history of
vague ankle pain with push-off and normal imaging studies. -
The clinical examination involves
palpating the involved ligaments and bones. The fibula should be
palpated in a proximal to distal direction. The proximal tibiofibular
joint should be assessed for tenderness or associated injury. -
Two clinical tests can be used to isolate syndesmotic ligament injury.
-
The squeeze test, described by Hopkinson
et al., involves squeezing the fibula at the midcalf. If this maneuver
reproduces distal tibiofibular pain, it is likely that the patient has
sustained some injury to the syndesmotic region. -
The single best physical examination test
for a syndesmotic injury is probably the external rotation stress test.
The patient is seated, with the knee flexed at 90 degrees. The examiner
stabilizes the patient’s leg and externally rotates the foot. If this
reproduces pain at the syndesmosis, the test is positive, and the
physician should assume, in the absence of bony injuries, that a
syndesmotic injury has occurred.
-
-
The radiographic evaluation of a
syndesmotic injury, in an acute setting, involves an attempt at
weight-bearing radiographs of the ankle (AP, mortise, lateral) and, if
negative, an external rotation stress view. -
Without injury, a weight-bearing mortise view should show:
-
No widening of the medial clear space between the medial malleolus and the medial border of the talus.
-
A tibiofibular clear space (the interval
between the medial border of the fibula and the lateral border of the
posterior tibial malleolus) of 6 mm or less.
-
-
When routine x-rays are negative, and the
patient is still suspected of having a syndesmotic injury, stress
radiographs can be considered. The examiner should inspect stress
radiographs for widening of the medial joint space and tibiofibular
clear space on the mortise view and for posterior displacement of the
fibula relative to the tibia on the lateral view. -
In difficult-to-diagnose acute cases or
latent presentations, an MRI evaluation of the syndesmosis may
delineate injury to the syndesmotic ligaments.
-
Tibiofibular syndesmotic ligamentous
injuries are slower to recover than other ankle ligamentous injuries
and may benefit from a more restrictive approach to initial management. -
Patients are immobilized in a
non-weight-bearing cast for 2 to 3 weeks after injury. This is followed
by use of a protective, modified, articulated ankle-foot orthosis that
eliminates external rotation stress on the ankle for a variable period,
depending on the functional needs and sports activities of the patient. -
Operative treatment is considered for
patients with irreducible diastasis. To hold the syndesmotic ligaments
while healing, two screws usually placed at the superior margin of the
syndesmosis in a nonlagged fashion, from the fibula into the tibia. The
patients are maintained non-weight bearing for 6 weeks, and the screws
are removed approximately 12 to 16 weeks after fixation.
-
Most Achilles tendon problems are related to overuse injuries and are multifactorial.
-
The principal factors include host susceptibility and mechanical overload.
-
The spectrum of injury ranges from paratenonitis to tendinosis to acute rupture.
-
In a trauma setting, a true rupture is the most common presentation.
-
Delayed or missed diagnosis of Achilles tendon rupture by primary treating physicians is relatively common (up to 25%).
-
The Achilles tendon is the largest tendon in the body.
-
It lacks a true synovial sheath and
instead has a paratenon with visceral and parietal layers permitting
approximately 1.5 cm of tendon glide. -
It receives its blood supply from three sources:
-
The musculotendinous junction.
-
The osseous insertion.
-
Multiple mesosternal vessels on the anterior surface of the tendon.
-
 |
|
Figure
38.10. The Thompson test for continuity of the gastrocnemius-soleus complex. Without rupture of the Achilles tendon, squeezing the calf causes active plantar flexion of the foot. With rupture, squeezing the superficial posterior compartment of the leg does not induce plantar flexion of the foot. (Adapted from Browner B, Jupiter J, Levine A. Skeletal Trauma: Fractures, Dislocations, and Ligamentous Injuries, 2nd ed. Philadelphia: WB Saunders, 1997.)
|
-
With either partial or complete Achilles
tendon rupture, patients typically experience sharp pain, often
described as feeling like being kicked in the leg. -
With a partial rupture, physical examination may only reveal a localized, tender area of swelling.
-
With complete rupture, examination normally reveals a palpable defect in the tendon.
-
In this setting, the Thompson test is
generally positive (i.e., squeezing the calf does not cause active
plantar flexion), and the patient usually is incapable of performing a
single heel-raise (Fig. 38.10). -
The Thompson test can be falsely positive
when the accessory ankle flexors (posterior tibialis, flexor digitorum
longus, flexor hallucis longus muscles, or accessory soleus muscles)
are squeezed together with the contents of the superficial posterior
leg compartment.
-
-
Goals are to restore normal
musculotendinous length and tension and thereby to optimize ultimate
strength and function of the gastrocnemius-soleus complex. -
Whether operative or nonoperative treatment best achieves these goals remains a matter of controversy.
