Amputations
Authors: Doyle, James R.
Title: Hand and Wrist, 1st Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > Section III – Emergency Department > 14 – Amputations
14
Amputations
General Principles
The management of thumb or finger amputation is a
complex topic with many variable methods of treatment. Digital
amputations may involve the terminal aspect of the digit or a
substantial portion of the ray, and general principles of management
will be presented in this chapter. This chapter will also include a
section on replantation.
complex topic with many variable methods of treatment. Digital
amputations may involve the terminal aspect of the digit or a
substantial portion of the ray, and general principles of management
will be presented in this chapter. This chapter will also include a
section on replantation.
The goals of treatment include restoration of adequate
sensibility without hypersensitivity, good function and appearance, and
a short period of recovery.
sensibility without hypersensitivity, good function and appearance, and
a short period of recovery.
The treatment of each case is based on the patient’s
age, occupation, functional needs, the digit injured, and the surgeon’s
experience with various techniques.
age, occupation, functional needs, the digit injured, and the surgeon’s
experience with various techniques.
Treatment methods range from healing by secondary
intention with dressing changes, to primary closure (without tension)
with local tissue, to split-thickness or full-thickness skin grafts, to
various forms of local or distant flaps.
intention with dressing changes, to primary closure (without tension)
with local tissue, to split-thickness or full-thickness skin grafts, to
various forms of local or distant flaps.
Pertinent Anatomy
Terminal Phalanx
Most amputations in the hand involve the terminal
phalanx, and this chapter will focus on that level of amputation. The
anatomy of the terminal phalanx represents a complex functional unit
that consists of bone and soft tissue in the form of thick skin that
covers a fat pad with fibrous tissue elements that separate the fat
into compartments. This complex structure includes nerves and
specialized end organs that provide sensibility to the digital tip in
the form of pressure, pain, temperature, and identification of form and
texture.
phalanx, and this chapter will focus on that level of amputation. The
anatomy of the terminal phalanx represents a complex functional unit
that consists of bone and soft tissue in the form of thick skin that
covers a fat pad with fibrous tissue elements that separate the fat
into compartments. This complex structure includes nerves and
specialized end organs that provide sensibility to the digital tip in
the form of pressure, pain, temperature, and identification of form and
texture.
It is the hand, through the digital tips, that obtains
information from the environment, which it passes to the brain and
ultimately executes a given function in conjunction with the remaining
components of the upper extremity. The hand is under central control,
mediated by specialized end organs and nerve endings in and beneath the
skin, as well as by joint receptors. Although the hand also may be
under visual control, this modality is a less effective control method
compared to the modalities of sensibility and proprioception: compare
the effective use of the hand by a blind person to the relatively poor
hand function in a sighted person who has lost sensibility due to
Hansen’s disease. Thus, it should be readily apparent that the tips of
our digits are critically important to hand function. The
contour of the terminal phalanx with its nail is multiplanar and its
shape and specialized end organs can never be restored surgically in
spite of our best efforts at reconstruction.
information from the environment, which it passes to the brain and
ultimately executes a given function in conjunction with the remaining
components of the upper extremity. The hand is under central control,
mediated by specialized end organs and nerve endings in and beneath the
skin, as well as by joint receptors. Although the hand also may be
under visual control, this modality is a less effective control method
compared to the modalities of sensibility and proprioception: compare
the effective use of the hand by a blind person to the relatively poor
hand function in a sighted person who has lost sensibility due to
Hansen’s disease. Thus, it should be readily apparent that the tips of
our digits are critically important to hand function. The
contour of the terminal phalanx with its nail is multiplanar and its
shape and specialized end organs can never be restored surgically in
spite of our best efforts at reconstruction.
Nail Unit
The nail unit consists of the nail plate, the nail fold,
the nail bed (sterile and germinal matrix), a vascular supply, and
nerves. The nail unit assists in digital pad sensibility by providing
support and counter pressure for the digital pad. Grasping and pinching
are aided by the nail unit, which provides dorsal and peripheral
anchoring, and provides stability to the palmar pad. The functional
spectrum may include everything from scratching an itch to picking up
and manipulating small objects. The anatomy and terminology of the nail
unit is depicted in Figure 14-1.
the nail bed (sterile and germinal matrix), a vascular supply, and
nerves. The nail unit assists in digital pad sensibility by providing
support and counter pressure for the digital pad. Grasping and pinching
are aided by the nail unit, which provides dorsal and peripheral
anchoring, and provides stability to the palmar pad. The functional
spectrum may include everything from scratching an itch to picking up
and manipulating small objects. The anatomy and terminology of the nail
unit is depicted in Figure 14-1.
Nail Plate
The hard, often shiny, fingernail or thumbnail is called
the nail plate. The nail plate is homologous to the stratum corneum of
the epidermis, and consists of compacted, anucleate, keratin-filled
squames with dorsal, intermediate, and palmar layers. It is slightly
convex in the longitudinal axis and more convex in the transverse axis.
The lunula is a white opacity immediately distal to the central aspect
of the proximal nail fold, and is said to be due to comparatively poor
vascularization of the germinal matrix
the nail plate. The nail plate is homologous to the stratum corneum of
the epidermis, and consists of compacted, anucleate, keratin-filled
squames with dorsal, intermediate, and palmar layers. It is slightly
convex in the longitudinal axis and more convex in the transverse axis.
The lunula is a white opacity immediately distal to the central aspect
of the proximal nail fold, and is said to be due to comparatively poor
vascularization of the germinal matrix
Nail Fold
Proximally, the nail plate extends under the semilunar
nail fold, which is lined with dorsal and palmar epidermis. The stratum
corneum layer of the dorsal layer of epidermis extends distally over
the nail plate to form the cuticle or eponychium.
nail fold, which is lined with dorsal and palmar epidermis. The stratum
corneum layer of the dorsal layer of epidermis extends distally over
the nail plate to form the cuticle or eponychium.
P.227
 |
|
Figure 14-1 The anatomy and terminology of the nail unit and terminal phalanx.
|
Nail Bed
The nail plate rests on the nail bed (sterile and
germinal matrix), which is defined as all the soft tissue immediately
beneath the nail plate that participates in nail generation and
migration. The nail bed is a specialized form of epithelium, with a
proximal zone of germinal matrix and a distal zone of sterile matrix.
The germinal matrix is proximal, and the distal margin of the lunula is
approximately at the junction between the germinal and sterile matrix.
