Abnormalities of Movement
involve any portion of the body. They usually result from disease
involving various parts of the motor system, and the etiologies are
many. The character of the movement depends on both the site of the
lesion and the underlying pathology. Movement disorders disrupt motor
function not by causing weakness but by producing either abnormal,
involuntary, unwanted movements (hyperkinetic movement disorders), or
by curtailing the amount of normal free flowing, fluid movement
(hypokinetic movement disorders).
Parkinson disease (PD). Other disease processes may produce a similar
clinical picture, characterized by decreased movement and rigidity;
these have been grouped together as the akinetic-rigid syndromes. About
80% of the instances of akinetic-rigid syndrome are due to PD (Table 21.1).
The terms parkinson syndrome or parkinson plus are sometimes used to
designate such other disorders, and the features that resemble PD are
referred to as parkinsonism, or parkinsonian. Parkinsonism is a
clinical diagnosis appropriate in the presence of resting tremor,
bradykinesia, rigidity, and impaired postural reflexes. Parkinson
disease is but one cause of parkinsonism, and it must be differentiated
from other conditions that may have some of its typical features as a
component of another disorder.
the dopaminergic nigrostriatal pathway. It is the second most common
movement disorder behind essential tremor. Cardinal manifestations
include bradykinesia, rigidity, tremor, an expressionless face, and
postural instability. Asymmetry is characteristic. The disease often
begins asymmetrically; the signs may be so lateralized as to warrant
the designation of hemi-PD, and some asymmetry usually persists even
when the disease is well established. The major manifestations vary
from case to case.
which principally affects the axial muscles and the proximal and flexor
groups of the extremities, causing an increased tone to passive
movement. The rigidity has a rhythmic quality referred to as cogwheel
rigidity, presumably due to the superimposition of the tremor.
Cogwheeling may be brought out as the examiner passively moves an elbow
or wrist by having the patient grit the teeth, look at the ceiling, or
use the opposite hand to make a fist, trace circles in the air, or
imitate throwing a ball. The rigidity is present evenly throughout the
range of movement, without the ebb at the extremes of the range that
occurs in spasticity.
|
TABLE 21.1 The Differential Diagnosis of Parkinson Disease
|
||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||
movements. Strictly speaking, akinesia means an absence of movement,
bradykinesia a slowness of movement, and hypokinesia a decreased amount
or amplitude of movement, but the term bradykinesia is often used to
encompass all three. There is loss of associated and automatic
movements, with masking of the face, infrequent smiling and blinking,
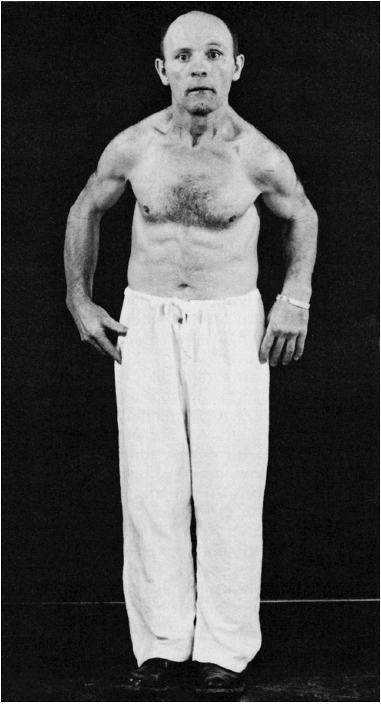
and loss of swinging of the arms in walking (Figure 21.1).
and difficulty walking. The gait abnormality is stereotypical: slow and
shuffling with a reduced stride length, sometimes markedly so, a
stooped flexed posture of the body and extremities, reduced arm swing,
and a tendency to turn “en-bloc.” Impaired postural reflexes lead to a
tendency to fall forward (propulsion), which the patient tries to avoid
by walking with increasing speed but with very short steps, the
festinating gait. Falls are common. If a patient, standing upright, is
gently pushed either backward or forward, she cannot maintain balance
and will fall in the direction pushed. Facial immobility and lack of
expressiveness is a common feature of PD (hypomimia, masked face). A
decreased rate of blinking, accompanied by slight eyelid retraction,
causes patients to have a staring expression (reptilian stare). The
voice is typically soft, breathy, monotonous, and tremulous. Other
common manifestations include hyperhidrosis, greasy seborrhea,
micrographia, somnolence, difficulty turning over in bed,
blepharospasm, and apraxia of eyelid opening. Oculogyric crisis, forced
involuntary eye deviation, usually upward, is a feature of
postencephalitic PD and can occur in drug-induced parkinsonism, but it
does not happen in idiopathic PD. Other common manifestations include
foot dystonia, “striatal toe,” an exaggerated glabellar tap reflex
(Myerson sign), and impaired handwriting (especially micrographia).
