SURGICAL MANAGEMENT OF DEGENERATIVE SCOLIOSIS
VIII – THE SPINE > Spinal Deformity > CHAPTER 160 – SURGICAL
MANAGEMENT OF DEGENERATIVE SCOLIOSIS
the adult secondary to degenerative disc disease. It may be difficult
in many cases to determine whether scoliosis is arising de novo
or if patients had mild to moderate degrees of scoliosis that became
symptomatic or progressed late in adulthood. The treatment of
degenerative scoliosis follows many of the same principles as the
treatment of adult idiopathic scoliosis, however, so the distinction in
many cases may be moot. This chapter discusses the factors that should
be considered in treating patients with this condition.
not progress, and they may not be symptomatic. With more advanced
disease, axial pain and neurogenic claudication are typical symptoms.
As with any degenerative spine disease, facet hypertrophy, diffuse disc
bulges, disc degeneration, and narrowing and redundant ligamentum
flavum can result in spinal stenosis and produce symptoms of neurogenic
claudication and radiculopathy (25). The degree
of compression can be aggravated in the presence of lateral listhesis
or spondylolisthesis, by traction on the nerve roots.
another occurs in the coronal plane, appears to correlate with a
greater risk of curve progression (25,27).
Significant lateral listhesis, particularly when it occurs at multiple
adjacent levels, can result in significant truncal imbalance with
resultant pain and fatigue. In many patients, these symptoms can be
managed conservatively with anti-inflammatories, physical therapy, and
epidural steroids. With progression of the patient’s curvature,
however, failure to respond to conservative measures or significant
compromise of the patient’s quality of life may call for consideration
of surgical intervention.
Risk factors for curve progression include curve magnitude greater than
30°, osteoporosis, and lateral listhesis or rotatory spondylolisthesis (9,14).
Prior decompressive surgery, such as a laminectomy, can increase curve
progression as well, sometimes secondary to development of a
postsurgical fracture of the pars interarticularis and
spondylolisthesis. Rapid progression of scoliosis in a patient with a
prior laminectomy is highly suspect for a pars fracture, which should
be sought in the workup of such a patient.
with a lateral wedge component may aggravate or cause development of
scoliosis. These patients may have a relative loss of lumbar lordosis
as well. Patients with lateral listhesis appear to be at greater risk for curve progression (25,27),
and, in addition, they are subject to traction on their nerve roots at
the involved levels. Asymmetric wear on the facet joints may contribute
to facet arthropathy, leading to central or foraminal stenosis.
Although most patients present with pain secondary to nerve root
compression, others present with weakness. Pain and weakness may be
particularly intractable from severe disc space collapse, with or
without listhesis, and decreasing space between the adjacent pedicles
results in foraminal stenosis. Patients with stenosis secondary to
degenerative scoliosis suffer a similar pathophysiology as a cause of
their neurogenic claudication—namely, a vascular insufficiency to the
neural elements secondary to the stenosis, which is generally worsened
by lumbar extension.
claudication occur in similar patient populations, and it is important
to distinguish the true cause of the patient’s leg pain. A careful
history, palpation of distal pulses, examination of feet and skin, and,
if indicated, referral to a vascular specialist may be needed. In
general, neurogenic claudication is improved by forward flexion of the
spine, including sitting, and it may be worse going downhill because
hyperextension is necessary (see Chapter 147).
However, at least some patients with stenosis secondary to degenerative
scoliosis have reported that their extremity symptoms are not reliably
relieved by forward flexion (11).
according to the conditions that cause the most symptoms. For example,
the patient with more back pain secondary to the degenerative disease
can be managed successfully using nonsteroidal anti-inflammatories,
rest, physical therapy, cardiovascular conditioning, and, occasionally,
bracing. Patients with neurogenic claudication may respond to any of
these measures but may receive relief from epidural cortisone
injections. Bracing can be used on occasion for the patient with mild
degenerative scoliosis with back pain only. Rigid bracing has not been
shown to prevent progression in adults with scoliosis. However, bracing
may be a reasonable alternative for a patient who has a degenerative
scoliosis with mild to moderate progression, but who is medically
unable to tolerate a major reconstructive procedure.