A sagittal section of the distal phalanx reveals a wedge-shaped
collection of germinal cells within the proximal portion of the nail
bed. Dorsal and palmar components of the matrix are noted. The palmar
matrix cells are continuous distally with the nail bed. The nail bed is
grooved and ridged longitudinally, which matches a similar pattern on
the undersurface of the nail plate, and which may help stabilize the
nail for functional demands. Beneath the epithelium of the nail bed is
a dermis layer that is anchored to the underlying periosteum of the
distal phalanx by fibrous tissue. Keratinized cells are extruded from
the dorsal and palmar germinal matrix cells to produce the nail plate,
with the major production coming from the palmar cells. The area of
epidermis under the distal edge of the nail plate is called the
hyponychium. The stratum corneum layer is undulant and constantly being
shed. The hyponychium provides an important barrier against entry of
bacteria.
germinal matrix), which is defined as all the soft tissue immediately
beneath the nail plate that participates in nail generation and
migration. The nail bed is a specialized form of epithelium, with a
proximal zone of germinal matrix and a distal zone of sterile matrix.
The germinal matrix is proximal, and the distal margin of the lunula is
approximately at the junction between the germinal and sterile matrix.
A sagittal section of the distal phalanx reveals a wedge-shaped
collection of germinal cells within the proximal portion of the nail
bed. Dorsal and palmar components of the matrix are noted. The palmar
matrix cells are continuous distally with the nail bed. The nail bed is
grooved and ridged longitudinally, which matches a similar pattern on
the undersurface of the nail plate, and which may help stabilize the
nail for functional demands. Beneath the epithelium of the nail bed is
a dermis layer that is anchored to the underlying periosteum of the
distal phalanx by fibrous tissue. Keratinized cells are extruded from
the dorsal and palmar germinal matrix cells to produce the nail plate,
with the major production coming from the palmar cells. The area of
epidermis under the distal edge of the nail plate is called the
hyponychium. The stratum corneum layer is undulant and constantly being
shed. The hyponychium provides an important barrier against entry of
bacteria.
Clinical Significance
A smooth nail bed is essential for the regrowth of a
normal nail plate. In nail-bed injuries, primary healing cannot occur
if the bed is not accurately reapproximated. If the scar is in the
dorsal matrix, a dull streak may appear in the nail plate; if the scar
is in the intermediate portion of the germinal matrix, a split or
absent nail may occur; if the scar is in the palmar nail or sterile
matrix, a split or nonadherence of the nail beyond the scar may occur.
normal nail plate. In nail-bed injuries, primary healing cannot occur
if the bed is not accurately reapproximated. If the scar is in the
dorsal matrix, a dull streak may appear in the nail plate; if the scar
is in the intermediate portion of the germinal matrix, a split or
absent nail may occur; if the scar is in the palmar nail or sterile
matrix, a split or nonadherence of the nail beyond the scar may occur.
Blood Supply and Drainage
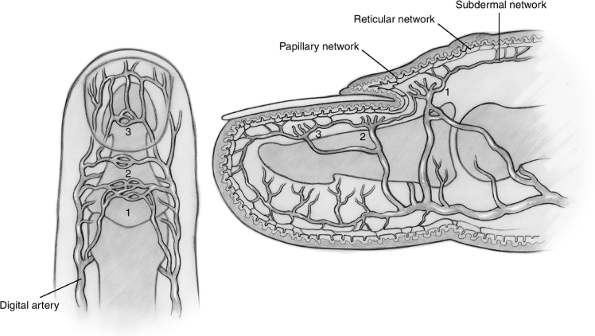
The arterial blood supply to the nail bed comes from two
dorsal branches from the common palmar digital artery; the proximal
vessel is a dorsal branch to the nail fold, and the second courses
along the lateral nail plate margin and sends branches to the nail bed (Figure 14-2). These vessels anastomose dorsally with their counterparts to form arcades.
dorsal branches from the common palmar digital artery; the proximal
vessel is a dorsal branch to the nail fold, and the second courses
along the lateral nail plate margin and sends branches to the nail bed (Figure 14-2). These vessels anastomose dorsally with their counterparts to form arcades.
Branches from these vessels and the arcades form sinuses
surrounded by muscle fibers, and help to regulate the blood pressure
and blood supply to the extremities. These networks have been
identified as papillary, reticular, and subdermal, and correspond to
the general architecture of the vessels of the skin. The dermis of the
nail bed is well vascularized, and includes large arteriovenous shunts
(glomera). There is reduced vascular density in the region of the
germinal matrix, in contrast to an increased vascular density in the
sterile matrix. The comparatively less-vascularized germinal matrix
demonstrates a well-developed subdermal network located near a zone of
loose connective tissue that is poorly vascularized near the proximal
part of the distal phalanx. This zone may be a sliding apparatus
between the nail and the distal attachment of the extensor tendon. A
coalescence of veins in the skin, proximal to the nail fold, that
course proximally in a random fashion over the dorsum of the digit,
provides venous drainage. These veins are of sufficient size for
microvascular anastomosis.
surrounded by muscle fibers, and help to regulate the blood pressure
and blood supply to the extremities. These networks have been
identified as papillary, reticular, and subdermal, and correspond to
the general architecture of the vessels of the skin. The dermis of the
nail bed is well vascularized, and includes large arteriovenous shunts
(glomera). There is reduced vascular density in the region of the
germinal matrix, in contrast to an increased vascular density in the
sterile matrix. The comparatively less-vascularized germinal matrix
demonstrates a well-developed subdermal network located near a zone of
loose connective tissue that is poorly vascularized near the proximal
part of the distal phalanx. This zone may be a sliding apparatus
between the nail and the distal attachment of the extensor tendon. A
coalescence of veins in the skin, proximal to the nail fold, that
course proximally in a random fashion over the dorsum of the digit,
provides venous drainage. These veins are of sufficient size for
microvascular anastomosis.
Nerve Supply
Branches from the paired digital nerves innervate the
nail unit. The most common pattern (70%) is represented by a branch
that passes beneath the nail plate and into the nail bed at
approximately the level of the lunula and a second branch that passes
distally to end at the hyponychial area. There are numerous sensory
nerve endings, including Merkel discs and Meissner corpuscles.
nail unit. The most common pattern (70%) is represented by a branch
that passes beneath the nail plate and into the nail bed at
approximately the level of the lunula and a second branch that passes
distally to end at the hyponychial area. There are numerous sensory
nerve endings, including Merkel discs and Meissner corpuscles.
