Tension Band Wiring of the Patella
accounting for 1% of all fractures. Most of these fractures occur in
patients between 20 and 50 years of age. The incidence in males is
twice that for females. Although the treatment of minimally displaced
patella fractures is relatively straightforward, the treatment of
displaced patella fractures remains controversial. This chapter
discusses open reduction and internal fixation (ORIF) of a displaced
patella fracture using a tension-band wire construct.
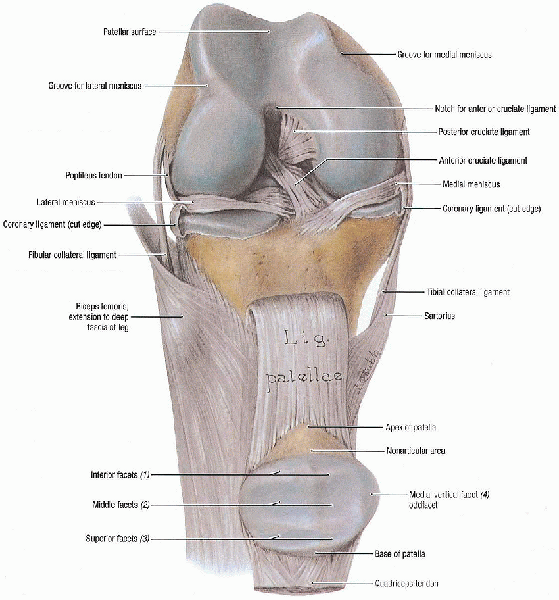
It is subcutaneous, covered only by a prepatellar bursa, a thin layer
of subcutaneous tissue, and skin. It is oval with its apex distal. Most
of the quadriceps aponeurosis inserts onto its proximal pole; its apex
provides the origin for the patella tendon. Posteriorly, the proximal
75% of the patella is covered with articular cartilage that partially
conforms to the articular surface of the distal femur. There are two
major articular facets in the patella, the medial and lateral facets,
separated by the major vertical ridge. There is a second vertical ridge
near the medial border that isolates the odd facet from the medial
facet. The lateral facet is generally the broadest of the three facets,
occupying more than 50% of the articular surface.
descriptive. Fractures are classified as nondisplaced or displaced.
Generally accepted parameters for displacement are a greater than 3-mm
fracture gap or 2-mm articular surface step-off. After the fracture is
defined as nondisplaced or displaced, its pattern is categorized. There
are three major categories of patella fractures: transverse, vertical,
and stellate. Polar fractures are considered transverse fractures. The
base or the apex fragments may be very small, however, and represent
disruption of the quadriceps or patella tendon. Comminuted or stellate
fractures are interchangeable terms, as are the terms vertical,
longitudinal, and marginal fractures. There can be a combination of
fracture patterns in a given injury.
displaced patellar fractures. Displacement more than 3 mm or articular
incongruity of more than 2 mm is considered strong indication for
surgical treatment. ORIF is indicated for displaced patellar fractures
that have fragments large enough to be reduced and stably repaired and
is the treatment of choice for most patellar fractures. Anterior
tension banding is the fixation method most commonly used for patella
fractures; this method converts the tension forces of the extensor
mechanism to compressive forces at the articular surface during knee
flexion. Partial patellectomy is indicated for cases that have severe
comminution of the inferior or superior pole that is not amenable to
ORIF techniques. Total patellectomy is generally indicated when the
patellar is so severely comminuted that a well-reduced and stable
construct cannot be achieved with ORIF.
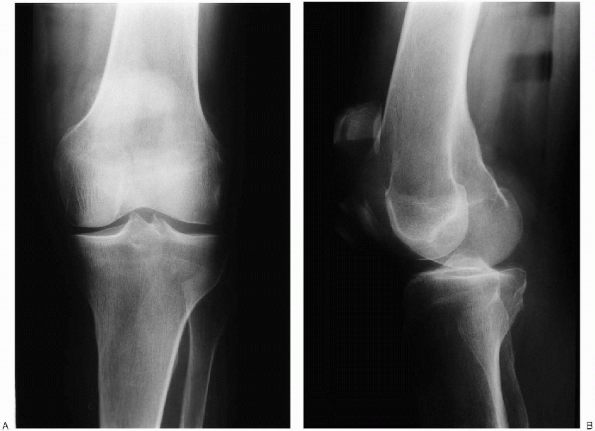
A supine anteroposterior radiograph is obtained, centered over the
patella. Care should be taken to have the patella centered midline on
the femur; this usually requires slight internal rotation of the
extremity. On the anteroposterior view, a
bipartite or tripartite patella can be mistaken for an acute fracture;
these forms represent a failure of fusion of the ossification centers.
