Partial Thickness Rotator Cuff Tears: Diagnosis and Treatment
III – Shoulder Reconstruction > Part B – Evaluation and Treatment of
Shoulder Disorders > 38 – Partial Thickness Rotator Cuff Tears:
Diagnosis and Treatment
tears is poorly understood. To begin with, two types of tears need to
be considered. Specifically, there are bursal surface tears, whose
history and treatment is relatively well-known and straightforward. The
second type is an articular side tear, whose history, diagnosis, and
treatment are not as clear-cut. It has only been since the advent of
shoulder arthroscopy and increasing diagnostic abilities with MRI that
we have been able to make the diagnosis. The few series available with
respect to the treatment of this problem are sometimes contradictory.
The largest issue is that the natural history of partial cuff tears is
relatively unknown. Furthermore, as with many shoulder injuries, the
patient becomes more symptomatic with increasing activity levels or
demands placed on the injured shoulder. The treatment of this problem
is certainly different in a professional baseball pitcher as compared
with a middle-aged weekend athlete.
partial-thickness tears are on the articular side. When
partial-thickness tears are openly explored, significant delamination
can be encountered, with the articular surface fibers demonstrating the
greatest degree of damage. Most degenerative tears originate on the
articular side of the supraspinatus tendon, near the insertion, and
appear to be primarily from intrinsic tendinopathy and not secondary to
anatomic variations or wear from contiguous structures. This finding
may be owing to the poor blood supply of the articular side of the
supraspinatus insertion. Codman first observed a hypovascular critical
zone just proximal to the insertion of the supraspinatus tendon in
1934. It has subsequently been corroborated that the articular side of
the supraspinatus insertion has only sparse vascularity, with almost no
vessels; the bursal side, however, was well vascularized. This critical
zone of ischemia on the articular side seems to correspond well with
the common site of rupture of the tendon. The relative ischemia of this
area may be one reason why the cuff is unable to repair itself.
this hypovascular zone. This area corresponds well with the crescent
described by Burkhart. Immediately medial to this well-defined area of
degeneration one can often see the rotator cable, a consistent
thickening in the tendon. Typically, the tissue that makes up the cable
and all tissue medial to that point is intrinsically healthy. The loss
of this crescentic area is perhaps a normal part of aging, and its
presence does not necessarily indicate a repairable lesion. Most
patients can still elevate their arm with this defect since stress
transmission occurs through the cable. This may explain why a
significant percent of all tears of the rotator cuff are asymptomatic.
is in a key position and is therefore susceptible to overuse and
injury. Given the hypovascularity of the tissues, it is not surprising
that most tears originate in this tendon. When eccentric tensile
overload occurs at a rate that is greater than the ability of the
rotator cuff to repair itself, injury occurs. At some point weakness of
the musculotendinous unit results in damage to the tendon and
ultimately failure. Direct trauma to the shoulder may initiate the same
process. A weak, fatigued, or injured rotator cuff is unable to oppose
the superior pull of the deltoid effectively and keep the humeral head
centered on the glenoid during elevation
of
the arm. This leads to inappropriate superior migration of the humeral
head with active elevation of the arm, functionally narrowing the
subacromial space. Continued dysfunction of the rotator cuff and
further superior migration of the humeral head cause abutment against
the undersurface of the acromion and the coracoacromial ligament,
leading to signs of secondary impingement.
|
TABLE 38-1 Classification of Partial Rotator Cuff Tears
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
degenerative osseous changes. This process of secondary impingement
further damages the already injured and weakened cuff. Subacromial
impingement does occur, but in most circumstances it is a secondary
phenomenon.
full-thickness rotator tears. Most focus on the size of the tear and
offer some prognostic criteria following repair. The classification
scheme used for partial-thickness tears is somewhat different in that
it takes into account the status of both the articular and bursal sides
of the tendon.
Orthopedic Institute (SCOI) classification. The scheme separates tears
into articular (A), bursal (B), and complete (C) types. The degree of
tendon damage is further separated into degree of tearing on a
numerical scale of 0 to 4. The grading begins with 0, which is a normal
cuff, and culminates with grade 4 (Table 38-1).