Advancing disease is characterized by increasing gait difficulty,
worsening of tremor and bradykinesia, motor fluctuations related to
levodopa therapy, behavioral changes, cognitive impairment,
hallucinations, intractable drooling, and sleep impairment. The
impairment of cognition in PD is extremely variable, ranging from
minimal involvement to profound dementia. Some degree of cognitive
blunting may occur in 20% to 40% of patients. Early, prominent, and
nonvisual hallucinations raise the possibility of dementia with Lewy
bodies.
 |
|
FIGURE 21.1 • A patient with Parkinson disease, showing rigidity, masked facies, and typical posture.
|
differential diagnosis essentially is between other conditions causing
tremor, of which essential tremor is the commonest, and other
akinetic-rigid syndromes. Clinical features that favor PD include
prominent rest tremor, asymmetric signs, preservation of balance and
postural reflexes in the early stages of the disease, and a good
response to levodopa replacement therapy. The other degenerative
disorders with parkinsonian features typically produce other neurologic
signs, such as gaze limitation, cerebellar signs, pyramidal signs,
severe dementia, apraxia and other parietal lobe signs, or
dysautonomia, although these other manifestations may not be apparent
early in the course. Certain drugs can induce a reversible condition
that mimics PD. The most common agents that cause drug-induced
parkinsonism are antipsychotics, especially the high-potency piperazine
compounds such as haloperidol. Some of the other conditions important
in the differential diagnosis of PD include multiple system atrophy,
progressive supranuclear palsy, corticobasal degeneration, and diffuse
Lewy body disease.
rare, autosomal recessive disorder due to abnormal copper deposition in
the brain. The usual age of onset is between the ages of 10 and 20, and
major manifestations include tremor, rigidity, dystonia and abnormal
involuntary movements of various types, dysarthria, dementia,
parkinsonian features, spasticity, cerebellar signs, and psychiatric
abnormalities (anxiety, depression, psychosis). Kayser-Fleischer rings
are crescents of green-brown discoloration of the cornea due to copper
deposits in Descemet membrane; these are essentially always present in
patients with neurologic involvement but may not be visible without a
slit lamp. Hallervorden-Spatz syndrome, or neurodegeneration with brain
iron accumulation type-1, is a rare, autosomal recessive disorder
associated with macroscopic rust-brown discoloration of the globus
pallidus and substantia nigra due to iron deposition. The clinical
phenotype is variable but usually includes rigidity, involuntary
movements, ataxia, and dystonia.
|
TABLE 21.2 Abnormal Involuntary Movements as a Spectrum of Movements
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
are abnormal involuntary movements that occur in a host of neurologic
conditions. Hyperkinesias come in many forms, ranging from tremor to
chorea to muscle fasciculations to myoclonic jerks. Any level of the
motor system, from the motor cortex to the muscle itself, may be
involved in their production. The only common characteristic is that
the movements are spontaneous and, for the most part, not under
volitional control. They may be rhythmic or random, fleeting or
sustained, predictable or unpredictable, and may occur in isolation or
accompanied by other neurologic signs. Table 21.2 summarizes some of these features.
should be noted: (a) the part of the body involved; (b) the extent or
distribution of the movement; (c) the pattern, rhythmicity, and
regularity; (d) the course, speed, and frequency; (e) the amplitude and
force of the movement; (f) the relationship to posture, rest, activity,
various stimuli, fatigue, and time of day; (g) the response to heat and
cold; (h) the relationship to the emotional state; (i) the degree that
movements are suppressible by attention or the use of sensory tricks;
and (j) the presence or absence of the movements during sleep. In
general, involuntary movements are increased by stress and anxiety and
decrease or disappear with sleep. Truly involuntary movements must be
separated from complex or bizarre voluntary movements, such as
mannerisms or compulsions.