These normal variants usually manifest in the superolateral corner of
the patella and are usually bilateral. Comparison views of the other
knee should be taken when there is a question regarding the presence of
a fracture or bipartite patella.
lateral view, with the knee slightly flexed. The lateral view should
include the proximal tibia to exclude tibial tubercle avulsion. The
position of the patella with respect to the femur and the tibia should
be evaluated. Patella baja may indicate a quadriceps tendon rupture,
and patella alta may indicate a patella tendon rupture. The lateral
view is most helpful in quantifying the amount of fracture displacement
and articular incongruity.
to diagnose longitudinal fractures and osteochondral defects. A
tomogram or bone scan can be used to diagnose occult stress fractures.
Computed tomography does not seem to add more information than
conventional radiographs.
 |
|
FIGURE 29-1. Articular surfaces and ligaments of knee joint. (From Agur AMR, Lee MJ. Grant’s atlas of anatomy, 10th ed. Philadelphia: Lippincott Williams & Wilkins, 1999, with permission.)
|
-
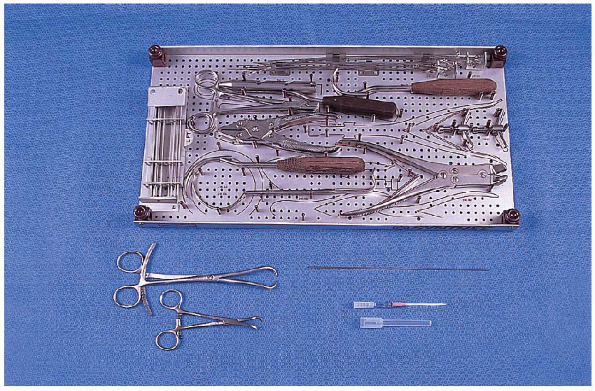
0.062-inch Kirschner wires (K-wires)
-
Wire driver
-
Cerclage wire set
-
14-gauge angiocatheter
-
Large and small, pointed reduction clamps
-
Small fragment set
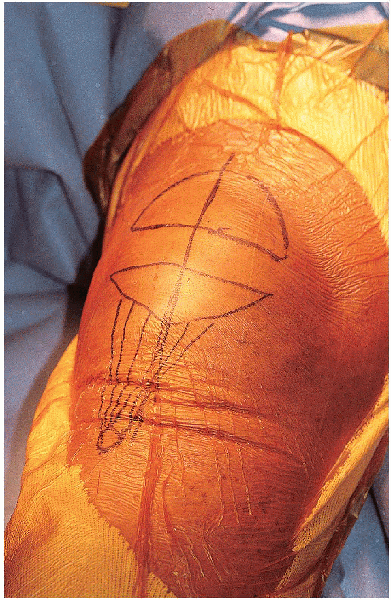
rotate, a small bump can be placed under the ipsilateral hip. The leg
is draped free. Surgery is performed under tourniquet control. Before
inflating the tourniquet, the quadriceps is pulled distally to ensure
that it is not trapped under the tourniquet, which can displace the
patella proximally, making reduction difficult.
 |
|
FIGURE 29-2. Anteroposterior (A) and lateral (B) radiographs show a displaced patella fracture.
|
 |
|
FIGURE 29-3. Equipment for tension band wiring of the patella: top: cerclage wire set; bottom, left to right: small and large pointed reduction clamps, 0.062-inch Kirschner wire, and 14-gauge angiocatheter.
|
 |
|
FIGURE 29-4. Supine patient positioning for open reduction and internal fixation of the patella.
|
incision is carried down through the subcutaneous tissue and through
the prepatellar bursa. The skin incision and approach are facilitated
by slight knee flexion. A hematoma is usually encountered as soon as
the bursa is opened and typically leads directly into the fracture site.