When recording a tear, all three areas are represented even if they are
normal. For example, an A1/B2/C0 tear would be understood as a partial
articular-sided tear with minimal fraying in a localized area with the
bursal side having cuff fiber failure and bursal injury, extending
<2 cm. Finally, despite the degree of injury on both sides, there is
no complete tearing, hence the C0 designation.
commonly seen entity has recently been termed a PASTA lesion, which is
an acronym for a partial articular supraspinatus tendon avulsion. These
are the injuries that will be discussed more thoroughly in this chapter
as they are typically more symptomatic than the bursal-side tears,
which are more common in sedentary and typically older individuals.
one who is relatively active in an overhead sport or a manual laborer.
In most cases, the onset is insidious and does not present with much
acute symptomatology. In many, the symptoms are initially vague and are
more often stamina issues rather than inability to perform at a high
level.
Patients are often vague about the time of onset of symptoms and the
inciting event. Pain needs to be evaluated for quality, location, and
duration of symptoms. Actions that worsen symptoms and interventions
that improve them are important variables. The timing of onset of pain
(how many tosses and at what velocity before symptoms occur), the point
in the throwing cycle at which symptoms are greatest, and past history
of treatment and prior shoulder problems should be elicited.
<45 years of age. In many overhead athletes, the history includes a
lack of ability to participate at high levels for prolonged periods of
time. A baseball pitcher, for example, would typically state that he is
able to throw effectively for a few innings, but then his speed and
control will start to decrease considerably more quickly than in the
past.
and subacromial impingement, these patients are unlikely to complain of
significant night pain. They typically have no resting pain and are
unlikely to need treatment if they do not participate in the offending
activity.
any patient with shoulder pain is to evaluate both sides for symmetry
(or lack thereof) and for scapulothoracic dyskinesia, which can be a
subtle finding. Males should be examined with their entire upper body
exposed, whereas women should be examined with either a tube top or a
gown that allows visualization of both shoulders and scapulae. It is
important to examine all of the anatomic areas of the shoulder when
diagnosing a partial rotator cuff tear, especially as it relates to the
possibility of subtle instability or labral tears. There is a high rate
of concomitant labral injuries (especially Superior Labrum, Anterior to
Posterior Tear [SLAP]) in patients with partial tears.
cuff tear can be unimpressive, despite later finding a very significant
tear on diagnostic imaging. Typically, the patient has a full passive
and active range of motion with the exception perhaps of a limitation
in internal rotation in high-level throwers. It is important to assess
both shoulders for range of motion, especially at the extremes of
internal and external rotation. Most patients do not have any
significant scapulothoracic asymmetry.
significant partial tears are weakness with forward flexion, adduction,
and internal rotation. This tends to put the leading edge of the
supraspinatus on tension and is a sensitive indicator of continuity of
this portion. Another test that may be positive is pain with 90 degrees
of abduction with resistance. This test may actually reproduce the pain
that many throwers experience in their motion. Since the typical
complaints are of pain in the posterior aspect of the shoulder in the
late cocking and early acceleration phases of throwing, placing the
shoulder into 90 degrees of abduction, 15 to 20 degrees of forward
flexion, and maximum external rotation will recreate the symptoms. A
test is considered positive when it recreates complaints of pain that
are well localized in the posterior aspect of the shoulder. This test
has high sensitivity for diagnosis of partial-thickness undersurface
tears of the rotator cuff or posterior labrum. The traditional
supraspinatus examination with the arm forward flexed about 30 degrees
and the hand in a neutral position is typically nondiagnostic in these
patients.
impingement signs are usually negative. There may be some focal
tenderness over the greater tuberosity at the leading edge of the
supraspinatus, but that is difficult to elicit in a well-muscled
athlete.
 |
|
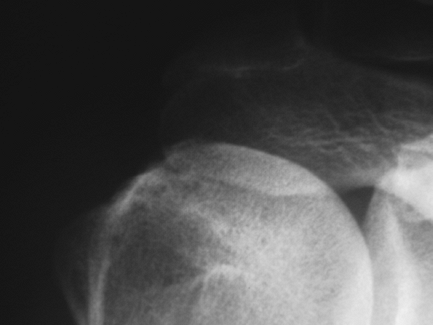
Figure 38-1 Radiograph depicting greater tuberosity sclerosis in a patient with a 75% full-thickness supraspinatus tear.
|
scapular anteroposterior (AP), an outlet view, and an axillary
projection. Occasionally, a specific acromioclavicular joint view is
also warranted. In most cases, the radiographs are normal. The most
frequent positive findings are an area of greater tuberosity sclerosis
or perhaps cysts over the area of the tear (Fig. 38-1).