rhythmic, purposeless, oscillatory movements. The excursion may be
small or large, and may involve one or more parts of the body. A simple
tremor involves only a single muscle group; a compound tremor involves
several muscle groups and may have several elements in combination,
resulting in a series of complex movements. A tremor may be present at
rest or with activity. Some tremors are accentuated by having the
patient hold the fingers extended and separated with the arms
outstretched. Slow movements, writing, and drawing circles or spirals
may bring tremor out.
rate, amplitude, rhythmicity, relationship to rest and movement,
etiology, and underlying pathology. Other important factors may include
the relationship to fatigue, emotion, self-consciousness, heat, cold,
and the use of medications, alcohol, or street drugs. Tremor may be
unilateral or bilateral and most commonly involves distal parts of the
extremities—the fingers or hands—but may also affect the arms, feet,
legs, tongue, eyelids, jaw, and head, and may occasionally seem to
involve the entire body. The rate may be slow, medium, or fast.
Oscillations of 3 to 5 Hz are considered slow, 10 to 20 Hz rapid.
Amplitude may be fine, coarse, or medium. Tremor may be constant or
intermittent, rhythmic or relatively nonrhythmic, although a certain
amount of rhythmicity is implied in the term tremor. Irregular “tremor”
may be due to myoclonus.
classification into two primary tremor types: rest and action. Resting
(static) tremors are present mainly during relaxation (e.g., with the
hands
in
the lap), and attenuate when the part is used. Rest tremor is seen
primarily in PD and other parkinsonian syndromes. Action tremors appear
when performing some activity. Action tremors are divided into
subtypes: postural, kinetic, task-specific, and isometric. Only when
they are very severe are action tremors present at rest. Postural
tremors become evident when the limbs are maintained in an antigravity
position (e.g., arms outstretched). Common types of postural tremor are
enhanced physiologic tremor and essential tremor (ET). Kinetic tremor
appears when making a voluntary movement, and may occur at the
beginning, during, or at the end of the movement. The most common
example is an intention (terminal) tremor. Intention tremor is a form
of action tremor seen primarily in cerebellar disease. The tremor
appears when precision is required to touch a target, as in the
finger-nose-finger or toe-to-finger test. It progressively worsens
during the movement. Approaching the target causes the limb to shake,
usually side-to-side perpendicular to the line of travel, and the
amplitude of the oscillation increases toward the end of the movement.
Some tremors fall into more than one potential classification. Most
tremors are accentuated by emotional excitement, and many normal
individuals develop tremor with anxiety, apprehension, and fatigue.
frequency varies from 8 to 12 Hz, averaging about 10 Hz in the young
adult, somewhat slower in children and older persons. The visible
tremor brought out in normal persons by anxiety, fright, and other
conditions with increased adrenergic activity is accentuated or
enhanced physiologic tremor. A typical example of enhanced physiologic
tremor is that seen in hyperthyroidism. The tremor involves principally
the fingers and hands, and may be fine and difficult to see. Similar
tremor occurs due to the effects of alcohol, nicotine, caffeine,
amphetamines, ephedrine, and other stimulants (Table 21.3).
|
TABLE 21.3 Some Drugs that Cause Tremor
|
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
but may be coarse when severe. The intention tremor of multiple
sclerosis (MS) and cerebellar disease is usually of medium amplitude
and may vary in degree from mild to severe; it may be coarse and
irregular, especially when associated with ataxia. Coarse tremors occur
in a variety of disease states, and are usually slow. Parkinsonian
tremor is one of the most characteristic. Coarse tremor also occurs in
Wilson disease and other extrapyramidal syndromes. The tremor of
general paresis and alcoholism may also be coarse, especially if the
movements are diffuse, as in delirium tremens. Psychogenic tremor and
the tremor associated with midbrain and cerebellar disease may also be
coarse and slow. Two of the commonest causes of tremor are PD and ET.
frequently in diseases of the basal ganglia and extrapyramidal
pathways. The most characteristic tremor of this type is seen in PD and
the various parkinsonian syndromes. The tremor of PD is fairly
rhythmic, gross, from 2 to 6 Hz, and may involve the hands, feet, jaw,
tongue, lips, and pharynx, but not the head. It is typically a resting
tremor that lessens during voluntary movement and disappears in sleep.