 Care
Careshould be taken to minimize direct dissection of the fracture
fragments. The soft tissues surrounding the patella often hold
nondisplaced fractures in place, and if this arrangement is disrupted,
they may displace,
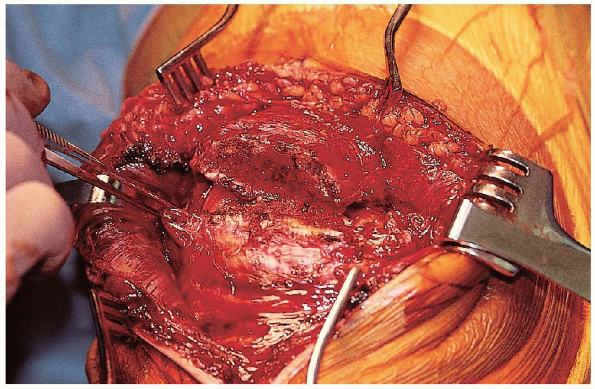
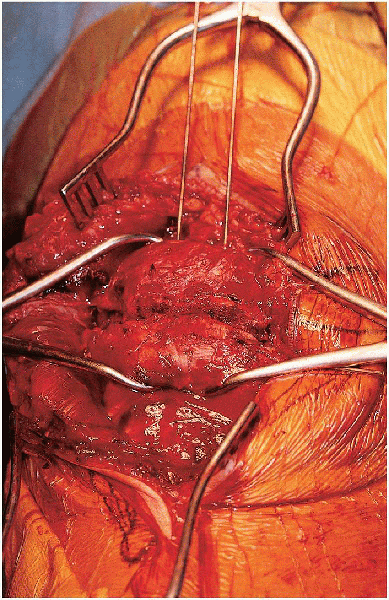
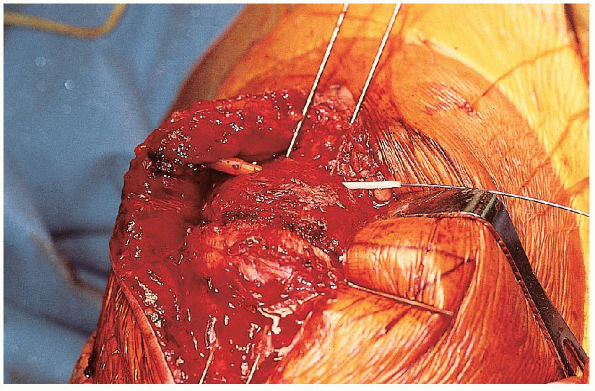
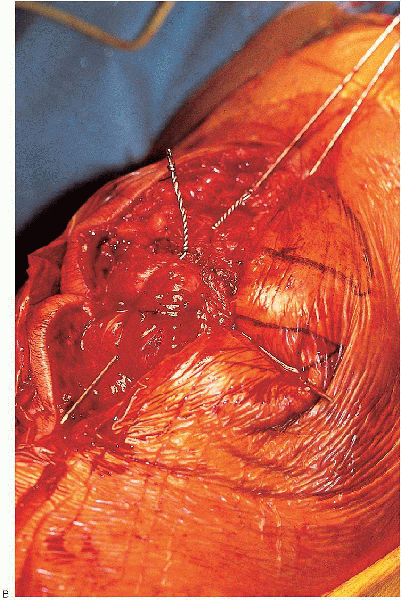
creating a more complicated and unstable fracture pattern. The displaced fracture should be exposed (Fig. 29-6).  Clot should be removed with a combination of small curettes and the use of a small suction-tip device.
Clot should be removed with a combination of small curettes and the use of a small suction-tip device. 