These areas usually correspond to the areas of tendon avulsion and
indicate the chronicity and repetitive nature of the injury.
it is typically not helpful in these partial tears. As with most
arthrograms (and ultrasound), the technique is definitely operator
dependent and the sensitivity varies depending on the experience of the
technician.
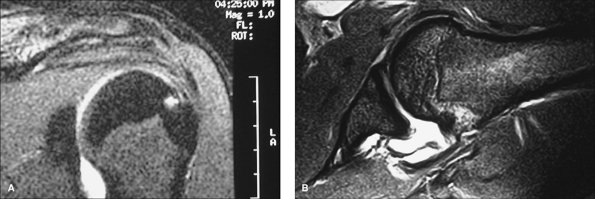
with a gadolinium arthrogram. These lesions are typically not seen on
traditional MRI studies performed and as such should be highly
suspected in a patient with the proper history and examination
findings. Not only does the arthrogram portion improve the
visualization of the rotator cuff pathology, but it also helps the
evaluation of the labral structures that are frequently injured in
these patients.
to consider the inclusion of a series that positions the arm in an
abducted and externally rotated position. It is not rare to see what
appears to be a small and insignificant tear become a rather large tear
with this maneuver (Fig. 38-2).
there is usually no significant retraction and, more important, no
significant muscle atrophy or fatty infiltration. This is an important
consideration, as either of these findings will significantly impact
the patient’s recovery following a surgical repair.
partial-thickness tear have included one that is >50% of the full
thickness of the involved tendon, with lesser tears requiring only
debridement of the frayed tissue. Most studies have indicated that the
supraspinatus footprint is between 12 and 16 mm long such that a tear
>6 to 8 mm thick is an indication for surgery. The determination of
the size of the tendon is difficult to make preoperatively based on MRI
findings alone. It is therefore important to discuss this with each
patient and make sure that the treatment alternatives are understood.
Namely, that in tears that involve <25% of the footprint, a simple
debridement and correction of any associated lesions may be all that is
required. In addition, the determination of the degree of weakness
preoperatively is important. In those patients in whom the clinical
examination showed significant weakness and <25% of the tendon
appears to be involved at the time of arthroscopy, the decision may be
to repair the tear. The concept of individualizing the treatment based
on the patient’s age, activity level, and desire to return to the prior
level is extremely important.
these patients is that the natural history of the problem is poorly
understood. The typical young, active patient who is a repetitive
thrower and is unable to participate at the desired activity level
makes the problem easy to manage because any partial tear that makes
throwing ineffective following a concerted conservative course of
rotator cuff strengthening and pain control should undergo surgical
repair. Patients who are more sedentary, or whose activity level is
minimally affected, present a diagnostic dilemma, since the natural
history of the progression of these partial tears into full-thickness
tears
is
not completely known. However, cadaveric studies have shown that most
partial-thickness tears are articular sided, and mechanical testing on
these partial tears has led to complete disruption in a great
percentage of samples. Although the correlation between cadaveric
studies and in vivo pathophysiology is not always direct, it is
important to consider this point in significant partial tears or in
those unresponsive to conservative measures.
 |
|
Figure 38-2 A: Coronal MRI (T2) view of a patient with clinical signs consistent with a partial rotator cuff tear. B: MRI (T2) view in abduction and external rotation depicting a near full-thickness tear of the supraspinatus.
|
intervention in a patient who meets the criteria described above. One
important consideration is that the patient must have full passive
range of motion. There may be some minor limitations in active motion
especially at the extremes of internal and external rotation. Any
significant limitation, however, should be dealt with preoperatively
with passive stretching. A significant limitation that is not resolved
with aggressive conservative modalities preoperatively may require a
capsular release. This is especially common in throwing athletes in
whom the particular motion that is restricted is internal rotation.