The tremor fluctuates, increasing in amplitude but not rate when the
patient becomes excited. The tremor often is more apparent when the
patient is walking. The movement in the hand characteristically
consists of alternate contractions of agonist and antagonist, involving
the flexors, extensors, abductors, and adductors of the fingers and
thumb, together with motion of the wrist and arm. As a result there is
a repetitive movement of the thumb on the first two fingers, together
with the motion of the wrist, producing the classical pill-rolling. The
tremor may be unilateral at onset; it may even begin in a single digit,
but in most cases eventually becomes bilateral.
disorders, and is often familial. Senile tremor is ET occurring during
senescence with a negative family history. Essential tremor is higher
in frequency and lower in amplitude than the tremor of PD. There is a
postural and action tremor that tends to affect the hands, head, and
voice. It is made worse by anxiety. A common problem is differentiating
the tremor of early PD from ET. The tremor of PD is most prominent at
rest, while that of ET occurs with a sustained posture, such as with
the hands outstretched, or on action. Parkinsonian tremor may persist
with hands outstretched but usually damps, at least momentarily, when
making a deliberate movement, whereas ET usually worsens with any
attempt at a precise action. The ET patient may have great difficulty
sipping water from a cup, but the PD patient may do so without spilling
a drop. The head and voice are often involved with ET, only rarely with
PD, although the tremor in PD may involve the lips and jaw. Alcohol and
beta blockers often improve ET but have no effect on parkinsonian
tremor.
purposeless, random, nonrhythmic hyperkinesias. The movements are
spontaneous, abrupt, brief, rapid, jerky, and unsustained. Individual
movements are discrete, but they are variable in type and location,
causing an irregular pattern of chaotic, multiform, constantly changing
movements that seem to flow from one body part to another. The
movements may at times appear purposeful to a casual observer, but they
are actually random and aimless. They are present at rest but are
increased by activity, tension, emotional stress, and
self-consciousness. The patient may be able to temporarily and
partially suppress the movements, and they disappear in sleep.
They may involve one extremity, one half of the body (hemichorea), or
be generalized. They occur most characteristically in the distal parts
of the upper extremities, but may also involve the proximal parts,
lower extremities, trunk,
face,
tongue, lips, and pharynx. When asked to hold the hands outstretched,
there may be constant random movements of individual fingers
(piano-playing movements). If the patient holds the examiner’s finger
in her fist, there are constant twitches of individual fingers
(milkmaid grip). The patient may try to incorporate a spontaneous,
involuntary movement into a semi-purposeful movement in order to mask
the chorea (parakinesia). If a choreic movement suddenly makes a hand
fly upward, the patient may continue the movement and reach up and
scratch her nose. In addition to the abnormal movements, there is
hypotonia of the skeletal muscles, with decreased resistance to passive
movement. The outstretched hands are held with hyperextension of the
fingers with flexion and dorsal arching of the wrist (spooning). Motor
impersistence—the inability to sustain a contraction—frequently
accompanies chorea. The patient is frequently unable to hold the tongue
out for any length of time; when asked to do so, the tongue shoots out,
then jerks back quickly (snake, darting, flycatcher, or trombone
tongue). The blink rate is increased. Many disorders may cause chorea,
among them Huntington disease and Sydenham chorea.
autosomal dominant, neurodegenerative condition that is inexorably
progressive and ultimately fatal. The onset is usually between the ages
of 35 and 50, and the typical course is from 15 to 20 years. Patients
are usually reduced to a vegetative state about 10 to 15 years after
onset.
deterioration. The abnormal movements may affect the larger muscle
groups and the proximal extremities, causing repeated shrugging of the
shoulder or flail-like movements of the arm and twisting and lashing
movements that lie between those of chorea and athetosis. Facial
grimacing may be marked. Movements of the fingers and hands are often
accentuated as the patient walks. Pronounced chorea of the arms and
legs when walking may lead to a bizarre, prancing gait. Cognitive
impairment usually begins at about the same time as the abnormal
movements, but may precede it, and progresses in tandem. Most patients
also develop psychiatric abnormalities, particularly personality
changes and mood disorders.
relationship to streptococcal infection, and has become a rarity in
developed countries. Chorea gravidarum occurs during pregnancy. Chorea
can be seen as a manifestation of many systemic illnesses, such as
systemic lupus erythematosus, hyperthyroidism, nonketotic
hyperglycemia, and others. Chorea may be a transient side effect of
many medications. It may be a persisting feature of past or present
exposure to psychoactive drugs as part of the syndrome of tardive
dyskinesia.