Irrigation should be used liberally to help remove the hematoma and
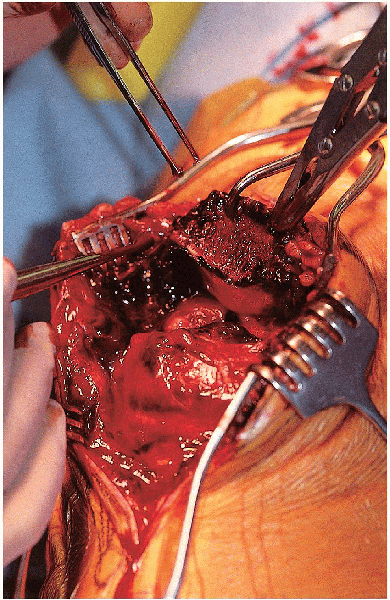
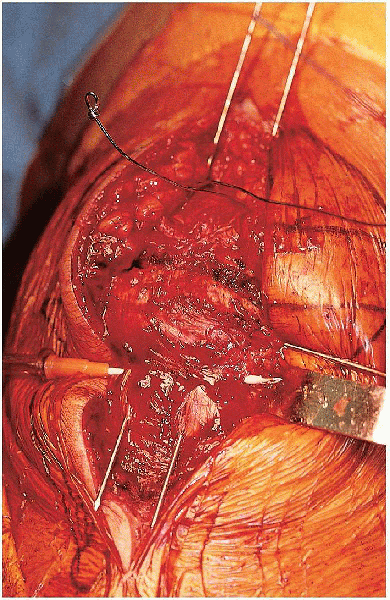
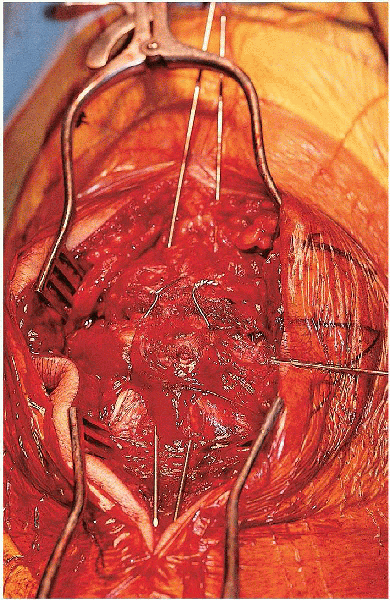
small inconsequential comminuted fragments. The extent of the medial
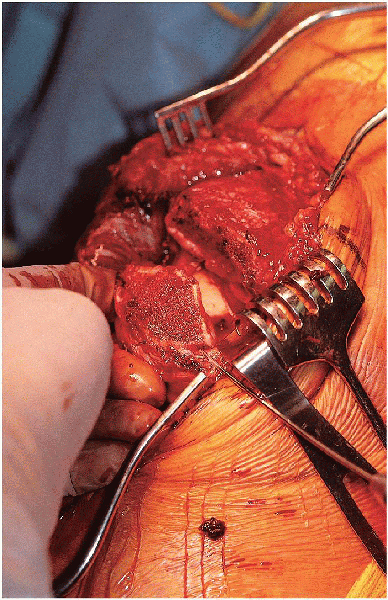
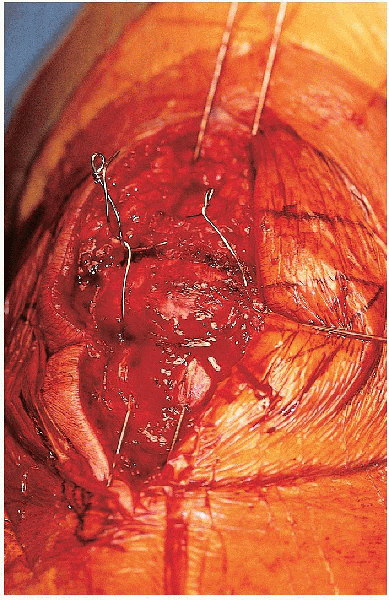
and lateral retinacular injuries should be identified (Fig. 29-7). The undersurface of the patella, in addition to the patella groove, should be inspected for evidence of articular damage (Fig. 29-8). The
knee joint should be inspected and irrigated to remove any loose fragments.
 |
|
FIGURE 29-5. The longitudinal skin incision is centered over the patella.
|
 |
|
FIGURE 29-6. Exposure of the displaced fracture fragments.
|
 |
|
FIGURE 29-7. Identification of the medial and lateral retinacular tears.
|
 |
|
FIGURE 29-8. Exposure of the undersurface of the patella.
|
thoroughly irrigated, the fracture edges carefully exposed, and the
fracture pattern delineated, a preliminary reduction is performed. The
small bump behind the knee needs to be removed at this time, because
flexion of the knee makes reduction more difficult. Fracture
reduction can be facilitated through use of K-wires or tenaculum clamps
positioned in the proximal and distal fragments to act as “joysticks.”