orthosis for more severe scoliosis or kyphosis, or it may simply be a
lightweight, corset-type brace for milder curves. However, since
symptom improvement is the primary goal, rather than curve control,
results with a specific patient will be the final determining factor.
neurologic deterioration are the main indications for surgical
intervention. In general, bracing in adults is discouraged because it
does not halt progression and may result in patient dependence on the
brace and associated trunk deconditioning. However, in certain cases,
such as an elderly patient who is too ill to tolerate a major surgical
procedure, or a patient whose severely osteoporotic bone is too weak to
support instrumentation, bracing may slow progression or attenuate the
pain symptoms.
improved by stabilization and fusion of her degenerative scoliosis can
be difficult. Once surgery has been deemed likely to help such a
patient, however, choice of the fusion levels requires consideration of
curve pattern, sagittal and coronal balance, pain locale, levels
needing decompression, and the presence of degenerated or listhetic
levels, as well as patient expectations and activity levels. Facet
blocks, discography, and nerve root blocks may be helpful in
determining symptomatic levels, although their predictive value for
fusion surgery has not been proven. Grubb et al. (12)
used provocative discography to help determine fusion levels in adult
scoliosis patients (degenerative and idiopathic) and felt that this
aided them in their surgical planning. However, in their study, all
positive discograms were at morphologically abnormal levels, and it is
not clear whether they might have included such levels based on
radiographic or magnetic resonance imaging (MRI)–determined
degenerative levels. Fortunately, fusion for back pain secondary to
scoliosis appears more predictable than fusion for back pain secondary
to degenerative disc disease without deformity. We do not routinely
perform discography in these patients, because it
has not proven of benefit in predicting the outcome of fusion surgery.
claudication should have their stenosis decompressed concurrently with
stabilization of the curvature. In most patients, an MRI will give
adequate information for localization of stenotic levels; in some
patients, however, the lateral deformity or rotatory component
precludes clear delineation of the anatomy. In these cases, computed
tomography (CT) or myelography is indicated for preoperative planning.
neurogenic claudication, and only mild degrees of scoliosis, it may be
reasonable to address the compressive symptoms with laminotomy,
laminectomy, or foraminotomy as needed. Aggressive decompression can
result in curve progression; this isolated procedure should be reserved
for milder cases in which limited decompression can be expected to help
the patient. Be sure the patient understands the possibility of curve
progression and recurrence of symptoms.
alone may be sufficient. The majority of patients with degenerative
scoliosis will require instrumentation and grafting to achieve fusion
over multiple segments that require stabilization. Because of the
increased pseudarthrosis rate with multiple-level fusions, it is rare
to have a patient who can be managed without instrumentation. However,
certain older patients, particularly the medically fragile, may better
tolerate laminectomy and limited uninstrumented fusion (i.e., at the
level where there is a degenerative spondylolisthesis). In some
patients, moderate to severe osteoporosis may preclude fixation, but,
as with laminectomy alone, there is a risk of curve progression and
recurrence of symptoms. Therefore, this approach is limited to patients
who clearly understand the limitations of what surgery can accomplish
for them and are willing to risk recurrent symptoms. In general, we
have not found age or osteopenia to be a contraindication for fusion
with instrumentation.
several factors. The levels that should be fused should include at
least the entirety of the symptomatic curve, but often additional
levels must be included to address symptomatic degenerative levels and
permit maintenance or restoration of coronal and sagittal balance.
Generally, preoperative bending films can help predict the amount of
correction that can be obtained after exposure, facetectomy, and
application of appropriate corrective forces. The end vertebra,
particularly distally, should be a vertebra that is level on side
bending. Sagittal balance is exceedingly important to consider,
particularly because many of these patients have osteoporosis. Most
degenerative curves are kyphotic; if the kyphosis is not flexible, a
combined anterior–posterior approach may be indicated to achieve
sagittal realignment and successful arthrodesis. It is also important
not to end the fusion at a kyphotic segment. Many of these patients
have lumbar or thoracolumbar curvatures, and including only the major
curve often can result in ending the fusion at the mid or lower
thoracic spine—in the middle of the kyphosis. Such patients are at
considerable risk for development of progressive junctional kyphosis,
and in general it is best to include the minor compensatory thoracic
curve and end the fusion at the end vertebra of the kyphosis (usually
T-4 or T-5).
nonkyphotic thoracolumbar junction can the fusion safely stop at the
thoracolumbar junction. Choosing the distal end vertebra can be
difficult in the patient with degenerative scoliosis and low back pain.