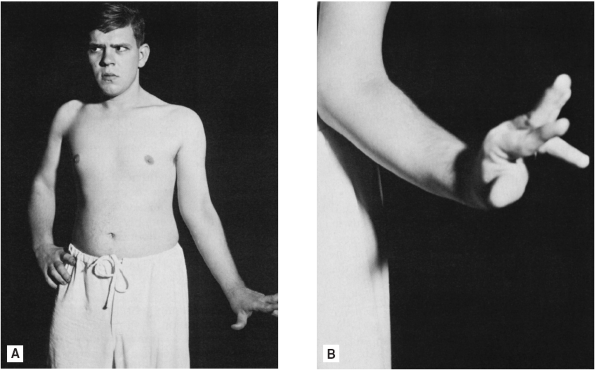
sustained, and larger in amplitude than those in chorea. They are
involuntary, irregular, coarse, somewhat rhythmic, and writhing or
squirming in character. They may involve the extremities, face, neck,
and trunk. In the extremities they affect mainly the distal portions,
the fingers, hands, and toes. The movements are characterized by any
combination of flexion, extension, abduction, pronation, and
supination, often alternating and in varying degrees (Figure 21.2).
They flow randomly from one body part to another, and the direction of
movement changes randomly. The affected limbs are in constant motion.
The movements can often be brought out or intensified by voluntary
activity of another body part (overflow phenomenon). They disappear in
sleep. Voluntary movements are impaired, and coordinated action may be
difficult or impossible. Athetosis is usually congenital, the result of
perinatal injury to the basal ganglia. Choreoathetosis refers to
movements that lie between chorea and athetosis in rate and
rhythmicity, and may represent a transitional form. Slow athetoid
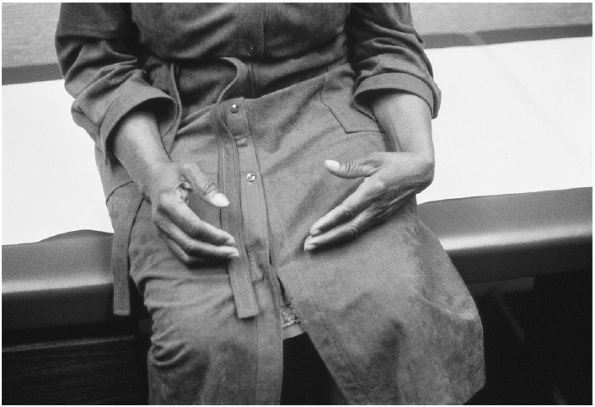
movements begin to blend with dystonia. Pseudoathetosis (sensory
athetosis) is a term used to describe similar undulating
and
writhing movements of the extremities due to loss of position sense as
a result of a parietal lobe lesion, or peripheral deafferentation due
to such conditions as tabes dorsalis, posterolateral sclerosis, and
peripheral nerve disease (Figure 21.3). The movements are more marked when the eyes are closed and are usually unassociated with an increase in muscle tone.
 |
|
FIGURE 21.2 • A patient with congenital unilateral athetosis.
|
muscle contractions that force the affected parts of the body into
abnormal movements or postures, sometimes with co-contraction of
agonists and antagonists. Dystonia often affects the extremities, neck,
trunk, eyelids, face, or vocal cords. It may be either constant or
intermittent, and generalized, segmental, focal, multifocal, or in a
hemi-distribution. Dystonic movements are patterned, tending to recur
in the same location,
in
contrast to the random and fleeting nature of chorea. The speed of
dystonia varies widely, from slow, sustained, and cramp-like (athetotic
dystonia) to quick and flicking (myoclonic dystonia). Action dystonia
occurs when carrying out a voluntary movement. As in athetosis,
overflow may occur, with the dystonia brought out by use of another
part of the body.
 |
|
FIGURE 21.3 • Pseudoathetosis of the hand in a patient with a parietal lobe lesion.
|
similar in many respects to athetosis, but involving larger portions of
the body, often producing distorted postures of the limbs and trunk.