P.228
 |
|
Figure 14-2
Arterial supply of the distal phalanx. 1, Network of nail wall; 2, arcade of germinal matrix; 3, arcade of sterile matrix. See text for details. |
Nail Plate Growth
Growth rate is determined by the turnover rate of the
germinal matrix, which varies with age, digit (the long finger nail
grows faster than the small fingernail), environmental temperature,
season, time of day, and nutritional status. Rate of growth in the long
finger is approximately 0.1 mm/day. As the matrix cells enlarge, they
grow distally due to the confinement of the nail fold, and they are
flattened by the pressure of newly forming cells beneath them. This
pressure and confinement result in a nail plate that is flat and grows
distally. The dorsal layer of the germinal matrix produces nail cells
that are relatively shiny, and if these cells are removed or damaged,
the nail surface will appear dull.
germinal matrix, which varies with age, digit (the long finger nail
grows faster than the small fingernail), environmental temperature,
season, time of day, and nutritional status. Rate of growth in the long
finger is approximately 0.1 mm/day. As the matrix cells enlarge, they
grow distally due to the confinement of the nail fold, and they are
flattened by the pressure of newly forming cells beneath them. This
pressure and confinement result in a nail plate that is flat and grows
distally. The dorsal layer of the germinal matrix produces nail cells
that are relatively shiny, and if these cells are removed or damaged,
the nail surface will appear dull.
Relationship of the Germinal Matrix to the Extensor Tendon Insertion
Based on microscopic dissection, the distance from the
terminal aspect of insertion of the extensor tendon and the proximal
edge of the germinal matrix was found to average 1.2 mm, with a range
of 0.9 to 1.8 mm.
terminal aspect of insertion of the extensor tendon and the proximal
edge of the germinal matrix was found to average 1.2 mm, with a range
of 0.9 to 1.8 mm.
The clinical significance of this fact is that when the
extensor tendon insertion is visualized during operative procedures on
the dorsum of the distal phalanx, care should be taken to avoid damage
to the germinal matrix. Conversely, when the germinal matrix is being
removed for total ablation of a nail, dissection does not need to be
carried proximal to the most distal fibers of the extensor tendon.
extensor tendon insertion is visualized during operative procedures on
the dorsum of the distal phalanx, care should be taken to avoid damage
to the germinal matrix. Conversely, when the germinal matrix is being
removed for total ablation of a nail, dissection does not need to be
carried proximal to the most distal fibers of the extensor tendon.
Treatment
Digital Tip Amputations With or Without Bone Involvement
-
These injuries may occur in a variety of
planes in relationship to the long axis of the digit. The osseous
phalanx may or may not be exposed. -
The following discussion and case
presentations illustrate various techniques that may be used based on
the nature of the injury. -
The reader should understand that there
is no ideal treatment for fingertip amputations, and that differences
of opinion exist among the surgeons who treat these injuries. -
Many of the following procedures are
technically challenging, and most, if not all, may have cosmetic and
functional issues related to the procedure. -
The choice of a given technique may relate to the surgeon’s experience and preference.
-
The procedure should be matched to each patient and his or her cosmetic and functional needs.
Nonsurgical Treatment
-
Fingertip avulsions in children may be treated by sterile dressing changes as the primary form of treatment.
-
Most, if not all, soft tissue avulsions
of the digit tips in children will rapidly regrow the lost skin. This
may be the only treatment required. -
In some instances the avulsed part may be
reapplied as a biologic dressing with the understanding that it may or
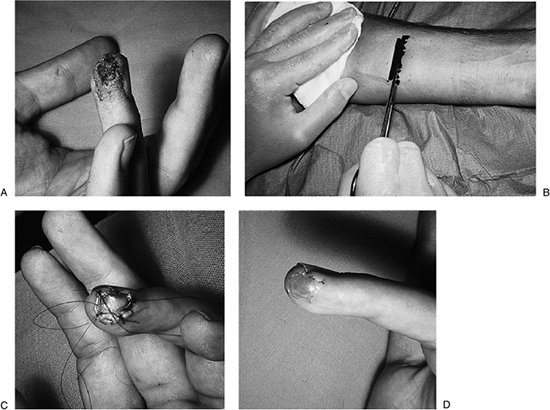
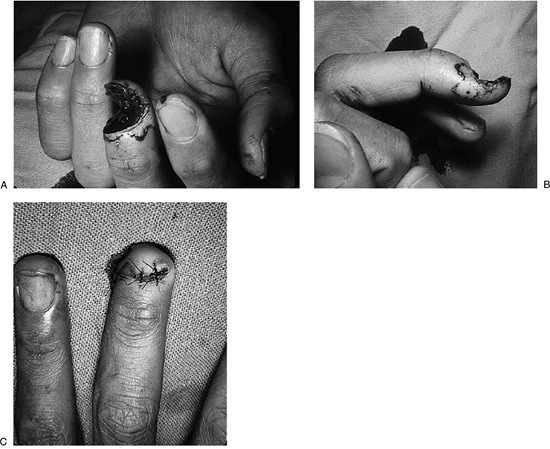
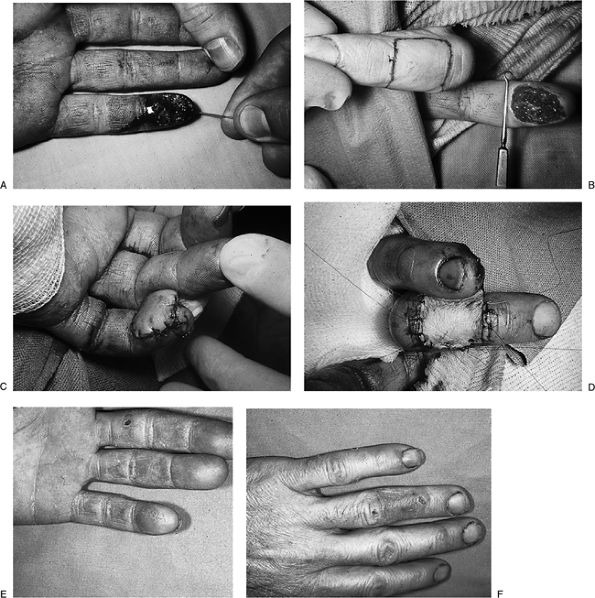
may not survive.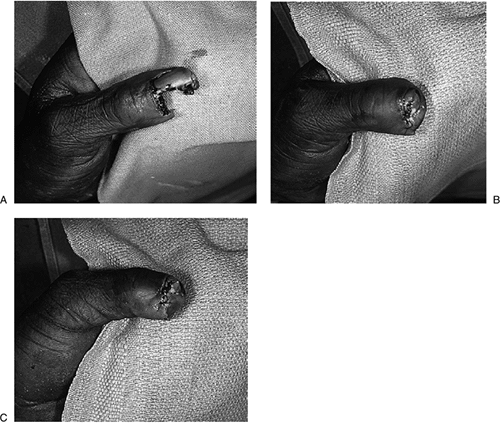 Figure 14-3 A. Significant loss of the terminal pulp of the thumb as a result of a power saw injury to the non-dominant left thumb. B, C.
