Trigger Finger Release
clinical condition characterized by a painful “locking” or “clicking”
of the digit. It can occur in any digit, but most commonly occurs in
the thumb (30% to 60%), followed by the index and ring fingers and,
occasionally, in the little finger. Many conditions have been
associated with “triggering” including rheumatoid arthritis, diabetes,
Dupuytren’s disease, and partial tendon lacerations. In addition, an
infant or toddler may have a congenital trigger digit.
an inner membranous synovial portion and (b) an outer retinacular
pulley portion. The synovial portion has a visceral layer and a
parietal layer. The visceral layer is intimate with the tendon, known
as the epitenon layer, and the parietal layer is the outer layer that
constitutes the synovial pouch.
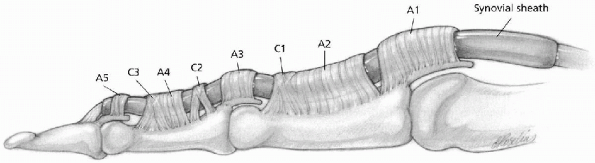
of a series of pulleys or fibrous bands overlying the synovial portion.
The pulleys are named by their shape (transverse, annular, and
cruciate) within a proximal to distal numbering system. Specifically,
there are annular (A) 1 through 5 and cruciate (C) 1 through 3. The
arrangement of the pulleys in a proximal to distal orientation are as
follows: A-1 over the metacarpophalangeal joint, A-2 over the proximal
portion of the proximal phalanx, C-1 at the level of the distal aspect
of the proximal phalanx, A-3 over the proximal interphalangeal joint,
C-2 at the proximal portion of the middle phalanx, A-4 over the middle
portion of the middle phalanx, C-3 at the distal aspect of the middle
phalanx, and A-5 over the distal interphalangeal joint (Fig. 15-1).
The most proximal pulley is a transverse pulley formed by the palmar
aponeurosis. The transverse fascicular fibers of the palmar aponeurosis
that overlie the proximal flexor tendon sheath are anchored on either
side of the tendon to the deep palmar interosseous fascia by thick,
vertical fibrous bands. Consequently, a proximal pulley is formed
around the flexor tendon, approximately 1 cm in length.
 |
|
FIGURE 15-1.
Digital flexor sheath. The digital flexor tendon sheath is composed of synovial (membranous) and retinacular (pulley) tissue components. The membranous portion is a synovial tube sealed at both ends. The retinacular (pulley) portion is a series of transverse (the palmar aponeurosis pulley), annular, and cruciform fibrous tissue condensations, which begin in the distal palm and end at the distal interphalangeal (DIP) joint. The floor or dorsal aspect of this tunnel is composed of the palmar plates of the metacarpophalangeal, proximal interphalangeal, and DIP joints and the palmar surfaces of the proximal and middle phalanges. (From Doyle JR. Hand. In: Doyle JR, Botte MJ, eds. Surgical anatomy of the hand and upper extremity. Philadelphia: Lippincott Williams & Wilkins, 2003:522-666, with permission.) |
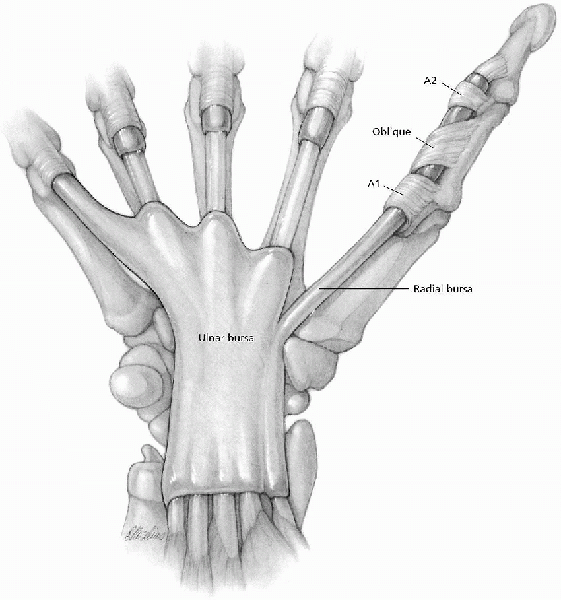
different. The thumb has an A-1 pulley overlying the
metacarpophalangeal joint, followed by the oblique pulley (an extension
of the adductor aponeurosis) over the proximal phalanx and an A-2
pulley. There are no cruciate pulleys (Fig. 15-2).