The movements are slow, bizarre, and sometimes grotesque, with an
undulating, writhing, twisting, turning character, and a tendency for
the contraction to be sustained at the peak of the movement (torsion
dystonia, torsion spasm). The term dystonia is sometimes used to
describe the postures or positions assumed by the patient, as well as
for the hyperkinesia itself.
contractions in a limited distribution. A relatively common form of
focal dystonia is cervical dystonia (spasmodic torticollis), which
affects the neck, and sometimes the shoulder, muscles producing either
a sustained or jerky turning of the head to one side, often with some
element of head tilt. “Torti” implies a twisting or turning movement;
less common variants of cervical dystonia include retrocollis
(extension movement) and anterocollis (flexion movement). In the
beginning the twisting and turning may be intermittent or present only
in paroxysms (spasmodic), but later in the course of the syndrome there
is persistent contraction of the involved muscles with resulting
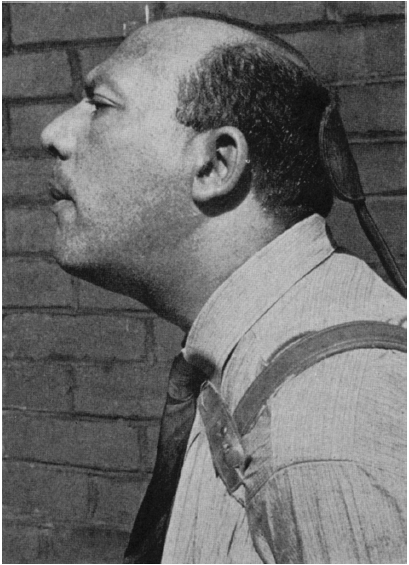
deviation of the head. Many if not most patients with cervical dystonia
learn they can straighten their head by placing a hand or finger
somewhere on the face, or performing some other maneuver to provide
sensory stimulation or light counterpressure (geste antagoniste,
sensory trick, counterpressure sign, Figure 21.4).
 |
|
FIGURE 21.4
• This patient with cervical dystonia causing retrocollis keeps a wooden spoon inserted into his suspenders to keep light counterpressure on the back of his head (geste antagoniste, sensory trick). (Reprinted with permission from Haymaker W. Bing’s Local Diagnosis in Neurological Disease. C.V. Mosby, St. Louis, 1969.) |
forearm muscles brought on by use of the part, most frequently by
writing. There are a number of other focal, occupational, or
task-specific dystonias related to specific activities. Blepharospasm
(upper facial dystonia) causes involuntary closure of both eyes.
Oromandibular dystonia involves the mouth, lips, and jaw. The
combination of blepharospasm and oromandibular dystonia constitutes
Meige (Brueghel) syndrome. Spasmodic dysphonia is dystonia of the vocal
cords.
neurologic syndrome of wild, flinging, incessant movements that occur
on one side of the body, usually due to infarction or hemorrhage in the
region of the contralateral subthalamic nucleus. The ballistic
movements of hemiballismus resemble those of chorea but are more
pronounced. The clinical distinction between severe hemichorea and
hemiballismus becomes arbitrary. Like chorea, hemiballistic movements
are involuntary and purposeless, but they are much more rapid and
forceful and involve the proximal portions of the extremities. When
fully developed, there are continuous, violent, swinging, flinging,
rolling, throwing, flailing movements of the involved extremities. The
movements are ceaseless during the waking state and disappear only with
deep sleep. They are usually unilateral, and involve one entire half of
the body.
but the term is often used to encompass complex involuntary movements
that do not neatly fit into another category. Dyskinesia is used most
often to refer to abnormal involuntary movements related to drugs.
Dyskinesias are a common dose-related complication of the treatment of
PD with levodopa and dopamine agonists. Orofacial dyskinesias are
involuntary movements of the mouth, face, jaw, or tongue that may
consist of grimacing, pursing of the mouth and lips, “fish-gaping”
movements, and writhing movements of the tongue. Tardive dyskinesias
are involuntary movements that usually develop in patients who have
received phenothiazines or related compounds. The movements typically
involve primarily the mouth, tongue, and jaw with incessant chewing,
smacking, licking, and tongue-thrusting movements that are difficult to
eradicate.
motor phenomena. In general, myoclonus may be defined as single or
repetitive, abrupt, brief, rapid, lightning-like, jerky, arrhythmic,
asynergic, involuntary contractions involving portions of muscles,
entire muscles, or groups of muscles. The movements are quicker than
chorea. Myoclonus is seen principally in the muscles of the extremities
and trunk, but the involvement is often multifocal, diffuse, or
widespread. It may involve the facial muscles, jaws, tongue, pharynx,
and larynx. There may be successive or simultaneous involvement of many
muscles. Myoclonus may appear symmetrically on both sides of the body;
such synchrony may be an attribute unique to myoclonus. The sudden,
shock-like contractions usually appear in paroxysms at irregular
intervals, during either the resting or active state, and may be
activated by emotional, mental, tactile, visual, and auditory stimuli.