Deciding whether L-4–L-5 and/or L-5–S-1 is symptomatic is crucial
because long fusions to the sacrum generally necessitate combined
anterior and posterior surgery and have a higher rate of complications.
Not including a symptomatic level will result in limited pain relief,
however, and thus it will decrease the success of the surgery. In
addition, fusions ending at L-4 or L-5 are at risk for development of
symptomatic degeneration below the fusion. This development 5–10 years
after the surgery may be acceptable for the older patient, but its
occurrence 2 years or so after the surgery is not. Therefore, consider
whether a more distal fusion is indicated. Involvement of the
lumbosacral region is very common in degenerative scoliosis, and the
majority of these patients require combined anterior and posterior
spinal fusion to the sacrum.
hook-and-rod systems are preferred for instrumentation of degenerative
scoliosis. These systems allow much better correction of coronal and
particularly sagittal plane deformity. However, such surgery is
technically demanding, and the surgeon must have a clear understanding
of the corrective forces that should be applied and how they affect the
patient’s curvature, coronal balance, sagittal balance, and shoulder
obliquity. The following considerations are important:
-
It is rare to be able to perform rod rotation in the patient who has degenerative scoliosis.
-
If the patient has significant
osteoporosis, and multiple-level laminectomy is not required for
coexisting spinal stenosis (see below), consider using sublaminar wires
supplemented by hooks and/or pedicle screws at strategic levels
(generally the end vertebra of each curve and sometimes the apical
vertebra as well). Such wires are quite easy to attach to rods and, for
an osteoporotic patient whose trabecular bone has numerous vascular
channels, their use can potentially decrease operative time and
therefore decrease blood loss. -
Do not affix rods to end vertebrae with
sublaminar wires, because wires do not provide axial control of the
spine and can allow axial collapse and subsequent junctional kyphosis.
Use pedicular fixation or hook combinations at the ends of constructs
to decrease the likelihood of this problem. -
To ensure coronal balance, we prefer to
obtain intraoperative long radiographs of the entire spine after the
correction has been partially or completely performed. Adjustments in
the corrective forces can be made at this time if desired. -
Although in situ
bending to fine-tune the coronal balance can be performed in some adult
scoliosis patients, most patients with degenerative scoliosis have
osteoporotic bone, and in situ bending can result in loss of fixation.
spinal stenosis as part of their degenerative process. As part of
preoperative planning, evaluate with an MRI or CT/myelogram any patient
with degenerative scoliosis who notes leg pain or buttock pain. As
previously noted, the MRI is adequate for many patients; with greater
degrees of curvature, however, CT/myelography gives better bony detail
and permits better understanding of the anatomy in the presence of the
curvature. It is important to identify symptomatic levels of stenosis
so that decompression can be performed at the time of posterior fusion.
In most cases, this can be determined anatomically according to
dermatomal levels and nerve root distributions; however, occasionally,
selective nerve root injections may be needed to determine which levels
with mild to moderate degrees of stenosis are the symptomatic ones.
pedicle screw instrumentation may be needed to attain fixation.
Generally, fusion rates are improved with instrumentation, particularly
in patients with conditions such as degenerative scoliosis (13).
As with deformity surgery in general, try to visualize the medial wall
of the pedicle before screw placement, to correctly account for spinal
rotation. This is a simple matter after laminotomy or laminectomy has
already been performed. Frazier et al. (8)
reported on patients who underwent decompression for spinal stenosis,
including 19 who had at least 15° of scoliosis preoperatively. The
majority of their patients with scoliosis did not have fusion performed
at the time of decompression. They found that a greater degree of
preoperative scoliosis was associated with less improvement in back
pain. We have not found curve severity to correlate with outcomes of
reconstructive surgery in these patients. We do take a more aggressive
approach, however, preferring to fuse patients with scoliosis who are
undergoing a laminectomy even if the underlying medical condition
permits only limited fusion.
with degenerative scoliosis will require anterior and posterior
procedures to achieve fusion, as well as coronal and sagittal balance.