Figure 14-3 A. Significant loss of the terminal pulp of the thumb as a result of a power saw injury to the non-dominant left thumb. B, C.
Treatment was via primary closure, by “folding over” the remaining
local tissues. This provided for excellent tissue coverage with good
sensibility and circulation. Rapid healing occurred in this unemployed
elderly male. -
Significant bone protrusion, if evident, may need to be trimmed back.
-
Secondary reconstruction may be used as necessary.
P.229
Surgical Treatment
Primary Closure by Local Tissue
-
Suitable local tissues, if present, may provide very satisfactory tissue for primary coverage of amputation defects.
-
The advantage of this method includes
rapid healing with minimal and acceptable shortening, and coverage of
the defect with substantial and sensate skin. -
This technique is illustrated in Figure 14-3 and Figure 14-4.
Primary Closure With Shortening of the Bone
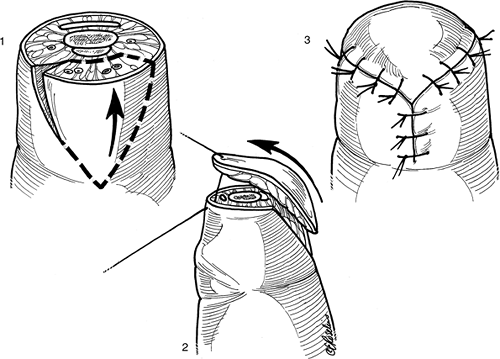
The shortening of the osseous phalanx to obtain satisfactory soft tissue coverage is illustrated in Figure 14-5.
-
After shortening the bone and smoothing
its edges with a rasp to round its contour, dorsal and palmar flaps are
fashioned and then closed in the coronal plane. -
The key to closure by this method is to shorten the bone sufficiently to achieve closure of the skin and soft tissues without tension.
-
Prior to closure, the digital nerves are
identified and gently retracted distally and cut with a scalpel so that
they retract proximally into the soft tissues.
Closure by Skin Graft
-
Split-thickness skin graft may be used to promote rapid healing of fingertip amputations.
-
The use of a split-thickness skin graft
removed from the forearm with a sterile razor blade and sutured into
place over the defect is shown in Figure 14-6. Rapid healing occurred.-
It might be argued that sterile dressings
(without a skin graft) might have achieved the same end result, but it
may have taken a little longer.
-
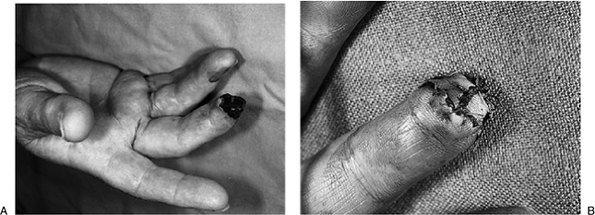
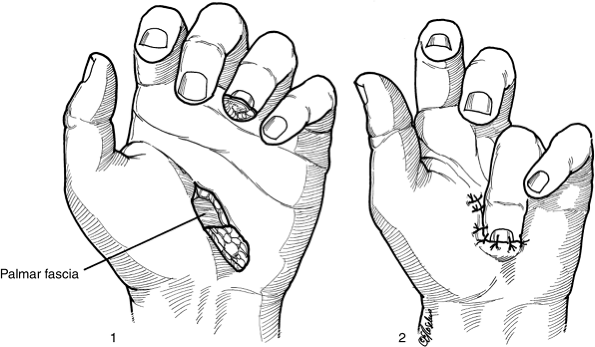
Caveat: Figure 14-7
illustrates the result of a skin graft removed from the forearm of an
African American and sutured to a skin loss defect at the tip of his
index finger. This resulted in a poor color match, and should be
avoided. Figure 14-7B shows a suitable
location for removal of a full-thickness skin graft with a suitable
color match. The longitudinal axis of the graft is parallel and in the
proximal palmar crease. The resultant defect may be closed after
limited
illustrates the result of a skin graft removed from the forearm of an
African American and sutured to a skin loss defect at the tip of his
index finger. This resulted in a poor color match, and should be
avoided. Figure 14-7B shows a suitable
location for removal of a full-thickness skin graft with a suitable
color match. The longitudinal axis of the graft is parallel and in the
proximal palmar crease. The resultant defect may be closed after
limited
P.230
excision
of the palmar fascia in the base of the wound and minimal undermining
of the edges. Another suitable source of skin graft is from the
“instep” region of the plantar surface of the foot.
 |
|
Figure 14-4 A, B. A high-speed router blade removed the distal and dorsal aspect of this self-employed carpenter’s left middle finger. C. Rapid healing with good tissue coverage was achieved by “folding over” the remaining portions of the terminal phalanx.
|
Figure 14-8 shows a young
African American female with skin loss at the tip of her left thumb,
which was treated by application of a full-thickness skin graft from
the “instep” on the plantar surface of her foot. The skin graft and
donor site healed with minimal scarring, and a good color match was
achieved.
African American female with skin loss at the tip of her left thumb,
which was treated by application of a full-thickness skin graft from
the “instep” on the plantar surface of her foot. The skin graft and
donor site healed with minimal scarring, and a good color match was
achieved.
Closure by Local Flaps
Local flaps include the VY-plasty, the Kutler, and the Moberg advancement flaps.
VY-Plasty
-
This flap is used for closing transversely oriented amputations, and is an alternative to the “fishmouth” closure. Figure 14-9
shows a patient with a three-finger amputation who was treated with a
VY-plasty in the ring and index fingers and with a fishmouth closure in
the middle finger. -
A V-shaped flap is developed as shown in Figure 14-9B, and is mobilized and advanced distally to form a Y-shaped configuration.