digit is the A-1 pulley and the palmar aponeurosis. In the thumb, it
consists only of the A-1 pulley. Histologic changes have been shown to
occur in these portions of the retinacular sheath and in the tendon
itself. A normal A-1 pulley has a convex, well-vascularized outer layer
and a concave, avascular inner gliding surface. The inner layer is
fibrocartilaginous, composed of type I collagen, fibroblasts, and
chondrocytes. The number and type of chondrocytes in the A-1 pulley of
a trigger digit is abnormal. The normal A-1 pulley
is
predominately composed of type I collagen, whereas trigger digit
pulleys are composed mainly of type III collagen. Also, the number of
chondrocytes is greatly increased from normal. Hence, the pathology is
a proliferation of chondrocytes not synovial cells.
 |
|
FIGURE 15-2.
The membranous and retinacular components of the synovial sheaths in the proximal fingers, thumb, palm, and wrist. Note that the retinacular portion of the thumb flexor sheath is comprised of only two annular and one oblique pulley. The radial bursa is a continuation of the flexor pollicis longus synovial sheath, which extends from the region of the interphalangeal joint of the thumb to 2.5 cm proximal to the wrist flexion crease. In the index, long, and ring fingers, the membranous portion of the sheath begins at the neck of the metacarpals and continues distally to end at the distal interphalangeal joint. In most instances, the membranous portion of the small finger synovial sheath continues proximally to the wrist. (From Doyle JR. Hand. In: Doyle JR, Botte MJ, eds., Surgical anatomy of the hand and upper extremity. Philadelphia: Lippincott Williams & Wilkins, 2003:522-666, with permission.) |
unclear. Studies have shown that increased compressive forces on
connective tissue can produce fibrocartilaginous metaplasia. With full
finger flexion, the pressure on the A-1 pulley is 500 to 700 mm Hg,
whereas in the neutral position the pressures are only 0 to 50 mm Hg.
The repetitive compressive loads caused by frequent finger flexion may
be the mechanical factor leading to increased chondrocyte
proliferation. A similar metaplasia occurs in the corresponding
adjacent portion of the flexor tendon superficialis with the formation
of Notta’s nodule.
congenital. The acquired trigger digit most commonly occurs in the
fifth or successive decades. There is a predilection for females, with
a 6:1 female to male incidence. Adults (acquired triggers) most often
present with snapping or intermittent locking, especially in the
morning. The patient often complains of pain over the
metacarpophalangeal joint, aggravated with applied pressure on the A-1
while the patient actively flexes and extends the digit. The digit may
“lock” prohibiting active extension of the proximal interphalangeal
joint. In the case of a locked trigger digit, the joints are passively
extended one at a time, beginning with the distal interphalangeal joint
and then the proximal interphalangeal joint. Alternatively, the digit
may become locked in extension not allowing active flexion. This is not
as common, but when it does occur, it is usually in the thumb.
the first pediatric visit or later as the child begins to use his or
her thumbs. Therefore, it is speculated that they are not true
congenital triggers but rather acquired in the first weeks to months.
The frequency of congenital trigger digits ranges from 1 in 2,000
(0.05%) to as high as 1 in 50 (2%). In contrast to adults, children
have an equal distribution by sex and present with a locked digit. The
thumb is the most common in either group, but much more so in children,
especially bilateral trigger thumbs that occur about 25% of the time.
metacarpophalangeal and interphalangeal joints. Anteroposterior (AP),
lateral, and oblique views of the hand and individual digit are
obtained.
-
Lead hand (optional)
-
Small right-angle retractors (at least three)
-
Blunt-tipped dissecting scissors
-
Surgical arm board
-
Tourniquet
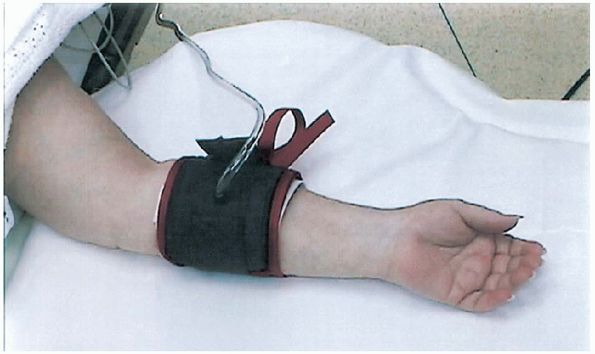
anesthetic with sedation as needed for the patient’s emotional and
physical comfort. The patient is supine on the operating table with his
or her arm comfortably positioned on the hand table, fully supinated (Fig. 15-3).