In the case of a simple central transverse fracture, the surgeon can
proceed directly to the tension-band technique. In more complex
fractures, the goal is to try to reduce the fragments to create a
transverse fracture pattern that can then be further stabilized with a
tension-band technique. An example of this is a transverse fracture
pattern that also has a vertical split through the proximal or distal
fragments. The vertical split is first reduced and held temporarily
with a large, pointed reduction forceps. This is then temporarily
stabilized with 1.2-mm K-wires. Definitive stabilization of this
fragment depends on its size and can be with K-wires or small-fragment
or mini-fragment screws. After this has been performed, the tenaculum
clamps and the provisional fixation are removed. The goal is to try to
convert a complex fracture pattern into a simple transverse pattern.
 |
|
FIGURE 29-9. A: Retrograde insertion of a Kirschner wire through the proximal patella fragment. B: Insertion of a second Kirschner wire, parallel to the first wire. C: The two Kirschner wires are driven back until they are flush with the fracture surface.
|
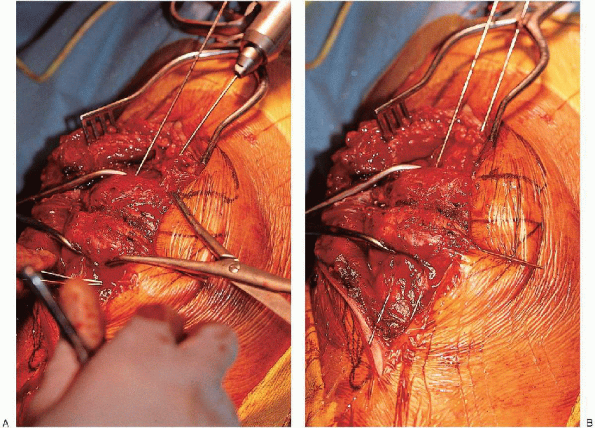
a transverse fracture pattern has been created, a tension-band wire
technique is performed. Two 0.062-inch K-wires are inserted retrograde
through the proximal fragment, perpendicular to the fracture and
parallel to each other (Fig. 29-9).
 The wires should be approximately 5
The wires should be approximately 5mm from the anterior surface of the patella. Anterior placement of
these wires allows a more effective tension band effect. The two
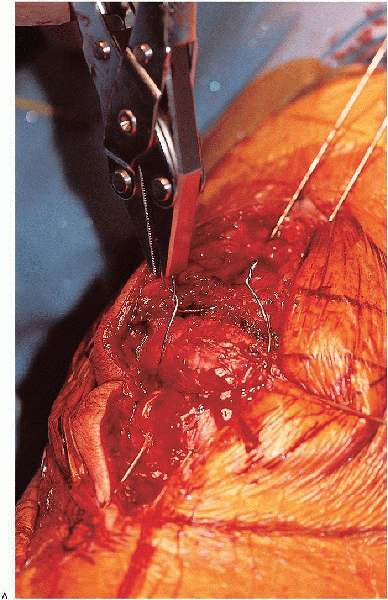
fracture fragments are then reduced and held with a large, pointed
reduction forceps (Fig. 29-10). 
Care should be taken to ensure that the articular surface is
anatomically reduced by inspecting the anterior cortical and posterior
articular surfaces. The articular surface can be inspected through the
preexisting tears in the retinaculum.  If there is no significant tear in the retinaculum, a small medial or lateral arthrotomy should be made to allow
If there is no significant tear in the retinaculum, a small medial or lateral arthrotomy should be made to allow
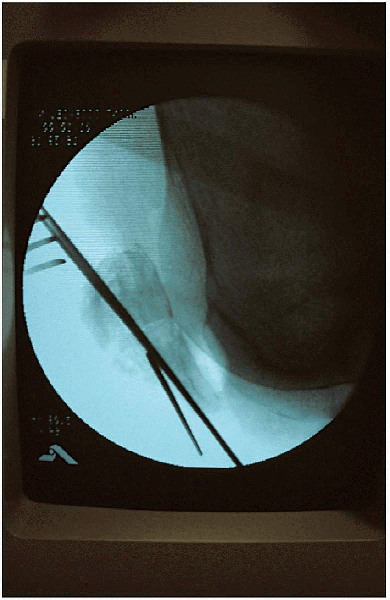
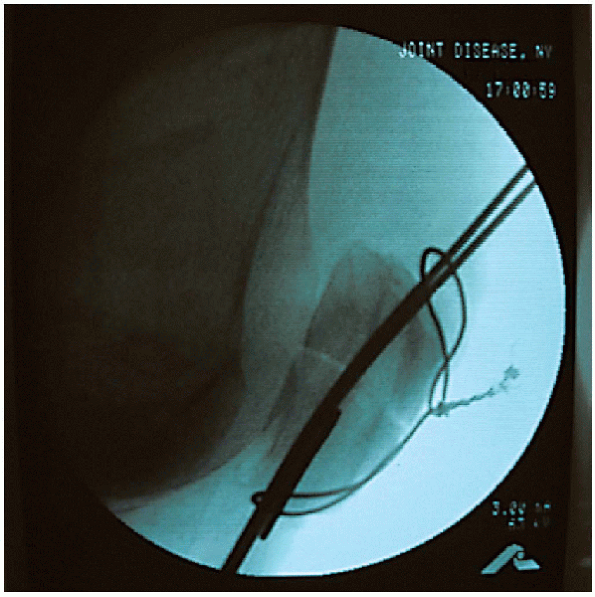
inspection or palpation of the articular surface. The K-wires are then sequentially advanced through the distal fragment (Fig. 29-11). 