-
Mobilization of the V is carefully performed to avoid loss of its blood supply.
-
Bone shortening is used as required.
-
Figure 14-9C
demonstrates the end result of the VY-plasty in the index and ring
fingers, and the end result of the “fishmouth” closure in the middle
finger. -
The VY technique is depicted in Figure 14-10.
The Kutler Bilateral VY Advancement Flaps
-
This bilateral flap is also a VY advancement flap that is formed on both sides of the digit.
-
The flaps are advanced to meet in the midline of the amputation.
-
Figure 14-11 illustrates the technique, and Figure 14-12 shows a clinical example.
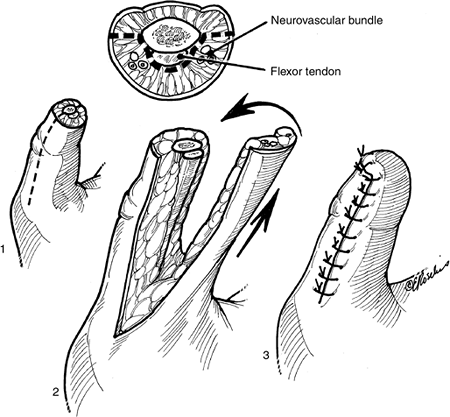
The Volar Advancement Flap
-
This flap is also known as the Moberg flap.
-
It is a palmar neurovascular advancement
flap that has the potential for excellent sensibility for, and
substantial coverage of, an amputated digit. -
It is ideally used in the thumb, and may
not be successful in the fingers for a variety of reasons, including
flexion contracture and occasional loss of vascularity in the flap.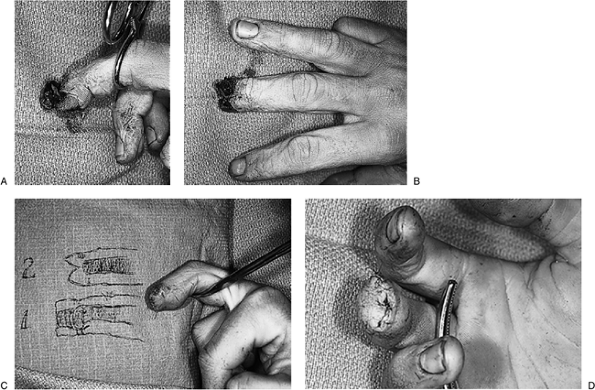 Figure 14-5 A, B. Preoperative and injury views of a crush injury to the terminal phalanx of the right middle finger. C, D.
Figure 14-5 A, B. Preoperative and injury views of a crush injury to the terminal phalanx of the right middle finger. C, D.
Revision was accomplished by shortening the osseous phalanx and closing
the wound using the “fishmouth” technique, which consists of the
formation of dorsal and palmar flaps that are sutured together in the
midline. -
Figure 14-13 shows the excellent coverage that can be obtained with this advancement flap.
-
The details of the technique are depicted in Figure 14-14.
P.231
Closure by Distant Pedicle Flaps
Thenar Flap
-
This distant pedicle flap is useful for
covering the distal aspect of the index and middle fingers, and, like
other distant pedicle flaps, is intended to maintain the length of the
digit. -
This flap is best used in those patients
who do not have any proclivity for joint stiffness. Some have indicated
that it is best used in younger patients who do not have as significant
a potential for stiffness as older patients.
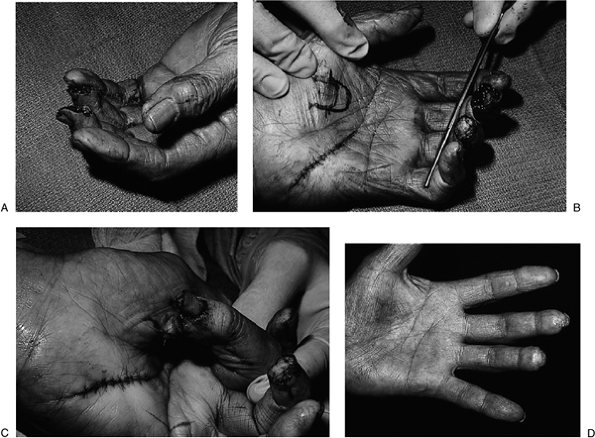
Figure 14-15 shows a clinical
sequence of a male Pacific Islander with amputations of the tips of the
middle and ring fingers. Significant loss of pulp was noted in the
middle finger. A thenar flap was used to restore the pad on the middle
finger, and a full-thickness skin graft from the hypothenar eminence
was used to cover the amputation at the tip of the ring finger. This
graft site was selected as a ready source of full-thickness skin that
provided durable coverage for the palmar side of the finger. It also
provided an excellent color match for this dark-skinned patient. The
end result is noted in Figure 14-15D. A good
color match is noted in both digits, the flap and full-thickness donor
sites are barely noticeable, and good hand function was recovered. Figure 14-16 is an artist’s depiction of the technique.
sequence of a male Pacific Islander with amputations of the tips of the
middle and ring fingers. Significant loss of pulp was noted in the
middle finger. A thenar flap was used to restore the pad on the middle
finger, and a full-thickness skin graft from the hypothenar eminence
was used to cover the amputation at the tip of the ring finger. This
graft site was selected as a ready source of full-thickness skin that
provided durable coverage for the palmar side of the finger. It also
provided an excellent color match for this dark-skinned patient. The
end result is noted in Figure 14-15D. A good
color match is noted in both digits, the flap and full-thickness donor
sites are barely noticeable, and good hand function was recovered. Figure 14-16 is an artist’s depiction of the technique.
Cross-Finger Flap
-
The cross-finger flap is another
technique to cover the tip of an amputated finger; as with other flaps,
it is designed to maintain finger length and cover the defect with
durable and sensate skin. -
It is very useful for restoring the loss of the pulp on the flexor aspect of the finger.