recently expanded as a result of the use of the arthroscope. With that
in mind, most algorithms include the use of the arthroscope to make the
diagnosis, especially those tears that are on the articular side. The
treatment of outer surface tears can certainly be undertaken without
the arthroscope with a traditional open technique, although as
previously mentioned, there is a significant likelihood that a
concomitant intra-articular surgical lesion exists, most commonly a
labral tear. If the surgery is performed in an open fashion, the
intra-articular visualization is at the very least compromised.
techniques that use suture anchors for solid cuff fixation. Two
techniques are commonly used. One is the transtendon technique in which
the remaining rotator cuff material is left intact and the tear is
fixed with suture anchors placed through small incisions in the cuff.
The other technique involves completion of the tear followed by
arthroscopic repair (identical to what is performed in full thickness
tears). The general guidelines for one technique over the other include
the use of the transtendon technique in those tears where >75% of
the tendon is intact. In tears where a larger portion of the tendon is
involved, the tear is completed and a standard arthroscopic repair is
performed. These are guidelines only, and the treatment should be based
on the individual physician’s experience with each technique.
lateral decubitus position for shoulder arthroscopy with hypotensive
anesthesia. The transtendon repair technique is used in most cases, as
this preserves a more significant portion of the normal rotator cuff
and recreates the original footprint more effectively.
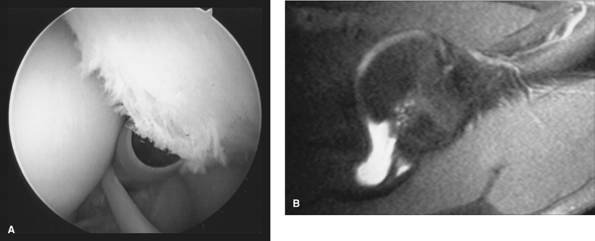
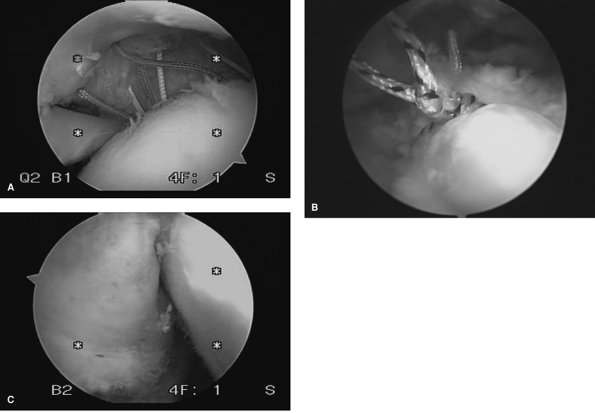
tear is delineated arthroscopically. The entire visualized cuff should
be palpated and delineated for any significant intrasubstance
delamination (Fig. 38-3).
A spinal needle is now inserted from the lateral aspect of the joint
into the area of the tear. The needle is then threaded with a large
suture that can easily be found in the subacromial space. The
subacromial space is then entered and the suture tag is found. A
determination of the degree of bursal-sided tearing, if any, is made.
If significant bursal tearing is noted, then a decision should be made
to complete the tear and treat it in the standard fashion for a
full-thickness tear.
bursectomy is performed in anticipation of a transtendon repair and
consequent suture tying in the subacromial space. If a complete
bursectomy is not performed, significant difficulty will be encountered
in the final stages of the repair as suture tying becomes very
difficult without complete visualization. Once the subacromial space is
cleared and any
osteophytes or coracoacromial pathology is addressed, the glenohumeral joint is then re-entered.
 |
|
Figure 38-3 Intrasubstance delamination of a rotator cuff. A: MRI (T1) view of an inner surface delamination. B: Intra-articular visualization of this significant lesion.
|
 |
|
Figure 38-4
Preparation of the cuff tissue and the footprint of a partial-thickness tear. Right shoulder, posterior portal view. Note the anchor already in place at the anterior edge. |
 |
|
Figure 38-5 Suture penetrator being used for grasping a suture directly from the anchor after piercing the rotator cuff tissue.
