Ankle Arthritis
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Ankle Arthritis
Ankle Arthritis
Mark Clough MD
Description
-
The ankle joint is subject to osteoarthritis, but less frequently than other joints, such as the hip and knee (1).
-
Trauma and abnormal ankle mechanics are the most common causes of ankle arthritis (2,3).
-
Demographically, posttraumatic ankle arthritis presents in a younger age group than does primary osteoarthritis.
-
Chronic ankle instability, OCDs, and osteonecrosis also lead to degenerative arthritis.
-
Ankle and foot arthritis are common in patients with rheumatoid arthritis and other inflammatory arthropathies.
-
Cartilage in the ankle is thinner and more uniform in its matrix than is that in the hip and knee (4).
Geriatric Considerations
Caution with NSAIDs or COX-2 inhibitors for symptomatic treatment because of potential cardiovascular complications
Pediatric Considerations
No specific considerations
Pregnancy Considerations
To avoid bleeding complications, do not treat a symptomatic pregnant patient with NSAIDs.
General Prevention
-
Proper treatment of ankle fractures may decrease the development of posttraumatic arthritis (5).
-
Weight loss is helpful in reducing joint loading, which may help to slow or prevent the development of arthritis.
Epidemiology
Incidence
Symptomatic ankle arthritis is rare and has been reported to be 9 times less common than symptomatic knee and hip arthritis (6).
Risk Factors
-
Ankle trauma
-
Ankle instability
-
Inflammatory arthritis
Etiology
-
Trauma:
-
Malleolar fractures
-
Tibial plafond (pilon) fractures
-
Talar fractures
-
-
Ankle instability
-
Inflammatory disease (e.g., rheumatoid arthritis)
-
Osteonecrosis
-
OATS of the talus
-
Infection
Signs and Symptoms
-
Pain
-
Swelling
-
Giving way or locking
-
Stiffness
-
Deformity
History
-
Identify previous trauma and treatment.
-
Identify underlying medical problems.
Physical Exam
-
Examine the patient (seated and standing).
-
Palpate for ankle joint effusion or warmth.
-
Assess ROM and ankle ligament stability.
-
Palpate the ankle joint line for tenderness and differentiate it from subtalar pain.
-
Assess motor and sensory function to evaluate for neurologic impairment.
-
Palpate dorsalis pedis and posterior tibial pulses; check capillary refill.
-
Observe gait pattern, identify antalgic
pattern, and identify external rotation or circumduction secondary to
diminished dorsiflexion
Tests
Imaging
-
Radiography:
-
Obtain standard radiographs of the ankle, including AP, lateral, and mortise views.
-
Assess for arthritic changes, including joint space narrowing, subchondral cysts, osteophytes, and sclerosis.
-
-
A CT scan may show the extent of the arthritis, including subtalar involvement.
-
Consider MRI if an OATS, osteonecrosis,
or tumor is suspected on radiographs, or to evaluate further for
soft-tissue and/or tendinous abnormalities.
Differential Diagnosis
-
Osteochondritis dissecans
-
Osteonecrosis/AVN
-
Posterior tibial tendinitis
-
Subtalar joint arthritis
-
Tumor
General Measures
-
First line treatment is generally nonoperative.
-
NSAIDs
-
Orthotic devices, including ankle-foot orthosis (brace)
-
Footwear modifications (e.g., rocker bottom sole, solid ankle cushion heel)
-
Intra-articular corticosteroid injections
-
Weight loss
-
-
If nonoperative treatment is ineffective after 3–6 months, the patient may be counseled about surgery.
Activity
-
The patient should decrease excessive walking and avoid high-impact activities such as running, jumping, or cutting maneuvers.
-
Encourage low-impact exercise, including stationary bicycle and aquatic exercises.
-
Consider use of assistive devices such as a cane or crutches.
Special Therapy
Physical Therapy
Not typically prescribed in primary management but may be useful postoperatively
Medication (Drugs)
First Line
-
NSAIDs
-
Analgesics
Complementary and Alternative Therapies
It is unclear if glucosamine is efficacious in the treatment of ankle arthritis.
Surgery
-
Considered after failure of nonsurgical measures
-
Ankle arthroscopy can be used for débridement of impinging osteophytes, loose bodies, and chondral defects.
-
Articular distraction arthroplasty of ankle joint with external fixation is an option for mild to moderate stages of arthritis (7).
-
Supramalleolar tibial osteotomy for fracture malunion, tibial malalignment, or partial joint arthritic involvement (8)
-
Ankle arthrodesis (fusion) via screw fixation is the gold standard of salvage surgery for ankle arthritis (Fig. 1).
-
Fusion has the widest indications,
including posttraumatic or degenerative arthritis, postinfection
arthritis, large OCDs, rheumatoid or inflammatory arthritis, and talar
osteonecrosis (9). Fig. 1. Lateral radiograph of ankle arthrodesis (fusion).
Fig. 1. Lateral radiograph of ankle arthrodesis (fusion). -
Patients generally are satisfied with outcomes and pain relief despite limitations in ROM (9).