-
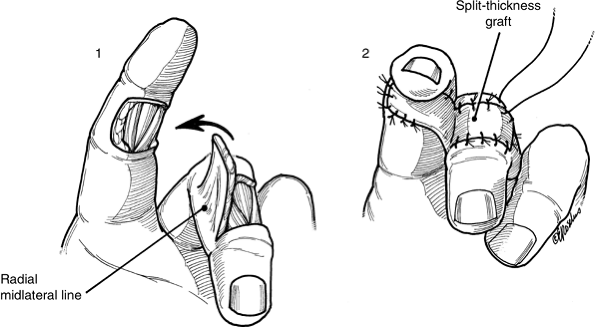
Figure 14-17
depicts the sequence of a cross-finger flap used to restore an avulsion
of the pulp lost on the flexor surface of the terminal phalanx on the
left little finger.![]() Figure 14-6 A. The clinical appearance of a skin defect on the ulnar side of the terminal phalanx of the left ring finger. B. A sterile razor blade is used to remove a split-thickness skin graft from the forearm. C.
Figure 14-6 A. The clinical appearance of a skin defect on the ulnar side of the terminal phalanx of the left ring finger. B. A sterile razor blade is used to remove a split-thickness skin graft from the forearm. C.
The skin graft is sutured into place, and the tails of the suture are
left long enough to tie over a cotton stent (not shown) in order to
keep the graft firmly applied to its bed. D. A complete take of the graft was noted at 10 days.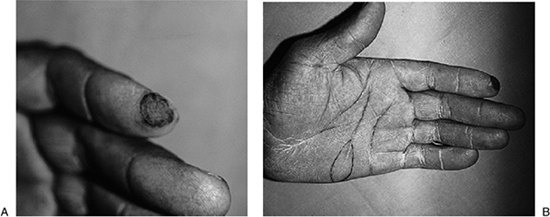 Figure 14-7 A.
Figure 14-7 A.
This African American male had a split-thickness skin graft removed
from his forearm and applied to a defect at the tip of his left index
finger. Note the poor color match. B. Area of a more suitable donor site.![]() Figure 14-8 A. This young African American female had a skin defect on the tip of her left thumb. B. A full-thickness skin graft was removed from the “instep” region of the plantar surface of her foot and closed primarily. C. The graft was sutured in place over the defect beneath a stent, with excellent healing and color match.
Figure 14-8 A. This young African American female had a skin defect on the tip of her left thumb. B. A full-thickness skin graft was removed from the “instep” region of the plantar surface of her foot and closed primarily. C. The graft was sutured in place over the defect beneath a stent, with excellent healing and color match. -
The pedicle flap is raised from the
dorsum of the adjacent ring finger down to the paratenon of the
extensor mechanism, and it includes the skin and subcutaneous tissue. -
The flap is hinged on the ulnar side of the ring finger, and then sutured to the defect on the little finger.
-
The defect on the ring finger is covered with a moderately thick, split-thickness skin graft.
-
The flap is divided in 12 to 14 days, and the free margin further inset into the defect.
-
Figure 14-18 is an artist’s depiction of the cross finger pedicle flap.
P.232
P.233
Nail Bed Injuries
Subungual Hematoma
-
Subungual hematoma may occur following
crushing-type injuries due to the abundant blood supply of the nail
bed. It may cause severe pain in the digit. It is discussed here
because of its association with fingertip injuries. -
Drainage of the hematoma with the incandescent end of a paper clip is a painless way to relieve this condition.
-
A radiograph to rule out an associated fracture is useful.
-
Some have argued that draining a
subungual hematoma in the presence of a fracture may result in an “open
fracture,” but if a fracture is present by radiograph, sterile
dressings may be used until the drainage site closes.
Lacerations and Avulsions
-
Nail-bed injuries may occur in conjunction with digit amputations.
-
They may occur as simple or complex lacerations and avulsions.
-
The nail plate may be present in whole or
part, and should not be discarded. Instead, it should be used as a
stent following the repair of the nail bed. -
Secondary or delayed reconstruction of
these injuries is unpredictable, and the best results are achieved by
treatment at the time of the initial injury.
Lacerations
-
Some surgeons advocate removal of an
attached or partially intact nail plate to facilitate the repair of the
underlying nail bed. -
In most cases, however, it may be left in
place, where it will act as a biologic stent to recontour and promote
the healing of the underlying laceration. Often, the nail is partially
avulsed and elevated from its bed. In those cases, the nail may be
removed and saved for later reapplication as a biologic stent. -
Simple lacerations of the nail bed are repaired under digital anesthesia and a suitable tourniquet.
-
Loupe magnification is useful, and the laceration is sutured with 6-0 or 7-0 chromic or plain gut.
-
Following repair, the nail plate is replaced over the repaired nail bed and under the proximal nail fold.
-
This will act as a biologic stent, and will help to contour the nail bed.
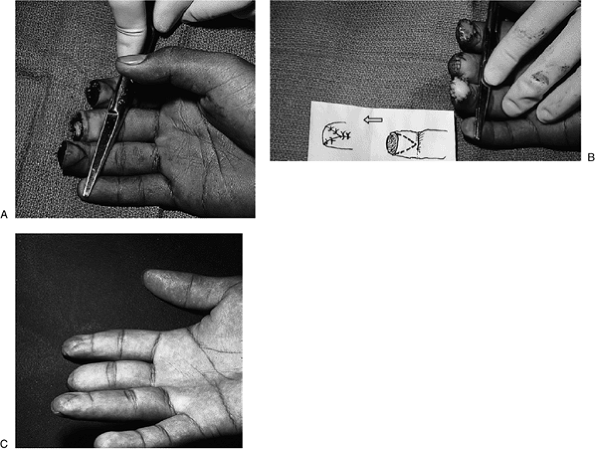 Figure 14-9 A. Triple amputation in a patient’s right hand. B.
Figure 14-9 A. Triple amputation in a patient’s right hand. B.
A VY-plasty has been performed on the index and ring fingers, and a
“fish-mouth” closure has been performed on the middle finger. C. Note the final result in the three fingers.![]() Figure 14-10
Figure 14-10
Artist’s depiction of the VY-plasty technique. The technique is most
useful in transverse amputations. Bone shortening is performed as
required.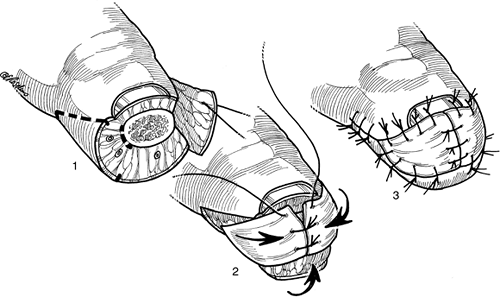 Figure 14-11 Artist’s depiction of the Kutler bilateral VY-plasty technique for fingertip amputations.