The digital block is given after the patient is sedated by the
anesthesiologist. The block is performed at the level of the distal
palmar crease in line with the affected digit. The injection site is
prepped with an alcohol swab and the lidocaine is injected into the
tendon sheath and, with a small adjustment of the needle tip, into the
subcutaneous tissue overlying the tendon sheath. A
tourniquet is applied to the forearm, not the upper arm, because it is
less painful for the awake patient to have compression across the
smaller muscle mass of the forearm as opposed to the larger muscle mass
of the upper arm. The tourniquet is usually applied 100 mm Hg
above the patient’s systolic blood pressure (about 250 mm Hg). The hand
is then prepped as to the surgeon’s preference. Perioperative
antibiotics are usually not required in surgery of the hand that
involves only the soft tissues unless the patient is immunocompromised
(i.e., diabetic, immune deficiency disease, steroid use), but this is
governed by the surgeon’s preference as well. Depending on the
patient’s degree of sedation, the hand may be positioned in the lead
hand for
control of the other digits and elimination of sudden movements.
 |
|
FIGURE 15-3. Patient position.
|
 |
|
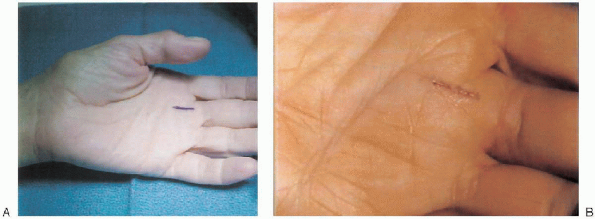
FIGURE 15-4. A: Guide for palmar incision. B: Longitudinal skin incision for middle-digit trigger release.
|
skin incision at the level of the A-1 pulley parallel to the distal
palmar crease. The A-1 pulley is then divided longitudinally. However,
the principle of an extensile approach is not easily performed using
this type of incision. A more pliable incision is a longitudinal skin
incision over the A-1 pulley located between the distal palmar crease
and the proximal digital crease (Fig. 15-4). Care
must be taken not to extend the incision into either the distal palmar
crease or the proximal digital crease, because this would violate the
rule of never crossing a crease at a right angle and may lead to
contractures. The palmar skin has multiple longitudinal skin
creases that can be used as a guide for the incision, and, thus,
cosmetic scarring is reduced.
single incision through the skin is followed by dissection straight
down to the tendon sheath with a pair of blunt-tipped scissors. The
neurovascular bundles lie parallel and on either side of the tendon
sheath. To protect the neurovascular bundles, the dissection is
performed with the scissor tips positioned perpendicular and directly
over the tendon, with spreading performed in a longitudinal fashion
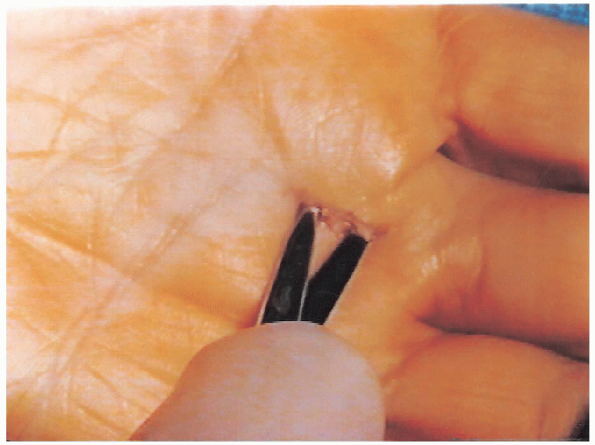
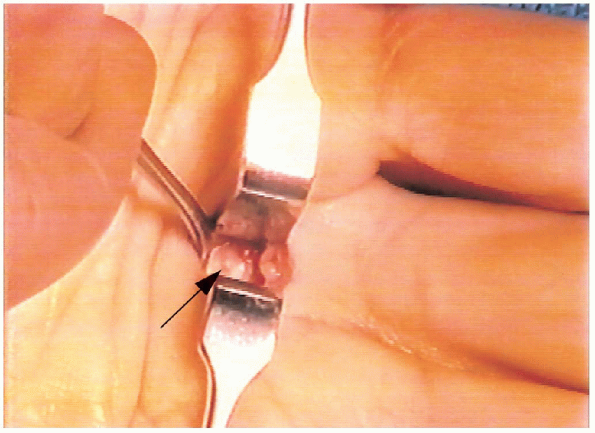
only (i.e., in line with the course of the tendon) (Fig. 15-5). Also, blunt retractors are placed to hold the subcutaneous fat aside, along with the neurovascular bundles. As long as the dissection is maintained over the tendon, the bundles are protected. This technique allows easy and full visualization of the A-1 pulley for a complete release (Fig. 15-6). The pulley is incised longitudinally up to the level of the A-2 distally.