-
Proponents of surgical repair point to
lower recurrent rupture rates, improved strength, and a higher
percentage of patients who return to sports activities. -
Proponents of nonoperative treatment
stress the high surgical complication rates resulting from wound
infection, skin necrosis, and nerve injuries. -
When major complications, including recurrent ruptures, are compared, both forms of treatment have similar complication rates.
-
Most authors tend to treat active
patients who are interested in continuing athletic endeavors with
operative treatment and inactive patients or those with other
complicating medical factors (e.g., immunosuppression, soft tissue
injuries, history of recurrent lower extremity infections, vascular or
neurologic impairment) with nonoperative approaches.
P.422 -
-
Nonoperative treatment begins with a period of immobilization.
-
Initially, the leg is placed in a splint for 2 weeks, with the foot in plantar flexion to allow hematoma consolidation.
-
Thereafter, a short or long leg cast is
placed for 6 to 8 weeks, with less plantar flexion and progressive
weight bearing generally permitted at 2 to 4 weeks after injury. -
After removal of the cast, a heel lift is used while making the transition back to wearing normal shoes.
-
Progressive resistance exercises for the
calf muscles are started at 8 to 10 weeks, with a return to athletic
activities at 4 to 6 months. -
Patients are informed that attainment of
maximal plantar flexion power may take 12 months or more and that some
residual weakness is common.
-
-
Surgical treatment is often preferred when treating younger and more athletic patients.
-
Several different operative techniques have been described, including percutaneous and open approaches.
-
Percutaneous approaches have the
advantage of decreased dissection but have historically carried the
disadvantages of potential entrapment of the sural nerve and an
increased chance of inadequate tendon capture. -
Open approaches have the intrinsic
advantages of permitting complete evaluation of the injury and
inspection of final tendon end reapproximation; however, they carry the
disadvantages of higher rates of wound dehiscence and skin adhesion
problems.-
The surgical technique uses a medial longitudinal approach to avoid injury to the sural nerve.
-
The paratenon is carefully dissected, and
sutures are placed in each tendon end for tendon reapproximation. The
paratenon is closed in a separate layer.
-
-
Postoperative management consists of a
partial weight bearing short leg cast for 6 to 8 weeks. This is
followed by use of a 1-cm heel lift for 1 month. As with nonoperatively
treated patients, progressive resistance exercises are started at 8 to
10 weeks, with a return to sports at 4 to 6 months. -
With distal ruptures or sleeve avulsions,
an open technique and reattachment of the tendon to the calcaneus is
performed. This is usually done with transosseous suture fixation.
-
-
Subluxation and dislocation of the peroneal tendons are uncommon and usually result from sports activities.
-
The injury is easily misdiagnosed as an ankle sprain, and it can result in recurrent or chronic dislocation.
-
Presentation is similar to that of a lateral ankle sprain with lateral ankle swelling, tenderness, and ecchymosis.
-
Patients with peroneal tendon subluxation or dislocation demonstrate tenderness posterior to the lateral malleolus.
-
The anterior drawer test is negative, and the patient has discomfort and apprehension with resisted eversion of the foot.
-
Radiographic evaluation of a patient with
peroneal tendon subluxation or dislocation may reveal a small fleck of
bone off the posterior aspect of the lateral malleolus, which is best
seen on the internal oblique or mortise view. -
If the diagnosis is unclear, as a result
of swelling and diffuse ecchymosis, an MRI evaluation may help to
delineate this soft tissue injury.
-
When the initial reduction of dislocated tendons is stable, nonoperative techniques can be successful.
-
Management consists of immobilization in
a well-molded cast with the foot in slight plantar flexion and mild
inversion in an attempt to relax the superior peroneal retinaculum and
to maintain reduction in the retrofibular space. Non–weight-bearing
immobilization is continued for 6 weeks to allow adequate time for
retinacular and periosteal healing.
-
-
When the diagnosis is made on a delayed
basis or the patient presents with recurrent dislocations, operative
treatment is considered because nonoperative measures are unlikely to
work.-
Surgical alternatives include transfer of
the lateral Achilles tendon sheath, fibular osteotomy to create a
deeper groove for the tendons, rerouting of the peroneal tendons under
the fibulocalcaneal ligament, or simple reconstructive repair of the
superior peroneal retinaculum with relocation of the tendons. -
Postoperatively, the leg is splinted for
1 to 2 weeks in a slightly inverted and plantar flexed position;
patients are then started on a passive motion exercise program to
reduce scar formation in the peroneal groove and to increase the
likelihood of good tendon nutrition and retinacular healing. Weight
bearing is initiated 6 weeks postoperatively, and rehabilitation and
focusing of strength and ROM are initiated soon thereafter.
-