Figure 14-11 Artist’s depiction of the Kutler bilateral VY-plasty technique for fingertip amputations. -
Replacement of the nail plate will prevent scar formation between the proximal nail fold and the bed.
-
If the nail is not available, a thin
piece of sterile silicone sheet may be cut to duplicate its shape and
may be inserted as a replacement. -
The replaced nail will be pushed out as the new nail grows.
-
Local wound care and dressings are used to protect the nail bed until the new nail plate covers the matrix.
P.234
P.235
Avulsions
-
Small avulsion defects may be repaired by undermining and advancing the surrounding nail bed to close the defect.
-
If a portion of the nail bed remains
attached to the undersurface of the nail, it may be reapplied to fill
the defect as a free graft.![]() Figure 14-12 A clinical example of the Kutler bilateral VY-plasty.
Figure 14-12 A clinical example of the Kutler bilateral VY-plasty. -
If insufficient tissue is available, the
great toe can be used with minimal morbidity. The toenail is removed,
and a split graft is removed from the nail bed. -
A split graft satisfies the needs of the injured nail bed, and allows healing of the great toe nail bed without side effects.
-
The graft is sutured into the defect with fine absorbable sutures as previously described.
Late Reconstruction
-
Nail deformities may occur in spite of
appropriate treatment, and may be related more to the nature of the
original injury than the treatment. -
Common deformities seen are hook nails, split nails and non-adherent nails.
Hook Nail
-
Loss of bony support to the distal aspect
of the nail bed and plate often results in “hooking,” in which the
distal aspect of the nail grows towards the palm.P.236P.237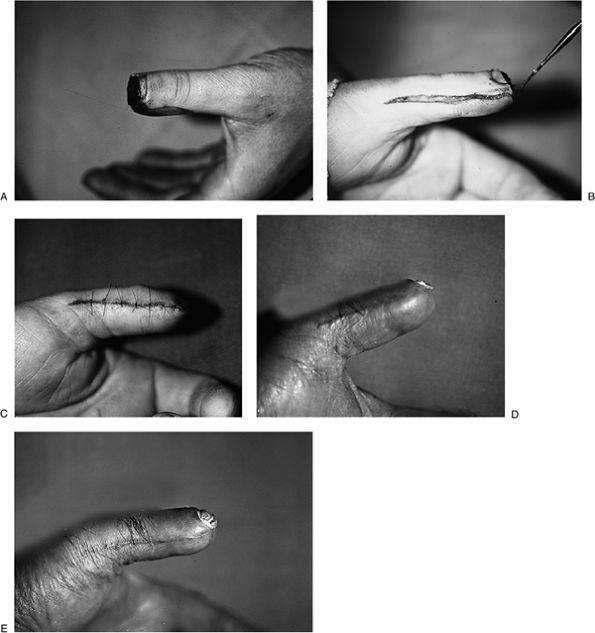 Figure 14-13 The Moberg advancement flap for thumb tip amputations. A. Note the transverse amputation through the distal aspect of the left thumb. B.
Figure 14-13 The Moberg advancement flap for thumb tip amputations. A. Note the transverse amputation through the distal aspect of the left thumb. B.
A skin hook is used to gently advance the flap that has been incised
bilaterally. The flap includes the neurovascular bundles, and is
released down to the level of the flexor sheath. C.
The distal margin of the flap has been advanced to meet the distal edge
of the thumbnail, and has been sutured in place with slight flexion of
the interphalangeal (IP) joint to facilitate a tension-free closure. D, E. Note the excellent pad over the tip of the thumb.![]() Figure 14-14
Figure 14-14
Artist’s depiction of the Moberg advancement flap. The bilateral
midaxial incision is carried to the region of the osseous structures
and flexor sheath, and the neurovascular bundle is protected in the
flap. -
This can be corrected by removing the nail and trimming the matrix back to the level of the bony support.
-
The defect is then closed with an advancement flap without placing any tension on the matrix.
Split and Nonadherent Nail
-
Split nails result from a longitudinal scar in the matrix, with an absence of nail-producing cells.
-
If the scar is in the dorsal matrix, only
a dull streak may appear in the nail plate. If the scar is in the
intermediate portion of the germinal matrix, a split or absent nail may
occur. If the scar is in the palmar nail or sterile matrix, a split or
non-adherence of the nail beyond the scar may occur. -
Nonadherent nails may result from scarring of the germinal matrix, or from a scar in the sterile matrix.
-
Treatment involves excising the scar and replacing it with nail matrix.
-
Typically, if the defect is large enough to cause a split nail, it cannot be closed primarily and will need a graft.
-
If the defect is in the sterile matrix, it can be treated with a split-thickness graft.
-
The germinal matrix requires a
full-thickness graft, which can be taken from the second toe. This will
result in a cosmetic defect of a lesser degree than by using the great
toe, and still provide adequate matrix for nail regeneration.
-
-
A nonadherent nail typically results from scar in the sterile matrix.
-
This is similarly treated with excision of the scar and placement of a split-thickness matrix graft.
-
-
In severely deformed or bothersome split
or loose nails, another option is to remove the entire nail unit and
replace it with a split-thickness skin graft.
Replantation
Indications
Indications for replantation have been refined since the
first successful limb reattachment was performed in 1962. The current
indications for digital replantation are patients with multiple digit
amputations, thumb amputations, pediatric patients with amputations,
and single digit amputations distal to the
insertion of the flexor digitorum superficialis tendon. Multilevel
amputations offer a greater technical challenge, but may not represent
an absolute contraindication to replantation.
first successful limb reattachment was performed in 1962. The current
indications for digital replantation are patients with multiple digit
amputations, thumb amputations, pediatric patients with amputations,
and single digit amputations distal to the
insertion of the flexor digitorum superficialis tendon. Multilevel
amputations offer a greater technical challenge, but may not represent
an absolute contraindication to replantation.
Factors such as associated injuries, age, and associated
systemic illness all play a role in the decision-making process.
Avulsion injuries, and those with massive contamination, may preclude a
successful result.
systemic illness all play a role in the decision-making process.
Avulsion injuries, and those with massive contamination, may preclude a
successful result.