The proximal subcutaneous tissue is dissected by spreading above and
below the palmar aponeurosis. The palmar aponeurosis is seen as white
fibrous bands fanning out above the tendon. This transverse pulley is
incised bluntly with the scissors.

 |
|
FIGURE 15-5. Longitudinal dissection performed perpendicular to and directly over the tendon.
|
the A-1 pulley. This decision is governed solely by surgeon’s
preference unless a retinacular cyst exists. If this is the case,
the
cyst with the pulley should be excised and sent to the pathology
department. Also, occasionally there is an abundance of tenosynovium
present on the tendons, which may be excised and sent to the pathology
department as well.
 |
|
FIGURE 15-6. Visualization of the A-1 pulley. Note retinacular cyst (arrow) on A-1 pulley of flexor tendon sheath.
|
 |
|
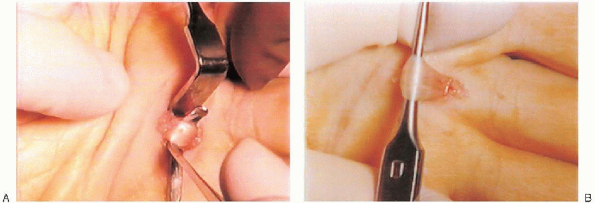
FIGURE 15-7. A: A retractor is passed beneath the flexor digitorum superficialis tendon. B: The retractor is used to gently elevate the tendon to lyse adhesions.
|
the pulley is released, the flexor digitorum superficialis (FDS) tendon
is clearly seen with the flexor digitorum profundus (FDP) tendon lying
beneath.

Occasionally, adhesions between these tendons occur and must be lysed.
A right-angle retractor is passed beneath the FDS tendon (Fig. 15-7A), and the tendon is gently pulled up and out of the incision to separate it from the FDP tendon (Fig. 15-7B). One
must check that both slips of the FDS tendon are retracted, because the
FDS divides into Campers’ chiasm at this level. Extreme care must be
taken that the neurovascular bundles are not accidentally retracted out