There are several indications for combined techniques in this complex
patient population.
-
Inflexible sagittal-plane imbalance is
one of the most common indications for combined surgery. Relative
lumbar kyphosis must be corrected to achieve sagittal plane balance.
The use of structural allografts facilitates the restoration of lumbar
lordosis. We favor femoral allografts, packed with autogenous
cancellous graft; Harms-type mesh cages with autograft may also be
used. Consideration of the scoliotic deformity is necessary; otherwise,
mere placement of the structural grafts on the side of the
approach—usually the curve convexity—will limit correction of the
scoliosis. -
Degenerative curves of significant
magnitude, especially with limited flexibility, may also require
combined surgery. Coronal imbalance may also indicate the need for
combined surgery. -
Patients who require a long fusion to the
sacrum should also have a combined procedure because posterior fusion
alone in this setting has a high incidence of failure (4,12).
Most of these patients have significant degeneration across the
lumbosacral junction, and many also have thoracolumbar kyphosis (which
is a contraindication for ending the fusion at the thoracolumbar
junction), so combined surgery is frequently indicated. -
In patients who have had failed posterior instrumented fusions, consider combined surgery. We and others (1,10,23) have found iliac fixation in the form of Galveston rods or iliac screws to be useful for achieving distal
P.4119
fixation (Fig. 160.1).
For patients with reasonable bone quality, anterior structural
allograft at the lumbosacral junction coupled with sacral screws alone
that penetrate the anterior cortex may be adequate. Others (2,7,16,17) have used iliosacral screws or intrasacral screws (Jackson technique) for distal fixation.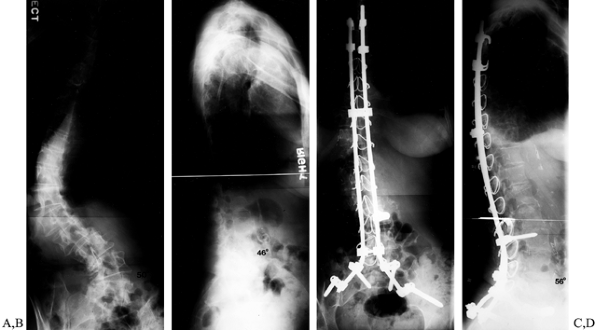 Figure 160.1.
Figure 160.1.
This 71-year-old woman was first diagnosed with scoliosis at age 45. In
the 5 years previous to presentation at this institution, she developed
increasing low back pain and increasing prominence of her right hip.
Anteroposterior (A) and lateral (B)
standing radiographs demonstrate degenerative scoliosis with collapsing
curve. The patient underwent a staged anterior and posterior spinal
fusion, T-5 to the sacrum; the posterior fusion included multiple
sublaminar wires and iliac screws. Her postoperative course had some
brief episodes of cardiac ectopy and a urinary tract infection.
Postoperative radiographs (C,D) demonstrate
correction of the deformity, with coronal and sagittal balance
achieved. At 2-year follow-up, she was doing well, with excellent
improvement of her function and marked pain relief.
fixation is preferred for combined surgery in this patient population.
Sublaminar wires may be used as a component of the fixation, but use
fixed components (hooks in a claw construct in the mid and upper
thoracic spine, pedicle screws at the thoracolumbar junction) at the
proximal end of the construct to decrease the risk of junctional
kyphosis.
procedures under a single anesthetic to lower overall incidence of
complications, nutritional depletion, and blood loss (5,21,24).