Timing
Muscle tissue is susceptible to irreversible changes
after 6 hours of ischemia at room temperature. Digits do not contain
muscle, and thus their warm ischemia time is much longer. Successful
replantations in digits have occurred after 33 hours of warm ischemia
time, and after 94 hours of cold ischemia. These recorded times are at
the extreme end of the spectrum of allowable elapsed times prior to
replantation; do not take them as an acceptable norm. Thus,
transportation of the patient and the amputated part should be as rapid
as possible to a center with a replantation capability. When the part
has been properly cooled, successful replantation has been achieved in
patients after 24 to 30 hours.
after 6 hours of ischemia at room temperature. Digits do not contain
muscle, and thus their warm ischemia time is much longer. Successful
replantations in digits have occurred after 33 hours of warm ischemia
time, and after 94 hours of cold ischemia. These recorded times are at
the extreme end of the spectrum of allowable elapsed times prior to
replantation; do not take them as an acceptable norm. Thus,
transportation of the patient and the amputated part should be as rapid
as possible to a center with a replantation capability. When the part
has been properly cooled, successful replantation has been achieved in
patients after 24 to 30 hours.
P.238
 |
|
Figure 14-15 The thenar flap and color-matched, full-thickness skin graft. A. Note the significant loss of pulp in the middle finger, and the loss of skin over the tip of the ring finger. B.
A full-thickness skin graft was harvested from the hypothenar eminence, the defect closed, and the graft sutured to the ring finger; note the generous length of the thenar flap. C. The thenar flap has been elevated and attached to the tip of the middle finger. D. Note the excellent functional and cosmetic result. |
 |
|
Figure 14-16 Artist’s depiction of the technique for the thenar flap.
|
P.239
 |
|
Figure 14-17 The cross-finger pedicle flap.
|
Steps in Replantation
-
The amputated part must be located and
sent with the patient to the most appropriate emergency room. Placing
the amputated part in a small plastic bag and laying it on ice is
advisable. The part should not be frozen (no dry ice) or otherwise manipulated. -
Ideally, after the patient arrives at the emergency room, an on-call replantation team would divide into two treatment units.
-
One team takes the amputated part to the
operating room where it is cleaned as needed and kept cool and moist.
This team debrides the amputated part as needed and identifies and tags
vital structures, including nerves, veins, arteries and tendons. -
The other team should assess the patient
with a medical history and physical examination, obtain appropriate
laboratory studies, and start general supportive measures as indicated.
-
-
The details of the replantation procedure
is beyond the scope of this text, but they include the shortening and
fixation of the bone, repairing flexor and extensor tendons,
anastomosis of one or more arteries and two veins, repairing the
nerves, and skin coverage.P.240P.241![]() Figure 14-18 Artist’s depiction of the cross finger flap.
Figure 14-18 Artist’s depiction of the cross finger flap.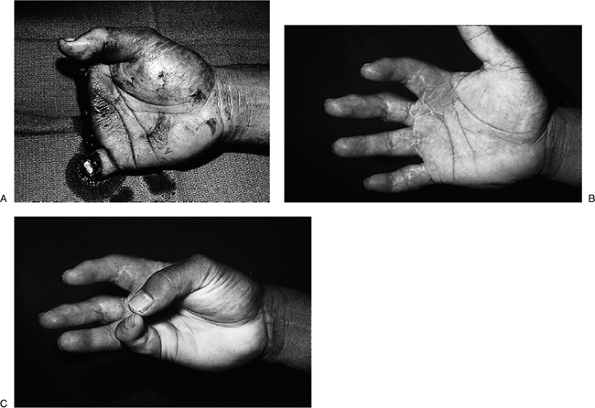 Figure 14-19 Four-finger amputation and successful replantation. A. This 34-year-old print shop worker sustained a traumatic amputation of four fingers in a paper cutter. B. Successful reattachment was achieved of all four digits. C. He regained useful function and sensibility in the hand and returned to work in the print shop.
Figure 14-19 Four-finger amputation and successful replantation. A. This 34-year-old print shop worker sustained a traumatic amputation of four fingers in a paper cutter. B. Successful reattachment was achieved of all four digits. C. He regained useful function and sensibility in the hand and returned to work in the print shop. -
Postoperative care includes aspirin for
its antiplatelet effect, and some form of anticoagulant therapy of the
surgeon’s choice. The patient should not be allowed to smoke or drink
caffeinated beverages. -
Postoperative monitoring may be
accomplished by noting clinical signs such as color, pulp turgor, and
capillary refill. However, skin temperature measurements or pulse
oximetry may be more reliable. -
Figure 14-19 illustrates a typical replantation patient.
Suggested Reading
Atasoy E, Godfrey A, Kalisman M. The antenna procedure for the “hook-nail” deformity. J Hand Surg 1983;8:55–58.
Atasoy
E, Ioalimidis, Kasdan ML, Kutz JE. Reconstruction of the amputated
fingertip with a triangular volar flap. J Bone Joint Surg
1970;52A:921–926.
E, Ioalimidis, Kasdan ML, Kutz JE. Reconstruction of the amputated
fingertip with a triangular volar flap. J Bone Joint Surg
1970;52A:921–926.
Chang
J, Jones N. Twelve simple maneuvers to optimize digital replantation
and revascularization. Tech in Hand Upper Extremity Surgery
2004;8:161–166.
J, Jones N. Twelve simple maneuvers to optimize digital replantation
and revascularization. Tech in Hand Upper Extremity Surgery
2004;8:161–166.
Chow SP, Ho E. Open treatment of fingertip injuries in adults. J Hand Surg 1982;7:470–476.
Cronin TD. The cross finger flap: a new method of repair. Am Surg 1951;17:419–425.
Das SK, Brown HG. Management of lost finger tips in children. Hand 1978;10:16–27.
Flatt AE. The thenar flap. J Bone Joint Surg 1957;39B:80–85.
Graham
B. Major replantation versus revision amputation and prosthetic fitting
in the upper extremity: a late functional outcomes study. J Hand Surg
1998;23:783–791.
B. Major replantation versus revision amputation and prosthetic fitting
in the upper extremity: a late functional outcomes study. J Hand Surg
1998;23:783–791.
Kumar VP, Satku K. Treatment and prevention of “hook nail” deformity with anatomic correlation. J Hand Surg 1993;18A:617–620.
Kutler W. A new method for finger tip amputation. JAMA 1947; 133:29–30.
Moberg E. Aspects of sensation in reconstructive surgery of the upper extremity. J Bone Joint Surg 1964; 46A:817–825.
Yong FC, Teoh LC. Nail bed reconstruction with split-thickness nail bed grafts. J Hand Surg 1992;17B:193–197.