of wound during this step. The finger is passively extended at the proximal interphalangeal joint while maintaining traction on the FDS tendon.

Often, the lysis of the adhesions is audible. Finally, because this
procedure is often performed with local anesthesia, the patient is
asked to actively flex the affected finger to confirm full resolution
of the tendon locking.
the neurovascular bundles and the initial skin incision. The common
digital nerve of the thumb arises from the radial division of the
median nerve and lies on the superficial surface of the flexor pollicis
brevis before it divides into the ulnar and radial digital nerves. The
ulnar branch continues along its distally directed course up the ulnar
border of the thumb, whereas the radial digital nerve must cross
superficial to the flexor pollicis longus (FPL) tendon to reach the
subcutaneous tissue on the radial side of the thumb. This
crossing occurs just beneath the deep dermis at the level of the
metacarpophalangeal crease, leaving the radial digital nerve prone to
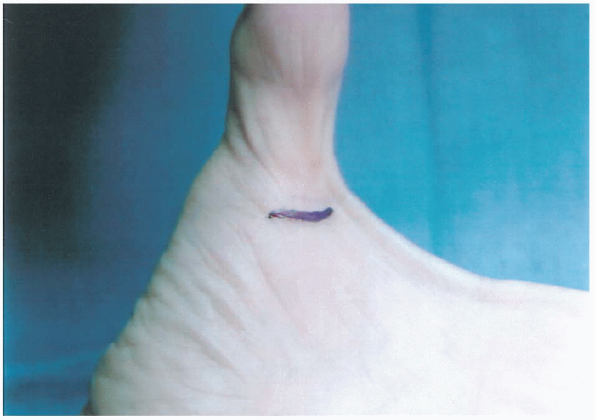
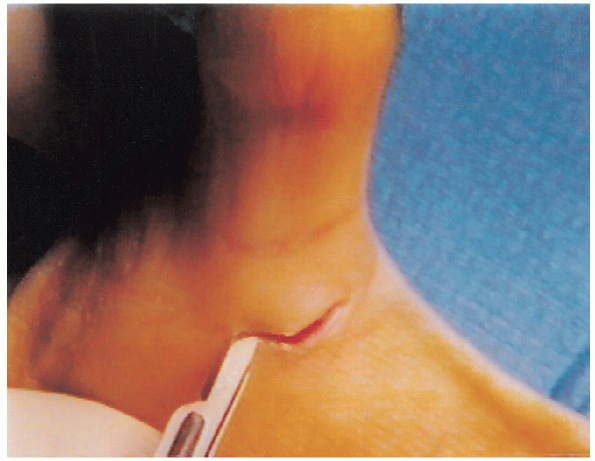
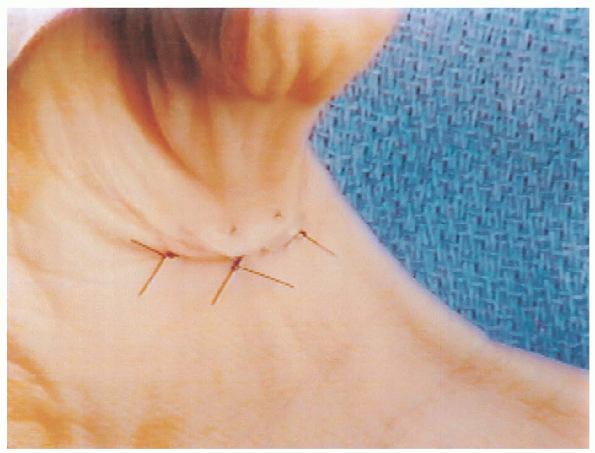
injury. A transverse incision is recommended at the thumb digital crease to limit the vulnerability of the radial digital nerve (Figs. 15-8 and 15-9).
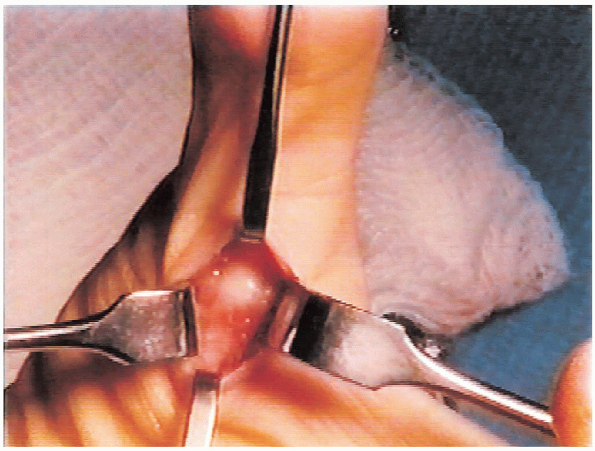
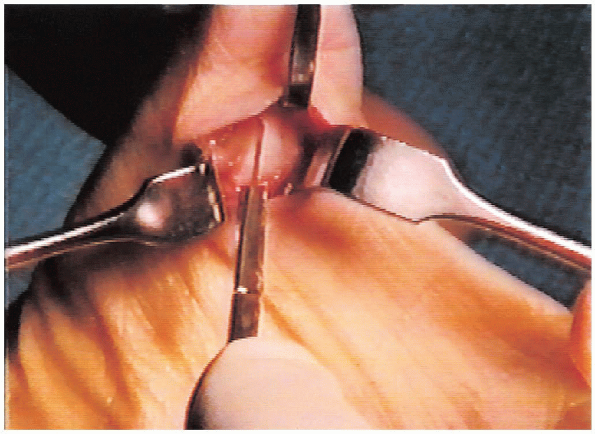
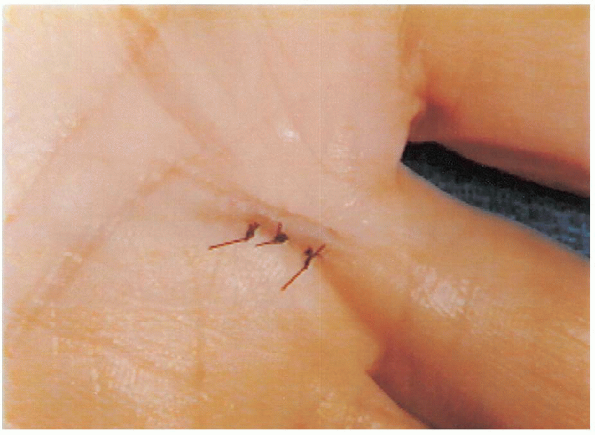
Similar to a trigger finger, dissection is performed longitudinally
over the FPL tendon with the neurovascular bundles retracted on either
side (Fig. 15-10). The A-1 pulley is then released in a longitudinal fashion (Fig. 15-11). 