They should be advanced distally at least 1 cm beyond the inferior tip
of the patella. The adequacy of the reduction should be checked
clinically and radiographically (Fig. 29-12).
 |
|
FIGURE 29-10. Fracture reduction and provisional fixation using a large, pointed reduction clamp.
|
 A cerclage wire (usually 1.2 mm thick) is threaded through the catheter and used as a tension band (Fig. 29-14). It
A cerclage wire (usually 1.2 mm thick) is threaded through the catheter and used as a tension band (Fig. 29-14). Itis important that the cerclage wire contact the proximal and distal
poles of the patella, without intervening soft tissue; otherwise, with
knee motion, the fragments may slip apart on the K-wires until the
tension band becomes taut. The angiocatheter is then passed deep to the distal end of the K-wires, hugging the patella cortex (Fig. 29-15).
The tension band is crossed anterior to the patella in figure-of-eight
fashion and threaded through the distal angiocatheter.
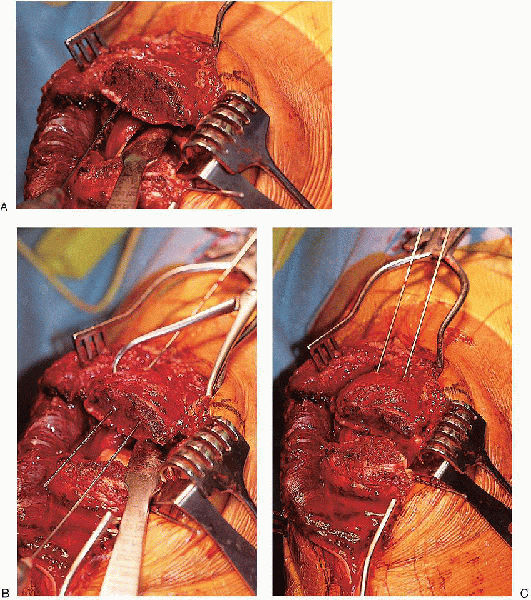
 Two loops are made in the tension band wire, one on either side of the patella (Fig. 29-16). The tension band wire is then tightened by a double knot technique with the knee in extension (Fig. 29-17).
Two loops are made in the tension band wire, one on either side of the patella (Fig. 29-16). The tension band wire is then tightened by a double knot technique with the knee in extension (Fig. 29-17).  Before
Beforetwisting, the wire should be tensioned by lifting up on the clamp. This
ensures that both wires twist around each other rather than one wire
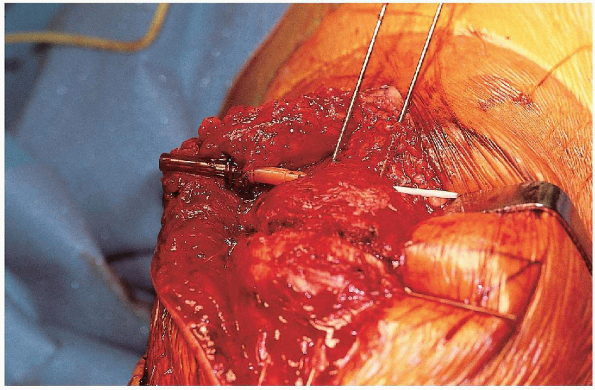
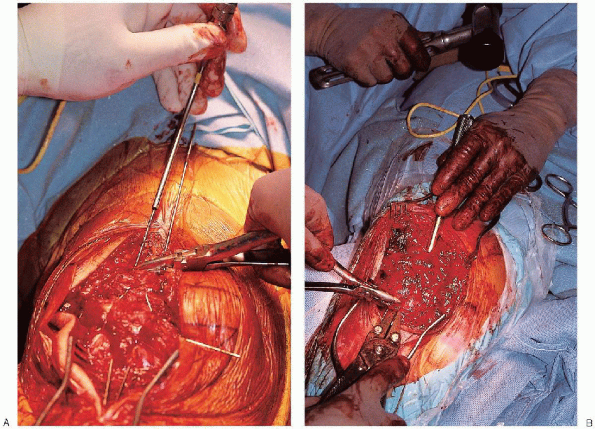
wrapping around the other wire. The reduction should be checked periodically while the wire is being tightened (Fig. 29-18). The knots of the cerclage wire are cut, bent over, and impacted into the bone (Fig. 29-19). The proximal ends of the longitudinal wires are bent over, twisted to face posteriorly, and tapped into the cortex (Fig. 29-20)
 ; the distal ends are flared away from each other and cut below the edge of the patella tendon.