Older patients, particularly those with coexisting medical conditions
or significant osteoporosis, may be less able to tolerate the lengthy
anesthetic, however. Older patients with significantly osteoporotic
bone may experience increased blood loss, which can lead to development
of a coagulopathy during a prolonged procedure.
cannot be completed in 8–10 hours, then stage the procedure. The
scheduled delay between stages may be 3–7 days, depending on coexisting
medical conditions, the age of the patient, and scheduling issues. The
occurrence of complications, however, may further delay the
second-stage procedure.
depletion, which may lead to an increased incidence of infection,
pneumonia, and urinary tract infection (5,21,24). We have shown that, particularly in the older patient population, use of total parenteral nutrition may decrease the
rate of nutritional depletion, which may in turn decrease the risk of complications (15).
average of 70% reduction of pain in patients fused for painful
degenerative scoliosis, which is somewhat less than that seen for
patients fused for painful adult idiopathic scoliosis (80% pain relief).
-
Perform a standard thoracoabdominal or
retroperitoneal approach on the convexity of the curve to be addressed.
Be sure to prep down to the pubic symphysis if L-5–S-1 is to be fused,
as is the case in most of these patients. -
Identify segmental vessels and ligate or
clip. Sweep the psoas muscle posteriorly, using bipolar cautery to
control bleeding. Use blunt but careful dissection to sweep the great
vessels forward. The common iliac will need to be mobilized if L-4–L5
or L-5–S-1 is to be exposed. This generally requires ligating the
recurrent lumbar vein. -
Incise the disc space with a #11 blade.
Use a rongeur to remove loose disc material, and a rongeur or osteotome
to remove the osteophyte so that the endplate can be visualized. Peel
the disc from the endplate using a Cobb elevator—exercise care in
patients with osteoporosis. -
Remove additional disc material with a
curved or straight curette, supplementing with a rongeur. A Blount
spreader may be used with care to keep the disc space from collapsing
in the convexity. The release must extend across to the contralateral
annulus. If there is significant kyphosis, divide the anterior
longitudinal ligament. -
The distalmost levels generally are in
the fractional curve and also are most important for maintaining
lordosis. Therefore, placement of the structural allograft should not
block correction. If disc spaces in the convexity are to be placed,
take care to place them as far toward the concavity as possible; do not
place so large a graft that correction is blocked. For disc spaces that
are not to receive structural allograft, pack morcelized cancellous
bone lightly within, preferably autograft, although allograft can be
used. -
Measure the height of the disc space to
be filled with allograft. We use femoral shaft pieces cut at the time
of surgery to fit the evacuated disc space. (Other surgeons prefer mesh
cages.) The graft should be snug but not overly tight; that is, the
release should open the disc space, not the graft itself. After
confirming the size, fill the marrow cavity of the femoral allograft
with rib graft or local bone graft, or morcelized cancellous allograft,
and impact gently into place. Forcing an overly large graft or
inadequate release will result in graft breakage (with high risk for
pseudarthrosis) or endplate fracture (with increased risk for
subsidence). -
Use interference screws to prevent
allograft migration. Place a 6.5 mm cancellous screw with a plastic
washer lateral to the graft, into the vertebral body. Alternatively, a
long enough screw can be placed lateral to the adjacent graft,
skewering the graft below, to prevent migration of two allografts. It
may be necessary to burr a small impression into the lateral aspect of
the adjacent allograft to allow the washer to seat snugly. Although
theoretically possible, we have not generally found that these screws
impair our ability to place pedicle screws during the posterior
instrumentation. Since instituting the use of these interference
screws, we have not needed to replace anterior structural allograft.
-
Osteoporotic bone is nearly always
present and its vascular channels can contribute to greater bleeding
rates than seen in the patient with normal bone. -
Many of these patients may have chronic
hypertension, coronary artery disease, or other vascular conditions
that contraindicate or limit the use of controlled hypotension to
decrease surgical blood loss. -
One must select fusion levels carefully. Ending the fusion at a kyphotic level can lead to junctional kyphosis.
-
Although sublaminar wires may be
preferred in many patients because their use spreads corrective forces
over many levels, they should not be used at the end vertebra because
they do not control the spine in the axial plane; they may also result
in junctional kyphosis. Use hooks or screws at the ends of the
construct. -
Overcorrection of the curve may lead to truncal imbalance, which, if significant, may require revision surgery.