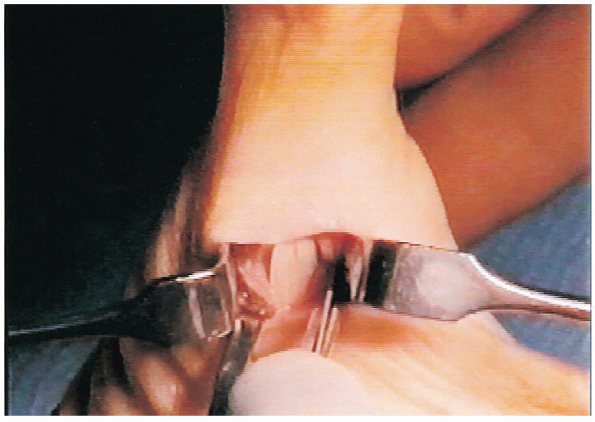
There is no need to manually retract the FPL tendon because there is
only one tendon present in the sheath, unlike a trigger finger and,
therefore, no intertendinous adhesions to lyse (Fig. 15-12). 
 |
|
FIGURE 15-8. Guide for thumb incision.
|
 |
|
FIGURE 15-9. Incision on left trigger thumb.
|
 |
|
FIGURE 15-10. Flexor pollicis longus tendon in sheath.
|
 |
|
FIGURE 15-11. Incising A-1 pulley.
|
 |
|
FIGURE 15-12. Flexor pollicis longus tendon as viewed after incision of the A-1 pulley.
|
 |
|
FIGURE 15-13. Skin closure of thumb after trigger release.
|
 |
|
FIGURE 15-14. Skin closure of middle digit after trigger release.
|
 |
|
FIGURE 15-15. Final postoperative dressing after release of thumb and middle-digit triggers.
|
 |
|
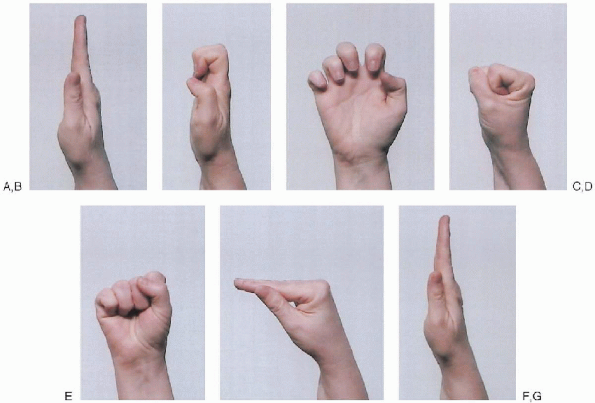
FIGURE 15-16.
Stretching exercise called “tendon gliding” (see video for correct motion sequence). Points to remember for different positions: (A) start with fingers pointing straight-up; (B) “curl” fingers until the tips touch the palm (lateral view); (C) palmar view; (D) roll knuckles all the way down into a tight fist; (E) palmar view; (F) maintain straight fingers; and (G) extend fingers fully. Repeat exercise 10 times, at least six times per day, until full motion returns. |
All the other digits and the proximal interphalangeal joint of the
involved digit should remain free with unobstructed motion.
patient is encouraged to use the fingers immediately following surgery
and as much as possible postoperatively but to keep the dressing clean
and dry. The patient returns to the office 1 week later for dressing
and suture removal. All patients require postoperative therapy but may
not require a therapist. The patient is taught to massage the
incisional scar and to perform range of motion and stretching exercises
(Fig. 15-16)

and gradual strengthening exercises. Depending on the patient, a
therapist may be required to assist in these therapeutic exercises.