P.17 -
-
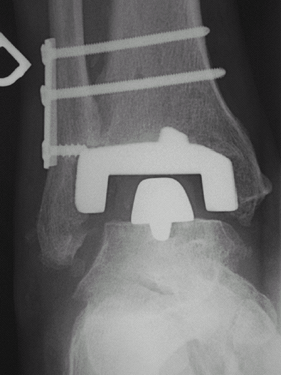
Total ankle arthroplasty is becoming more accepted with the introduction of later-generation designs (10) (Fig. 2).
-
Possible advantages compared with fusion: Greater ROM and potential for less hindfoot/midfoot arthritis from altered mechanics
-
Disadvantages compared with fusion: More
perioperative complications, finite lifespan of implants, potential for
implant failure and bony loss that can complicate future revision
surgery
-
 |
|
Fig. 2. Anteroposterior radiograph of total ankle arthroplasty (replacement).
|
Prognosis
-
Prognosis is fair.
-
Many patients with severe arthritis ultimately need surgery to control pain.
Complications
-
Nonoperative treatment: Few complications
-
Surgical management: Wound-healing
problems, malalignment, secondary hindfoot and midfoot arthritis,
infection, and damage to local nerves and blood vessels
Patient Monitoring
The patient with ankle arthritis should be followed to monitor symptoms and to discuss treatment options.
References
1. Stauffer RN, Chao EYS, Brewster RC. Force and motion analysis of the normal, diseased, and prosthetic ankle joint. Clin Orthop Relat Res 1977;127:189–196.
2. Miller RA, DeCoster TA, Mizel MS. What’s new in foot and ankle surgery? J Bone Joint Surg 2005;87A:909–917.
3. Demetriades L, Strauss E, Gallina J. Osteoarthritis of the ankle. Clin Orthop Relat Res 1998;349:28–42.
4. Swann
AC, Seedhom BB. The stiffness of normal articular cartilage and the
predominant acting stress levels: implications for the aetiology of
osteoarthrosis. Br J Rheumatol 1993;32:16–25.
AC, Seedhom BB. The stiffness of normal articular cartilage and the
predominant acting stress levels: implications for the aetiology of
osteoarthrosis. Br J Rheumatol 1993;32:16–25.
5. Lindsjo U. Operative treatment of ankle fracture-dislocations. A follow-up study of 306/321 consecutive cases. Clin Orthop Relat Res 1985;199:28–38.
6. Cushnaghan
J, Dieppe P. Study of 500 patients with limb joint osteoarthritis. I.
Analysis by age, sex, and distribution of symptomatic joint sites. Ann Rheum Dis 1991;50:8–13.
J, Dieppe P. Study of 500 patients with limb joint osteoarthritis. I.
Analysis by age, sex, and distribution of symptomatic joint sites. Ann Rheum Dis 1991;50:8–13.
7. van
Valburg AA, van Roermund PM, Lammens J, et al. Can Ilizarov joint
distraction delay the need for an arthrodesis of the ankle? A
preliminary report. J Bone Joint Surg 1995;77B:720–725.
Valburg AA, van Roermund PM, Lammens J, et al. Can Ilizarov joint
distraction delay the need for an arthrodesis of the ankle? A
preliminary report. J Bone Joint Surg 1995;77B:720–725.
8. Stamatis
ED, Cooper PS, Myerson MS. Supramalleolar osteotomy for the treatment
of distal tibial angular deformities and arthritis of the ankle joint. Foot Ankle Int 2003;24:754–764.
ED, Cooper PS, Myerson MS. Supramalleolar osteotomy for the treatment
of distal tibial angular deformities and arthritis of the ankle joint. Foot Ankle Int 2003;24:754–764.
9. Coester LM, Saltzman CL, Leupold J, et al. Long-term results following ankle arthrodesis for post-traumatic arthritis. J Bone Joint Surg 2001;83A:219–228.
10. Knecht SI, Estin M, Callaghan JJ, et al. The Agility total ankle arthroplasty. Seven to sixteen-year follow-up. J Bone Joint Surg 2004;86A:1161–1171.
Codes
ICD9-CM
716.97 Arthropathy, ankle not otherwise specified
Patient Teaching
The clinician should thoroughly discuss with the patient
the risks and benefits of surgical treatment, as well as alternatives
and expected outcomes.
the risks and benefits of surgical treatment, as well as alternatives
and expected outcomes.
FAQ
Q: What is the most common cause of ankle arthritis?
A: Trauma.
Q: How does arthritis of the ankle differ from arthritis of the hip and knee?
A:
Most cases of ankle arthritis are posttraumatic in nature and present
at a younger age than do hip or knee arthritis, which are typically
primary osteoarthritis.
Most cases of ankle arthritis are posttraumatic in nature and present
at a younger age than do hip or knee arthritis, which are typically
primary osteoarthritis.
Q: What are potential nonsurgical treatment options?
A: Activity modification, medications, corticosteroid injections, brace, shoe modifications, cane.
Q: What is currently the most common surgical option for severe ankle arthritis?
A: Ankle arthrodesis (fusion).