-
Patients who undergo fusion surgery are
at risk for developing degeneration above or below the fusion. Consider
including severely degenerated adjacent levels to avoid rapid
development of this problem. Extending the fusion should be balanced by
the consideration of how much surgery should be done on the older, less
healthy patient. -
Although osteoporotic patients have not
been shown to have a higher rate of pseudarthrosis, poorer fixation due
to poor bone quality, combined with autogenous bone graft from a site
with more fat infiltration and fewer osteoprogenitor cells, is of
concern.
undergoing spinal surgery is about 60% (6,12,18,19,22).
Although the rate is not significantly greater with increasing age
(60–70 years, 70–80 years), there is no doubt that older patients are
less able to tolerate complications and recover quickly from them. Keep
this in mind when planning the surgery. We have shown that older
patients may be more at risk for development of complications such as
pneumonia and urinary tract infections, particularly if they are
undergoing staged surgery. Consider nutritional supplementation to
decrease their risk of nutritional depletion (15).
Thromboembolic disease leading to pulmonary embolism occurs more
commonly in older patients, particularly after combined anterior and
posterior surgery (3). Our current practice is
to use elastic stockings and sequential compression boots for
prophylaxis of deep venous thrombosis. We remain vigilant in patients
who have combined surgery, but we do not routinely anticoagulate these
patients.
published studies in this patient population include small numbers of
patients, we estimate it to be 1% to 5%. Discuss fully the numerous
potential risks of spinal surgery with the patient, as well as her
family, if desired, when she is offered any spinal surgery.
suggested that endoscopic surgery, both thoracoscopy and lumbar
endoscopy, may result in lower morbidity and decreased length of
hospital stay (20,26).
Unfortunately, such techniques are difficult to learn and have not yet
been proven to demonstrate comparable fusion rates to that achieved in
open procedures. In general, for degenerative scoliosis, the indicated
anterior procedure is in the lumbar or lumbosacral spine. Currently,
most of the lumbar endoscopic techniques have concentrated on
screw-in–type cages, which are not well suited for degenerative
scoliosis because of the presence of multiplanar deformity.
scoliosis is complex and requires a thorough understanding of a
multitude of factors, including pain sources, coronal and sagittal
balance, fusion techniques, indications for decompression, indications
for combined anterior and posterior surgery, and instrumentation
choices, as well as the potential for complications. With appropriate
patient selection, however, and realistic expectations of surgery on
the part of both the patient and the surgeon, the majority of patients
will have a satisfactory outcome.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
O, Dendrinos G, Ogilvie J, et al. Management of Adult Spinal Deformity
with Combined Anterior-posterior Arthrodesis and Luque-Galveston
Instrumentation. J Spinal Disorder 1991;4:131.
JF, Caudle R, Ashmun RD, Roach J. Immediate Complications of
Cotrel-Dubousset Instrumentation to the Sacro-pelvis: A Clinical and
Biomechanical Study. Spine 1990;15:932.
D, Lipson S, Fossel A, et al. Associations between Spinal Deformity and
Outcomes after Decompression for Spinal Stenosis. Spine 1997;22:2025.
S, Fontaine F, Kelley B, et al. Nutritional Depletion in Staged Spinal
Reconstructive Surgery: The Effect of Total Parenteral Nutrition. Spine 1998;23:1401.
RP, Ebelke DK, McManus AC. Clinical Results and Standing Radiographic
Sagittal Plane Analysis in Spondylolisthesis Insrumented to the Sacrum
with New Techniques. Orthop Trans 1995–1996;19:593.
BR, Tolo VT, McAfee PC, Burest P. Nutritional Deficiencies after Staged
Anterior and Posterior Spinal Reconstructive Surgery. Clin Orthop 1988;234:5.
ET, Krengel WF, King HA, Lagrone MO. Comparison of Same-day Sequential
Anterior and Posterior Spinal Fusion with Delayed Two-staged Anterior
and Posterior Spinal Fusion. Spine 1994;19:1256.
J, Ben-Yishay A, Mack M. Video-assisted Thoracoscopic Excision of
Herniated Thoracic Disc: Description of Technique and Preliminary
Experience in the First 29 Cases. J Spinal Disord 1998;11:183.