Myoclonic movements often affect entire muscles or muscle groups,
producing clonic movements of the extremities. They may be so violent
as to cause an entire limb to be suddenly flung out, and may even throw
the patient to the ground. Myoclonus may also be subtle, a quick flick
of a finger or foot.
conditions, and their significance varies. Sleep starts and hiccups are
physiologic forms of myoclonus that occur in normals. Myoclonus is
frequently encountered in epilepsy. Massive myoclonic spasms of infancy
are characterized by frequent, sudden, violent jerking attacks with
flexion of the neck and trunk and adduction or abduction
and
extension of the arms and legs (infantile spasms, West syndrome. The
progressive myoclonic epilepsies are a group of disorders that cause
both generalized seizures and myoclonus. Patients with juvenile
myoclonic epilepsy have generalized tonic-clonic seizures that are
associated with frequent myoclonic jerks predominantly affecting the
arms, especially on awakening. The condition is familial, with both
dominant and recessive forms, and is relatively benign.
of conditions, including metabolic disorders (especially uremic and
anoxic encephalopathy), Creutzfeldt-Jakob disease, Alzheimer disease,
and Huntington disease. Opsoclonus refers to random, chaotic,
lightning-fast eye movements. Opsoclonus accompanied by myoclonus may
occur as a postinfectious encephalopathy or as a paraneoplastic
syndrome, especially due to occult neuroblastoma. Action myoclonus
occurs with use of the involved limb. A syndrome of action or intention
myoclonus may develop as a sequel to cerebral anoxia.
term has also been applied to rhythmic and localized motor phenomena.
Palatal myoclonus is characterized by involuntary, rhythmic movements
of the soft palate and pharynx, sometimes of the larynx, eye muscles,
and diaphragm, and occasionally of other muscles. The movements are
generally not influenced by drugs or sleep. Palatal myoclonus occurs
with lesions involving the connections between the inferior olivary,
dentate, and red nuclei. Palatal myoclonus is also referred to as
palatal microtremor. Tremors are due to alternating agonist-antagonist
contractions, rhythmic myoclonus to contraction-relaxation cycles of an
agonist. In addition, tremors usually disappear in sleep and these
palatal movements do not. Whether palatal myoclonus is best
characterized as rhythmic myoclonus or a tremor remains unclear.
hepatic encephalopathy, asterixis is an inability to sustain normal
muscle tone. With the arms outstretched and wrists extended, “like
stopping traffic,” the lapse in postural tone may cause the hands to
suddenly flop downward, then quickly recover, causing a slow and
irregular flapping motion. When severe, the entire arm may drop.
involuntary movements. In another type of abnormal movement the patient
has some degree of awareness of the movement, but must make a movement
in response to the urge of some compelling inner force. The patient
experiences tension and restlessness, which are temporarily relieved by
making a particular movement. Such movements have been called
“unvoluntary.” Examples include tics, akathisia, stereotypies,
compulsions, and restless legs.
movements that are more often seen in children than adults. A tic may
be defined as a coordinated, repetitive, seemingly purposeful act
involving a group of muscles in their normal synergistic relationships.
Tics are stereotyped, recurrent movements that may seem purposeful but
are relatively involuntary. Patients are able to suppress the movements
temporarily with concentration, but they quickly return when attention
is diverted to some other task. Voluntary suppression causes a sense of
intolerable mounting tension and an urge to move that is temporarily
relieved by indulgence in a tic. Tics are exaggerated by emotional
strain and tension; they cease during sleep.
(maladie des tics) have multifocal tics, compulsive behavior, imitative
gestures, stereotyped movements, grunts and groans, and evidence of
regressive behavior. Tics are very common and usually benign; patients
with Tourette syndrome have exaggerated, complex tics, which together
with the other features of the disease can be very disabling. The large
repertoire of tics and the combination of motor and vocal tics
distinguish Tourette syndrome from ordinary tics.
restlessness and urge to move that causes them to remain in almost
constant motion. It occurs most often as a result of treatment with
major psychotropic drugs. A stereotypy is a repetitive, purposeless but
often seemingly purposeful, involuntary, patterned motor activity.