; the distal ends are flared away from each other and cut below the edge of the patella tendon.  If
Ifthe K-wires are not buried deep to the quadriceps mechanism, they will
cause soft tissue irritation and are at increased risk for wire
backout. The distal aspect of the K-wires are flared away from each to
minimize the risk for wire backout; they are not bent as much as the
proximal aspect of the wires to facilitate hardware removal. An additional circumferential wire is used if there are associated longitudinal or stellate fracture lines.
 |
|
FIGURE 29-11. A and B: Advancement of the Kirschner wires across the fracture.
|
the fixation stability, and the quality of reduction and implant position are verified radiographically (Fig. 29-21).
The medial and lateral retinacular defects are repaired and the
remainder of the incision closed in layers. Skin closure depends on the
integrity of the skin. Subcuticular closure gives excellent cosmetic
results but should be reserved for cases without skin injuries and
minimal swelling. If there is concern regarding damage to the skin,
nylon sutures should be used. A sterile dressing is applied consisting
of fluffs, Webril, and an Ace wrap. The leg is placed into a knee
immobilizer.
 |
|
FIGURE 29-12.
Lateral radiograph verifying fracture reduction and implant position. An additional Kirschner wire had been placed in the distal fragment because of a nondisplaced, longitudinal fracture fragment. |
 |
|
FIGURE 29-13. Passage of a 14-gauge angiocatheter deep to the Kirschner wires, hugging the proximal cortex of the patella.
|
 |
|
FIGURE 29-14. Insertion of a cerclage wire through the angiocatheter.
|
 |
|
FIGURE 29-15. Passage of the angiocatheter deep to the distal aspect of the Kirschner wires.
|
fixation stability. In patients with stable fixation, knee motion is
initiated on postoperative day 1 with use of a continuous passive
motion (CPM) machine. The patient is mobilized out of bed to ambulate
while bearing weight as tolerated with the knee in full extension.
Quadriceps strengthening is started in the early postoperative period.
After there is radiographic evidence of healing, progressive
weight-bearing and resistive exercises are started. The patient is
progressively weaned from the brace, depending on the motion and
strength. Full rehabilitation usually takes 4 to 6 months. If there are
any symptoms or signs of loss of fixation during the postoperative
period, range-of-motion exercises are stopped, and the patient is
immobilized and followed closely.
 |
|
FIGURE 29-16. Placement of two loops in the tension band wire, one on either side of the patella.
|
of motion is not possible. The repair should be protected in a knee
immobilizer or a knee brace with the hinges locked. The braces are
removed only for wound checks and extremity cleaning. Quadriceps sets
can be initiated, but the repair is protected until there are signs of
healing. Range-of-motion activity is delayed for 3 to 6 weeks.
 |
|
FIGURE 29-16. (Continued)
|
 |
|
FIGURE 29-17. A and B: Tightening of the tension band wire with the knee in extension.
|
 |
|
FIGURE 29-18. Lateral radiograph verifying fracture reduction and the implant’s position.
|
 |
|
FIGURE 29-19. The cerclage wire knots have been cut, bent over, and impacted into the bone.
|
 |
|
FIGURE 29-20. Bending of the proximal aspect of the longitudinal Kirschner wires (A) and impaction of the longitudinal Kirschner wires deep to the quadriceps (B).
|
 |
|
FIGURE 29-21. Final anteroposterior (A) and lateral (B) radiographs.
|