|
needle localization of the appropriate spot for suture anchor placement
is now performed. In general, the traditional rule of thumb of one
anchor per centimeter of tearing in the anterior to posterior dimension
is followed. The appropriate number of anchors is then placed by making
one longitudinal incision in the remaining cuff (parallel to the fibers
of the tendon) just large enough to accommodate the suture anchor. In
most cases, only one cuff incision is necessary, since the humerus can
be rotated to position the anchors appropriately in the tuberosity. As
the anchors are placed in the tuberosity, the sutures are pulled out of
the anterior portal. All of the sutures are pulled out through this
portal prior to beginning suture passing through the cuff.
are now passed through the tissue. Various suture-passing devices are
available for this process, and they include needle-type devices with
various curvatures and cannulated centers that allow suture shuttling
through the appropriate point in the cuff. In addition, other
penetrating devices allow for piercing the cuff tissue directly and
grasping the suture (Fig. 38-5).
with the technique is to advance a larger amount of cuff than is
necessary, thus effectively overtensioning the cuff and leading to
later excessive limitation of motion. It is important to gauge the
amount of tissue that is taken with each suture and allow for a
comfortable recreation of the footprint without undue tension following
knot tying.
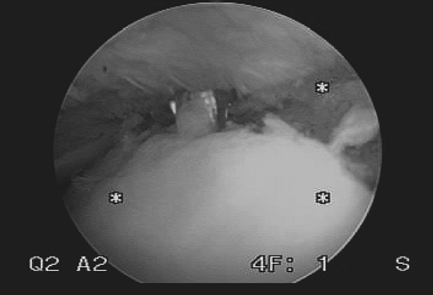
space is again visualized from posterior and the knots are tied in a
methodical fashion from anterior to posterior (Fig. 38-6). The basic principles of knot tying should be followed, namely a sliding locking knot that is backed up with reverse
half hitches. In addition, only one pair of sutures should be in the
portal while tying is taking place at any one time to avoid tangling of
sutures.
 |
|
Figure 38-6 Sutures passed following anchor insertion (Right shoulder, posterior portal view). A: Intraarticular visualization of the final suture position. B: Subacromial visualization of the final sutures. C: Final intraarticular visualization of the cuff repair.
|
immobilized in a sling for 4 weeks with the institution of early elbow
and hand range of motion exercises. During the second week, pendulum
exercises are begun and gradually increased in range and frequency with
a minimum of pain. The maximum forward flexion at this point (until 6
weeks postoperative) is kept to <90 degrees. At 6 weeks, the patient
is allowed to begin active elevation and strengthening as tolerated.
Typically a throwing program is instituted at 4 months. This is
predicated on a complete range of motion and at near-complete (grade
4+/5) strength in all of the rotator cuff muscles and deltoid. Full,
unrestricted activities including throwing are allowed at 6 months
postoperatively.
articular-sided tear in an active individual is likely to progress.
Furthermore, simple acromioplasty does not predictably return the
athlete to any semblance of his or her prior activity. The best results
attained with partial-thickness tears have been in those cases where a
repair has been performed. Several series delineate the arthroscopic
evaluation and debridement of these tears with an acromioplasty. These
have uniformly shown a lower rate of return to high-level activities as
compared with series of repairs, regardless of the technique chosen. Up
to 94% satisfactory results have been reported with arthroscopic
decompression and mini-open rotator cuff repair.
different in that many of these cases have a mechanical cause such as a
prominent anterior acromion. In those cases, a debridement of the tear
and subsequent acromioplasty may be of benefit in many patients. In
general, the patients with this injury tend to be older and less
active. Although degenerative labral tears are often encountered, these
typically do not need any surgical fixation, unlike the patients with
articular-side tears.
SS. Arthroscopic debridement and decompression for selected rotator
cuff tears. Clinical results, pathomechanics, and patient selection
based on biomechanical parameters. Orthop Clin North Am 1993;24:111–123.
SY, Lee JK. Horizontal component of partial-thickness tears of rotator
cuff: imaging characteristics and comparison of ABER view with oblique
coronal view at MR arthrography initial results. Radiology. 2002;224:470–476.
ES, Snyder SJ. Arthroscopic management of partial, full thickness and
complex rotator cuff tears: indications, techniques and complications. Arthroscopy. 2003;66:304–312.