Common foot shaking and other mannerisms are examples of simple
stereotypies. More complex stereotypies may involve ritualistic
behavior, such as the compulsions of obsessive-compulsive disorder.
Stereotypies most commonly occur in psychiatric disorders, but may also
be a part of neurologic disorders, such as tardive dyskinesia and
Tourette syndrome. Hyperekplexia refers to disorders characterized by
an excessive startle response in the absence of other evidence of
neurologic disease, sometimes accompanied by echolalia, automatic
behavior, or automatic obedience. Colorful names have been used for
variants of the condition described in different geographic regions
(jumping Frenchmen of Maine, latah, myriachit).
generally do not occur during sleep. There are some disorders, however,
that occur primarily during sleep. Restless legs syndrome is a common
disorder causing unpleasant and difficult-to-describe sensations in the
legs that are temporarily relieved by movement. The symptoms commonly
occur at night as the patient is drifting off to sleep. Many affected
individuals get up and walk around to obtain respite.
twitching movements due to contraction of a bundle, or fasciculus, of
muscle fibers. They are usually not extensive enough to cause movement
of joints, except occasionally the digits. They vary in size and
intensity, from so faint and small as to only slightly ripple the
surface of the overlying skin, to coarse and impossible to overlook.
They are random, irregular, fleeting, and inconstant. At times they are
abundant; at other times they require a careful search. Fasciculations
always seem to strike where the examiner is not looking, and are
usually seen from the corner of the eye. Fasciculations are brought out
by fatigue and cold. When assessing fasciculations, the patient should
be warm, comfortable, and completely relaxed. Good light is necessary
in order to visualize fasciculations; oblique lighting is best. Many
patients are unaware of fasciculations; others may see or feel them, or
both. Fasciculations continue in sleep. Fasciculations are a
characteristic feature of motor neuron disease. They serve as a very
useful marker for the disease, and the diagnosis should remain
circumspect when fasciculations are not demonstrable. Fasciculations of
small hand muscles in chronic anterior horn cell disease, particularly
spinal muscular atrophy, may cause small amplitude, subtle finger
twitches called minipolymyoclonus (polyminimyoclonus), which are of
course not real myoclonus. Although fasciculations are most
characteristic of motor neuronopathies, they can occur in any chronic
denervating process, including radiculopathy and peripheral neuropathy.
Except for thyrotoxicosis, myopathies generally do not cause
fasciculations. Fasciculations unaccompanied by atrophy or weakness do
not necessarily indicate the presence of a serious disease process.
About 70% of the population, especially health care workers, have
occasional benign fasciculations.
transient, or persistent quivering movements that affect a few muscle
bundles within a single muscle but usually are not extensive enough to
cause movement at a joint. The movements are somewhat coarser, slower,
and undulating (“worm-like”), usually more prolonged, and involve a
wider local area than fasciculations. They usually are not affected by
motion or position, and they persist during sleep. Myokymia often
occurs in normal individuals, causing persistent, focal twitching of a
muscle, most commonly the orbicularis oculi. Myokymia usually occurs in
isolation, without evidence of an accompanying neurologic disease.
Myokymia occurs in a variety of disease states. It may be generalized
or focal/segmental. Focal myokymia is much more common than generalized
myokymia. Myokymia sometimes occurs
in
the facial muscles in patients with MS or other lesions of the
brainstem or cranial nerves. Focal limb myokymia is particularly
characteristic of radiation damage to a nerve or plexus. Generalized
myokymia (Isaacs syndrome) causes generalized muscle stiffness and
persistent contraction because of underlying continuous muscle fiber
activity.
of muscles. The tonic contraction may cause either alteration of
position or limitation of movement. They may occur in almost any
muscle. A painful, tonic, spasmodic muscular contraction is often
spoken of as a cramp. Spasms that limit movement may be defensive or
protective. Spasms are often of reflex origin, due to peripheral
irritation affecting either muscles or nerves. Pain is a common cause
of defensive spasm and reflex rigidity. Carpopedal spasm is a common
manifestation of tetany and hyperventilation.
